Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 55(5); 2021 > Article
-
Original Article
SMARCA4/BRG1 protein-deficient thoracic tumors dictate re-examination of small biopsy reporting in non–small cell lung cancer -
Anurag Mehta1
 , Divya Bansal2
, Divya Bansal2 , Rupal Tripathi3
, Rupal Tripathi3 , Ankush Jajodia4
, Ankush Jajodia4
-
Journal of Pathology and Translational Medicine 2021;55(5):307-316.
DOI: https://doi.org/10.4132/jptm.2021.05.11
Published online: June 21, 2021
1Department of Laboratory, Molecular and Transfusion Services, Rajiv Gandhi Cancer Institute and Research Centre (RGCIRC), New Delhi, India
2Department of Pathology, Rajiv Gandhi Cancer Institute and Research Centre (RGCIRC), New Delhi, India
3Department of Research, Rajiv Gandhi Cancer Institute and Research Centre (RGCIRC), New Delhi, India
4Department of Radiology, Rajiv Gandhi Cancer Institute and Research Centre (RGCIRC), New Delhi, India
- Corresponding Author: Divya Bansal, MD, Department of Pathology, Rajiv Gandhi Cancer Institute and Research Centre (RGCIRC), New Delhi 110085, India, Tel: +91-9971869669, Fax: +91-11-27051037, E-mail: divyabansalrgci@gmail.com
© 2021 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background
- SMARCA4/BRG1 protein–deficient lung adenocarcinomas and thoracic sarcoma are recently described entities that lack distinctive histological features, transcription termination factor 1 (TTF1) reactivity, and actionable driver mutations. The current diagnostic path for small lung biopsies as recommended by the World Health Organization (WHO, 2015) is likely to categorize these as non–small cell carcinoma–not otherwise specified (NSCC-NOS). The present study attempts to define the subtle but distinctive clinicopathologic features of SMARCA4/BRG1 protein-deficient thoracic tumors; highlight their unique biology; and addresses the unmet need to segregate these using a new, tissue-proficient diagnostic pathway.
-
Methods
- All lung biopsies and those from metastatic sites in patients with suspected advanced lung cancer and classified as NSCC-NOS as per WHO (2015) guidelines were subjected to BRG1 testing by immunohistochemistry. SMARCA4/BRG1 protein–deficient thoracic tumors were evaluated by an extended immunohistochemistry panel. Predictive biomarker and programmed death–ligand 1 testing was conducted in all cases.
-
Results
- Of 110 cases, nine were found to be SMARCA4/BRG1 protein-deficient; six were identified as SMARCA4/BRG1 protein–deficient lung adenocarcinomas, and three were SMARCA4/BRG1 protein-deficient thoracic sarcomas. The histology ranged from poorly differentiated to undifferentiated to rhabdoid. None of the cases showed significant expression of TTF1 or p40, and no actionable mutation was identified.
-
Conclusions
- It is difficult to separate BRG1-deficient lung adenocarcinomas and thoracic sarcomas based on morphology alone. We propose a diagnostic pathway for small biopsies of thoracic tumors to segregate these distinct entities so that they can be studied more efficaciously for new biomarkers and therapeutic options.
- Study place and study duration
- The present study is an analysis of nine cases of SD-TT diagnosed at Rajiv Gandhi Cancer Institute and Research Center, New Delhi, from 1 September 2020 to 15 January 2021. Clinicoradiological details were obtained from the electronic medical records (EMR), and follow-up information was gathered either through EMR or via telephone.
- Study population
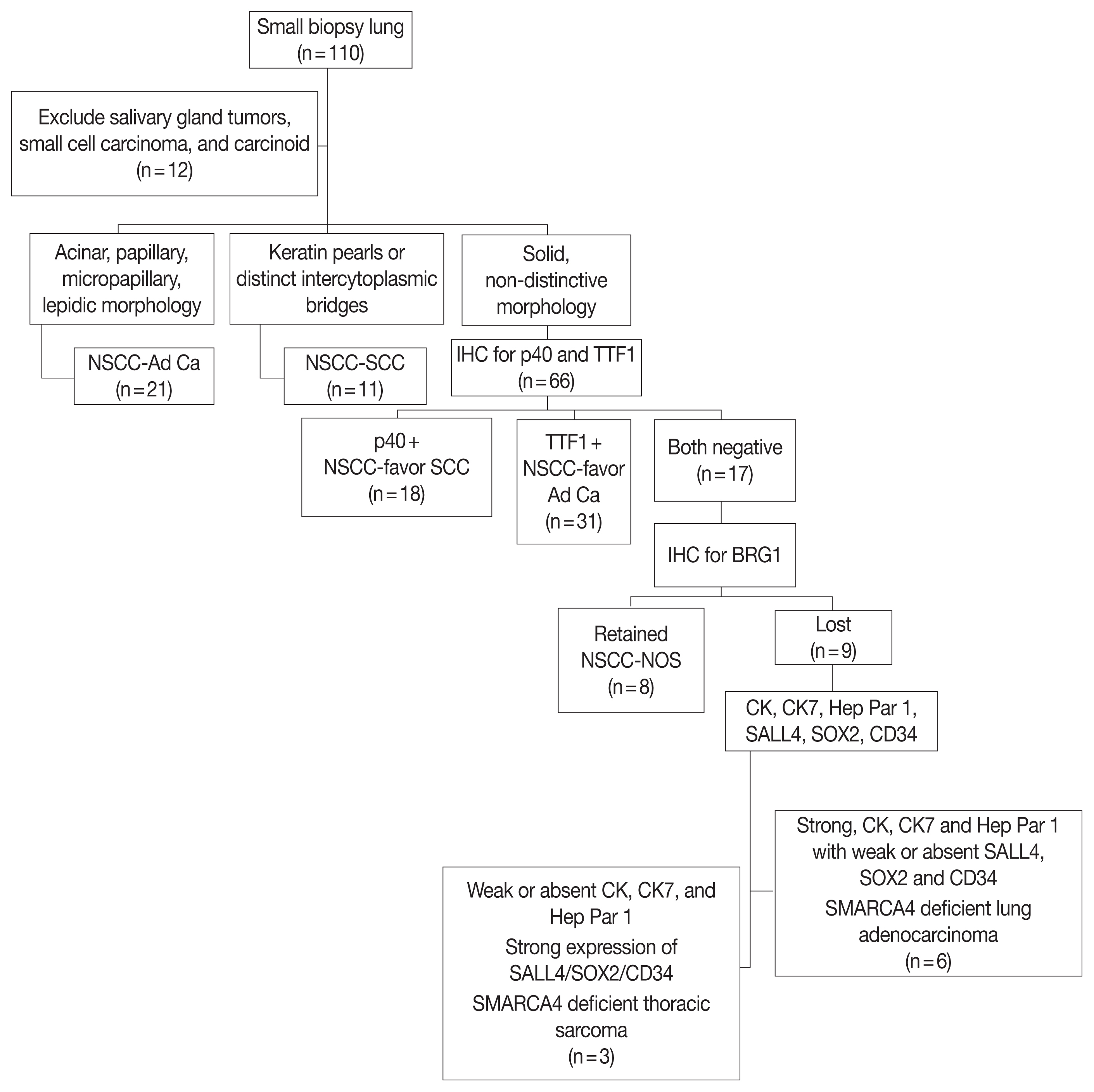
- The current World Health Organization (WHO) guidelines do not advocate extensive immunophenotyping beyond transcription termination factor 1 (TTF1) and p40 for classifying small biopsy specimens from suspected lung cancers and classify lung carcinomas as NSCC-NOS in the absence of both TTF1 and p40 [18]. SD-TT have been shown to be confined largely to TTF1-negative/low expression NSCC [10,11,19]. We reaffirmed these findings using two tissue microarrays of 25 samples of TTF1-negative and TTF1-positive NSCC subjected to BRG1 IHC testing. None of the TTF1-positive (moderate to strong nuclear expression) NSCCs showed loss of BRG1 expression, while eight of 25 cases of TTF1-negative NSCC showed loss of BRG1 expression. With similar findings noted in the literature, we applied additional IHC for BRG1 expression for this subset of lung cancers to identify SD-TT starting in September 2020. Nine such cases were identified to be BRG1 deficient. Of these, eight were newly diagnosed, and one (case number 4) underwent repeat biopsy for programmed death–ligand 1 (PD-L1) tumor proportion scoring after failure of multiple lines of cytotoxic therapy.
- Immunohistochemistry
- All lung biopsies and those from metastatic sites in patients with suspected advance lung cancers were classified per WHO (2015) guidelines [18] into NSCC-Adenocarcinoma (Ad Ca)/favor adenocarcinoma, NSCC–squamous cell carcinoma (SCC)/favor SCC, and NSCC-NOS using only p40 (clone BC28, ready-to-use [RTU], Zytomed Systems, Berlin, Germany) and TTF1 (clone-SP141, RTU, Ventana, Tucson, AZ, USA) IHC. Those classified as NSCC-NOS were tested for expression of SMARCA4/BRG1 protein (1:100, EPNCIR111A, Abcam, Cambridge, UK). Cases with loss of BRG1 protein were classified as SD-TT and further evaluated using an extended IHC panel of panCK (1:200, AE1, AE3, 5D3, Zytomed), cytokeratin 7 (CK7; 1:200, OV-TL 12/30, Thermo Fisher Scientific, Waltham, MA, USA), epithelial membrane antigen (EMA; 1:50, E29, Dako, Santa Clara, CA, USA), Hep Par 1 (OCHIE5, RTU, PathnSitu, Pleasanton, CA, USA), SALL4 (EP299, RTU, PathnSitu), SOX2 (1:100, SP76, Cell Marque, Darmstadt, Germany), CD34 (QBEnd10, RTU, Dako), synaptophysin (1:100, MRQ-40, Cell Marque), SMARCB1/INI1 (MRQ-27, RTU, Cell Marque), and E-cadherin (NCH-38, 1:100, Dako). Tissues were formalin-fixed, paraffin-embedded, sectioned to 4 μm thickness, and then fixed for 6–48 hours in neutral buffered formalin before conventional tissue processing and staining by IHC. Antigen retrieval at alkaline pH of 8.6 in Tris-EDTA buffer and further staining steps were performed on an automated IHC staining instrument (Benchmark XT, Ventana Medical Systems, Inc. [F. Hoffmann-La Roche Ltd.]). The chromogenic signal was generated using the Ventana UltraView universal 3,3′-diaminobenzidine (DAB) detection kit (Ventana Medical Systems, Inc. [F. Hoffmann-La Roche Ltd.]). All IHC stains were applied with appropriate positive controls. For IHC analysis, moderate to strong staining intensity in > 5% of tumor cells with nuclear (TTF-1, p40, SOX2, and SALL4), cytoplasmic (panCK, CK7, CD34, Hep Par 1, and synaptophysin), or membranous (EMA and E-cadherin) pattern was considered positive. BRG1 immunostaining that exhibited a null phenotype in tumor cells with strong nuclear staining in the stromal fibroblasts as well as the endothelial and inflammatory cells was deemed as lost and defined the SD-TT cohort.
- Anaplastic lymphoma kinase 1 (ALK-1) protein expression was assessed using a U.S. Food and Drug Administration (FDA)–approved IHC assay employing anti-ALK (D5F3) rabbit monoclonal primary antibody with other proprietary components of the Ventana ALK assay on the Ventana Benchmark XT Autostainer (using the Ventana Optiview DAB and amplification kit).
- PD-L1 expression testing was performed using rabbit Anti-Human PD-L1 monoclonal antibody (clone SP263) on the Ventana Benchmark XT, and partial or complete membranous expression of any intensity in ≥1% of tumor cells was considered significant.
- DNA extraction and polymerase chain reaction
- A predictive biomarker search was performed for epidermal growth factor receptor (EGFR) using the Qiagen EGFR Therascreen RGQ polymerase chain reaction (PCR) kit, an FDA-approved amplification refractory mutation system. Five sections of 4 μM each were collected in Eppendorf tubes by manual macro-dissection to enrich tumor fraction wherever necessary. DNA was extracted using the Qiagen DNeasy blood and tissue kit (Hilden, Germany). The DNA was quality checked on the Qubit fluorometer. Multiplexed reverse transcription PCR was carried out on a ROTORGENE thermal cycler (Qiagen) in eight tubes along with positive and no template controls. Interpretation was conducted per the manufacturer’s instructions.
- Fluorescence in situ hybridization
- Fluorescence in situ hybridization (FISH) analysis was performed on 4 μM formalin-fixed and paraffin-embedded tissue sections following a standardized protocol that included pretreatment (dewax/proteolysis), denaturation, probe application, and hybridization; application of 4′,6-diamidino-2-phenylindole (DAPI)/antifade solution; and analysis of slides using Leica fluorescent microscopy (DM6000B). ROS1 (ROS proto-oncogene 1, receptor tyrosine kinase) rearrangement was tested by FISH using a dual-color break-apart probe (ZytoLight Spec ROS1, ZytoVision, Germany) as previously described [20].
- One case (case No. 1) was subjected to a targeted panel for multigene profiling using the Oncomine focus assay on the Ion Torrent Personal Genome Machine (Ion PGM, Thermo Fisher Scientific). Reaffirmation of the next-generation sequencing findings for copy number gain used FISH for c-MYC. The XL MYC BA spectral orange-labeled probe hybridizing proximal to the MYC gene region at 8q24.21 and a green-labeled probe hybridizing distal to the MYC gene region at 8q24.21 were applied (Metasystems Probes GmbH, Altlussheim, Germany). No centromeric probe was used. The number of c-MYC signals per cell was counted in 100 tumor cells and averaged. c-MYC copy number gain was defined as average copy number ≥ 3.0.
MATERIALS AND METHODS
- Clinical findings
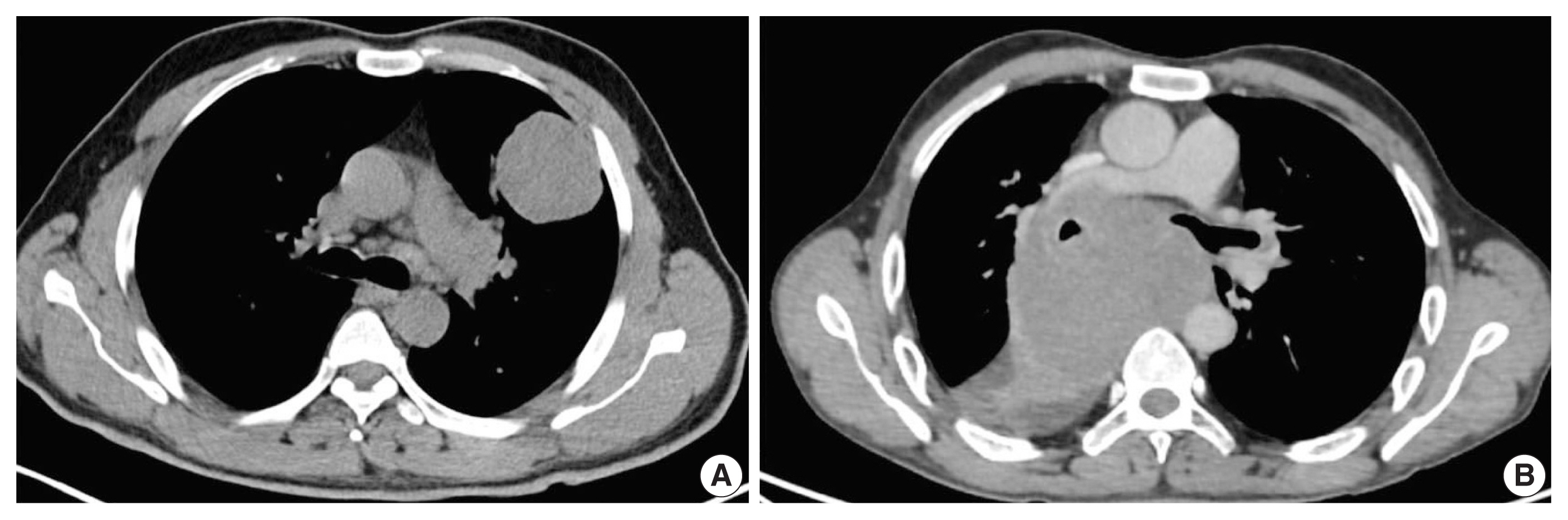
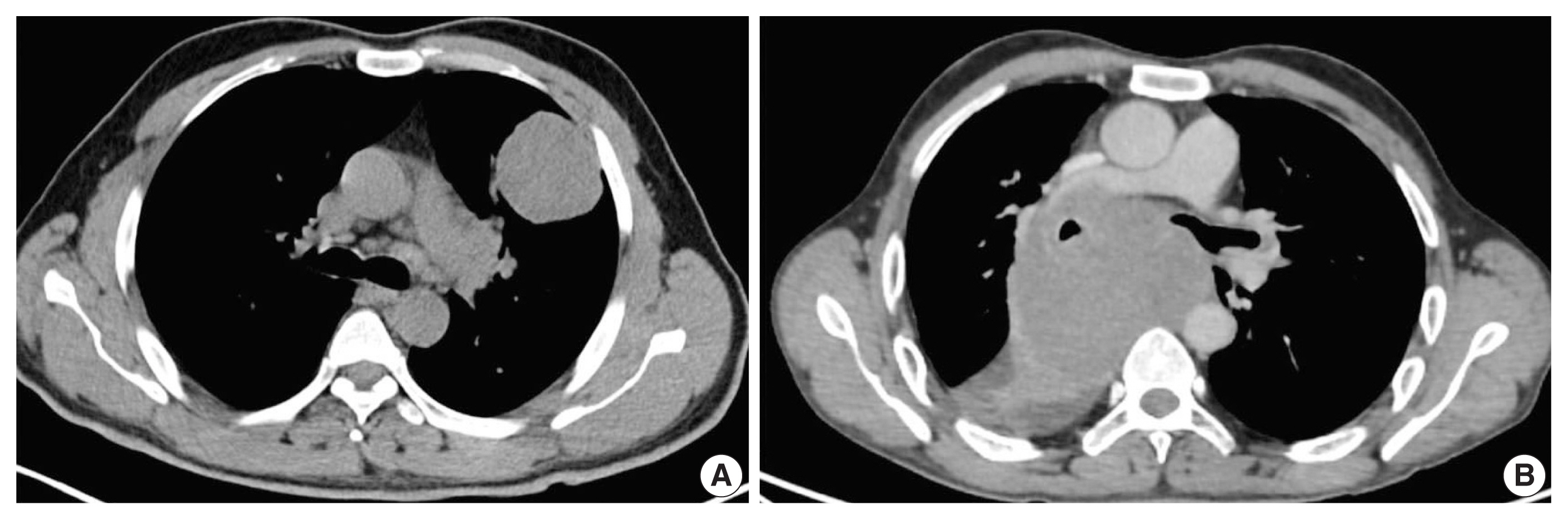
- A total of 110 cases of thoracic tumors was identified during this period, of which nine (8.1%) were found to be SMARCA4 deficient. Six cases (case Nos. 1–6) were SD-LUAD, and three (case Nos. 7–9) were SD-TS. Patient age ranged from 45–73 years, with a male to female ratio of 3.5:1. All cases of SD-LUAD had history of smoking, lung mass, bulky lymphadenopathy, and bony involvement. All cases of SD-TS had a significant history of smoking; two (case No. 7, case No. 9) had massive lung disease (Fig. 1A), while one had mediastinal disease (case No. 8) (Fig. 1B). All cases of SD-TS also had bulky lymphadenopathy. However, no bony involvement was noted in any SD-TS patients. The clinical features of SD-TT are summarized in Table 1.
- Pathological findings in SD-LUAD
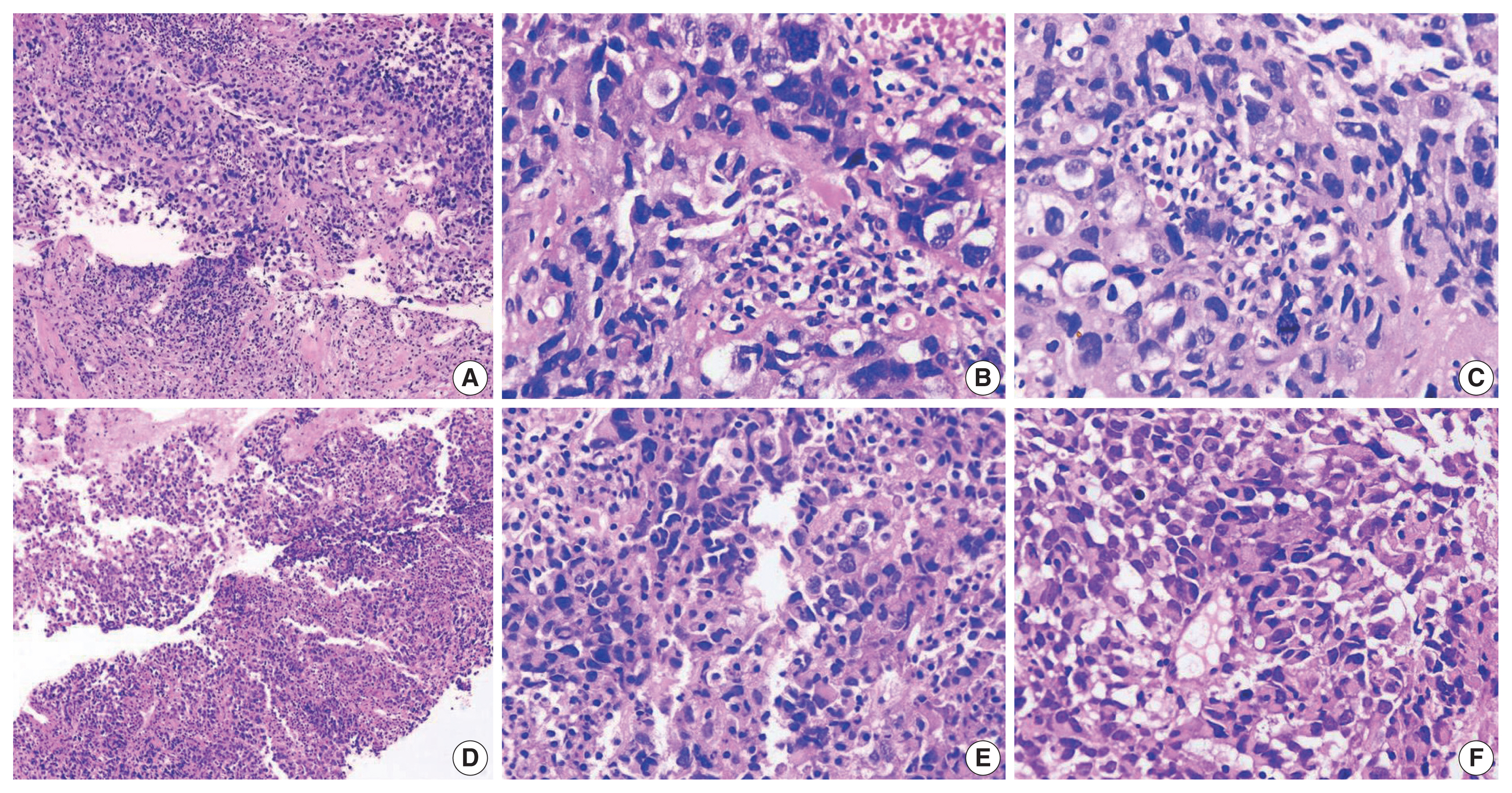
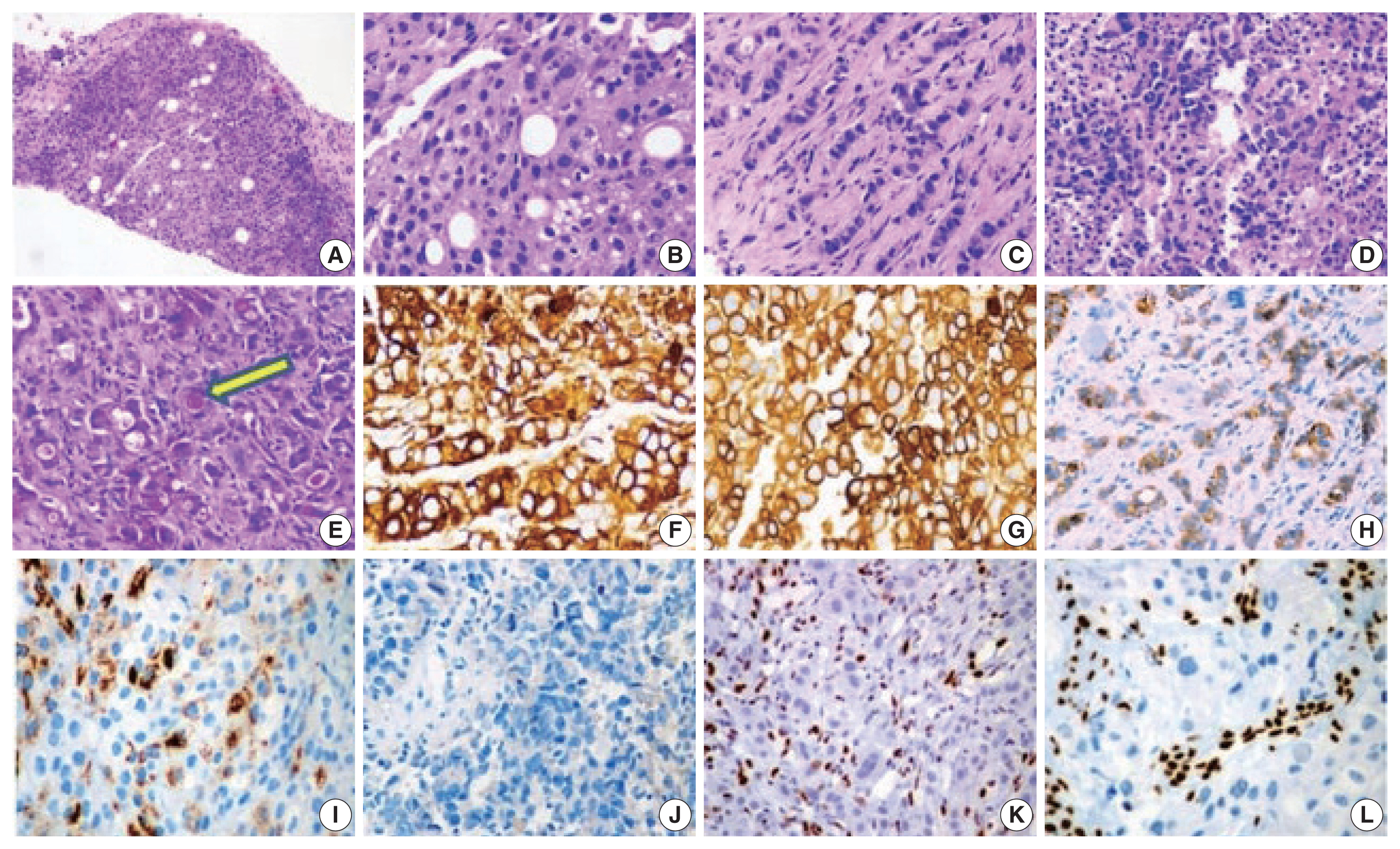
- The histopathologic characteristics of SD-LUAD are summarized in Table 2 (case Nos. 1–6) and shown in Fig. 2A–D. All six cases of SD-LUAD had a solid pattern of growth in the biopsied material, while case No. 2 also showed a vague acinar pattern focally. One case (case No. 2) had an Indian file pattern of growth that resembled lobular carcinoma of breast (Fig. 2C); however, E-cadherin expression was intact, and none of the IHC markers for breast cancer (GATA3, estrogen receptor, and progesterone receptor) were positive. Case Nos. 4 and 6 showed multicell trabecular patterns (3–4 cell layer thick) reminiscent of hepatocellular carcinoma. All tumors were characterized by large constituent cells possessing eosinophilic to clear cytoplasm (Fig. 2A, B). Scattered populations of rhabdoid cells were seen in two cases (case Nos. 3 and 5) (Fig. 2D). Four cases (case Nos. 1, 2, 4, and 6) exhibited scattered cells with blue intracytoplasmic mucin, which were mucicarmine positive (Fig. 2E).
- The cytoplasmic margins of large polygonal cells were sharp and mimicked squamous morphology. The nuclei were large and irregularly contoured with cloudy chromatin. The rhabdoid population of tumor cells showed well-described, eccentric nuclei with prominent eosinophilic nucleoli and a cytoplasmic globule filled with hyaline content (Fig. 2D). Mitosis was intense. Apoptosis and wide swaths of necrosis were common. All our cases revealed inflamed stroma rich in lymphocytes and neutrophils (Fig. 2D). Neutrophilic emperipolesis was observed in three cases (Table 2).
- The IHC profile of SD-LUAD is summarized in Table 3 and shown in Fig. 2F–L. Cases Nos. 1, 2, 4, and 6 exhibited diffuse positivity for CK, CK7, and BerEp4 (Fig. 2F–H) and variably intense positivity for Hep Par 1 (Fig. 2I), but none of the cases was positive for SOX2, CD34, or SALL4. Diffuse positivity for CK7 and BerEp4 was consistent with adenocarcinoma appellation. Case Nos. 3 and 5 had strong CK and Hep Par 1 positivity along with focal positivity for two of three markers of stemness (SOX2, CD34, and SALL4), while both of them were negative for CK7 and BerEp4. Cases that showed focal expression of markers of stemness also had focal rhabdoid morphology.
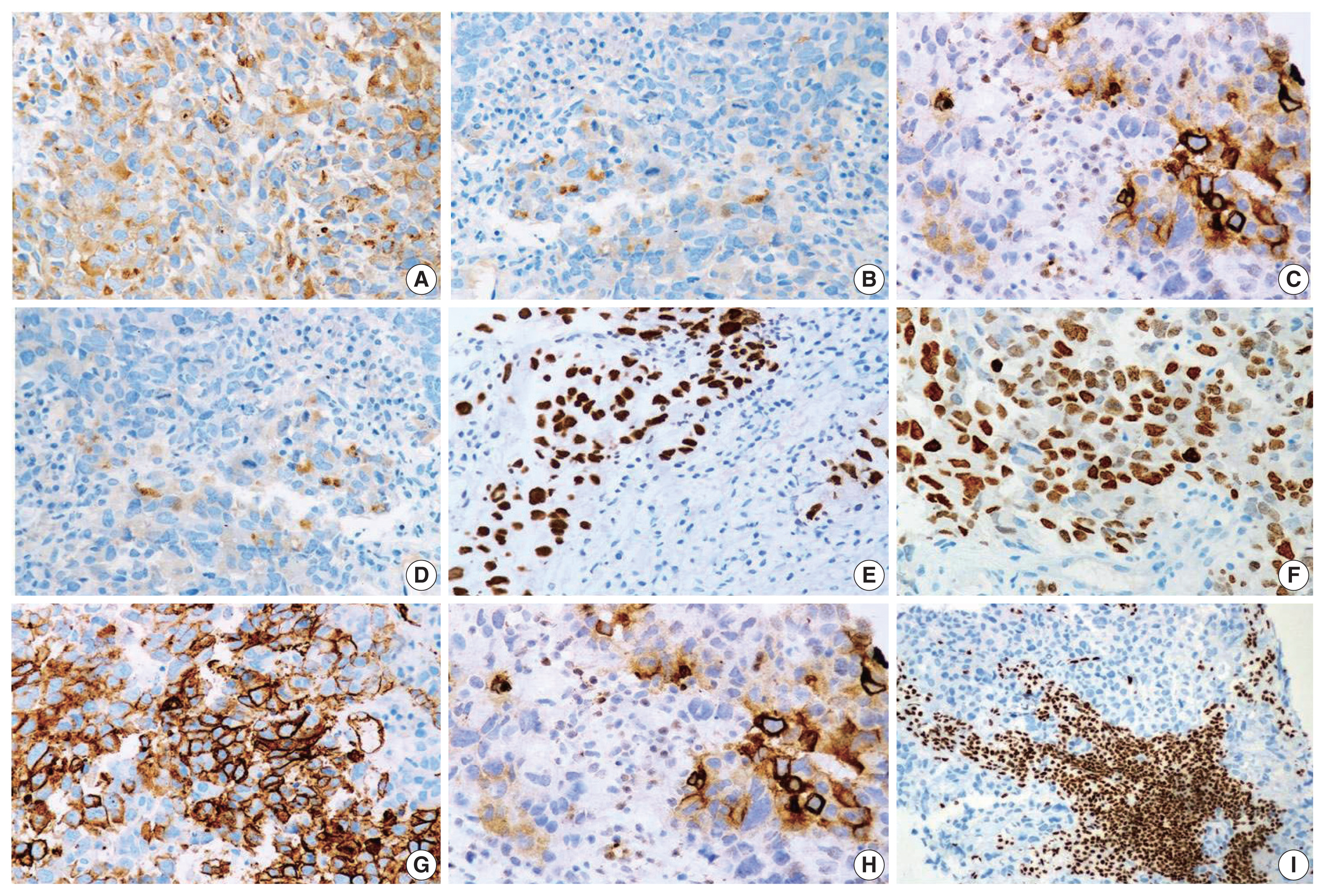
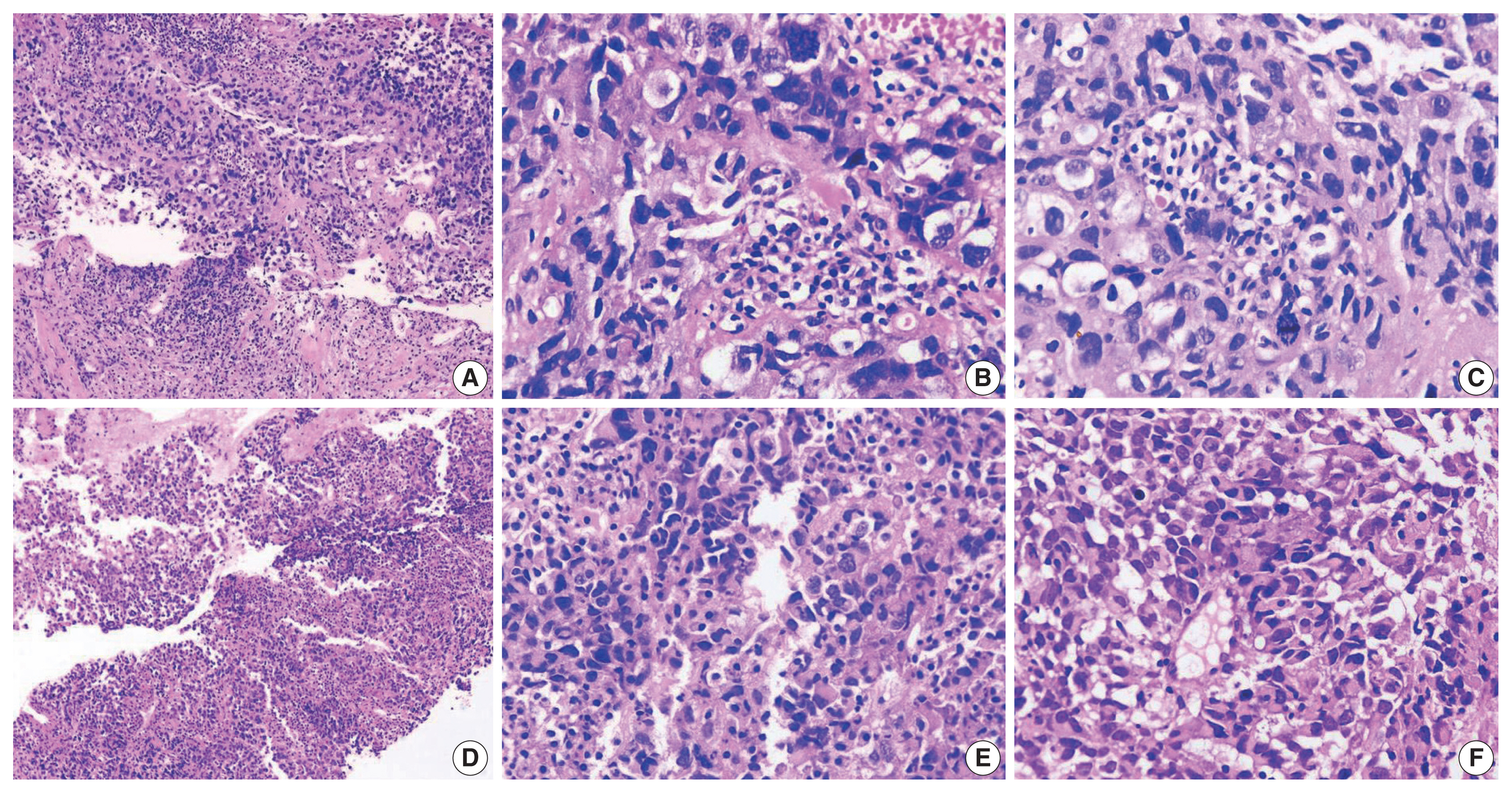
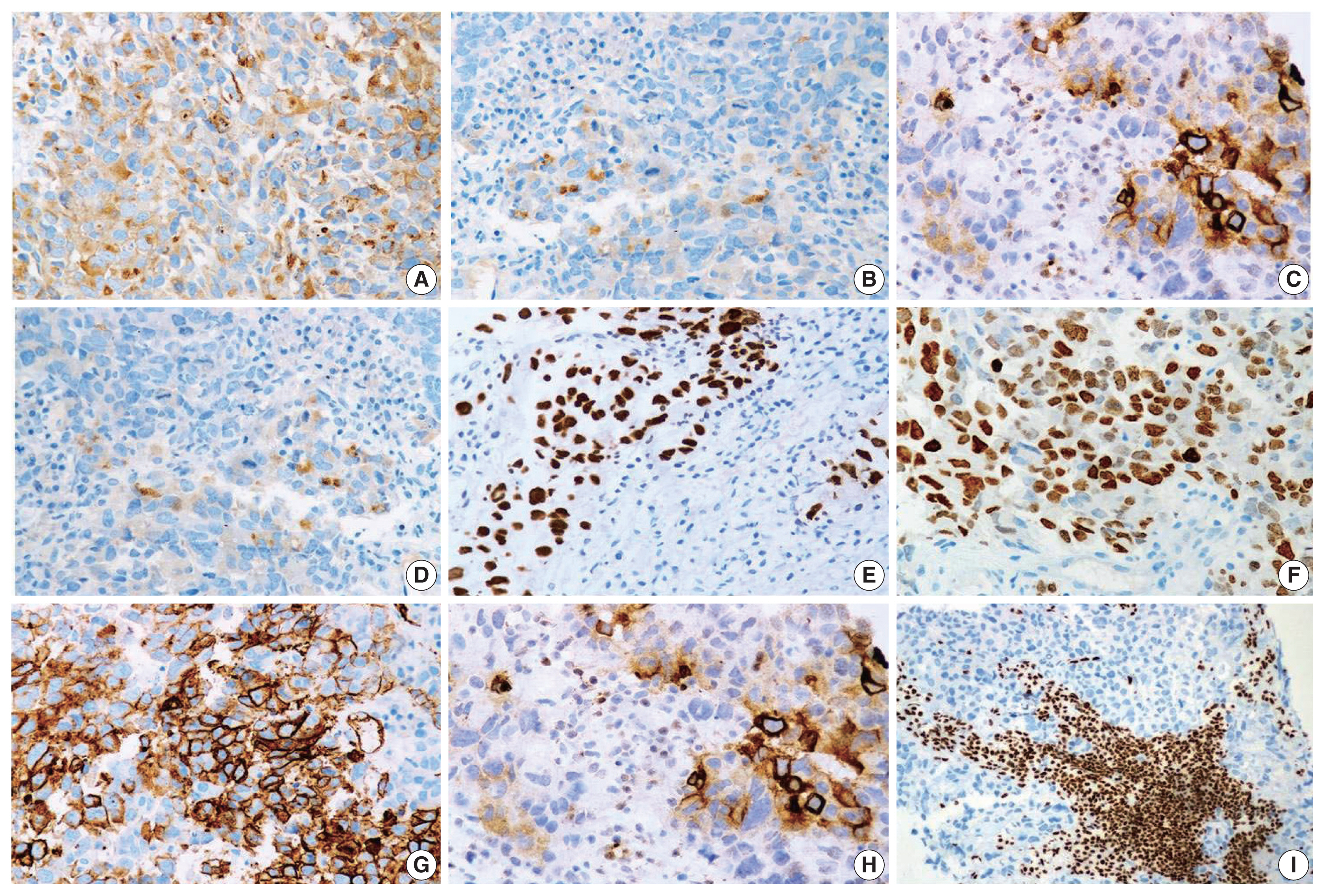
- Pathological findings in SD-TS
- The histopathologic characteristics of SD-TS are summarized in Table 2 (case Nos. 7–9) and shown in Fig. 3A–F. All three cases had a solid pattern of growth with pure rhabdoid morphology seen in two cases (case Nos. 7 and 9) (Fig. 3D–F). One case (case No. 8) had morphology similar to the features described in SD-LUAD (Fig. 3A–C). None of these cases showed areas of spindling, myxoid change, or any other feature that raised suspicion of sarcomatous histogenesis. Additional features noted in SD-LUAD such as inflamed stroma, neutrophilic emperipolesis, necrosis, brisk mitoses, and apoptosis were seen in these tumors (Table 2, Fig. 3D, E). On IHC, all cases had weak focal positivity for CK (Fig. 4A); two cases exhibited focal expression of CK7 (case Nos. 7 and 8) (Fig. 4B, C), and one case (case No. 9) showed weak focal expression for EMA. Hep Par 1 (Fig. 4D) and synaptophysin (Fig. 4H) were focally expressed in case No. 7, and p40 was focally expressed in case No. 8. Case Nos. 7 and 8 showed diffuse positivity for stem cell markers SALL4, SOX2, and CD34 (Fig. 4E–G) along with BRG1 loss (Fig. 4I), while case No. 9 had focal CD34 positivity in combination with BRG1 loss. SMARCB1/INI1 was intact in all cases. Table 3 and Fig. 4 show the IHC of SD-TS.
- Molecular analysis
- On molecular analysis, no actionable mutation in EGFR, ALK-1, or ROS1 gene was identified in SD-TT (Table 3). The targeted panel for biomarker detection in case No. 1 showed a copy number gain of c-MYC gene to 7.46 against the normal ploidy of 2, which was confirmed by FISH (copy number gain of 8.2 signals per cell). Significant PD-L1 (≥ 1%) expression was seen in two cases (case Nos. 4 and 6) (Table 3).
- Clinical outcome
- Follow-up information was available for all cases of SD-LUAD (Table 1). Three cases of SD-LUAD (case Nos. 1, 2, and 5) were on supportive care and died within two weeks of diagnosis. One case (case No. 4), which was reclassified as SD-LUAD and had received multiple lines of chemotherapy, died 23 months after initial diagnosis and within one month of repeat biopsy. All cases of SD-TS opted for further treatment in their respective cities and are alive, as learned telephonically. The duration of observation in this subgroup was 3–4 months, but the status of objective response and nature of therapy are not known.
RESULTS
- Mammalian SWI/SNF chromatin remodeling is dependent on ATPase activity that resides in BRG1 or its ortholog brahma [1,3,4]. Two thoracic tumors are caused by somatic loss of heterozygosity resulting from biallelic loss of SMARCA4, namely SD-LUAD and SD-TS. The existing literature on these tumors has brought greater awareness about clinicopathologic characteristics, prognosis, and therapeutic consequences [10–17].
- In a recently published, large series on SD-TT, the majority of cases was male, chronic smokers, and ranged in age from 30–80 years (mean, 58 years). Most had large thoracic mass with bulky lymphadenopathy, and nearly all patients had stage IV disease with bone metastasis [17]. Seven of our nine cases of SD-TT were also male, middle aged to elderly, and chronic smokers. Similarly, all our SD-LUAD cases had significant lung mass and stage IV disease with bony metastasis. A surprising observation in our cohort was lack of bone metastasis in SD-TS, whereas all cases of SD-LUAD had extensive bone involvement. This observation contradicts the dedifferentiation hypothesis [14,16] for emergence of SD-TS from SD-LUAD, though weak expression of epithelial markers in SD-TS and stem cell markers in SD-LUAD suggest the possibility of transition from SD-LUAD to SD-TS.
- Morphological patterns of SD-LUAD have been recognized, from less common, well-differentiated to more common, poorly-differentiated malignant tumors [11]. All our cases had a predominant solid growth pattern with scattered clear to signet ring cells and inflamed stroma, similar to the findings seen in other studies [11,12]. Scattered cells with intracytoplasmic mucin were noted in four of six cases. This observation replicates the findings of Agaimy et al. [11]. Two cases with trabecular pattern of TTF1 negativity and Hep Par 1 expression, could easily be misinterpreted as hepatoid adenocarcinomas or hepatocellular carcinomas without BRG1 testing. We contend that all cases of malignancy of unknown origin (MUO) with hepatoid immunophenotype be tested for lack of BRG1 expression to correctly diagnose SD-TT. However, the aberrant expression of Hep Par 1 has not been explained well in the existing literature and is possibly a result of extensive chromatin remodeling associated with SMARCA4 loss. SD-LUAD tumors were negative for p40, TTF1, Napsin A, neuroendocrine markers, and CK5/6 but expressed CK7 in four of the six cases and Hep Par 1 and EMA in all cases, which was in line with observation from other studies [10–12]. Two cases of SD-LUAD (case Nos. 3 and 5) with scattered rhabdoid cells, despite showing diffuse positivity for CK, were negative for CK7 and had weak and focal Hep Par 1 expression and weak SOX2 and CD34, which placed them between SD-LUAD and SD-TS. These cases represent a possible transition toward SD-TS and support the concept of a biologic continuum between these tumors [17,19]. Notably, CK and EMA expression levels were strong in these two cases, unlike the other SD-TS, allowing us to categorize them as SD-LUAD.
- The prevailing literature remains controversial as to whether SD-TS represent a distinct entity and, if so, whether there is an evolutionary relation between SD-LUAD and SD-TS [14,16,17]. There are no unambiguous clinico-radiological or histopathological findings to differentiate between them [10–17]. Perret et al. [14] proposed criteria for SD-TS of 1) rhabdoid or poorly differentiated phenotype; (2) complete loss of expression of SMARCA4 and SMARCA2; and (3) focal or diffuse expression of at least two of the following markers: SOX2, CD34, or SALL4.
- SD-TS patients in our case series had dominance of rhabdoid tumor cells, but the overall morphology was indistinguishable from that of SD-LUAD. No spindle cell cytology, myxoid alterations, or a known growth pattern exclusive to sarcomatous histogenesis was observed. Separation from the latter was achieved solely by immunophenotyping, which revealed diffuse and strong staining for stem cell markers CD34, SOX2, and SALL4 and focal staining for keratin and Hep Par 1 in SD-TS in two of the three cases. Also, these two cases had no expression of EMA. The third case had undifferentiated round cell to rhabdoid morphology with BRG1 loss but focal staining for CD34 and CK and weak, focal staining for EMA. In such cases, other tumors like epithelioid mesotheliomas, which can show BRG1 loss, must be excluded by clinico-radiological features and negativity for other mesothelial markers (CK5/6, calretinin, and WT1) [14]. Further, complete absence or weak focal presence of EMA with focal positivity for CK helps to exclude sarcomatoid/undifferentiated carcinomas.
- Predictive biomarker testing for sensitizing EGFR mutation and ALK-1 and ROS1 rearrangement was negative in all SD-TT cases in this cohort. Case No. 1, which was tested by massively parallel sequencing for broad predictive biomarkers, showed copy number gain for c-MYC but none of the actionable genetic alterations. Lack of currently druggable genetic alterations is the hallmark of SD-LUAD. This finding in our series is a reiteration of similar findings in previous studies [19,21]. This confirms the futility of expensive biomarker testing in this subset of lung adenocarcinoma and highlights the need to filter such cases upfront to avoid wasting effort and resources. Furthermore, for these tumors with a different biology and an aggressive course with no actionable drivers yet, a better understanding of their mechanistic nuances with new and efficacious therapeutic options are needed [22], some of which such as EZH2 inhibitors [23] and immune check point inhibitors [24,25] have started emerging. To fulfill the referred objective of differentiating SD-TT from NSCC-NOS, we followed a simple tissue proficient diagnostic schema as shown in Fig. 5.
- There are certain limitations in the present study. First, the number of cases studied is small. Second, the study only confirmed that BRG1 loss is confined to TTF1-negative NSCLC based on small tissue microarray and might not agree with all existing literature [10]. Third, no confirmatory molecular testing targeting SMARCA4 gene mutation was performed. Fourth, the diagnostic pathway requires extensive use of IHC to separate SD-TT into SD-LUAD and SD-TS once BRG1 loss is established. However, such extension of IHC is acceptable in the BRG1-deficient subset that lacks actionable biomarkers and omits biomarker testing without therapeutic impact.
- To conclude, SD-LUAD and SD-TS are difficult to differentiate from each other and from other NSCLC based on morphology alone. They are likely to be reported as NSCC-NOS with immunonegativity to p40 and TTF1, necessitating biomarker testing with a waste of time and resources. We argue that the diagnostic pathway presented here can help to diagnose such cases so that they can be studied more effectively for new biomarkers and therapeutic techniques. Overall, this study highlights the need and method of delineating SD-TT in reporting of small biopsy for NSCLC and shares a useable workflow to clarify tumor type. Finally, awareness of this entity can help prevent misdiagnosis of MUO as hepatic or hepatoid carcinomas with consequent negative effects.
DISCUSSION
Ethics Statement
All procedures performed in the current study were approved by Institutional Review Board (vide letter no: RGCIRC/IRB-BHR/33/2021 dated 6th January 2021) in accordance with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Author Contributions
Conceptualization: AM. Data curation: DB, RT. Formal analysis: AM, DB. Investigation: AM, DB, AJ. Methodology: AM, DB. Resources: RT, AJ. Supervision: AM. Visualization: AM, DB. Writing—original draft: DB, AM, RT. Writing—review & editing: AM, DB. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
No funding to declare.

- 1. Oike T, Ogiwara H, Nakano T, Yokota J, Kohno T. Inactivating mutations in SWI/SNF chromatin remodeling genes in human cancer. Jpn J Clin Oncol 2013; 43: 849-55. ArticlePubMed
- 2. Shain AH, Pollack JR. The spectrum of SWI/SNF mutations, ubiquitous in human cancers. PLoS One 2013; 8: e55119.ArticlePubMedPMC
- 3. Wang X, Haswell JR, Roberts CW. Molecular pathways: SWI/SNF (BAF) complexes are frequently mutated in cancer: mechanisms and potential therapeutic insights. Clin Cancer Res 2014; 20: 21-7. ArticlePubMedPDF
- 4. Ganguly D, Sims M, Cai C, Fan M, Pfeffer LM. Chromatin remodeling factor BRG1 regulates stemness and chemosensitivity of glioma initiating cells. Stem Cells 2018; 36: 1804-15. ArticlePubMedPMCPDF
- 5. Agaimy A. The expanding family of SMARCB1(INI1)-deficient neoplasia: implications of phenotypic, biological, and molecular heterogeneity. Adv Anat Pathol 2014; 21: 394-410. PubMed
- 6. Jelinic P, Mueller JJ, Olvera N, et al. Recurrent SMARCA4 mutations in small cell carcinoma of the ovary. Nat Genet 2014; 46: 424-6. ArticlePubMedPMCPDF
- 7. Stewart CJ, Crook ML. SWI/SNF complex deficiency and mismatch repair protein expression in undifferentiated and dedifferentiated endometrial carcinoma. Pathology 2015; 47: 439-45. ArticlePubMed
- 8. Agaimy A, Daum O, Markl B, Lichtmannegger I, Michal M, Hartmann A. SWI/SNF Complex-deficient undifferentiated/rhabdoid carcinomas of the gastrointestinal tract: a series of 13 cases highlighting mutually exclusive loss of SMARCA4 and SMARCA2 and frequent co-inactivation of SMARCB1 and SMARCA2. Am J Surg Pathol 2016; 40: 544-53. PubMed
- 9. AACR Project GENIE Consortium. AACR Project GENIE: powering precision medicine through an international consortium. Cancer Discov 2017; 7: 818-31. PubMedPMC
- 10. Herpel E, Rieker RJ, Dienemann H, et al. SMARCA4 and SMARCA2 deficiency in non-small cell lung cancer: immunohistochemical survey of 316 consecutive specimens. Ann Diagn Pathol 2017; 26: 47-51. ArticlePubMed
- 11. Agaimy A, Fuchs F, Moskalev EA, Sirbu H, Hartmann A, Haller F. SMARCA4-deficient pulmonary adenocarcinoma: clinicopathological, immunohistochemical, and molecular characteristics of a novel aggressive neoplasm with a consistent TTF1(neg)/CK7(pos)/Hep-Par-1(pos) immunophenotype. Virchows Arch 2017; 471: 599-609. ArticlePubMedPDF
- 12. Nambirajan A, Singh V, Bhardwaj N, Mittal S, Kumar S, Jain D. SMARCA4/BRG1-deficient non-small cell lung carcinomas: a case series and review of the literature. Arch Pathol Lab Med 2021; 145: 90-8. ArticlePubMedPDF
- 13. Le Loarer F, Watson S, Pierron G, et al. SMARCA4 inactivation defines a group of undifferentiated thoracic malignancies transcriptionally related to BAF-deficient sarcomas. Nat Genet 2015; 47: 1200-5. ArticlePubMedPDF
- 14. Perret R, Chalabreysse L, Watson S, et al. SMARCA4-deficient thoracic sarcomas: clinicopathologic study of 30 cses with an emphasis on their nosology and differential diagnoses. Am J Surg Pathol 2019; 43: 455-65. PubMed
- 15. Yoshida A, Kobayashi E, Kubo T, et al. Clinicopathological and molecular characterization of SMARCA4-deficient thoracic sarcomas with comparison to potentially related entities. Mod Pathol 2017; 30: 797-809. ArticlePubMedPDF
- 16. Sauter JL, Graham RP, Larsen BT, Jenkins SM, Roden AC, Boland JM. SMARCA4-deficient thoracic sarcoma: a distinctive clinicopathological entity with undifferentiated rhabdoid morphology and aggressive behavior. Mod Pathol 2017; 30: 1422-32. ArticlePubMedPDF
- 17. Rekhtman N, Montecalvo J, Chang JC, et al. SMARCA4-deficient thoracic sarcomatoid tumors represent primarily smoking-related undifferentiated carcinomas rather than primary thoracic sarcomas. J Thorac Oncol 2020; 15: 231-47. ArticlePubMed
- 18. Nicholsan AG, Geisinger K, Aisner SC, et al. Terminology and criteria in non-resection specimens. In: Travis WD, Brambilla E, Burke AP, Marx A, Nicholson AG, eds. WHO classification of tumors of the lung, pleura, thymus and heart. 4th ed.Lyon: IARC Press, 2015; 26-37.
- 19. Matsubara D, Kishaba Y, Ishikawa S, et al. Lung cancer with loss of BRG1/BRM, shows epithelial mesenchymal transition phenotype and distinct histologic and genetic features. Cancer Sci 2013; 104: 266-73. PubMedPMC
- 20. Mehta A, Saifi M, Batra U, Suryavanshi M, Gupta K. Incidence of ROS1-rearranged non-small-cell lung carcinoma in India and efficacy of crizotinib in lung adenocarcinoma patients. Lung Cancer (Auckl) 2020; 11: 19-25. PubMedPMC
- 21. Cancer Genome Atlas Research Network. Comprehensive molecular profiling of lung adenocarcinoma. Nature 2014; 511: 543-50. ArticlePubMedPMCPDF
- 22. Bell EH, Chakraborty AR, Mo X, et al. SMARCA4/BRG1 is a novel prognostic biomarker predictive of cisplatin-based chemotherapy outcomes in resected non-small cell lung cancer. Clin Cancer Res 2016; 22: 2396-404. ArticlePubMedPDF
- 23. Chan-Penebre E, Armstrong K, Drew A, et al. Selective killing of SMARCA2- and SMARCA4-deficient small cell carcinoma of the ovary, hypercalcemic type cells by inhibition of EZH2: in vitro and in vivo preclinical models. Mol Cancer Ther 2017; 16: 850-60. ArticlePubMedPDF
- 24. Naito T, Udagawa H, Umemura S, et al. Non-small cell lung cancer with loss of expression of the SWI/SNF complex is associated with aggressive clinicopathological features, PD-L1-positive status, and high tumor mutation burden. Lung Cancer 2019; 138: 35-42. ArticlePubMed
- 25. Takada K, Sugita S, Murase K, et al. Exceptionally rapid response to pembrolizumab in a SMARCA4-deficient thoracic sarcoma over-expressing PD-L1: a case report. Thorac Cancer 2019; 10: 2312-5. ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations

- Unravelling switch/sucrose non-fermentable (SWI-SNF) complex-deficient thoracic tumours: a clinicopathological comparative on undifferentiated tumours and non-small cell lung carcinomas with BRG1 and BRM deficiency
Ridhi Sood, Arshi Tandon, Warisa Khatoon, Jayashimman Vasanthraman, Aruna Nambirajan, Anant Mohan, Prabhat Singh Malik, Deepali Jain
Journal of Clinical Pathology.2025; 78(6): 370. CrossRef - Clinicopathologic and genomic analyses of SMARCA4-mutated non-small cell lung carcinoma implicate the needs for tailored treatment strategies
Bokyung Ahn, Deokhoon Kim, Wonjun Ji, Sung-Min Chun, Goeun Lee, Se Jin Jang, Hee Sang Hwang
Lung Cancer.2025; 201: 108445. CrossRef - SMARCA4-deficient non-small cell lung cancer with metastasis to the sigmoid colon: a case report
Rong Xiao, Guang Fu, Xinglan Li, Tao Lu
World Journal of Surgical Oncology.2025;[Epub] CrossRef - Case report: The first account of undifferentiated sarcoma with epithelioid features originating in the pleura
Ling-Xi Xiao, Li Liu, Wang Deng
Frontiers in Medicine.2024;[Epub] CrossRef - SMARCA4-deficient central nervous system metastases: A case series and systematic review
Meaghan Morris, Kerime Ararat, Hannah Cutshall, Murat Gokden, Analiz Rodriguez, Lisa Rooper, Matthew Lindberg, James Stephen Nix
Journal of Neuropathology & Experimental Neurology.2024; 83(8): 638. CrossRef - Chemotherapy and Immune Checkpoint Inhibitors in a Case of SMARCA4-dUT: A Case Report and Review of Literature
Akriti Pokhrel, Ruchi Yadav, Kapil Kumar Manvar, Richard Wu, Vijay Jaswani, Carrie Brooke Wasserman, Jen C. Wang
Journal of Investigative Medicine High Impact Case Reports.2023;[Epub] CrossRef - TTF1-positive SMARCA4/BRG1 deficient lung adenocarcinoma
Anurag Mehta, Himanshi Diwan, Divya Bansal, Manoj Gupta
Journal of Pathology and Translational Medicine.2022; 56(1): 53. CrossRef - Delineation of a SMARCA4-specific competing endogenous RNA network and its function in hepatocellular carcinoma
Lei Zhang, Ting Sun, Xiao-Ye Wu, Fa-Ming Fei, Zhen-Zhen Gao
World Journal of Clinical Cases.2022; 10(29): 10501. CrossRef - Artificial intelligence platform, RADR®, aids in the discovery of DNA damaging agent for the ultra-rare cancer Atypical Teratoid Rhabdoid Tumors
Joseph McDermott, Drew Sturtevant, Umesh Kathad, Sudhir Varma, Jianli Zhou, Aditya Kulkarni, Neha Biyani, Caleb Schimke, William C. Reinhold, Fathi Elloumi, Peter Carr, Yves Pommier, Kishor Bhatia
Frontiers in Drug Discovery.2022;[Epub] CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
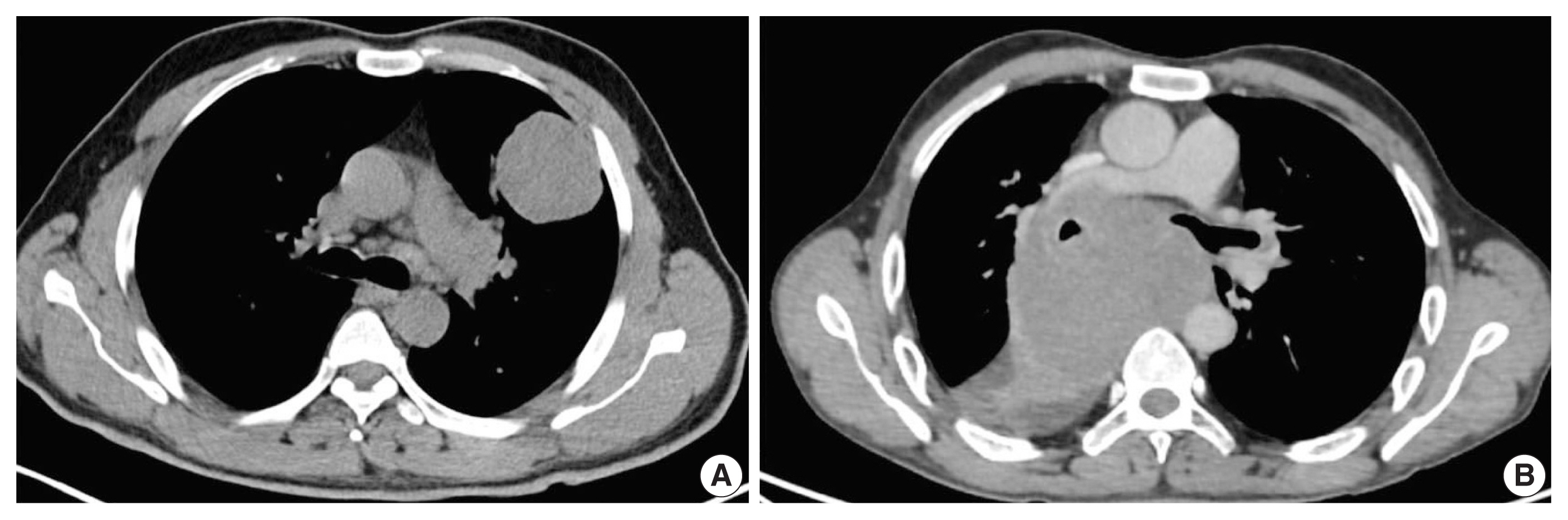

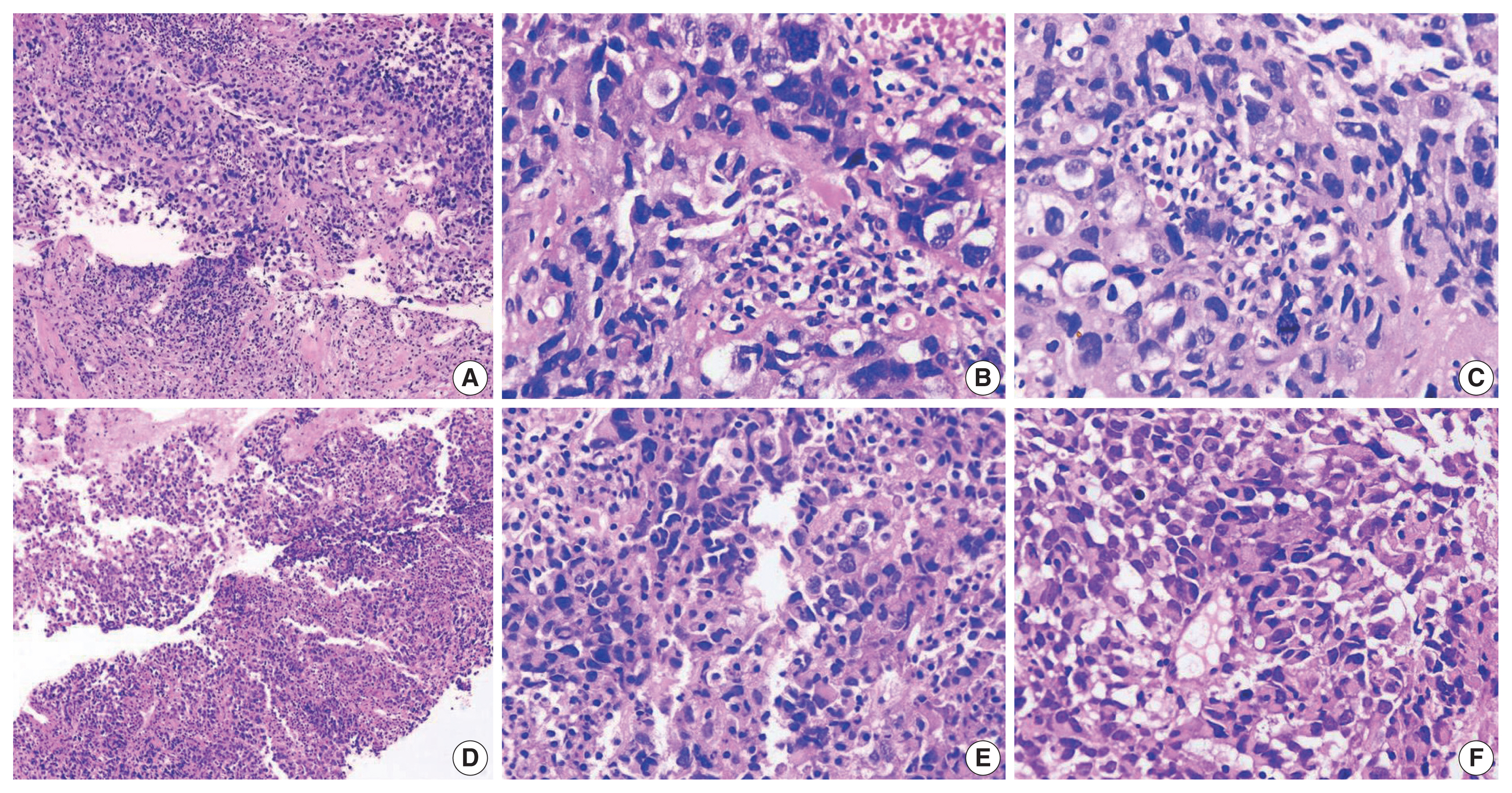
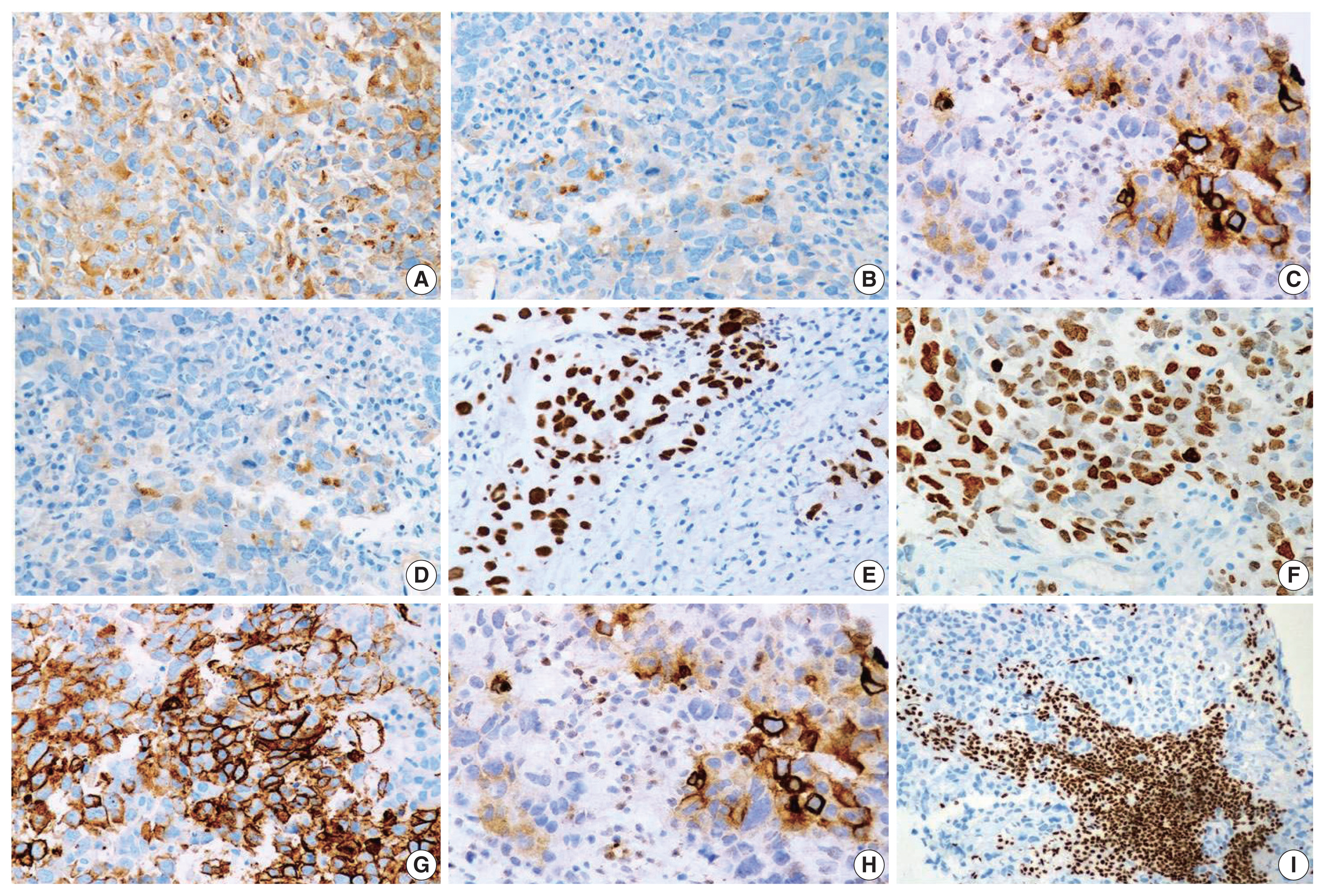
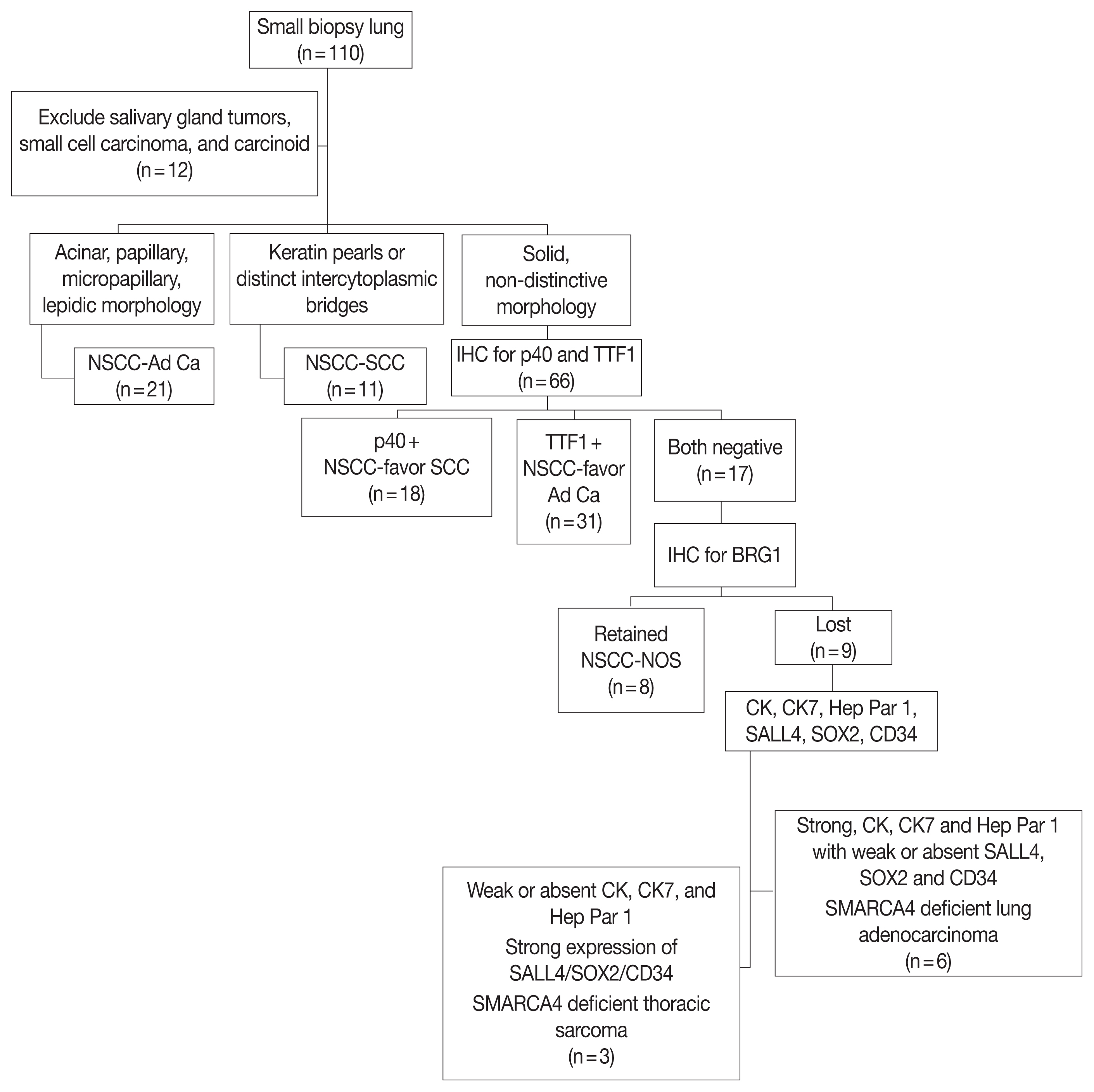
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
| Case No. | Age/Sex | Smoking | Biopsy site | Metastasis | TNM stage | Radiological findings | Treatment | Present status |
|---|---|---|---|---|---|---|---|---|
| 1 | 67/M | Present | Cervical lymph node | Present | IV | Bilateral lung nodules, mediastinal and cervical lymph nodes, skeletal and adrenal metastasis | Supportive care | Died, 7 days |
| 2 | 47/M | Present | Pleura | Present | IV | Pleura based mass, supraclavicular LAP, rib and vertebral body | Supportive care | Died, 15 days |
| 3 | 65/F | Present | Left upper lobe lung | Present | IV | Left lung mass, pleural effusion, mediastinal LAP, multiple bones | 1st cycle of platinum doublet | Alive |
| 4 | 45/M | Present | Left upper lobe lung (second biopsy after treatment failure) | Present | IV | Centrally non-enhancing lung mass (necrotic), mediastinal LAP, vertebral body | Multiple lines of chemotherapy | Died a month after 2nd biopsy (OS, 23 mo) |
| 5 | 73/F | Present | Right iliac blade | Present | IV | Left lung mass, mediastinal LAP, multiple bone, brain and liver metastasis | Supportive care | Died, 15 days |
| 6 | 66/M | Present | Left scapular soft tissue deposit | Present | IV | Right lung mass, mediastinal and cervical LAP, skeletal, adrenal | 1st cycle of Platinum doublet | Alive |
| 7 | 49/M | Present | Left upper lobe lung | Absent | IIIC | Left lung mass, mediastinal LAP, supraclavicular LN | Platinum doublet at another centre | Alive |
| 8 | 46/M | Present | Right parahilar region | Present | IV | Right mediastinal mass, pleural effusion and mediastinal LAP | Platinum doublet at another centre | Alive |
| 9 | 60/M | Present | Right supraclavicular LN | Absent | IIIC | Right lung mass mediastinal LAP, supraclavicular LN | Platinum doublet at another centre | Alive |
| Case No. | Architectural pattern | Cell type | Cytoplasm | Nuclear features | Stroma | Emperipolesis | Necrosis | Mitoses (/10 hpf) |
|---|---|---|---|---|---|---|---|---|
| 1 | Diffuse with sieve like appearance | Large polygonal with scattered clear cells | Eosinophilic with mucin | Cloudy chromatin | Inflamed | Present | Present, extensive | 24 |
| 2 | Indian file pattern mimicking lobular carcinoma breast with few nests and tubules | Large polygonal with scattered clear cells | Eosinophilic with mucin | Fragile looking chromatin with indented nuclei | Desmoplasia with moderate inflammation | Absent | Focal | 12 |
| 3 | Solid | Large polygonal with scattered clear cells scattered rhabdoid cells | Eosinophilic with globular inclusions | Indented nuclei, and prominent eosinophilic nucleoli | Inflamed | Absent | Present | > 50 |
| 4 | Solid, trabecular | Large polygonal with scattered clear cells | Eosinophilic with mucin | Cloudy chromatin | Inflamed | Present | Present, extensive | 30 |
| 5 | Solid | Large polygonal with scattered clear cells, scattered rhabdoid cells | Eosinophilic with globular inclusions | Fragile looking chromatin with indented nuclei | Inflamed | Present | Present, extensive | 30 |
| 6 | Solid, trabecular | Large polygonal with scattered clear cells | Eosinophilic with mucin | Cloudy chromatin | Desmoplasia with mild inflammation | Absent | Focal | 15 |
| 7 | Solid | Pure rhabdoid | Globular inclusions | Cloudy chromatin | Markedly inflamed | Present | Absent | 30 |
| 8 | Solid | Large polygonal with scattered clear cells | Eosinophilic with globular inclusions | Fragile looking chromatin with indented nuclei | Inflamed | Absent | Present, extensive | > 50 |
| 9 | Solid | Pure rhabdoid | Globular inclusions | Cloudy chromatin | Inflamed | Absent | Present, extensive | > 50 |
| Case No. | CK | CK7 | EMA | TTF1 | Hep Par 1 | SALL4 | SOX2 | CD34 | p40 | BRG1 | Status of predictive biomarker (EGFR, ALK-1, ROS1) | PD-L1 membranous expression (% positivity in tumor cells and intensity) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Pos | Pos | Pos | Neg | Pos | Neg | Neg | Neg | Neg | Loss | Negative c-MYC-copy number gain 7.46 |
< 1 |
| 2 | Pos | Pos | Pos | Neg | Pos | Neg | Neg | Neg | Neg | Loss | Negative | < 1 |
| 3 | Pos | Neg | Focal Pos | Neg | Pos | Neg | Pos | Focal Pos | Neg | Loss | Negative | < 1 |
| 4 | Pos | Pos | Pos | Neg | Pos | Neg | Neg | Neg | Neg | Loss | Negative | 60 |
| 5 | Pos | Neg | Focal Pos | Neg | Pos | Neg | Focal Pos | Pos | Neg | Loss | Negative | < 1 |
| 6 | Pos | Pos | Pos | Neg | Pos | Neg | Neg | Neg | Neg | Loss | Negative | 70 |
| 7 | Weak, focal Pos | Weak, focal Pos | Neg | Neg | Focal Pos | Pos | Pos | Pos | Neg | Loss | Negative | < 1 |
| 8 | Weak, focal Pos | Strong, focal Pos | Neg | Neg | Neg | Pos | Pos | Pos | Focal Pos | Loss | Negative | < 1 |
| 9 | Weak, focal Pos | Neg | Weak, focal Pos | Neg | Neg | Neg | Neg | Focal Pos | Neg | Loss | Negative | < 1 |
M, male; LAP, lymphadenopathy; F, female; OS, overall survival; LN, lymph node.
hpf, high-power field.
CK, cytokeratin; EMA, epithelial membrane antigen; TTF1, transcription termination factor 1; EGFR, epidermal growth factor receptor; ALK-1, anaplastic lymphoma kinase 1; PD-L1, programmed death–ligand 1; Pos, positive; Neg, negative.

 E-submission
E-submission