Search
- Page Path
- HOME > Search
- Primary Merkel cell carcinoma of the salivary gland: a clinicopathologic study of four cases with a review of literature
- Gyuheon Choi, Joon Seon Song, Hee Jin Lee, Gi Hwan Kim, Young Ho Jung, Yoon Se Lee, Kyung-Ja Cho
- J Pathol Transl Med. 2025;59(3):171-179. Published online April 30, 2025
- DOI: https://doi.org/10.4132/jptm.2025.03.25
- 3,561 View
- 153 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Primary Merkel cell carcinoma of the salivary gland is currently not listed in the World Health Organization classification. However, cases of Merkel cell type neuroendocrine carcinomas of the salivary gland with perinuclear cytokeratin 20 positivity have been intermittently reported. We here investigated the clinicopathologic features of additional cases.
Methods
Data of four cases of Merkel cell type small cell neuroendocrine carcinoma of the salivary gland were retrieved. To confirm the tumors’ primary nature, clinical records and pathologic materials were reviewed. Optimal immunohistochemical staining was performed to support the diagnosis.
Results
All tumors were located in the parotid gland. Possibilities of metastasis were excluded in all cases through a meticulous clinicopathological review. Tumor histology was consistent with the diagnosis of small cell neuroendocrine carcinoma. Tumors’ immunohistochemical phenotypes were consistent with Merkel cell carcinoma, including Merkel cell polyomavirus large T antigen positivity in two of the four cases.
Conclusions
Merkel cell carcinomas can originate in salivary glands and are partly associated with Merkel cell polyomavirus infection as in cutaneous Merkel cell carcinomas. -
Citations
Citations to this article as recorded by- Parotid intranodal metastasis of Merkel cell carcinoma: a rare case report
Tong Gao, Dengshun Wang, Hongwei Yu, Yu’e Wang, Haibin Lu
BMC Oral Health.2025;[Epub] CrossRef
- Parotid intranodal metastasis of Merkel cell carcinoma: a rare case report
- Exploring histological predictive biomarkers for immune checkpoint inhibitor therapy response in non–small cell lung cancer
- Uiju Cho, Soyoung Im, Hyung Soon Park
- J Pathol Transl Med. 2024;58(2):49-58. Published online February 26, 2024
- DOI: https://doi.org/10.4132/jptm.2024.01.31
- 9,349 View
- 344 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Treatment challenges persist in advanced lung cancer despite the development of therapies beyond the traditional platinum-based chemotherapy. The early 2000s marked a shift to tyrosine kinase inhibitors targeting epidermal growth factor receptor, ushering in personalized genetic-based treatment. A further significant advance was the development of immune checkpoint inhibitors (ICIs), especially for non–small cell lung cancer. These target programmed death-ligand 1 (PD-L1) and cytotoxic T lymphocyte antigen 4, which enhanced the immune response against tumor cells. However, not all patients respond, and immune-related toxicities arise. This review emphasizes identifying biomarkers for ICI response prediction. While PD-L1 is a widely used, validated biomarker, its predictive accuracy is imperfect. Investigating tumor-infiltrating lymphocytes, tertiary lymphoid structure, and emerging biomarkers such as high endothelial venule, Human leukocyte antigen class I, T-cell immunoreceptors with Ig and ITIM domains, and lymphocyte activation gene-3 counts is promising. Understanding and exploring additional predictive biomarkers for ICI response are crucial for enhancing patient stratification and overall care in lung cancer treatment.
-
Citations
Citations to this article as recorded by- Machine learning methods for histopathological image analysis: Updates in 2024
Daisuke Komura, Mieko Ochi, Shumpei Ishikawa
Computational and Structural Biotechnology Journal.2025; 27: 383. CrossRef - Beyond single biomarkers: multi-omics strategies to predict immunotherapy outcomes in blood cancers
Mohammad Pirouzbakht, Soroosh Hamzeh, Hamed Soleimani Samarkhazan
Clinical and Experimental Medicine.2025;[Epub] CrossRef - Temporal changes in tongue color during immune checkpoint inhibitor therapy in patients with non-small-cell lung cancer: a prospective observational study using digital tongue diagnosis
Eunbyul Cho, Woosu Choi, Jun Hyeok Lim, Ji Woong Son, Seung Hun Jang, Seung Hyeun Lee, Jong Gwon Choi, In-Jae Oh, Tae-Won Jang, Seong Hoon Yoon, Seung Joon Kim, Chang-Min Choi, Sung Yong Lee, Mi Mi Ko, Mi-Kyung Jeong
Oncology Reviews.2025;[Epub] CrossRef
- Machine learning methods for histopathological image analysis: Updates in 2024
- TTF1-positive SMARCA4/BRG1 deficient lung adenocarcinoma
- Anurag Mehta, Himanshi Diwan, Divya Bansal, Manoj Gupta
- J Pathol Transl Med. 2022;56(1):53-56. Published online November 16, 2021
- DOI: https://doi.org/10.4132/jptm.2021.09.16
- 8,186 View
- 195 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - SMARCA4/BRG1-deficient lung adenocarcinoma (SD-LUAD) is being recognized as a distinct subtype based on subtle differences in its clinical, morphological, and immunophenotypic attributes compared to other non–small cell lung carcinomas. We present here a case of SD-LUAD with curious thyroid transcription factor 1 (TTF1) expression in a morphologically heterogenous lung adenocarcinoma. The better differentiated area showed preservation of TTF1 expression, and a poorly differentiated tumor had loss of TTF1 expression with universal BRG1 loss.
-
Citations
Citations to this article as recorded by- SMARCA4-deficient Non–small Cell Lung Cancer on 18F-FDG PET/CT
Tao Liu, Hengshan Ji, Siyuan Jiang, Rongxin Qi, Xiaodie Zhou, Jingjing Sun, Jiang Wu
Clinical Nuclear Medicine Open.2025;[Epub] CrossRef - Case Report: SMARCA4-deficient NSCLC with brain metastasis harboring co-mutations in chromatin remodeling and DNA damage repair pathways
Jiaqin Song, Shikun Yang, Lei Xia
Frontiers in Oncology.2025;[Epub] CrossRef - One Case of Non-Small Cell Lung Cancer with SMARCA4 Deletion Was Reported
允龙 宋
Medical Diagnosis.2024; 14(01): 137. CrossRef - Delineation of a SMARCA4-specific competing endogenous RNA network and its function in hepatocellular carcinoma
Lei Zhang, Ting Sun, Xiao-Ye Wu, Fa-Ming Fei, Zhen-Zhen Gao
World Journal of Clinical Cases.2022; 10(29): 10501. CrossRef - Novel germline SMARCA4 mutation in Small Cell Carcinoma of the Ovary, Hypercalcemic Type
Anurag Mehta, Himanshi Diwan, Diksha Karki, Divya Bansal, Meenakshi Kamboj, Anila Sharma, Shrinidhi Nathany, Sakshi Mattoo, Dushyant Kumar
Current Problems in Cancer: Case Reports.2022; 8: 100205. CrossRef
- SMARCA4-deficient Non–small Cell Lung Cancer on 18F-FDG PET/CT
- Programmed death-ligand 1 expression and tumor-infiltrating lymphocytes in non-small cell lung cancer: association with clinicopathologic parameters
- Gaurav Garg, Kuruswamy Thurai Prasad, Navneet Singh, Parul Gupta, Valliappan Muthu, Ashim Das, Amanjit Bal
- J Pathol Transl Med. 2021;55(6):398-405. Published online October 6, 2021
- DOI: https://doi.org/10.4132/jptm.2021.08.08
- 5,422 View
- 167 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Data on the prevalence of programmed death-ligand 1 (PD-L1) expression and tumor-infiltrating lymphocytes (TILs) in non–small cell lung cancer (NSCLC) and their clinical significance in Indian patients are limited.
Methods
Newly diagnosed NSCLC cases (adenocarcinoma or squamous cell carcinoma [SqCC] histology) were included in the present study. The TILs were evaluated based on morphology on hematoxylin and eosin–stained slides. PD-L1 expression in tumors was assessed using immunohistochemistry with rabbit monoclonal antibody (SP263) on the Ventana automated immunostainer. Tumors with PD-L1 expression > 50% on tumor cells were considered PD-L1–positive. Tumors in which TILs occupy > 25% of stroma were considered to have high TILs. The association of PD-L1 expression and TILs with various clinical parameters including overall survival (OS) was investigated.
Results
The present study included 128 cases of NSCLC (67 adenocarcinoma, 61 SqCC). PD-L1 positivity was observed in 17.2% of the patients with NSCLC. Baseline characteristics of PD-L1–positive subjects were similar to PD-L1–negative subjects except for a higher prevalence of liver metastasis (18.2% vs. 2.8%; p = .018) and a higher probability of diagnosis from extrapulmonary biopsies. High TILs were observed in 26.6% of the subjects. However, PD-L1 expression and high TIL did not affect OS.
Conclusions
PD-L1 positivity and high TILs were observed in 20% and 25% of the patients with NSCLC, respectively, however, neither were predictors of survival in SqCC. -
Citations
Citations to this article as recorded by- PDL1 and IDO‐2 Immunohistochemistry in Bronchoalveolar Lavage Versus Bronchoscopic Biopsy of Non‐Small Cell Lung Cancer
Menna Allah Hesham Mohammed Fekry, Yosria Mohammed El‐Gohary, Hesham Radwan Abd‐Elaziz, Tarek Hamdy Hassan, Mona Mostafa Ahmed
Cytopathology.2025;[Epub] CrossRef - Multiplex plasma protein assays as a diagnostic tool for lung cancer
Mohammad Tanvir Ahamed, Jenny Forshed, Adrian Levitsky, Janne Lehtiö, Amanj Bajalan, Maria Pernemalm, Lars E. Eriksson, Björn Andersson
Cancer Science.2024; 115(10): 3439. CrossRef - Real-world prevalence of PD-L1 expression in non-small cell lung cancer: an Australia-wide multi-centre retrospective observational study
Prudence A. Russell, Alexandra L. Farrall, Sarita Prabhakaran, Khashayar Asadi, Wade Barrett, Caroline Cooper, Wendy Cooper, Samuel Cotton, Edwina Duhig, Matthew Egan, Stephen Fox, David Godbolt, Shilpa Gupta, Aniza Hassan, Connull Leslie, Trishe Leong, D
Pathology.2023; 55(7): 922. CrossRef
- PDL1 and IDO‐2 Immunohistochemistry in Bronchoalveolar Lavage Versus Bronchoscopic Biopsy of Non‐Small Cell Lung Cancer
- Correlation of TTF-1 immunoexpression and EGFR mutation spectrum in non–small cell lung carcinoma
- Tripti Nakra, Varsha Singh, Aruna Nambirajan, Prabhat Singh Malik, Anant Mohan, Deepali Jain
- J Pathol Transl Med. 2021;55(4):279-288. Published online July 8, 2021
- DOI: https://doi.org/10.4132/jptm.2021.05.10
- 7,981 View
- 186 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Thyroid transcription factor (TTF-1) is a diagnostic marker expressed in 75%–85% of primary lung adenocarcinomas (ACs). Activating mutations in the tyrosine kinase domain of the epidermal growth factor receptor (EGFR) gene is the most common targetable driver alteration in lung AC. Previous studies have shown a positive correlation between TTF-1 and EGFR mutation status. We aimed to determine the predictive value of TTF-1 immunoexpression for underlying EGFR mutation status in a large Indian cohort.
Methods
This retrospective designed study was conducted with medical record data from 2011 to 2020. All cases of primary lung AC and non–small cell lung carcinoma not otherwise specified (NSCLC, NOS) with known TTF-1 expression diagnosed by immunohistochemistry using 8G7G3/1 antibodies and EGFR mutation status diagnosed by quantitative polymerase chain reaction were retrieved, reviewed, and the
results
were analyzed. Results: Among 909 patient samples diagnosed as lung AC and NSCLC, NOS, TTF-1 was positive in 76.8% cases (698/909) and EGFR mutations were detected in 29.6% (269/909). A strong positive correlation was present between TTF-1 positivity and EGFR mutation status (odds ratio, 3.61; p < .001), with TTF-1 positivity showing high sensitivity (90%) and negative predictive value (87%) for EGFR mutation. TTF-1 immunoexpression did not show significant correlation with uncommon/dual EGFR mutations (odds ratio, 1.69; p = .098). EGFR–tyrosine kinase inhibitor therapy was significantly superior to chemotherapy among EGFR mutant cases irrespective of TTF-1 status; however, no significant differences among survival outcomes were observed.
Conclusions
Our study confirms a strong positive correlation between TTF-1 expression and common EGFR mutations (exon 19 deletion and exon 21 L858R) in advanced lung AC with significantly high negative predictive value of TTF-1 for EGFR mutations. -
Citations
Citations to this article as recorded by- Baseline retinoblastoma transcriptional corepressor 1 (Rb1) functional inactivation is a pre-requisite but not sufficient for small-cell histological transformation in epidermal growth factor receptor (EGFR) mutant lung adenocarcinomas post-tyrosine kinas
Aruna Nambirajan, Amber Rathor, Hemavathi Baskarane, Anju GS, Sachin Khurana, Somagattu Sushmitha, Aparna Sharma, Prabhat Singh Malik, Deepali Jain
Virchows Archiv.2025; 487(3): 639. CrossRef - Lung Carcinoids in Adolescents and Young Adults (AYAs): A Still Overlooked Clinical Entity
Alice Laffi, Laura Pala, Chiara Catania, Marzia Locatelli, Priscilla Cascetta, Emilia Cocorocchio, Giovanni Luca Ceresoli, Daniele Laszlo, Flaminia Facella, Emily Governini, Marzia Bendoni, Giuseppe Pelosi, Fabio Conforti, Tommaso Martino De Pas
Current Oncology.2025; 32(8): 458. CrossRef - Correlation between TTF-1 expression and EGFR mutations in moroccan lung adenocarcinoma: A prospective six-year study
Sara Boukansa, Ismail Mouhrach, Fatima El Agy, Mokhtar El Mekhtoume, Laila Bouguenouch, Mounia Serraj, Bouchra Amara, Yassine Ouadnouni, Mohamed Smahi, Badreeddine Alami, Nawfel Mellas, Zineb Benbrahim, Hinde El Fatemi
Cancer Treatment and Research Communications.2025; 45: 101012. CrossRef - Mutation profile and programmed death ligand 1 status of patients with non‐small cell lung cancer diagnosed with “adenocarcinoma” and “non‐small cell carcinoma favor adenocarcinoma”
Naoko Shigeta, Tomoyuki Yokose, Shuji Murakami, Tetsuya Isaka, Kanako Shinada, Emi Yoshioka, Atsuya Narita, Kengo Katakura, Tetsuro Kondo, Terufumi Kato, Takuya Nagashima, Haruhiro Saito, Hiroyuki Ito
Thoracic Cancer.2024; 15(6): 458. CrossRef - Significance of NKX2-1 as a biomarker for clinical prognosis, immune infiltration, and drug therapy in lung squamous cell carcinoma
Huiyue Lin, Juyong Wang, Qing Shi, Minmin Wu
PeerJ.2024; 12: e17338. CrossRef - TTF-1 is a highly sensitive but not fully specific marker for pulmonary and thyroidal cancer: a tissue microarray study evaluating more than 17,000 tumors from 152 different tumor entities
Katharina Möller, Tayyaba Gulzar, Maximilian Lennartz, Florian Viehweger, Martina Kluth, Claudia Hube-Magg, Christian Bernreuther, Ahmed Abdulwahab Bawahab, Ronald Simon, Till S. Clauditz, Guido Sauter, Ria Schlichter, Andrea Hinsch, Simon Kind, Frank Jac
Virchows Archiv.2024; 485(5): 815. CrossRef - Identifying immunohistochemical biomarkers panel for non-small cell lung cancer in optimizing treatment and forecasting efficacy
Xiaoya Zhang, Junhong Meng, Mingyue Gao, Cheng Gong, Cong Peng, Duxian Liu
BMC Cancer.2024;[Epub] CrossRef - Expression landscapes in non-small cell lung cancer shaped by the thyroid transcription factor 1
Herdee Gloriane C. Luna, Marcelo Severino Imasa, Necy Juat, Katherine V. Hernandez, Treah May Sayo, Gloria Cristal-Luna, Sheena Marie Asur-Galang, Mirasol Bellengan, Kent John Duga, Bien Brian Buenaobra, Marvin I. De los Santos, Daniel Medina, Jamirah Sam
Lung Cancer.2023; 176: 121. CrossRef - Malignant pleural effusion cell blocks are reliable resources for PD-L1 analysis in advanced lung adenocarcinomas: a concordance study with matched histologic samples
Swati Mahajan, Aruna Nambirajan, Ishan Gupta, Nalini Gupta, Parikshaa Gupta, Deepali Jain
Journal of the American Society of Cytopathology.2022; 11(5): 253. CrossRef - Clinicopathologic Features and Molecular Biomarkers as Predictors of Epidermal Growth Factor Receptor Gene Mutation in Non-Small Cell Lung Cancer Patients
Lanlan Liu, Xianzhi Xiong
Current Oncology.2021; 29(1): 77. CrossRef
- Baseline retinoblastoma transcriptional corepressor 1 (Rb1) functional inactivation is a pre-requisite but not sufficient for small-cell histological transformation in epidermal growth factor receptor (EGFR) mutant lung adenocarcinomas post-tyrosine kinas
- SMARCA4/BRG1 protein-deficient thoracic tumors dictate re-examination of small biopsy reporting in non–small cell lung cancer
- Anurag Mehta, Divya Bansal, Rupal Tripathi, Ankush Jajodia
- J Pathol Transl Med. 2021;55(5):307-316. Published online June 21, 2021
- DOI: https://doi.org/10.4132/jptm.2021.05.11
- 11,636 View
- 336 Download
- 12 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
SMARCA4/BRG1 protein–deficient lung adenocarcinomas and thoracic sarcoma are recently described entities that lack distinctive histological features, transcription termination factor 1 (TTF1) reactivity, and actionable driver mutations. The current diagnostic path for small lung biopsies as recommended by the World Health Organization (WHO, 2015) is likely to categorize these as non– small cell carcinoma–not otherwise specified (NSCC-NOS). The present study attempts to define the subtle but distinctive clinicopathologic features of SMARCA4/BRG1 protein-deficient thoracic tumors; highlight their unique biology; and addresses the unmet need to segregate these using a new, tissue-proficient diagnostic pathway.
Methods
All lung biopsies and those from metastatic sites in patients with suspected advanced lung cancer and classified as NSCC-NOS as per WHO (2015) guidelines were subjected to BRG1 testing by immunohistochemistry. SMARCA4/BRG1 protein–deficient thoracic tumors were evaluated by an extended immunohistochemistry panel. Predictive biomarker and programmed death–ligand 1 testing was conducted in all cases.
Results
Of 110 cases, nine were found to be SMARCA4/BRG1 protein-deficient; six were identified as SMARCA4/BRG1 protein–deficient lung adenocarcinomas, and three were SMARCA4/BRG1 protein-deficient thoracic sarcomas. The histology ranged from poorly differentiated to undifferentiated to rhabdoid. None of the cases showed significant expression of TTF1 or p40, and no actionable mutation was identified.
Conclusions
It is difficult to separate BRG1-deficient lung adenocarcinomas and thoracic sarcomas based on morphology alone. We propose a diagnostic pathway for small biopsies of thoracic tumors to segregate these distinct entities so that they can be studied more efficaciously for new biomarkers and therapeutic options. -
Citations
Citations to this article as recorded by- Unravelling switch/sucrose non-fermentable (SWI-SNF) complex-deficient thoracic tumours: a clinicopathological comparative on undifferentiated tumours and non-small cell lung carcinomas with BRG1 and BRM deficiency
Ridhi Sood, Arshi Tandon, Warisa Khatoon, Jayashimman Vasanthraman, Aruna Nambirajan, Anant Mohan, Prabhat Singh Malik, Deepali Jain
Journal of Clinical Pathology.2025; 78(6): 370. CrossRef - Clinicopathologic and genomic analyses of SMARCA4-mutated non-small cell lung carcinoma implicate the needs for tailored treatment strategies
Bokyung Ahn, Deokhoon Kim, Wonjun Ji, Sung-Min Chun, Goeun Lee, Se Jin Jang, Hee Sang Hwang
Lung Cancer.2025; 201: 108445. CrossRef - SMARCA4-deficient non-small cell lung cancer with metastasis to the sigmoid colon: a case report
Rong Xiao, Guang Fu, Xinglan Li, Tao Lu
World Journal of Surgical Oncology.2025;[Epub] CrossRef - Clinicopathological and molecular perspectives on thoracic SMARCA4-deficient undifferentiated tumors and SMARCA4-deficient non-small cell lung carcinomas
Sumanta Das, Pallavi Mishra, Sunita Ahlawat
Pathologica.2025; 117(5): 455. CrossRef - Case report: The first account of undifferentiated sarcoma with epithelioid features originating in the pleura
Ling-Xi Xiao, Li Liu, Wang Deng
Frontiers in Medicine.2024;[Epub] CrossRef - SMARCA4-deficient central nervous system metastases: A case series and systematic review
Meaghan Morris, Kerime Ararat, Hannah Cutshall, Murat Gokden, Analiz Rodriguez, Lisa Rooper, Matthew Lindberg, James Stephen Nix
Journal of Neuropathology & Experimental Neurology.2024; 83(8): 638. CrossRef - Chemotherapy and Immune Checkpoint Inhibitors in a Case of SMARCA4-dUT: A Case Report and Review of Literature
Akriti Pokhrel, Ruchi Yadav, Kapil Kumar Manvar, Richard Wu, Vijay Jaswani, Carrie Brooke Wasserman, Jen C. Wang
Journal of Investigative Medicine High Impact Case Reports.2023;[Epub] CrossRef - TTF1-positive SMARCA4/BRG1 deficient lung adenocarcinoma
Anurag Mehta, Himanshi Diwan, Divya Bansal, Manoj Gupta
Journal of Pathology and Translational Medicine.2022; 56(1): 53. CrossRef - Delineation of a SMARCA4-specific competing endogenous RNA network and its function in hepatocellular carcinoma
Lei Zhang, Ting Sun, Xiao-Ye Wu, Fa-Ming Fei, Zhen-Zhen Gao
World Journal of Clinical Cases.2022; 10(29): 10501. CrossRef - Artificial intelligence platform, RADR®, aids in the discovery of DNA damaging agent for the ultra-rare cancer Atypical Teratoid Rhabdoid Tumors
Joseph McDermott, Drew Sturtevant, Umesh Kathad, Sudhir Varma, Jianli Zhou, Aditya Kulkarni, Neha Biyani, Caleb Schimke, William C. Reinhold, Fathi Elloumi, Peter Carr, Yves Pommier, Kishor Bhatia
Frontiers in Drug Discovery.2022;[Epub] CrossRef
- Unravelling switch/sucrose non-fermentable (SWI-SNF) complex-deficient thoracic tumours: a clinicopathological comparative on undifferentiated tumours and non-small cell lung carcinomas with BRG1 and BRM deficiency
- Current status and future perspectives of liquid biopsy in non-small cell lung cancer
- Sunhee Chang, Jae Young Hur, Yoon-La Choi, Chang Hun Lee, Wan Seop Kim
- J Pathol Transl Med. 2020;54(3):204-212. Published online April 15, 2020
- DOI: https://doi.org/10.4132/jptm.2020.02.27
- 11,330 View
- 296 Download
- 20 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF - With advances in target therapy, molecular analysis of tumors is routinely required for treatment decisions in patients with advanced non-small cell lung cancer (NSCLC). Liquid biopsy refers to the sampling and analysis of circulating cell-free tumor DNA (ctDNA) in various body fluids, primarily blood. Because the technique is minimally invasive, liquid biopsies are the future in cancer management. Epidermal growth factor receptor (EGFR) ctDNA tests have been performed in routine clinical practice in advanced NSCLC patients to guide tyrosine kinase inhibitor treatment. In the near future, liquid biopsy will be a crucial prognostic, predictive, and diagnostic method in NSCLC. Here we present the current status and future perspectives of liquid biopsy in NSCLC.
-
Citations
Citations to this article as recorded by- Comparison of tissue-based and plasma-based testing for EGFR mutation in non–small cell lung cancer patients
Yoon Kyung Kang, Dong Hoon Shin, Joon Young Park, Chung Su Hwang, Hyun Jung Lee, Jung Hee Lee, Jee Yeon Kim, JooYoung Na
Journal of Pathology and Translational Medicine.2025; 59(1): 60. CrossRef - Lab-in-a-Fiber detection and capture of cells
João C. Varela, Achar V. Harish, Pawel Maniewski, Timothy Gibbon, Oana Tudoran, Rainer Heuchel, Matthias Löhr, Walter Margulis, Aman Russom, Fredrik Laurell
Scientific Reports.2025;[Epub] CrossRef - Lung Cancer Diagnosis and Prognostic Monitoring Through Cell-Free RNA via Liquid Biopsy
Yuanming Pan, Chongbo Jiang, Mengchan Ye, Dongmei Li, Jinghui Wang
Therapeutics and Clinical Risk Management.2025; Volume 21: 1615. CrossRef - Unlocking the future of cancer diagnosis – promises and challenges of ctDNA-based liquid biopsies in non-small cell lung cancer
Chiara Reina, Berina Šabanović, Chiara Lazzari, Vanesa Gregorc, Christopher Heeschen
Translational Research.2024; 272: 41. CrossRef - Tailored point-of-care biosensors for liquid biopsy in the field of oncology
Sima Singh, Pritam Saha Podder, Matt Russo, Charles Henry, Stefano Cinti
Lab on a Chip.2023; 23(1): 44. CrossRef - Emerging role of non-invasive and liquid biopsy biomarkers in pancreatic cancer
Akash Bararia, Prosenjeet Chakraborty, Paromita Roy, Bitan Kumar Chattopadhay, Amlan Das, Aniruddha Chatterjee, Nilabja Sikdar
World Journal of Gastroenterology.2023; 29(15): 2241. CrossRef - Liquid biopsy in the management of advanced lung cancer: Implementation and practical aspects
Gabriela Fernandes, Ana Rodrigues, Cláudia Matos, Fernando Barata, Luís Cirnes, Lurdes Ferreira, José Albino Lopes, Margarida Felizardo, Paula Fidalgo, Ulisses Brito, Bárbara Parente
Cancer Treatment and Research Communications.2023; 36: 100725. CrossRef - Tweezer PCR: A Highly Specific Method for Accurate Identification of Low-Abundance Mutations
Shanglin Li, Yin Gu, Zhi Geng, Kaiyi Li, Yawei Hu, Qiang Liu, Rongxin Fu, Peng Liu
Analytical Chemistry.2023; 95(48): 17679. CrossRef - Mesonephric-like Adenocarcinoma of the Ovary: Clinicopathological and Molecular Characteristics
Hyun Hee Koh, Eunhyang Park, Hyun-Soo Kim
Diagnostics.2022; 12(2): 326. CrossRef - Alveolar Soft Part Sarcoma of the Uterus: Clinicopathological and Molecular Characteristics
Yurimi Lee, Kiyong Na, Ha Young Woo, Hyun-Soo Kim
Diagnostics.2022; 12(5): 1102. CrossRef - Exosomal MicroRNA Analyses in Esophageal Squamous Cell Carcinoma Cell Lines
Sora Kim, Gwang Ha Kim, Su Jin Park, Chae Hwa Kwon, Hoseok I, Moon Won Lee, Bong Eun Lee
Journal of Clinical Medicine.2022; 11(15): 4426. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Update on molecular pathology and role of liquid biopsy in nonsmall cell lung cancer
Pamela Abdayem, David Planchard
European Respiratory Review.2021; 30(161): 200294. CrossRef - Dynamics of Specific cfDNA Fragments in the Plasma of Full Marathon Participants
Takehito Sugasawa, Shin-ichiro Fujita, Tomoaki Kuji, Noriyo Ishibashi, Kenshirou Tamai, Yasushi Kawakami, Kazuhiro Takekoshi
Genes.2021; 12(5): 676. CrossRef - Future Perspectives in Detecting EGFR and ALK Gene Alterations in Liquid Biopsies of Patients with NSCLC
Daniela Ferreira, Juliana Miranda, Paula Martins-Lopes, Filomena Adega, Raquel Chaves
International Journal of Molecular Sciences.2021; 22(8): 3815. CrossRef - Real-World Analysis of the EGFR Mutation Test in Tissue and Plasma Samples from Non-Small Cell Lung Cancer
Hyunwoo Lee, Joungho Han, Yoon-La Choi
Diagnostics.2021; 11(9): 1695. CrossRef - Objective Quantitation of EGFR Protein Levels using Quantitative Dot Blot Method for the Prognosis of Gastric Cancer Patients
Lei Xin, Fangrong Tang, Bo Song, Maozhou Yang, Jiandi Zhang
Journal of Gastric Cancer.2021; 21(4): 335. CrossRef - The Role of the Liquid Biopsy in Decision-Making for Patients with Non-Small Cell Lung Cancer
D. Akhoundova, J. Mosquera Martinez, L. E. Musmann, C. Britschgi, C. Rütsche, M. Rechsteiner, E. Nadal, M. R. Garcia Campelo, A. Curioni-Fontecedro
Journal of Clinical Medicine.2020; 9(11): 3674. CrossRef - Expanding opportunities in precision oncology
T Raja
Cancer Research, Statistics, and Treatment.2020; 3(4): 863. CrossRef
- Comparison of tissue-based and plasma-based testing for EGFR mutation in non–small cell lung cancer patients
- PD-L1 Testing in Non-small Cell Lung Cancer: Past, Present, and Future
- Hyojin Kim, Jin-Haeng Chung
- J Pathol Transl Med. 2019;53(4):199-206. Published online May 2, 2019
- DOI: https://doi.org/10.4132/jptm.2019.04.24
- Correction in: J Pathol Transl Med 2020;54(2):196
- 19,142 View
- 656 Download
- 73 Web of Science
- 69 Crossref
-
 Abstract
Abstract
 PDF
PDF - Blockade of the programmed cell death-1 (PD-1) axis has already been established as an effective treatment of non-small cell lung cancer. Immunohistochemistry (IHC) for programmed death-ligand 1 (PD-L1) protein is the only available biomarker that can guide treatment with immune checkpoint inhibitors in non-small cell lung cancer. Because each PD-1/PD-L1 blockade was approved together with a specific PD-L1 IHC assay used in the clinical trials, pathologists have been challenged with performing various assays with a limited sample. To provide a more unified understanding of this, several cross-validation studies between platforms have been performed and showed consistent results. However, the interchangeability of assays may be limited in practice because of the risk of misclassification of patients for the treatment. Furthermore, several issues, including the temporal and spatial heterogeneity of PD-L1 expression in the tumor, and the potential for cytology specimens to be used as an alternative to tissue samples for PD-L1 testing, have still not been resolved. In the future, one of the main aims of immunotherapy research should be to find a novel predictive biomarker for PD-1 blockade therapy and a way to combine it with PD-L1 IHC and other tests.
-
Citations
Citations to this article as recorded by- Impact of patient and tumor characteristics on various aspects of the non-small cell lung cancer patient journey in Romania, Bulgaria, Serbia: A multicenter, non-interventional, retrospective cohort study
Alexandra C. Preda, Rossitza Krasteva, Mihailo Stjepanović, Krassimir Koynov, Assia Konsoulova, Georgeta P. Iorga, Anghel A. Udrea, Anca Zgura, Tudor-Eliade Ciuleanu, Raluca Patru, Jeliazko Arabadjiev, Ivan Tonev, Zoran Andrić, Goran Stojanović, Mihaela P
Cancer Treatment and Research Communications.2026; 46: 101056. CrossRef - Impact of first-line maintenance immunotherapy with or without pemetrexed for non-squamous advanced/metastatic non-small cell lung cancer lacking targetable mutations: a real-world analysis in England
Fabio Gomes, L. Niall Gilding, Vivian Tan, Katerina Christoforou, Joanne Rule, Amine Aziez, Adam Januszewski, Anna Minchom
Clinical Lung Cancer.2026;[Epub] CrossRef - A patient similarity-embedded Bayesian approach to prognostic biomarker inference with application to thoracic cancer immunity
Duo Yu, Meilin Huang, Michael J Kane, Brian P Hobbs
Journal of the Royal Statistical Society Series C: Applied Statistics.2025; 74(3): 800. CrossRef - Programmed Cell Death Ligand 1 (PD-L1) and major Histocompatibility Complex Class I (MHC Class I) Expression Patterns and Their Pathologic Associations in triple-Negative Breast Cancer
Ponkrit Kaewkedsri, Piyapharom Intarawichian, Sirawich Jessadapattarakul, Waritta Kunprom, Supinda Koonmee, Malinee Thanee, Ongart Somintara, Anongporn Wongbuddha, Payia Chadbunchachai, Supajit Nawapun, Chaiwat Aphivatanasiri
Breast Cancer: Targets and Therapy.2025; Volume 17: 123. CrossRef - Exploring immune checkpoint inhibitors: Focus on PD-1/PD-L1 axis and beyond
Durre Aden, Samreen Zaheer, Niti Sureka, Monal Trisal, Jai Kumar Chaurasia, Sufian Zaheer
Pathology - Research and Practice.2025; 269: 155864. CrossRef - Prognostic value of HER2 expression in cervical adenocarcinoma: A retrospective cohort study
Qing Xu, Zhuomin Yin, Yueqi Li, Xiu Zhu, Hanmei Lou, Juan Ni
Oncology Letters.2025; 29(5): 1. CrossRef - PD-1/PD-L1 blockade therapy with atezolizumab: a new paradigm in the treatment of non-small cell lung cancer (NSCLC)
Samaneh Moradi, Pedram Sarikhani, Rafid Jihad Albadr, Waam Mohammed Taher, Mariem Alwan, Mahmood Jasem Jawad, Hiba Mushtaq, Niyousha Vakilzadehian
Discover Oncology.2025;[Epub] CrossRef - PD‐L1 Scoring Models for Non‐Small Cell Lung Cancer in China: Current Status, AI‐Assisted Solutions and Future Perspectives
Ziling Huang, Shen Wang, Jiansong Zhou, Haiquan Chen, Yuan Li
Thoracic Cancer.2025;[Epub] CrossRef - Advancing Precision Medicine in PDAC: An Ethical Scoping Review and Call to Action for IHC Implementation
Lyanne A. Delgado-Coka, Lucia Roa-Peña, Andrew Flescher, Luisa F. Escobar-Hoyos, Kenneth R. Shroyer
Cancers.2025; 17(12): 1899. CrossRef - A Prospective Exploratory Study of Functional Immunity Assessed by Pretreatment Interferon Gamma Release Assay in Relation to Different Systemic Therapies in Patients With Advanced-Stage NSCLC
Hsu-Ching Huang, Han-Jhih Chang, Chi-Lu Chiang, Hsin-Yi Huang, Yung-Hung Luo, Yuh-Min Chen, Tsu-Hui Shiao, Chao-Hua Chiu
JTO Clinical and Research Reports.2025; 6(8): 100845. CrossRef - A panorama of lung cancer biomarkers
Ana Sofia Silva Mesquita, Maire Iumi Maeda, Juliana Cabral Duarte Brandão, Nicolle Cavalcante Gaglionone, Igor Campos da Silva, Milena Perez Mak, Ellen Caroline Toledo do Nascimento
Surgical and Experimental Pathology.2025;[Epub] CrossRef - Unraveling Resistance in Lung Cancer Immunotherapy: Clinical Milestones, Mechanistic Insights, and Future Strategies
Maria Vitale, Raffaella Pagliaro, Giuseppe Viscardi, Lucio Pastore, Giuseppe Castaldo, Fabio Perrotta, Susan F. Campbell, Andrea Bianco, Filippo Scialò
International Journal of Molecular Sciences.2025; 26(18): 9244. CrossRef - Precision Oncology in Lung Cancer Surgery
Patrick Bou-Samra, Sunil Singhal
Surgical Oncology Clinics of North America.2024; 33(2): 311. CrossRef - Expression of PD-L1 clones (22C3 and 28-8) in hepatocellular carcinoma: a tertiary cancer care hospital experience
Kashif Asghar, Shaarif Bashir, Muhammad Hassan, Asim Farooq, Muhammad Abu Bakar, Sundus Bilal, Maryam Hameed, Shafqat Mehmood, Asif Loya
Egyptian Liver Journal.2024;[Epub] CrossRef - Engineering Proteus mirabilis improves antitumor efficacy via enhancing cytotoxic T cell responses
Hong Zhang, Yinlin Luo, Xincheng Zhao, Xiande Liu
Molecular Therapy: Oncology.2024; 32(1): 200770. CrossRef - Unlocking the potential of oncology biomarkers: advancements in clinical theranostics
Ankit Kumar Dubey, Ishnoor Kaur, Reecha Madaan, Shikha Raheja, Rajni Bala, Manoj Garg, Suresh Kumar, Viney Lather, Vineet Mittal, Deepti Pandita, Rohit Gundamaraju, Rajeev K. Singla, Rohit Sharma
Drug Metabolism and Personalized Therapy.2024; 39(1): 5. CrossRef - Exploring histological predictive biomarkers for immune checkpoint inhibitor therapy response in non–small cell lung cancer
Uiju Cho, Soyoung Im, Hyung Soon Park
Journal of Pathology and Translational Medicine.2024; 58(2): 49. CrossRef - Predicting efficacy assessment of combined treatment of radiotherapy and nivolumab for NSCLC patients through virtual clinical trials using QSP modeling
Miriam Schirru, Hamza Charef, Khalil-Elmehdi Ismaili, Frédérique Fenneteau, Didier Zugaj, Pierre-Olivier Tremblay, Fahima Nekka
Journal of Pharmacokinetics and Pharmacodynamics.2024; 51(4): 319. CrossRef - Predictions of PD-L1 Expression Based on CT Imaging Features in Lung Squamous Cell Carcinoma
Seong Hee Yeo, Hyun Jung Yoon, Injoong Kim, Yeo Jin Kim, Young Lee, Yoon Ki Cha, So Hyeon Bak
Journal of the Korean Society of Radiology.2024; 85(2): 394. CrossRef - Assessment of Programmed Cell Death Ligand-1 Expression in Non-small Cell Lung Carcinomas by Immunohistochemistry
Sandeep Mani, Archana Lakshmanan, Annapurneswari Subramanyan
Apollo Medicine.2024; 21(1): 57. CrossRef - The efficacy of immune checkpoint inhibitors on low PD‐L1 cervical cancer: A meta‐analysis
Wutao Chen, Nan Zhang, Zhihong He, Qing Li, You Wang, Weihua Lou, Wen Di
Health Science Reports.2024;[Epub] CrossRef - Molecular Characteristics and Pretreatment Neutrophil-to-Lymphocyte Ratio as Predictors of Durable Clinical Benefit from Immune Checkpoint Inhibition in Non-Small Cell Lung Cancer
Arpeet T. Shah, Isabelle Blanchard, Sukhmani K. Padda, Heather A. Wakelee, Joel W. Neal
Clinical Lung Cancer.2024; 25(6): 550. CrossRef - Optimizing immunofluorescence with high-dynamic-range imaging to enhance PD-L1 expression evaluation for 3D pathology assessment from NSCLC tumor tissue
Hsien-Neng Huang, Chun-Wei Kuo, Yu-Ling Hung, Chia-Hung Yang, Yu-Han Hsieh, Yu-Chieh Lin, Margaret Dah-Tsyr Chang, Yen-Yin Lin, Jen-Chung Ko
Scientific Reports.2024;[Epub] CrossRef - The Role of Programmed Cell Death Ligand 1 Expression in Pituitary Tumours: Lessons from the Current Literature
Mariana Lopes-Pinto, Ema Lacerda-Nobre, Ana Luísa Silva, Francisco Tortosa, Pedro Marques
Neuroendocrinology.2024; 114(8): 709. CrossRef - Real‑world evidence of advanced non‑small cell lung carcinoma treated with an immune checkpoint inhibitor plus chemotherapy
Zihan Xu, Huien Zhang, Guikai Ma, Wenjuan Meng, Junliang Du, Xin Wu, Baohong Yang, Ningning Wang, Yanhong Ding, Qingyun Zhang, Na Li, Xuede Zhang, Guohua Yu, Shuzhen Liu, Zhenhua Li
Oncology Letters.2024;[Epub] CrossRef - Clinical impact of concomitant BIO-three use in advanced or recurrent non-small cell lung cancer treated with immune-checkpoint inhibitor
Hitomi Nakatsukasa, Masaya Takahashi, Masahito Shibano, Yusuke Ishigami, Tomoya Kawaguchi, Yasutaka Nakamura, Hiroyasu Kaneda
International Journal of Clinical Oncology.2024; 29(12): 1840. CrossRef - Special issue “The advance of solid tumor research in China”: FGFR4 alterations predict efficacy of immune checkpoint inhibitors in nonsmall cell lung cancer
Guanghui Gao, Longgang Cui, Fei Zhou, Tao Jiang, Wanying Wang, Shiqi Mao, Fengying Wu, Fangli Jiang, Bei Zhang, Ting Bei, Wenchuan Xie, Cheng Zhang, Hougang Zhang, Chan Gao, Xiaochen Zhao, Yuezong Bai, Caicun Zhou, Shengxiang Ren
International Journal of Cancer.2023; 152(1): 79. CrossRef - Molecular Classification of Extrapulmonary Neuroendocrine Carcinomas With Emphasis on POU2F3-positive Tuft Cell Carcinoma
Jiwon Koh, Haeryoung Kim, Kyung Chul Moon, Cheol Lee, Kyoungbun Lee, Han Suk Ryu, Kyeong Cheon Jung, Yoon Kyung Jeon
American Journal of Surgical Pathology.2023; 47(2): 183. CrossRef - Biomarkers for Predicting Response to Personalized Immunotherapy in Gastric Cancer
Moonsik Kim, Ji Yun Jeong, An Na Seo
Diagnostics.2023; 13(17): 2782. CrossRef - PD-L1 Expression in Pituitary Neuroendocrine Tumors/Pituitary Adenomas
Giulia Cossu, Stefano La Rosa, Jean Philippe Brouland, Nelly Pitteloud, Ethan Harel, Federico Santoni, Maxime Brunner, Roy Thomas Daniel, Mahmoud Messerer
Cancers.2023; 15(18): 4471. CrossRef - Prognostic Significance of Programmed Cell Death Ligand 1 Expression in High-Grade Serous Ovarian Carcinoma: A Systematic Review and Meta-Analysis
Jeongwan Kang, Kang Min Han, Hera Jung, Hyunchul Kim
Diagnostics.2023; 13(20): 3258. CrossRef - A targeted expression panel for classification, gene fusion detection and PD-L1 measurements – Can molecular profiling replace immunohistochemistry in non-small cell lung cancer?
Anita Tranberg Simonsen, Amalie Utke, Johanne Lade-Keller, Lasse Westphal Thomsen, Torben Steiniche, Magnus Stougaard
Experimental and Molecular Pathology.2022; 125: 104749. CrossRef - Program death ligand‐1 immunocytochemistry in lung cancer cytological samples: A systematic review
Swati Satturwar, Ilaria Girolami, Enrico Munari, Francesco Ciompi, Albino Eccher, Liron Pantanowitz
Diagnostic Cytopathology.2022; 50(6): 313. CrossRef - Computer-assisted three-dimensional quantitation of programmed death-ligand 1 in non-small cell lung cancer using tissue clearing technology
Yen-Yu Lin, Lei-Chi Wang, Yu-Han Hsieh, Yu-Ling Hung, Yung-An Chen, Yu-Chieh Lin, Yen-Yin Lin, Teh-Ying Chou
Journal of Translational Medicine.2022;[Epub] CrossRef - Correlation Between Pretreatment Neutrophil-to-Lymphocyte Ratio and Programmed Death-Ligand 1 Expression as Prognostic Markers in Non-Small Cell Lung Cancer
Cristina-Florina Pirlog, Horia Teodor Cotan, Andreea Parosanu, Cristina Orlov Slavu, Ana Maria Popa, Cristian Iaciu, Mihaela Olaru, Alexandru Vlad Oprita, Irina Nita, Cornelia Nitipir
Cureus.2022;[Epub] CrossRef - Expert opinion on NSCLC small specimen biomarker testing — Part 2: Analysis, reporting, and quality assessment
Frédérique Penault-Llorca, Keith M. Kerr, Pilar Garrido, Erik Thunnissen, Elisabeth Dequeker, Nicola Normanno, Simon J. Patton, Jenni Fairley, Joshua Kapp, Daniëlle de Ridder, Aleš Ryška, Holger Moch
Virchows Archiv.2022; 481(3): 351. CrossRef - Novel Inflammasome-Based Risk Score for Predicting Survival and Efficacy to Immunotherapy in Early-Stage Non-Small Cell Lung Cancer
Chih-Cheng Tsao, Hsin-Hung Wu, Ying-Fu Wang, Po-Chien Shen, Wen-Ting Wu, Huang-Yun Chen, Yang-Hong Dai
Biomedicines.2022; 10(7): 1539. CrossRef - Comparative Analysis of Mutation Status and Immune Landscape for Squamous Cell Carcinomas at Different Anatomical sites
Wenqi Ti, Tianhui Wei, Jianbo Wang, Yufeng Cheng
Frontiers in Immunology.2022;[Epub] CrossRef - Pan-cancer analysis of the angiotensin II receptor-associated protein as a prognostic and immunological gene predicting immunotherapy responses in pan-cancer
Kai Hong, Yingjue Zhang, Lingli Yao, Jiabo Zhang, Xianneng Sheng, Lihua Song, Yu Guo, Yangyang Guo
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef - Molecular imaging of immune checkpoints in oncology: Current and future applications
Shushan Ge, Tongtong Jia, Jihui Li, Bin Zhang, Shengming Deng, Shibiao Sang
Cancer Letters.2022; 548: 215896. CrossRef - PD-L1 expression and association with genetic background in pheochromocytoma and paraganglioma
Katerina Hadrava Vanova, Ondrej Uher, Leah Meuter, Suman Ghosal, Sara Talvacchio, Mayank Patel, Jiri Neuzil, Karel Pacak
Frontiers in Oncology.2022;[Epub] CrossRef - Case report: Variable response to immunotherapy in ovarian cancer: Our experience within the current state of the art
Nicoletta Provinciali, Marco Greppi, Silvia Pesce, Mariangela Rutigliani, Irene Maria Briata, Tania Buttiron Webber, Marianna Fava, Andrea DeCensi, Emanuela Marcenaro
Frontiers in Immunology.2022;[Epub] CrossRef - PD-L1 Is Preferentially Expressed in PIT-1 Positive Pituitary Neuroendocrine Tumours
John Turchini, Loretta Sioson, Adele Clarkson, Amy Sheen, Anthony J. Gill
Endocrine Pathology.2021; 32(3): 408. CrossRef - Comprehensive tumor molecular profile analysis in clinical practice
Mustafa Özdoğan, Eirini Papadopoulou, Nikolaos Tsoulos, Aikaterini Tsantikidi, Vasiliki-Metaxa Mariatou, Georgios Tsaousis, Evgenia Kapeni, Evgenia Bourkoula, Dimitrios Fotiou, Georgios Kapetsis, Ioannis Boukovinas, Nikolaos Touroutoglou, Athanasios Fassa
BMC Medical Genomics.2021;[Epub] CrossRef - CT-Based Hand-crafted Radiomic Signatures Can Predict PD-L1 Expression Levels in Non-small Cell Lung Cancer: a Two-Center Study
Zekun Jiang, Yinjun Dong, Linke Yang, Yunhong Lv, Shuai Dong, Shuanghu Yuan, Dengwang Li, Liheng Liu
Journal of Digital Imaging.2021; 34(5): 1073. CrossRef - Deep Learning of Histopathological Features for the Prediction of Tumour Molecular Genetics
Pierre Murchan, Cathal Ó’Brien, Shane O’Connell, Ciara S. McNevin, Anne-Marie Baird, Orla Sheils, Pilib Ó Broin, Stephen P. Finn
Diagnostics.2021; 11(8): 1406. CrossRef - Molecular Imaging and the PD-L1 Pathway: From Bench to Clinic
David Leung, Samuel Bonacorsi, Ralph Adam Smith, Wolfgang Weber, Wendy Hayes
Frontiers in Oncology.2021;[Epub] CrossRef - A Comparative Study of Immunotherapy as Second-Line Treatment and beyond in Patients with Advanced Non-Small-Cell Lung Carcinoma
Jerónimo Rafael Rodríguez-Cid, Sonia Carrasco-Cara Chards, Iván Romarico González-Espinoza, Vanessa García-Montes, Julio César Garibay-Díaz, Osvaldo Hernández-Flores, Rodrigo Riera-Sala, Anna Gozalishvili-Boncheva, Jorge Arturo Alatorre-Alexander, Luis Ma
Lung Cancer Management.2021;[Epub] CrossRef - Clinical utility of the C‐reactive protein:albumin ratio in non‐small cell lung cancer patients treated with nivolumab
Taisuke Araki, Kazunari Tateishi, Kei Sonehara, Shuko Hirota, Masamichi Komatsu, Manabu Yamamoto, Shintaro Kanda, Hiroshi Kuraishi, Masayuki Hanaoka, Tomonobu Koizumi
Thoracic Cancer.2021; 12(5): 603. CrossRef - Programmed Cell Death Ligand 1‐Transfected Mouse Bone Marrow Mesenchymal Stem Cells as Targeted Therapy for Rheumatoid Arthritis
Qiong-ying Hu, Yun Yuan, Yu-chen Li, Lu-yao Yang, Xiang-yu Zhou, Da-qian Xiong, Zi-yi Zhao, Hiroshi Tanaka
BioMed Research International.2021;[Epub] CrossRef - PD-L1 testing and clinical management of newly diagnosed metastatic non-small cell lung cancer in Spain: MOREL study
Belen Rubio-Viqueira, Margarita Majem Tarruella, Martín Lázaro, Sergio Vázquez Estévez, Juan Felipe Córdoba-Ortega, Inmaculada Maestu Maiques, Jorge García González, Ana Blasco Cordellat, Javier Valdivia-Bautista, Carmen González Arenas, Jose Miguel Sánch
Lung Cancer Management.2021;[Epub] CrossRef - Can Systems Biology Advance Clinical Precision Oncology?
Andrea Rocca, Boris N. Kholodenko
Cancers.2021; 13(24): 6312. CrossRef - Do we need PD‐L1 as a biomarker for thyroid cytologic and histologic specimens?
Marc P. Pusztaszeri, Massimo Bongiovanni, Fadi Brimo
Cancer Cytopathology.2020; 128(3): 160. CrossRef - Gut metabolomics profiling of non-small cell lung cancer (NSCLC) patients under immunotherapy treatment
Andrea Botticelli, Pamela Vernocchi, Federico Marini, Andrea Quagliariello, Bruna Cerbelli, Sofia Reddel, Federica Del Chierico, Francesca Di Pietro, Raffaele Giusti, Alberta Tomassini, Ottavia Giampaoli, Alfredo Miccheli, Ilaria Grazia Zizzari, Marianna
Journal of Translational Medicine.2020;[Epub] CrossRef - Immune checkpoint inhibitors in advanced non–small cell lung cancer: A metacentric experience from India
Santosh Kumar, Srujana Joga, Bivas Biswas, Deepak Dabkara, Kuruswamy Thurai Prasad, Navneet Singh, Prabhat Singh Malik, Sachin Khurana, Sandip Ganguly, Valliappan Muthu, Ullas Batra
Current Problems in Cancer.2020; 44(3): 100549. CrossRef - Utility of CT radiomics for prediction of PD‐L1 expression in advanced lung adenocarcinomas
Jiyoung Yoon, Young Joo Suh, Kyunghwa Han, Hyoun Cho, Hye‐Jeong Lee, Jin Hur, Byoung Wook Choi
Thoracic Cancer.2020; 11(4): 993. CrossRef - Immune checkpoint inhibitors of the PD-1/PD-L1-axis in non-small cell lung cancer: promise, controversies and ambiguities in the novel treatment paradigm
Lars H. Breimer, Petros Nousios, Louise Olsson, Hans Brunnström
Scandinavian Journal of Clinical and Laboratory Investigation.2020; 80(5): 360. CrossRef - Tumour mutational burden as a biomarker for immunotherapy: Current data and emerging concepts
Jean-David Fumet, Caroline Truntzer, Mark Yarchoan, Francois Ghiringhelli
European Journal of Cancer.2020; 131: 40. CrossRef - Precision Medicine for NSCLC in the Era of Immunotherapy: New Biomarkers to Select the Most Suitable Treatment or the Most Suitable Patient
Giovanni Rossi, Alessandro Russo, Marco Tagliamento, Alessandro Tuzi, Olga Nigro, Giacomo Vallome, Claudio Sini, Massimiliano Grassi, Maria Giovanna Dal Bello, Simona Coco, Luca Longo, Lodovica Zullo, Enrica Teresa Tanda, Chiara Dellepiane, Paolo Pronzato
Cancers.2020; 12(5): 1125. CrossRef - Current status and future perspectives of liquid biopsy in non-small cell lung cancer
Sunhee Chang, Jae Young Hur, Yoon-La Choi, Chang Hun Lee, Wan Seop Kim
Journal of Pathology and Translational Medicine.2020; 54(3): 204. CrossRef - Digital Pathology and PD-L1 Testing in Non Small Cell Lung Cancer: A Workshop Record
Fabio Pagni, Umberto Malapelle, Claudio Doglioni, Gabriella Fontanini, Filippo Fraggetta, Paolo Graziano, Antonio Marchetti, Elena Guerini Rocco, Pasquale Pisapia, Elena V. Vigliar, Fiamma Buttitta, Marta Jaconi, Nicola Fusco, Massimo Barberis, Giancarlo
Cancers.2020; 12(7): 1800. CrossRef - PD-L1 in Systemic Immunity: Unraveling Its Contribution to PD-1/PD-L1 Blockade Immunotherapy
Ana Bocanegra, Ester Blanco, Gonzalo Fernandez-Hinojal, Hugo Arasanz, Luisa Chocarro, Miren Zuazo, Pilar Morente, Ruth Vera, David Escors, Grazyna Kochan
International Journal of Molecular Sciences.2020; 21(16): 5918. CrossRef - PD-1 blockade in recurrent or metastatic cervical cancer: Data from cemiplimab phase I expansion cohorts and characterization of PD-L1 expression in cervical cancer
Danny Rischin, Marta Gil-Martin, Antonio González-Martin, Irene Braña, June Y. Hou, Daniel Cho, Gerald S. Falchook, Silvia Formenti, Salma Jabbour, Kathleen Moore, Aung Naing, Kyriakos P. Papadopoulos, Joaquina Baranda, Wen Fury, Minjie Feng, Elizabeth St
Gynecologic Oncology.2020; 159(2): 322. CrossRef - Atezolizumab: A Review in Extensive-Stage SCLC
James E. Frampton
Drugs.2020; 80(15): 1587. CrossRef - Prognostic and clinicopathological roles of programmed death‐ligand 1 (PD‐L1) expression in thymic epithelial tumors: A meta‐analysis
Hyun Min Koh, Bo Gun Jang, Hyun Ju Lee, Chang Lim Hyun
Thoracic Cancer.2020; 11(11): 3086. CrossRef - Präzisionsmedizin bei NSCLC im Zeitalter der Immuntherapie: Neue Biomarker zur Selektion der am besten geeigneten Therapie oder des am besten geeigneten Patienten
Giovanni Rossi, Alessandro Russo, Marco Tagliamento, Alessandro Tuzi, Olga Nigro, Giacomo Vollome, Claudio Sini, Massimiliano Grassi, Maria Giovanna Dal Bello, Simona Coco, Luca Longo, Lodovica Zullo, Enrica Teresa Tanda, Chiara Dellepiane, Paolo Pronzato
Kompass Pneumologie.2020; 8(6): 300. CrossRef - Association with PD-L1 Expression and Clinicopathological Features in 1000 Lung Cancers: A Large Single-Institution Study of Surgically Resected Lung Cancers with a High Prevalence of EGFR Mutation
Seung Eun Lee, Yu Jin Kim, Minjung Sung, Mi-Sook Lee, Joungho Han, Hong Kwan Kim, Yoon-La Choi
International Journal of Molecular Sciences.2019; 20(19): 4794. CrossRef - Detailed Characterization of Immune Cell Infiltrate and Expression of Immune Checkpoint Molecules PD-L1/CTLA-4 and MMR Proteins in Testicular Germ Cell Tumors Disclose Novel Disease Biomarkers
João Lobo, Ângelo Rodrigues, Rita Guimarães, Mariana Cantante, Paula Lopes, Joaquina Maurício, Jorge Oliveira, Carmen Jerónimo, Rui Henrique
Cancers.2019; 11(10): 1535. CrossRef - Basis of PD1/PD-L1 Therapies
Barbara Seliger
Journal of Clinical Medicine.2019; 8(12): 2168. CrossRef
- Impact of patient and tumor characteristics on various aspects of the non-small cell lung cancer patient journey in Romania, Bulgaria, Serbia: A multicenter, non-interventional, retrospective cohort study
- Association between Expression of 8-OHdG and Cigarette Smoking in Non-small Cell Lung Cancer
- Ae Ri An, Kyoung Min Kim, Ho Sung Park, Kyu Yun Jang, Woo Sung Moon, Myoung Jae Kang, Yong Chul Lee, Jong Hun Kim, Han Jung Chae, Myoung Ja Chung
- J Pathol Transl Med. 2019;53(4):217-224. Published online March 11, 2019
- DOI: https://doi.org/10.4132/jptm.2019.02.20
- 9,619 View
- 247 Download
- 22 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Exposure to cigarette smoking (CS) is a major risk factor for the development of lung cancer. CS is known to cause oxidative DNA damage and mutation of tumor-related genes, and these factors are involved in carcinogenesis. 8-Hydroxydeoxyguanosine (8-OHdG) is considered to be a reliable biomarker for oxidative DNA damage. Increased levels of 8-OHdG are associated with a number of pathological conditions, including cancer. There are no reports on the expression of 8-OHdG by immunohistochemistry in non-small cell lung cancer (NSCLC).
Methods
We investigated the expression of 8-OHdG and p53 in 203 NSCLC tissues using immunohistochemistry and correlated it with clinicopathological features including smoking.
Results
The expression of 8-OHdG was observed in 83.3% of NSCLC. It was significantly correlated with a low T category, negative lymph node status, never-smoker, and longer overall survival (p < .05) by univariate analysis. But multivariate analysis revealed that 8-OHdG was not an independent prognostic factor for overall survival in NSCLC patients. The aberrant expression of p53 significantly correlated with smoking, male, squamous cell carcinoma, and Ki-67 positivity (p < .05).
Conclusions
The expression of 8-OHdG was associated with good prognostic factors. It was positively correlated with never-smokers in NSCLC, suggesting that oxidative damage of DNA cannot be explained by smoking alone and may depend on complex control mechanisms. -
Citations
Citations to this article as recorded by- Sustainable framework for automated segmentation and prediction of lung cancer in CT image using CapsNet with U-net segmentation
S.R. Vijayakumar, S. Aarthy, D. Deepa, P. Suresh
Biomedical Signal Processing and Control.2025; 99: 106873. CrossRef - Endolysosomal cation channel MCOLN as the novel regulator of redox homeostasis
Yahao Gao, Lei Xu, Ying Chen
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2025; 1871(7): 167910. CrossRef - Catalase: The golden key to regulate oxidative stress in breast cancer
Jia-Wei Liu, Wen-Jia Chen, Yang-Zheng Lan, Jing Liu
World Journal of Clinical Oncology.2025;[Epub] CrossRef - Association of sirtuin 1 rs10997868 and rs730821 polymorphisms with sirtuin 1 and hydroxy-2′-deoxyguanosine levels in healthy smokers: A case–control study
Samar Sultan
Journal of International Medical Research.2025;[Epub] CrossRef - Increased pretreatment triglyceride glucose-body mass index associated with poor prognosis in patients with advanced non-small cell lung cancer
Shaoming Guo, Yi Zhao, Yue Jiang, Huaping Ye, Ying Wang
Clinical Nutrition ESPEN.2024; 59: 412. CrossRef - Oxidative Damage and Telomere Length as Markers of Lung Cancer Development among Chronic Obstructive Pulmonary Disease (COPD) Smokers
Elizabeth Córdoba-Lanús, Luis M. Montuenga, Angélica Domínguez-de-Barros, Alexis Oliva, Delia Mayato, Ana Remírez-Sanz, Francisca Gonzalvo, Bartolomé Celli, Javier J. Zulueta, Ciro Casanova
Antioxidants.2024; 13(2): 156. CrossRef - Automated determination of 8-OHdG in cells and tissue via immunofluorescence using a specially created antibody
Tobias Jung, Nicole Findik, Bianca Hartmann, Katja Hanack, Kai Grossmann, Dirk Roggenbuck, Marc Wegmann, René Mantke, Markus Deckert, Tilman Grune
Biotechnology Reports.2024; 42: e00833. CrossRef - Combination treatment of zinc and selenium intervention ameliorated BPA-exposed germ cell damage in SD rats: elucidation of molecular mechanisms
Chittaranjan Sahu, Gopabandhu Jena
Naunyn-Schmiedeberg's Archives of Pharmacology.2024; 397(9): 6685. CrossRef - Interplay of arsenic exposure and cigarette smoking on oxidative DNA damage in healthy males
Sepideh Nemati-Mansour, Mohammad Mosaferi, Javad Babaie, Asghar Mohammadpoorasl, Reza Dehghanzadeh, Leila Nikniaz, Mohammad Miri
Environmental Sciences Europe.2024;[Epub] CrossRef - The role of tissue persistent organic pollutants and genetic polymorphisms in patients with benign and malignant kidney tumors
Rasih Kocagöz, İlgen Onat, Merve Demirbügen Öz, Burak Turna, Banu Sarsık Kumbaracı, Mehmet Nurullah Orman, Halit Sinan Süzen, Hilmi Orhan
Environmental Toxicology and Pharmacology.2024; 110: 104495. CrossRef - Mitochondrial Plasticity and Glucose Metabolic Alterations in Human Cancer under Oxidative Stress—From Viewpoints of Chronic Inflammation and Neutrophil Extracellular Traps (NETs)
Hui-Ting Lee, Chen-Sung Lin, Chao-Yu Liu, Po Chen, Chang-Youh Tsai, Yau-Huei Wei
International Journal of Molecular Sciences.2024; 25(17): 9458. CrossRef - Oxidative DNA Damage and Arterial Hypertension in Light of Current ESC Guidelines
Radka Hazuková, Zdeněk Zadák, Miloslav Pleskot, Petr Zdráhal, Martin Pumprla, Miloš Táborský
International Journal of Molecular Sciences.2024; 25(23): 12557. CrossRef - Significance of 8-OHdG Expression as a Predictor of Survival in Colorectal Cancer
Myunghee Kang, Soyeon Jeong, Sungjin Park, Seungyoon Nam, Jun-Won Chung, Kyoung Oh Kim, Jungsuk An, Jung Ho Kim
Cancers.2023; 15(18): 4613. CrossRef - Serum 8-Hydroxy-2′-deoxyguanosine Predicts Severity and Prognosis of Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease
Peng Cao, Chen Zhang, Dong-Xu Hua, Meng-Die Li, Bian-Bian Lv, Lin Fu, Hui Zhao
Lung.2022; 200(1): 31. CrossRef - Redox signaling at the crossroads of human health and disease
Jing Zuo, Zhe Zhang, Maochao Luo, Li Zhou, Edouard C. Nice, Wei Zhang, Chuang Wang, Canhua Huang
MedComm.2022;[Epub] CrossRef - Assessment of MDA and 8-OHdG expressions in ovine pulmonary adenocarcinomas by immunohistochemical and immunofluorescence methods
Emin Karakurt, Enver Beytut, Serpil Dağ, Hilmi Nuhoğlu, Ayfer Yıldız, Emre Kurtbaş
Acta Veterinaria Brno.2022; 91(3): 235. CrossRef - Dietary Antioxidants and Lung Cancer Risk in Smokers and Non-Smokers
Naser A. Alsharairi
Healthcare.2022; 10(12): 2501. CrossRef - Targeting oxidative stress in disease: promise and limitations of antioxidant therapy
Henry Jay Forman, Hongqiao Zhang
Nature Reviews Drug Discovery.2021; 20(9): 689. CrossRef - Association between tobacco substance usage and a missense mutation in the tumor suppressor gene P53 in the Saudi Arabian population
Mikhlid H. Almutairi, Bader O. Almutairi, Turki M. Alrubie, Sultan N. Alharbi, Narasimha R. Parine, Abdulwahed F. Alrefaei, Ibrahim Aldeailej, Abdullah Alamri, Abdelhabib Semlali, Alvaro Galli
PLOS ONE.2021; 16(1): e0245133. CrossRef - Measurement of uranium concentrations in urine samples of adult healthy groups in Najaf governorate with estimation of urine concentrations of 8-OHdG compound as biomarker for DNA damage
Samia K. Abbas, Dhuha S. Saleh, Hayder S. Hussain
Journal of Physics: Conference Series.2021; 1879(3): 032097. CrossRef - Common Data Model and Database System Development for the Korea Biobank Network
Soo-Jeong Ko, Wona Choi, Ki-Hoon Kim, Seo-Joon Lee, Haesook Min, Seol-Whan Oh, In Young Choi
Applied Sciences.2021; 11(24): 11825. CrossRef - EVALUATION OF OXIDATIVE STATUS IN PATIENTS WITH CHRONIC PERIODONTITIS AND ADDITIONAL TOBACCO ABUSE: A CROSS-SECTIONAL STUDY
Didem ÖZKAL EMİNOĞLU, Varol ÇANAKÇI
Atatürk Üniversitesi Diş Hekimliği Fakültesi Dergisi.2020; : 1. CrossRef
- Sustainable framework for automated segmentation and prediction of lung cancer in CT image using CapsNet with U-net segmentation
- Human Leukocyte Antigen Class I and Programmed Death-Ligand 1 Coexpression Is an Independent Poor Prognostic Factor in Adenocarcinoma of the Lung
- Yeon Bi Han, Hyun Jung Kwon, Soo Young Park, Eun-Sun Kim, Hyojin Kim, Jin-Haeng Chung
- J Pathol Transl Med. 2019;53(2):86-93. Published online January 14, 2019
- DOI: https://doi.org/10.4132/jptm.2018.12.26
- 7,833 View
- 136 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Both human leukocyte antigen (HLA) class I and programmed death-ligand 1 (PD-L1) molecules are known to play important roles in cancer immunity. In this study, we evaluated HLA class I expression in resected adenocarcinoma of the lung, and investigated its prognostic impact in correlation with PD-L1 expression.
Methods
HLA class I and PD-L1 expression was evaluated by immunohistochemistry in a total of 403 resected lung adenocarcinomas using tissue microarray. Correlations between the expression of HLA class I/PD-L1 and clinicopathologic features and prognostic significance were analyzed.
Results
HLA class I expression was reduced in 91.6% of adenocarcinoma, and more frequently reduced in patients with younger age, absence of vascular invasion, and low pathologic stage (p = .033, p = .007, and p = .012, respectively). Positive PD-L1 expression in tumor cells was 16.1% (1% cut-off), and associated with poor differentiation, presence of vascular invasion and nodal metastasis (p < .001, p = .002, and p = .032, respectively). On survival analysis, HLA class I or PD-L1 expression alone did not show any statistical significance. On the integrated analysis, HLA class I (+)/PD-L1 (+) subgroup showed a significantly shorter overall survival than other groups (p = .001). Multivariate analysis revealed that coexpression of HLA class I and PD-L1 was an independent poor prognostic factor of lung adenocarcinoma. (p < .001; hazard ratio, 6.106; 95% confidence interval, 2.260 to 16.501).
Conclusions
Lung adenocarcinoma with coexpression of HLA class I and PD-L1 was associated with poor prognosis. This subgroup may evade immune attack by expressing PD-L1 protein despite HLA expression. -
Citations
Citations to this article as recorded by- Assessment of cancer cell‐expressed HLA class I molecules and their immunopathological implications
Terufumi Kubo, Shiori Asano, Kenta Sasaki, Kenji Murata, Takayuki Kanaseki, Tomohide Tsukahara, Yoshihiko Hirohashi, Toshihiko Torigoe
HLA.2024;[Epub] CrossRef - Prognostic and Clinical Significance of Human Leukocyte Antigen Class I Expression in Breast Cancer: A Meta-Analysis
Weiqiang Qiao, Zhiqiang Jia, Wanying Guo, Qipeng Liu, Xiao Guo, Miao Deng
Molecular Diagnosis & Therapy.2023; 27(5): 573. CrossRef - Loss of HLA-class-I expression in non-small-cell lung cancer: Association with prognosis and anaerobic metabolism
Ioannis M. Koukourakis, Alexandra Giatromanolaki, Achilleas Mitrakas, Michael I. Koukourakis
Cellular Immunology.2022; 373: 104495. CrossRef
- Assessment of cancer cell‐expressed HLA class I molecules and their immunopathological implications
- Prognostic Role of S100A8 and S100A9 Protein Expressions in Non-small Cell Carcinoma of the Lung
- Hyun Min Koh, Hyo Jung An, Gyung Hyuck Ko, Jeong Hee Lee, Jong Sil Lee, Dong Chul Kim, Jung Wook Yang, Min Hye Kim, Sung Hwan Kim, Kyung Nyeo Jeon, Gyeong-Won Lee, Se Min Jang, Dae Hyun Song
- J Pathol Transl Med. 2019;53(1):13-22. Published online November 26, 2018
- DOI: https://doi.org/10.4132/jptm.2018.11.12
- 9,547 View
- 249 Download
- 17 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
S100A8 and S100A9 have been gaining recognition for modulating tumor growthand metastasis. This study aimed at evaluating the clinical significance of S100A8 and S100A9 innon-small cell lung cancer (NSCLC).
Methods
We analyzed the relationship between S100A8and S100A9 expressions, clinicopathological characteristics, and prognostic significance in tumorcells and peritumoral inflammatory cells.
Results
The positive staining of S100A8 in tumorcells was significantly increased in male (p < .001), smoker (p = .034), surgical method other thanlobectomy (p = .024), squamous cell carcinoma (SQCC) (p < .001) and higher TNM stage (p = .022)compared with female, non-smoker, lobectomy, adenocarcinoma (ADC), and lower stage. Theproportion of tumor cells stained for S100A8 was related to histologic type (p < .001) and patientsex (p = .027). The proportion of inflammatory cells stained for S100A8 was correlated with patientage (p = .022), whereas the proportion of inflammatory cells stained for S100A9 was correlatedwith patient sex (p < .001) and smoking history (p = .031). Moreover, positive staining in tumorcells, more than 50% of the tumor cells stained and less than 30% of the inflammatory cellsstained for S100A8 and S100A9 suggested a tendency towards increased survivability in SQCCbut towards decreased survivability in ADC.
Conclusions
S100A8 and S100A9 expressions might be potential prognostic markers in patients with NSCLC. -
Citations
Citations to this article as recorded by- S100A8 as a potential therapeutic target for cancer metastasis
Atsuko Deguchi, Yoshiro Maru
Cancer Science.2025; 116(2): 322. CrossRef - Identifying candidate biomarkers for detecting bronchogenic carcinoma stages using metaheuristic algorithms based on information fusion theory
Bagher Khalvati, Kaveh Kavousi, Amir Hosein Keyhanipour, Masoud Arabfard
Discover Oncology.2025;[Epub] CrossRef - A review on clinical implications of S100 proteins in lung diseases
Vineesh V. Raveendran, Somaya AlQattan, Eid AlMutairy
Frontiers in Medicine.2025;[Epub] CrossRef - Differential Expression of S100A8 in Tumor and Immune Compartments of Endometrial Carcinoma and Its Clinical Relevance
Dae Hyun Song, Min Hye Kim, Juseok Yang, Hyen Chul Jo, Ji Eun Park, Jong Chul Baek
Medicina.2025; 61(11): 1918. CrossRef - The role of S100A8 and S100A9 in external auditory canal cholesteatoma
Guanwen He, Weijing Han, Zhongshou Zhu, Rifu Wei, Chang Lin
Frontiers in Immunology.2024;[Epub] CrossRef - Gene expression related to lung cancer altered by PHMG-p treatment in PBTE cells
Yoon Hee Park, Sang Hoon Jeong, Hyejin Lee, Cherry Kim, Yoon Jeong Nam, Ja Young Kang, Jin Young Choi, Yu-Seon Lee, Su A. Park, Jaeyoung Kim, Eun-Kee Park, Yong-Wook Baek, Hong Lee, Ju-Han Lee
Molecular & Cellular Toxicology.2023; 19(1): 205. CrossRef - Discovery of protein biomarkers for venous thromboembolism in non-small cell lung cancer patients through data-independent acquisition mass spectrometry
Yanhong Liu, Lan Gao, Yanru Fan, Rufei Ma, Yunxia An, Guanghui Chen, Yan Xie
Frontiers in Oncology.2023;[Epub] CrossRef - S100A8 and S100A9 in Cancer
Yu Chen, Yuzhen Ouyang, Zhixin Li, Xiufang Wang, Jian Ma
Biochimica et Biophysica Acta (BBA) - Reviews on Cancer.2023; 1878(3): 188891. CrossRef - Gene expression of S100a8/a9 predicts Staphylococcus aureus-induced septic arthritis in mice
Meghshree Deshmukh, Santhilal Subhash, Zhicheng Hu, Majd Mohammad, Anders Jarneborn, Rille Pullerits, Tao Jin, Pradeep Kumar Kopparapu
Frontiers in Microbiology.2023;[Epub] CrossRef - Single-cell immunophenotyping revealed the association of CD4+ central and CD4+ effector memory T cells linking exacerbating chronic obstructive pulmonary disease and NSCLC
Nikolett Gémes, József Á. Balog, Patrícia Neuperger, Erzsébet Schlegl, Imre Barta, János Fillinger, Balázs Antus, Ágnes Zvara, Zoltán Hegedűs, Zsolt Czimmerer, Máté Manczinger, Gergő Mihály Balogh, József Tóvári, László G. Puskás, Gábor J. Szebeni
Frontiers in Immunology.2023;[Epub] CrossRef - A Prognostic Gene Signature for Hepatocellular Carcinoma
Rong Chen, Meng Zhao, Yanli An, Dongfang Liu, Qiusha Tang, Gaojun Teng
Frontiers in Oncology.2022;[Epub] CrossRef - The S100 protein family in lung cancer
Ting Wang, Ge Du, Dong Wang
Clinica Chimica Acta.2021; 520: 67. CrossRef - The associations of serum S100A9 with the severity and prognosis in patients with community-acquired pneumonia: a prospective cohort study
Hong-Yan Liu, Hui-Xian Xiang, Ying Xiang, Zheng Xu, Chun-Mei Feng, Jun Fei, Lin Fu, Hui Zhao
BMC Infectious Diseases.2021;[Epub] CrossRef - Saliva proteomic analysis reveals possible biomarkers of renal cell carcinoma
Xiao Li Zhang, Zheng Zhi Wu, Yun Xu, Ji Guo Wang, Yong Qiang Wang, Mei Qun Cao, Chang Hao Wang
Open Chemistry.2020; 18(1): 918. CrossRef - Prognostic Role of S100A8 in Human Solid Cancers: A Systematic Review and Validation
An Huang, Wei Fan, Jiacui Liu, Ben Huang, Qingyuan Cheng, Ping Wang, Yiping Duan, Tiantian Ma, Liangyue Chen, Yanping Wang, Mingxia Yu
Frontiers in Oncology.2020;[Epub] CrossRef
- S100A8 as a potential therapeutic target for cancer metastasis
- p40 Immunohistochemistry Is an Excellent Marker in Primary Lung Squamous Cell Carcinoma
- Khairunisa Ahmad Affandi, Nur Maya Sabrina Tizen, Muaatamarulain Mustangin, Reena Rahayu MdReena Rahayu Md Zin
- J Pathol Transl Med. 2018;52(5):283-289. Published online August 31, 2018
- DOI: https://doi.org/10.4132/jptm.2018.08.14
- 25,950 View
- 346 Download
- 34 Web of Science
- 38 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Lung cancer is the third most common cancer worldwide. With major advances in the molecular testing of lung cancers and the introduction of targeted therapies, the distinction between adenocarcinoma and squamous cell carcinoma as well as pathologic subtyping has become important. Recent studies showed that p40 is highly specific for squamous and basal cells and is superior to p63 for diagnosing lung squamous cell carcinoma. The aim of this study was to evaluate the use of p40 immunohistochemical stain in the diagnosis of non-small cell lung carcinoma and its potential to replace current p63 antibody as the best immunohistochemical squamous marker.
Methods
Seventy formalin-fixed paraffin-embedded cases previously diagnosed as primary lung squamous cell carcinoma (n = 35) and lung adenocarcinoma (n = 35) from January 2008 to December 2016 were retrieved. The results of tumour cell immunoreactivity for p40 and p63 antibodies in lung squamous cell carcinoma and lung adenocarcinoma were compared.
Results
p40 was expressed in 27 cases of lung squamous cell carcinoma (77.1%). All cases of lung adenocarcinoma (35/35, 100%) were negative for p40. p63 expression was positive in 30 cases of lung squamous cell carcinoma (85.7%) and 13 cases of lung adenocarcinoma (37.1%). Reactivity for both p40 and p63 in lung squamous cell carcinoma was strong and diffuse, whereas variable reactivity was observed in lung adenocarcinoma.
Conclusions
p40 is an excellent marker for distinguishing lung squamous cell carcinoma from adenocarcinoma, and p40 expression is equivalent to p63 expression in lung squamous cell carcinoma. -
Citations
Citations to this article as recorded by- Immunohistochemical expression of ΔNp63 versus pan-p63 in normal and neoplastic feline tissues
Igor R. Santos, Carolina B. Brunner, Milena C. Paz, Gabriela Hartmann, Gabrielle Z. Tres, Luciana Sonne, Welden Panziera, David Driemeier, Marcele B. Bandinelli, Saulo P. Pavarini
Veterinary Pathology.2026;[Epub] CrossRef - Partial Response to Repotrectinib in ROS1-Rearranged Lung Squamous Cell Carcinoma: A Brief Report
Yukiko Yoshida, Hajime Asahina, Ken Kuwahara, Hidenori Mizugaki, Noriyuki Yamada, Hiroshi Yokouchi, Naohiro Nomura, Yoshihiro Matsuno, Satoshi Oizumi
Clinical Lung Cancer.2026;[Epub] CrossRef - Morphologic and immunohistochemical study of HPV-related cervical adenosquamous carcinoma: Reappraisal of a poorly defined entity
Zhenwei Zhang, M. Ruhul Quddus, C James Sung, Kamaljeet Singh
Human Pathology.2026; 170: 106052. CrossRef - Cancer of Unknown Primary With Squamous Cell Carcinoma Phenotype Presenting as Isolated Axillary Mass
Nicole Liang, Mohamed Alshal, Lynne J Goebel
Cureus.2025;[Epub] CrossRef - A critical appraisal of the clinico-radiological, histopathological and immunohistochemical profile of CT-guided and bronchoscopy-guided biopsies in lung lesions
Mukta Pujani, Ruchi Arora Sachdeva, S. Zafar Abbas, Charu Agarwal, Minakshi Bhardwaj, Varsha Chauhan, Jyoti Rajpoot, Dipti Sidam, Aniruna Dey
Lung India.2025; 42(3): 218. CrossRef - An Organoid Model for Translational Cancer Research Recapitulates Histoarchitecture and Molecular Hallmarks of Non-Small-Cell Lung Cancer
Camilla T. Ekanger, Maria P. Ramnefjell, Maren S. F. Guttormsen, Joakim Hekland, Kristin Dahl-Michelsen, Maria L. Lotsberg, Ning Lu, Linda E. B. Stuhr, Laurence Hoareau, Pirjo-Riitta Salminen, Fabian Gärtner, Marianne Aanerud, Lars A. Akslen, James B. Lor
Cancers.2025; 17(11): 1873. CrossRef - Accessing utility of immunohistochemistry, PD-L1 correlation with stage of cancer and EGFR mutation with disease survival in primary lung carcinoma
Kartavya Kumar Verma, Amit Bugalia, Ajoy Kumar behera, Nighat Hussain
Surgical and Experimental Pathology.2025;[Epub] CrossRef - Small intestinal SMARCA4‑deficient undifferentiated carcinoma with intussusception: A case report
Xiaoshan Cai, Shanshan Liu, Linqian Li, Yuming Zhang, Qin Guo, Ze Chen, Meihua Qu, Yubing Wang, Ben Yang, Xianwen Yue
Oncology Letters.2025; 31(2): 1. CrossRef - Clinicopathological and molecular perspectives on thoracic SMARCA4-deficient undifferentiated tumors and SMARCA4-deficient non-small cell lung carcinomas
Sumanta Das, Pallavi Mishra, Sunita Ahlawat
Pathologica.2025; 117(5): 455. CrossRef - Clinico-Pathological Profile of Non-Small Cell Lung Carcinoma with Emphasis on Diagnostic Immunohistochemistry – An Institutional Experience
Shubhika Rao Sachdeva, Bhavna Nayal, Ananth Pai
Medical Journal of Dr. D.Y. Patil Vidyapeeth.2025; 18(Suppl 2): S288. CrossRef - Lack of imbalance between the master regulators TTF1/NKX2-1 and ΔNp63/p40 implies adverse prognosis in non-small cell lung cancer
Martina Vescio, Matteo Bulloni, Giuseppe Pelosi, Linda Pattini
Scientific Reports.2024;[Epub] CrossRef - Adeno-to-squamous transition drives resistance to KRAS inhibition in LKB1 mutant lung cancer
Xinyuan Tong, Ayushi S. Patel, Eejung Kim, Hongjun Li, Yueqing Chen, Shuai Li, Shengwu Liu, Julien Dilly, Kevin S. Kapner, Ningxia Zhang, Yun Xue, Laura Hover, Suman Mukhopadhyay, Fiona Sherman, Khrystyna Myndzar, Priyanka Sahu, Yijun Gao, Fei Li, Fuming
Cancer Cell.2024; 42(3): 413. CrossRef - Common practice issues in pulmonary cytology/small biopsy: Diagnostic pitfalls and appropriate use of immunohistochemical stains
Jessie Xiong, Erik Polsdofer, Jian Jing
Human Pathology Reports.2024; 36: 300735. CrossRef - Integrating AI-Powered Digital Pathology and Imaging Mass Cytometry Identifies Key Classifiers of Tumor Cells, Stroma, and Immune Cells in Non–Small Cell Lung Cancer
Alessandra Rigamonti, Marika Viatore, Rebecca Polidori, Daoud Rahal, Marco Erreni, Maria Rita Fumagalli, Damiano Zanini, Andrea Doni, Anna Rita Putignano, Paola Bossi, Emanuele Voulaz, Marco Alloisio, Sabrina Rossi, Paolo Andrea Zucali, Armando Santoro, V
Cancer Research.2024; 84(7): 1165. CrossRef - Advances in combined neuroendocrine carcinoma of lung cancer
Zesen Han, Fujun Yang, Fang Wang, Huayu Zheng, Xiujian Chen, Hongyu Meng, Fenglei Li
Pathology and Oncology Research.2024;[Epub] CrossRef - Evolving Precision First-Line Systemic Treatment for Patients with Unresectable Non-Small Cell Lung Cancer
Tianhong Li, Weijie Ma, Ebaa Al-Obeidi
Cancers.2024; 16(13): 2350. CrossRef - Antibody-Conjugated Nanodiamond Enzyme for Targeted Non-Small-Cell Lung Cancer by Regulating Oxidative Stress
Xiaoying Guan, Jingwen Yang, Ziying Liu, Guowei Yang, Xiumei Tian
ACS Applied Nano Materials.2024; 7(20): 23670. CrossRef - Multifocal Pulmonary Opacities in an Elderly Smoker
Patton C McClelland, Zachary Jarrett, Christian C Lamb, Mateo Houle
Cureus.2024;[Epub] CrossRef - Clonal dynamics and Stereo-seq resolve origin and phenotypic plasticity of adenosquamous carcinoma
Ruiying Zhao, Yunhua Xu, Yedan Chen, Jiajun Zhang, Fei Teng, Sha Liao, Shengnan Chen, Qian Wu, Chan Xiang, Jiaohui Pang, Zhanxian Shang, Jikai Zhao, Hairong Bao, Hua Bao, Yang Shao, Shun Lu, Yuchen Han
npj Precision Oncology.2023;[Epub] CrossRef - Keratin 5 in Lung Cancer Specimens: Comparison of Four Antibody Clones and KRT5 mRNA-ISH
Christian Thomsen, Laura Blok-Husum, Jeanette Bæhr Georgsen, Torben Steiniche, Mogens Vyberg
Applied Immunohistochemistry & Molecular Morphology.2023; 31(6): 347. CrossRef - Carcinoma of unknown primary (CUP): an update for histopathologists
Katie Beauchamp, Bruce Moran, Timothy O’Brien, Donal Brennan, John Crown, Kieran Sheahan, Maura Bríd Cotter
Cancer and Metastasis Reviews.2023; 42(4): 1189. CrossRef - Advances in Genomic Data and Biomarkers: Revolutionizing NSCLC Diagnosis and Treatment
Juan Carlos Restrepo, Diana Dueñas, Zuray Corredor, Yamil Liscano
Cancers.2023; 15(13): 3474. CrossRef - Kallikrein-related peptidase 13 expression and clinicopathological features in lung squamous cell carcinoma
Ryusuke Sumiya, Kazuhiko Yamada, Teruki Hagiwara, Satoshi Nagasaka, Hideki Miyazaki, Toru Igari, Yuki Kawamura
Molecular and Clinical Oncology.2023;[Epub] CrossRef - Pre-clinical lung squamous cell carcinoma mouse models to identify novel biomarkers and therapeutic interventions
Priyanka Sahu, Chantal Donovan, Keshav Raj Paudel, Sophie Pickles, Vrushali Chimankar, Richard Y. Kim, Jay C. Horvart, Kamal Dua, Antonio Ieni, Francesco Nucera, Helle Bielefeldt-Ohmann, Sarah Mazilli, Gaetano Caramori, J. Guy Lyons, Philip M. Hansbro
Frontiers in Oncology.2023;[Epub] CrossRef - Intraosseous clear cell mucoepidermoid carcinoma: A case report and evaluation
Adesh S. Manchanda, Ramandeep S. Narang, Komaldeep K. Sandhu
Journal of Oral and Maxillofacial Pathology.2023; 27(4): 780. CrossRef - A targeted expression panel for classification, gene fusion detection and PD-L1 measurements – Can molecular profiling replace immunohistochemistry in non-small cell lung cancer?
Anita Tranberg Simonsen, Amalie Utke, Johanne Lade-Keller, Lasse Westphal Thomsen, Torben Steiniche, Magnus Stougaard
Experimental and Molecular Pathology.2022; 125: 104749. CrossRef - Basal cell carcinoma arising in association with maxillary odontogenic keratocyst in a patient with Gorlin-Goltz syndrome
Mutsuki Kawabe, Yoshitane Tsukamoto, Shohei Matuo, Shuji Kanda, Susumu Hashitani
Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology.2022; 34(3): 333. CrossRef - Cutaneous Metastases from Thymic Carcinoma Primary Tumor: A Rare Case
Eva Krishna Sutedja, Trustia Rizqandaru, Kartika Ruchiatan, Endang Sutedja
International Medical Case Reports Journal.2022; Volume 15: 293. CrossRef - Primary nonkeratinizing squamous cell carcinoma of the scapular bone: A case report
Yang Li, Jian-Lin Zuo, Jin-Shuo Tang, Xian-Yue Shen, Sheng-Hao Xu, Jian-Lin Xiao
World Journal of Clinical Cases.2021; 9(4): 976. CrossRef - Survival-associated N6-adenosine methyltransferase signatures in lung squamous cell carcinoma and clinical verification
Jialin Qu, Li Wang, Man Jiang, Zhimin Wei, Guangming Fu, Xiaochun Zhang
BMC Cancer.2021;[Epub] CrossRef - Pulmonary adenomyoma presenting as a right cardiophrenic angle mass
Osigbemhe Iyalomhe, Sam Sadigh, Charuhas Deshpande, Leslie Litzky, Anna Moran, Scott Simpson
Radiology Case Reports.2020; 15(5): 502. CrossRef - Head-to-Head Comparison of p63 and p40 in Non-Neuroendocrine Carcinomas of the Tubal Gut
Ahmed M. Bakhshwin, Ilyssa O. Gordon, Kathryn Bock Brown, Xiuli Liu, Daniela S. Allende
International Journal of Surgical Pathology.2020; 28(8): 835. CrossRef - Greater specificity of p40 compared with p63 in distinguishing squamous cell carcinoma from adenocarcinoma in effusion cellblocks
Nah Ihm Kim, Ji Shin Lee
Cytojournal.2020; 17: 13. CrossRef - Incidental Thyroid Mass in a Patient With Oropharyngeal Squamous Cell Carcinoma
Kinneri Mehta, Misha Movahed-Ezazi, Akshay V. Patel
JAMA Otolaryngology–Head & Neck Surgery.2020; 146(9): 859. CrossRef - Three dimensional texture analysis of noncontrast chest CT in differentiating solitary solid lung squamous cell carcinoma from adenocarcinoma and correlation to immunohistochemical markers
Rui Han, Roshan Arjal, Jin Dong, Hong Jiang, Huan Liu, Dongyou Zhang, Lu Huang
Thoracic Cancer.2020; 11(11): 3099. CrossRef - The role of the immunohistochemical marker p40 in the differential diagnosis of adenocarcinoma and nonkeratinizing squamous cell cancer of the lung
E.M. Olyushina, M.M. Byakhova, L.E. Zavalishina, Yu.Yu. Andreeva, A.B. Semenova, G.A. Frank
Arkhiv patologii.2020; 82(5): 50. CrossRef - Role of Immunocytochemistry in the Cytological Diagnosis of Pulmonary Tumors
Jasna Metovic, Luisella Righi, Luisa Delsedime, Marco Volante, Mauro Papotti
Acta Cytologica.2020; 64(1-2): 16. CrossRef - Subtyping Lung Cancer Using DNA Methylation in Liquid Biopsies
Sandra P. Nunes, Francisca Diniz, Catarina Moreira-Barbosa, Vera Constâncio, Ana Victor Silva, Júlio Oliveira, Marta Soares, Sofia Paulino, Ana Luísa Cunha, Jéssica Rodrigues, Luís Antunes, Rui Henrique, Carmen Jerónimo
Journal of Clinical Medicine.2019; 8(9): 1500. CrossRef
- Immunohistochemical expression of ΔNp63 versus pan-p63 in normal and neoplastic feline tissues
- Molecular Screening of Small Biopsy Samples Using Next-Generation Sequencing in Korean Patients with Advanced Non-small Cell Lung Cancer: Korean Lung Cancer Consortium (KLCC-13-01)
- Bo Mi Ku, Mi Hwa Heo, Joo-Hang Kim, Byoung Chul Cho, Eun Kyung Cho, Young Joo Min, Ki Hyeong Lee, Jong-Mu Sun, Se-Hoon Lee, Jin Seok Ahn, Keunchil Park, Tae Jung Kim, Ho Yun Lee, Hojoong Kim, Kyung-Jong Lee, Myung-Ju Ahn
- J Pathol Transl Med. 2018;52(3):148-156. Published online March 26, 2018
- DOI: https://doi.org/10.4132/jptm.2018.03.12
- 10,655 View
- 315 Download
- 16 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Non-small cell lung cancer (NSCLC) is a common type of cancer with poor prognosis. As individual cancers exhibit unique mutation patterns, identifying and characterizing gene mutations in NSCLC might help predict patient outcomes and guide treatment. The aim of this study was to evaluate the clinical adequacy of molecular testing using next-generation sequencing (NGS) for small biopsy samples and characterize the mutational landscape of Korean patients with advanced NSCLC.
Methods
DNA was extracted from small biopsy samples of 162 patients with advanced NSCLC. Targeted NGS of genomic alterations was conducted using Ion AmpliSeq Cancer Hotspot Panel v2.
Results
The median age of patients was 64 years (range, 32 to 83 years) and the majority had stage IV NSCLC at the time of cancer diagnosis (90%). Among the 162 patients, 161 patients (99.4%) had novel or hotspot mutations (range, 1 to 21 mutated genes). Mutations were found in 41 genes. Three of the most frequently mutated genes were TP53 (151, 93.2%), KDR (104, 64.2%), and epidermal growth factor receptor (EGFR; 69, 42.6%). We also observed coexistence of EGFR and other oncogene (such as KRAS, PIC3CA, PTEN, and STK11) mutations. Given that 69.6% (48/69) of EGFR mutant patients were treated with EGFR tyrosine kinase inhibitors, EGFR mutant status had higher prognostic ability in this study.
Conclusions
These results suggest that targeted NGS using small biopsy samples is feasible and allows for the detection of both common and rare mutations in NSCLC. -
Citations
Citations to this article as recorded by- The clinical relevance of surgical specimens for RNA sequencing in lung cancer: a cohort study
Jung Seop Eom, Soo Han Kim, Kyungbin Kim, Ahrong Kim, Hyo Yeong Ahn, Jeongha Mok, Jeong Su Cho, Min Ki Lee, Ju Sun Song, Mi-Hyun Kim
Frontiers in Oncology.2024;[Epub] CrossRef - PTEN, PTENP1, microRNAs, and ceRNA Networks: Precision Targeting in Cancer Therapeutics
Glena Travis, Eileen M. McGowan, Ann M. Simpson, Deborah J. Marsh, Najah T. Nassif
Cancers.2023; 15(20): 4954. CrossRef - Worldwide Prevalence of Epidermal Growth Factor Receptor Mutations in Non-Small Cell Lung Cancer: A Meta-Analysis
Barbara Melosky, Kato Kambartel, Maik Häntschel, Margherita Bennetts, Dana J. Nickens, Julia Brinkmann, Antonin Kayser, Michael Moran, Federico Cappuzzo
Molecular Diagnosis & Therapy.2022; 26(1): 7. CrossRef - Landscape of EGFR mutations in lung adenocarcinoma: a single institute experience with comparison of PANAMutyper testing and targeted next-generation sequencing
Jeonghyo Lee, Yeon Bi Han, Hyun Jung Kwon, Song Kook Lee, Hyojin Kim, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2022; 56(5): 249. CrossRef - Suitability of transbronchial brushing cytology specimens for next‐generation sequencing in peripheral lung cancer
Naoki Furuya, Shingo Matsumoto, Kazutaka Kakinuma, Kei Morikawa, Takeo Inoue, Hisashi Saji, Koichi Goto, Masamichi Mineshita
Cancer Science.2021; 112(1): 380. CrossRef - KLHL38 involvement in non-small cell lung cancer progression via activation of the Akt signaling pathway
Yitong Xu, Chenglong Wang, Xizi Jiang, Yao Zhang, Hongbo Su, Jun Jiang, Hongjiu Ren, Xueshan Qiu
Cell Death & Disease.2021;[Epub] CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Targeting non-small cell lung cancer: driver mutation beyond epidermal growth factor mutation and anaplastic lymphoma kinase fusion
Quincy S. Chu
Therapeutic Advances in Medical Oncology.2020;[Epub] CrossRef Concomitant Mutations in EGFR 19Del/L858R Mutation and Their Association with Response to EGFR-TKIs in NSCLC Patients
Hengrui Liang, Caichen Li, Yi Zhao, Shen Zhao, Jun Huang, Xiuyu Cai, Bo Cheng, Shan Xiong, Jianfu Li, Wei Wang, Changbin Zhu, Weiwei Li, Jianxing He, Wenhua Liang
Cancer Management and Research.2020; Volume 12: 8653. CrossRef- Prognostic role of Rab27A and Rab27B expression in patients with non‐small cell lung carcinoma
Hyun Min Koh, Dae Hyun Song
Thoracic Cancer.2019; 10(2): 143. CrossRef - PD‐L1 expression in ROS1‐rearranged non‐small cell lung cancer: A study using simultaneous genotypic screening of EGFR, ALK, and ROS1
Jongmin Lee, Chan Kwon Park, Hyoung‐Kyu Yoon, Young Jo Sa, In Sook Woo, Hyo Rim Kim, Sue Youn Kim, Tae‐Jung Kim
Thoracic Cancer.2019; 10(1): 103. CrossRef - Targeted Next-Generation Sequencing Validates the Use of Diagnostic Biopsies as a Suitable Alternative to Resection Material for Mutation Screening in Colorectal Cancer
Hersh A. Ham-Karim, Henry Okuchukwu Ebili, Kirsty Manger, Wakkas Fadhil, Narmeen S. Ahmad, Susan D. Richman, Mohammad Ilyas
Molecular Diagnosis & Therapy.2019; 23(3): 383. CrossRef - Small lung tumor biopsy samples are feasible for high quality targeted next generation sequencing
Hidenori Kage, Shinji Kohsaka, Aya Shinozaki‐Ushiku, Yoshihisa Hiraishi, Jiro Sato, Kazuhiro Nagayama, Tetsuo Ushiku, Daiya Takai, Jun Nakajima, Kiyoshi Miyagawa, Hiroyuki Aburatani, Hiroyuki Mano, Takahide Nagase
Cancer Science.2019; 110(8): 2652. CrossRef - PTEN in Lung Cancer: Dealing with the Problem, Building on New Knowledge and Turning the Game Around
Anastasios Gkountakos, Giulia Sartori, Italia Falcone, Geny Piro, Ludovica Ciuffreda, Carmine Carbone, Giampaolo Tortora, Aldo Scarpa, Emilio Bria, Michele Milella, Rafael Rosell, Vincenzo Corbo, Sara Pilotto
Cancers.2019; 11(8): 1141. CrossRef
- The clinical relevance of surgical specimens for RNA sequencing in lung cancer: a cohort study
- Transformation to Small Cell Lung Cancer of Pulmonary Adenocarcinoma: Clinicopathologic Analysis of Six Cases
- Soomin Ahn, Soo Hyun Hwang, Joungho Han, Yoon-La Choi, Se-Hoon Lee, Jin Seok Ahn, Keunchil Park, Myung-Ju Ahn, Woong-Yang Park
- J Pathol Transl Med. 2016;50(4):258-263. Published online May 10, 2016
- DOI: https://doi.org/10.4132/jptm.2016.04.19
- 14,090 View
- 253 Download
- 53 Web of Science
- 49 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) are considered the first line treatment for a subset of EGFR-mutated non-small cell lung cancer (NSCLC) patients. Although transformation to small cell lung cancer (SCLC) is one of the known mechanisms of resistance to EGFR TKIs, it is not certain whether transformation to SCLC is exclusively found as a mechanism of TKI resistance in EGFR-mutant tumors.
Methods
We identified six patients with primary lung adenocarcinoma that showed transformation to SCLC on second biopsy (n = 401) during a 6-year period. Clinicopathologic information was analyzed and EGFR mutation results were compared between initial and second biopsy samples.
Results
Six patients showed transformation from adenocarcinoma to SCLC, of which four were pure SCLCs and two were combined adenocarcinoma and SCLCs. Clinically, four cases were EGFR-mutant tumors from non-smoking females who underwent TKI treatment, and the EGFR mutation was retained in the transformed SCLC tumors. The remaining two adenocarcinomas were EGFR wild-type, and one of these patients received EGFR TKI treatment.
Conclusions
NSCLC can acquire a neuroendocrine phenotype with or without EGFR TKI treatment. -
Citations
Citations to this article as recorded by- Patients outcomes in lung adenocarcinoma transforming to small-cell lung cancer after tyrosine kinase inhibitor therapy
Shuai Wang, Yongsen Wang, Xuan Wu, Li Yang, Xiaoju Zhang
World Journal of Surgical Oncology.2025;[Epub] CrossRef - Baseline retinoblastoma transcriptional corepressor 1 (Rb1) functional inactivation is a pre-requisite but not sufficient for small-cell histological transformation in epidermal growth factor receptor (EGFR) mutant lung adenocarcinomas post-tyrosine kinas
Aruna Nambirajan, Amber Rathor, Hemavathi Baskarane, Anju GS, Sachin Khurana, Somagattu Sushmitha, Aparna Sharma, Prabhat Singh Malik, Deepali Jain
Virchows Archiv.2025; 487(3): 639. CrossRef - Case Report: Transforming small cell lung cancer: two cases report and literature review
Jinlong Liu, Jing Ai, Lize Zhao, Yimeng Qian, Qingxin Zhao, Chunling Ma, Yu Zhao, Jing Zhao
Frontiers in Oncology.2025;[Epub] CrossRef - Exploration of CT-based discrimination and diagnosis of various pathological types of ground glass nodules in the lungs
Haihui Wu, Xiong Zhang, Zheng Zhong
BMC Medical Imaging.2025;[Epub] CrossRef - Correlation between treatments and outcomes of patients with EGFR-mutated non-small-cell lung cancer that transitioned into small-cell lung cancer: an international retrospective study
C. Catania, S.V. Liu, M. Garassino, A. Delmonte, V. Scotti, F. Cappuzzo, C. Genova, A. Russo, M. Russano, C. Bennati, I. Colantonio, S. Martini, M. Pino, F. Conforti, L. Pala, G. Minuti, F. Citarella, E. Olmetto, A. Esposito, P. Cascetta, A. Di Lello, T.
ESMO Open.2025; 10(7): 105326. CrossRef - TPM3–NTRK1 fusion confers resistance to osimertinib in lung adenocarcinoma: a model in a continuous cell line
Fang Cao, Jiayin Dai, Kun Dong, Zhenli Yang, Yanli Zhu, Changsong Qi, Dongmei Lin, Xiaocui Bian, Yuqin Liu
Human Cell.2025;[Epub] CrossRef - Small cell lung cancer transdifferentiation: not a negligible phenomenon
Lilla Horvath, Kristiina Boettiger, Zsolt Megyesfalvi, Balázs Döme, Clemens Aigner, Anita Horváth-Rózsás, Judit Berta
Current Opinion in Oncology.2025;[Epub] CrossRef - Transformation to small cell lung cancer is irrespective of EGFR and accelerated by SMAD4-mediated ASCL1 transcription independently of RB1 in non-small cell lung cancer
Xi Ding, Min-xing Shi, Di Liu, Jing-xue Cao, Kai-xuan Zhang, Run-dong Zhang, Li-ping Zhang, Kai-xing Ai, Bo Su, Jie Zhang
Cell Communication and Signaling.2024;[Epub] CrossRef - The study of primary and acquired resistance to first-line osimertinib to improve the outcome of EGFR-mutated advanced Non-small cell lung cancer patients: the challenge is open for new therapeutic strategies
Alessandra Ferro, Gian Marco Marinato, Cristiana Mulargiu, Monica Marino, Giulia Pasello, Valentina Guarneri, Laura Bonanno
Critical Reviews in Oncology/Hematology.2024; 196: 104295. CrossRef - Comprehensive molecular and clinical insights into non-small cell lung cancer transformation to small cell lung cancer with an illustrative case report
Kresimir Tomic, Kristina Krpina, Lara Baticic, Miroslav Samarzija, Semir Vranic
Journal of Drug Targeting.2024; 32(5): 499. CrossRef - Transcriptomic Heterogeneity of EGFR-Mutant Non–Small Cell Lung Cancer Evolution Toward Small-Cell Lung Cancer
Songji Oh, Jaemoon Koh, Tae Min Kim, Soyeon Kim, Jeonghwan Youk, Miso Kim, Bhumsuk Keam, Yoon Kyung Jeon, Ja-Lok Ku, Dong-Wan Kim, Doo Hyun Chung, Dae Seog Heo
Clinical Cancer Research.2024; 30(20): 4729. CrossRef - Transformation of lung adenocarcinoma into small cell lung cancer after treatment with epidermal growth factor receptor tyrosine kinase inhibitors
Linwu Kuang, Yangkai Li
Oncology and Translational Medicine.2024; 10(6): 286. CrossRef - Exon-18-EGFR Mutated Transformed Small-Cell Lung Cancer: A Case Report and Literature Review
Nunzio Digiacomo, Tommaso De Pas, Giovanna Rossi, Paola Bossi, Erika Stucchi, Fabio Conforti, Emilia Cocorocchio, Daniele Laszlo, Laura Pala, Emma Zattarin, Chiara Catania
Current Oncology.2023; 30(3): 3494. CrossRef - Current knowledge of small cell lung cancer transformation from non-small cell lung cancer
Giuseppe Giaccone, Yongfeng He
Seminars in Cancer Biology.2023; 94: 1. CrossRef - Targeting the EGFR signaling pathway in cancer therapy: What’s new in 2023?
Sushanta Halder, Soumi Basu, Shobhit P. Lall, Apar K. Ganti, Surinder K. Batra, Parthasarathy Seshacharyulu
Expert Opinion on Therapeutic Targets.2023; 27(4-5): 305. CrossRef - Outcomes in Patients With Lung Adenocarcinoma With Transformation to Small Cell Lung Cancer After EGFR Tyrosine Kinase Inhibitors Resistance: A Systematic Review and Pooled Analysis
Jinhe Xu, Lihuan Xu, Baoshan Wang, Wencui Kong, Ying Chen, Zongyang Yu
Frontiers in Oncology.2022;[Epub] CrossRef - Small cell lung cancer transformation: From pathogenesis to treatment
Xiaomeng Yin, Yueyi Li, Hang Wang, Tingting Jia, Enli Wang, Yuling Luo, Yuhao Wei, Zeyi Qin, Xuelei Ma
Seminars in Cancer Biology.2022; 86: 595. CrossRef - Small Cell Lung Cancer Transformation following Treatment in EGFR-Mutated Non-Small Cell Lung Cancer
Isa Mambetsariev, Leonidas Arvanitis, Jeremy Fricke, Rebecca Pharaon, Angel R. Baroz, Michelle Afkhami, Marianna Koczywas, Erminia Massarelli, Ravi Salgia
Journal of Clinical Medicine.2022; 11(5): 1429. CrossRef - Morphologic-Molecular Transformation of Oncogene Addicted Non-Small Cell Lung Cancer
Fiorella Calabrese, Federica Pezzuto, Francesca Lunardi, Francesco Fortarezza, Sofia-Eleni Tzorakoleftheraki, Maria Vittoria Resi, Mariaenrica Tiné, Giulia Pasello, Paul Hofman
International Journal of Molecular Sciences.2022; 23(8): 4164. CrossRef - Genomic and Gene Expression Studies Helped to Define the Heterogeneity of Small-Cell Lung Cancer and Other Lung Neuroendocrine Tumors and to Identify New Therapeutic Targets
Ugo Testa, Elvira Pelosi, Germana Castelli
Onco.2022; 2(3): 186. CrossRef - Neuroendocrine transformation from EGFR/ALK-wild type or TKI-naïve non-small cell lung cancer: An under-recognized phenomenon
Xiao Chu, Yuyin Xu, Ye Li, Yue Zhou, Li Chu, Xi Yang, Jianjiao Ni, Yida Li, Tiantian Guo, Zhiqin Zheng, Qiang Zheng, Qianlan Yao, Yuan Li, Xiaoyan Zhou, Zhengfei Zhu
Lung Cancer.2022; 169: 22. CrossRef - Three Third-Generation Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors in Non-Small Cell Lung Cancer: Similarities and Differences
Ling Chen, Yangqingqing Zhou, Chaosheng Gan, XiaoLi Wang, Yihui Liu, Chunhui Dong, Ruiyuan He, Jin Yang
Cancer Investigation.2022; 40(7): 590. CrossRef - Histomorphological transformation from non-small cell lung carcinoma to small cell lung carcinoma after targeted therapy or immunotherapy: A report of two cases
Hao Liu, Li-Hong Chen, Zhi-Hui Zhang, Ning Wang, Si-Hui Zhuang, Hao Chen, Jin Du, Li-Juan Pang, Yan Qi
Frontiers in Oncology.2022;[Epub] CrossRef - Impressive response to dabrafenib, trametinib, and osimertinib in a metastatic EGFR-mutant/BRAF V600E lung adenocarcinoma patient
Maurício Fernando Silva Almeida Ribeiro, Franciele Hinterholz Knebel, Fabiana Bettoni, Rodrigo Saddi, Karina Perez Sacardo, Felipe Sales Nogueira Amorim Canedo, João Victor Machado Alessi, Andrea Kazumi Shimada, José Flávio Gomes Marin, Anamaria Aranha Ca
npj Precision Oncology.2021;[Epub] CrossRef - Histological transformation of non-small cell lung cancer: Clinical analysis of nine cases
Cai-Bao Jin, Ling Yang
World Journal of Clinical Cases.2021; 9(18): 4617. CrossRef - Lamellarin 14, a derivative of marine alkaloids, inhibits the T790M/C797S mutant epidermal growth factor receptor
Naoyuki Nishiya, Yusuke Oku, Chie Ishikawa, Tsutomu Fukuda, Shingo Dan, Tetsuo Mashima, Masaru Ushijima, Yoko Furukawa, Yuka Sasaki, Keishi Otsu, Tomoko Sakyo, Masanori Abe, Honami Yonezawa, Fumito Ishibashi, Masaaki Matsuura, Akihiro Tomida, Hiroyuki Sei
Cancer Science.2021; 112(5): 1963. CrossRef - Case Report: Transformation From Non-Small Cell Lung Cancer to Small Cell Lung Cancer During Anti-PD-1 Therapy: A Report of Two Cases
Qian Shen, Jingjing Qu, Lingyan Sheng, Qiqi Gao, Jianying Zhou
Frontiers in Oncology.2021;[Epub] CrossRef - Exploring the resistance mechanisms of second-line osimertinib and their prognostic implications using next-generation sequencing in patients with non-small-cell lung cancer
Kyoungmin Lee, Deokhoon Kim, Shinkyo Yoon, Dae Ho Lee, Sang-We Kim
European Journal of Cancer.2021; 148: 202. CrossRef - Comprehensive analysis of treatment modes and clinical outcomes of small cell lung cancer transformed from epidermal growth factor receptor mutant lung adenocarcinoma
Shouzheng Wang, Tongji Xie, Xuezhi Hao, Yan Wang, Xingsheng Hu, Lin Wang, Yan Li, Junling Li, Puyuan Xing
Thoracic Cancer.2021; 12(19): 2585. CrossRef - EGFR-Mutant SCLC Exhibits Heterogeneous Phenotypes and Resistance to Common Antineoplastic Drugs
Chih-An Lin, Sung-Liang Yu, Hsuan-Yu Chen, Huei-Wen Chen, Shr-Uen Lin, Chia-Ching Chang, Chong-Jen Yu, Pan-Chyr Yang, Chao-Chi Ho
Journal of Thoracic Oncology.2019; 14(3): 513. CrossRef - The clinicopathologic of pulmonary adenocarcinoma transformation to small cell lung cancer
Haiyan Yang, Li Liu, Chunhua Zhou, Yi Xiong, Yijuan Hu, Nong Yang, Jingjing Qu
Medicine.2019; 98(12): e14893. CrossRef - Chemistry and pharmacological diversity of quinoxaline motifs as anticancer agents
Olayinka O. Ajani, Martins T. Nlebemuo, Joseph A. Adekoya, Kehinde O. Ogunniran, Tolutope O. Siyanbola, Christiana O. Ajanaku
Acta Pharmaceutica.2019; 69(2): 177. CrossRef - Resistance to EGFR inhibitors in non-small cell lung cancer: Clinical management and future perspectives
Chiara Tomasello, Cinzia Baldessari, Martina Napolitano, Giulia Orsi, Giulia Grizzi, Federica Bertolini, Fausto Barbieri, Stefano Cascinu
Critical Reviews in Oncology/Hematology.2018; 123: 149. CrossRef - Small cell lung cancer transformation from EGFR-mutated lung adenocarcinoma: A case report and literatures review
Yangyang Liu
Cancer Biology & Therapy.2018; 19(6): 445. CrossRef - Anaplastic lymphoma kinase (ALK)-expressing Lung Adenocarcinoma with Combined Neuroendocrine Component or Neuroendocrine Transformation: Implications for Neuroendocrine Transformation and Response to ALK-tyrosine Kinase Inhibitors
Jongmin Sim, Hyunjin Kim, Jiyeon Hyeon, Yoon-La Choi, Joungho Han
Journal of Korean Medical Science.2018;[Epub] CrossRef - Assessment of Resistance Mechanisms and Clinical Implications in Patients WithEGFRT790M–Positive Lung Cancer and Acquired Resistance to Osimertinib
Geoffrey R. Oxnard, Yuebi Hu, Kathryn F. Mileham, Hatim Husain, Daniel B. Costa, Philip Tracy, Nora Feeney, Lynette M. Sholl, Suzanne E. Dahlberg, Amanda J. Redig, David J. Kwiatkowski, Michael S. Rabin, Cloud P. Paweletz, Kenneth S. Thress, Pasi A. Jänne
JAMA Oncology.2018; 4(11): 1527. CrossRef - Clinicopathological and genomic comparisons between different histologic components in combined small cell lung cancer and non-small cell lung cancer
Mong-Wei Lin, Kang-Yi Su, Te-Jen Su, Chia-Ching Chang, Jing-Wei Lin, Yi-Hsuan Lee, Sung-Liang Yu, Jin-Shing Chen, Min-Shu Hsieh
Lung Cancer.2018; 125: 282. CrossRef - Transformation to small‑cell lung cancer following treatment with icotinib in a patient with lung adenocarcinoma
Hongyang Lu, Bo Chen, Jing Qin, Fajun Xie, Na Han, Zhiyu Huang
Oncology Letters.2018;[Epub] CrossRef - Histological transformation of adenocarcinoma to small cell carcinoma lung as a rare mechanism of resistance to epidermal growth factor receptor-tyrosine kinase inhibitors: Report of a case with review of literature
Monalisa Hui, ShantveerG Uppin, BalaJoseph Stalin, G Sadashivudu
Lung India.2018; 35(2): 160. CrossRef - A rare case of squamous cell carcinoma lung with multiple locoregional recurrences and histological transformation
Ram Niwas, Shibdas Chakrabarti, Viswesvaran Balasubramanian, ManasKamal Sen, JagdishChander Suri
Lung India.2018; 35(6): 511. CrossRef - Small cell lung cancer transformation during immunotherapy with nivolumab: A case report
Takuma Imakita, Kohei Fujita, Osamu Kanai, Tsuyoshi Terashima, Tadashi Mio
Respiratory Medicine Case Reports.2017; 21: 52. CrossRef - Pulmonary neuroendocrine tumor in a female wolf (Canis lupus lupus)
Ayako SHIRAKI, Toshinori YOSHIDA, Masahi KAWASHIMA, Hirotada MURAYAMA, Rei NAGAHARA, Nanao ITO, Makoto SHIBUTANI
Journal of Veterinary Medical Science.2017; 79(3): 588. CrossRef - Secondary biopsy of non‐oncogenic‐driven lung cancer may reveal a clinically sensible histologic change. A brief report of two paradigmatic cases
Maria C. Mengoli, Giulia Orsi, Filippo Lococo, Giulia Grizzi, Fausto Barbieri, Federica Bertolini, Giulio Rossi, Silvia Novello
Thoracic Cancer.2017; 8(4): 359. CrossRef - Small-cell lung cancer in never smokers: The clinicopathological features including the prognosis
Masahiro Yamasaki, Naomi Saito, Wakako Daido, Sayaka Ishiyama, Naoko Deguchi, Masaya Taniwaki, Akio Sakatani, Megumu Fujihara, Nobuyuki Ohashi, Ken-ichi Arita
Cancer Treatment and Research Communications.2017; 12: 1. CrossRef - Clonal History and Genetic Predictors of Transformation Into Small-Cell Carcinomas From Lung Adenocarcinomas
June-Koo Lee, Junehawk Lee, Sehui Kim, Soyeon Kim, Jeonghwan Youk, Seongyeol Park, Yohan An, Bhumsuk Keam, Dong-Wan Kim, Dae Seog Heo, Young Tae Kim, Jin-Soo Kim, Se Hyun Kim, Jong Seok Lee, Se-Hoon Lee, Keunchil Park, Ja-Lok Ku, Yoon Kyung Jeon, Doo Hyun
Journal of Clinical Oncology.2017; 35(26): 3065. CrossRef - Australian recommendations for EGFR T790M testing in advanced non-small cell lung cancer
Thomas John, Jeffrey J Bowden, Stephen Clarke, Stephen B Fox, Kerryn Garrett, Keith Horwood, Christos S Karapetis
Asia-Pacific Journal of Clinical Oncology.2017; 13(4): 296. CrossRef - Metastatic Squamous Cell Carcinoma from Lung Adenocarcinoma after Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor Therapy
Hyung Kyu Park, Youjeong Seo, Yoon-La Choi, Myung-Ju Ahn, Joungho Han
Journal of Pathology and Translational Medicine.2017; 51(4): 441. CrossRef - Sequential occurrence of small cell and non-small lung cancer in a male patient: Is it a transformation?
Ahsan Wahab, Kavitha Kesari, Siddique Chaudhary, Mahin Khan, Hafiz Khan, Susan Smith, Yanis Boumber
Cancer Biology & Therapy.2017; 18(12): 940. CrossRef - The expression of S100B protein in serum of patients with brain metastases from small-cell lung cancer and its clinical significance
Shanling Mu, Hong Ma, Jun Shi, Dezhi Zhen
Oncology Letters.2017;[Epub] CrossRef
- Patients outcomes in lung adenocarcinoma transforming to small-cell lung cancer after tyrosine kinase inhibitor therapy
- Prognostic Significance of Aquaporin 5 Expression in Non-small Cell Lung Cancer
- Young Min Jo, Tae In Park, Hwa Young Lee, Ji Yun Jeong, Won Kee Lee
- J Pathol Transl Med. 2016;50(2):122-128. Published online February 8, 2016
- DOI: https://doi.org/10.4132/jptm.2015.10.31
- 13,478 View
- 85 Download
- 15 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Aquaporins are water channel proteins that play a major role in the movement of water in various human tissues. Recently, it has been found that aquaporins have influence in the carcinogenesis of human malignancies. We analyzed the prognostic impact of aquaporin 5 (AQP5) in non-small lung cancer (NSCLC). Methods: Seventy-six cases of NSCLC were studied, including 44 cases of adenocarcinoma (ADC) and 32 cases of squamous cell carcinoma (SQCC). Tissue microarray was constructed and immunohistochemical staining for AQP5 was performed. Results: AQP5 was positive in 59.2% of the total enrolled NSCLCs (63.7% in ADC and 53.1% in SQCC). The difference in expression of AQP5 according to the histologic grade of the tumor was significant (p<.047), but not in a serial order. When ADC and SQCC were separately evaluated, no significant difference was observed according to the histologic grade of the tumor (p=.076 in ADC and p=.631 in SQCC). No difference was observed between AQP5 expression and other demographic data and tumor characteristics. Disease-free survival (DFS) was higher in AQP5 negative cases than positive cases in ADC (p=.047), but no significance was found in SQCC (p=.068). We were unable to find a significance between AQP5 overexpression and overall survival in either ADC (p=.210) or SQCC (p=.533). Conclusions: AQP5 expression is associated with DFS in ADC of the lung and tumor grade of NSCLC. The present study suggests that AQP5 can be a prognostic factor of NSCLC. -
Citations
Citations to this article as recorded by- AQP5 promotes epithelial-mesenchymal transition and tumor growth through activating the Wnt/β-catenin pathway in triple-negative breast cancer
Zhengcai Zhu, Tao Li, Honggang Wang, Lianghe Jiao
Mutation Research - Fundamental and Molecular Mechanisms of Mutagenesis.2024; 829: 111868. CrossRef - Aquaporin-mediated dysregulation of cell migration in disease states
Ian M. Smith, Shohini Banerjee, Allison K. Moses, Kimberly M. Stroka
Cellular and Molecular Life Sciences.2023;[Epub] CrossRef - The Role of Aquaporin 5 (AQP5) in Lung Adenocarcinoma: A Review Article
Lukasz Jaskiewicz, Anna Romaszko-Wojtowicz, Anna Doboszynska, Agnieszka Skowronska
Cells.2023; 12(3): 468. CrossRef - Aquaporins 1, 3 and 5 in Different Tumors, their Expression, Prognosis Value and Role as New Therapeutic Targets
Mahdieh-Sadat Moosavi, Yalda Elham
Pathology & Oncology Research.2020; 26(2): 615. CrossRef - Aquaporins in lung health and disease: Emerging roles, regulation, and clinical implications
Ekta Yadav, Niket Yadav, Ariel Hus, Jagjit S. Yadav
Respiratory Medicine.2020; 174: 106193. CrossRef - Combined Systematic Review and Transcriptomic Analyses of Mammalian Aquaporin Classes 1 to 10 as Biomarkers and Prognostic Indicators in Diverse Cancers
Pak Hin Chow, Joanne Bowen, Andrea J Yool
Cancers.2020; 12(7): 1911. CrossRef - Prognostic Role of S100A8 and S100A9 Protein Expressions in Non-small Cell Carcinoma of the Lung
Hyun Min Koh, Hyo Jung An, Gyung Hyuck Ko, Jeong Hee Lee, Jong Sil Lee, Dong Chul Kim, Jung Wook Yang, Min Hye Kim, Sung Hwan Kim, Kyung Nyeo Jeon, Gyeong-Won Lee, Se Min Jang, Dae Hyun Song
Journal of Pathology and Translational Medicine.2019; 53(1): 13. CrossRef - Effect of FGF/FGFR pathway blocking on lung adenocarcinoma and its cancer‐associated fibroblasts
Ahmed E Hegab, Mari Ozaki, Naofumi Kameyama, Jingtao Gao, Shizuko Kagawa, Hiroyuki Yasuda, Kenzo Soejima, Yongjun Yin, Robert D Guzy, Yoshikazu Nakamura, David M Ornitz, Tomoko Betsuyaku
The Journal of Pathology.2019; 249(2): 193. CrossRef - Anti-cancer effect of Aquaporin 5 silencing in colorectal cancer cells in association with inhibition of Wnt/β-catenin pathway
Wei Wang, Qing Li, Tao Yang, Dongsheng Li, Feng Ding, Hongzhi Sun, Guang Bai
Cytotechnology.2018; 70(2): 615. CrossRef - Knockdown of aquaporin-5 sensitizes colorectal cancer cells to 5-fluorouracil via inhibition of the Wnt–β-catenin signaling pathway
Qing Li, Tao Yang, Dongsheng Li, Feng Ding, Guang Bai, Wei Wang, Hongzhi Sun
Biochemistry and Cell Biology.2018; 96(5): 572. CrossRef - Implications of KRAS mutations in acquired resistance to treatment in NSCLC
Marzia Del Re, Eleonora Rofi, Giuliana Restante, Stefania Crucitta, Elena Arrigoni, Stefano Fogli, Massimo Di Maio, Iacopo Petrini, Romano Danesi
Oncotarget.2018; 9(5): 6630. CrossRef
- AQP5 promotes epithelial-mesenchymal transition and tumor growth through activating the Wnt/β-catenin pathway in triple-negative breast cancer
- Comprehensive Cytomorphologic Analysis of Pulmonary Adenoid Cystic Carcinoma: Comparison to Small Cell Carcinoma and Non-pulmonary Adenoid Cystic Carcinoma
- Seokhwi Kim, Jinah Chu, Hojoong Kim, Joungho Han
- J Pathol Transl Med. 2015;49(6):511-519. Published online October 19, 2015
- DOI: https://doi.org/10.4132/jptm.2015.09.07
- 11,233 View
- 74 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Cytologic diagnosis of pulmonary adenoid cystic carcinoma (AdCC) is frequently challenging and differential diagnosis with small cell carcinoma is often difficult. Methods: Eleven cytologically diagnosed cases of pulmonary AdCC were collected and reviewed according to fifteen cytomorphologic characteristics: small cell size, cellular uniformity, coarse chromatin, hyperchromasia, distinct nucleolus, frequent nuclear molding, granular cytoplasm, organoid cluster, sheet formation, irregular border of cluster, hyaline globule, hyaline basement membrane material, individual cell necrosis or apoptotic body, and necrotic background. Twenty cases of small cell carcinoma and fifteen cases of non-pulmonary AdCC were also reviewed for the comparison. Results: Statistically significant differences were identified between pulmonary AdCC and small cell carcinoma in fourteen of the fifteen cytomorphologic criteria (differences in sheet formation were not statistically significant). Cellular uniformity, distinct nucleolus, granular cytoplasm, distinct cell border, organoid cluster, hyaline globule, and hyaline basement membrane material were characteristic features of AdCC. Frequent nuclear molding, individual cell necrosis, and necrotic background were almost exclusively identified in small cell carcinoma. Although coarse chromatin and irregular cluster border were observed in both, they favored the diagnosis of small cell carcinoma. Hyaline globules were more frequently seen in non-pulmonary AdCC cases. Conclusions: Using the fifteen cytomorphologic criteria described by this study, pulmonary AdCC could be successfully distinguished from small cell carcinoma. Such a comprehensive approach to an individual case is recommended for the cytologic diagnosis of pulmonary AdCC. -
Citations
Citations to this article as recorded by- Primary pulmonary adenoid cystic carcinoma: A study of clinicopathological features and molecular alterations in twenty-one cases
Zhiyuan Yao, Tong Qiu, Changlei Li, Weimao Kong, Guangqi Li, Peng Song, Guohua Wang, Wenjie Jiao
Lung Cancer.2025; 201: 108414. CrossRef - Recent developments in the pathology of primary pulmonary salivary gland‐type tumours
Julia R Naso, Anja C Roden
Histopathology.2024; 84(1): 102. CrossRef - Bronchial cytology of pulmonary adenoid cystic carcinoma – A multi-institute series with emphasis on immunocytochemistry
Joanna K.M. Ng, Ka Pang Chan, Gary M. Tse, Joshua J.X. Li
Annals of Diagnostic Pathology.2023; 64: 152132. CrossRef - Pulmonary adenoid cystic carcinoma: molecular characteristics and literature review
Zhixin Chen, Jiapeng Jiang, Ying Fan, Hongyang Lu
Diagnostic Pathology.2023;[Epub] CrossRef - Recent updates in salivary gland tumors of the lung
Anja C. Roden
Seminars in Diagnostic Pathology.2021; 38(5): 98. CrossRef - Cytology of Primary Salivary Gland-Type Tumors of the Lower Respiratory Tract: Report of 15 Cases and Review of the Literature
Chiara Saglietti, Marco Volante, Stefano La Rosa, Igor Letovanec, Marc Pusztaszeri, Gaia Gatti, Massimo Bongiovanni
Frontiers in Medicine.2017;[Epub] CrossRef
- Primary pulmonary adenoid cystic carcinoma: A study of clinicopathological features and molecular alterations in twenty-one cases
- A Ciliated Cyst with Müllerian Differentiation Arising in the Posterior Mediastinum
- So Jung Lee, Chung Su Hwang, Do Youn Park, Gi Young Huh, Chang Hun Lee
- Korean J Pathol. 2014;48(5):401-404. Published online October 27, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.5.401
- 9,556 View
- 80 Download
- 10 Crossref
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Cyst of Hattori: literature review and case presentation
R. B. Berdnikov, K. A. Andryuschenko, N. S. Zavarov, E. M. Petrunina, A. V. Bazhenov, A. S. Romakhin
PULMONOLOGIYA.2025; 35(4): 553. CrossRef - Cyst of Hattori: A Rare Cyst in the Posterior Mediastinum
Matthew D. Turner, Elicia Goodale, Barry C. Gibney, Maria Cecilia D. Reyes
International Journal of Surgical Pathology.2023; 31(4): 431. CrossRef - A large retroperitoneal Mullerian cyst: case report and review of the literature
Elena Parmentier, Jody Valk, Paul Willemsen, Caroline Mattelaer
Acta Chirurgica Belgica.2021; 121(4): 278. CrossRef - A case of resected Mullerian cyst in posterior mediastinum
Yoshiyuki Susaki, Noriyoshi Sawabata
The Journal of the Japanese Association for Chest Surgery.2020; 34(2): 137. CrossRef - Serosal Inclusion Cysts and Arteriovenous Fistulas in Paraprostatic Area of a Dog
Daisuke KOJIMA, Kyoko KOJIMA, Kazumi OTA, Yoshihiko KOJIMA
Journal of the Japan Veterinary Medical Association.2020; 73(9): 511. CrossRef - A surgical case of Mullerian cyst in the posterior mediastinum
Yusuke Kita, Yoshimasa Tokunaga, Taku Okamoto
The Journal of the Japanese Association for Chest Surgery.2019; 33(1): 68. CrossRef - CT and MRI characteristics for differentiating mediastinal Müllerian cysts from bronchogenic cysts
M. Kawaguchi, H. Kato, A. Hara, N. Suzui, H. Tomita, T. Miyazaki, H. Iwata, M. Matsuo
Clinical Radiology.2019; 74(12): 976.e19. CrossRef - A case of Mullerian cyst arising in the posterior mediastinum
Masahiro Adachi, Isao Sano, Shintaro Hashimoto, Ryoichiro Doi, Hideki Taniguchi, Kazuto Shigematsu
The Journal of the Japanese Association for Chest Surgery.2018; 32(6): 713. CrossRef - Two resected cases of Mullerian cyst in the posterior mediastinum
Shotaro Hashimoto, Masato Hisano, Masato Morimoto
The Journal of the Japanese Association for Chest Surgery.2018; 32(7): 818. CrossRef - Posterior mediastinal Müllerian cyst: a rare cause of pain in a young woman
Rebecca Weedle, Keith Conway, Igor Saftic, Alan Soo
Asian Cardiovascular and Thoracic Annals.2017; 25(6): 466. CrossRef
- Cyst of Hattori: literature review and case presentation
- Morphologic Analysis of Pulmonary Neuroendocrine Tumors
- Seung Seok Lee, Myunghee Kang, Seung Yeon Ha, Jungsuk An, Mee Sook Roh, Chang Won Ha, Jungho Han
- Korean J Pathol. 2013;47(1):16-20. Published online February 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.1.16
- 7,813 View
- 52 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Few studies on how to diagnose pulmonary neuroendocrine tumors through morphometric analysis have been reported. In this study, we measured and analyzed the characteristic parameters of pulmonary neuroendocrine tumors using an image analyzer to aid in diagnosis.
Methods Sixteen cases of typical carcinoid tumor, 5 cases of atypical carcinoid tumor, 15 cases of small cell carcinoma, and 51 cases of large cell neuroendocrine carcinoma were analyzed. Using an image analyzer, we measured the nuclear area, perimeter, and the major and minor axes.
Results The mean nuclear area was 0.318±0.101 µm2 in typical carcinoid tumors, 0.326±0.119 µm2 in atypical carcinoid tumors, 0.314±0.107 µm2 in small cell carcinomas, and 0.446±0.145 µm2 in large cell neuroendocrine carcinomas. The mean nuclear circumference was 2.268±0.600 µm in typical carcinoid tumors, 2.408±0.680 µm in atypical carcinoid tumors, 2.158±0.438 µm in small cell carcinomas, and 3.247±1.276 µm in large cell neuroendocrine carcinomas. All parameters were useful in distinguishing large cell neuroendocrine carcinoma from other tumors (p=0.001) and in particular, nuclear circumference was the most effective (p=0.001).
Conclusions Pulmonary neuroendocrine tumors showed nuclear morphology differences by subtype. Therefore, evaluation of quantitative nuclear parameters improves the accuracy and reliability of diagnosis.
-
Citations
Citations to this article as recorded by- Clinical Significance of Persistent Tumor in Bone Marrow during Treatment of High-risk Neuroblastoma
Young Bae Choi, Go Eun Bae, Na Hee Lee, Jung-Sun Kim, Soo Hyun Lee, Keon Hee Yoo, Ki Woong Sung, Hong Hoe Koo
Journal of Korean Medical Science.2015; 30(8): 1062. CrossRef - Morphologic Alteration of Metastatic Neuroblastic Tumor in Bone Marrow after Chemotherapy
Go Eun Bae, Yeon-Lim Suh, Ki Woong Sung, Jung-Sun Kim
Korean Journal of Pathology.2013; 47(5): 433. CrossRef
- Clinical Significance of Persistent Tumor in Bone Marrow during Treatment of High-risk Neuroblastoma
- Clinicopathologic Implication of Ezrin Expression in Non-small Cell Lung Cancer
- Ho Won Lee, Eui Han Kim, Mee-Hye Oh
- Korean J Pathol. 2012;46(5):470-477. Published online October 25, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.5.470
- 10,280 View
- 31 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Ezrin, a member of the ezrin-radixin-moesin family, is implicated in tumor progression, metastatic dissemination, and adverse outcomes, in several cancer types. In this study, we explored the clinicopathological significance of ezrin expression in non-small cell lung carcinomas (NSCLCs).
Methods Immunohistochemical analysis of tissue microarray with 112 surgically resected NSCLC specimens, was performed to examine the ezrin expression. We also correlated ezrin expression with other clinicopathological features and prognosis.
Results The ezrin-positive group revealed significantly higher correlation with pleural invasion (p=0.016) and pathologic stage (p=0.050). Univariate survival analysis showed that ezrin-positive group had a significantly shorter cancer-specific survival than ezrin-negative group (p=0.016). Meanwhile, female (p=0.030), no pleural invasion (p=0.023), no lymphatic invasion (p=0.026), and early pathologic stage (p=0.008) significantly correlated with longer survival. Multivariate survival analysis showed that variables such as ezrin positivity (p=0.032), female (p=0.035), and early pathologic stage (p=0.001) were independent prognostic factors for NSCLC.
Conclusions Ezrin might be a molecular marker to predict poor prognosis of NSCLC.
-
Citations
Citations to this article as recorded by- Immunoexpression of E-cadherin, β-catenin and Ezrin in non-small cell lung carcinomas
Daniela Florentina Grecu, Bianca Cătălina Andreiana , Claudiu Mărgăritescu , Alexandru Florian Grecu , Marian Valentin Zorilă , Daniela Marinescu , Alex Emilian Stepan
Romanian Journal of Morphology and Embryology.2025; 65(4): 661. CrossRef - Perspectives for Targeting Ezrin in Cancer Development and Progression
Jean Carlos Lipreri da Silva, Hugo Passos Vicari, João Agostinho Machado-Neto
Future Pharmacology.2023; 3(1): 61. CrossRef - CIGB-300 Anticancer Peptide Differentially Interacts with CK2 Subunits and Regulates Specific Signaling Mediators in a Highly Sensitive Large Cell Lung Carcinoma Cell Model
George V. Pérez, Mauro Rosales, Ailyn C. Ramón, Arielis Rodríguez-Ulloa, Vladimir Besada, Luis J. González, Daylen Aguilar, Dania Vázquez-Blomquist, Viviana Falcón, Evelin Caballero, Paulo C. Carvalho, Rodrigo Soares Caldeira, Ke Yang, Yasser Perera, Silv
Biomedicines.2022; 11(1): 43. CrossRef - Increased Tumor Growth Rate and Mesenchymal Properties of NSCLC-Patient-Derived Xenograft Models during Serial Transplantation
José Miguel Pardo-Sánchez, Nuria Mancheño, José Cerón, Carlos Jordá, Emilio Ansotegui, Óscar Juan, Sarai Palanca, Antonio Cremades, Carolina Gandía, Rosa Farràs
Cancers.2021; 13(12): 2980. CrossRef - Loss of ARID1A expression is associated with poor prognosis in non-small cell lung cancer
Si-Hyong Jang, Ji-Hye Lee, Hyun Ju Lee, Hyundeuk Cho, Hyein Ahn, In Hag Song, Mee-Hye Oh
Pathology - Research and Practice.2020; 216(11): 153156. CrossRef - Ezrin Mediates Invasion and Metastasis in Tumorigenesis: A Review
Yanan Song, Xiaokun Ma, Miao Zhang, Menghan Wang, Guoyu Wang, Ying Ye, Wei Xia
Frontiers in Cell and Developmental Biology.2020;[Epub] CrossRef - Correlation of Ezrin Expression Pattern and Clinical Outcomes in Ewing Sarcoma
Thomas Cash, Hong Yin, Courtney McCracken, Zhi Geng, Steven G. DuBois, Bahig M. Shehata, Thomas A. Olson, Howard M. Katzenstein, Cynthia Wetmore
Sarcoma.2017; 2017: 1. CrossRef - Prognostic and Clinicopathological Significance of Transducer-Like Enhancer of Split 1 Expression in Gastric Cancer
Ji-Hye Lee, Myoung-Won Son, Kyung-Ju Kim, Mee-Hye Oh, Hyundeuk Cho, Hyun Ju Lee, Si-Hyong Jang, Moon Soo Lee
Journal of Gastric Cancer.2016; 16(1): 21. CrossRef - Significance of DEK overexpression for the prognostic evaluation of non-small cell lung carcinoma
XIN LIU, DONGDONG QI, JUJIE QI, ZESHU MAO, XIANGDAN LI, JINHUI ZHANG, JINZI LI, WENBIN GAO
Oncology Reports.2016; 35(1): 155. CrossRef - Silencing of high‐mobility group box 2 (HMGB2) modulates cisplatin and 5‐fluorouracil sensitivity in head and neck squamous cell carcinoma
Nazia Syed, Sandip Chavan, Nandini A. Sahasrabuddhe, Santosh Renuse, Gajanan Sathe, Vishalakshi Nanjappa, Aneesha Radhakrishnan, Remya Raja, Sneha M. Pinto, Anand Srinivasan, T. S. Keshava Prasad, Kotteazeth Srikumar, Harsha Gowda, Vani Santosh, David Sid
PROTEOMICS.2015; 15(2-3): 383. CrossRef - Prognostic Value of Ezrin in Various Cancers: A Systematic Review and Updated Meta-analysis
Jianwei Li, Kuanhai Wei, Hailang Yu, Dan Jin, Gang Wang, Bin Yu
Scientific Reports.2015;[Epub] CrossRef - Radixin Enhances Colon Cancer Cell Invasion by Increasing MMP-7 Production via Rac1-ERK Pathway
Qi-Hong Jiang, Ai-Xiang Wang, Yan Chen
The Scientific World Journal.2014; 2014: 1. CrossRef - Clinical significance of microRNA-183/Ezrin axis in judging the prognosis of patients with osteosarcoma
Yisila Mu, Haoshaqiang Zhang, Lixin Che, Kun Li
Medical Oncology.2014;[Epub] CrossRef - Prognostic implications of ezrin and phosphorylated ezrin expression in non-small cell lung cancer
Tiefeng Jin, Jingchun Jin, Xiangyu Li, Songnan Zhang, Yun Ho Choi, Yingshi Piao, Xionghu Shen, Zhenhua Lin
BMC Cancer.2014;[Epub] CrossRef - Prognostic Value of Ezrin in Solid Tumors: A Meta-Analysis of the Literature
Kun Han, WeiXiang Qi, ZhiHua Gan, Zan Shen, Yang Yao, DaLiu Min, Yves St-Pierre
PLoS ONE.2013; 8(7): e68527. CrossRef
- Immunoexpression of E-cadherin, β-catenin and Ezrin in non-small cell lung carcinomas
- Interobserver Variability in Diagnosing High-Grade Neuroendocrine Carcinoma of the Lung and Comparing It with the Morphometric Analysis
- Seung Yeon Ha, Joungho Han, Wan-Seop Kim, Byung Seong Suh, Mee Sook Roh
- Korean J Pathol. 2012;46(1):42-47. Published online February 23, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.1.42
- 9,567 View
- 48 Download
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Distinguishing small cell lung carcinoma (SCLC) and large cell neuroendocrine carcinoma (LCNEC) of the lung is difficult with little information about interobserver variability.
Methods One hundred twenty-nine cases of resected SCLC and LCNEC were independently evaluated by four pathologists and classified according to the 2004 World Health Organization criteria. Agreement was regarded as "unanimous" if all four pathologists agreed on the classification. The kappa statistic was calculated to measure the degree of agreement between pathologists. We also measured cell size using image analysis, and receiver-operating-characteristic curve analysis was performed to evaluate cell size in predicting the diagnosis of high-grade neuroendocrine (NE) carcinomas in 66 cases.
Results Unanimous agreement was achieved in 55.0% of 129 cases. The kappa values ranged from 0.35 to 0.81. Morphometric analysis reaffirmed that there was a continuous spectrum of cell size from SCLC to LCNEC and showed that tumors with cells falling in the middle size range were difficult to categorize and lacked unanimous agreement.
Conclusions Our results provide an objective explanation for considerable interobserver variability in the diagnosis of high-grade pulmonary NE carcinomas. Further studies would need to define more stringent and objective definitions of cytologic and architectural characteristics to reliably distinguish between SCLC and LCNEC.
-
Citations
Citations to this article as recorded by- Case report: A patient with EGFR L861Q positive adenosquamous lung carcinoma transforming into large cell neuroendocrine cancer after treatment with Almonertinib
Kele Cheng, Yong Zhu, Ran Sang, Zhongsheng Kuang, Yang Cao
Frontiers in Oncology.2025;[Epub] CrossRef - Deep Learning–Based Retinoblastoma Protein Subtyping of Pulmonary Large-Cell Neuroendocrine Carcinoma on Small Hematoxylin and Eosin–Stained Specimens
Teodora E. Trandafir, Frank W.J. Heijboer, Farhan Akram, Jules L. Derks, Yunlei Li, Lisa M. Hillen, Ernst-Jan M. Speel, Zsolt Megyesfalvi, Balazs Dome, Andrew P. Stubbs, Anne-Marie C. Dingemans, Jan H. von der Thüsen
Laboratory Investigation.2025; 105(9): 104192. CrossRef - Treatment outcomes in patients with stage IV large cell neuroendocrine carcinoma: a nationwide registry study
Frank W.J. Heijboer, Jules L. Derks, Francien H. van Nederveen, Lisa M. Hillen, Michael A. den Bakker, Teodora Radonic, Ronald A.M. Damhuis, Ernst-Jan M. Speel, Jan H. von der Thüsen, Anne-Marie C. Dingemans
Lung Cancer.2025; 210: 108830. CrossRef - Updates on lung neuroendocrine neoplasm classification
Giulia Vocino Trucco, Luisella Righi, Marco Volante, Mauro Papotti
Histopathology.2024; 84(1): 67. CrossRef - Recent advancement of HDAC inhibitors against breast cancer
Syed Abdulla Mehmood, Kantrol Kumar Sahu, Sounok Sengupta, Sangh Partap, Rajshekhar Karpoormath, Brajesh Kumar, Deepak Kumar
Medical Oncology.2023;[Epub] CrossRef - Genomic Feature of a Rare Case of Mix Small-Cell and Large-Cell Neuroendocrine Lung Carcinoma: A Case Report
Youcai Zhu, Feng Zhang, Dong Yu, Fang Wang, Manxiang Yin, Liangye Chen, Chun Xiao, Yueyan Huang, Feng Ding
Frontiers in Oncology.2022;[Epub] CrossRef - Small-Cell Carcinoma of the Lung: What We Learned about It?
Luisella Righi, Marco Volante, Mauro Papotti
Acta Cytologica.2022; 66(4): 257. CrossRef - Hierarchical identification of a transcriptional panel for the histological diagnosis of lung neuroendocrine tumors
Juxuan Zhang, Jiaxing Deng, Xiao Feng, Yilong Tan, Xin Li, Yixin Liu, Mengyue Li, Haitao Qi, Lefan Tang, Qingwei Meng, Haidan Yan, Lishuang Qi
Frontiers in Genetics.2022;[Epub] CrossRef - Immunohistochemical Staining With Neuroendocrine Markers is Essential in the Diagnosis of Neuroendocrine Neoplasms of the Esophagogastric Junction
Dea N.M. Jepsen, Anne-Marie K. Fiehn, Rajendra S. Garbyal, Ulla Engel, Jakob Holm, Birgitte Federspiel
Applied Immunohistochemistry & Molecular Morphology.2021; 29(6): 454. CrossRef - Improving differential diagnosis of pulmonary large cell neuroendocrine carcinoma and small cell lung cancer via a transcriptomic, biological pathway-based machine learning model
Junhong Guo, Likun Hou, Wei Zhang, Zhengwei Dong, Lei Zhang, Chunyan Wu
Translational Oncology.2021; 14(12): 101222. CrossRef - Are Neuroendocrine Negative Small Cell Lung Cancer and Large Cell Neuroendocrine Carcinoma with WT RB1 two Faces of the Same Entity?
Dmitriy Sonkin, Anish Thomas, Beverly A Teicher
Lung Cancer Management.2019;[Epub] CrossRef - Ki-67 labeling index of neuroendocrine tumors of the lung has a high level of correspondence between biopsy samples and surgical specimens when strict counting guidelines are applied
Alessandra Fabbri, Mara Cossa, Angelica Sonzogni, Mauro Papotti, Luisella Righi, Gaia Gatti, Patrick Maisonneuve, Barbara Valeri, Ugo Pastorino, Giuseppe Pelosi
Virchows Archiv.2017; 470(2): 153. CrossRef - The Use of Immunohistochemistry Improves the Diagnosis of Small Cell Lung Cancer and Its Differential Diagnosis. An International Reproducibility Study in a Demanding Set of Cases
Erik Thunnissen, Alain C. Borczuk, Douglas B. Flieder, Birgit Witte, Mary Beth Beasley, Jin-Haeng Chung, Sanja Dacic, Sylvie Lantuejoul, Prudence A. Russell, Michael den Bakker, Johan Botling, Elisabeth Brambilla, Erienne de Cuba, Kim R. Geisinger, Kenzo
Journal of Thoracic Oncology.2017; 12(2): 334. CrossRef - Reply to Letter “The Use of Immunohistochemistry Improves the Diagnosis of Small Cell Lung Cancer and Its Differential Diagnosis. An International Reproducibility Study in a Demanding Set of Cases.”
Erik Thunnissen, Birgit I. Witte, Masayuki Noguchi, Yasushi Yatabe
Journal of Thoracic Oncology.2017; 12(6): e70. CrossRef - What clinicians are asking pathologists when dealing with lung neuroendocrine neoplasms?
Giuseppe Pelosi, Alessandra Fabbri, Mara Cossa, Angelica Sonzogni, Barbara Valeri, Luisella Righi, Mauro Papotti
Seminars in Diagnostic Pathology.2015; 32(6): 469. CrossRef - Unraveling Tumor Grading and Genomic Landscape in Lung Neuroendocrine Tumors
Giuseppe Pelosi, Mauro Papotti, Guido Rindi, Aldo Scarpa
Endocrine Pathology.2014; 25(2): 151. CrossRef - Grading the neuroendocrine tumors of the lung: an evidence-based proposal
G Rindi, C Klersy, F Inzani, G Fellegara, L Ampollini, A Ardizzoni, N Campanini, P Carbognani, T M De Pas, D Galetta, P L Granone, L Righi, M Rusca, L Spaggiari, M Tiseo, G Viale, M Volante, M Papotti, G Pelosi
Endocrine-Related Cancer.2014; 21(1): 1. CrossRef - Controversial issues and new discoveries in lung neuroendocrine tumors
Giuseppe Pelosi, Kenzo Hiroshima, Mari Mino-Kenudson
Diagnostic Histopathology.2014; 20(10): 392. CrossRef - BAI3, CDX2 and VIL1: a panel of three antibodies to distinguish small cell from large cell neuroendocrine lung carcinomas
Muhammad F Bari, Helen Brown, Andrew G Nicholson, Keith M Kerr, John R Gosney, William A Wallace, Irshad Soomro, Salli Muller, Danielle Peat, Jonathan D Moore, Lesley A Ward, Maxim B Freidin, Eric Lim, Manu Vatish, David R J Snead
Histopathology.2014; 64(4): 547. CrossRef - Neuroendocrine tumours—challenges in the diagnosis and classification of pulmonary neuroendocrine tumours
M A den Bakker, F B J M Thunnissen
Journal of Clinical Pathology.2013; 66(10): 862. CrossRef - Morphologic Analysis of Pulmonary Neuroendocrine Tumors
Seung Seok Lee, Myunghee Kang, Seung Yeon Ha, Jungsuk An, Mee Sook Roh, Chang Won Ha, Jungho Han
Korean Journal of Pathology.2013; 47(1): 16. CrossRef - Altered expression of microRNA miR‐21, miR‐155, and let‐7a and their roles in pulmonary neuroendocrine tumors
Hyoun Wook Lee, Eun Hee Lee, Seung Yeon Ha, Chang Hun Lee, Hee Kyung Chang, Sunhee Chang, Kun Young Kwon, Il Seon Hwang, Mee Sook Roh, Jeong Wook Seo
Pathology International.2012; 62(9): 583. CrossRef
- Case report: A patient with EGFR L861Q positive adenosquamous lung carcinoma transforming into large cell neuroendocrine cancer after treatment with Almonertinib
- Composite Tumor of Adenocarcinoma and Small Cell Neuroendocrine Carcinoma of the Uterine Cervix: A Case Report.
- Hye Rim Park, Yong Woo Lee, Young Euy Park
- J Pathol Transl Med. 1990;1(1):111-120.
- 2,122 View
- 45 Download
-
 Abstract
Abstract
 PDF
PDF - Small cell neuroendocrine carcinoma of the uterine cervix is a distinct subtype of cervical cancer that appears analogous to oat cell carcinoma and carcinoid tumors of the lung. It has been assumed to be derived from the neural crest via argyrophilic cells in the normal endocervix. We have recently encountered a case of small cell neuroendocrine carcinoma of the uterine cervix coexisting with adenocarcinoma which was argyrophil negative. A 66-year-old multiparous woman was admitted because of vaginal bleeding for 2 months. Cervicovaginal smear revealed several scattered clusters and sheets of monotonous small cells with some peripheral palisading in the background of hemorrhage and necrosis. Radical hysterectomy specimen revealed and ulcerofungating tumor on endocervical canal which was composed of two components. Major component of the tumor was made up of monomorphic population of small oval-shaped tumor cells arranged in sheets and partly in acinar structeres or trabecular fashion. Other component was adenocarcinoma, endocervical well-differentiated type. Argyropilia was present on the Grimelius stain and immunohistochemical studies revealed diffuse positivity to neuron-specific enolase and carcinoembryonic antigen. Electron microscopic examination showed clusters of small round to oval cells, which had a few well-formed desmosomes and several membrane-bound, dense-core neurosectetory granules.
- The Histone Acetyltransferase hMOF is Overexpressed in Non-small Cell Lung Carcinoma.
- Joon Seon Song, Sung Min Chun, Ji Young Lee, Dong Kwan Kim, Yong Hee Kim, Se Jin Jang
- Korean J Pathol. 2011;45(4):386-396.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.4.386
- 5,943 View
- 69 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
One of the histone acetyltransferases (HATs) family of proteins, human MOF (hMOF, MYST1), is involved in histone H4 acetylation, particularly at lysine 16 (H4K16Ac), an epigenetic mark of active genes. Dysregulation of the epigenetic mark influences cellular biology and possibly leads to oncogenesis. We examined the involvement of hMOF and H4K16Ac in primary non-small cell lung cancer (NSCLC).
METHODS
Reverse transcription polymerase chain reaction using fresh-frozen lung cancer tissues and lung cancer cell lines and immunohistochemistry for hMOF and H4K16Ac via tissue microarray of 551 formalin-fixed paraffin-embedded NSCLC tissue blocks were conducted.
RESULTS
hMOF mRNA was frequently overexpressed in lung cancer tissues, compared with normal lung tissues (10/20, 50%). NSCLC tissues were positive for hMOF in 37.6% (184/489) and H4K16Ac in 24.7% (122/493) of cases. hMOF protein expression was tightly correlated with the H4K16Ac level in tumors (p<0.001). Knockdown of hMOF mRNA with siRNA led to a significant inhibition of growth in the Calu-6 cell line.
CONCLUSIONS
hMOF was frequently expressed in NSCLC and was correlated with H4K16Ac. To our knowledge, this is the first study that has focused on the expression status of HATs and hMOF in NSCLC. Our results clearly suggest a potential oncogenic role of the gene and support its utility as a potential therapeutic target. -
Citations
Citations to this article as recorded by- Stabilization of MOF (KAT8) by USP10 promotes esophageal squamous cell carcinoma proliferation and metastasis through epigenetic activation of ANXA2/Wnt signaling
Peichao Li, Lingxiao Yang, Sun Young Park, Fanrong Liu, Alex H. Li, Yilin Zhu, Huacong Sui, Fengyuan Gao, Lingbing Li, Lan Ye, Yongxin Zou, Zhongxian Tian, Yunpeng Zhao, Max Costa, Hong Sun, Xiaogang Zhao
Oncogene.2024; 43(12): 899. CrossRef - The Biological Significance of Targeting Acetylation-Mediated Gene Regulation for Designing New Mechanistic Tools and Potential Therapeutics
Chenise O’Garro, Loveth Igbineweka, Zonaira Ali, Mihaly Mezei, Shiraz Mujtaba
Biomolecules.2021; 11(3): 455. CrossRef - Histone Acetyltransferase MOF Orchestrates Outcomes at the Crossroad of Oncogenesis, DNA Damage Response, Proliferation, and Stem Cell Development
Mayank Singh, Albino Bacolla, Shilpi Chaudhary, Clayton R. Hunt, Shruti Pandita, Ravi Chauhan, Ashna Gupta, John A. Tainer, Tej K. Pandita
Molecular and Cellular Biology.2020;[Epub] CrossRef - The Functional Analysis of Histone Acetyltransferase MOF in Tumorigenesis
Jiaming Su, Fei Wang, Yong Cai, Jingji Jin
International Journal of Molecular Sciences.2016; 17(1): 99. CrossRef - Expression of hMOF, but not HDAC4, is responsible for the global histone H4K16 acetylation in gastric carcinoma
LIN ZHU, JIAXING YANG, LINHONG ZHAO, XUE YU, LINGYAO WANG, FEI WANG, YONG CAI, JINGJI JIN
International Journal of Oncology.2015; 46(6): 2535. CrossRef - Arsenic Trioxide Reduces Global Histone H4 Acetylation at Lysine 16 through Direct Binding to Histone Acetyltransferase hMOF in Human Cells
Da Liu, Donglu Wu, Linhong Zhao, Yang Yang, Jian Ding, Liguo Dong, Lianghai Hu, Fei Wang, Xiaoming Zhao, Yong Cai, Jingji Jin, Tim Thomas
PLOS ONE.2015; 10(10): e0141014. CrossRef - The histone acetyltransferase hMOF suppresses hepatocellular carcinoma growth
Jin Zhang, Hui Liu, Hao Pan, Yuan Yang, Gang Huang, Yun Yang, Wei-Ping Zhou, Ze-Ya Pan
Biochemical and Biophysical Research Communications.2014; 452(3): 575. CrossRef - Regulation and function of histone acetyltransferase MOF
Yang Yang, Xiaofei Han, Jingyun Guan, Xiangzhi Li
Frontiers of Medicine.2014; 8(1): 79. CrossRef - The histone acetylranseferase hMOF acetylates Nrf2 and regulates anti‐drug responses in human non‐small cell lung cancer
Zhiwei Chen, Xiangyun Ye, Naiwang Tang, Shengping Shen, Ziming Li, Xiaomin Niu, Shun Lu, Ling Xu
British Journal of Pharmacology.2014; 171(13): 3196. CrossRef - Correlation of low expression of hMOF with clinicopathological features of colorectal carcinoma, gastric cancer and renal cell carcinoma
LINGLING CAO, LIN ZHU, JIAXING YANG, JIAMING SU, JINSONG NI, YUJUN DU, DA LIU, YANFANG WANG, FEI WANG, JINGJI JIN, YONG CAI
International Journal of Oncology.2014; 44(4): 1207. CrossRef - Coactivator MYST1 Regulates Nuclear Factor-κB and Androgen Receptor Functions During Proliferation of Prostate Cancer Cells
Anbalagan Jaganathan, Pratima Chaurasia, Guang-Qian Xiao, Marc Philizaire, Xiang Lv, Shen Yao, Kerry L. Burnstein, De-Pei Liu, Alice C. Levine, Shiraz Mujtaba
Molecular Endocrinology.2014; 28(6): 872. CrossRef - A potential diagnostic marker for ovarian cancer: Involvement of the histone acetyltransferase, human males absent on the first
NING LIU, RUI ZHANG, XIAOMING ZHAO, JIAMING SU, XIAOLEI BIAN, JINSONG NI, YING YUE, YONG CAI, JINGJI JIN
Oncology Letters.2013; 6(2): 393. CrossRef - Epigenetic change in kidney tumor: downregulation of histone acetyltransferase MYST1 in human renal cell carcinoma
Yong Wang, Rui Zhang, Donglu Wu, Zhihua Lu, Wentao Sun, Yong Cai, Chunxi Wang, Jingji Jin
Journal of Experimental & Clinical Cancer Research.2013;[Epub] CrossRef
- Stabilization of MOF (KAT8) by USP10 promotes esophageal squamous cell carcinoma proliferation and metastasis through epigenetic activation of ANXA2/Wnt signaling
- Distinction of Pulmonary Large Cell Neuroendocrine Carcinoma from Small Cell Lung Carcinoma Using a Panel of Bcl-2, p63, and 34betaE12.
- Jun Zhe Li, Chan Choi, Yoo Duk Choi, Kook Joo Na
- Korean J Pathol. 2011;45(2):170-174.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.2.170
- 3,866 View
- 33 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Making the distinction between large cell neuroendocrine carcinoma (LCNEC) and small cell lung carcinoma (SCLC) is difficult in some samples of biopsy tissues, but we have to separate LCNEC from SCLC because the two types of cancer may need different therapy and they have different prognostic implications. Thus far, there are no specific immunohistochemical markers that allow distinguishing these two kinds of tumors.
METHODS
We performed an immunohistochemical analysis to study the expressions of p63, Bcl-2, and 34betaE12 and to investigate whether these 3 molecules have correlations in LCNEC and SCLC. We also evaluated the expression of the neuroendocrine markers chromogranin, synaptophysin and CD56.
RESULTS
A statistical analysis was performed for p63, Bcl-2, and 34betaE12 in separate and combined panels. According to the combinations of p63, Bcl-2, and 34betaE12, there were frequent expressions of p63-/Bcl-2+ or Bcl-2+/34betaE12- in the SCLC, and there was a superior proportion of them in the SCLC rather than that in the LCNEC. The p63-/Bcl-2+ and Bcl-2+/34betaE12- antibody combinations showed higher specificities compared to any single antibody for diagnosing SCLC.
CONCLUSIONS
Bcl-2 and selective p63 or 34betaE12 made up a most useful panel of markers for making the differential diagnosis of LCNEC and SCLC. -
Citations
Citations to this article as recorded by- Evaluation of Serum LDH, p53 and BCL2 in Lung Cancer Patients
Pawar Komal, Rajvik Kruti, Vora Hemangini
Gujarat Cancer Society Research Journal.2020; 22(2): 22. CrossRef
- Evaluation of Serum LDH, p53 and BCL2 in Lung Cancer Patients
- Morphometric Analysis for Pulmonary Small Cell Carcinoma Using Image Analysis.
- Sun Min Jeong, Seung Yeon Ha, Jungsuk An, Hyun Yee Cho, Dong Hae Chung, Na Rae Kim, Sanghui Park
- Korean J Pathol. 2011;45(1):87-91.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.1.87
- 4,308 View
- 28 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
There are few studies of how to diagnose small cell lung cancer in cytological tests through morphometric analysis. We tried to measure and analyze characteristics of small cell carcinoma in lung by image analysis.
METHODS
We studied three types of cytologic specimens from 89 patients who were diagnosed with small cell lung cancer by immunohistochemistry. We measured area, perimeter, maximal length and maximal width of cells from small cell carcinoma using image analysis.
RESULTS
In lung aspirates, the nuclear mean area, perimeter, maximal length and maximal width of small cell lung cancer were 218.69 microm2, 55 microm, 18.48 microm and 14.65 microm. In bronchial washings, nuclear measurements were 194.66 microm2, 50.07 microm, 16.27 microm and 14.1 microm. In pleural fluid, values were 177.85 microm2, 48.09 microm, 15.7 microm and 13.37 microm.
CONCLUSIONS
Nuclear size of small cell lung carcinoma is variable and depends on the cytology method. Nuclei are spindle-shaped and larger in small cell carcinoma from lung aspirates than in bronchial washings or pleural fluid. The cytoplasms of the cells in bronchial washings and pleural fluid were swollen. Therefore, one should consider morphologic changes when trying to diagnose small cell lung cancer through cytological tests. -
Citations
Citations to this article as recorded by- Interobserver Variability in Diagnosing High-Grade Neuroendocrine Carcinoma of the Lung and Comparing It with the Morphometric Analysis
Seung Yeon Ha, Joungho Han, Wan-Seop Kim, Byung Seong Suh, Mee Sook Roh
Korean Journal of Pathology.2012; 46(1): 42. CrossRef
- Interobserver Variability in Diagnosing High-Grade Neuroendocrine Carcinoma of the Lung and Comparing It with the Morphometric Analysis
- Clinicopathological Significance of S100A4 Expression in Non-small Cell Lung Carcinomas.
- Eun Ah Jung, Hyun Deuk Cho, Ji Hye Lee, Mee Hye Oh
- Korean J Pathol. 2010;44(5):477-482.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.5.477
- 4,504 View
- 28 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
S100A4 has been implicated in invasion and metastasis of various malignant tumors. The aim of this study was to investigate whether or not S100A4 plays an important role in non-small cell lung carcinomas (NSCLCs).
METHODS
Sixty-seven patients with NSCLC including 37 with squamous cell carcinomas (SCCs) and 30 with adenocarcinomas (ADs) who had undergone surgical resection were analyzed. S100A4 expression was analyzed by immunohistochemistry using tissue microarray blocks.
RESULTS
S100A4 expression was positive in 56 (83.6%) of 67 NSCLC cases. ADs were more frequently S100A4 positive than SCCs (p = 0.017). However, no significant correlation was observed between S100A4 expression and age, gender, pT, pN or tumor, node and metastasis (TNM) stage. Two distant metastatic cases revealed an S100A4 positive reaction. Kaplan-Meier survival curves with the log-rank test showed no correlation with 3-year survival (p = 0.782) or 5-year survival (p = 0.227) in either group of patients according to S100A4 expression.
CONCLUSIONS
S100A4 expression was not correlated with age, gender, pT, pN or TNM stage or survival in patients with NSCLCs. Therefore, S100A4 expression may not be useful as a prognostic marker for NSCLCs. However, S100A4 expression showed a higher positivity in ADs than in SCCs. -
Citations
Citations to this article as recorded by- Clinicopathological and prognostic value of S100A4 expression in non-small cell lung cancer: a meta-analysis
Jing Zhang, Yanhui Gu, Xiaoli Liu, Ximin Rao, Guichuan Huang, Yao Ouyang
Bioscience Reports.2020;[Epub] CrossRef - S100A4 promotes endometrial cancer progress through epithelial-mesenchymal transition regulation
TENG HUA, SHUANGGE LIU, XIAOYAN XIN, LIQIONG CAI, RUI SHI, SHUQI CHI, DILU FENG, HONGBO WANG
Oncology Reports.2016; 35(6): 3419. CrossRef - Prognostic value of cytoplasmic expression of S100A4 protein in endometrial carcinoma
HYE IN CHONG, JEONG HEE LEE, MAN SOO YOON, DONG SOO SUH, KYUNGBIN KIM, JEE YEON KIM, KYUNG UN CHOI
Oncology Reports.2014; 31(6): 2701. CrossRef - Clinical significance of E-cadherin, β-catenin, vimentin and S100A4 expression in completely resected squamous cell lung carcinoma
Hua Zhang, Jun Liu, Dongsheng Yue, Liuwei Gao, Daowei Wang, Hongdian Zhang, Changli Wang
Journal of Clinical Pathology.2013; 66(11): 937. CrossRef - Expression of S100A4, ephrin-A1 and osteopontin in non-small cell lung cancer
Ane Kongsgaard, Marius Lund-Iversen, Gisle Berge, Odd Terje Brustugun, Steinar K Solberg, Gunhild M Mælandsmo, Kjetil Boye
BMC Cancer.2012;[Epub] CrossRef - Clinicopathologic Implication of Ezrin Expression in Non-small Cell Lung Cancer
Ho Won Lee, Eui Han Kim, Mee-Hye Oh
Korean Journal of Pathology.2012; 46(5): 470. CrossRef
- Clinicopathological and prognostic value of S100A4 expression in non-small cell lung cancer: a meta-analysis
- Expression of MUC1 and MUC4 and Its Prognostic Significance in Non-Small Cell Lung Carcinoma.
- Ji Min Jeon, Hye Won Lee, Ji Young Park, Hye Ra Jung, Ilseon Hwang, Sun Young Kwon, Mi Sun Choe, Yu Na Kang, Sang Pyo Kim, Sang Sook Lee, Won Il Choi, Kun Young Kwon
- Korean J Pathol. 2010;44(4):397-403.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.4.397
- 5,468 View
- 60 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Mucin (MUC)1 and MUC4 (MUC1, 4) are high molecular weight glycoproteins expressed in normal and malignant epithelial cells, and these expressions are related to the prognosis of some carcinomas. In non-small cell lung carcinoma (NSCLC), the relationship between MUC1, 4 expressions and their prognostic significance is not well known. We evaluated these relationships in a series of NSCLC: 1) between MUC1, 4 expression levels and histologic subtypes, and 2) between high expression of MUC1, 4 and their prognostic significance.
METHODS
We performed immunohistochemical staining for MUC1, 4 in paraffin-embedded tissues from 165 NSCLC cases arranged in a tissue microarray.
RESULTS
We found a significant correlation between MUC1, 4 expressions and NSCLC histologic subtypes (p < 0.05). High MUC1 expression was characteristic of adenocarcinoma. Low MUC1, 4 expressions were characteristic of squamous cell carcinoma. In adenocarcinoma, we found significant association between diffuse MUC1 expression and short patient survival (p = 0.005). In squamous cell carcinoma, diffuse MUC4 expression showed long patient survival trend (p = 0.128).
CONCLUSIONS
MUC1, 4 expression levels were significantly correlated with NSCLC histologic subtypes. Diffuse MUC1 expression was significantly associated with shortened survival in NSCLC patients, especially in adenocarcinoma. -
Citations
Citations to this article as recorded by- Inhibition of MUC1-C Increases ROS and Cell Death in Mouse Embryonic Stem Cells
Jeong-A Park, Sangkyu Park, Jun-Kyu Choi, Myung-Kwan Han, Younghee Lee
International Journal of Stem Cells.2020;[Epub] CrossRef - Assessing the prognostic significance of MUC4β in mucoepidermoid carcinoma of the salivary glands: An immunohistochemical study
Poonam R. Sawant, Anita Spadigam, Anita Dhupar, Shaheen Syed, Karla Carvalho
Heliyon.2019; 5(11): e02753. CrossRef - Ultrasensitive cytosensing based on an aptamer modified nanobiosensor with a bioconjugate: Detection of human non-small-cell lung cancer cells
Tanveer A. Mir, Jang-Hee Yoon, N.G. Gurudatt, Mi-Sook Won, Yoon-Bo Shim
Biosensors and Bioelectronics.2015; 74: 594. CrossRef - Expression of MUC1 and MUC4 in Gallbladder Adenocarcinoma
Su-Mi Kim, Sun-Ju Oh, Bang Hur
Korean Journal of Pathology.2012; 46(5): 429. CrossRef - MUC4 and MUC1 Expression in Adenocarcinoma of the Stomach Correlates with Vessel Invasion and Lymph Node Metastasis: An Immunohistochemical Study of Early Gastric Cancer
Yukihiro Tamura, Michiyo Higashi, Sho Kitamoto, Seiya Yokoyama, Masahiko Osako, Michiko Horinouchi, Takeshi Shimizu, Mineo Tabata, Surinder K. Batra, Masamichi Goto, Suguru Yonezawa, Fazlul H. Sarkar
PLoS ONE.2012; 7(11): e49251. CrossRef - Prognostic significance of membrane-associated mucins 1 and 4 in gastric adenocarcinoma
ILSEON HWANG, YU NA KANG, JIN YOUNG KIM, YOUNG ROK DO, HONG SUK SONG, KEON UK PARK
Experimental and Therapeutic Medicine.2012; 4(2): 311. CrossRef
- Inhibition of MUC1-C Increases ROS and Cell Death in Mouse Embryonic Stem Cells
- Primary Extrapulmonary Small Cell Carcinoma of the Appendix: A Case Report.
- Jong Hyeok Park, Ki Jae Park, Young Hoon Roh, Mee Sook Roh
- Korean J Pathol. 2010;44(1):101-105.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.1.101
- 3,439 View
- 28 Download
-
 Abstract
Abstract
 PDF
PDF - Primary extrapulmonary small cell carcinoma (EPSCC) of the appendix is an extremely rare entity, and there has been only one previous report on this in the English medical literature. We report here on the first Korean case of EPSCC of the appendix in a 55-year-old woman. The patient had no history of an identified pulmonary tumor, and she presented with constipation and lower abdominal pain. The patient underwent right hemicolectomy with regional lymph node dissection and bilateral salphigo-oophorectomy. The histology of the entire appendiceal tumor revealed pure EPSCC with diffuse immunoreactivity for pancytokeratin, cytokeratin 7, cytokeratin 20, CD56, thyroid transcription factor 1, c-kit and carcinoembryonic antigen, and there was focal weak immunoreactivity for chromogranin A and synaptophysin. After the second cycle of chemotherapy, the condition of the patient gradually deteriorated due to cancer peritonei and the patient died 7 months later. EPSCC of the appendix is a distinctive clinicopathological entity that displays highly aggressive behavior and an unfavorable outcome.
- Expression of p63 and its Isoform, deltaNp63, in Non-Small Cell Lung Carcinoma.
- Ick Doo Kim, Dong Hoon Shin, Kyung Un Choi, Do Youn Park, Gi Yeong Huh, Mee Young Sol, Min Ki Lee, Young Dae Kim, Chang Hun Lee
- Korean J Pathol. 2009;43(4):321-328.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.4.321
- 4,115 View
- 58 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Several studies have been conducted on the role of the p63 gene family in non-small cell lung carcinoma (NSCLC). Nevertheless, the role of these genes in the development and progression of NSCLC remains controversial. This study was designed to examine the expression and clinicopathologic significance of the p63 family in NSCLC.
METHODS
Immunohistochemical staining was performed on 92 cases of NSCLC (47 squamous cell carcinomas [SqCCs] and 45 adenocarcinomas [ACs]) using tissue microarray blocks. The results were analyzed and correlated with clinicopathologic data. RESULTS: The expression of delta Np63 (Delta Np63) was elevated in SqCC (39/47), but not in AC (2/45; p<0.01). Both p63 and Delta Np63 had high expression in 39 SqCCs; p63 and Delta Np63 also had a similar geomorphologic distribution in most positive tumors. The expression of Delta Np63 was correlated with histologic type, gender, pT stage, p53 expression, and p63 expression. pT and pN stages were independent factors in survival (p<0.05, respectively).
CONCLUSIONS
The major p63 isoform in NSCLC, Delta Np63, had a strong correlation with p53 and p63, and was exclusively expressed in SqCC. However, our findings suggest that Delta Np63 was not an independent prognostic factor for NSCLC.
- Clinicopathologic Significance of CD44s, CD44v5 and CD44v6 Expression in Non Small Cell Lung Carcinomas.
- Jae Kyun Kim, Chang Hun Lee, Kyeong Min Lee, Jin Mi Song
- Korean J Pathol. 2004;38(2):93-99.
- 2,079 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
CD44 is a polymorphic family of transmembrane glycoproteins generated by alternative splicing of messenger RNA and is involved in the mechanism of tumor invasion and metastasis.
METHODS
The expression of selected CD44 molecules (CD44s, CD44v5, and CD44v6) was determined immunohistochemically in 84 cases of non small cell lung carcinomas (NSCLCs). The results were compared with PCNA index, microvessel density (MVD), and clinicopathological parameters including patient? survival.
RESULTS
CD44s showed a positive reaction in 61.9% (52/84) of NSCLCs, CD44v5 in 73.8% (62/84), and CD44v6 in 39.3% (33/84). Squamous cell carcinomas (SCCs) displayed preferential expression of all CD44 molecules in comparison with adenocarcinomas (ACs) (p<0.001). As a whole, the expression of CD44 molecules was not correlated with clinical parameters (stage, TNM-T, and TNM-N), PCNA index, or MVD. For ACs only, however, CD44v5 expression was negatively correlated with PCNA index (p<0.05). Poor survival was correlated with CD44v5 expression in ACs and CD44v6 in SCCs (both, p<0.05).
CONCLUSIONS
These findings suggest that CD44 molecule in NSCLC could be a distinctive phenotypic marker for SCC, and the possibility that CD44v5 and CD44v6 are in some way instrumental in conditioning the biologic behavior of NSCLC according to major histologic types.
- Small Cell Osteosarcoma Similar to Ewing's Sarcoma in Histologic Findings and MIC2 Expression: A case report.
- Yoon Mee Kim, Suk Woo Yang, Mee Yon Cho, Soon Won Hong, Byung Ho Choi
- Korean J Pathol. 1999;33(3):204-209.
- 2,501 View
- 38 Download
-
 Abstract
Abstract
 PDF
PDF - Small cell osteosarcoma is a rare form of osteosarcoma and the histological differential diagnosis from other small round cell tumors (SRCTs) is difficult. The immunohistochemical stain for MIC2 has been considered an useful diagnostic marker for Ewing's sarcoma and primitive neuroectodermal tumors but recently, other SRCTs such as malignant lymphoma and embryonal rhabdomyosarcoma also showed positive reaction. Therefore, the usefulness of MIC2 must still be proven. We experienced a case of small cell osteosarcoma of the mandible in a 25-year-old man. Histologically, the tumor consisted of small round cells that resembled those of Ewing's sarcoma. Immunohistochemically, the tumor cells expressed diffuse strong positive reaction for MIC2 gene products. However, the scanty foci of lacy osteoid material between the tumor cells seemed to be diagnostic of osteosarcoma. The histologic and immunohistochemical findings of this case suggest close relationship between small cell osteosarcoma and Ewing's sarcoma.
- Fine Needle Aspiration Cytology of Small Cell Carcinoma of the Parotid Gland: A Case Report .
- Chan Kwon Jung, Eun Sun Jung, Youn Soo Lee, Sun Moo Kim, Byung Kee Kim
- J Pathol Transl Med. 1999;10(2):163-167.
- 1,965 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - Primary small cell carcinoma of the salivary gland is a rare neoplasm that accounts for approximately 1.8% of all primary major salivary gland malignancies. Because of its rarity, it is difficult to diagnose small cell carcinoma of the parotid gland by fine needle aspiration cytology(FNAC). We experienced a case of primary small cell carcinoma of the parotid gland in a 72-year-old woman who presented with two palpable masses of the left infraauricular and ocular regions of two to three month's duration, respectively. Aspirate smears from the left infraauricular area were highly cellular on necrotic and lymphocytic background and showed individually dispersed cells or three-dimensional clusters of small cells. The tumor cells were round to oval with a very high nucleocytoplasmic ratio. Nuclei were about two times the size of lymphocytes and had uniformly dispersed but hyperchromatic to pyknotic chromatin. Nucleoli were occasionally visible but were generally inconspicuous. Numerous mitotic figures were detected. The clusters of these small tumor cells exhibited angular nuclear molding, irregular nuclear outlines, and occasionally rosette like arrangement. The tumor was confirmed by histology and immunohistochemistry.
- Primary Undifferentiated Carcinoma of the Endometrium with Small Cell and Trophoblastic Differentiation.
- Chul Hwan Kim, Seoung Hye Park, In Sun Kim, Seung Yong Paik
- Korean J Pathol. 1990;24(1):58-64.
- 2,112 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - This report describes a very rare case of primary undifferentiated carcinoma of the endometrium with small cell and trophoblastic differentiation. The patient was 54-year-old woman with complaints of vaginal bleeding and palpable lower abdominal mass. The light microscopic findings revealed predominantly small cells with round nuclei, spindle cells, and large cells with hyperchromatic bizarre nuclei. Foci of syncytiotrophoblastic giant cells are scattered, especially in the hemorrhagic areas. Immunohistochemical stainging for neuron specific enolase and beta-hCG showed positive reactions to small cells and syncytiotrophoblastic giant cells, respectively. Argentaffin and argyrophil stains, however, showed negative reactions to small cells. The histogenesis of small cell undifferentiated carcinoma of the endometrium remains unclear; however, it may arise from epithelial precursors instead of neuroendocrine cells, and syncytiotrophoblastic cells may be differentiated or dedifferentiated from the undifferentiated carcinoma cells.
- Carcinoid Tumor of the Uterine Cercix: A light and electron microscopic study of two cases.
- Moon Hyang Park, Jung Dal Lee, Yoon Young Hwang
- Korean J Pathol. 1990;24(1):70-76.
- 1,982 View
- 12 Download
-
 Abstract
Abstract
 PDF
PDF - Two cases of carcinoid tumor of the uterine cervix were reported with emphasis on the histologic, cytologic, histochemical and electron microscopic appearance of tumor cells. Based on the light microscopic findings, one case was a well differentiated carcinoid with acinus formation, and the other was a poorly differentiated anaplastic type, being composed of small cells similar to those of oat cell carcinoma of the lung. Both tumors demonstrated scattered argyrophilic cells on Grimelius stain, and contained neurosecretory granules on electron microscopy. They were in stages II b and IV, respectively, at the time of presentation. The latter patient was treated with vinblastin, platinol and bleomycin, but died in 9 months after the initial diagnosis. The former was lost to follow-up study. Importance of distinction between this highly malignant tumor and other varieties of cervical cancer was emphasized.
- Protein Expression and Gene Amplification of Epidermal Growth Factor Receptor in Non-Small Cell Lung Cancer: Correlation with the Response to Gefitinib Therapy.
- Jinyoung Yoo, Kyungji Lee, Ji Han Jung, Byoung Yong Shim, Sung Hwan Kim, Deog Gon Cho, Myeong Im Ahn, Chi Hong Kim, Kyu Do Cho, Hoon Kyo Kim, Seok Jin Kang
- Korean J Pathol. 2008;42(1):1-8.
- 2,282 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Gefitinib is an EGFR tyrosine kinase inhibitor that has shown dramatic effectiveness in a subset of non-small cell lung cancer (NSCLC) patients. We evaluated the response rate to gefitinib, and the significance of the EGFR and HER2/neu status as predictive markers of the tumor response.
METHODS
The EGFR and HER2/neu protein expressions, as determined by immunohistochemistry (IHC) and gene amplification via chromogenic in situ hybridization (CISH), were analyzed in biopsy specimens from 46 patients with advanced NSCLC. After their failure with the first-line treatment, all the patients had received gefitinib treatment.
RESULTS
A partial response (PR) was achieved in 8 patients (17.4%). An EGFR overexpression was detected in 80.4% (37/46) of the tumors, and this was observed exclusively in patients with a PR (100% vs 75.3%, respectively; p=0.076). EGFR gene amplification was present in 47.8% of the tumors (22/46). HER2/neu was overexpressed in 13%(6/46) and it was amplified in 17% (7/46). The overall survival was prolonged in the female patients (p=0.007), and in patients with T1 and T2 disease (p=0.039), adenocarcinoma (p=0.010), a PR (p=0.022), an EGFR IHC+ status (p=0.033), an EGFR IHC+/CISH+ status (p=0.010), or an EGFR+/HER2/neu+ status (p=0.030). On multivariate analysis, gender, T disease and EGFR IHC/CISH remained the significant predictors of survival.
CONCLUSIONS
Gefitinib showed a modest effect for the patients with chemotherapy-refractory advanced NSCLC. A combination of EGFR IHC and CISH might be important for identifying those patients who are most likely to benefit from gefitinib therapy.
- Malignant Small Cell Tumor of the Thoracopulmonary Region (Askin Tumor): Report of a case.
- Young Im Han, Hye Jin Lee, Kang Suek Suh, Sun Kyung Lee
- Korean J Pathol. 1995;29(5):687-690.
- 2,151 View
- 10 Download
-
 Abstract
Abstract
- Malignant small cell tumor(MSCT) of the thoracopulmonary region(Askin tumor) is extremely rare and is seen predominantly in children and adolescents. This tumor represents a distinct clinicopathologic entity of neuroectodertnal origin, arising from the soft tissues of the chest wall or peripheral lung. This tumor tends to recur locally, but does not seem to disseminate widely. The overall survival is poor. Recently, we experienced a case of the MSCT of the thoracopulmonary region of a 12-year-old female. She was admitted because of a chest wall mass on radiographic examination, and a complaint of intermittent chest pain. Grossly, the mass was lobulated, round and had a solid appearance with focal necrosis and hemorrhage on the cut surface. Histologically, small round to oval cells were arranged in compact sheets, nests and lobular patterns with intervening fibrovascular stroma. Ultrastructurally, the presence of loose-fitting membrane-bound neurosecretory granules was noted.
- Small Cell Carcinoma of the Ovary, Hypercalcemic Type, Large Cell Variant.
- Jong Sil Lee, Jong Hak Lee, Yu Kyung Kim, Sun Hoo Park, Gyung Hyuck Ko
- Korean J Pathol. 2001;35(5):440-443.
- 2,469 View
- 38 Download
-
 Abstract
Abstract
 PDF
PDF - We report the clinical and pathological features, including the immunohistochemical and electron microscopic findings, of a case of hypercalcemic type, large cell variant, ovarian small cell carcinoma. A 44-year-old woman complained of abdominal pain and dysmenorrhea. A mass on the left ovary was detected by computer tomographic scan. A total hysterectomy with bilateral salpingo-oophorectomy was done. Histologically, the tumor was predominantly composed of large cells with abundant eosinophilic cytoplasm and prominent nucleoli. Mucin-containing cells and myxoid stroma were also present. Typical follicle-like spaces with lined by small, closely packed epithelial cells with scanty cytoplasm were occasionally seen. No dense core granules were identified on electron microscopic examination.
- Cytologic Findings of Primary Small Cell Carcinoma of the Urinary Bladder: A case report.
- Mi Seon Kwon, Geung Hwan Ahn, Jin Haeng Chung, Seung Sook Lee, Jae Soo Koh
- J Pathol Transl Med. 2001;12(2):121-126.
- 2,241 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - Primary small cell carcinoma of the urinary bladder is a rare malignant tumor. A more rapidly fatal course may be seen in advanced stages of small cell carcinoma as compared to similar stages of urothelial carcinoma. It is very important to recognize this distinct form of bladder cancer by urinary cytology. The differential diagnosis of small cell carcinoma of the urinary bladder includes metastatic small cell carcinoma, urothelial carcinoma, and primary or secondary malignant lymphoma. This article highlights the urinary cytologic diagnosis of a case of primary small cell carcinoma. A 59-year-old male presented with gross hematuria for five months. Urinary cytology showed high cellularity consisting of tiny monotonous tumor cells in the necrotic background. The tumor cells occurred predominantly singly, but a few in clusters. The cytoplasm was so scanty that only a very narrow rim of it was seen. The nuclei were oval or round and had finely stippled chromatin. Rarely, the nuclei contain visible nucleoli. Frequently cell molding was noted in clusters. Many single cells demonstrated nuclear pyknosis or karyorrhexis. The histologic findings of transurethral resection and partial cystectomy specimen were those of small cell carcinoma. Cytologic distinction may be very difficult but careful attention to clinical features and cellualr details can classify these neoplasms correctly.
- Desmoplastic Small Round Cell Tumor of the Sigmoid Colon.
- Kwang Il Kim, Jung Yeol Kim, Insun Kim
- Korean J Pathol. 2001;35(5):451-454.
- 2,060 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Desmoplastic small round cell tumor (DSRCT) is a distinctive disease with a multidirectional differentiation and an aggressive clinical course. It mostly occurs in mesothelial-lined sites, and tumors originating in the paratesticular region, pleura and central nervous system are rarely reported. We report a case of DSRCT occurring in the sigmoid colon of a 39-year-old man, which was difficult to distinguish from small cell neuroendocrine carcinoma. The tumor was characterized by small round cells with irregular nests, cords, or rosette-like structures in the striking desmoplastic stroma. Some tumor cells had a rhabdoid feature with eosinophilic cytoplasmic globules. The tumor cells showed immunoreactivity for cytokeratin, epithelial membrane antigen, vimentin, desmin, neuron-specific enolase and Leu-7. Electron microscopic finding revealed perinuclear globoid whorls of intermediate filaments pushing the nucleus eccentrically.
- Establishment and Characterization of a Small Cell Lung Cancer Cell Line(JePa-1).
- Mi Ja Lee, Ho Jong Jeon, Jong Hoon Chung
- Korean J Pathol. 1997;31(8):695-710.
- 2,112 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - Lung cancer is the most common malignant tumor worldwide and its incidence continues to rise each year. Recent development of molecular biologic method has led to advances in determining the etiologic factors of lung cancer and the establishment of cell lines has provided a lot of information on the through chemosensitivity, radiation biology studies, cytogenetics, and molecular biologic studies, which permits improved treatment for lung cancer. We established a small cell lung cancer cell line, designated JePa-1, obtained from malignant pericardial effusion of small cell lung cancer patient and characterized its morphologic and molecular biologic features. the JePa-1 cell line grew relatively slowly (doubling time 45hrs) as very loosely adherent floating aggregates growing in small clumps with distinct cell outlines and intertwined cords. Also JePa-1 cell line secreted antidiuretic hormones. Electronmicroscopic examination revealed that JePa-1 cell line and xenografts contained electron dense core granules, characteristic of being of neuroendocrine origin. To investigate the tumorigenic capacity, the JePa-1 cell line was injected into SCID and nude mice. Tumors taken from xenografts were observed in 3 out of 4 of the SCID mice and 2 out of 4 of the nude mice. The histologic characteristics of the xenografts were similar to those of the cell line and the original cytologic finding of the pericardial fluid, suggesting small cell carcinoma. The results of immunohistochemical markers showed reactivity for Rb protein, c-myc, TGF-alpha, TGF-beta , EGFR, keratin, NSE, chromogranin, and EMA. The DNA ploidy and the index of the JePa-1 cells was tetraploid and 2.13, respectively. The positive rate for the Rb, c-myc and K-ras proteins of the JePa-1 cell line were 98.9%, 99.3%, and 99.7% respectively as determined by flow cytometry. Cytogenetic analysis using the G-banding technique showed 65 chromosomes with various numerical and structural abnormalities. On examination of the expression of TGF-alpha, TGF-beta , and EGFR by PCR, only the EGFR was positive Through the establishment of JePa-1 cell line, we report in this paper the characterization of a small cell lung cancer such as morphologic and immunocytochemical features, growth characteristics in culture, hormone production, expression of oncoprotein and several growth factors, tumorigenicity, chromosomal abnormalities, and DNA ploidy and index. The JePa-1 cell line will be valuable in vitro studies for the etiology, treatment and the prognostic factors in small cell lung cancer.
- Intraabdominal Desmoplastic Small Cell Tumors with Divergent Differentiation: Report of two cases with immunohistochemical and ultrastructural studies.
- Young Ha Oh, Nam Hoon Kim, Joo Seob Keum, Moon Hyang Park
- Korean J Pathol. 1996;30(1):40-49.
- 2,003 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - We studied two intraabdominal desmoplastic small cell tumors. The patients were two men, 37 and 23 years old, with jaundice and palpable abdominal masses. On exploratory laparotomy, each patient revealed a huge mass in the greater omentum with disseminated peritoneal seeding, measuring 32 cm and 11 cm in its greatest dimension, respectively. The tumor involved the diaphragm, rectal shelf, and cul de sac in case 1, and it involved the porta hepatis, retroperitoneum, and serosal surface of the ascending and transverse colon in case 2. Omentectomy of the huge mass and satellite masses was performed in each patient. Both tumors showed nearly the same histopathologic features. The histologic pattern was suggestive of a metastatic small cell carcinoma, but there was no specific, single primary site. The tumors consisted of variably sized, discrete islands of epithelial-like small cells in dense desmoplastic stroma. The tumor cells revealed divergent epithelial, mesenchymal, and neural differentiation by histologic, immunohistochemical, and electron microscopic observations. Only one cycle of chemotherapy including cisplatin and VP-16 was given in case 1 because of a subsequent hepatic problem, who, thereafter, showed massive intraabdominal recurrent tumors 6 months after diagnosis. In case 2, the poor condition of the patient had made chemotherapy and radiotherapy impossible. Case 2 died of disseminated intravascular coagulation following progressive cachexia 7 months after diagnosis.
- Carcinosarcoma (True Malignant Mixed Tumor) of the Parotid Gland: A Report of a Case with Small Cell Carcinoma as the Carcinoma Component.
- Hun Soo Kim, Hyang Jung Cho, Yeun Tai Chung, Soon Ah Park, Hae Joong Cho, Jin Man Kim
- Korean J Pathol. 2008;42(3):175-180.
- 2,458 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - True malignant mixed tumor (carcinosarcoma) of the salivary gland is an extremely rare tumor. By definition, it is a heterologous neoplasm that's composed of both malignant epithelial and mesenchymal components. We report here on a case of an 83 year old female patient with a parotid gland mass. Histologic examination showed a biphasic pattern of growth with both a poorly differentiated epithelial component and a sarcomatous spindle cell background. The immunohistochemical and ultrastructural findings support the diagnosis of a small cell neuroendocrine epithelial tumor and an undifferentiated malignant mesenchymal features. The histologic and ultrastructural features along with the immunohistochemical findings are presented. We also review the literature and we discuss the different opinions on the exact histogenesis of the true malignant mixed tumor of the salivary gland. To the best of our knowledge, this histological pattern has not been previously reported in the English medical literature.
- Immunohistochemical Study on the Expression of p53 and Bcl-2 Proteins in Non-Small Cell Lung Carcinomas.
- Ok Ju Lee, Do Youn Park, Kang Suek Suh
- Korean J Pathol. 1997;31(9):823-831.
- 1,976 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - To address the possible prognostic value of p53 and Bcl-2 proteins in non-small cell lung carcinomas (NSCLCs), the authors studied 43 cases of NSCLCs diagnosed between the years 1990 to 1995 at Pusan National University Hospital. The patients were treated either by pneumonectomy or lobectomy of the lung. The expression of p53 and Bcl-2 proteins was semiquantitatively analyzed in paraffin sections by immunohistochemical method and correlated with clinicopathologic prognostic parameters of NSCLCs. Overexpression of the p53 protein was found in 31 cases (72.1%) of the 43 NSCLCs. Overexpression of the p53 protein was significantly correlated with the decreasing degree of histologic differentiation, increasing tumor stage, and cigarette smoking. Bcl-2 expression was found in 19 cases (44.2%) of the 43 NSCLCs. Increased expression of the Bcl-2 protein was significantly correlated only with decreasing tumor stage. An inverse relationship was found between p53 and Bcl-2 proteins, but it was not statistically significant. Thus p53 and Bcl-2 proteins, as demonstrated immunohistochemically in routine paraffin sections, could be of value in prediction of the aggressiveness and prognosis of NSCLCs, in agreement with the central role of p53 and Bcl-2 proteins in the evolution of NSCLCs associated with cigarette smoking.
- Urinary Cytologic Findings of Small Cell Neuroendocrine Carcinoma: A Case Report.
- Dong Hoon Kim, Dong Wook Kang, Kyung Hee Kim, Ju Heon Kim, Mee Ja Park
- J Pathol Transl Med. 2002;13(2):78-83.
- 2,002 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - We report the cytologic features of a case of primary small cell carcinoma of the urinary bladder with high grade transitional cell and signet ring cell carcinomatous components. A 64-year-old male presented with gross hematuria for one week. Computed tomography revealed an ill-defined mass in the left lateral wall of the urinary bladder. Urinary cytology showed hypercellularity with predominantly isolated single cells and clustered cells. They have scanty cytoplasm and naked hyperchromatic nuclei with finely granular nuclear chromatin and rare nucleoli. The tumor cells occurred predominantly singe cells, but a few in clusters. Nuclear molding was prominent. No glandular formation or nesting was noted. The second tumor cells had high nuclear/cytoplasmic ratio, irregular nuclear membrane, and coarse granular chromatin. The background was inflamed and necrotic. The histologic findings of transurethral resection were mainly composed of small cell carcinoma, and partly transitional cell and signet ring cell carcinomatous components. Small cell neuroendocrine carcinoma have distinctive cytologic features to make a proper diagnosis.
- An Analysis of HER-2/neu, ERCC1, and GST-pi in Advanced Non-Small Cell Lung Cancer Patients Who are Treated with Platinum-based Chemotherapy.
- Kyung Jin Seo, Byoung Yong Shim, Hoon Kyo Kim, Ji Han Jung, Jinyoung Yoo, Seok Jin Kang, Kyo Young Lee
- Korean J Pathol. 2008;42(6):327-334.
- 2,240 View
- 31 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Platinum-based chemotherapy has shown to be an effective first-line treatment for patients with advanced stage, unresectable non-small cell lung cancer (NSCLC). We evaluated the response rate to combination chemotherapy with cisplatin and taxane, and the significance of the HER-2/neu, ERCC1, and GST-pi status as predictive markers for the tumor response. METHODS: The HER-2/neu, ERCC1, and GST-pi status were analyzed in the biopsy specimens obtained from 35 patients with advanced stage NSCLC prior to cisplatin plus either paclitaxel or docetaxel chemotherapy. RESULTS: The response rate of the tumors to combination chemotherapy was 62.9% (22/35). HER-2/neu was amplified in 51.4% (18/35) of the tumors, and this was observed exclusively in patients with progressive disease (p=0.014). ERCC1 was overexpressed in 77.2% of the specimens (27/35), and this showed a tendency to correlate with the tumor response (p=0.057). GST-pi was detected in 85.7% of the specimens (30/35). Seventy-seven percent of the patients with a negative HER-2/neu and positive ERCC1 status showed a partial response, which was in contrast to only a 25% response rate for the patients with a positive HER-2/neu and negative ERCC1 status (p=0.006). The overall survival was prolonged in the patients without HER-2/neu amplification (15 vs 8.5 months, respectively, p=0.008). On multivariate analysis, the HER-2/neu status remained the significant predictor of survival (p=0.005). CONCLUSIONS: A combination of the ERCC1, HER-2/neu status may define a subset of patients with the most favorable response to combination chemotherapy regimens for treating advanced NSCLC.
- Association of CXCR4 Expression with Metastasis and Survival among Patients with Non-small Cell Lung Cancer.
- Joon Seon Song, Jin Kyung Jung, Jong Chul Park, Dong Kwan Kim, Se Jin Jang
- Korean J Pathol. 2008;42(6):358-364.
- 2,229 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Expression of CXCR4 chemokine receptor, initially described to be involved in the homing of lymphocytes in inflammatory tissue, on breast cancer cell lines is associated with the development of lung metastases. In the present study, we evaluated CXCR4 expression in patients with non-small cell lung cancer (NSCLC). METHODS: Tissue microarray blocks were constructed from 408 formalin-fixed, paraffin-embedded NSCLC samples and analyzed via immunohistochemical staining. RESULTS: We observed CXCR4 expression in 214 (66.3%) of the 323 tumors with cytoplasmic or nuclear staining patterns. These tumors were then divided into 109 negative, 166 weak-positive and 48 strong-positive expression groups. Strong expression of CXCR4 correlated with NSCLC recurrence (p=0.047) and distant metastasis (p=0.035). However, lymph node metastasis (p=0.683) and locoregional recurrence (p=0.856) were not associated with CXCR4 expression. Interestingly, the median overall survival times relative to CXCR4 expression were 71 months in the CXCR4-negative group, 43 months in the weakly positive CXCR4 group and 23 months in the strongly positive CXCR4 group. Strongly positive CXCR4 staining was associated with significantly worse outcomes (p=0.005, log-rank test).
CONCLUSIONS
Expression of CXCR4 was associated with distant NSCLC metastases and shorter survival times.
- Cytodiagnosis of Primary Small Cell Carcinoma of the Urinary Bladder: A Case Report.
- Hye Sun Kim, Aee Ree Kim, Chul Hwan Kim, Yang Seok Chae, Nam Hee Won
- J Pathol Transl Med. 1994;5(2):167-171.
- 1,827 View
- 15 Download
-
 Abstract
Abstract
 PDF
PDF - Samll cell carcinoma of the urinary bladder is a rare tumor which occurs in about 0.48% of all bladder tumors. We report cytologic features of small cell carcinoma of the urinary bladder in a 66-year-old man who had painless total gross hematuria, which was confirmed by partial cystectomy. In urine cytology, abundant tumor cells appeared in scattered and clustered forms in a bloody background. The tumor cells were small and uniform in size with a high nuclear/cytoplasmic ratio. The nuclei of the tumor cells were hyperchromatic, characteristically molded and showed inconspicuous nucleoli. The cytoplasms were scanty and plae blue.
- Relationship among the Expression of Cyclin D1, p21, and p53 Protein, and Prognosis in Non-Small Cell Lung Carcinomas.
- Seok Woo Yang, Sang Ho Cho, Woo Ick Yang, Woo Hee Jung, Chul Min Ahn, Doo Yun Lee
- Korean J Pathol. 1999;33(12):1120-1130.
- 2,154 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Recently, cell cycle regulators have been suggested as new prognostic factors of the lung cancer. In this study, we evaluated the expression of cyclin D1, p21, and p53 using the X2-test, with regard to the stage of the patients, histologic type, and histologic differentiation in the 135 cases of non-small cell lung carcinomas (NSCLC). To evaluate the confounding effects among cyclin D1, p21, and p53 on X2-test analysis, we used the Mantel-Haenzel test. The NSCLC in this study included 82 cases of squamous cell carcinoma and 53 cases of adenocarcinoma. Each nuclear staining of cyclin D1, p21, and p53 was observed in 65 cases (48.1%), in 54 cases (40.0%), and in 81 cases (60.0%) of NSCLCs, respectively. Only p53 expression was significantly associated with the stage (stage I, II, IIIa) (p<0.05) and squamous cell carcinoma (p<0.05). On the other hand, cyclin D1 expression was significantly associated with the histologic differentiation. The confounding effects among cyclin D1, p21, and p53 revealed that only p21 expression changed the relationship between p53 and stage. In this regard, further study is needed.
- Differential Diagnosis between Small Cell Carcinoma and Adenocarcinoma of Lung in Fine Needle Aspiration Cytology.
- Young Hee Choi, Jae Soo Koh, Sunhoo Park, Min Suk Kim, Soo Youn Cho, Jung Soon Kim, Hwa Jung Ha, Seung Sook Lee
- J Pathol Transl Med. 2006;17(2):120-125.
- 2,801 View
- 71 Download
-
 Abstract
Abstract
 PDF
PDF - Distinguishing small cell carcinoma from other lung malignancies is of great clinico-therapeutic significance. Small cell carcinoma is an aggressive tumor with a tendency to metastasize early. Survival time if untreated is low but this tumor is highly responsive to chemotherapy. We have occasionally experienced difficulties in differentiation between adenocarcinoma and small cell carcinoma of the lung in fine needle aspiration cytology (FNAC). The aim of this study was to investigate the possibility of distinguishing small cell carcinoma from adenocarcinoma of the lung in FNAC. We evaluated cytomorphological features of FNAC specimens from 62 small cell carcinomas and 57 adenocarcinomas from the lung that were confirmed by biopsy and/or immunohistochemistry on cell block. Cytomorphological details of the two tumors were compared. Nuclear smearing and nearly absent cytoplasm were the most distinct findings in small cell carcinoma compared to adenocarcinoma (p<0.05). Necrotic background, architecture and chromatin pattern, nuclear molding and nucleoli were significantly different (p<0.05). Nuclear size, nuclear membrane nature and nuclear size variation however were not helpful in distinguishing the two tumors. Combining several features described above, small cell carcinoma can be properly differentiated from adenocarcinoma on FNAC. FNAC is proposed as a diagnostic tool of small cell carcinoma of the lung in the case of inaccessibility to biopsy, and so may allow the proper therapeutic strategies to be determined in such cases.
- Fine Needle Aspiration Cytology of Metastatic Cell Carcinoma of Lymph Nodes: Comparison to Non-Hodgkin's Lymphoma on 5 Cases.
- Yeon Mee Kim, Hye Je Cho, Ill Hyang Ko
- J Pathol Transl Med. 1996;7(1):44-50.
- 3,870 View
- 93 Download
-
 Abstract
Abstract
 PDF
PDF - Small cell carcinoma of the lung is characterized by cells with finely stippled chromatin and scanty cytoplasm as well as a particularly aggressive clinical course and favorable response to the chemotherapy. Recently percutaneous fine needle aspiration(FNA) biopsy has become both widely established and highly respected for the diagnosis of lung cancer. However metastatic small cell carcinoma of lymph node should be cytologically differentiated from the small round cell tumor of particular sites, especially malignant lymphoma, because small cell carcinoma of classic oat cell type may simulate small cell non-Hodgkin's lymphoma. We report five cases of metastatic small cell carcinoma of intermediate cell type diagnosed by FNA of the enlarged lymph nodes of the neck and axilla. The cytologic smears contained diffuse small neoplastic cells larger than lymphocytes with dense, pyknotic nuclei and extremely scanty cytoplasm. Apparently viable large tumor cells have vesicular nuclei with granular, sometimes very coarse chromatin. The characteristic cytologic features of small cell carcinoma as compared to malignant lymphoma were as follows.: 1) small cells with dense pyknotic nuclei are evenly distributed in the background of apparently viable larger tumor cells, admixed with mature lymphocytes and phagocytic macrophages. 2) small loose aggregates of cells with nuclear molding are indicative of small cell carcinoma rather than non-Hodgkin's lymphoma. 3) the cytoplasmic and nuclear fragments of tumor necrosis are more dominant in the smears of small cell carcinoma. 4) nuclear membrane and nucleoli are generally indistinct in small cell carcinoma due to condensation of chromatin.
- Expression of p53 and Vascular Endothelial Growth Factor mRNA in Angiogenesis of Non-Small Cell Lung Carcinoma.
- Jun Seog Kim, Tae In Park, Myoung Hoon Lee, Eun Kyoung Kwak, Ji Young Park, Jung Sik Kwak, Jong Min Chae
- Korean J Pathol. 2003;37(1):35-40.
- 2,074 View
- 12 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Angiogenesis is one of the most important factors in the progression and me-tastasis of malignancies. Angiogenesis is a multistep process requiring the interaction of numerous factors able to stimulate the growth and development of new vessels. But, understanding of the mechanism involved in VEGF expression is unclear.
METHODS
Expressions of p53 and VEGF, and neovasculiarization were examined in 19 cases of surgically resected non-small cell carcinoma of the lung by the immunohistochemical staining. Furthermore, VEGF mRNA expressions were quantified in all cases using the real-time quantitative RT-PCR. These results were compared with clinicopathologic parameters such as histologic grade and stage.
RESULTS
Tumors with high aberrant p53 expressions showed significantly higher VEGF mRNA ex-pressions and microvessel counts than those with low p53 expressions. Expressions of p53 as well as VEGF and micovessel counts were closely associated with the tumor stage, but not with the histologic grade and other clinical parameters.
CONCLUSIONS
These results suggest that aberrant p53 expression may play a role in the regulation of VEGF expression and may be involved in controlling angiogenesis in non-small cell carcinoma of the lung.

 E-submission
E-submission
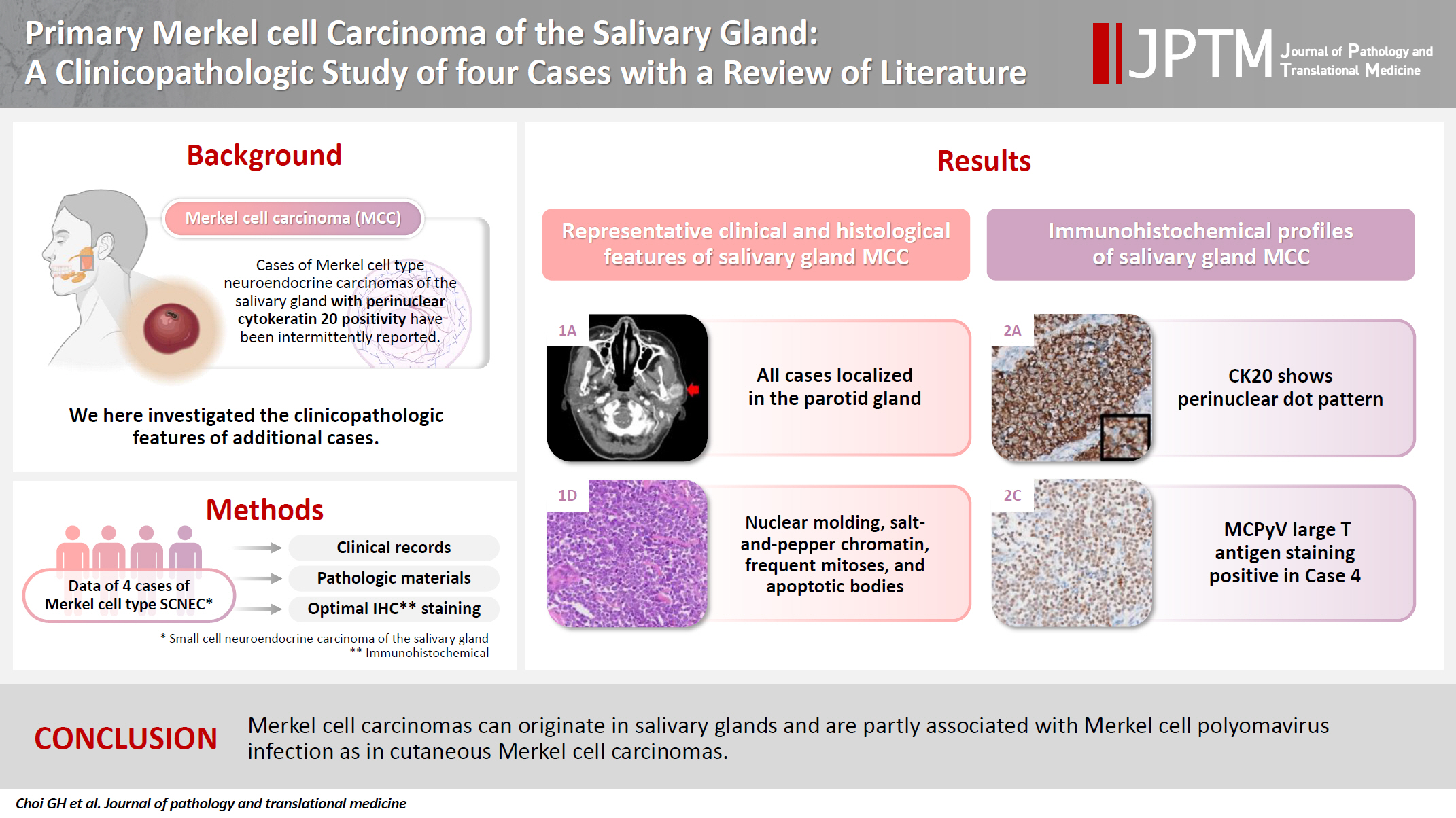

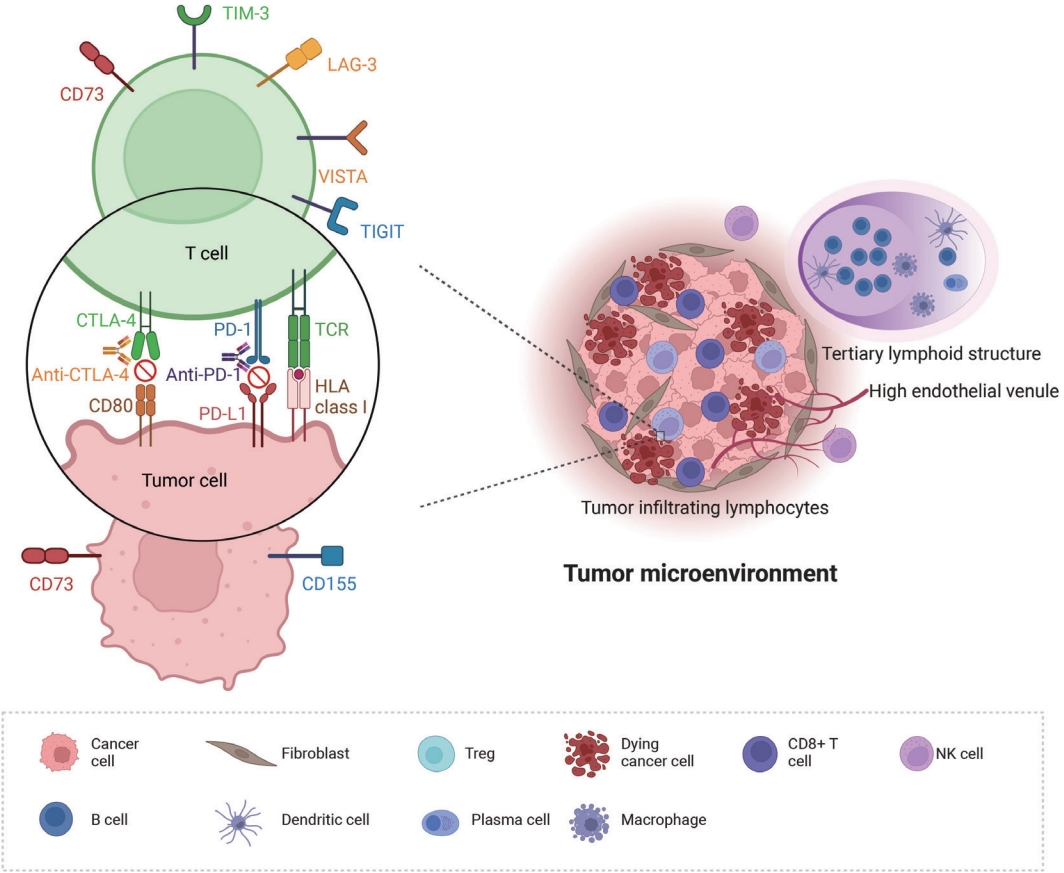
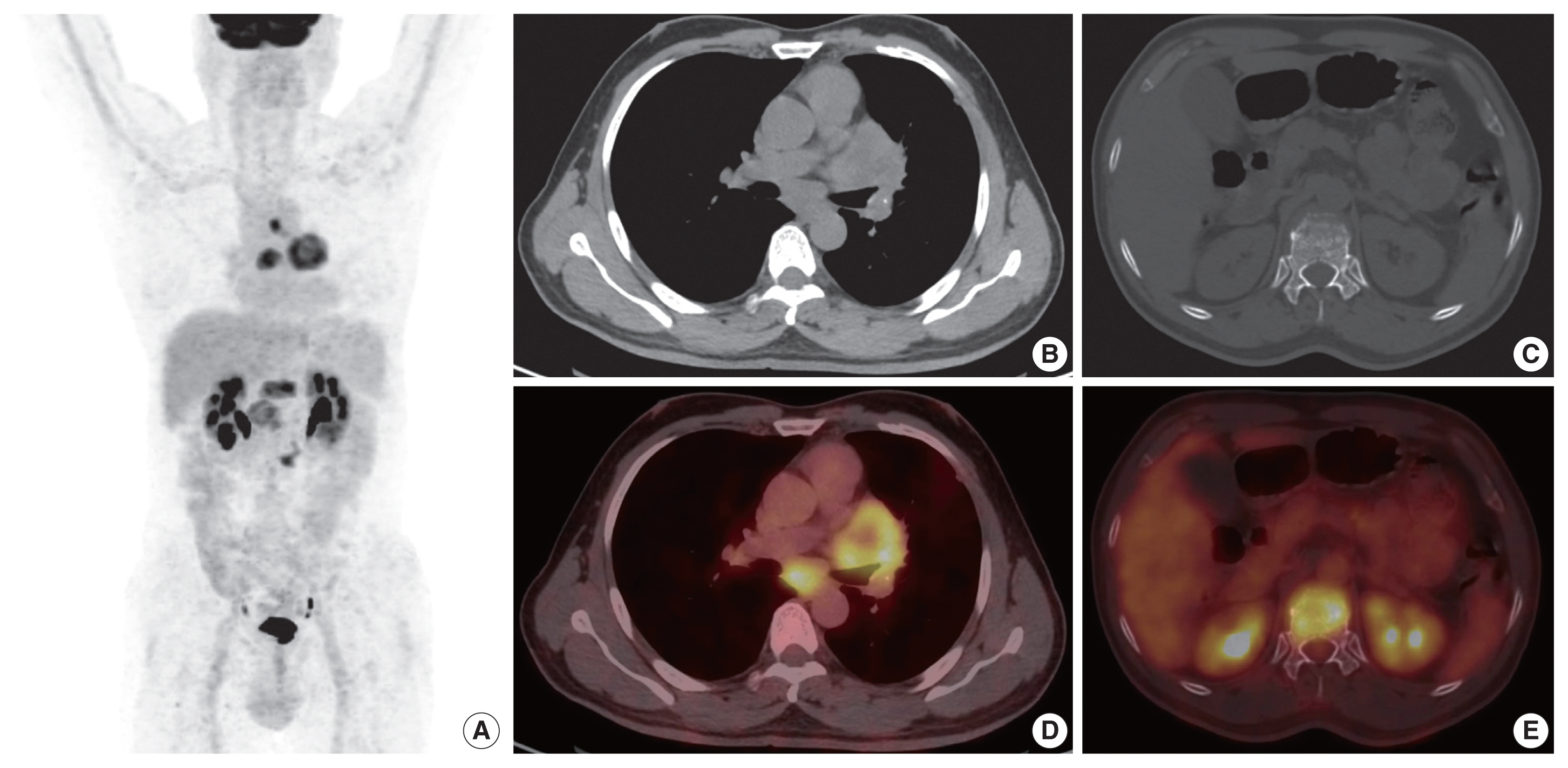
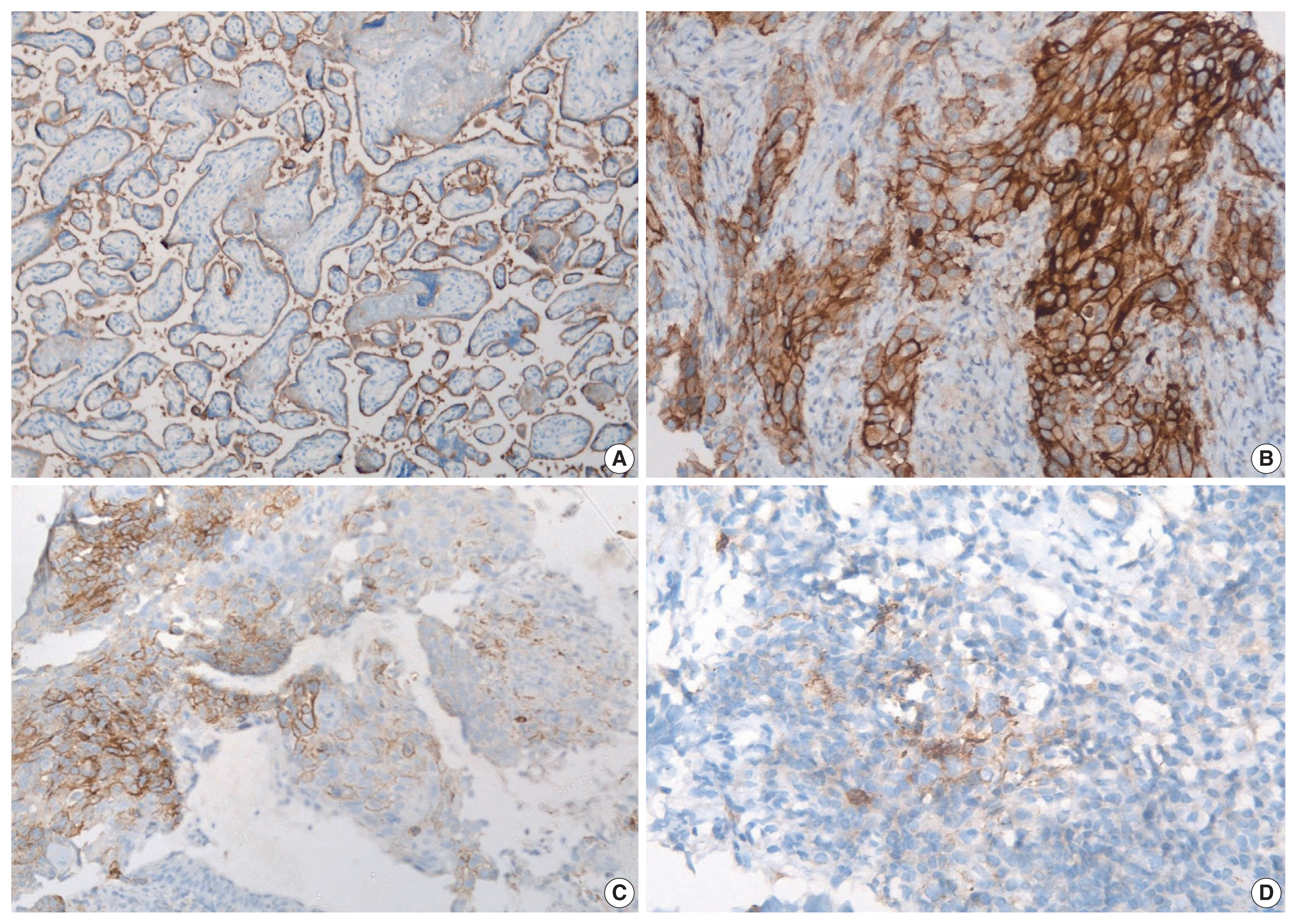
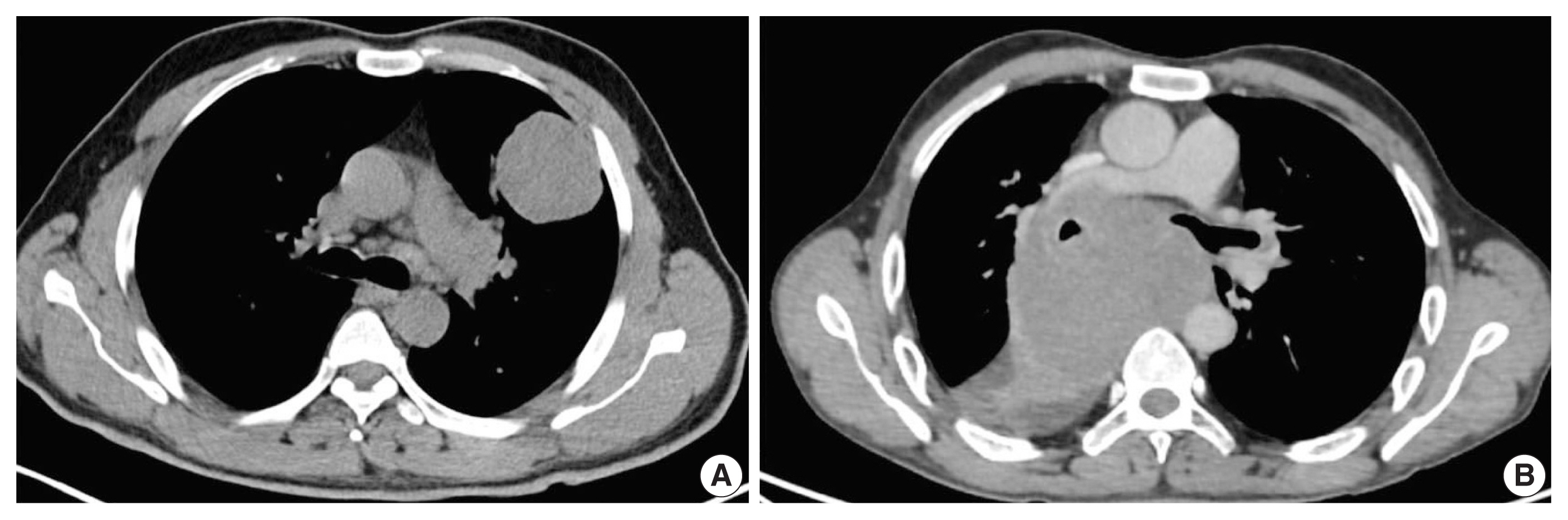
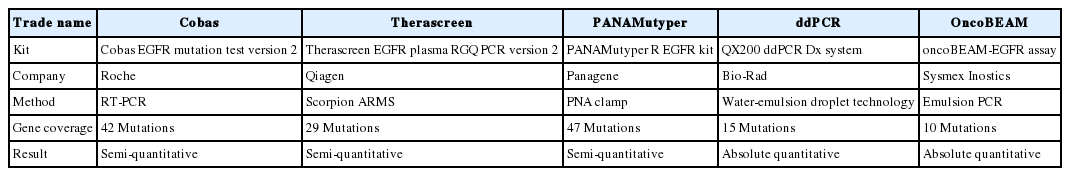
 First
First Prev
Prev



