Search
- Page Path
- HOME > Search
- Comparison of tissue-based and plasma-based testing for EGFR mutation in non–small cell lung cancer patients
- Yoon Kyung Kang, Dong Hoon Shin, Joon Young Park, Chung Su Hwang, Hyun Jung Lee, Jung Hee Lee, Jee Yeon Kim, JooYoung Na
- J Pathol Transl Med. 2025;59(1):60-67. Published online January 15, 2025
- DOI: https://doi.org/10.4132/jptm.2024.10.01
- 4,727 View
- 198 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Epidermal growth factor receptor (EGFR) gene mutation testing is crucial for the administration of tyrosine kinase inhibitors to treat non–small cell lung cancer. In addition to traditional tissue-based tests, liquid biopsies using plasma are increasingly utilized, particularly for detecting T790M mutations. This study compared tissue- and plasma-based EGFR testing methods.
Methods
A total of 248 patients were tested for EGFR mutations using tissue and plasma samples from 2018 to 2023 at Pusan National University Yangsan Hospital. Tissue tests were performed using PANAmutyper, and plasma tests were performed using the Cobas EGFR Mutation Test v2.
Results
All 248 patients underwent tissue-based EGFR testing, and 245 (98.8%) showed positive results. Of the 408 plasma tests, 237 (58.1%) were positive. For the T790M mutation, tissue biopsies were performed 87 times in 69 patients, and 30 positive cases (38.6%) were detected. Plasma testing for the T790M mutation was conducted 333 times in 207 patients, yielding 62 positive results (18.6%). Of these, 57 (27.5%) were confirmed to have the mutation via plasma testing. Combined tissue and plasma tests for the T790M mutation were positive in nine patients (13.4%), while 17 (25.4%) were positive in tissue only and 12 (17.9%) in plasma only. This mutation was not detected in 28 patients (43.3%).
Conclusions
Although the tissue- and plasma-based tests showed a sensitivity of 37.3% and 32.8%, respectively, combined testing increased the detection rate to 56.7%. Thus, neither test demonstrated superiority, rather, they were complementary.
- Landscape of EGFR mutations in lung adenocarcinoma: a single institute experience with comparison of PANAMutyper testing and targeted next-generation sequencing
- Jeonghyo Lee, Yeon Bi Han, Hyun Jung Kwon, Song Kook Lee, Hyojin Kim, Jin-Haeng Chung
- J Pathol Transl Med. 2022;56(5):249-259. Published online September 13, 2022
- DOI: https://doi.org/10.4132/jptm.2022.06.11
- 8,754 View
- 144 Download
- 7 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Activating mutations in the tyrosine kinase domain of epidermal growth factor receptor (EGFR) are predictive biomarkers for response to EGFR–tyrosine kinase inhibitor (TKI) therapy in lung adenocarcinoma (LUAD). Here, we characterized the clinicopathologic features associated with EGFR mutations via peptide nucleic acid clamping-assisted fluorescence melting curve analysis (PANAMutyper) and evaluated the feasibility of targeted deep sequencing for detecting the mutations.
Methods
We examined EGFR mutations in exons 18 through 21 for 2,088 LUADs from July 2017 to April 2020 using PANAMutyper. Of these, we performed targeted deep sequencing in 73 patients and evaluated EGFR-mutation status and TKI clinical response.
Results
EGFR mutation was identified in 55.7% of LUADs by PANAMutyper, with mutation rates higher in females (69.3%) and never smokers (67.1%) and highest in the age range of 50 to 59 years (64.9%). For the 73 patients evaluated using both methods, next-generation sequencing (NGS) identified EGFR mutation–positive results in 14 of 61 patients (23.0%) who were EGFR-negative according to PANAMutyper testing. Of the 10 patients reportedly harboring a sensitizing mutation according to NGS, seven received TKI treatment, with all showing partial response or stable disease. In the 12 PANAMutyper-positive cases, NGS identified two additional mutations in exon 18, whereas a discordant negative result was observed in two cases.
Conclusions
Although PANAMutyper identified high frequencies of EGFR mutations, targeted deep sequencing revealed additional uncommon EGFR mutations. These findings suggested that appropriate use of NGS may benefit LUAD patients with otherwise negative screening test results. -
Citations
Citations to this article as recorded by- Comparison of tissue-based and plasma-based testing for EGFR mutation in non–small cell lung cancer patients
Yoon Kyung Kang, Dong Hoon Shin, Joon Young Park, Chung Su Hwang, Hyun Jung Lee, Jung Hee Lee, Jee Yeon Kim, JooYoung Na
Journal of Pathology and Translational Medicine.2025; 59(1): 60. CrossRef - Localization of epidermal growth factor receptor-mutations using PNA:DNA probes in clinical specimens from patients with non-small cell lung cancer
Haruo Miyata, Hajime Shigeto, Tomoatsu Ikeya, Tadashi Ashizawa, Akira Iizuka, Yasufumi Kikuchi, Chie Maeda, Akari Kanematsu, Kazue Yamashita, Kenichi Urakami, Yuji Shimoda, Takeshi Nagashima, Keiichi Ohshima, Yasuhisa Ohde, Mitsuhiro Isaka, Takashi Sugino
Scientific Reports.2025;[Epub] CrossRef - Molecular characteristics and responses to EGFR tyrosine kinase inhibitors in non-small cell lung cancer patients with EGFR exon 19 insertions
Yang Li, Yunfeng Ni, Feng Lv, Yan Shi, Yedan Chen, Xiaoying Wu, Jiaohui Pang, Long Huang, Yang Shao, Tao Wang, Jie Min, Yang Song
BMC Medicine.2025;[Epub] CrossRef - Detection of EGFR exon 20 insertion mutations in non-small cell lung cancer: implications for consistent nomenclature in precision medicine
Jieun Park, Boram Lee, Ji-Young Song, Minjung Sung, Mi Jeong Kwon, Chae Rin Kim, Sangjin Lee, Young Kee Shin, Yoon-La Choi
Pathology.2024; 56(5): 653. CrossRef - Histo-pillar strip for optimal histogel block construction and biomarker analysis in 3D-lung cancer patient-derived organoids
Sang-Yun Lee, Eunyoung Lee, Ji-O Ryu, Kyuhwan Kim, Yongki Hwang, Bosung Ku, Seok Whan Moon, Mi Hyoung Moon, Kyung Soo Kim, Kwanyong Hyun, Jeong Uk Lim, Chan Kwon Park, Sung Won Kim, Chang Dong Yeo, Dong Woo Lee, Seung Joon Kim
Biofabrication.2024; 16(4): 045017. CrossRef
- Comparison of tissue-based and plasma-based testing for EGFR mutation in non–small cell lung cancer patients
- A case of concomitant EGFR/ALK alteration against a mutated EGFR background in early-stage lung adenocarcinoma
- Ki-Chang Lee, Jiwon Koh, Doo Hyun Chung, Yoon Kyung Jeon
- J Pathol Transl Med. 2021;55(2):139-144. Published online January 22, 2021
- DOI: https://doi.org/10.4132/jptm.2020.12.16
- 5,223 View
- 111 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Rare cases of lung adenocarcinoma (LUAD) with concomitant epidermal growth factor receptor (EGFR) mutation and anaplastic lymphoma kinase (ALK) translocation have been reported. However, their clonal and evolutional relationship remains unclear. We report a case of early-stage EGFR-mutated LUAD with a focal concomitant EGFR/ALK alteration. A 63-year-old male underwent lobectomy to remove a 1.9-cm-sized lung nodule, which was diagnosed with EGFR-mutated LUAD. ALK immunohistochemistry (IHC) showed focal positivity within the part of the tumor characterized by lepidic pattern, also confirmed by fluorescence in-situ hybridization (FISH). Targeted next-generation sequencing was performed separately on the ALK IHC/FISH-positive and -negative areas. EGFR L833V/L858R mutations were detected in both areas, whereas EML4 (echinoderm microtubule-associated protein-like 4)-ALK translocations was confirmed only in the ALK IHC/FISH-positive area, suggesting the divergence of an EGFR/ALK co-altered subclone from the original EGFR-mutant clone. Our study suggests that concurrent alterations of EGFR and ALK can arise via divergent tumor evolution, even in the relatively early phases of tumorigenesis.
-
Citations
Citations to this article as recorded by- Machine learning-based characterization of a PANoptosis-associated model for enhancing prognosis and immunotherapy response in lung adenocarcinoma patients
Ziqiao Fu, Jia Zeng, Xiaomin Xiong, Weimin Zhong
Discover Oncology.2025;[Epub] CrossRef - Identification and validation of molecular subtype and prognostic signature for lung adenocarcinoma based on neutrophil extracellular traps
Yanhua Zuo, Guangyi Leng, Ping Leng
Pathology and Oncology Research.2023;[Epub] CrossRef - Machine Learning-Based Integration Develops a Macrophage-Related Index for Predicting Prognosis and Immunotherapy Response in Lung Adenocarcinoma
Zuwei Li, Minzhang Guo, Wanli Lin, Peiyuan Huang
Archives of Medical Research.2023; 54(7): 102897. CrossRef - Big data analysis identified a telomere-related signature predicting the prognosis and drug sensitivity in lung adenocarcinoma
Weiyi Zhang
Medicine.2023; 102(46): e35526. CrossRef
- Machine learning-based characterization of a PANoptosis-associated model for enhancing prognosis and immunotherapy response in lung adenocarcinoma patients
- Current status and future perspectives of liquid biopsy in non-small cell lung cancer
- Sunhee Chang, Jae Young Hur, Yoon-La Choi, Chang Hun Lee, Wan Seop Kim
- J Pathol Transl Med. 2020;54(3):204-212. Published online April 15, 2020
- DOI: https://doi.org/10.4132/jptm.2020.02.27
- 11,349 View
- 296 Download
- 20 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF - With advances in target therapy, molecular analysis of tumors is routinely required for treatment decisions in patients with advanced non-small cell lung cancer (NSCLC). Liquid biopsy refers to the sampling and analysis of circulating cell-free tumor DNA (ctDNA) in various body fluids, primarily blood. Because the technique is minimally invasive, liquid biopsies are the future in cancer management. Epidermal growth factor receptor (EGFR) ctDNA tests have been performed in routine clinical practice in advanced NSCLC patients to guide tyrosine kinase inhibitor treatment. In the near future, liquid biopsy will be a crucial prognostic, predictive, and diagnostic method in NSCLC. Here we present the current status and future perspectives of liquid biopsy in NSCLC.
-
Citations
Citations to this article as recorded by- Comparison of tissue-based and plasma-based testing for EGFR mutation in non–small cell lung cancer patients
Yoon Kyung Kang, Dong Hoon Shin, Joon Young Park, Chung Su Hwang, Hyun Jung Lee, Jung Hee Lee, Jee Yeon Kim, JooYoung Na
Journal of Pathology and Translational Medicine.2025; 59(1): 60. CrossRef - Lab-in-a-Fiber detection and capture of cells
João C. Varela, Achar V. Harish, Pawel Maniewski, Timothy Gibbon, Oana Tudoran, Rainer Heuchel, Matthias Löhr, Walter Margulis, Aman Russom, Fredrik Laurell
Scientific Reports.2025;[Epub] CrossRef - Lung Cancer Diagnosis and Prognostic Monitoring Through Cell-Free RNA via Liquid Biopsy
Yuanming Pan, Chongbo Jiang, Mengchan Ye, Dongmei Li, Jinghui Wang
Therapeutics and Clinical Risk Management.2025; Volume 21: 1615. CrossRef - Unlocking the future of cancer diagnosis – promises and challenges of ctDNA-based liquid biopsies in non-small cell lung cancer
Chiara Reina, Berina Šabanović, Chiara Lazzari, Vanesa Gregorc, Christopher Heeschen
Translational Research.2024; 272: 41. CrossRef - Tailored point-of-care biosensors for liquid biopsy in the field of oncology
Sima Singh, Pritam Saha Podder, Matt Russo, Charles Henry, Stefano Cinti
Lab on a Chip.2023; 23(1): 44. CrossRef - Emerging role of non-invasive and liquid biopsy biomarkers in pancreatic cancer
Akash Bararia, Prosenjeet Chakraborty, Paromita Roy, Bitan Kumar Chattopadhay, Amlan Das, Aniruddha Chatterjee, Nilabja Sikdar
World Journal of Gastroenterology.2023; 29(15): 2241. CrossRef - Liquid biopsy in the management of advanced lung cancer: Implementation and practical aspects
Gabriela Fernandes, Ana Rodrigues, Cláudia Matos, Fernando Barata, Luís Cirnes, Lurdes Ferreira, José Albino Lopes, Margarida Felizardo, Paula Fidalgo, Ulisses Brito, Bárbara Parente
Cancer Treatment and Research Communications.2023; 36: 100725. CrossRef - Tweezer PCR: A Highly Specific Method for Accurate Identification of Low-Abundance Mutations
Shanglin Li, Yin Gu, Zhi Geng, Kaiyi Li, Yawei Hu, Qiang Liu, Rongxin Fu, Peng Liu
Analytical Chemistry.2023; 95(48): 17679. CrossRef - Mesonephric-like Adenocarcinoma of the Ovary: Clinicopathological and Molecular Characteristics
Hyun Hee Koh, Eunhyang Park, Hyun-Soo Kim
Diagnostics.2022; 12(2): 326. CrossRef - Alveolar Soft Part Sarcoma of the Uterus: Clinicopathological and Molecular Characteristics
Yurimi Lee, Kiyong Na, Ha Young Woo, Hyun-Soo Kim
Diagnostics.2022; 12(5): 1102. CrossRef - Exosomal MicroRNA Analyses in Esophageal Squamous Cell Carcinoma Cell Lines
Sora Kim, Gwang Ha Kim, Su Jin Park, Chae Hwa Kwon, Hoseok I, Moon Won Lee, Bong Eun Lee
Journal of Clinical Medicine.2022; 11(15): 4426. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Update on molecular pathology and role of liquid biopsy in nonsmall cell lung cancer
Pamela Abdayem, David Planchard
European Respiratory Review.2021; 30(161): 200294. CrossRef - Dynamics of Specific cfDNA Fragments in the Plasma of Full Marathon Participants
Takehito Sugasawa, Shin-ichiro Fujita, Tomoaki Kuji, Noriyo Ishibashi, Kenshirou Tamai, Yasushi Kawakami, Kazuhiro Takekoshi
Genes.2021; 12(5): 676. CrossRef - Future Perspectives in Detecting EGFR and ALK Gene Alterations in Liquid Biopsies of Patients with NSCLC
Daniela Ferreira, Juliana Miranda, Paula Martins-Lopes, Filomena Adega, Raquel Chaves
International Journal of Molecular Sciences.2021; 22(8): 3815. CrossRef - Real-World Analysis of the EGFR Mutation Test in Tissue and Plasma Samples from Non-Small Cell Lung Cancer
Hyunwoo Lee, Joungho Han, Yoon-La Choi
Diagnostics.2021; 11(9): 1695. CrossRef - Objective Quantitation of EGFR Protein Levels using Quantitative Dot Blot Method for the Prognosis of Gastric Cancer Patients
Lei Xin, Fangrong Tang, Bo Song, Maozhou Yang, Jiandi Zhang
Journal of Gastric Cancer.2021; 21(4): 335. CrossRef - The Role of the Liquid Biopsy in Decision-Making for Patients with Non-Small Cell Lung Cancer
D. Akhoundova, J. Mosquera Martinez, L. E. Musmann, C. Britschgi, C. Rütsche, M. Rechsteiner, E. Nadal, M. R. Garcia Campelo, A. Curioni-Fontecedro
Journal of Clinical Medicine.2020; 9(11): 3674. CrossRef - Expanding opportunities in precision oncology
T Raja
Cancer Research, Statistics, and Treatment.2020; 3(4): 863. CrossRef
- Comparison of tissue-based and plasma-based testing for EGFR mutation in non–small cell lung cancer patients
- Clinicopathologic characteristics of HER2-positive pure mucinous carcinoma of the breast
- Yunjeong Jang, Hera Jung, Han-Na Kim, Youjeong Seo, Emad Alsharif, Seok Jin Nam, Seok Won Kim, Jeong Eon Lee, Yeon Hee Park, Eun Yoon Cho, Soo Youn Cho
- J Pathol Transl Med. 2020;54(1):95-102. Published online November 13, 2019
- DOI: https://doi.org/10.4132/jptm.2019.10.24
- 10,713 View
- 293 Download
- 22 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Pure mucinous carcinoma (PMC) is a rare type of breast cancer, estimated to represent 2% of invasive breast cancer. PMC is typically positive for estrogen receptors (ER) and progesterone receptors (PR) and negative for human epidermal growth factor receptor 2 (HER2). The clinicopathologic characteristics of HER2-positive PMC have not been investigated.
Methods
Pathology archives were searched for PMC diagnosed from January 1999 to April 2018. Clinicopathologic data and microscopic findings were reviewed and compared between HER2-positive PMC and HER2-negative PMC. We also analyzed the differences in disease-free survival (DFS) and overall survival according to clinicopathologic parameters including HER2 status in overall PMC cases.
Results
There were 21 HER2-positive cases (4.8%) in 438 PMCs. The average tumor size of HER2-positive PMC was 32.21 mm (± 26.55). Lymph node metastasis was present in seven cases. Compared to HER2-negative PMC, HER2-positive PMC presented with a more advanced T category (p < .001), more frequent lymph node metastasis (p = .009), and a higher nuclear and histologic grade (p < .001). Microscopically, signet ring cells were frequently observed in HER2-positive PMC (p < .001), whereas a micropapillary pattern was more frequent in HER2-negative PMC (p = .012). HER2-positive PMC was more frequently negative for ER (33.3% vs. 1.2%) and PR (28.6% vs. 7.2%) than HER2-negative PMC and showed a high Ki-67 labeling index. During follow-up, distant metastasis and recurrence developed in three HER2-positive PMC patients. Multivariate analysis revealed that only HER2-positivity and lymph node status were significantly associated with DFS.
Conclusions
Our results suggest that HER2-positive PMC is a more aggressive subgroup of PMC. HER2 positivity should be considered for adequate management of PMC. -
Citations
Citations to this article as recorded by- Mucin‐producing breast lesions: a practical approach to diagnosis
Sunayana Misra, Mihir Gudi, Kimberly H Allison, Edi Brogi, Cecily Quinn, Hannah Y Wen, Puay Hoon Tan
Histopathology.2026;[Epub] CrossRef - Clinicopathological characteristics of mucinous breast cancer: a retrospective analysis of a 6-years study from national cancer center in Vietnam
Thi Huyen Phung, Thanh Tung Pham, Huu Thang Nguyen, Dinh Thach Nguyen, Thanh Long Nguyen, Thi Hoai Hoang
Breast Cancer Research and Treatment.2025; 209(3): 667. CrossRef - Poor response of HER2-positive mucinous carcinomas of breast to neoadjuvant HER2-targeted therapy: A study of four cases
Min Han, Daniel Schmolze, Javier A. Arias-Stella, Christina H. Wei, Joanne Mortimer, Fang Fan
Annals of Diagnostic Pathology.2025; 74: 152396. CrossRef - Comprehensive Immunohistochemical Analysis of Mesonephric Marker Expression in Low-grade Endometrial Endometrioid Carcinoma
Yurimi Lee, Sangjoon Choi, Hyun-Soo Kim
International Journal of Gynecological Pathology.2024; 43(3): 221. CrossRef - Clinicopathological features and prognosis of mucinous breast carcinoma with a micropapillary structure
Beibei Yang, Menglu Shen, Bo Sun, Jing Zhao, Meng Wang
Thoracic Cancer.2024; 15(36): 2530. CrossRef - Pure Mucinous Carcinoma of the Breast: Radiologic-Pathologic Correlation
Cherie M Kuzmiak, Benjamin C Calhoun
Journal of Breast Imaging.2023;[Epub] CrossRef - Role of circ-FOXO3 and miR-23a in radiosensitivity of breast cancer
Elahe Abdollahi, Hossein Mozdarani, Behrooz Z. Alizadeh
Breast Cancer.2023; 30(5): 714. CrossRef - On Ultrasonographic Features of Mucinous Carcinoma with Micropapillary Pattern
Wei-Sen Yang, Yang Li, Ya Gao
Breast Cancer: Targets and Therapy.2023; Volume 15: 473. CrossRef - Spectrum of Mucin-containing Lesions of the Breast: Multimodality Imaging Review with Pathologic Correlation
Janice N. Thai, Melinda F. Lerwill, Shinn-Huey S. Chou
RadioGraphics.2023;[Epub] CrossRef - Mesonephric-like Adenocarcinoma of the Ovary: Clinicopathological and Molecular Characteristics
Hyun Hee Koh, Eunhyang Park, Hyun-Soo Kim
Diagnostics.2022; 12(2): 326. CrossRef - Alveolar Soft Part Sarcoma of the Uterus: Clinicopathological and Molecular Characteristics
Yurimi Lee, Kiyong Na, Ha Young Woo, Hyun-Soo Kim
Diagnostics.2022; 12(5): 1102. CrossRef - Metastasis of the Mucionous adenocarcinoma of breast to the mandibular gingiva: Rare case report
Ivana Mijatov, Aleksandra Fejsa Levakov, Aleksandar Spasić, Jelena Nikolić, Saša Mijatov
Medicine.2022; 101(38): e30732. CrossRef - Endometrioid Carcinomas of the Ovaries and Endometrium Involving Endocervical Polyps: Comprehensive Clinicopathological Analyses
Jihee Sohn, Yurimi Lee, Hyun-Soo Kim
Diagnostics.2022; 12(10): 2339. CrossRef - Serous Carcinoma of the Endometrium with Mesonephric-Like Differentiation Initially Misdiagnosed as Uterine Mesonephric-Like Adenocarcinoma: A Case Report with Emphasis on the Immunostaining and the Identification of Splice Site TP53 Mutation
Sangjoon Choi, Yoon Yang Jung, Hyun-Soo Kim
Diagnostics.2021; 11(4): 717. CrossRef - HER2 positive mucinous carcinoma of breast with micropapillary features: Report of a case and review of literature
Dinesh Chandra Doval, Rupal Tripathi, Sunil Pasricha, Pankaj Goyal, Chaturbhuj Agrawal, Anurag Mehta
Human Pathology: Case Reports.2021; 25: 200531. CrossRef - Carcinoma mucosecretor de mama HER2-positivo, un caso clínico
A.M. González Aranda, E. Martínez Gómez, A. Santana Costa, F. Arnanz Velasco, M.H. González de Diego, A. Zapico Goñi
Clínica e Investigación en Ginecología y Obstetricia.2021; 48(4): 100685. CrossRef - Clinicopathologic features of unexpectedly HER2 positive breast carcinomas: An institutional experience
Carissa LaBoy, Kalliopi P. Siziopikou, Lauren Rosen, Luis Z. Blanco, Jennifer L. Pincus
Pathology - Research and Practice.2021; 222: 153441. CrossRef - Mesonephric-like Differentiation of Endometrial Endometrioid Carcinoma: Clinicopathological and Molecular Characteristics Distinct from Those of Uterine Mesonephric-like Adenocarcinoma
Sujin Park, Go Eun Bae, Jiyoung Kim, Hyun-Soo Kim
Diagnostics.2021; 11(8): 1450. CrossRef - Mesonephric-like Adenocarcinoma of the Uterine Corpus: Comprehensive Immunohistochemical Analyses Using Markers for Mesonephric, Endometrioid and Serous Tumors
Hyunjin Kim, Kiyong Na, Go Eun Bae, Hyun-Soo Kim
Diagnostics.2021; 11(11): 2042. CrossRef
- Mucin‐producing breast lesions: a practical approach to diagnosis
- Analysis of the molecular subtypes of preoperative core needle biopsy and surgical specimens in invasive breast cancer
- Ye Sul Jeong, Jun Kang, Jieun Lee, Tae-Kyung Yoo, Sung Hun Kim, Ahwon Lee
- J Pathol Transl Med. 2020;54(1):87-94. Published online November 13, 2019
- DOI: https://doi.org/10.4132/jptm.2019.10.14
- 10,140 View
- 212 Download
- 17 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Accurate molecular classification of breast core needle biopsy (CNB) tissue is important for determining neoadjuvant systemic therapies for invasive breast cancer. The researchers aimed to evaluate the concordance rate (CR) of molecular subtypes between CNBs and surgical specimens.
Methods
This study was conducted with invasive breast cancer patients who underwent surgery after CNB at Seoul St. Mary’s Hospital between December 2014 and December 2017. Estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), and Ki67 were analyzed using immunohistochemistry. ER and PR were evaluated by Allred score (0–8). HER2 was graded from 0 to +3, and all 2+ cases were reflex tested with silver in situ hybridization. The labeling index of Ki67 was counted by either manual scoring or digital image analysis. Molecular subtypes were classified using the above surrogate markers.
Results
In total, 629 patients were evaluated. The CRs of ER, PR, HER2, and Ki67 were 96.5% (kappa, 0.883; p<.001), 93.0% (kappa, 0.824; p<.001), 99.7% (kappa, 0.988; p<.001), and 78.7% (kappa, 0.577; p<.001), respectively. Digital image analysis of Ki67 in CNB showed better concordance with Ki67 in surgical specimens (CR, 82.3%; kappa, 0.639 for digital image analysis vs. CR, 76.2%; kappa, 0.534 for manual counting). The CRs of luminal A, luminal B, HER2, and triple negative types were 89.0%, 70.0%, 82.9%, and 77.2%, respectively.
Conclusions
CNB was reasonably accurate for determining ER, PR, HER2, Ki67, and molecular subtypes. Using digital image analysis for Ki67 in CNB produced more accurate molecular classifications. -
Citations
Citations to this article as recorded by- Predicting the Efficacy of Breast Cancer Neoadjuvant Chemotherapy Using Ultrasonography and Machine Learning
Meihong Jia, Huizhan Li, Wenli Xiao, Jiping Xue, Zhifen Wang, Xia He, Xin Wang, Dianxia Men
Ultrasound in Medicine & Biology.2026;[Epub] CrossRef - Correlation between ultrasonography and elastography parameters and molecular subtypes of breast cancer in young women
Dian-xia Men, Hui-zhan Li, Juan Dong, Meng-hua Xue, Zhi-fen Wang, Wen-li Xiao, Ji-ping Xue, Mei-hong Jia
Annals of Medicine.2025;[Epub] CrossRef - Concordance of Oncotype DX Breast Recurrence Score Assay Results Between Paired Core Needle Biopsy and Surgical Excision Specimens in Hormone Receptor Positive, Human Epidermal Growth Factor Receptor 2 Negative, Early-Stage Breast Cancer
Aziza Nassar, Jodi Carter, Paige Innis, Andrea Pingitore Blacklock, Jennifer Racz, Matthew Petitt, Purva Singla, Helena Hanna, Abigail Lochala, Christy A. Russell, Minetta C. Liu
JCO Precision Oncology.2025;[Epub] CrossRef - Impact of immunohistochemistry staining conditions on the incidence of human epidermal growth factor receptor 2 (HER2)-low breast cancer
Min Chong Kim, Sun Young Kwon, Hye Ra Jung, Young Kyung Bae
Virchows Archiv.2024; 485(6): 1117. CrossRef - Study on Intratumoral Heterogeneity of Expression of Estrogen Receptor, Progesterone Receptor, and Human Epidermal Growth Factor Receptor 2 in Carcinoma Breast
Ragavi Uthayasuriyan, Sheba K Jacob, Saloni Naresh Shah
Apollo Medicine.2024; 21(1): 51. CrossRef - Concordance of HER2 status between core needle biopsy and surgical resection specimens of breast cancer: an analysis focusing on the HER2-low status
Sei Na, Milim Kim, Yujun Park, Hyun Jung Kwon, Hee-Chul Shin, Eun-Kyu Kim, Mijung Jang, Sun Mi Kim, So Yeon Park
Breast Cancer.2024; 31(4): 705. CrossRef - Concordance of immunohistochemistry for predictive and prognostic factors in breast cancer between biopsy and surgical excision: a single-centre experience and review of the literature
Chiara Rossi, Sara Fraticelli, Marianna Fanizza, Alberta Ferrari, Elisa Ferraris, Alessia Messina, Angelica Della Valle, Chiara Annunziata Pasqualina Anghelone, Angioletta Lasagna, Gianpiero Rizzo, Lorenzo Perrone, Maria Grazia Sommaruga, Giulia Meloni, S
Breast Cancer Research and Treatment.2023; 198(3): 573. CrossRef - Single-center study on clinicopathological and typical molecular pathologic features of metastatic brain tumor
Su Hwa Kim, Young Suk Lee, Sung Hak Lee, Yeoun Eun Sung, Ahwon Lee, Jun Kang, Jae-Sung Park, Sin Soo Jeun, Youn Soo Lee
Journal of Pathology and Translational Medicine.2023; 57(4): 217. CrossRef - The Role of Diffusion-Weighted Imaging Based on Maximum-Intensity Projection in Young Patients with Marked Background Parenchymal Enhancement on Contrast-Enhanced Breast MRI
Ga-Eun Park, Bong-Joo Kang, Sung-hun Kim, Na-Young Jung
Life.2023; 13(8): 1744. CrossRef - Concordance between core needle biopsy and surgical excision specimens for Ki‐67 in breast cancer – a systematic review of the literature
Jahnavi Kalvala, Ruth M Parks, Andrew R Green, Kwok‐Leung Cheung
Histopathology.2022; 80(3): 468. CrossRef - İnvaziv Meme Kanserinde Preoperatif Kor İğne Biyopsi ile Postoperatif Cerrahi Spesmenler Arasında ER, PR, HER2 ve Ki67 Açısından Karşılaştırma
Pınar CELEPLİ, Pelin Seher ÖZTEKİN, Salih CELEPLİ, İrem BİGAT, Sema HÜCÜMENOĞLU
Akdeniz Medical Journal.2022; : 179. CrossRef - Concordance of breast cancer biomarker testing in core needle biopsy and surgical specimens: A single institution experience
Jessica A. Slostad, Nicole K. Yun, Aimee E. Schad, Surbhi Warrior, Louis F. Fogg, Ruta Rao
Cancer Medicine.2022; 11(24): 4954. CrossRef - N-Cadherin Distinguishes Intrahepatic Cholangiocarcinoma from Liver Metastases of Ductal Adenocarcinoma of the Pancreas
Tiemo S. Gerber, Benjamin Goeppert, Anne Hausen, Hagen R. Witzel, Fabian Bartsch, Mario Schindeldecker, Lisa-Katharina Gröger, Dirk A. Ridder, Oscar Cahyadi, Irene Esposito, Matthias M. Gaida, Peter Schirmacher, Peter R. Galle, Hauke Lang, Wilfried Roth,
Cancers.2022; 14(13): 3091. CrossRef - Association of Ki-67 Change Pattern After Core Needle Biopsy and Prognosis in HR+/HER2− Early Breast Cancer Patients
Shuai Li, Xiaosong Chen, Kunwei Shen
Frontiers in Surgery.2022;[Epub] CrossRef - MRI Features for Prediction Malignant Intra-Mammary Lymph Nodes: Correlations with Mammography and Ultrasound
Meejung Kim, Bong Joo Kang, Ga Eun Park
Investigative Magnetic Resonance Imaging.2022; 26(2): 135. CrossRef - A single centre experience in Turkey for comparison between core needle biopsy and surgical specimen evaluation results for HER2, SISH, estrogen receptors and progesterone receptors in breast cancer patients
Hatice Karaman, Fatma Senel, Arzu Tasdemir, Ipek Özer, Merve Dogan
Journal of Cancer Research and Therapeutics.2022; 18(6): 1789. CrossRef - Meme kanseri trucut ve rezeksiyon materyallerinde yeni moleküler sınıflama, tanı ve hormon reseptörlerinin durumu tutarlı mı?
Yeliz ARMAN KARAKAYA, Sevda YILMAZ, Hande KARABAŞ
Pamukkale Medical Journal.2021;[Epub] CrossRef - What shear wave elastography parameter best differentiates breast cancer and predicts its histologic aggressiveness?
Hyunjin Kim, Jeongmin Lee, Bong Joo Kang, Sung Hun Kim
Ultrasonography.2021; 40(2): 265. CrossRef - Risk-based decision-making in the treatment of HER2-positive early breast cancer: Recommendations based on the current state of knowledge
Christian Jackisch, Patricia Cortazar, Charles E. Geyer, Luca Gianni, Joseph Gligorov, Zuzana Machackova, Edith A. Perez, Andreas Schneeweiss, Sara M. Tolaney, Michael Untch, Andrew Wardley, Martine Piccart
Cancer Treatment Reviews.2021; 99: 102229. CrossRef - Factors influencing agreement of breast cancer luminal molecular subtype by Ki67 labeling index between core needle biopsy and surgical resection specimens
Kristina A. Tendl-Schulz, Fabian Rössler, Philipp Wimmer, Ulrike M. Heber, Martina Mittlböck, Nicolas Kozakowski, Katja Pinker, Rupert Bartsch, Peter Dubsky, Florian Fitzal, Martin Filipits, Fanny Carolina Eckel, Eva-Maria Langthaler, Günther Steger, Mich
Virchows Archiv.2020; 477(4): 545. CrossRef
- Predicting the Efficacy of Breast Cancer Neoadjuvant Chemotherapy Using Ultrasonography and Machine Learning
- Expression of female sex hormone receptors and its relation to clinicopathological characteristics and prognosis of lung adenocarcinoma
- Jin Hwan Lee, Han Kyeom Kim, Bong Kyung Shin
- J Pathol Transl Med. 2020;54(1):103-111. Published online November 13, 2019
- DOI: https://doi.org/10.4132/jptm.2019.10.12
- 7,971 View
- 141 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Adenocarcinoma (ADC) of the lung exhibits different clinicopathological characteristics in men and women. Recent studies have suggested that these differences originate from the expression of female sex hormone receptors in tumor cells. The aim of the present study was to evaluate the immunohistochemical expression of female sex hormone receptors in lung ADC and determine the expression patterns in patients with different clinicopathological characteristics.
Methods
A total of 84 patients with lung ADC who underwent surgical resection and/or core biopsy were recruited for the present study. Immunohistochemical staining was performed for estrogen receptor α (ERα), estrogen receptor β (ERβ), progesterone receptor (PR), epidermal growth factor receptor (EGFR), EGFR E746- A750 del, and EGFR L858R using tissue microarray.
Results
A total of 39 (46.4%) ERα-positive, 71 (84.5%) ERβ-positive, and 46 (54.8%) PR-positive lung ADCs were identified. In addition, there were 81 (96.4%) EGFR-positive, 14 (16.7%) EGFR E746-A750 del–positive, and 34 (40.5%) EGFR L858R–positive cases. The expression of female sex hormone receptors was not significantly different in clinicopathologically different subsets of lung ADC.
Conclusions
Expression of female sex hormone receptors is not associated with the prognosis and clinicopathological characteristics of patients with lung ADC. -
Citations
Citations to this article as recorded by- Molecular characteristics of non-small cell lung cancer tissue based on quantitative indicators of progesterone receptors expression
I. P. Romanov, T. A. Bogush, A. M. Scherbakov, A. A. Alimov, E. A. Bogush, A. B. Ravcheeva, A. Lee, V. S. Kosorukov
Antibiot Khimioter = Antibiotics and Chemotherapy.2024; 69(1-2): 29. CrossRef - Genes Co-Expressed with ESR2 Influence Clinical Outcomes in Cancer Patients: TCGA Data Analysis
Julia Maria Lipowicz, Agnieszka Malińska, Michał Nowicki, Agnieszka Anna Rawłuszko-Wieczorek
International Journal of Molecular Sciences.2024; 25(16): 8707. CrossRef - Complex Differential Diagnosis between Primary Breast Cancer and Breast Metastasis from EGFR-Mutated Lung Adenocarcinoma: Case Report and Literature Review
Carmine Valenza, Francesca Maria Porta, Alessandra Rappa, Elena Guerini-Rocco, Giuseppe Viale, Massimo Barberis, Filippo de Marinis, Giuseppe Curigliano, Chiara Catania
Current Oncology.2021; 28(5): 3384. CrossRef - Development of a 15‐Gene Signature Model as a Prognostic Tool in Sex Hormone‐Dependent Cancers
Zhi Xia, Jian Xiao, Aibin Liu, Qiong Chen, Arumugam R. Jayakumar
BioMed Research International.2021;[Epub] CrossRef - Gender-specific aspects of epidemiology, molecular genetics and outcome: lung cancer
Nuria Mederos, Alex Friedlaender, Solange Peters, Alfredo Addeo
ESMO Open.2020; 5(Suppl 4): e000796. CrossRef
- Molecular characteristics of non-small cell lung cancer tissue based on quantitative indicators of progesterone receptors expression
- Morule-like features in pulmonary adenocarcinoma associated with epidermal growth factor receptor mutations: two case reports with targeted next-generation sequencing analysis
- Yoo Jin Lee, Harim Oh, Eojin Kim, Bokyung Ahn, Jeong Hyeon Lee, Youngseok Lee, Yang Seok Chae, Chul Hwan Kim
- J Pathol Transl Med. 2020;54(1):119-122. Published online November 1, 2019
- DOI: https://doi.org/10.4132/jptm.2019.09.30
- 6,563 View
- 138 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Morules, or morule-like features, can be identified in benign and malignant lesions in various organs. Morular features are unusual in pulmonary adenocarcinoma cases with only 26 cases reported to date. Here, we describe two cases of pulmonary adenocarcinoma with morule-like features in Korean women. One patient had a non-mucinous-type adenocarcinoma in situ and the other had an acinarpredominant adenocarcinoma with a micropapillary component. Both patients showed multiple intra-alveolar, nodular, whorled proliferative foci composed of atypical spindle cells with eosinophilic cytoplasm. Targeted next-generation sequencing was performed on DNA extracted from formalin-fixed paraffin-embedded samples of the tumors. Results showed unusual epidermal growth factor receptor (EGFR) mutations, which are associated with drug resistance to EGFR tyrosine kinase inhibitors, revealing the importance of identifying morule-like features in pulmonary adenocarcinoma and the need for additional study, since there are few reported cases.
-
Citations
Citations to this article as recorded by- Pulmonary adenocarcinoma in situ with morule - like components: A surgical case report
Mitsuteru Yosida, Mitsuru Tomita, Naoya Kawakita, Teruki Shimizu, Ryou Yamada, Hiromitsu Takizawa, Hisanori Uehara
Respiratory Medicine Case Reports.2024; 48: 102008. CrossRef - Clinicopathological, Radiological, and Molecular Features of Primary Lung Adenocarcinoma with Morule-Like Components
Li-Li Wang, Li Ding, Peng Zhao, Jing-Jing Guan, Xiao-Bin Ji, Xiao-Li Zhou, Shi-Hong Shao, Yu-Wei Zou, Wei-Wei Fu, Dong-Liang Lin, Dong Pan
Disease Markers.2021; 2021: 1. CrossRef
- Pulmonary adenocarcinoma in situ with morule - like components: A surgical case report
- Serous Adenocarcinoma of Fallopian Tubes: Histological and Immunohistochemical Aspects
- Natalia Hyriavenko, Mykola Lyndin, Kateryna Sikora, Artem Piddubnyi, Ludmila Karpenko, Olha Kravtsova, Dmytrii Hyriavenko, Olena Diachenko, Vladyslav Sikora, Anatolii Romaniuk
- J Pathol Transl Med. 2019;53(4):236-243. Published online April 11, 2019
- DOI: https://doi.org/10.4132/jptm.2019.03.21
- 8,497 View
- 132 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Although primary cancer of the fallopian tubes is a relatively rare type of tumor in female reproductive organs, its mortality is quite high. It is important to identify molecular and biological markers of this malignancy that determine its specific phenotype.
Methods
The study was carried out on samples received from 71 female patients with primary cancer of the fallopian tubes. The main molecular and biological properties, including hormone status (estrogen receptor [ER], progesterone receptor [PR]), human epidermal growth factor receptor (HER2)/neu expression, proliferative potential (Ki-67), apoptosis (p53, Bcl-2), and pro-angiogenic (vascular endothelial growth factor) quality of serous tumors were studied in comparison with clinical and morphological characteristics.
Results
ER and PR expression is accompanied by low grade neoplasia, early clinical disease stage, and absence of lymphogenic metastasis (p < .001). HER2/neu expression is not typical for primary cancer of the fallopian tubes. Ki-67 expression is characterized by an inverse correlation with ER and PR (p < .05) and is associated with lymphogenic metastasis (p < .01). p53+ status correlates with high grade malignancy, tumor progression, metastasis, negative ER/PR (p < .001), and negative Bcl-2 status (p < .05). Positive Bcl-2 status is positively correlated with ER and PR expression and low grade malignancy.
Conclusions
Complex morphologic (histological and immunohistochemical) study of postoperative material allows estimation of the degree of malignancy and tumor spread to enable appropriate treatment for each case. -
Citations
Citations to this article as recorded by- Rare non-serous fallopian tube cancers: institutional experience and literature review
Dmitrii Sumtsov, Georgyi Sumtsov, Nataliia Hyriavenko, Mykola Lyndin, Kateryna Sikora, Nataliia Kalashnik, Svitlana Smiian, Igor Gladchuk
Wiener Medizinische Wochenschrift.2024; 174(9-10): 199. CrossRef - UŞAQLIQ BORULARININ BİRİNCİLİ XƏRÇƏNGİ: DİAQNOSTİKASI VƏ MÜALİCƏSİNİN NƏTİCƏLƏRİ
D.G. Sumtsov, G.O. Sumtsov, N.I. Hyriavenko, S.A. Smiian, N.V. Kalashnyk, K.O. Sikora, N.M. Rozhkovska, I.Z. Gladchuk
Azerbaijan Medical Journal.2023; (4): 75. CrossRef - FEATURES OF ENDOMETRIUM STRUCTURE IN ALCOHOL-ABUSING HIV-INFECTED INDIVIDUALS
M. Lytvynenko
Inter Collegas.2021; 8(1): 52. CrossRef - Concurrent Clostridial Enteritis and Oviductal Adenocarcinoma with Carcinomatosis in an Adult Alpaca (Vicugna pacos)
Mandy Womble, Megan E. Schreeg, Allison Hoch, Enoch B. de Souza Meira, Derek Foster, Christopher Premanandan, Tatiane T. Negrão Watanabe
Journal of Comparative Pathology.2021; 189: 52. CrossRef - Problems of primary fallopian tube cancer diagnostics during and after surgery
D.G. Sumtsov, I.Z. Gladchuk, G.O. Sumtsov, N.I. Hyriavenko, M.S. Lyndin, V.V. Sikora, V.M. Zaporozhan
REPRODUCTIVE ENDOCRINOLOGY.2021; (59): 66. CrossRef
- Rare non-serous fallopian tube cancers: institutional experience and literature review
- Provisional Guideline Recommendation for EGFR Gene Mutation Testing in Liquid Samples of Lung Cancer Patients: A Proposal by the Korean Cardiopulmonary Pathology Study Group
- Dong Hoon Shin, Hyo Sup Shim, Tae Jung Kim, Heae Surng Park, Yun La Choi, Wan Seop Kim, Lucia Kim, Sun Hee Chang, Joon Seon Song, Hyo jin Kim, Jung Ho Han, Chang Hun Lee, Geon Kook Lee, Se Jin Jang
- J Pathol Transl Med. 2019;53(3):153-158. Published online February 28, 2019
- DOI: https://doi.org/10.4132/jptm.2019.02.22
- 10,572 View
- 265 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - Liquid biopsy for detection of mutation from circulating tumor DNA is a new technology which is attractive in that it is non-invasive. Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKI) is an effective first line drug for advanced non-small cell lung cancer patients who harbor activating EGFR mutation. During the course of treatment, resistance against TKI arises which can be contributed to EGFR T790M mutation in about 50–60% of patients. Third generation TKI may overcome the resistance. In patients who cannot undergo tissue biopsy due to variable reasons, liquid biopsy is an excellent alternative for the detection of EGFR T790M mutation. However, this relatively novel method requires standardization and vigorous quality insurance. Thus, a standard set of guideline recommendations for liquid biopsy for EGFR mutation testing suitable for the Korean medical community is necessary. In this article, we propose a set of provisional guideline recommendations that was discussed and approved by the Cardiopulmonary Pathology Study Group of the Korean Society of Pathologists.
-
Citations
Citations to this article as recorded by- Comparison of tissue-based and plasma-based testing for EGFR mutation in non–small cell lung cancer patients
Yoon Kyung Kang, Dong Hoon Shin, Joon Young Park, Chung Su Hwang, Hyun Jung Lee, Jung Hee Lee, Jee Yeon Kim, JooYoung Na
Journal of Pathology and Translational Medicine.2025; 59(1): 60. CrossRef - Improving non-small-cell lung cancer survival through molecular characterization: Perspective of a multidisciplinary expert panel
M.G.O. Fernandes, A.S. Vilariça, B. Fernandes, C. Camacho, C. Saraiva, F. Estevinho, H. Novais e Bastos, J.M. Lopes, P. Fidalgo, P. Garrido, S. Alves, S. Silva, T. Sequeira, F. Barata
Pulmonology.2024; 30(1): 4. CrossRef - Unlocking the future of cancer diagnosis – promises and challenges of ctDNA-based liquid biopsies in non-small cell lung cancer
Chiara Reina, Berina Šabanović, Chiara Lazzari, Vanesa Gregorc, Christopher Heeschen
Translational Research.2024; 272: 41. CrossRef - Exosomes in Lung Cancer: Actors and Heralds of Tumor Development
Amaia Sandúa, Estibaliz Alegre, Álvaro González
Cancers.2021; 13(17): 4330. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Current status and future perspectives of liquid biopsy in non-small cell lung cancer
Sunhee Chang, Jae Young Hur, Yoon-La Choi, Chang Hun Lee, Wan Seop Kim
Journal of Pathology and Translational Medicine.2020; 54(3): 204. CrossRef - Prevalence of T790M mutation among TKI-therapy resistant Lebanese lung cancer patients based on liquid biopsy analysis: a first report from a major tertiary care center
Hazem Assi, Arafat Tfayli, Nada Assaf, Sarah Abou Daya, Aram H. Bidikian, Dima Kawsarani, Puzant Fermanian, Ghazi Zaatari, Rami Mahfouz
Molecular Biology Reports.2019; 46(4): 3671. CrossRef
- Comparison of tissue-based and plasma-based testing for EGFR mutation in non–small cell lung cancer patients
- Potential Role for a Panel of Immunohistochemical Markers in the Management of Endometrial Carcinoma
- Amany Salama, Mohammad Arafa, Eman ElZahaf, Abdelhadi Mohamed Shebl, Azmy Abd El-Hameed Awad, Sylvia A. Ashamallah, Reda Hemida, Anas Gamal, Abd AlRahman Foda, Khaled Zalata, El-Said M. Abdel-Hady
- J Pathol Transl Med. 2019;53(3):164-172. Published online February 28, 2019
- DOI: https://doi.org/10.4132/jptm.2019.02.12
- 11,632 View
- 384 Download
- 13 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
In order to improve the efficacy of endometrial carcinoma (EC) treatment, identifying prognostic factors for high risk patients is a high research priority. This study aimed to assess the relationships among the expression of estrogen receptors (ER), progesterone receptors (PR), human epidermal growth factor receptor 2 (HER2), Ki-67, and the different histopathological prognostic parameters in EC and to assess the value of these in the management of EC.
Methods
We examined 109 cases of EC. Immunohistochemistry for ER, PR, HER2, and Ki-67 were evaluated in relation to age, tumor size, International Federation of Gynecology and Obstetrics (FIGO) stage and grade, depth of infiltration, cervical and ovarian involvement, lymphovascular space invasion (LVSI), and lymph node (LN) metastasis.
Results
The mean age of patients in this study was 59.8 ± 8.2 years. Low ER and PR expression scores and high Ki-67 expression showed highly significant associations with non-endometrioid histology (p = .007, p < .001, and p < .001, respectively) and poor differentiation (p = .007, p < .001, and p <. 001, respectively). Low PR score showed a significant association with advanced stage (p = .009). Low ER score was highly associated with LVSI (p = .006), and low PR scores were associated significantly with LN metastasis (p = .026). HER2 expression was significantly related to advanced stages (p = .04), increased depth of infiltration (p = .02), LVSI (p = .017), ovarian involvement (p = .038), and LN metastasis (p = .038). There was a close relationship between HER2 expression and uterine cervical involvement (p = .009). Higher Ki-67 values were associated with LN involvement (p = .012).
Conclusions
The over-expression of HER2 and Ki-67 and low expression of ER and PR indicate a more malignant EC behavior. An immunohistochemical panel for the identification of high risk tumors can contribute significantly to prognostic assessments. -
Citations
Citations to this article as recorded by- Tissue Microarray for Gynecological Pathology Studies: A Mini-Review
Mohammad Arafa, Abd AlRahman Foda, Amany Salama, Ola Shalaby, Muna Al-Jabri, Fatma Al Hinai, Afrah Al-Rashdi, Samya Al-Husaini, Suaad Al-Badi
Journal of Microscopy and Ultrastructure.2026;[Epub] CrossRef - Clinicopathological Correlation of Hormone Receptors, Angiogenesis, and Tumor Budding in Endometrial Carcinoma: A Tertiary Care Center Study
Senjuti Dasgupta, Arpita Das, Ujjwal Bandyopadhyay
The Journal of Obstetrics and Gynecology of India.2025;[Epub] CrossRef - Multiparameter MRI-based radiomics analysis for preoperative prediction of type II endometrial cancer
Yingying Cao, Wei Zhang, Xiaorong Wang, Xiaojing Lv, Yaping Zhang, Kai Guo, Shuai Ren, Yuan Li, Zhongqiu Wang, Jingya Chen
Heliyon.2024; 10(12): e32940. CrossRef - Correlation of PD-L1 expression with different clinico-pathological and immunohistochemical features of ovarian surface epithelial tumors
Asem Shalaby, Ola Shalaby, Hazem Abdullah, Mohamed Rachid Boulassel, Mohammad Arafa
Clinical and Translational Oncology.2024; 27(2): 699. CrossRef - Estrogen/Progesterone Receptor Loss, CTNNB1 and KRAS Mutations Are Associated With Local Recurrence or Distant Metastasis in Low-Grade Endometrial Endometrioid Carcinoma
Rajni Chibbar, Sabrina Foerstner, Janarathnee Suresh, Richa Chibbar, Alexandre Piche, Deeksha Kundapur, Rani Kanthan, Vijayanand Kundapur, Cheng Han Lee, Anita Agrawal, Raymond Lai
Applied Immunohistochemistry & Molecular Morphology.2023; 31(3): 181. CrossRef - Exploring the Prognostic and Predictive Roles of Ki-67 in Endometrial Cancer
Laura Paleari, Mariangela Rutigliani, Oriana D’Ecclesiis, Sara Gandini, Irene Maria Briata, Tania Buttiron Webber, Nicoletta Provinciali, Andrea DeCensi
International Journal of Translational Medicine.2023; 3(4): 479. CrossRef - Analysis of human epidermal growth factor receptor 2 immunohistochemical expression in high-grade endometrial carcinomas and its association with variable clinical outcomes
Malames M. Faisal, Marwa M. Shakweer, Ghada Refaat, Khaled S. Mohammed, Tarek I. ElMallawy, Magda H. Nasreldin, Laila M. Farid, Mariam B. Abouelkhair
Egyptian Journal of Pathology.2023; 43(2): 119. CrossRef - Correlation of PD-L1 immunohistochemical expression with microsatellite instability and p53 status in endometrial carcinoma
Mohammad Arafa, Abdelhadi Mohamed Shebl, Amany Salama, Eman ElZahaf, Sylvia A. Ashamallah, Abd AlRahman Foda, AzmyAbd El-Hameed Awad, Asem Shalaby
European Journal of Obstetrics & Gynecology and Reproductive Biology: X.2022; 16: 100172. CrossRef - Immunohistochemical Expression of Oestrogen and Epidermal Growth Factor Receptors in Endometrial Cancerous in Sudanese Patients
Salwa Abdalraheem Abubaker, Mohamed Elfatih Abdelwadoud, Mutaz Mohamed Ali, Hadia Alhaj Ahmad, Abuobieda Mohamed Khlafalla, Osman Mohammed Elmahi, Hisham Ali Waggiallah
Journal Of Biochemical Technology.2021; 12(1): 58. CrossRef - Expression of ER/PR Receptor, Her-2/neu, Ki67 and p53 in Endometrial Carcinoma: Clinicopathological Implication and Prognostic Value
V. B. Shivkumar, Manisha A. Atram, Nitin M. Gangane
Indian Journal of Gynecologic Oncology.2020;[Epub] CrossRef - Immunohistochemical study of ER, PR, p53 and Ki67 expression in patients with endometrial adenocarcinoma and atypical endometrial hyperplasia
Rachana Lakhe, Ravi M Swami, Preeti Doshi, Manjiri N Karandikar, Ravindra Nimbargi
IP Archives of Cytology and Histopathology Research.2020; 5(4): 274. CrossRef
- Tissue Microarray for Gynecological Pathology Studies: A Mini-Review
- Uterine Malignant Mixed Müllerian Tumors Following Treatment with Selective Estrogen Receptor Modulators in Patients with Breast Cancer: A Report of 13 Cases and Their Clinicopathologic Characteristics
- Byung-Kwan Jeong, Chang O. Sung, Kyu-Rae Kim
- J Pathol Transl Med. 2019;53(1):31-39. Published online December 18, 2018
- DOI: https://doi.org/10.4132/jptm.2018.11.16
- 8,445 View
- 102 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Breast cancer treatment with selective estrogen receptor modulators (SERMs) increasesthe incidence of uterine malignant mixed Müllerian tumors (uMMMTs). We examine clinicopathologiccharacteristics and prognosis of SERM-associated uMMMTs (S-uMMMTs) and discusspossible pathogenetic mechanisms.
Methods
Among 28,104 patients with breast cancer, clinicopathologicfeatures and incidence of uMMMT were compared between patients who underwentSERM treatment and those who did not. Of 92 uMMMT cases that occurred during the same period,incidence, dose, and duration of SERM treatment, as well as overall survival rate, were comparedfor patients with breast cancer who underwent SERM treatment and those who did not (S-uMMMTvs NS-uMMMT) and for patients without breast cancer (de novo-uMMMT). Histopathologicalfindings and immunophenotypes for myogenin, desmin, p53, WT-1, estrogen receptor (ER) α, ERβ,progesterone receptor, and GATA-3 were compared between S-uMMMT and de novo-uMMMT.
Results
The incidence of S-uMMMT was significantly higher than that of NS-uMMMT (6.35-fold).All patients with SERM were postmenopausal and received daily 20–40 mg SERM. CumulativeSERM dose ranged from 21.9 to 73.0 g (mean, 46.0) over 39–192 months (mean, 107). Clinicopathologicfeatures, such as International Federation of Gynecology and Obstetrics stage andoverall survival, were not significantly different between patients with S-uMMMT and NS-uMMMTor between patients with S-uMMMT and de novo-uMMMT. All 11 S-uMMMT cases available forimmunostaining exhibited strong overexpression/null expression of p53 protein and significantlyincreased ERβ expression in carcinomatous and sarcomatous components.
Conclusions
SERMtherapy seemingly increases risk of S-uMMMT development; however, clinicopathologic featureswere similar in all uMMMTs from different backgrounds. p53 mutation and increased ERβ expressionmight be involved in the etiology of S-uMMMT. -
Citations
Citations to this article as recorded by- Uterine carcinosarcomas: A case series of 9 cases from a low-income country
Boubacar Efared, Halidou Hamadou Koura, Aïchatou Balaraba Abani Bako, Idrissa Boubacar, Habiba Salifou Boureima, Garba Mahamadou, Hassan Nouhou
Medicine.2024; 103(40): e39773. CrossRef - Uterine carcinosarcoma: Unraveling the role of epithelial‐to‐mesenchymal transition in progression and therapeutic potential
Mohan Shankar Gopinatha Pillai, Pallab Shaw, Arpan Dey Bhowmik, Resham Bhattacharya, Geeta Rao, Shailendra Kumar Dhar Dwivedi
The FASEB Journal.2024;[Epub] CrossRef - Tamoxifen/toremifene
Reactions Weekly.2019; 1758(1): 330. CrossRef - Molecular Basis of Tumor Heterogeneity in Endometrial Carcinosarcoma
Susanna Leskela, Belen Pérez-Mies, Juan Manuel Rosa-Rosa, Eva Cristobal, Michele Biscuola, María L. Palacios-Berraquero, SuFey Ong, Xavier Matias-Guiu Guia, José Palacios
Cancers.2019; 11(7): 964. CrossRef
- Uterine carcinosarcomas: A case series of 9 cases from a low-income country
- Molecular Screening of Small Biopsy Samples Using Next-Generation Sequencing in Korean Patients with Advanced Non-small Cell Lung Cancer: Korean Lung Cancer Consortium (KLCC-13-01)
- Bo Mi Ku, Mi Hwa Heo, Joo-Hang Kim, Byoung Chul Cho, Eun Kyung Cho, Young Joo Min, Ki Hyeong Lee, Jong-Mu Sun, Se-Hoon Lee, Jin Seok Ahn, Keunchil Park, Tae Jung Kim, Ho Yun Lee, Hojoong Kim, Kyung-Jong Lee, Myung-Ju Ahn
- J Pathol Transl Med. 2018;52(3):148-156. Published online March 26, 2018
- DOI: https://doi.org/10.4132/jptm.2018.03.12
- 10,689 View
- 315 Download
- 16 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Non-small cell lung cancer (NSCLC) is a common type of cancer with poor prognosis. As individual cancers exhibit unique mutation patterns, identifying and characterizing gene mutations in NSCLC might help predict patient outcomes and guide treatment. The aim of this study was to evaluate the clinical adequacy of molecular testing using next-generation sequencing (NGS) for small biopsy samples and characterize the mutational landscape of Korean patients with advanced NSCLC.
Methods
DNA was extracted from small biopsy samples of 162 patients with advanced NSCLC. Targeted NGS of genomic alterations was conducted using Ion AmpliSeq Cancer Hotspot Panel v2.
Results
The median age of patients was 64 years (range, 32 to 83 years) and the majority had stage IV NSCLC at the time of cancer diagnosis (90%). Among the 162 patients, 161 patients (99.4%) had novel or hotspot mutations (range, 1 to 21 mutated genes). Mutations were found in 41 genes. Three of the most frequently mutated genes were TP53 (151, 93.2%), KDR (104, 64.2%), and epidermal growth factor receptor (EGFR; 69, 42.6%). We also observed coexistence of EGFR and other oncogene (such as KRAS, PIC3CA, PTEN, and STK11) mutations. Given that 69.6% (48/69) of EGFR mutant patients were treated with EGFR tyrosine kinase inhibitors, EGFR mutant status had higher prognostic ability in this study.
Conclusions
These results suggest that targeted NGS using small biopsy samples is feasible and allows for the detection of both common and rare mutations in NSCLC. -
Citations
Citations to this article as recorded by- The clinical relevance of surgical specimens for RNA sequencing in lung cancer: a cohort study
Jung Seop Eom, Soo Han Kim, Kyungbin Kim, Ahrong Kim, Hyo Yeong Ahn, Jeongha Mok, Jeong Su Cho, Min Ki Lee, Ju Sun Song, Mi-Hyun Kim
Frontiers in Oncology.2024;[Epub] CrossRef - PTEN, PTENP1, microRNAs, and ceRNA Networks: Precision Targeting in Cancer Therapeutics
Glena Travis, Eileen M. McGowan, Ann M. Simpson, Deborah J. Marsh, Najah T. Nassif
Cancers.2023; 15(20): 4954. CrossRef - Worldwide Prevalence of Epidermal Growth Factor Receptor Mutations in Non-Small Cell Lung Cancer: A Meta-Analysis
Barbara Melosky, Kato Kambartel, Maik Häntschel, Margherita Bennetts, Dana J. Nickens, Julia Brinkmann, Antonin Kayser, Michael Moran, Federico Cappuzzo
Molecular Diagnosis & Therapy.2022; 26(1): 7. CrossRef - Landscape of EGFR mutations in lung adenocarcinoma: a single institute experience with comparison of PANAMutyper testing and targeted next-generation sequencing
Jeonghyo Lee, Yeon Bi Han, Hyun Jung Kwon, Song Kook Lee, Hyojin Kim, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2022; 56(5): 249. CrossRef - Suitability of transbronchial brushing cytology specimens for next‐generation sequencing in peripheral lung cancer
Naoki Furuya, Shingo Matsumoto, Kazutaka Kakinuma, Kei Morikawa, Takeo Inoue, Hisashi Saji, Koichi Goto, Masamichi Mineshita
Cancer Science.2021; 112(1): 380. CrossRef - KLHL38 involvement in non-small cell lung cancer progression via activation of the Akt signaling pathway
Yitong Xu, Chenglong Wang, Xizi Jiang, Yao Zhang, Hongbo Su, Jun Jiang, Hongjiu Ren, Xueshan Qiu
Cell Death & Disease.2021;[Epub] CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Targeting non-small cell lung cancer: driver mutation beyond epidermal growth factor mutation and anaplastic lymphoma kinase fusion
Quincy S. Chu
Therapeutic Advances in Medical Oncology.2020;[Epub] CrossRef Concomitant Mutations in EGFR 19Del/L858R Mutation and Their Association with Response to EGFR-TKIs in NSCLC Patients
Hengrui Liang, Caichen Li, Yi Zhao, Shen Zhao, Jun Huang, Xiuyu Cai, Bo Cheng, Shan Xiong, Jianfu Li, Wei Wang, Changbin Zhu, Weiwei Li, Jianxing He, Wenhua Liang
Cancer Management and Research.2020; Volume 12: 8653. CrossRef- Prognostic role of Rab27A and Rab27B expression in patients with non‐small cell lung carcinoma
Hyun Min Koh, Dae Hyun Song
Thoracic Cancer.2019; 10(2): 143. CrossRef - PD‐L1 expression in ROS1‐rearranged non‐small cell lung cancer: A study using simultaneous genotypic screening of EGFR, ALK, and ROS1
Jongmin Lee, Chan Kwon Park, Hyoung‐Kyu Yoon, Young Jo Sa, In Sook Woo, Hyo Rim Kim, Sue Youn Kim, Tae‐Jung Kim
Thoracic Cancer.2019; 10(1): 103. CrossRef - Targeted Next-Generation Sequencing Validates the Use of Diagnostic Biopsies as a Suitable Alternative to Resection Material for Mutation Screening in Colorectal Cancer
Hersh A. Ham-Karim, Henry Okuchukwu Ebili, Kirsty Manger, Wakkas Fadhil, Narmeen S. Ahmad, Susan D. Richman, Mohammad Ilyas
Molecular Diagnosis & Therapy.2019; 23(3): 383. CrossRef - Small lung tumor biopsy samples are feasible for high quality targeted next generation sequencing
Hidenori Kage, Shinji Kohsaka, Aya Shinozaki‐Ushiku, Yoshihisa Hiraishi, Jiro Sato, Kazuhiro Nagayama, Tetsuo Ushiku, Daiya Takai, Jun Nakajima, Kiyoshi Miyagawa, Hiroyuki Aburatani, Hiroyuki Mano, Takahide Nagase
Cancer Science.2019; 110(8): 2652. CrossRef - PTEN in Lung Cancer: Dealing with the Problem, Building on New Knowledge and Turning the Game Around
Anastasios Gkountakos, Giulia Sartori, Italia Falcone, Geny Piro, Ludovica Ciuffreda, Carmine Carbone, Giampaolo Tortora, Aldo Scarpa, Emilio Bria, Michele Milella, Rafael Rosell, Vincenzo Corbo, Sara Pilotto
Cancers.2019; 11(8): 1141. CrossRef
- The clinical relevance of surgical specimens for RNA sequencing in lung cancer: a cohort study
- Loss of Progesterone Receptor Expression Is an Early Tumorigenesis Event Associated with Tumor Progression and Shorter Survival in Pancreatic Neuroendocrine Tumor Patients
- Sung Joo Kim, Soyeon An, Jae Hoon Lee, Joo Young Kim, Ki-Byung Song, Dae Wook Hwang, Song Cheol Kim, Eunsil Yu, Seung-Mo Hong
- J Pathol Transl Med. 2017;51(4):388-395. Published online June 8, 2017
- DOI: https://doi.org/10.4132/jptm.2017.03.19
- 9,022 View
- 138 Download
- 18 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Pancreatic neuroendocrine tumors (PanNETs) are the second most common pancreatic neoplasms and there is no well-elucidated biomarker to stratify their detection and prognosis. Previous studies have reported that progesterone receptor (PR) expression status was associated with poorer survival in PanNET patients.
Methods
To validate previous studies, PR protein expression was assessed in 21 neuroendocrine microadenomas and 277 PanNETs and compared with clinicopathologic factors including patient survival.
Results
PR expression was gradually decreased from normal islets (49/49 cases, 100%) to neuroendocrine microadenoma (14/21, 66.6%) to PanNETs (60/277, 21.3%; p < .001). PanNETs with loss of PR expression were associated with increased tumor size (p < .001), World Health Organization grade (p = .001), pT classification (p < .001), perineural invasion (p = .028), lymph node metastasis (p = .004), activation of alternative lengthening of telomeres (p = .005), other peptide hormonal expression (p < .001) and ATRX/DAXX expression (p = .015). PanNET patients with loss of PR expression (5-year survival rate, 64.1%) had significantly poorer recurrence-free survival outcomes than those with intact PR expression (90%) by univariate (p = .012) but not multivariate analyses. Similarly, PanNET patients with PR expression loss (5-year survival rate, 76%) had significantly poorer overall survival by univariate (p = .015) but not multivariate analyses.
Conclusions
Loss of PR expression was noted in neuroendocrine microadenomas and was observed in the majority of PanNETs. This was associated with increased grade, tumor size, and advanced pT and pN classification; and was correlated with decreased patient survival time by univariate but not multivariate analyses. Loss of PR expression can provide additional information on shorter disease-free survival in PanNET patients. -
Citations
Citations to this article as recorded by- Incidence and Prognostic Implications of Lymphovascular Invasion in Node‐Negative Pancreatic Neuroendocrine Tumors: Results From the US Neuroendocrine Study Group
Kota Sahara, Diamantis I. Tsilimigras, Yuki Homma, Jun Kawashima, Shishir K. Maithel, Flavio Rocha, Sharon Weber, Ryan Fields, Kamran Idrees, George A. Poultsides, Cliff Cho, Itaru Endo, Timothy M. Pawlik
Journal of Surgical Oncology.2025; 131(3): 465. CrossRef - Sex Differences in the Survival of Patients with Neuroendocrine Neoplasms: A Comparative Study of Two National Databases
Mohamed Mortagy, Marie Line El Asmar, Kandiah Chandrakumaran, John Ramage
Cancers.2024; 16(13): 2376. CrossRef - Association Between Female Sex and Better Survival in Gastroenteropancreatic Neuroendocrine Tumors
Jeremy Chang, Mohammed O. Suraju, Catherine G. Tran, Carlos H.F. Chan, Po Hien Ear, James R. Howe, Scott K. Sherman
Journal of Surgical Research.2024; 302: 53. CrossRef - Venous invasion and lymphatic invasion are correlated with the postoperative prognosis of pancreatic neuroendocrine neoplasm
Sho Kiritani, Junichi Arita, Yuichiro Mihara, Rihito Nagata, Akihiko Ichida, Yoshikuni Kawaguchi, Takeaki Ishizawa, Nobuhisa Akamatsu, Junichi Kaneko, Kiyoshi Hasegawa
Surgery.2023; 173(2): 365. CrossRef - Combined Infiltrative Macroscopic Growth Pattern and Infiltrative Microscopic Tumor Border Status Is a Novel Surrogate Marker of Poor Prognosis in Patients With Pancreatic Neuroendocrine Tumor
Bokyung Ahn, Joo Young Kim, Seung-Mo Hong
Archives of Pathology & Laboratory Medicine.2023; 147(1): 100. CrossRef - HORMONET: a phase II trial of tamoxifen for estrogen/progesterone receptor-positive neuroendocrine tumors
Milton J. Barros, Jonathan Strosberg, Taymeyah Al-Toubah, Victor Hugo F. de Jesus, Lais Durant, Celso A. Mello, Tiago C. Felismino, Louise De Brot, Rodrigo G. Taboada, Mauro D. Donadio, Rachel P. Riechelmann
Therapeutic Advances in Medical Oncology.2023;[Epub] CrossRef - Diagnostic and Prognostic Impact of Progesterone Receptor Immunohistochemistry: A Study Evaluating More Than 16,000 Tumors
Florian Viehweger, Lisa-Marie Tinger, David Dum, Natalia Gorbokon, Anne Menz, Ria Uhlig, Franziska Büscheck, Andreas M. Luebke, Claudia Hube-Magg, Andrea Hinsch, Doris Höflmayer, Christoph Fraune, Patrick Lebok, Sören Weidemann, Maximilian Lennartz, Frank
Analytical Cellular Pathology.2022; 2022: 1. CrossRef - Prognostic Nomograms to Predict Overall Survival and Cancer-Specific Survival of Patients With Pancreatic Neuroendocrine Tumors
Zuoli Song, Sumei Wang, Yujing Wu, Jinjuan Zhang, Shuye Liu
Pancreas.2021; 50(3): 414. CrossRef - Pancreatic High-Grade Neuroendocrine Neoplasms in the Korean Population: A Multicenter Study
Haeryoung Kim, Soyeon An, Kyoungbun Lee, Sangjeong Ahn, Do Youn Park, Jo-Heon Kim, Dong-Wook Kang, Min-Ju Kim, Mee Soo Chang, Eun Sun Jung, Joon Mee Kim, Yoon Jung Choi, So-Young Jin, Hee Kyung Chang, Mee-Yon Cho, Yun Kyung Kang, Myunghee Kang, Soomin Ahn
Cancer Research and Treatment.2020; 52(1): 263. CrossRef - Systemic distribution of progesterone receptor subtypes in human tissues
Teeranut Asavasupreechar, Ryoko Saito, Yasuhiro Miki, Dean P. Edwards, Viroj Boonyaratanakornkit, Hironobu Sasano
The Journal of Steroid Biochemistry and Molecular Biology.2020; 199: 105599. CrossRef - Progesteron receptor expression in insulin producing cells of neuroendocrine neoplasms
Tomoyoshi Tachibana, Atsuko Kasajima, Takeshi Aoki, Tomoaki Tabata, Keely McNamara, Samaneh Yazdani, Sato Satoko, Fumiyoshi Fujishima, Fuyuhiko Motoi, Michiaki Unno, Hironobu Sasano
The Journal of Steroid Biochemistry and Molecular Biology.2020; 201: 105694. CrossRef - Prognostic and predictive factors on overall survival and surgical outcomes in pancreatic neuroendocrine tumors: recent advances and controversies
Lingaku Lee, Tetsuhide Ito, Robert T Jensen
Expert Review of Anticancer Therapy.2019; 19(12): 1029. CrossRef - Immunohistochemistry, carcinomas of unknown primary, and incidence rates
Edward B. Stelow, Hadi Yaziji
Seminars in Diagnostic Pathology.2018; 35(2): 143. CrossRef - Carbonic anhydrase 9 expression in well-differentiated pancreatic neuroendocrine neoplasms might be associated with aggressive behavior and poor survival
Joo Young Kim, Sang Hwa Lee, Soyeon An, Sung Joo Kim, You-Na Sung, Ki-Byung Song, Dae Wook Hwang, Song Cheol Kim, Seung-Mo Hong
Virchows Archiv.2018; 472(5): 739. CrossRef - Prognostic value of progesterone receptor in solid pseudopapillary neoplasm of the pancreas: evaluation of a pooled case series
Feiyang Wang, Zibo Meng, Shoukang Li, Yushun Zhang, Heshui Wu
BMC Gastroenterology.2018;[Epub] CrossRef - Estrogens modulate progesterone receptor expression and may contribute to progesterone-mediated apoptotic β-cell death
Viviane Abreu Nunes
Endocrinology&Metabolism International Journal.2018;[Epub] CrossRef
- Incidence and Prognostic Implications of Lymphovascular Invasion in Node‐Negative Pancreatic Neuroendocrine Tumors: Results From the US Neuroendocrine Study Group
- Basaloid Squamous Cell Carcinoma of the Head and Neck: Subclassification into Basal, Ductal, and Mixed Subtypes Based on Comparison of Clinico-pathologic Features and Expression of p53, Cyclin D1, Epidermal Growth Factor Receptor, p16, and Human Papillomavirus
- Kyung-Ja Cho, Se Un Jeong, Sung Bae Kim, Sang-wook Lee, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim
- J Pathol Transl Med. 2017;51(4):374-380. Published online June 8, 2017
- DOI: https://doi.org/10.4132/jptm.2017.03.03
- 21,337 View
- 483 Download
- 11 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Basaloid squamous cell carcinoma (BSCC) is a rare variant of squamous cell carcinoma with distinct pathologic characteristics. The histogenesis of BSCC is not fully understood, and the cancer has been suggested to originate from a totipotent primitive cell in the basal cell layer of the surface epithelium or in the proximal duct of secretory glands.
Methods
Twenty-six cases of head and neck BSCC from Asan Medical Center, Seoul, Korea, reported during a 14-year-period were subclassified into basal, ductal, and mixed subtypes according to the expression of basal (cytokeratin [CK] 5/6, p63) or ductal markers (CK7, CK8/18). The cases were also subject to immunohistochemical study for CK19, p53, cyclin D1, epidermal growth factor receptor (EGFR), and p16 and to in situ hybridization for human papillomavirus (HPV), and the results were clinico-pathologically compared.
Results
Mixed subtype (12 cases) was the most common, and these cases showed hypopharyngeal predilection, older age, and higher expression of CK19, p53, and EGFR than other subtypes. The basal subtype (nine cases) showed frequent comedo-necrosis and high expression of cyclin D1. The ductal subtype (five cases) showed the lowest expression of p53, cyclin D1, and EGFR. A small number of p16- and/or HPV-positive cases were not restricted to one subtype. BSCC was the cause of death in 19 patients, and the average follow-up period for all patients was 79.5 months. Overall survival among the three subtypes was not significantly different.
Conclusions
The results of this study suggest a heterogeneous pathogenesis of head and neck BSCC. Each subtype showed variable histology and immunoprofiles, although the clinical implication of heterogeneity was not determined in this study. -
Citations
Citations to this article as recorded by- Histopathological variants of head and neck squamous cell carcinomas: A multicenter study in Latin America
Heitor Albergoni Silveira, Karina Helen Martins, Ana Lia Anbinder, Thais Aguiar Santos, Elton Fernandes Barros, Pollianna Muniz Alves, Cassiano Francisco Weege Nonaka, Ana Terezinha Marques Mesquita, Matheus Henrique Lopes Dominguete, Rafael Rodrigues Dia
Annals of Diagnostic Pathology.2026; 80: 152565. CrossRef - HPV-associated oropharyngeal cancer: epidemiology, molecular biology and clinical management
Matt Lechner, Jacklyn Liu, Liam Masterson, Tim R. Fenton
Nature Reviews Clinical Oncology.2022; 19(5): 306. CrossRef - Neoadjuvant treatment combined with planned endoscopic surgery in locally advanced sphenoid sinus basaloid squamous cell carcinoma
Yinghong Zhang, Suqing Tian, Yali Du, Qiang Zuo, Li Zhu, Furong Ma
Medicine: Case Reports and Study Protocols.2022; 3(6): e0044. CrossRef - Cetuximab and paclitaxel combination therapy for recurrent basaloid squamous cell carcinoma in the ethmoid sinus
Satoshi Koyama, Kazunori Fujiwara, Tsuyoshi Morisaki, Taihei Fujii, Yosuke Nakamura, Takahiro Fukuhara, Hiromi Takeuchi
Auris Nasus Larynx.2021; 48(6): 1189. CrossRef - Constitutive Hedgehog/GLI2 signaling drives extracutaneous basaloid squamous cell carcinoma development and bone remodeling
Marina Grachtchouk, Jianhong Liu, Mark E Hutchin, Paul W Harms, Dafydd Thomas, Lebing Wei, Aiqin Wang, Donelle Cummings, Lori Lowe, Jonathan Garlick, James Sciubba, Arul M Chinnaiyan, Monique E Verhaegen, Andrzej A Dlugosz
Carcinogenesis.2021; 42(8): 1100. CrossRef - Conjunctival ‘mucoepidermoid carcinoma’ revisited: a revision of terminology, based on morphologic, immunohistochemical and molecular findings of 14 cases, and the 2018 WHO Classification of Tumours of the Eye
Hardeep S. Mudhar, Tatyana Milman, Paul J.L. Zhang, Carol L. Shields, Ralph C. Eagle, Sara E. Lally, Jerry A. Shields, Sachin M. Salvi, Paul A. Rundle, Jennifer Tan, Ian G. Rennie
Modern Pathology.2020; 33(7): 1242. CrossRef - Basaloid squamous cell carcinoma with adenoid cystic‐like features of the head and neck region: A report of two cases
Kimihide Kusafuka, Haruna Yagi, Satoshi Baba, Hiroshi Inagaki, Chinatsu Tsuchiya, Kazuki Hirata, Aya Muramatsu, Makoto Suzuki, Kazumori Arai, Tadashi Terada
Pathology International.2020; 70(10): 767. CrossRef - Association study of cell cycle proteins and human papillomavirus in laryngeal cancer in Chinese population
Lifang Cui, Congling Qu, Honggang Liu
Clinical Otolaryngology.2019; 44(3): 323. CrossRef - Liver metastatic basaloid squamous cell carcinoma with negative expression of pancytokeratin: a case report and literature review
Linxiu Liu, Xuemin Xue, Liyan Xue
Diagnostic Pathology.2019;[Epub] CrossRef - Basaloid Squamous Cell Carcinoma at the Floor of the Mouth and Mandible: A Case Report
Jun-Sang Lee, Uk-Kyu Kim, Dae-Seok Hwang, Jun-Ho Lee, Hong-Seok Choi, Na-Rae Choi, Mi Heon Ryu, Gyoo Cheon Kim
The Korean Journal of Oral and Maxillofacial Pathology.2019; 43(5): 197. CrossRef - p53 and p16 expression in oral cavity squamous cell and basaloid squamous cell carcinoma
Allisson Filipe Lopes Martins, Carlos Henrique Pereira, Marília Oliveira Morais, Paulo Otávio Carmo Souza, Lucas Borges Fleury Fernandes, Aline Carvalho Batista, Elismauro Francisco Mendonça
Oral Cancer.2018; 2(1-2): 7. CrossRef - Expression and role of EGFR, cyclin�D1 and KRAS in laryngocarcinoma tissues
Xinsheng Lin, Guofeng Wen, Shuangle Wang, Hangui Lu, Chuangwei Li, Xin Wang
Experimental and Therapeutic Medicine.2018;[Epub] CrossRef
- Histopathological variants of head and neck squamous cell carcinomas: A multicenter study in Latin America
- Higher Expression of Toll-like Receptors 3, 7, 8, and 9 in Pityriasis Rosea
- Mostafa Abou El-Ela, Mohamed El-Komy, Rania Abdel Hay, Rehab Hegazy, Amin Sharobim, Laila Rashed, Khalda Amr
- J Pathol Transl Med. 2017;51(2):148-151. Published online February 13, 2017
- DOI: https://doi.org/10.4132/jptm.2016.09.09
- 8,912 View
- 100 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Pityriasis rosea (PR) is a common papulosquamous skin disease in which an infective agent may be implicated. Toll-like receptors (TLRs) play an important role in immune responses and in the pathophysiology of inflammatory skin diseases. Our aim was to determine the possible roles of TLRs 3, 7, 8, and 9 in the pathogenesis of PR. Methods: Twenty-four PR patients and 24 healthy individuals (as controls) were included in this case control study. All recruits were subjected to routine laboratory investigations. Biopsies were obtained from one active PR lesion and from healthy skin of controls for the detection of TLR 3, 7, 8, and 9 gene expression using real-time polymerase chain reaction. Results: This study included 24 patients (8 females and 16 males) with active PR lesions, with a mean age of 28.62 years. Twenty four healthy age- and sex-matched individuals were included as controls (8 females and 16 males, with a mean age of 30.83 years). The results of the routine laboratory tests revealed no significant differences between both groups. Significantly elevated expression of all studied TLRs were detected in PR patients relative to healthy controls (p < .001). Conclusions: TLRs 3, 7, 8, and 9 might be involved in the pathogenesis of PR. -
Citations
Citations to this article as recorded by- Toll-like Receptor-Mediated Immunomodulation of Th1-Type Response Stimulated by Recombinant Antigen of Type 2 Porcine Reproductive and Respiratory Syndrome Virus (PRRSV-2)
Rika Wahyuningtyas, Mei-Li Wu, Wen-Bin Chung, Hso-Chi Chaung, Ko-Tung Chang
Viruses.2023; 15(3): 775. CrossRef - Pityriasis Rosea: An Updated Review
Alexander K.C. Leung, Joseph M. Lam, Kin Fon Leong, Kam Lun Hon
Current Pediatric Reviews.2021; 17(3): 201. CrossRef - Double-blind randomized placebo-controlled trial to evaluate the efficacy and safety of short-course low-dose oral prednisolone in pityriasis rosea
Sidharth Sonthalia, Akshy Kumar, Vijay Zawar, Adity Priya, Pravesh Yadav, Sakshi Srivastava, Atula Gupta
Journal of Dermatological Treatment.2018; 29(6): 617. CrossRef
- Toll-like Receptor-Mediated Immunomodulation of Th1-Type Response Stimulated by Recombinant Antigen of Type 2 Porcine Reproductive and Respiratory Syndrome Virus (PRRSV-2)
- Transformation to Small Cell Lung Cancer of Pulmonary Adenocarcinoma: Clinicopathologic Analysis of Six Cases
- Soomin Ahn, Soo Hyun Hwang, Joungho Han, Yoon-La Choi, Se-Hoon Lee, Jin Seok Ahn, Keunchil Park, Myung-Ju Ahn, Woong-Yang Park
- J Pathol Transl Med. 2016;50(4):258-263. Published online May 10, 2016
- DOI: https://doi.org/10.4132/jptm.2016.04.19
- 14,128 View
- 253 Download
- 54 Web of Science
- 49 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) are considered the first line treatment for a subset of EGFR-mutated non-small cell lung cancer (NSCLC) patients. Although transformation to small cell lung cancer (SCLC) is one of the known mechanisms of resistance to EGFR TKIs, it is not certain whether transformation to SCLC is exclusively found as a mechanism of TKI resistance in EGFR-mutant tumors.
Methods
We identified six patients with primary lung adenocarcinoma that showed transformation to SCLC on second biopsy (n = 401) during a 6-year period. Clinicopathologic information was analyzed and EGFR mutation results were compared between initial and second biopsy samples.
Results
Six patients showed transformation from adenocarcinoma to SCLC, of which four were pure SCLCs and two were combined adenocarcinoma and SCLCs. Clinically, four cases were EGFR-mutant tumors from non-smoking females who underwent TKI treatment, and the EGFR mutation was retained in the transformed SCLC tumors. The remaining two adenocarcinomas were EGFR wild-type, and one of these patients received EGFR TKI treatment.
Conclusions
NSCLC can acquire a neuroendocrine phenotype with or without EGFR TKI treatment. -
Citations
Citations to this article as recorded by- Patients outcomes in lung adenocarcinoma transforming to small-cell lung cancer after tyrosine kinase inhibitor therapy
Shuai Wang, Yongsen Wang, Xuan Wu, Li Yang, Xiaoju Zhang
World Journal of Surgical Oncology.2025;[Epub] CrossRef - Baseline retinoblastoma transcriptional corepressor 1 (Rb1) functional inactivation is a pre-requisite but not sufficient for small-cell histological transformation in epidermal growth factor receptor (EGFR) mutant lung adenocarcinomas post-tyrosine kinas
Aruna Nambirajan, Amber Rathor, Hemavathi Baskarane, Anju GS, Sachin Khurana, Somagattu Sushmitha, Aparna Sharma, Prabhat Singh Malik, Deepali Jain
Virchows Archiv.2025; 487(3): 639. CrossRef - Case Report: Transforming small cell lung cancer: two cases report and literature review
Jinlong Liu, Jing Ai, Lize Zhao, Yimeng Qian, Qingxin Zhao, Chunling Ma, Yu Zhao, Jing Zhao
Frontiers in Oncology.2025;[Epub] CrossRef - Exploration of CT-based discrimination and diagnosis of various pathological types of ground glass nodules in the lungs
Haihui Wu, Xiong Zhang, Zheng Zhong
BMC Medical Imaging.2025;[Epub] CrossRef - Correlation between treatments and outcomes of patients with EGFR-mutated non-small-cell lung cancer that transitioned into small-cell lung cancer: an international retrospective study
C. Catania, S.V. Liu, M. Garassino, A. Delmonte, V. Scotti, F. Cappuzzo, C. Genova, A. Russo, M. Russano, C. Bennati, I. Colantonio, S. Martini, M. Pino, F. Conforti, L. Pala, G. Minuti, F. Citarella, E. Olmetto, A. Esposito, P. Cascetta, A. Di Lello, T.
ESMO Open.2025; 10(7): 105326. CrossRef - TPM3–NTRK1 fusion confers resistance to osimertinib in lung adenocarcinoma: a model in a continuous cell line
Fang Cao, Jiayin Dai, Kun Dong, Zhenli Yang, Yanli Zhu, Changsong Qi, Dongmei Lin, Xiaocui Bian, Yuqin Liu
Human Cell.2025;[Epub] CrossRef - Small cell lung cancer transdifferentiation: not a negligible phenomenon
Lilla Horvath, Kristiina Boettiger, Zsolt Megyesfalvi, Balázs Döme, Clemens Aigner, Anita Horváth-Rózsás, Judit Berta
Current Opinion in Oncology.2025;[Epub] CrossRef - Transformation to small cell lung cancer is irrespective of EGFR and accelerated by SMAD4-mediated ASCL1 transcription independently of RB1 in non-small cell lung cancer
Xi Ding, Min-xing Shi, Di Liu, Jing-xue Cao, Kai-xuan Zhang, Run-dong Zhang, Li-ping Zhang, Kai-xing Ai, Bo Su, Jie Zhang
Cell Communication and Signaling.2024;[Epub] CrossRef - The study of primary and acquired resistance to first-line osimertinib to improve the outcome of EGFR-mutated advanced Non-small cell lung cancer patients: the challenge is open for new therapeutic strategies
Alessandra Ferro, Gian Marco Marinato, Cristiana Mulargiu, Monica Marino, Giulia Pasello, Valentina Guarneri, Laura Bonanno
Critical Reviews in Oncology/Hematology.2024; 196: 104295. CrossRef - Comprehensive molecular and clinical insights into non-small cell lung cancer transformation to small cell lung cancer with an illustrative case report
Kresimir Tomic, Kristina Krpina, Lara Baticic, Miroslav Samarzija, Semir Vranic
Journal of Drug Targeting.2024; 32(5): 499. CrossRef - Transcriptomic Heterogeneity of EGFR-Mutant Non–Small Cell Lung Cancer Evolution Toward Small-Cell Lung Cancer
Songji Oh, Jaemoon Koh, Tae Min Kim, Soyeon Kim, Jeonghwan Youk, Miso Kim, Bhumsuk Keam, Yoon Kyung Jeon, Ja-Lok Ku, Dong-Wan Kim, Doo Hyun Chung, Dae Seog Heo
Clinical Cancer Research.2024; 30(20): 4729. CrossRef - Transformation of lung adenocarcinoma into small cell lung cancer after treatment with epidermal growth factor receptor tyrosine kinase inhibitors
Linwu Kuang, Yangkai Li
Oncology and Translational Medicine.2024; 10(6): 286. CrossRef - Exon-18-EGFR Mutated Transformed Small-Cell Lung Cancer: A Case Report and Literature Review
Nunzio Digiacomo, Tommaso De Pas, Giovanna Rossi, Paola Bossi, Erika Stucchi, Fabio Conforti, Emilia Cocorocchio, Daniele Laszlo, Laura Pala, Emma Zattarin, Chiara Catania
Current Oncology.2023; 30(3): 3494. CrossRef - Current knowledge of small cell lung cancer transformation from non-small cell lung cancer
Giuseppe Giaccone, Yongfeng He
Seminars in Cancer Biology.2023; 94: 1. CrossRef - Targeting the EGFR signaling pathway in cancer therapy: What’s new in 2023?
Sushanta Halder, Soumi Basu, Shobhit P. Lall, Apar K. Ganti, Surinder K. Batra, Parthasarathy Seshacharyulu
Expert Opinion on Therapeutic Targets.2023; 27(4-5): 305. CrossRef - Outcomes in Patients With Lung Adenocarcinoma With Transformation to Small Cell Lung Cancer After EGFR Tyrosine Kinase Inhibitors Resistance: A Systematic Review and Pooled Analysis
Jinhe Xu, Lihuan Xu, Baoshan Wang, Wencui Kong, Ying Chen, Zongyang Yu
Frontiers in Oncology.2022;[Epub] CrossRef - Small cell lung cancer transformation: From pathogenesis to treatment
Xiaomeng Yin, Yueyi Li, Hang Wang, Tingting Jia, Enli Wang, Yuling Luo, Yuhao Wei, Zeyi Qin, Xuelei Ma
Seminars in Cancer Biology.2022; 86: 595. CrossRef - Small Cell Lung Cancer Transformation following Treatment in EGFR-Mutated Non-Small Cell Lung Cancer
Isa Mambetsariev, Leonidas Arvanitis, Jeremy Fricke, Rebecca Pharaon, Angel R. Baroz, Michelle Afkhami, Marianna Koczywas, Erminia Massarelli, Ravi Salgia
Journal of Clinical Medicine.2022; 11(5): 1429. CrossRef - Morphologic-Molecular Transformation of Oncogene Addicted Non-Small Cell Lung Cancer
Fiorella Calabrese, Federica Pezzuto, Francesca Lunardi, Francesco Fortarezza, Sofia-Eleni Tzorakoleftheraki, Maria Vittoria Resi, Mariaenrica Tiné, Giulia Pasello, Paul Hofman
International Journal of Molecular Sciences.2022; 23(8): 4164. CrossRef - Genomic and Gene Expression Studies Helped to Define the Heterogeneity of Small-Cell Lung Cancer and Other Lung Neuroendocrine Tumors and to Identify New Therapeutic Targets
Ugo Testa, Elvira Pelosi, Germana Castelli
Onco.2022; 2(3): 186. CrossRef - Neuroendocrine transformation from EGFR/ALK-wild type or TKI-naïve non-small cell lung cancer: An under-recognized phenomenon
Xiao Chu, Yuyin Xu, Ye Li, Yue Zhou, Li Chu, Xi Yang, Jianjiao Ni, Yida Li, Tiantian Guo, Zhiqin Zheng, Qiang Zheng, Qianlan Yao, Yuan Li, Xiaoyan Zhou, Zhengfei Zhu
Lung Cancer.2022; 169: 22. CrossRef - Three Third-Generation Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors in Non-Small Cell Lung Cancer: Similarities and Differences
Ling Chen, Yangqingqing Zhou, Chaosheng Gan, XiaoLi Wang, Yihui Liu, Chunhui Dong, Ruiyuan He, Jin Yang
Cancer Investigation.2022; 40(7): 590. CrossRef - Histomorphological transformation from non-small cell lung carcinoma to small cell lung carcinoma after targeted therapy or immunotherapy: A report of two cases
Hao Liu, Li-Hong Chen, Zhi-Hui Zhang, Ning Wang, Si-Hui Zhuang, Hao Chen, Jin Du, Li-Juan Pang, Yan Qi
Frontiers in Oncology.2022;[Epub] CrossRef - Impressive response to dabrafenib, trametinib, and osimertinib in a metastatic EGFR-mutant/BRAF V600E lung adenocarcinoma patient
Maurício Fernando Silva Almeida Ribeiro, Franciele Hinterholz Knebel, Fabiana Bettoni, Rodrigo Saddi, Karina Perez Sacardo, Felipe Sales Nogueira Amorim Canedo, João Victor Machado Alessi, Andrea Kazumi Shimada, José Flávio Gomes Marin, Anamaria Aranha Ca
npj Precision Oncology.2021;[Epub] CrossRef - Histological transformation of non-small cell lung cancer: Clinical analysis of nine cases
Cai-Bao Jin, Ling Yang
World Journal of Clinical Cases.2021; 9(18): 4617. CrossRef - Lamellarin 14, a derivative of marine alkaloids, inhibits the T790M/C797S mutant epidermal growth factor receptor
Naoyuki Nishiya, Yusuke Oku, Chie Ishikawa, Tsutomu Fukuda, Shingo Dan, Tetsuo Mashima, Masaru Ushijima, Yoko Furukawa, Yuka Sasaki, Keishi Otsu, Tomoko Sakyo, Masanori Abe, Honami Yonezawa, Fumito Ishibashi, Masaaki Matsuura, Akihiro Tomida, Hiroyuki Sei
Cancer Science.2021; 112(5): 1963. CrossRef - Case Report: Transformation From Non-Small Cell Lung Cancer to Small Cell Lung Cancer During Anti-PD-1 Therapy: A Report of Two Cases
Qian Shen, Jingjing Qu, Lingyan Sheng, Qiqi Gao, Jianying Zhou
Frontiers in Oncology.2021;[Epub] CrossRef - Exploring the resistance mechanisms of second-line osimertinib and their prognostic implications using next-generation sequencing in patients with non-small-cell lung cancer
Kyoungmin Lee, Deokhoon Kim, Shinkyo Yoon, Dae Ho Lee, Sang-We Kim
European Journal of Cancer.2021; 148: 202. CrossRef - Comprehensive analysis of treatment modes and clinical outcomes of small cell lung cancer transformed from epidermal growth factor receptor mutant lung adenocarcinoma
Shouzheng Wang, Tongji Xie, Xuezhi Hao, Yan Wang, Xingsheng Hu, Lin Wang, Yan Li, Junling Li, Puyuan Xing
Thoracic Cancer.2021; 12(19): 2585. CrossRef - EGFR-Mutant SCLC Exhibits Heterogeneous Phenotypes and Resistance to Common Antineoplastic Drugs
Chih-An Lin, Sung-Liang Yu, Hsuan-Yu Chen, Huei-Wen Chen, Shr-Uen Lin, Chia-Ching Chang, Chong-Jen Yu, Pan-Chyr Yang, Chao-Chi Ho
Journal of Thoracic Oncology.2019; 14(3): 513. CrossRef - The clinicopathologic of pulmonary adenocarcinoma transformation to small cell lung cancer
Haiyan Yang, Li Liu, Chunhua Zhou, Yi Xiong, Yijuan Hu, Nong Yang, Jingjing Qu
Medicine.2019; 98(12): e14893. CrossRef - Chemistry and pharmacological diversity of quinoxaline motifs as anticancer agents
Olayinka O. Ajani, Martins T. Nlebemuo, Joseph A. Adekoya, Kehinde O. Ogunniran, Tolutope O. Siyanbola, Christiana O. Ajanaku
Acta Pharmaceutica.2019; 69(2): 177. CrossRef - Resistance to EGFR inhibitors in non-small cell lung cancer: Clinical management and future perspectives
Chiara Tomasello, Cinzia Baldessari, Martina Napolitano, Giulia Orsi, Giulia Grizzi, Federica Bertolini, Fausto Barbieri, Stefano Cascinu
Critical Reviews in Oncology/Hematology.2018; 123: 149. CrossRef - Small cell lung cancer transformation from EGFR-mutated lung adenocarcinoma: A case report and literatures review
Yangyang Liu
Cancer Biology & Therapy.2018; 19(6): 445. CrossRef - Anaplastic lymphoma kinase (ALK)-expressing Lung Adenocarcinoma with Combined Neuroendocrine Component or Neuroendocrine Transformation: Implications for Neuroendocrine Transformation and Response to ALK-tyrosine Kinase Inhibitors
Jongmin Sim, Hyunjin Kim, Jiyeon Hyeon, Yoon-La Choi, Joungho Han
Journal of Korean Medical Science.2018;[Epub] CrossRef - Assessment of Resistance Mechanisms and Clinical Implications in Patients WithEGFRT790M–Positive Lung Cancer and Acquired Resistance to Osimertinib
Geoffrey R. Oxnard, Yuebi Hu, Kathryn F. Mileham, Hatim Husain, Daniel B. Costa, Philip Tracy, Nora Feeney, Lynette M. Sholl, Suzanne E. Dahlberg, Amanda J. Redig, David J. Kwiatkowski, Michael S. Rabin, Cloud P. Paweletz, Kenneth S. Thress, Pasi A. Jänne
JAMA Oncology.2018; 4(11): 1527. CrossRef - Clinicopathological and genomic comparisons between different histologic components in combined small cell lung cancer and non-small cell lung cancer
Mong-Wei Lin, Kang-Yi Su, Te-Jen Su, Chia-Ching Chang, Jing-Wei Lin, Yi-Hsuan Lee, Sung-Liang Yu, Jin-Shing Chen, Min-Shu Hsieh
Lung Cancer.2018; 125: 282. CrossRef - Transformation to small‑cell lung cancer following treatment with icotinib in a patient with lung adenocarcinoma
Hongyang Lu, Bo Chen, Jing Qin, Fajun Xie, Na Han, Zhiyu Huang
Oncology Letters.2018;[Epub] CrossRef - Histological transformation of adenocarcinoma to small cell carcinoma lung as a rare mechanism of resistance to epidermal growth factor receptor-tyrosine kinase inhibitors: Report of a case with review of literature
Monalisa Hui, ShantveerG Uppin, BalaJoseph Stalin, G Sadashivudu
Lung India.2018; 35(2): 160. CrossRef - A rare case of squamous cell carcinoma lung with multiple locoregional recurrences and histological transformation
Ram Niwas, Shibdas Chakrabarti, Viswesvaran Balasubramanian, ManasKamal Sen, JagdishChander Suri
Lung India.2018; 35(6): 511. CrossRef - Small cell lung cancer transformation during immunotherapy with nivolumab: A case report
Takuma Imakita, Kohei Fujita, Osamu Kanai, Tsuyoshi Terashima, Tadashi Mio
Respiratory Medicine Case Reports.2017; 21: 52. CrossRef - Pulmonary neuroendocrine tumor in a female wolf (Canis lupus lupus)
Ayako SHIRAKI, Toshinori YOSHIDA, Masahi KAWASHIMA, Hirotada MURAYAMA, Rei NAGAHARA, Nanao ITO, Makoto SHIBUTANI
Journal of Veterinary Medical Science.2017; 79(3): 588. CrossRef - Secondary biopsy of non‐oncogenic‐driven lung cancer may reveal a clinically sensible histologic change. A brief report of two paradigmatic cases
Maria C. Mengoli, Giulia Orsi, Filippo Lococo, Giulia Grizzi, Fausto Barbieri, Federica Bertolini, Giulio Rossi, Silvia Novello
Thoracic Cancer.2017; 8(4): 359. CrossRef - Small-cell lung cancer in never smokers: The clinicopathological features including the prognosis
Masahiro Yamasaki, Naomi Saito, Wakako Daido, Sayaka Ishiyama, Naoko Deguchi, Masaya Taniwaki, Akio Sakatani, Megumu Fujihara, Nobuyuki Ohashi, Ken-ichi Arita
Cancer Treatment and Research Communications.2017; 12: 1. CrossRef - Clonal History and Genetic Predictors of Transformation Into Small-Cell Carcinomas From Lung Adenocarcinomas
June-Koo Lee, Junehawk Lee, Sehui Kim, Soyeon Kim, Jeonghwan Youk, Seongyeol Park, Yohan An, Bhumsuk Keam, Dong-Wan Kim, Dae Seog Heo, Young Tae Kim, Jin-Soo Kim, Se Hyun Kim, Jong Seok Lee, Se-Hoon Lee, Keunchil Park, Ja-Lok Ku, Yoon Kyung Jeon, Doo Hyun
Journal of Clinical Oncology.2017; 35(26): 3065. CrossRef - Australian recommendations for EGFR T790M testing in advanced non-small cell lung cancer
Thomas John, Jeffrey J Bowden, Stephen Clarke, Stephen B Fox, Kerryn Garrett, Keith Horwood, Christos S Karapetis
Asia-Pacific Journal of Clinical Oncology.2017; 13(4): 296. CrossRef - Metastatic Squamous Cell Carcinoma from Lung Adenocarcinoma after Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor Therapy
Hyung Kyu Park, Youjeong Seo, Yoon-La Choi, Myung-Ju Ahn, Joungho Han
Journal of Pathology and Translational Medicine.2017; 51(4): 441. CrossRef - Sequential occurrence of small cell and non-small lung cancer in a male patient: Is it a transformation?
Ahsan Wahab, Kavitha Kesari, Siddique Chaudhary, Mahin Khan, Hafiz Khan, Susan Smith, Yanis Boumber
Cancer Biology & Therapy.2017; 18(12): 940. CrossRef - The expression of S100B protein in serum of patients with brain metastases from small-cell lung cancer and its clinical significance
Shanling Mu, Hong Ma, Jun Shi, Dezhi Zhen
Oncology Letters.2017;[Epub] CrossRef
- Patients outcomes in lung adenocarcinoma transforming to small-cell lung cancer after tyrosine kinase inhibitor therapy
- Non-small Cell Lung Cancer with Concomitant EGFR, KRAS, and ALK Mutation: Clinicopathologic Features of 12 Cases
- Taebum Lee, Boram Lee, Yoon-La Choi, Joungho Han, Myung-Ju Ahn, Sang-Won Um
- J Pathol Transl Med. 2016;50(3):197-203. Published online April 18, 2016
- DOI: https://doi.org/10.4132/jptm.2016.03.09
- 21,998 View
- 319 Download
- 72 Web of Science
- 65 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Although epidermal growth factor receptor (EGFR), v-Ki-ras2 Kirsten rat sarcoma viral oncogene (KRAS), and anaplastic lymphoma kinase (ALK) mutations in non-small cell lung cancer (NSCLC) were thought to be mutually exclusive, some tumors harbor concomitant mutations. Discovering a driver mutation on the basis of morphologic features and therapeutic responses with mutation analysis can be used to understand pathogenesis and predict resistance in targeted therapy.
Methods
In 6,637 patients with NSCLC, 12 patients who had concomitant mutations were selected and clinicopathologic features were reviewed. Clinical characteristics included sex, age, smoking history, previous treatment, and targeted therapy with response and disease-free survival. Histologic features included dominant patterns, nuclear and cytoplasmic features.
Results
All patients were diagnosed with adenocarcinoma and had an EGFR mutation. Six patients had concomitant KRAS mutations and the other six had ALK mutations. Five of six EGFR-KRAS mutation patients showed papillary and acinar histologic patterns with hobnail cells. Three of six received EGFR tyrosine kinase inhibitor (TKI) and showed partial response for 7–29 months. All six EGFR-ALK mutation patients showed solid or cribriform patterns and three had signet ring cells. Five of six EGFR-ALK mutation patients received EGFR TKI and/or ALK inhibitor and four showed partial response or stable disease, except for one patient who had acquired an EGFR mutation.
Conclusions
EGFR and ALK mutations play an important role as driver mutations in double mutated NSCLC, and morphologic analysis can be used to predict treatment response. -
Citations
Citations to this article as recorded by- Integrative multi-omics machine learning reveals novel driver genes associations in lung adenocarcinoma
Fei Yuan, FeiMing Huang, Xiaoyu Cao, Yu-Hang Zhang, KaiYan Feng, YuSheng Bao, Tao Huang, Yu-Dong Cai
Biochimica et Biophysica Acta (BBA) - Proteins and Proteomics.2026; 1874(1): 141113. CrossRef - Ensartinib for EML4-ALK-positive lung adenocarcinoma with comorbid mutations in TP53, EGFR, and ERBB2: a case report
Xiaoqing Huang, Lingxian Zhou, Jianyong Xia, Haifeng Jian, Jinji Liu, Yunying Huang, Qingsheng Chen
Frontiers in Oncology.2025;[Epub] CrossRef - Dual EGFR L858R and KRAS G12A Mutations in Lung Adenocarcinoma: A Rare Case Report and Literature Review
Gang Wei, Jun Tang, Huaiwen Wang, Dongdong Zhang
Pharmacogenomics and Personalized Medicine.2025; Volume 18: 189. CrossRef -
Artificial Intelligence in Lung Cancer Imaging: From Data to Therapy
Michaela Cellina, Giuseppe De Padova, Nazarena Caldarelli, Dario Libri, Maurizio Cè, Carlo Martinenghi, Marco Alì, Sergio Papa, Gianpaolo Carrafiello
Critical Reviews™ in Oncogenesis.2024; 29(2): 1. CrossRef - Artificial Intelligence for Cardiothoracic Imaging: Overview of Current and Emerging Applications
Bruno Hochhegger, Romulo Pasini, Alysson Roncally Carvalho, Rosana Rodrigues, Stephan Altmayer, Leonardo Kayat Bittencourt, Edson Marchiori, Reza Forghani
Seminars in Roentgenology.2023; 58(2): 184. CrossRef - Genomic Landscape of Primary Resistance to Osimertinib Among Hispanic Patients with EGFR-Mutant Non-Small Cell Lung Cancer (NSCLC): Results of an Observational Longitudinal Cohort Study
Diego F. Chamorro, Andrés F. Cardona, July Rodríguez, Alejandro Ruiz-Patiño, Oscar Arrieta, Darwin A. Moreno-Pérez, Leonardo Rojas, Zyanya Lucia Zatarain-Barrón, Dora V. Ardila, Lucia Viola, Gonzalo Recondo, Juan B. Blaquier, Claudio Martín, Luis Raez, Su
Targeted Oncology.2023; 18(3): 425. CrossRef - Histone deacetylase inhibitor belinostat regulates metabolic reprogramming in killing KRAS‐mutant human lung cancer cells
Rebecca M. Peter, Md. Shahid Sarwar, Sarah Z. Mostafa, Yujue Wang, Xiaoyang Su, Ah‐Ng Kong
Molecular Carcinogenesis.2023; 62(8): 1136. CrossRef - Differential Distribution of Brain Metastases from Non-Small Cell Lung Cancer Based on Mutation Status
Bihong T. Chen, Taihao Jin, Ningrong Ye, Sean W. Chen, Russell C. Rockne, Stephanie Yoon, Isa Mambetsariev, Ebenezer Daniel, Ravi Salgia
Brain Sciences.2023; 13(7): 1057. CrossRef - Clinicopathological features and prognostic significance of pulmonary adenocarcinoma with signet ring cell components: meta-analysis and SEER analysis
Yang Tan, Ying-he Huang, Jia-wen Xue, Rui Zhang, Run Liu, Yan Wang, Zhen-Bo Feng
Clinical and Experimental Medicine.2023; 23(8): 4341. CrossRef - Ganoderma microsporum immunomodulatory protein as an extracellular epidermal growth factor receptor (EGFR) degrader for suppressing EGFR-positive lung cancer cells
Wei-Jyun Hua, Hsin Yeh, Zhi-Hu Lin, Ai-Jung Tseng, Li-Chen Huang, Wei-Lun Qiu, Tsung-Hsi Tu, Ding-Han Wang, Wei-Hung Hsu, Wei-Lun Hwang, Tung-Yi Lin
Cancer Letters.2023; 578: 216458. CrossRef - Next generation sequencing for detection of EGFR alterations in NSCLC: is more better?
Ullas Batra, Shrinidhi Nathany, Mansi Sharma, Parveen Jain, Anurag Mehta
Journal of Clinical Pathology.2022; 75(3): 164. CrossRef - Enkurin domain containing 1 (ENKD1) regulates the proliferation, migration and invasion of non‐small cell lung cancer cells
Ting Song, Peng Zhou, Chunjiao Sun, Na He, Haixia Li, Jie Ran, Jun Zhou, Yue Wu, Min Liu
Asia-Pacific Journal of Clinical Oncology.2022;[Epub] CrossRef - Targeting Mutant Kirsten Rat Sarcoma Viral Oncogene Homolog in Non-Small Cell Lung Cancer: Current Difficulties, Integrative Treatments and Future Perspectives
Jia-Xin Li, Run-Ze Li, Lin-Rui Ma, Peng Wang, Dong-Han Xu, Jie Huang, Li-Qi Li, Ling Tang, Ying Xie, Elaine Lai-Han Leung, Pei-Yu Yan
Frontiers in Pharmacology.2022;[Epub] CrossRef - Histone H3K9 methyltransferase SETDB1 augments invadopodia formation to promote tumor metastasis
Shuhei Ueshima, Jia Fang
Oncogene.2022; 41(24): 3370. CrossRef - ESMO expert consensus statements on the management of EGFR mutant non-small-cell lung cancer
A. Passaro, N. Leighl, F. Blackhall, S. Popat, K. Kerr, M.J. Ahn, M.E. Arcila, O. Arrieta, D. Planchard, F. de Marinis, A.M. Dingemans, R. Dziadziuszko, C. Faivre-Finn, J. Feldman, E. Felip, G. Curigliano, R. Herbst, P.A. Jänne, T. John, T. Mitsudomi, T.
Annals of Oncology.2022; 33(5): 466. CrossRef - Molecular Targets in Lung Cancer: Study of the Evolution of Biomarkers Associated with Treatment with Tyrosine Kinase Inhibitors—Has NF1 Tumor Suppressor a Key Role in Acquired Resistance?
Begoña O. Alen, Lara S. Estévez-Pérez, María Teresa Hermida-Romero, Ana Reguera-Arias, Rosario García-Campelo, Mercedes de la Torre-Bravos, Ángel Concha
Cancers.2022; 14(14): 3323. CrossRef - Analytical and clinical validation of a custom 15-gene next-generation sequencing panel for the evaluation of circulating tumor DNA mutations in patients with advanced non-small-cell lung cancer
Yock Ping Chow, Norziha Zainul Abidin, Ken Siong Kow, Lye Mun Tho, Chieh Lee Wong, Rama Krishna Kancha
PLOS ONE.2022; 17(10): e0276161. CrossRef - Potential Therapeutic Strategy for EGFR-Mutant Lung Cancer With Concomitant EML4-ALK Rearrangement—Combination of EGFR Tyrosine Kinase Inhibitors and ALK Inhibitors
Ming-Hung Huang, Jih-Hsiang Lee, Pei-Shan Hung, James Chih-Hsin Yang
JTO Clinical and Research Reports.2022; 3(11): 100405. CrossRef - Artificial Intelligence in Lung Cancer Imaging: Unfolding the Future
Michaela Cellina, Maurizio Cè, Giovanni Irmici, Velio Ascenti, Natallia Khenkina, Marco Toto-Brocchi, Carlo Martinenghi, Sergio Papa, Gianpaolo Carrafiello
Diagnostics.2022; 12(11): 2644. CrossRef - A single center analysis of first-line treatment in advanced KRAS mutant non-small cell lung cancer: real-world practice
Yanxia Liu, Yuan Gao, Ying Wang, Cong Zhao, Zhiyun Zhang, Baolan Li, Tongmei Zhang
BMC Cancer.2022;[Epub] CrossRef - High frequency of KRAS and EGFR mutation profiles in BRAF-negative thyroid carcinomas in Indonesia
Didik Setyo Heriyanto, Vincent Laiman, Nikko Vanda Limantara, Widyan Putra Anantawikrama, Fara Silvia Yuliani, Rita Cempaka, Sumadi Lukman Anwar
BMC Research Notes.2022;[Epub] CrossRef - Kirsten Rat Sarcoma Mutation in South Indians with Non-Small Lung Cancer
Gautam Balaram, Renjan Thomas, Suhas N. Ghorpade, Prarthana V. Kowsik, Baby Dharman, Yogesh Shivakumar, Shekar Patil, Satheesh Chiradoni Thungappa, HP Shashidhara, Somorat Bhattacharjee, Sridhar Papaiah Susheela, Radheshyam Naik, Srinivas Belagutty Jayapp
Journal of Precision Oncology.2022; 2(1): 3. CrossRef - Targeted next-generation sequencing for cancer-associated gene mutation and copy number detection in 206 patients with non–small-cell lung cancer
Songbai Zheng, Xiaodan Wang, Ying Fu, Beibei Li, Jianhua Xu, Haifang Wang, Zhen Huang, Hui Xu, Yurong Qiu, Yaozhou Shi, Kui Li
Bioengineered.2021; 12(1): 791. CrossRef - How mathematical modeling could contribute to the quantification of metastatic tumor burden under therapy: insights in immunotherapeutic treatment of non-small cell lung cancer
Pirmin Schlicke, Christina Kuttler, Christian Schumann
Theoretical Biology and Medical Modelling.2021;[Epub] CrossRef - A case of concomitant EGFR/ALK alteration against a mutated EGFR background in early-stage lung adenocarcinoma
Ki-Chang Lee, Jiwon Koh, Doo Hyun Chung, Yoon Kyung Jeon
Journal of Pathology and Translational Medicine.2021; 55(2): 139. CrossRef - Malfeasance of KRAS mutations in carcinogenesis
Rupal Tripathi, Shrinidhi Nathany, Anurag Mehta, Ullas Batra, Sakshi Mattoo, Mansi Sharma
Clinical and Experimental Medicine.2021; 21(3): 439. CrossRef - Detection of Low-Frequency KRAS Mutations in cfDNA From EGFR-Mutated NSCLC Patients After First-Line EGFR Tyrosine Kinase Inhibitors
Giorgia Nardo, Jessica Carlet, Ludovica Marra, Laura Bonanno, Alice Boscolo, Alessandro Dal Maso, Andrea Boscolo Bragadin, Stefano Indraccolo, Elisabetta Zulato
Frontiers in Oncology.2021;[Epub] CrossRef - Non-Small Cell Lung Cancer Harboring Concurrent EGFR Genomic Alterations: A Systematic Review and Critical Appraisal of the Double Dilemma
Valerio Gristina, Maria La Mantia, Antonio Galvano, Sofia Cutaia, Nadia Barraco, Marta Castiglia, Alessandro Perez, Marco Bono, Federica Iacono, Martina Greco, Katia Calcara, Valentina Calò, Sergio Rizzo, Lorena Incorvaia, Maria Chiara Lisanti, Giulia San
Journal of Molecular Pathology.2021; 2(2): 173. CrossRef - Testing for EGFR Mutations and ALK Rearrangements in Advanced Non-Small-Cell Lung Cancer: Considerations for Countries in Emerging Markets
Mercedes L Dalurzo, Alejandro Avilés-Salas, Fernando Augusto Soares, Yingyong Hou, Yuan Li, Anna Stroganova, Büge Öz, Arif Abdillah, Hui Wan, Yoon-La Choi
OncoTargets and Therapy.2021; Volume 14: 4671. CrossRef - Untangling the KRAS mutated lung cancer subsets and its therapeutic implications
Kulshrestha Ritu, Pawan Kumar, Amit Singh, K. Nupur, Sonam Spalgias, Parul Mrigpuri, Rajkumar
Molecular Biomedicine.2021;[Epub] CrossRef - Lorlatinib Induces Durable Disease Stabilization in a Pancreatic Cancer Patient with a ROS1 p.L1950F Mutation: Case Report
Janna-Lisa Velthaus, Peter Iglauer, Ronald Simon, Carsten Bokemeyer, Peter Bannas, Niklas Beumer, Charles D. Imbusch, Eray Goekkurt, Sonja Loges
Oncology Research and Treatment.2021; 44(9): 495. CrossRef - Proteasome-dependent degradation of Smad7 is critical for lung cancer metastasis
Lu Tong, Shihui Shen, Quan Huang, Junjiang Fu, Tianzhen Wang, Linian Pan, Pei Zhang, Geng Chen, Tingmei Huang, Ke Li, Qingwu Liu, Shaofang Xie, Xiao Yang, Robb E. Moses, Xiaotao Li, Lei Li
Cell Death & Differentiation.2020; 27(6): 1795. CrossRef - Circulating Cell-Free Dna As A Diagnostic and Prognostic Biomarker for Non-Small-Cell Lung Cancer: A Systematic Review and Meta-Analysis
Zhoumiao Chen, Huiwen Miao, Qingxin Zeng, Shaohua Xu, Zhao Chen, Kai Liu
Biomarkers in Medicine.2020; 14(7): 587. CrossRef - Influence of EGFR-activating mutations on sensitivity to tyrosine kinase inhibitors in a KRAS mutant non-small cell lung cancer cell line
Yoshinori Tsukumo, Mikihiko Naito, Takayoshi Suzuki, Srikumar Chellappan
PLOS ONE.2020; 15(3): e0229712. CrossRef - KRAS oncogene may be another target conquered in non‐small cell lung cancer (NSCLC)
Hanxiao Chen, Jun Zhao
Thoracic Cancer.2020; 11(12): 3425. CrossRef - Epidemiologic Features of NSCLC Gene Alterations in Hispanic Patients from Puerto Rico
Ruifang Zheng, Zhiwei Yin, Albert Alhatem, Derek Lyle, Bei You, Andrew S. Jiang, Dongfang Liu, Zsolt Jobbagy, Qing Wang, Seena Aisner, Jie-Gen Jiang
Cancers.2020; 12(12): 3492. CrossRef - Comprehensive pancancer genomic analysis reveals (RTK)-RAS-RAF-MEK as a key dysregulated pathway in cancer: Its clinical implications
Robin Imperial, Omer M Toor, Arif Hussain, Janakiraman Subramanian, Ashiq Masood
Seminars in Cancer Biology.2019; 54: 14. CrossRef - Epidermal growth factor receptor (EGFR), KRAS, and BRAF mutations in lung adenocarcinomas: A study from India
Varsha Singh, Prerna Guleria, Prabhat Singh Malik, Anant Mohan, Sanjay Thulkar, R M Pandey, Kalpana Luthra, Sudheer Arava, Ruma Ray, Deepali Jain
Current Problems in Cancer.2019; 43(5): 391. CrossRef - Clinical Validation of Coexisting Activating Mutations Within EGFR, Mitogen-Activated Protein Kinase, and Phosphatidylinositol 3-Kinase Pathways in Lung Cancers
Federico De Marchi, Lisa Haley, Henderson Fryer, Junaid Ibrahim, Katie Beierl, Gang Zheng, Christopher D. Gocke, James R. Eshleman, Deborah Belchis, Peter Illei, Ming-Tseh Lin
Archives of Pathology & Laboratory Medicine.2019; 143(2): 174. CrossRef - A sequential Monte Carlo algorithm for inference of subclonal structure in cancer
Oyetunji E. Ogundijo, Kaiyi Zhu, Xiaodong Wang, Dimitris Anastassiou, Xiang Li
PLOS ONE.2019; 14(1): e0211213. CrossRef - The Presence of Concomitant Mutations Affects the Activity of EGFR Tyrosine Kinase Inhibitors in EGFR-Mutant Non-Small Cell Lung Cancer (NSCLC) Patients
Anna Rachiglio, Francesca Fenizia, Maria Piccirillo, Domenico Galetta, Lucio Crinò, Bruno Vincenzi, Emiddio Barletta, Carmine Pinto, Francesco Ferraù, Matilde Lambiase, Agnese Montanino, Cristin Roma, Vienna Ludovini, Elisabetta Montagna, Antonella De Luc
Cancers.2019; 11(3): 341. CrossRef - Concurrent Driver Gene Mutations as Negative Predictive Factors in Epidermal Growth Factor Receptor-Positive Non-Small Cell Lung Cancer
Minjiang Chen, Yan Xu, Jing Zhao, Wei Zhong, Li Zhang, Yalan Bi, Mengzhao Wang
EBioMedicine.2019; 42: 304. CrossRef - Anaplastic Lymphoma Kinase (ALK)-positive Tumors
Rohan Gupta, Idoroenyi Amanam, Syed Rahmanuddin, Isa Mambetsariev, Yingyu Wang, Charity Huang, Karen Reckamp, Lalit Vora, Ravi Salgia
American Journal of Clinical Oncology.2019; 42(4): 337. CrossRef - Clinical features and therapeutic options in non‐small cell lung cancer patients with concomitant mutations of EGFR, ALK, ROS1, KRAS or BRAF
Xibin Zhuang, Chao Zhao, Jiayu Li, Chunxia Su, Xiaoxia Chen, Shengxiang Ren, Xuefei Li, Caicun Zhou
Cancer Medicine.2019; 8(6): 2858. CrossRef - Intrinsic Resistance to EGFR-Tyrosine Kinase Inhibitors in EGFR-Mutant Non-Small Cell Lung Cancer: Differences and Similarities with Acquired Resistance
Eric Santoni-Rugiu, Linea C. Melchior, Edyta M. Urbanska, Jan N. Jakobsen, Karin de Stricker, Morten Grauslund, Jens B. Sørensen
Cancers.2019; 11(7): 923. CrossRef - Clinical outcome of treatment of metastatic non-small cell lung cancer in patients harboring uncommon EGFR mutation
J. Chantharasamee, N. Poungvarin, P. Danchaivijitr, S. Techawatanawanna
BMC Cancer.2019;[Epub] CrossRef - Deregulated lncRNA expression profile in the mouse lung adenocarcinomas with KRAS‐G12D mutation and P53 knockout
Meiqin Zhang, Nan Jiang, Renjie Cui, Sichen Du, Huayuan Ou, Tinglan Chen, Runsheng Ge, Duan Ma, Jin Zhang
Journal of Cellular and Molecular Medicine.2019; 23(10): 6978. CrossRef - Open-Sourced CIViC Annotation Pipeline to Identify and Annotate Clinically Relevant Variants Using Single-Molecule Molecular Inversion Probes
Erica K. Barnell, Adam Waalkes, Matt C. Mosior, Kelsi Penewit, Kelsy C. Cotto, Arpad M. Danos, Lana M. Sheta, Katie M. Campbell, Kilannin Krysiak, Damian Rieke, Nicholas C. Spies, Zachary L. Skidmore, Colin C. Pritchard, Todd A. Fehniger, Ravindra Uppalur
JCO Clinical Cancer Informatics.2019; (3): 1. CrossRef - EGFR, KRAS, BRAF, ALK, and cMET genetic alterations in 1440 Sardinian patients with lung adenocarcinoma
Maria Colombino, Panagiotis Paliogiannis, Antonio Cossu, Davide Adriano Santeufemia, Maria Cristina Sini, Milena Casula, Grazia Palomba, Antonella Manca, Marina Pisano, Valentina Doneddu, Giuseppe Palmieri
BMC Pulmonary Medicine.2019;[Epub] CrossRef - Concomitant Presence of EGFR and ALK Fusion Gene Mutation in Adenocarcinoma of Lung: A Case Report and Review of the Literature
Nishitha Thumallapally, Hana Yu, Mohammad Farhan, Uroosa Ibrahim, Maricel Odiami
Journal of Pharmacy Practice.2018; 31(2): 244. CrossRef - Double Trouble: A Case Series on Concomitant Genetic Aberrations in NSCLC
Nele Van Der Steen, Yves Mentens, Marc Ramael, Leticia G. Leon, Paul Germonpré, Jose Ferri, David R. Gandara, Elisa Giovannetti, Godefridus J. Peters, Patrick Pauwels, Christian Rolfo
Clinical Lung Cancer.2018; 19(1): 35. CrossRef - KRAS oncogene in non-small cell lung cancer: clinical perspectives on the treatment of an old target
Marta Román, Iosune Baraibar, Inés López, Ernest Nadal, Christian Rolfo, Silvestre Vicent, Ignacio Gil-Bazo
Molecular Cancer.2018;[Epub] CrossRef - Pulmonary Adenocarcinoma, Harboring Both an EGFR Mutation and ALK Rearrangement, Presenting a Stable Disease to Erlotinib and a Partial Response to Alectinib
Akira Yokoyama, Atsuhisa Tamura, Kazuko Miyakawa, Kei Kusaka, Masahiro Shimada, Takashi Hirose, Hirotoshi Matsui, Masashi Kitani, Akira Hebisawa, Ken Ohta
Internal Medicine.2018; 57(16): 2377. CrossRef - Long-term survival with erlotinib in advanced lung adenocarcinoma harboring synchronous EGFR G719S and KRAS G12C mutations
Biagio Ricciuti, Sara Baglivo, Vienna Ludovini, Angelo Sidoni, Giulio Metro, Marta Brambilla, Annamaria Siggillino, Maria Sole Reda, Alberto Rebonato, Daniele Maiettini, Rita Chiari
Lung Cancer.2018; 120: 70. CrossRef - Concomitant driver mutations in advanced EGFR-mutated non-small-cell lung cancer and their impact on erlotinib treatment
Jan Nyrop Jakobsen, Eric Santoni-Rugiu, Morten Grauslund, Linea Melchior, Jens Benn Sørensen
Oncotarget.2018; 9(40): 26195. CrossRef - Implications of KRAS mutations in acquired resistance to treatment in NSCLC
Marzia Del Re, Eleonora Rofi, Giuliana Restante, Stefania Crucitta, Elena Arrigoni, Stefano Fogli, Massimo Di Maio, Iacopo Petrini, Romano Danesi
Oncotarget.2018; 9(5): 6630. CrossRef - Alk Immunohistochemistry is Highly Sensitive and Specific for the Detection of Alk Translocated Lung Adenocarcinomas: Lessons from An Audit of Lung Cancer Molecular Testing
YC Kheng, K Walsh, L Williams, WA Wallace, DJ Harrison, A Oniscu
Journal of the Royal College of Physicians of Edinburgh.2018; 48(1): 20. CrossRef - Targeting KRAS mutated non-small cell lung cancer: A history of failures and a future of hope for a diverse entity
Alexios Matikas, Dimitrios Mistriotis, Vasilios Georgoulias, Athanasios Kotsakis
Critical Reviews in Oncology/Hematology.2017; 110: 1. CrossRef - Clinical Outcome of ALK -Positive Non–Small Cell Lung Cancer (NSCLC) Patients with De Novo EGFR or KRAS Co-Mutations Receiving Tyrosine Kinase Inhibitors (TKIs)
Sabine Schmid, Oliver Gautschi, Sacha Rothschild, Michael Mark, Patrizia Froesch, Dirk Klingbiel, Hermann Reichegger, Wolfram Jochum, Joachim Diebold, Martin Früh
Journal of Thoracic Oncology.2017; 12(4): 681. CrossRef - EGFR and KRAS molecular genotyping for pulmonary carcinomas: Feasibility of a simple and rapid technique implementable in any department of pathology
Vincent Thomas De Montpréville, Maria-Rosa Ghigna, Ludovic Lacroix, Antoinette Lemoine, Benjamin Besse, Olaf Mercier, Élie Fadel, Peter Dorfmuller, Thierry Le Chevalier
Pathology - Research and Practice.2017; 213(7): 793. CrossRef - MET Exon 14 Skipping Mutations in Lung Adenocarcinoma: Clinicopathologic Implications and Prognostic Values
Geun Dong Lee, Seung Eun Lee, Doo-Yi Oh, Dan-bi Yu, Hae Min Jeong, Jooseok Kim, Sungyoul Hong, Hun Soon Jung, Ensel Oh, Ji-Young Song, Mi-Sook Lee, Mingi Kim, Kyungsoo Jung, Jhingook Kim, Young Kee Shin, Yoon-La Choi, Hyeong Ryul Kim
Journal of Thoracic Oncology.2017; 12(8): 1233. CrossRef - Non-Small-Cell Lung Cancer (NSCLC) Harboring ALK Translocations: Clinical Characteristics and Management in a Real-Life Setting: a French Retrospective Analysis (GFPC 02–14 Study)
Jean-Bernard Auliac, Isabelle Monnet, Catherine Dubos-Arvis, Anne Marie Chiappa, Nathalie Baize, Suzana Bota, Alain Vergnenegre, Helene Doubre, Chrystele Locher, Acya Bizieux, Gilles Robinet, Christos Chouaid
Targeted Oncology.2017; 12(6): 833. CrossRef - Concomitant EML4-ALK rearrangement and EGFR mutation in non-small cell lung cancer patients: a literature review of 100 cases
Giuseppe Lo Russo, Martina Imbimbo, Giulia Corrao, Claudia Proto, Diego Signorelli, Milena Vitali, Monica Ganzinelli, Laura Botta, Nicoletta Zilembo, Filippo de Braud, Marina Chiara Garassino
Oncotarget.2017; 8(35): 59889. CrossRef - Management of non-small cell lung cancer in the era of personalized medicine
Gaetano Rocco, Alessandro Morabito, Alessandra Leone, Paolo Muto, Francesco Fiore, Alfredo Budillon
The International Journal of Biochemistry & Cell Biology.2016; 78: 173. CrossRef - A long-term survivor of non-small-cell lung cancer harboring concomitant EGFR mutation and ALK translocation
Fumio Imamura, Takako Inoue, Madoka Kimura, Kazumi Nishino, Toru Kumagai
Respiratory Medicine Case Reports.2016; 19: 137. CrossRef
- Integrative multi-omics machine learning reveals novel driver genes associations in lung adenocarcinoma
- Analysis of Mutations in Epidermal Growth Factor Receptor Gene in Korean Patients with Non-small Cell Lung Cancer: Summary of a Nationwide Survey
- Sang Hwa Lee, Wan Seop Kim, Yoo Duk Choi, Jeong Wook Seo, Joung Ho Han, Mi Jin Kim, Lucia Kim, Geon Kook Lee, Chang Hun Lee, Mee Hye Oh, Gou Young Kim, Sun Hee Sung, Kyo Young Lee, Sun Hee Chang, Mee Sook Rho, Han Kyeom Kim, Soon Hee Jung, Se Jin Jang, The Cardiopulmonary Pathology Study Group of Korean Society of Pathologists
- J Pathol Transl Med. 2015;49(6):481-488. Published online October 13, 2015
- DOI: https://doi.org/10.4132/jptm.2015.09.14
- 12,744 View
- 108 Download
- 22 Web of Science
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Analysis of mutations in the epidermal growth factor receptor gene (EGFR) is important for predicting response to EGFR tyrosine kinase inhibitors. The overall rate of EGFR mutations in Korean patients is variable. To obtain comprehensive data on the status of EGFR mutations in Korean patients with lung cancer, the Cardiopulmonary Pathology Study Group of the Korean Society of Pathologists initiated a nationwide survey. Methods: We obtained 1,753 reports on EGFR mutations in patients with lung cancer from 15 hospitals between January and December 2009. We compared EGFR mutations with patient age, sex, history of smoking, histologic diagnosis, specimen type, procurement site, tumor cell dissection, and laboratory status. Results: The overall EGFR mutation rate was 34.3% in patients with non-small cell lung cancer (NSCLC) and 43.3% in patients with adenocarcinoma. EGFR mutation rate was significantly higher in women, never smokers, patients with adenocarcinoma, and patients who had undergone excisional biopsy. EGFR mutation rates did not differ with respect to patient age or procurement site among patients with NSCLC. Conclusions: EGFR mutation rates and statuses were similar to those in published data from other East Asian countries. -
Citations
Citations to this article as recorded by- Projected cancer burden attributable to population aging: Insight from a rapidly aging society
Minh‐Thao Tu, Hoejun Kwon, Yoon‐Jung Choi, Hyunsoon Cho
International Journal of Cancer.2026; 158(4): 951. CrossRef - Assessing mutation-clinical correlations and treatment outcomes in Vietnamese non-small cell lung cancer patients
Hoang-Bac Nguyen, Bang-Suong Nguyen-Thi, Huu-Huy Nguyen, Minh-Khoi Le, Quoc-Trung Lam, Tuan-Anh Nguyen
Practical Laboratory Medicine.2025; 45: e00477. CrossRef - Gradual Increase in Lung Cancer Risk Due to Particulate Matter Exposure in Patients With Pulmonary Function Impairments: A Nationwide Korean Database Analysis
Jongin Lee, Joon Young Choi, Jeong Uk Lim
Journal of Korean Medical Science.2025;[Epub] CrossRef - Real-world treatment outcomes in South Korean patients with epidermal growth factor receptor-mutant non-small cell lung cancer
Young Saing Kim, Eun Young Lee, Hyun Woo Lee, Jin-Hyuk Choi, Tae-Hwan Kim, Yong Won Choi, Mi Sun Ahn
The Korean Journal of Internal Medicine.2025; 40(6): 1029. CrossRef - The role of oncogenes and tumor suppressor genes in determining survival rates of lung cancer patients in the population of North Sumatra, Indonesia
Noni Novisari Soeroso, Fannie Rizki Ananda, Johan Samuel Sitanggang, Noverita Sprinse Vinolina
F1000Research.2023; 11: 853. CrossRef - Comprehensive analysis of NGS and ARMS-PCR for detecting EGFR mutations based on 4467 cases of NSCLC patients
Changlong He, Chengcheng Wei, Jun Wen, Shi Chen, Ling Chen, Yue Wu, Yifan Shen, Huili Bai, Yangli Zhang, Xueping Chen, Xiaosong Li
Journal of Cancer Research and Clinical Oncology.2022; 148(2): 321. CrossRef - Unique characteristics of G719X and S768I compound double mutations of epidermal growth factor receptor (EGFR) gene in lung cancer of coal-producing areas of East Yunnan in Southwestern China
Jun-Ling Wang, Yu-Dong Fu, Yan-Hong Gao, Xiu-Ping Li, Qian Xiong, Rui Li, Bo Hou, Ruo-Shan Huang, Jun-Feng Wang, Jian-Kun Zhang, Jia-Ling Lv, Chao Zhang, Hong-Wei Li
Genes and Environment.2022;[Epub] CrossRef - Continuous Vaginal Bleeding Induced By EGFR-TKI in Premenopausal Female Patients With EGFR Mutant NSCLC
Min Yu, Xiaoyu Li, Xueqian Wu, Weiya Wang, Yanying Li, Yan Zhang, Shuang Zhang, Yongsheng Wang
Frontiers in Oncology.2022;[Epub] CrossRef - The role of oncogenes and tumor suppressor genes in determining survival rates of lung cancer patients in the population of North Sumatra, Indonesia
Noni Novisari Soeroso, Fannie Rizki Ananda, Johan Samuel Sitanggang, Noverita Sprinse Vinolina
F1000Research.2022; 11: 853. CrossRef - Adverse Event Profiles of Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors in Adenocarcinoma Lung Patients in North Sumatera Population
Moh. Ramadhani Soeroso, Noni Novisari Soeroso, Setia Putra Tarigan, Elisna Syahruddin
Open Access Macedonian Journal of Medical Sciences.2022; 10(T7): 134. CrossRef - Landscape of EGFR mutations in lung adenocarcinoma: a single institute experience with comparison of PANAMutyper testing and targeted next-generation sequencing
Jeonghyo Lee, Yeon Bi Han, Hyun Jung Kwon, Song Kook Lee, Hyojin Kim, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2022; 56(5): 249. CrossRef - Traditional Chinese Medicine Syndromes are Associated with Driver Gene Mutations and Clinical Characteristics in Patients with Lung Adenocarcinoma
Jili Yang, Haiyan Lu, Niancai Jing, Bo Wang, Huanyu Guo, Shoukun Sun, Yue Zhang, Chan-Yen Kuo
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Exosome-based detection of EGFR T790M in plasma and pleural fluid of prospectively enrolled non-small cell lung cancer patients after first-line tyrosine kinase inhibitor therapy
Yoonjung Kim, Saeam Shin, Kyung-A Lee
Cancer Cell International.2021;[Epub] CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Osimertinib in Patients with T790M-Positive Advanced Non-small Cell Lung Cancer: Korean Subgroup Analysis from Phase II Studies
Myung-Ju Ahn, Ji-Youn Han, Dong-Wan Kim, Byoung Chul Cho, Jin-Hyoung Kang, Sang-We Kim, James Chih-Hsin Yang, Tetsuya Mitsudomi, Jong Seok Lee
Cancer Research and Treatment.2020; 52(1): 284. CrossRef - Long non-coding RNA ATB promotes human non-small cell lung cancer proliferation and metastasis by suppressing miR-141-3p
Guojie Lu, Yaosen Zhang, Klaus Roemer
PLOS ONE.2020; 15(2): e0229118. CrossRef - Prognostic Role of S100A8 and S100A9 Protein Expressions in Non-small Cell Carcinoma of the Lung
Hyun Min Koh, Hyo Jung An, Gyung Hyuck Ko, Jeong Hee Lee, Jong Sil Lee, Dong Chul Kim, Jung Wook Yang, Min Hye Kim, Sung Hwan Kim, Kyung Nyeo Jeon, Gyeong-Won Lee, Se Min Jang, Dae Hyun Song
Journal of Pathology and Translational Medicine.2019; 53(1): 13. CrossRef - Epidermal growth factor receptor T790M mutations in non-small cell lung cancer (NSCLC) of Yunnan in southwestern China
Yongchun Zhou, Yuhui Ma, Hutao Shi, Yaxi Du, Yunchao Huang
Scientific Reports.2018;[Epub] CrossRef - Does the efficacy of epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor differ according to the type of EGFR mutation in non-small cell lung cancer?
Yong Won Choi, Jin-Hyuk Choi
The Korean Journal of Internal Medicine.2017; 32(3): 422. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - MET Exon 14 Skipping Mutations in Lung Adenocarcinoma: Clinicopathologic Implications and Prognostic Values
Geun Dong Lee, Seung Eun Lee, Doo-Yi Oh, Dan-bi Yu, Hae Min Jeong, Jooseok Kim, Sungyoul Hong, Hun Soon Jung, Ensel Oh, Ji-Young Song, Mi-Sook Lee, Mingi Kim, Kyungsoo Jung, Jhingook Kim, Young Kee Shin, Yoon-La Choi, Hyeong Ryul Kim
Journal of Thoracic Oncology.2017; 12(8): 1233. CrossRef - Epidermal growth factor receptor (EGFR) mutations in non-small cell lung cancer (NSCLC) of Yunnan in southwestern China
Yongchun Zhou, Yanlong Yang, Chenggang Yang, Yunlan Chen, Changshao Yang, Yaxi Du, Guangqiang Zhao, Yinjin Guo, Lianhua Ye, Yunchao Huang
Oncotarget.2017; 8(9): 15023. CrossRef - Detection of EGFR and KRAS Mutation by Pyrosequencing Analysis in Cytologic Samples of Non-Small Cell Lung Cancer
Seung Eun Lee, So-Young Lee, Hyung-Kyu Park, Seo-Young Oh, Hee-Joung Kim, Kye-Young Lee, Wan-Seop Kim
Journal of Korean Medical Science.2016; 31(8): 1224. CrossRef - MassARRAY, pyrosequencing, and PNA clamping for EGFR mutation detection in lung cancer tissue and cytological samples: a multicenter study
Kyueng-Whan Min, Wan-Seop Kim, Se Jin Jang, Yoo Duk Choi, Sunhee Chang, Soon Hee Jung, Lucia Kim, Mee-Sook Roh, Choong Sik Lee, Jung Weon Shim, Mi Jin Kim, Geon Kook Lee
Journal of Cancer Research and Clinical Oncology.2016; 142(10): 2209. CrossRef - Clinicopathologic characteristics of EGFR, KRAS, and ALK alterations in 6,595 lung cancers
Boram Lee, Taebum Lee, Se-Hoon Lee, Yoon-La Choi, Joungho Han
Oncotarget.2016; 7(17): 23874. CrossRef
- Projected cancer burden attributable to population aging: Insight from a rapidly aging society
- Membranous Insulin-like Growth Factor-1 Receptor (IGF1R) Expression Is Predictive of Poor Prognosis in Patients with Epidermal Growth Factor Receptor (EGFR)-Mutant Lung Adenocarcinoma
- Eunhyang Park, Soo Young Park, Hyojin Kim, Ping-Li Sun, Yan Jin, Suk Ki Cho, Kwhanmien Kim, Choon-Taek Lee, Jin-Haeng Chung
- J Pathol Transl Med. 2015;49(5):382-388. Published online August 4, 2015
- DOI: https://doi.org/10.4132/jptm.2015.07.10
- 11,366 View
- 100 Download
- 23 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Insulin-like growth factor-1 receptor (IGF1R) is a membrane receptor-type tyrosine kinase that has attracted considerable attention as a potential therapeutic target, although its clinical significance in non-small cell lung cancer (NSCLC) is controversial. This study aimed to clarify the clinical significance of IGF1R expression in human NSCLC. Methods: IGF1R protein expression was evaluated using immunohistochemistry in 372 patients with NSCLC who underwent curative surgical resection (146 squamous cell carcinomas [SqCCs] and 226 adenocarcinomas [ADCs]). We then analyzed correlations between expression of IGF1R and clinicopathological and molecular features and prognostic significance. Results: Membranous and cytoplasmic IGF1R expression were significantly higher in SqCCs than in ADCs. In patients with SqCC, membranous IGF1R expression was associated with absence of vascular, lymphatic, and perineural invasion; lower stage; and better progression-free survival (PFS) (hazard ratio [HR], 0.586; p = .040). In patients with ADC, IGF1R expression did not have a significant prognostic value; however, in the subgroup of epidermal growth factor receptor (EGFR)-mutant ADC, membranous IGF1R expression was associated with lymphatic and perineural invasion, solid predominant histology, and higher cancer stage and was significantly associated with worse PFS (HR, 2.582; p = .009). Conclusions: Lung ADC and SqCC showed distinct IGF1R expression profiles that demonstrated prognostic significance. High membranous IGF1R expression was predictive of poor PFS in EGFR-mutant lung ADC, while it was predictive of better PFS in SqCC. These findings will help improve study design for subsequent investigations and select patients for future anti-IGF1R therapy. -
Citations
Citations to this article as recorded by- Expression of Amine Oxidase Proteins in Adrenal Cortical Neoplasm and Pheochromocytoma
Eun Kyung Kim, Ja Seung Koo
Biomedicines.2023; 11(7): 1896. CrossRef - Expression of EMP 1, 2, and 3 in Adrenal Cortical Neoplasm and Pheochromocytoma
Yoon Jin Cha, Ja Seung Koo
International Journal of Molecular Sciences.2023; 24(16): 13016. CrossRef - Clinico-pathological characteristics of IGFR1 and VEGF-A co-expression in early and locally advanced-stage lung adenocarcinoma
Wenting Liu, Junling Xia, Qingwu Du, Jingya Wang, Ting Mei, Tingting Qin
Journal of Cancer Research and Clinical Oncology.2023; 149(18): 16365. CrossRef - NT157 exerts antineoplastic activity by targeting JNK and AXL signaling in lung cancer cells
Lívia Bassani Lins de Miranda, Keli Lima, Juan Luiz Coelho-Silva, Fabiola Traina, Susumu S. Kobayashi, João Agostinho Machado-Neto
Scientific Reports.2022;[Epub] CrossRef - IRS2 Amplification as a Predictive Biomarker in Response to Ceritinib in Small Cell Lung Cancer
Mi-Sook Lee, Kyungsoo Jung, Ji-Young Song, Min-Jung Sung, Sung-Bin Ahn, Boram Lee, Doo-Yi Oh, Yoon-La Choi
Molecular Therapy - Oncolytics.2020; 16: 188. CrossRef - Understanding Lineage Plasticity as a Path to Targeted Therapy Failure in EGFR-Mutant Non-small Cell Lung Cancer
Tatiana Shaurova, Letian Zhang, David W. Goodrich, Pamela A. Hershberger
Frontiers in Genetics.2020;[Epub] CrossRef - Characterization of head and neck squamous cell carcinoma arising in young patients: Particular focus on molecular alteration and tumor immunity
Hyang Joo Ryu, Eun Kyung Kim, Byoung Chul Cho, Sun Och Yoon
Head & Neck.2019; 41(1): 198. CrossRef - Investigating Trk Protein Expression between Oropharyngeal and Non-oropharyngeal Squamous Cell Carcinoma: Clinical Implications and Possible Roles of Human Papillomavirus Infection
Yoon Ah Cho, Ji Myung Chung, Hyunmi Ryu, Eun Kyung Kim, Byoung Chul Cho, Sun Och Yoon
Cancer Research and Treatment.2019; 51(3): 1052. CrossRef - NOVA1 induction by inflammation and NOVA1 suppression by epigenetic regulation in head and neck squamous cell carcinoma
Eun Kyung Kim, Yoon Ah Cho, Mi-kyoung Seo, Hyunmi Ryu, Byoung Chul Cho, Yoon Woo Koh, Sun Och Yoon
Scientific Reports.2019;[Epub] CrossRef - Advances in studies of tyrosine kinase inhibitors and their acquired resistance
Qinlian Jiao, Lei Bi, Yidan Ren, Shuliang Song, Qin Wang, Yun-shan Wang
Molecular Cancer.2018;[Epub] CrossRef - The long coding RNA AFAP1-AS1 promotes tumor cell growth and invasion in pancreatic cancer through upregulating the IGF1R oncogene via sequestration of miR-133a
Bo Chen, Qinhua Li, Yongping Zhou, Xujing Wang, Qiqi Zhang, Yongkun Wang, Huiren Zhuang, Xiaohua Jiang, Wujun Xiong
Cell Cycle.2018; 17(16): 1949. CrossRef - Overexpression of lncRNA EGFR‑AS1 is associated with a poor prognosis and promotes chemotherapy resistance in non‑small cell lung cancer
Yu-Hua Xu, Jian-Ren Tu, Tian-Tian Zhao, Shi-Guang Xie, Sheng-Bo Tang
International Journal of Oncology.2018;[Epub] CrossRef - IGF-IR signaling in epithelial to mesenchymal transition and targeting IGF-IR therapy: overview and new insights
Heming Li, Izhar Singh Batth, Xiujuan Qu, Ling Xu, Na Song, Ruoyu Wang, Yunpeng Liu
Molecular Cancer.2017;[Epub] CrossRef - Insulin-like growth factor 1 receptor expression in advanced non-small-cell lung cancer and its impact on overall survival
Mojca Humar, Izidor Kern, Gregor Vlacic, Vedran Hadzic, Tanja Cufer
Radiology and Oncology.2017; 51(2): 195. CrossRef - IGF1R depletion facilitates MET-amplification as mechanism of acquired resistance to erlotinib in HCC827 NSCLC cells
Dianna Hussmann, Anne Tranberg Madsen, Kristine Raaby Jakobsen, Yonglun Luo, Boe Sandahl Sorensen, Anders Lade Nielsen
Oncotarget.2017; 8(20): 33300. CrossRef - Upregulated Neuro-oncological Ventral Antigen 1 (NOVA1) Expression Is Specific to Mature and Immature T- and NK-Cell Lymphomas
Eun Kyung Kim, Sun Och Yoon, Soo Hee Kim, Woo Ick Yang, Yoon Ah Cho, Soo Jeong Kim
Journal of Pathology and Translational Medicine.2016; 50(2): 104. CrossRef - The Clinical Significance of the Insulin-Like Growth Factor-1 Receptor Polymorphism in Non-Small-Cell Lung Cancer with Epidermal Growth Factor Receptor Mutation
Tu-Chen Liu, Ming-Ju Hsieh, Ming-Che Liu, Whei-Ling Chiang, Thomas Tsao, Shun-Fa Yang
International Journal of Molecular Sciences.2016; 17(5): 763. CrossRef
- Expression of Amine Oxidase Proteins in Adrenal Cortical Neoplasm and Pheochromocytoma
- Molecular Imaging in the Era of Personalized Medicine
- Kyung-Ho Jung, Kyung-Han Lee
- J Pathol Transl Med. 2015;49(1):5-12. Published online January 15, 2015
- DOI: https://doi.org/10.4132/jptm.2014.10.24
- 15,480 View
- 212 Download
- 32 Web of Science
- 27 Crossref
-
 Abstract
Abstract
 PDF
PDF - Clinical imaging creates visual representations of the body interior for disease assessment. The role of clinical imaging significantly overlaps with that of pathology, and diagnostic workflows largely depend on both fields. The field of clinical imaging is presently undergoing a radical change through the emergence of a new field called molecular imaging. This new technology, which lies at the intersection between imaging and molecular biology, enables noninvasive visualization of biochemical processes at the molecular level within living bodies. Molecular imaging differs from traditional anatomical imaging in that biomarkers known as imaging probes are used to visualize target molecules-of-interest. This ability opens up exciting new possibilities for applications in oncologic, neurological and cardiovascular diseases. Molecular imaging is expected to make major contributions to personalized medicine by allowing earlier diagnosis and predicting treatment response. The technique is also making a huge impact on pharmaceutical development by optimizing preclinical and clinical tests for new drug candidates. This review will describe the basic principles of molecular imaging and will briefly touch on three examples (from an immense list of new techniques) that may contribute to personalized medicine: receptor imaging, angiogenesis imaging, and apoptosis imaging.
-
Citations
Citations to this article as recorded by- Ionic Cell Microscopy: A new modality for visualizing cells using microfluidic impedance cytometry and generative artificial intelligence
Mahtab Kokabi, Gulam M. Rather, Mehdi Javanmard
Biosensors and Bioelectronics: X.2025; 24: 100619. CrossRef - Multimodal imaging in cancer detection: the role of SPIONs and USPIONs as contrast agents for MRI, SPECT, and PET
Zahra Shaghaghi, Ramin Mansouri, Sahar Nosrati, Maryam Alvandi
Future Oncology.2025; 21(18): 2367. CrossRef - Supramolecular fluorescence biosensing based on macrocycles
Jia-Hong Tian, Haiqi Xu, Xin-Yue Hu, Dong-Sheng Guo
Supramolecular Materials.2024; 3: 100063. CrossRef - A non-invasive osteopontin-targeted phase changeable fluorescent nanoprobe for molecular imaging of myocardial fibrosis
Xueli Zhao, Yuze Qin, Bo Wang, Jiao Liu, Yueyue Wang, Kun Chen, Jia Zhao, Lanlan Zhang, Yuanming Wu, Liwen Liu
Nanoscale Advances.2024; 6(14): 3590. CrossRef - The Role of Molecular Imaging in Personalized Medicine
Suliman Salih, Aisyah Elliyanti, Ajnas Alkatheeri, Fatima AlYafei, Bashayer Almarri, Hasina Khan
Journal of Personalized Medicine.2023; 13(2): 369. CrossRef - Development of a multifunctional platform for near-infrared imaging and targeted radionuclide therapy for tumors
Huihui He, Ke Li, Hang Li, Shiliang Zhu, Shuai Qin, Yong Mao, Jianguo Lin, Ling Qiu, Chunjing Yu
European Journal of Pharmaceutics and Biopharmaceutics.2023; 185: 107. CrossRef - Quantum Biotechnology
Nicolas P. Mauranyapin, Alex Terrasson, Warwick P. Bowen
Advanced Quantum Technologies.2022;[Epub] CrossRef - Preparation Fe3O4@chitosan-graphene quantum dots nanocomposites for fluorescence and magnetic resonance imaging
Kai Wang, Xiaoguang Xu, Yan Li, Mayifei Rong, Lifeng Wang, Liying Lu, Jian Wang, Fengwen Zhao, Bowen Sun, Yong Jiang
Chemical Physics Letters.2021; 783: 139060. CrossRef - Network Medicine: A Clinical Approach for Precision Medicine and Personalized Therapy in Coronary Heart Disease
Teresa Infante, Luca Del Viscovo, Maria Luisa De Rimini, Sergio Padula, Pio Caso, Claudio Napoli
Journal of Atherosclerosis and Thrombosis.2020; 27(4): 279. CrossRef - Nanodrug Delivery Systems for the Treatment of Ovarian Cancer
Jonathan M. Pantshwa, Pierre P. D. Kondiah, Yahya E. Choonara, Thashree Marimuthu, Viness Pillay
Cancers.2020; 12(1): 213. CrossRef - Molecular imaging of the urokinase plasminogen activator receptor: opportunities beyond cancer
V. M. Baart, R. D. Houvast, L. F. de Geus-Oei, P. H. A. Quax, P. J. K. Kuppen, A. L. Vahrmeijer, C. F. M. Sier
EJNMMI Research.2020;[Epub] CrossRef - In vivo SPECT imaging of an 131I-labeled PM 2.5 mimic substitute
Dong-Hui Pan, Jie Sheng, Xin-Yu Wang, Qian-Huan Huang, Jun-Jie Yan, Li-Zhen Wang, Run-Ling Yang, Dong-Jian Shi, Yu-Ping Xu, Ming-Qing Chen
Nuclear Science and Techniques.2020;[Epub] CrossRef - Optofluidics in bio-imaging applications
Sihui Chen, Rui Hao, Yi Zhang, Hui Yang
Photonics Research.2019; 7(5): 532. CrossRef - Nitrogen-vacancy centers in diamond for nanoscale magnetic resonance imaging applications
Alberto Boretti, Lorenzo Rosa, Jonathan Blackledge, Stefania Castelletto
Beilstein Journal of Nanotechnology.2019; 10: 2128. CrossRef - Online molecular image repository and analysis system: A multicenter collaborative open-source infrastructure for molecular imaging research and application
Mahabubur Rahman, Hiroshi Watabe
Computers in Biology and Medicine.2018; 96: 233. CrossRef - Nε-Acryloyllysine Piperazides as Irreversible Inhibitors of Transglutaminase 2: Synthesis, Structure–Activity Relationships, and Pharmacokinetic Profiling
Robert Wodtke, Christoph Hauser, Gloria Ruiz-Gómez, Elisabeth Jäckel, David Bauer, Martin Lohse, Alan Wong, Johanna Pufe, Friedrich-Alexander Ludwig, Steffen Fischer, Sandra Hauser, Dieter Greif, M. Teresa Pisabarro, Jens Pietzsch, Markus Pietsch, Reik Lö
Journal of Medicinal Chemistry.2018; 61(10): 4528. CrossRef - Genomic Interventions in Medicine
Oluwadurotimi S Aworunse, Oluwatomiwa Adeniji, Olusola L Oyesola, Itunuoluwa Isewon, Jelili Oyelade, Olawole O Obembe
Bioinformatics and Biology Insights.2018;[Epub] CrossRef - Restriction spectrum imaging: An evolving imaging biomarker in prostate MRI
Ryan L. Brunsing, Natalie M. Schenker-Ahmed, Nathan S. White, J. Kellogg Parsons, Christopher Kane, Joshua Kuperman, Hauke Bartsch, Andrew Karim Kader, Rebecca Rakow-Penner, Tyler M. Seibert, Daniel Margolis, Steven S. Raman, Carrie R. McDonald, Nikdokht
Journal of Magnetic Resonance Imaging.2017; 45(2): 323. CrossRef - Personalized medicine: a new option for nuclear medicine and molecular imaging in the third millennium
Orazio Schillaci, Nicoletta Urbano
European Journal of Nuclear Medicine and Molecular Imaging.2017; 44(4): 563. CrossRef - Nano-Magnetic Resonance Imaging (Nano-MRI) Gives Personalized Medicine a New Perspective
Lorenzo Rosa, Jonathan Blackledge, Albert Boretti
Biomedicines.2017; 5(1): 7. CrossRef - Optical nanoprobes for biomedical applications: shining a light on upconverting and near-infrared emitting nanoparticles for imaging, thermal sensing, and photodynamic therapy
E. Hemmer, P. Acosta-Mora, J. Méndez-Ramos, S. Fischer
Journal of Materials Chemistry B.2017; 5(23): 4365. CrossRef - Drug Discovery by Molecular Imaging and Monitoring Therapy Response in Lymphoma
Senthilkumar Kalimuthu, Ju Hye Jeong, Ji Min Oh, Byeong-Cheol Ahn
International Journal of Molecular Sciences.2017; 18(8): 1639. CrossRef - Chemistry and engineering of cyclodextrins for molecular imaging
Wing-Fu Lai, Andrey L. Rogach, Wing-Tak Wong
Chemical Society Reviews.2017; 46(20): 6379. CrossRef - Prototypes of Lanthanide(III) Agents Responsive to Enzymatic Activities in Three Complementary Imaging Modalities: Visible/Near-Infrared Luminescence, PARACEST-, and T1-MRI
Jiefang He, Célia S. Bonnet, Svetlana V. Eliseeva, Sara Lacerda, Thomas Chauvin, Pascal Retailleau, Frederic Szeremeta, Bernard Badet, Stéphane Petoud, Éva Tóth, Philippe Durand
Journal of the American Chemical Society.2016; 138(9): 2913. CrossRef - Nanoparticles in practice for molecular-imaging applications: An overview
Parasuraman Padmanabhan, Ajay Kumar, Sundramurthy Kumar, Ravi Kumar Chaudhary, Balázs Gulyás
Acta Biomaterialia.2016; 41: 1. CrossRef - A new neuroinformatics approach to personalized medicine in neurology: The Virtual Brain
Maria I. Falcon, Viktor Jirsa, Ana Solodkin
Current Opinion in Neurology.2016; 29(4): 429. CrossRef - Targeted multimodal nano-reporters for pre-procedural MRI and intra-operative image-guidance
Joonseok Lee, Andrew C. Gordon, Hacksung Kim, Wooram Park, Soojeong Cho, Byeongdu Lee, Andrew C. Larson, Elena A. Rozhkova, Dong-Hyun Kim
Biomaterials.2016; 109: 69. CrossRef
- Ionic Cell Microscopy: A new modality for visualizing cells using microfluidic impedance cytometry and generative artificial intelligence
- P2X7 Receptor Expression in Coexistence of Papillary Thyroid Carcinoma with Hashimoto's Thyroiditis
- Ji Hyun Kwon, Eun Sook Nam, Hyung Sik Shin, Seong Jin Cho, Hye Rim Park, Mi Jung Kwon
- Korean J Pathol. 2014;48(1):30-35. Published online February 25, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.1.30
- 11,143 View
- 56 Download
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF Background This study was aimed at investigating the relation of P2X7 receptor (P2X7R) expression with the clinicopathological features of papillary thyroid carcinoma (PTC) coexisting with Hashimoto's thyroiditis (HT).
Methods We examined 170 patients (84, PTC with HT; 86, PTC without HT). P2X7R expression was examined by immunohistochemical methods. The staining intensity and patterns were evaluated and scored using a semi-quantitative method.
Results The PTC with HT group was more likely to contain women and had less extrathyroid extension, lymph node (LN) metastasis, lymphovascular invasion, and recurrence than the PTC without HT group. Patients positive for P2X7R had significantly higher frequencies of lymphovascular invasion, extrathyroid extension, LN metastasis, and absence of HT. As shown by multivariate analysis, the expression of P2X7R was significantly higher if HT was absent and extrathyroid extension was present. In the PTC with HT group, the expression of P2X7R was significantly higher in patients with tumor multifocality, lymphovascular invasion, and extrathyroid extension. In the PTC without HT group, the expression of P2X7R was significantly higher in women and those having tumor multifocality.
Conclusions Coexistence of PTC with HT is associated with good prognostic factors, and P2X7R expression in PTC was correlated with poor prognostic factors and the absence of HT.
-
Citations
Citations to this article as recorded by- Research Progress in the Relationship Between P2X7R and Cervical Cancer
Yiqing Tang, Cuicui Qiao, Qianqian Li, Xiaodi Zhu, Ronglan Zhao, Xiaoxiang Peng
Reproductive Sciences.2023; 30(3): 823. CrossRef - Warthin-like papillary thyroid carcinoma: a case report and comprehensive review of the literature
Abdel Mouhaymen Missaoui, Fatma Hamza, Wafa Belabed, Manel Mellouli, Mohamed Maaloul, Slim Charfi, Issam Jardak, Tahya Sellami-Boudawara, Nabila Rekik, Mohamed Abid
Frontiers in Endocrinology.2023;[Epub] CrossRef - Mapping the path towards novel treatment strategies: a bibliometric analysis of Hashimoto’s thyroiditis research from 1990 to 2023
Manping Guo, Qingna Li, Xingfang Liu, Yiming Wang, Qiaoning Yang, Rui Li, Yang Zhao, Chenfei Li, Song Sheng, Hangkun Ma, Zhenghong Li, Rui Gao
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association between Hashimoto thyroiditis and clinical outcomes of papillary thyroid carcinoma: A meta-analysis
Qizhi Tang, Weiyu Pan, Liangyue Peng, Francis Moore
PLOS ONE.2022; 17(6): e0269995. CrossRef - Hashimoto’s Thyroiditis Minimizes Lymph Node Metastasis in BRAF Mutant Papillary Thyroid Carcinomas
Peter P. Issa, Mahmoud Omar, Yusef Buti, Chad P. Issa, Bert Chabot, Christopher J. Carnabatu, Ruhul Munshi, Mohammad Hussein, Mohamed Aboueisha, Mohamed Shama, Ralph L. Corsetti, Eman Toraih, Emad Kandil
Biomedicines.2022; 10(8): 2051. CrossRef - Overexpression of PD-L1 in Papillary Carcinoma and Its Association with Clinicopathological Variables
Servet KOCAÖZ, Gülay TURAN
Düzce Tıp Fakültesi Dergisi.2021; 23(3): 252. CrossRef - Effect of P2X7 receptor on tumorigenesis and its pharmacological properties
Wen-jun Zhang, Ce-gui Hu, Zheng-ming Zhu, Hong-liang Luo
Biomedicine & Pharmacotherapy.2020; 125: 109844. CrossRef - P2X7 in Cancer: From Molecular Mechanisms to Therapeutics
Romain Lara, Elena Adinolfi, Catherine A. Harwood, Mike Philpott, Julian A. Barden, Francesco Di Virgilio, Shaun McNulty
Frontiers in Pharmacology.2020;[Epub] CrossRef - The P2X7 Receptor in Inflammatory Diseases: Angel or Demon?
Luiz E. B. Savio, Paola de Andrade Mello, Cleide Gonçalves da Silva, Robson Coutinho-Silva
Frontiers in Pharmacology.2018;[Epub] CrossRef - Patients with Oncocytic Variant Papillary Thyroid Carcinoma Have a Similar Prognosis to Matched Classical Papillary Thyroid Carcinoma Controls
Azadeh A. Carr, Tina W.F. Yen, Diana I. Ortiz, Bryan C. Hunt, Gilbert Fareau, Becky L. Massey, Bruce H. Campbell, Kara L. Doffek, Douglas B. Evans, Tracy S. Wang
Thyroid.2018; 28(11): 1462. CrossRef - Extracellular purines, purinergic receptors and tumor growth
F Di Virgilio, E Adinolfi
Oncogene.2017; 36(3): 293. CrossRef - Multifaceted Effects of Extracellular Adenosine Triphosphate and Adenosine in the Tumor–Host Interaction and Therapeutic Perspectives
Paola de Andrade Mello, Robson Coutinho-Silva, Luiz Eduardo Baggio Savio
Frontiers in Immunology.2017;[Epub] CrossRef - Potential role of P2X7R in esophageal squamous cell carcinoma proliferation
André A Santos, Angélica R Cappellari, Fernanda O de Marchi, Marina P Gehring, Aline Zaparte, Caroline A Brandão, Tiago Giuliani Lopes, Vinicius D da Silva, Luis Felipe Ribeiro Pinto, Luiz Eduardo Baggio Savio, Aline Cristina Abreu Moreira-Souza, Robson C
Purinergic Signalling.2017; 13(3): 279. CrossRef - Potential relationship between Hashimoto's thyroiditis and BRAFV600E mutation status in papillary thyroid cancer
Rui‐chao Zeng, Lang‐ping Jin, En‐dong Chen, Si‐yang Dong, Ye‐feng Cai, Guan‐li Huang, Quan Li, Chun Jin, Xiao‐hua Zhang, Ou‐chen Wang
Head & Neck.2016;[Epub] CrossRef - Papillary thyroid carcinoma in Hashimoto’s thyroiditis as an incidental finding
Al Mogrampi Saad, A. Krexi, N. Papoulidis, M. Verroiotou, D. Michalakis, I. Fardellas
Hellenic Journal of Surgery.2016; 88(1): 47. CrossRef - Association of Hashimoto's thyroiditis and thyroid cancer
Salem I. Noureldine, Ralph P. Tufano
Current Opinion in Oncology.2015; 27(1): 21. CrossRef - Cribriform-morular variant of papillary thyroid carcinoma: a study of 3 cases featuring the PIK3CA mutation
Mi Jung Kwon, Young-Soo Rho, Jin Cheol Jeong, Hyung Sik Shin, Jong Seok Lee, Seong Jin Cho, Eun Sook Nam
Human Pathology.2015; 46(8): 1180. CrossRef - Understanding the roles of the P2X7 receptor in solid tumour progression and therapeutic perspectives
Sébastien Roger, Bilel Jelassi, Isabelle Couillin, Pablo Pelegrin, Pierre Besson, Lin-Hua Jiang
Biochimica et Biophysica Acta (BBA) - Biomembranes.2015; 1848(10): 2584. CrossRef - Purinergic signaling pathways in endocrine system
Ivana Bjelobaba, Marija M. Janjic, Stanko S. Stojilkovic
Autonomic Neuroscience.2015; 191: 102. CrossRef - P2X7 receptor stimulates breast cancer cell invasion and migration via the AKT pathway
JIYI XIA, XIAOLAN YU, LI TANG, GANG LI, TAO HE
Oncology Reports.2015; 34(1): 103. CrossRef - Regulation of the P2X7R by microRNA-216b in human breast cancer
Luming Zheng, Xukui Zhang, Feng Yang, Jian Zhu, Peng Zhou, Fang Yu, Lei Hou, Lei Xiao, Qingqing He, Baocheng Wang
Biochemical and Biophysical Research Communications.2014; 452(1): 197. CrossRef
- Research Progress in the Relationship Between P2X7R and Cervical Cancer
EGFR Gene Amplification and Protein Expression in Invasive Ductal Carcinoma of the Breast- Won Hwangbo, Jeong Hyeon Lee, Sangjeong Ahn, Seojin Kim, Kyong Hwa Park, Chul Hwan Kim, Insun Kim
- Korean J Pathol. 2013;47(2):107-115. Published online April 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.2.107
- 14,060 View
- 82 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The epidermal growth factor receptor (EGFR) is a surrogate marker for basal-like breast cancer. A recent study suggested that EGFR may be used as a target for breast cancer treatment.
Methods A total of 706 invasive ductal carcinomas (IDC) of the breast were immunophenotyped, and 82 cases with EGFR protein expression were studied for
EGFR gene amplification.Results EGFR protein was expressed in 121 of 706 IDCs (17.1%); 5.9% were of luminal type, 25.3% of epidermal growth factor receptor 2 (HER-2) type, and 79.3% of basal-like tumors.
EGFR gene amplification and high polysomy (fluorescentin situ hybridization [FISH]-positive) were found in 18 of 82 cases (22.0%); 41.2% of the HER-2+, EGFR+, cytokeratin 5/6- (CK5/6-) group, 11.2% of the HER-2-, EGFR+, CK5/6- group, and 19.1% of the HER-2-, EGFR+, CK5/6+ group. FISH-positive cases were detected in 8.3% of the EGFR protein 1+ expression cases, 15.9% of 2+ expression cases, and 38.5% of 3+ expression cases. In group 2, the tumors had a high Ki-67 labeling (>60%), but the patients showed better disease-free survival than those with tumors that co-expressed HER-2 or CK5/6.Conclusions EGFR-directed therapy can be considered in breast cancer patients with EGFR protein overexpression and gene amplification, and its therapeutic implication should be determined in HER-2 type breast cancer patients.
-
Citations
Citations to this article as recorded by- An overview of phenylsulfonylfuroxan-based nitric oxide donors for cancer treatment
Chao Gao, Xingyu Li, Tong Liu, Wanning Wang, Jianhui Wu
Bioorganic Chemistry.2025; 154: 108020. CrossRef - Identification of a cross-talk between EGFR and Wnt/beta-catenin signaling pathways in HepG2 liver cancer cells
Gurjinder Singh, Md Mehedi Hossain, Aadil Qadir Bhat, Mir Owais Ayaz, Nasima Bano, Rafiqa Eachkoti, Mohd Jamal Dar
Cellular Signalling.2021; 79: 109885. CrossRef - Blocking c-MET/ERBB1 Axis Prevents Brain Metastasis in ERBB2+ Breast Cancer
Shailendra K. Gautam, Ranjana K. Kanchan, Jawed A. Siddiqui, Shailendra K. Maurya, Sanchita Rauth, Naveenkumar Perumal, Pranita Atri, Ramakanth C. Venkata, Kavita Mallya, Sameer Mirza, Moorthy P. Ponnusamy, Vimla Band, Sidharth Mahapatra, Maneesh Jain, Su
Cancers.2020; 12(10): 2838. CrossRef - Evaluation of lapatinib cytotoxicity and genotoxicity on MDA-MB-231 breast cancer cell line
Mona A.M. Abo-Zeid, Mahmoud T. Abo-Elfadl, Amira M. Gamal-Eldeen
Environmental Toxicology and Pharmacology.2019; 71: 103207. CrossRef - Improved characterization of the relationship between long intergenic non‐coding RNA Linc00152 and the occurrence and development of malignancies
Jiasheng Xu, Jingjing Guo, Yangkai Jiang, Yujun Liu, Kaili Liao, Zhonghua Fu, Zhenfang Xiong
Cancer Medicine.2019; 8(10): 4722. CrossRef - Relationship between EGFR expression and subcellular localization with cancer development and clinical outcome
Ge Yan, Mohamed E.M. Saeed, Sebastian Foersch, Jose Schneider, Wilfried Roth, Thomas Efferth
Oncotarget.2019; 10(20): 1918. CrossRef - A novel matrine derivative WM622 inhibits hepatocellular carcinoma by inhibiting PI3K/AKT signaling pathways
Xiao Sun, Xiao-bin Zhuo, Yi-ping Hu, Xuan Zheng, Qing-jie Zhao
Molecular and Cellular Biochemistry.2018; 449(1-2): 47. CrossRef - lncRNA LINC00152 knockdown had effects to suppress biological activity of lung cancer via EGFR/PI3K/AKT pathway
Yan Zhang, Cheng Xiang, Yuling Wang, Yuanyuan Duan, Ci Liu, Yongli Jin, Yajing Zhang
Biomedicine & Pharmacotherapy.2017; 94: 644. CrossRef - Copy Number Profiling of MammaPrint™ Genes Reveals Association with the Prognosis of Breast Cancer Patients
Areej Fatima, Fomaz Tariq, Muhammad Faraz Arshad Malik, Muhammad Qasim, Farhan Haq
Journal of Breast Cancer.2017; 20(3): 246. CrossRef - Evaluation of serum epidermal growth factor receptor (EGFR) in correlation to circulating tumor cells in patients with metastatic breast cancer
Malgorzata Banys-Paluchowski, Isabell Witzel, Sabine Riethdorf, Brigitte Rack, Wolfgang Janni, Peter A. Fasching, Erich-Franz Solomayer, Bahriye Aktas, Sabine Kasimir-Bauer, Klaus Pantel, Tanja Fehm, Volkmar Müller
Scientific Reports.2017;[Epub] CrossRef - EGFR Is Regulated by TFAP2C in Luminal Breast Cancer and Is a Target for Vandetanib
James P. De Andrade, Jung M. Park, Vivian W. Gu, George W. Woodfield, Mikhail V. Kulak, Allison W. Lorenzen, Vincent T. Wu, Sarah E. Van Dorin, Philip M. Spanheimer, Ronald J. Weigel
Molecular Cancer Therapeutics.2016; 15(3): 503. CrossRef - Prognostic and predictive values of EGFR overexpression and EGFR copy number alteration in HER2-positive breast cancer
H J Lee, A N Seo, E J Kim, M H Jang, Y J Kim, J H Kim, S-W Kim, H S Ryu, I A Park, S-A Im, G Gong, K H Jung, H J Kim, S Y Park
British Journal of Cancer.2015; 112(1): 103. CrossRef - Epidermal growth factor receptor protein overexpression and gene amplification are associated with aggressive biological behaviors of esophageal squamous cell carcinoma
GANG LIN, XIAO-JIANG SUN, QIAN-BO HAN, ZHUN WANG, YA-PING XU, JIA-LEI GU, WEI WU, GU ZHANG, JIN-LIN HU, WEN-YONG SUN, WEI-MIN MAO
Oncology Letters.2015; 10(2): 901. CrossRef - Immunohistochemical Classification of Primary and Secondary Glioblastomas
Kyu Sang Lee, Gheeyoung Choe, Kyung Han Nam, An Na Seo, Sumi Yun, Kyung Ju Kim, Hwa Jin Cho, Sung Hye Park
Korean Journal of Pathology.2013; 47(6): 541. CrossRef - A Comparison of Tumor Biology in Primary Ductal CarcinomaIn SituRecurring as Invasive Carcinoma versus a NewIn Situ
Wenjing Zhou, Christine Johansson, Karin Jirström, Anita Ringberg, Carl Blomqvist, Rose-Marie Amini, Marie-Louise Fjallskog, Fredrik Wärnberg
International Journal of Breast Cancer.2013; 2013: 1. CrossRef
- An overview of phenylsulfonylfuroxan-based nitric oxide donors for cancer treatment
- Guideline Recommendations for
EGFR Mutation Testing in Lung Cancer: Proposal of the Korean Cardiopulmonary Pathology Study Group - Hyo Sup Shim, Jin-Haeng Chung, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Geon Kook Lee, Soon-Hee Jung, Se Jin Jang
- Korean J Pathol. 2013;47(2):100-106. Published online April 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.2.100
- 12,512 View
- 100 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Mutations of the epidermal growth factor receptor (
EGFR ) are the strongest predictive factor for response to EGFR tyrosine kinase inhibitors (TKIs), such as gefitinib and erlotinib. EGFR TKIs are approved in Korea as a first-line treatment for lung cancer patients with mutatedEGFR . Rapid and accurateEGFR mutation testing is essential for patient selection and establishing targeted therapies with EGFR TKIs. Thus, a standard set of guideline recommendations forEGFR mutation testing suitable for the Korean medical community is necessary. In this article, we propose a set of guideline recommendations forEGFR mutation testing that was discussed and approved by the Cardiopulmonary Pathology Study Group of the Korean Society of Pathologists.-
Citations
Citations to this article as recorded by- Establishment of a Flow Cytometry Protocol for Binarily Detecting Circulating Tumor Cells with EGFR Mutation
Cheng-Yu Chang, Chia-Chun Tu, Shian-Ren Lin, Chih-Hao Fang, Po-Wei Tseng, Wan-En Liao, Li-Yun Huang, Shiu-Lan Wang, Wan-Yu Lai, Yee Chao, Yen-Ling Chiu, Jan-Mou Lee
Diseases.2025; 13(12): 406. CrossRef - Favorable Conditions for the Detection of EGFR T790M Mutation Using Plasma Sample in Patients with Non-Small-Cell Lung Cancer
Insu Kim, Hee Yun Seol, Soo Han Kim, Mi-Hyun Kim, Min Ki Lee, Jung Seop Eom
Cancers.2023; 15(5): 1445. CrossRef - Novel Targets, Novel Treatments: The Changing Landscape of Non-Small Cell Lung Cancer
Dorine de Jong, Jeeban P. Das, Hong Ma, Jacienta Pailey Valiplackal, Conor Prendergast, Tina Roa, Brian Braumuller, Aileen Deng, Laurent Dercle, Randy Yeh, Mary M. Salvatore, Kathleen M. Capaccione
Cancers.2023; 15(10): 2855. CrossRef - Coordination games in cancer
Péter Bayer, Robert A. Gatenby, Patricia H. McDonald, Derek R. Duckett, Kateřina Staňková, Joel S. Brown, Jun Tanimoto
PLOS ONE.2022; 17(1): e0261578. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Primary HHV-8 (-) Effusion-Based Non-Germinal Center B Cell Diffuse Large B Cell Lymphoma Successfully Treated with Standard Anthracycline-Based Chemoimmunotherapy
Justin J Kuhlman, Muhamad Alhaj Moustafa, Liuyan Jiang, Han W Tun
Journal of Blood Medicine.2021; Volume 12: 833. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - Strategic management of transthoracic needle aspirates for histological subtyping and EGFR testing in patients with peripheral lung cancer: An institutional experience
Choonhee Son, Eun‐Ju Kang, Mee Sook Roh
Diagnostic Cytopathology.2015; 43(7): 532. CrossRef - Ultrasonography-Guided Core Biopsy of Supraclavicular Lymph Nodes for Diagnosis of Metastasis and Identification of Epidermal Growth Factor Receptor (EGFR) Mutation in Advanced Lung Cancer
Jooae Choe, Mi Young Kim, Jung Hwan Baek, Chang-Min Choi, Hwa Jung Kim
Medicine.2015; 94(29): e1209. CrossRef - Reliable EGFR mutation testing in ultrasound-guided supraclavicular lymph node fine-needle aspirates: a cohort study with diagnostic performance analysis
Amir Awwad, Sandeep Tiwari, Vishakha Sovani, David R Baldwin, Maruti Kumaran
BMJ Open Respiratory Research.2015; 2(1): e000075. CrossRef - Simultaneous diagnostic platform of genotyping EGFR, KRAS, and ALK in 510 Korean patients with non‐small‐cell lung cancer highlights significantly higher ALK rearrangement rate in advanced stage
Tae‐Jung Kim, Chan Kwon Park, Chang Dong Yeo, Kihoon Park, Chin Kook Rhee, Jusang Kim, Seung Joon Kim, Sang Haak Lee, Kyo‐Young Lee, Hyoung‐Kyu Yoon
Journal of Surgical Oncology.2014; 110(3): 245. CrossRef - Novel EGFR mutation-specific antibodies for lung adenocarcinoma: Highly specific but not sensitive detection of an E746_A750 deletion in exon 19 and an L858R mutation in exon 21 by immunohistochemistry
An Na Seo, Tae-In Park, Yan Jin, Ping-Li Sun, Hyojin Kim, Hyun Chang, Jin-Haeng Chung
Lung Cancer.2014; 83(3): 316. CrossRef - Molecular Pathology of Lung Cancer: Current Status and Future Directions
Mee Sook Roh
Tuberculosis and Respiratory Diseases.2014; 77(2): 49. CrossRef
- Establishment of a Flow Cytometry Protocol for Binarily Detecting Circulating Tumor Cells with EGFR Mutation
- Comparison of Direct Sequencing, PNA Clamping-Real Time Polymerase Chain Reaction, and Pyrosequencing Methods for the Detection of
EGFR Mutations in Non-small Cell Lung Carcinoma and the Correlation with Clinical Responses to EGFR Tyrosin - Hyun Ju Lee, Xianhua Xu, Hyojin Kim, Yan Jin, Pingli Sun, Ji Eun Kim, Jin-Haeng Chung
- Korean J Pathol. 2013;47(1):52-60. Published online February 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.1.52
- 12,685 View
- 93 Download
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The aims of this study were to evaluate the abilities of direct sequencing (DS), peptide nucleic acid (PNA) clamping, and pyrosequencing methods to detect epidermal growth factor receptor (
EGFR ) mutations in formalin-fixed paraffin-embedded (FFPE) non-small cell lung carcinoma (NSCLC) samples and to correlateEGFR mutational status as determined by each method with the clinical response toEGFR tyrosine kinase inhibitors (TKIs).Methods Sixty-one NSCLC patients treated with EGFR TKIs were identified to investigate somatic mutations in the
EGFR gene (exons 18-21).Results Mutations in the
EGFR gene were detected in 38 of the 61 patients (62%) by DS, 35 (57%) by PNA clamping and 37 (61%) by pyrosequencing. A total of 44 mutations (72%) were found by at least one of the three methods, and the concordances among the results were relatively high (82-85%; kappa coefficient, 0.713 to 0.736). There were 15 discordant cases (25%) among the three different methods.Conclusions All three
EGFR mutation tests had good concordance rates (over 82%) for FFPE samples. These results suggest that if the DNA quality and enrichment of tumor cells are assured, then DS, PNA clamping, and pyrosequencing are appropriate methods for the detection ofEGFR mutations.-
Citations
Citations to this article as recorded by- Recent Trends of Lung Cancer in Korea
Jae Guk Lee, Ho Cheol Kim, Chang-Min Choi
Tuberculosis and Respiratory Diseases.2021; 84(2): 89. CrossRef - Predictive value of KRAS mutation and excision repair cross-complementing 1 (ERCC1) protein overexpression in patients with colorectal cancer administered FOLFOX regimen
Sun Min Park, Sung Bong Choi, Yoon Suk Lee, In Kyu Lee
Asian Journal of Surgery.2021; 44(5): 715. CrossRef - Recent advances in diagnostic technologies in lung cancer
Hye Jung Park, Sang Hoon Lee, Yoon Soo Chang
The Korean Journal of Internal Medicine.2020; 35(2): 257. CrossRef - Afatinib is effective in the treatment of lung adenocarcinoma with uncommon EGFR p.L747P and p.L747S mutations
Sheng-Kai Liang, Jen-Chung Ko, James Chih-Hsin Yang, Jin-Yuan Shih
Lung Cancer.2019; 133: 103. CrossRef - Biomarker Testing for Patients With Advanced Non–Small Cell Lung Cancer: Real-World Issues and Tough Choices
Nathan A. Pennell, Maria E. Arcila, David R. Gandara, Howard West
American Society of Clinical Oncology Educational Book.2019; (39): 531. CrossRef - Evaluation of EGFR mutations in NSCLC with highly sensitive droplet digital PCR assays
Xi‑Wen Jiang, Wei Liu, Xiao‑Ya Zhu, Xiao‑Xie Xu
Molecular Medicine Reports.2019;[Epub] CrossRef - Peptide Nucleic Acid Clamping and Direct Sequencing in the Detection of Oncogenic Alterations in Lung Cancer: Systematic Review and Meta-Analysis
Jae-Uk Song, Jonghoo Lee
Yonsei Medical Journal.2018; 59(2): 211. CrossRef - Distribution of KRAS, DDR2, and TP53 gene mutations in lung cancer: An analysis of Iranian patients
Zahra Fathi, Seyed Ali Javad Mousavi, Raheleh Roudi, Farideh Ghazi, Sumitra Deb
PLOS ONE.2018; 13(7): e0200633. CrossRef - EGFR T790M mutation testing within the osimertinib AURA Phase I study
Simon Dearden, Helen Brown, Suzanne Jenkins, Kenneth S. Thress, Mireille Cantarini, Rebecca Cole, Malcolm Ranson, Pasi A. Jänne
Lung Cancer.2017; 109: 9. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - Mutations of the Epidermal Growth Factor Receptor Gene in Triple-Negative Breast Cancer
Aeri Kim, Min Hye Jang, Soo Jung Lee, Young Kyung Bae
Journal of Breast Cancer.2017; 20(2): 150. CrossRef - Double primary lung adenocarcinoma diagnosed by epidermal growth factor receptor mutation status
Oh Jung Kwon, Min Hyeok Lee, Sung Ju Kang, Seul Gi Kim, In Beom Jeong, Ji Yun Jeong, Eun Jung Cha, Do Yeun Cho, Young Jin Kim, Ji Woong Son
Yeungnam University Journal of Medicine.2017; 34(2): 270. CrossRef - Generation of lung cancer cell lines harboring EGFR T790M mutation by CRISPR/Cas9-mediated genome editing
Mi-Young Park, Min Hee Jung, Eun Young Eo, Seokjoong Kim, Sang Hoon Lee, Yeon Joo Lee, Jong Sun Park, Young Jae Cho, Jin Haeng Chung, Cheol Hyeon Kim, Ho Il Yoon, Jae Ho Lee, Choon-Taek Lee
Oncotarget.2017; 8(22): 36331. CrossRef - Comparison of EGFR mutation detection between the tissue and cytology using direct sequencing, pyrosequencing and peptide nucleic acid clamping in lung adenocarcinoma: Korean multicentre study
Kyueng-Whan Min, Wan-Seop Kim, Se Jin Jang, Yoo Duk Choi, Sunhee Chang, Soon Hee Jung, Lucia Kim, Mee Sook Roh, Choong Sik Lee, Jung Weon Shim, Mi Jin Kim, Geon Kook Lee
QJM.2016; 109(3): 167. CrossRef - Epidermal Growth Factor Receptor Mutation and Anaplastic Lymphoma Kinase Gene Fusion: Detection in Malignant Pleural Effusion by RNA or PNA Analysis
Yi-Lin Chen, Chung-Ta Lee, Cheng-Chan Lu, Shu-Ching Yang, Wan-Li Chen, Yang-Cheng Lee, Chung-Hsien Yang, Shu-Ling Peng, Wu-Chou Su, Nan-Haw Chow, Chung-Liang Ho, Javier S Castresana
PLOS ONE.2016; 11(6): e0158125. CrossRef - IDH Mutation Analysis in Ewing Sarcoma Family Tumors
Ki Yong Na, Byeong-Joo Noh, Ji-Youn Sung, Youn Wha Kim, Eduardo Santini Araujo, Yong-Koo Park
Journal of Pathology and Translational Medicine.2015; 49(3): 257. CrossRef - Immunohistochemical demonstration of alteration of β-catenin during tumor metastasis by different mechanisms according to histology in lung cancer
XIANHUA XU, JI EUN KIM, PING-LI SUN, SEOL BONG YOO, HYOJIN KIM, YAN JIN, JIN-HAENG CHUNG
Experimental and Therapeutic Medicine.2015; 9(2): 311. CrossRef - Detection of EGFR-TK Domain–activating Mutations in NSCLC With Generic PCR-based Methods
Rajendra B. Shahi, Sylvia De Brakeleer, Jacques De Grève, Caroline Geers, Peter In’t Veld, Erik Teugels
Applied Immunohistochemistry & Molecular Morphology.2015; 23(3): 163. CrossRef - Frequent aerogenous spread with decreased E-cadherin expression of ROS1- rearranged lung cancer predicts poor disease-free survival
Yan Jin, Ping-Li Sun, Soo Young Park, Hyojin Kim, Eunhyang Park, Gilhyang Kim, Sukki Cho, Kwhanmien Kim, Choon-Taek Lee, Jin-Haeng Chung
Lung Cancer.2015; 89(3): 343. CrossRef - Membranous Insulin-like Growth Factor-1 Receptor (IGF1R) Expression Is Predictive of Poor Prognosis in Patients with Epidermal Growth Factor Receptor (EGFR)-Mutant Lung Adenocarcinoma
Eunhyang Park, Soo Young Park, Hyojin Kim, Ping-Li Sun, Yan Jin, Suk Ki Cho, Kwhanmien Kim, Choon-Taek Lee, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2015; 49(5): 382. CrossRef - Peptide Nucleic Acid Clamping Versus Direct Sequencing for the Detection of EGFR Gene Mutation in Patients with Non-small Cell Lung Cancer
Seong-Hoon Yoon, Yoo-Duk Choi, In-Jae Oh, Kyu-Sik Kim, Hayoung Choi, Jinsun Chang, Hong-Joon Shin, Cheol-Kyu Park, Young-Chul Kim
Cancer Research and Treatment.2015; 47(4): 661. CrossRef - Analysis of Mutations in Epidermal Growth Factor Receptor Gene in Korean Patients with Non-small Cell Lung Cancer: Summary of a Nationwide Survey
Sang Hwa Lee, Wan Seop Kim, Yoo Duk Choi, Jeong Wook Seo, Joung Ho Han, Mi Jin Kim, Lucia Kim, Geon Kook Lee, Chang Hun Lee, Mee Hye Oh, Gou Young Kim, Sun Hee Sung, Kyo Young Lee, Sun Hee Chang, Mee Sook Rho, Han Kyeom Kim, Soon Hee Jung, Se Jin Jang
Journal of Pathology and Translational Medicine.2015; 49(6): 481. CrossRef - Novel EGFR mutation-specific antibodies for lung adenocarcinoma: Highly specific but not sensitive detection of an E746_A750 deletion in exon 19 and an L858R mutation in exon 21 by immunohistochemistry
An Na Seo, Tae-In Park, Yan Jin, Ping-Li Sun, Hyojin Kim, Hyun Chang, Jin-Haeng Chung
Lung Cancer.2014; 83(3): 316. CrossRef - Simultaneous diagnostic platform of genotyping EGFR, KRAS, and ALK in 510 Korean patients with non‐small‐cell lung cancer highlights significantly higher ALK rearrangement rate in advanced stage
Tae‐Jung Kim, Chan Kwon Park, Chang Dong Yeo, Kihoon Park, Chin Kook Rhee, Jusang Kim, Seung Joon Kim, Sang Haak Lee, Kyo‐Young Lee, Hyoung‐Kyu Yoon
Journal of Surgical Oncology.2014; 110(3): 245. CrossRef - Epidermal growth factor receptor mutations and anaplastic lymphoma kinase rearrangements in lung cancer with nodular ground-glass opacity
Sung-Jun Ko, Yeon Joo Lee, Jong Sun Park, Young-Jae Cho, Ho Il Yoon, Jin-Haeng Chung, Tae Jung Kim, Kyung Won Lee, Kwhanmien Kim, Sanghoon Jheon, Hyojin Kim, Jae Ho Lee, Choon-Taek Lee
BMC Cancer.2014;[Epub] CrossRef - Cytoplasmic YAP Expression is Associated with Prolonged Survival in Patients with Lung Adenocarcinomas and Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor Treatment
Ping-Li Sun, Ji Eun Kim, Seol Bong Yoo, Hyojin Kim, Yan Jin, Sanghoon Jheon, Kwhanmien Kim, Choon Taek Lee, Jin-Haeng Chung
Annals of Surgical Oncology.2014; 21(S4): 610. CrossRef - Sensitive methods for detection of the S768R substitution in exon 18 of the DDR2 gene in patients with central nervous system metastases of non-small cell lung cancer
Marcin Nicoś, Tomasz Powrózek, Paweł Krawczyk, Bożena Jarosz, Beata Pająk, Marek Sawicki, Krzysztof Kucharczyk, Tomasz Trojanowski, Janusz Milanowski
Medical Oncology.2014;[Epub] CrossRef - Clinicopathologic and prognostic significance of c-MYC copy number gain in lung adenocarcinomas
A N Seo, J M Yang, H Kim, S Jheon, K Kim, C T Lee, Y Jin, S Yun, J-H Chung, J H Paik
British Journal of Cancer.2014; 110(11): 2688. CrossRef - KRASMutation Detection in Non-small Cell Lung Cancer Using a Peptide Nucleic Acid-Mediated Polymerase Chain Reaction Clamping Method and Comparative Validation with Next-Generation Sequencing
Boram Lee, Boin Lee, Gangmin Han, Mi Jung Kwon, Joungho Han, Yoon-La Choi
Korean Journal of Pathology.2014; 48(2): 100. CrossRef - Guideline Recommendations forEGFRMutation Testing in Lung Cancer: Proposal of the Korean Cardiopulmonary Pathology Study Group
Hyo Sup Shim, Jin-Haeng Chung, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Geon Kook Lee, Soon-Hee Jung, Se Jin Jang
Korean Journal of Pathology.2013; 47(2): 100. CrossRef - Immunohistochemical Classification of Primary and Secondary Glioblastomas
Kyu Sang Lee, Gheeyoung Choe, Kyung Han Nam, An Na Seo, Sumi Yun, Kyung Ju Kim, Hwa Jin Cho, Sung Hye Park
Korean Journal of Pathology.2013; 47(6): 541. CrossRef
- Recent Trends of Lung Cancer in Korea
- Cystic Nephroma: A Case Report and Comparing Literature Review with Mixed Epithelial and Stromal Tumor of Kidney.
- Hyun Jung Kim, Choong Hee Noh, Giyoung Kwon, Eunah Shin, Jung Yeon Kim, Kyeongmee Park
- Korean J Pathol. 2011;45:S25-S28.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.S1.S25
- 3,604 View
- 43 Download
-
 Abstract
Abstract
 PDF
PDF - Cystic nephroma (CN) is a benign cystic neoplasm composed of mixed epithelial and stromal elements. Less than 200 cases have been reported. We had a patient, a 41-year-old woman, who had a huge typical CN. The patient was admitted for a right renal mass that was found incidentally. On laparaoscopic right nephrectomy, there was an encapsulated 7 cm multilocular cystic mass at the upper pole. Microscopically, the cystic wall was lined by a single layer of low cuboidal or hobnail epithelium without a solid area. The thin septa were composed of bland, ovarian type spindle cells. The main differential diagnoses were mixed epithelial and stromal tumor (MEST), low grade multilocular renal cell carcinoma, and tubulocystic carcinoma. The results of immunohistochemical staining were cytokeratin 7/19(+/+) and CD10(-) in lining epithelium, estrogen receptor/progesterone receptor(+/+) in stromal cells. After surgery, she was free of recurrence for 10 months. We report this rare case and compare it with other cystic renal tumors, especially MEST.
- SSTR2A Protein Expression in Neuroendocrine Neoplasms of the Colorectum.
- Young Eun Kim, Jeeyun Lee, Young Suk Park, Kyoung Mee Kim
- Korean J Pathol. 2011;45(3):276-280.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.3.276
- 4,191 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Expression studies of somatostatin receptor type 2A (SSTR2A) in neuroendocrine neoplasms (NENs) led to the development of clinically relevant diagnostic and therapeutic strategies. However, most of these strategies used in-house-developed antibodies and were focused on lung tumors. We evaluated commercially available SSTR2A antibodies in NENs of the colorectum to observe their subcellular localization and distribution within the resected tumor.
METHODS
The immunohistochemistry of 77 NENs located in the colorectum were studied using a commercially available antibody against SSTR2A.
RESULTS
Most neuroendocrine tumors (NET) grade (G)1 and G2 expressed the SSTR2A in the cytoplasm with apical or luminal localization. However, all neuroendocrine carcinomas (NEC) G3 were negative for SSTR2A.
CONCLUSIONS
Our data indicate that SSTR2A immunohistochemistry shows cytoplasmic staining with distinct subcellular localization in most NET G1 in the colorectum using a commercially available antibody. Low or no expression of SSTR2A in NET G2 and NEC G3 raises the possibility that SSTR2A may correlate with histologic differentiation and proliferative activity. Further validation studies in large case series are needed.
- Pathologic Characteristics of Ovarian Hemorrhagic Polycyst in Estrogen Receptor-alpha (ERalpha) Knockout Mice and Roles of ERalpha in Hemorrhagic Polycyst.
- Hyun Jin Son, Joo Heon Kim, Hye Kyung Lee, Mee Ja Park, Dong Wook Kang, Che Myong Ko
- Korean J Pathol. 2010;44(4):376-383.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.4.376
- 3,918 View
- 53 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Polycystic ovary syndrome (PCOS) is the most common endocrinopathy causing anovulation in women of childbearing age. It has been well established that estrogen receptor-alpha knockout (ERalphaKO) mice display several pathologic ovarian phenotypes of PCOS. The aims of this study were to determine ovarian pathology in new ERalphaKO mice using a CreloxP approach and intra-ovarian ERalpha function as regulating key aspects of PCOS.
METHODS
ERalphaKO mice, which were deficient in exon 3 of the ERalpha gene, were used. Immunohistochemical studies were done on ovaries of control and ERalphaKO mice using antibodies specific to ERalpha, ERbeta, inhibin-alpha, and alpha-smooth muscle actin (SMA), as well as histochemical staining using Sudan black-B.
RESULTS
All ovaries of ERalphaKO mice were larger than control mouse ovaries and displayed a disrupted theca-interstitial tissue organization, multiple atretic follicles and multiple hemorrhagic cysts. None of the ERalphaKO mouse ovaries showed a corpus luteum. In addition, heavy deposition of Sudan black-B positive foamy cells was seen. The theca externa of preantral immature follicles and hemorrhagic cysts showed strong expression of alpha-SMA.
CONCLUSIONS
ERalphaKO mice show hemorrhagic polycystic ovaries and hyperplasia of the theca externa. This study demonstrates that the ERalpha is the functional key to the pathogenesis of PCOS.
- Microvessel and Lymphatic Vessel Density and VEGFR-3 Expression of Papillary Thyroid Carcinoma with Comparative Analysis of Clinicopathological Characteristics.
- Harin Cheong, Hanna Kang, Hyung Kyung Kim, Ji Yoon Bae, Dong Eun Song, Min Sun Cho, Sun Hee Sung, Woon Sup Han, Heasoo Koo
- Korean J Pathol. 2010;44(3):243-251.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.3.243
- 4,393 View
- 32 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
This study was done to see if there were correlations between anatomic and molecular parameters such as microvessel density (MVD), lymphatic vessel density (LVD), and vascular endothelial growth factor receptor (VEGFR)-3 expression and various clinical parameters for papillary thyroid carcinomas of size > 1.0 cm (PTCs) and size < or = 1.0 cm (papillary thyroid microcarcinomas, PTMCs). PTMCs were divided into two subgroups (0-5 mm and 6-10 mm).
METHODS
We analyzed 197 thyroid carcinomas including 113 PTCs and 84 PTMCs. Tissue samples form 30 patients from each group matched for clinical characteristics were selected for immunostaining.
RESULTS
Although PTCs and PTMCs showed significant differences in clinical characteristics, they did not show significant difference in MVD, LVD, or VEGFR-3 expression. There was a significantly higher LVD in the PTMC subgroup with the larger tumors but no difference in clinical characteristics. LVD was higher in patients > 45 years old (more apparent in the PTC group) and LVD had suggestive correlations with multicentricity and extrathyroidal extension depending on analytic conditions.
CONCLUSIONS
Since LVD showed variable correlations with clinical variables for papillary carcinoma of the thyroid depending on analytic conditions, the individually planned treatments based on overall clinicopathological factors are advised. -
Citations
Citations to this article as recorded by- Freeze-dried bovine amniotic membrane as a cell delivery scaffold in a porcine model of radiation-induced chronic wounds
Daemyung Oh, Daegu Son, Jinhee Kim, Sun-Young Kwon
Archives of Plastic Surgery.2021; 48(4): 448. CrossRef - Polydeoxyribonucleotide Improves Peripheral Tissue Oxygenation and Accelerates Angiogenesis in Diabetic Foot Ulcers
Seoyoung Kim, Junhyung Kim, Jaehoon Choi, Woonhyeok Jeong, Sunyoung Kwon
Archives of Plastic Surgery.2017; 44(06): 482. CrossRef
- Freeze-dried bovine amniotic membrane as a cell delivery scaffold in a porcine model of radiation-induced chronic wounds
- An Approach to Diagnosing Gastrointestinal Stromal Tumors Using Immunohistochemistry of c-kit and PDGFRA with Molecular Analysis.
- Jeong Shik Kim, Jae Hoon Kim, Hyun Jin Oh, In Soo Suh, Jong Gwang Kim, Byung Wook Kang, Wan Sik Yu, Ho Young Chung, Han Ik Bae
- Korean J Pathol. 2010;44(2):173-178.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.2.173
- 4,029 View
- 45 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumors in the gastrointestinal tract. Recently, many methods for the diagnosis of GIST have been developed including molecular diagnosis.
METHODS
We selected 90 cases of GIST that had presented at Kyungpook National University Hospital between 1998 and 2007. Tissue microarrays were made using core areas of tumor tissues. Immunohistochemical staining for c-kit, protein kinase C-theta, and platelet-derived growth factor receptor alpha (PDGFRA) was done. Direct sequencing of hot spot exonal areas for c-kit and PDGFRA were done using extracted DNAs of all 90 paraffin block tissues.
RESULTS
Among the 90 cases, 83.3% (75/90) were c-kit positive, 16.6% (15/90) were c-kit negative, 93.3% (84/90) were PDGFRA positive, and 6.6% (6/90) cases were PDGFRA negative. Fifteen cases of c-kit negative GIST included 1 case of PDGFRA negative and 5 cases of PDGFRA negative GIST were ckit positive. The one case in which both c-kit and PDGFRA were negative, showed a c-kit mutation in exon 11.
CONCLUSIONS
Combined immunohistochemical staining of c-kit, discovered on GIST 1 (DOG1) and PDGFRA is helpful for the diagnosis of GIST. When all staining tests are negative for immunoreactivity, c-kit mutation analysis for exon 11, 9 should be done. Genotyping of kit and PDGFRA do not need to be examined initially, if it is only for the diagnosis of GIST.
- KIT/PDGFRA Expression and Mutation in Testicular Seminoma and Ovarian Dysgerminoma.
- Song Yi Choi, Kwang Sun Suh, Yong Beom Kim, Hyun Jeong Lee, Eun Sun Kim, Mee Ja Park
- Korean J Pathol. 2009;43(6):528-534.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.6.528
- 4,705 View
- 22 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
KIT and PDGFRA are tyrosine kinase receptors. Stem cell factor/KIT-mediated signaling plays a role in normal spermatogenesis, and the alteration of KIT is important in the pathogenesis of seminomas/dysgerminomas (SD). METHODS: To determine the role of expression and mutation of the KIT and PDGFRA genes, we analyzed 16 seminoma cases, 4 spermatocytic seminoma (SS) cases and 8 dysgerminoma cases for KIT and PDGFRA expression and mutation of KIT (exons 9, 11, 13, and 17) and PDGFRA (exons 12 and 18) using PCR-SSCP methods. RESULTS: KIT was immunohistochemically positive in all 24 SD cases, and one of four (25%) SS cases. PDGFRA was immunohistochemically evident in 16 of the 24 (66.6%) SD cases, and two of the four (50%) SS cases. KIT expression was significantly reduced in SS compared with seminoma (p=0.0035). Four cases (14.3%) displayed mutation in KIT exon 17 or PDGFRA exon 12. Distant metastasis was present in three cases (10.7%), one of which had a nonsense mutation in KIT. CONCLUSIONS: These results indicate that KIT is expressed in the majority of SD cases, but not in most SS cases. However, there was no significant correlation between the clinicopathologic features and mutation or expression of KIT and PDGFRA. -
Citations
Citations to this article as recorded by- Expression of DOG1, PDGFRA, and p16 in Gastrointestinal Stromal Tumors
Sung Hee Jung, Kwang Sun Suh, Dae Young Kang, Dong Wook Kang, Young-Beum Kim, Eun-Sun Kim
Gut and Liver.2011; 5(2): 171. CrossRef
- Expression of DOG1, PDGFRA, and p16 in Gastrointestinal Stromal Tumors
- Intron 1 Polymorphism, Mutation and the Protein Expression of Epidermal Growth Factor Receptor in Relation to the Gefitinib Sensitivity of Korean Lung Cancer Patients.
- Mi Jin Kim, Kyeong Cheol Shin, Kwan Ho Lee
- Korean J Pathol. 2009;43(6):509-516.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.6.509
- 3,579 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Epidermal growth factor receptor (EGFR) intron 1 polymorphism in non-small cell lung cancer (NSCLC) has been found to have therapeutic implications for the patients treated with EGFR tyrosine kinase inhibitors. However, its clinical significance as related to gefitinib responsiveness is still controversial. We examined CA repeat polymorphism in intron 1 of the EGFR gene and its relation with the EGFR gene mutation in NSCLC patients who were treated with gefitinib. METHODS: Sixty seven patients who were treated with gefitinib were analyzed for intron 1 polymorphism in the EGFR gene, the EGFR mutations and the EGFR protein expression. Two hundred twenty seven samples of NSCLC were analyzed for EGFR mutations. RESULTS: CA repeat was low in 27 patients (40.3%) and high in 40 (59.7%) patients. The response rate for gefitinib therapy was higher in the patient population with a low number of CA repeats in the EGFR gene (p=0.047) and in the patients with the mutated type of EGFR (p=0.048), though these two factors were not related. Thirty four patients (15.0%) harbored EGFR mutations. CONCLUSIONS: This study suggests that the intron 1 CA repeat polymorphism of the EGFR gene may serve as a predictor of the clinical outcome of NSCLC patients treated with gefitinib, and this without regard for EGFR mutation. Our data further supports the importance of EGFR mutations with regard to a distinct clinical profile and the prognostic implications for NSCLC patients.
- The EGFR Protein Expression and the Gene Copy Number Changes in Renal Cell Carcinomas.
- Sangho Lee, Jungsuk An, Aeree Kim, Young Sik Kim, Insun Kim
- Korean J Pathol. 2009;43(5):413-419.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.5.413
- 4,606 View
- 21 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The epidermal growth factor receptor (EGFR) is known to be involved in many tumor promoting activities. EGFR inhibition has been tried as a therapeutic modality in many human malignancies.
METHODS
The expression of EGFR protein and the gene copy number changes were studied in 135 clear cell carcinomas and 16 papillary renal cell carcinomas (RCCs), and these tumors were diagnosed between 1995 and 1997.
RESULTS
An EGFR protein expression (2+ and 3+) was found in 54.1% of the clear cell RCCs and in 43.8% of the papillary RCCs. In the clear cell RCCs, its expression was associated with male gender, the tumor size (> or =4 cm) and high T stages (T2 and T3), with statistical significance. Trisomy and polysomy of the EGFR gene were found in 27 (25.7%) and 40 (38.1%) of 105 clear cell RCCs, respectively. Trisomy and polysomy were correlated with an EGFR protein expression and a high clinical T stage, with statistical significance. Among 15 papillary RCCs, 13 tumors showed trisomy (86.7%) and one showed polysomy (6.7%). Amplification was not found in both the clear cell and papillary type RCCs.
CONCLUSIONS
A considerable numbers of RCCs showed an overexpression of EGFR protein and increased EGFR gene copy numbers, yet the clinical significance of conducting a FISH study in RCC patients seems to be limited. -
Citations
Citations to this article as recorded by- EGFR protein overexpression correlates with chromosome 7 polysomy and poor prognostic parameters in clear cell renal cell carcinoma
Gordana Đorđević, Koviljka Matušan Ilijaš, Ita Hadžisejdić, Anton Maričić, Blaženka Grahovac, Nives Jonjić
Journal of Biomedical Science.2012;[Epub] CrossRef
- EGFR protein overexpression correlates with chromosome 7 polysomy and poor prognostic parameters in clear cell renal cell carcinoma
- The Expressions of Nerve Growth Factor and Its Receptor p75NGFR in Hepatocellular Carcinoma: Their Relation with the Clinicopathologic Factors.
- Woo Sung Moon, Kyu Yun Jang, Myoung Ja Chung, Myoung Jae Kang, Dong Geun Lee, Ho Lee, Ho Sung Park
- Korean J Pathol. 2009;43(2):145-151.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.2.145
- 4,773 View
- 24 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Nerve growth factor (NGF) has been suggested to participate in tumor progression and it can interact with its receptor p75NGFR. In the present study, we investigated the expressions of NGF and p75NGFR in hepatocellular carcinoma (HCC).
METHODS
We performed immunohistochemistry for NGF, p75NGFR and PCNA in 45 cases of HCCs, and examined the relationships between the clinicopathologic factors and the immunohistochemical results.
RESULTS
NGF was detected in 84.4% (38/45) of the tumor cells and in 64.4% (29/45) of the non-tumorous hepatocytes. Furthermore, a NGF expression was present in 28.9% (13/45) of the endothelial cells in the HCCs, but in 80% (36/45) of the endothelial cells in the non-tumor liver tissue. The tumor cells were negative for p75NGFR in all the HCCs. Although a p75NGFR expression was present in all the nerve fibers in the non-tumor liver tissues, it was markedly reduced (42.2%; 19/45) in the HCCs and a p75NGFR expression was observed at the sinusoids or around the large vessels. The HCCs expressing NGF, either in the tumor cells or the endothelial cells, showed a larger size than those HCCs that didn't express NGF. The NGF positive tumors showed a tendency toward a higher PCNA-labeling index than did the negative tumors.
CONCLUSIONS
The changed localization of the NGF expression and the decreased expression of p75NGFR are associated with hepatic carcinogenesis. We suggest that a NGF expression may contribute to the progression of HCC. -
Citations
Citations to this article as recorded by- Expression of nerve growth factor and heme oxygenase-1 predict poor survival of breast carcinoma patients
Sang Jae Noh, Jun Sang Bae, Urangoo Jamiyandorj, Ho Sung Park, Keun Sang Kwon, Sung Hoo Jung, Hyun Jo Youn, Ho Lee, Byung-Hyun Park, Myoung Ja Chung, Woo Sung Moon, Myoung Jae Kang, Kyu Yun Jang
BMC Cancer.2013;[Epub] CrossRef
- Expression of nerve growth factor and heme oxygenase-1 predict poor survival of breast carcinoma patients
- Metaplastic Squamous Carcinoma of the Breast: Clinicopathologic Analysis of 17 Cases.
- Sun Ah Lee, Kyung Eun Lee, Byung In Moon, Woon Sup Han, Sun Hee Sung
- Korean J Pathol. 2009;43(1):20-25.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.1.20
- 4,948 View
- 48 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Squamous cell carcinoma of the breast is very rare and it is considered to arise from metaplastic change of ductal carcinoma. Metaplastic squamous cell carcinoma (MSC) of the breast includes pure squamous cell carcinoma, metaplastic adenosquamous carcinoma and low grade adenosquamous carcinoma. Most of the cases of MSC of the breast were reported to have lymph node metastasis and this has a worse prognosis than that of conventional invasive ductal carcinoma.
METHODS
We collected 17 cases of MSC of the breast from 1,173 cases of breast cancer and analyzed the clinicopathological characteristics.
RESULTS
The age range was 31 to 69 years (mean age: 47.2). The mean tumor size was 3.6 cm. Twelve cases (70.6%) had a negative nodal status. The majority of the cases were of a high nuclear grade (grade III: 76.5%), and a high histologic grade (grade III: 88.2%). All the cases had no amplification of HER2, and they were negative for hormonal receptors, except for 2 cases with weak positivity. All the cases showed positivity for EGFR (3+: 14 cases, 1+: 3 cases). Clinical relapse was found in 3 patients on follow up and two of them expired due to lung and bone metastasis.
CONCLUSIONS
MSC is associated with high nuclear and histologic grades, a high EGFR expression and they are triple negative for ER, PR, and HER2. The EGFR immunopositivity of MSC suggests a basal-like subtype. -
Citations
Citations to this article as recorded by- Eccrine ductal and acrosyringeal metaplasia in breast carcinomas: report of eight cases
Tibor Tot
Virchows Archiv.2019; 474(3): 383. CrossRef - Significance of Foxp3 Positive Regulatory T Cell and Tumor Infiltrating T Lymphocyte in Triple Negative Breast Cancer
Hanna Kang, Harin Cheong, Min Sun Cho, Heasoo Koo, Woon Sup Han, Kyung Eun Lee, Byung In Moon, Sun Hee Sung
The Korean Journal of Pathology.2011; 45(1): 53. CrossRef
- Eccrine ductal and acrosyringeal metaplasia in breast carcinomas: report of eight cases
- Pathological Analysis of 15 Cases of Phyllodes Tumors of the Breast.
- Sung Nam Kim, Woo Ho Kim, Sang Kook Lee
- Korean J Pathol. 1993;27(1):19-26.
- 2,157 View
- 15 Download
-
 Abstract
Abstract
 PDF
PDF - Retrospective clinicopathologic analysis of 15 patients with the phyllodes tumors(PT) of the breast, diagnosed at SNUH over 6 years period, was done. By light microscopy, 8 cases were diagnosed as benign, and 7 cases were diagnosed as malignant. Mean ages o the patients were 37 and 34 years in malignant and benign, respectively. Most of those cases were presented with a palpable mass of the breast. None of the patients with malignant PT had distant metastasis, Local recurrences were experienced in 3 patients among the malignant PT, and one patient among the benign PT. One of 7 malignant PT was coexisted with simultaneous ipsilateral infiltrating duct carcinoma. The clinical course was not well correlated with pathologic features. The prognostic significances of several histopathologic parameters were assessed for possible correlation with local recurrence, metastasis and death; stromal cellularity, stromal cellular atypism, mitotic activity, tumor contour, necrosis, tumor size and heterologous stromal elements. Immunohistochemistry using antibody to vimentin, proliferating cell nuclear antigen(PCNA) and epidermal growth factor receptor(EGF-R) were analysed. In the 5 cases of benign PT, the stromal cells stained diffusely positive for vimentin and 3 cases of malignant tumors show similar staining for vimentin. The percentage of PCNA-positive cells were higher in the malignant PT than in the benign ones; they were 3.5% to 60% in malignancy, while they were less than 60% in all benign PT. The results of EGF-R staining were correlated with the histologic classification; only 2 cases out of 8 benign PT show diffusely positive staining of EGF-R in the cytoplasm, but 6 cases out of 7 malignant PT show positive findings.
- The Expression of Transforming Growth Factor-1 and Its Signaling Receptors in Human Colorectal Carcinoma.
- Gyeong Seon Kim, Joo Heon Kim, Woo Sung Moon, Myoung Ja Chung, Dong Geun Lee, Myoung Jae Kang
- Korean J Pathol. 2001;35(2):115-122.
- 2,066 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Resistance to the potent growth inhibitory effects of TGF- (transforming growth factor-) is a characteristic of many malignancies. TGF- insensitivity has been attributed to alterations in the number and function of the TGF- receptors as well as disturbances of downstream signal transduction. The aim of this study was to examine the expression of TGF-1 and its receptors in human colorectal cancer tissue and determine its relationship with cancer growth and with prognostic factors.
METHODS
Immunohistochemical staining of TGF-1, TGF-RI, and TGF-RII was performed on 20 human colorectal adenomas, 30 carcinomas and 10 normal mucosas as a control.
RESULTS
The staining indices of TGF-1, TGF-RI, and TGF-RII increased in adenomas and carcinomas compared with normal mucosas and adenomas, respectively. In adenomas the staining index of TGF-1 significantly increased with the severity of atypism. The staining index of TGF-RII increased in the carcinomas in the right colon and rectum, compared with those in the left colon.
CONCLUSION
The enhanced expression of TGF-1, TGF-RI and II in the colorectal carcinoma suggests an important role of colorectal carcinogenesis and tumor progression.
- Angioleiomyoma of the Nasal Cavity: A Case Report.
- Su Jin Kim, Sook Hee Hong, Mee Sook Roh
- Korean J Pathol. 2004;38(3):181-183.
- 2,116 View
- 15 Download
-
 Abstract
Abstract
 PDF
PDF - Angioleiomyoma of the sinonasal area is an extremely rare benign neoplasm. To the best of our knowledge, only 26 cases have been described. Here, we report a case of angioleiomyoma arising in the nasal cavity of a 60-year-old woman. Microscopically, the tumor consisted of proliferating smooth muscle cells punctuated with thick-walled vessels with slit-like lumina. The tumor was negative for estrogen and progesterone receptor by immunohistochemical study. Further studies are needed to clarify whether the growth of this tumor is sex steroid-dependent.
- Application of Gene Rearrangement Analysis for Diagnosis of Malignant Lymphoma.
- Kyung Soo Kim, Chan Choi
- Korean J Pathol. 1995;29(4):415-422.
- 2,095 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - To evaluate the utility of gene rearrangement analysis, eight cases of malignant lymphoma, one case of Hodgkin's disease, two cases of angioiminunoblastic lymphadenopathy (AILD) and two cases of non-specific lymphadenitis were studied by immunohistochemical and genetic analysis. Southern blot analysis was perfon-ned by a using vacuum transfer system and a biotin labelled probe. This method was faster, safer, and more convenient than conventional methods. Gene rearrangement study showed rearranged novel bands in five of six cases of B cell lymphoma, in all cases of T cell lymphoma, and in all cases of AILD. No rearrangement of the B cell receptor(BCR) or of the T cell receptor(TCR) was seen in Hodgkin's disease or in nonspecific lymphadenitis. These results suggest that gene rearrangement analysis of BCR and TCR is a recommended method for the diagnosis of clonality in lymphoproliferative disorders. It would allow pathologists to differentiate lymphoma from polyclonal lymphoid proliferation and to provide information for cell lineage.
- The Expression of c-erbB-2, EGFR, p53 and Ki-67 in Ovarian Borderline Tumors and Carcinomas of the Ovary.
- Kyueng Whan Min, Moon Hyang Park
- Korean J Pathol. 2007;41(5):296-306.
- 2,647 View
- 63 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
An ovarian surface epithelial tumor is a heterogenous disease, and various biological and molecular factors are important for its development and progression. Several findings support EGFR or c-erbB-2 as adverse prognostic indicators for an ovarian carcinoma.
METHODS
We reviewed the histological and clinical findings of 52 carcinomas (17 endometrioid, 16 serous, 13 mucinous and 6 clear cell tumors), and 26 borderline (10 serous and 16 mucinous) tumors. Expression of c-erbB-2, EGFR, p53, and Ki-67 was evaluated on paraffinembedded tissue from a primary ovarian tumor by immunohistochemical methods.
RESULTS
Expression of c-erbB-2 was found in 7.6% of tumors and expression of EGFR was found in 9.6% of tumors by immunohistochemical analysis. No significance was found between cerbB- 2 and EGFR expression as indicators of a poor prognosis. The expression of p53 and Ki-67 (>50%) correlated with the grade and type of tumor in the ovarian cancers. p53 and Ki- 67 overexpression (>50%) was absent in the borderline ovarian tumors, whereas ovarian carcinomas showed expression of both p53 and Ki-67.
CONCLUSION
Expression of c-erbB- 2, EGFR, p53, and Ki-67 as determined by immunohistochemical analysis did not correlate with prognostic significance. However, p53 and Ki-67 expression may be used as markers to predict aggressive behavior, and to differentiate between malignant and borderline epithelial ovarian tumors. Further large-scale studies are required to clarify the significance of c-erbB-2 and EGFR expression in ovarian tumors.
- Epidermal Growth Factor Receptor Overexpression and the Tumor Response to Preoperative Radiochemotherapy for Patients with Advanced Rectal Cancer.
- Jinyoung Yoo, Ju Won Chyung, Ji Han Jung, Hyun Joo Choi, Seok Jin Kang, Kyo Young Lee
- Korean J Pathol. 2007;41(5):316-323.
- 2,112 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
An association between the epidermal growth factor receptor (EGFR) signaling pathway and the response of cancer cells to ionizing radiation has been previously described. Preoperative radiochemotherapy (PRCT) has been administered for treating locally advanced rectal cancer to improve the outcomes, and to preserve the sphincter from lowlying tumor. However, the responses of tumors to PRCT are variable and there are currently no reliable markers that predict the therapeutic benefits. We studied the association between EGFR overexpression and the tumor response to PRCT in rectal cancer.
METHODS
The EGFR protein expression, as determined by immunohistochemistry, was analyzed in the pretreatment biopsy specimens from 120 patients with advanced rectal cancer. The tumor response was graded in the surgically resected specimens by using a three-scale grading system: no response (NR), partial remission (PR) and complete remission (CR).
RESULTS
NR was identified in 70 cases (58.3%). Fifty patients (41.7%) responded to PRCT; 27 (22.5%) achieved a PR and 23 (19.2%) achieved a CR. EGFR overexpression was detected in 78 (65%) cases. Seventy-eight percent (39/50) of the tumors with a CR/PR revealed EGFR reactivity, whereas 55.7% (39/70) of the tumors with NR showed an EGFR expression (p=0.048).
CONCLUSIONS
The EGFR protein expression might be a valuable marker for identifying those patients who are most likely to benefit from PRCT.
- Rarity of EGFR and c-ErbB-2 Overexpressions in Hepatocellular Carcinoma: An Immunohistochemical Study.
- Woo Sung Moon, Hyun Jin Son, Ho Sung Park, Min Young Park
- Korean J Pathol. 2004;38(4):244-248.
- 2,303 View
- 13 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The overexpression of epidermal growth factor receptor (EGFR) and c-erbB-2 oncogenes has been implicated in the development of many types of cancer. However, the role of EGFR and c-erbB-2 overexpression in hepatocellular carcinoma (HCC) has not been fully elucidated.
METHODS
The aim of this study was to evaluate the immunohistochemical expression of EGFR and c-erbB-2 oncoprotein in a series of 52 HCCs.
RESULTS
All but one of the HCC tumor tissues were negative for EGFR monoclonal antibody, clone H11. All of the HCC tumor tissue samples were negative for EGFR monoclonal antibody, clone 29.1.1. However, strong EGFR immunoreactivity was detected in sinusoidal endothelial cells of HCC in 25 tumors (48%) using EGFR 29.1.1 antibody. The expression of c-erbB-2 was observed in 6% (3/52) of the HCCs. No significant correlation was found between p53 mutation and the expression of c-erbB-2.
CONCLUSION
Our results suggest that both EGFR and c-erbB-2 oncoprotein overexpressions in tumor cells are rare and do not seem to predominantly contribute to the malignant phenotype in HCC.
- Clinicopathologic Analysis of Epidermal Growth Factor Receptor Status in Non-small Cell Lung Cancer: Protein Expression, Gene Amplification and Survival Analysis.
- Seungkoo Lee, Jene Choi, Se Jin Jang
- Korean J Pathol. 2007;41(6):387-392.
- 2,020 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Abnormal over-expression or gene amplification of epidermal growth factor receptor (EGFR) is important in the prognosis of non-small cell lung cancer (NSCLC). We investigated the frequency of EGFR protein expression and gene amplification, and the correlation between EGFR status and survival in NSCLC.
METHODS
We examined 360 cases of microarrayed NSCLC tissues for the EGFR protein expression and EGFR gene amplification using immunohistochemistry and fluorescent in situ hybridization.
RESULTS
EGFR protein expression and EGFR gene amplification occurred in 110 cases (30.6%) and 24 cases (6.7%), respectively. EGFR protein expression and gene amplification were more frequent in squamous cell carcinoma than in adenocarcinoma. Differences in EGFR protein expression did not dramatically affect survival curves (p=0.740), but differences in gene amplification did (p<0.05): EGFR gene amplification was associated with a lower 5-year survival rate.
CONCLUSION
EGFR protein expression and gene amplification showed moderate correlation with each other. EGFR gene amplification predicted a poor prognosis, whereas EGFR protein expression did not.
- The Effects of Excitatory Amino Acids and Their Receptors on Neuronal Damage of Rat Brain in Hypoxic-Ischemic Encephalopathy.
- Heasoo Koo
- Korean J Pathol. 1995;29(5):545-562.
- 1,853 View
- 10 Download
-
 Abstract
Abstract
- Since the role of excitatory amino acids such as glutamate and aspartate and their receptors mediating cellular injury through various mechanisms were known in hypoxic-ischemic injury and associated diseases of central nervous system, blocking agents for transmitter release or receptors have been tried to reduce the cellular damages and subsequent sequelae experimentally. Several in vitro studies suggested two kinds of glutamate neurotoxicity: (1) rapid toxicity due to influx of sodium or chloride with resultant cellular edema and consequent damage, which is associated with N-methyl-D-Aspartate(NMDA) as well as non-NMDA receptors, (2) calcium mediated delayed toxicity associated mainly with NMDA receptor. This study was conducted to investigate the role of rapid toxicity in hypoxic-ischemic injury. Early lesions of 30 minutes to 24 hours after hypoxic-ischemic insult were examined by autoradiography with radiolabelled glutamate and kainitic acid (KA) as well as light and electron microscopy. Late changes were evaluated on formaldehyde-acetic acid-methanol(FAM) fixed brain 1 week after the insult. Cornus ammonis(CA) l of hippocampus showed the highest density of NMDA receptors, which was decreased constantly from 2 hours to 24 hours. In contrast, CA3 of hippocampus showed the highest density of KA receptors, which was the lowest at 6 hour and increased thereafter. Light microscopic examination showed the worst changes during 30 minutes to 6 hours. After 1 week, most of the cases showed degeneration of neurons and CAI and CA3 did not show the difference. Electron microscopic examination showed marked degenerative changes of neurons as well as neuropils starting from 30 minutes after the insult. In conclusion, rapid toxicity mediated by non-NMDA(KA) receptor seen in CA3 lead to permanent damage in 1 week old lesion.
- The Difference of Cathepsin D Expression between Invasive Ductal Carcinoma and Ductal Carcinoma In Situ of the Breast.
- Hye Kyoung Yoon, Soo Jin Jung
- Korean J Pathol. 2004;38(6):408-414.
- 2,079 View
- 15 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It is known that cathepsin D expression in host stromal cells is associated with a more aggressive tumor behavior in breast cancers.
METHODS
Cathepsin D expression was examined in 222 cases of invasive ductal carcinoma (CA) and 25 cases of ductal carcinoma in situ (DCIS) by the immunohistochemical staining. Cathepsin D expression was evaluated according to the expression site, either in the tumor cells (CD-T) or in the stromal cells (CD-S), and graded according to the immunopositivity. The differences of CD-T and CD-S in each case were evaluated according to the pathologic parameters and estrogen receptor (ER)/progesterone receptor (PR) status.
RESULTS
The rate of CD-S was significantly higher in the CA than in the DCIS (p<0.0001). In the CA, the rate of CD-S was higher than that of CD-T, while in the DCIS, the rate of CD-T was higher than that of CD-S. In the CA, the rate of CD-S and the tumor grade showed a positive relationship (p=0.0281). There were positive correlations between the ER positivity and CD-S (p=0.0236), and between the PR positivity and CD-T (p=0.0246). For the DCIS, no significant relationships were noted between the pathologic parameters including ER/PR status and CD-T/CD-S.
CONCLUSION
Cathepsin D expression in the stromal cells seems to be related to the invasiveness and aggressive biological behavior in breast cancers. In addition, there might be some relationship betweeen the ER positivity and CD-S, and between the PR positivity and CD-T.
- Epidermal Growth Factor Receptor Expression of Non-small Cell Carcinoma and Its Relationship with Genomic Mutation.
- Sang hee Seok, Mi Jin Kim
- Korean J Pathol. 2008;42(2):94-99.
- 2,199 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It has recently been clarified that epidermal growth factor receptor (EGFR), which is a receptor tyrosine kinase of the erbB family, is abnormally activated in non-small cell lung carcinomas (NSCLC) and this fact is being utilized for creating targeted therapy. In this study, we aimed to identify the frequency of the EGFR expression and gene mutation in NSCLC, and to determine the correlation between them.
METHODS
Immunohistochemical staining for EGFR, C-erbB-2, cytokeratin 7, p53 and thyroid transcription factor-1, and EGFR mutation analysis were performed using paraffin-embedded archival tissue from 228 cases of NSCLC; this included 112 squamous cell carcinomas and 116 adenocarcinomas.
RESULTS
An EGFR expression and gene mutation occurred in 112 casees (53.5%) and 52 cases (22.8%), respectively. EGRF mutation was more frequent in the adenocarcinomas than in the squamous cell carcinomas, in non-smokers than in smokers, and in females than in males. EGFR mutation was significantly associated with an EGFR protein expression, and especially in adenocarcinomas.
CONCLUSION
The EGFR expression in NSCLC was associated with EGFR mutation, and especially in adenocarcinomas. More studies are needed to prove the clinical significance of the EGFR expression for creating targeted therapy to treat NSCLC.
- The Expressions of Tyrosine Kinase Receptors, EphA2, c-met and c-erbB-2 in the Human Breast.
- Soo Kee Min, Hyun Deuk Cho, Seong Jin Cho, Hye Rim Park, Hyung Sik Shin, Young Euy Park, Bom Woo Yeom
- Korean J Pathol. 2005;39(1):15-22.
- 2,096 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Tyrosine kinase receptor (TKR) is an important protein for normal-development, growth and tumorigenesis in human tissues. The purpose of this study was to evaluate the effect of TKR in the progression of breast cancer.
METHODS
The expressions of EphA2, c-met and c-erbB-2 were examined, by using immunohistochemical methods and RT-PCR, in samples of breast tissue that included 111 samples of normal epithelium, 34 samples of ductal carcinoma in situ (DCIS), and 109 samples of invasive ductal carcinomas (IDC). The results were compared with the prognostic parameters of breast cancer including the tumor grade, growth pattern, lymph node metastasis and the expressions of ER, PR, p53 and Ki-67.
RESULTS
The protein expressions of the three TKRs were higher in DCIS and IDC than in normal epithelium. The protein expression of EphA2 was correlated with a tumor grade, a labeling index of Ki-67, and the protein expression of c-met. Overexpression of c-erbB-2 was correlated with lymph node metastasis. The mRNA levels of the three TKRs were correlated with each other in normal tissue and IDC. The level of c-met mRNA was higher in the low grade tumors.
CONCLUSIONS
The three TKRs may play roles in the tumorigenesis of human breast cancer. The overexpressions of EphA2 and c-erbB-2 may be a poor prognostic parameter in breast cancers.
- An Immunohistochemical Study of the Relationships between Estrogen and Progesterone Receptors and Proliferating Cell Nuclear Antigen in Endometrial Hyperplasia and Adenocarcinoma.
- Seol Mi Park, Hye Kyoung Yoon, Jong Eun Joo
- Korean J Pathol. 1996;30(1):15-22.
- 2,186 View
- 37 Download
-
 Abstract
Abstract
 PDF
PDF - Estrogen and progesterone receptors exist in the epithelial and stromal cells of the endometrium. Proliferative disorders of the endometrium may be associated with autocrine and paracrine actions of estrogen and progesterone in epithelial and stromal cells. This study was performed to evaluate the differences estrogen and progesterone receptor(ER/PR) expression in the epithelial and stromal cells of endometrial hyperplasias and adenocarcinomas using immunohistochemical methods. Immunohistochemical analysis of proliferating cell nuclear antigen(PCNA) was done to evaluate a possible correlation between PCNA and hormone receptor expression. Evaluation was based on samples from 31 simple hyperplasias, 30 complex hyperplasias, and 32 adenocarcinomas. The immunohistochemical expression of ER, PR and PCNA in epithelial and stromal cells were examined according to a scoring system based on the percentage of positive cells and the staining intensity. The results were as follows; 1) The expression of ER and PR in epithelial cells showed a graded, significant decreases in simple hyperplasia, complex hyperplasia and endometrial carcinoma, in that order(ER: P=0.008, PR: P= 0.026). 2) PR expression in the stromal cells showed a significant decrease between hyperplasia and adenocarcinoma(P=0.003). The difference in ER expression was not significant. 3) In stromal cells, the decrease in PR expression was more prominent than the decrease in ER expression when complex hyperplasia was compared to simple hyperplasia. 4) The PCNA expression in simple and complex hyperplasia and adenocarcinoma was not higher than the expression of PCNA in nomal proliferative endometrium. There was no significant difference in PCNA expression between simple and complex hyperplasia and adenocarcinoma(P=0.073). 5) A negative correlation between PCNA and ER/PR expression was not demonstrated in simple and complex hyperplasia, or in adenocarcinoma. Endometrial hyperplasia and adenocarcinoma are probably related to a paracrine action of estrogen and progesterone in epithelial and stromal cells. A progressive loss of PR expression in stromal cells may induce abnormal proliferation of endometrium due to a disrupted hormonal balance.
- Diffuse Leiomyomatosis of the Uterus: A Brief Case Report.
- Su Jin Kim, Mee Sook Roh
- Korean J Pathol. 2005;39(1):63-65.
- 3,385 View
- 97 Download
-
 Abstract
Abstract
 PDF
PDF - Diffuse leiomyomatosis of the uterus is a rare condition that is distinguished from the uterine leiomyoma due to the diffuse involvement of the myometrium by numerous, ill-defined, smooth muscle nodules. We present here a case of diffuse uterine leiomyomatosis in a 34-year-old woman. The hysterectomy revealed a symmetrically enlarged uterus containing numerous, small, ill-defined leiomyomatous nodules. Microscopically, the nodules were composed of compact fascicles and interweaving bundles of uniform benign smooth muscle cells. On the immunohistochemical staining, the progesterone receptor level was higher in the leiomyomatosis than in the adjacent normal myometrial tissue, but the estrogen receptor level and Ki-67 labeling index were equal in both areas. At the twelve months follow-up, this patient has been doing very well with no evidence of pelvic or intraabdominal recurrence of disease.
- S Phase Kinase Associated Protein 2 Expression in Breast Cancer and Its Prognostic Implications.
- Eun Deok Chang, Eun Jung Lee, Se Jeong Oh, Chang Suk Kang
- Korean J Pathol. 2005;39(2):69-73.
- 1,979 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
S Phase Kinase Associated Protein 2 (Skp2), an F-box protein necessary for DNA replication, has recently been demonstrated to be an oncogene. The purpose of this study was to examine the Skp2 expression and to investigate its association with expressions of estrogen receptor (ER), androgen receptor (AR) and HER-2, as well as clinicopathological variables including tumor recurrence.
METHODS
The expressions of Skp2, ER and AR were examined by immunohistochemistry and HER-2 amplification by chromogenic in situ hybridization (CISH) in 117 cases of breast carcinoma.
RESULTS
Skp2 was expressed in 26 patients (22.2%) and was significantly correlated with tumor type (p=0.031), tumor grade (p=0.017) and ER expression (p=0.038). Twenty four (20.5%) of 117 patients had a tumor recurrence, and 6 patients (5.1%) died of multifocal metastases. Tumor recurrence was significantly correlated with histological grade (p=0.041) and lymph node status (p<0.001).
CONCLUSIONS
Although Skp2 expression was statistically insignificant in association with tumor recurrence, it might be useful as a biologic predictor in breast cancer. The simple and reliable immunohistochemical assay presented in this study can be a routine part of breast cancer evaluation and may influence patient management.

 E-submission
E-submission
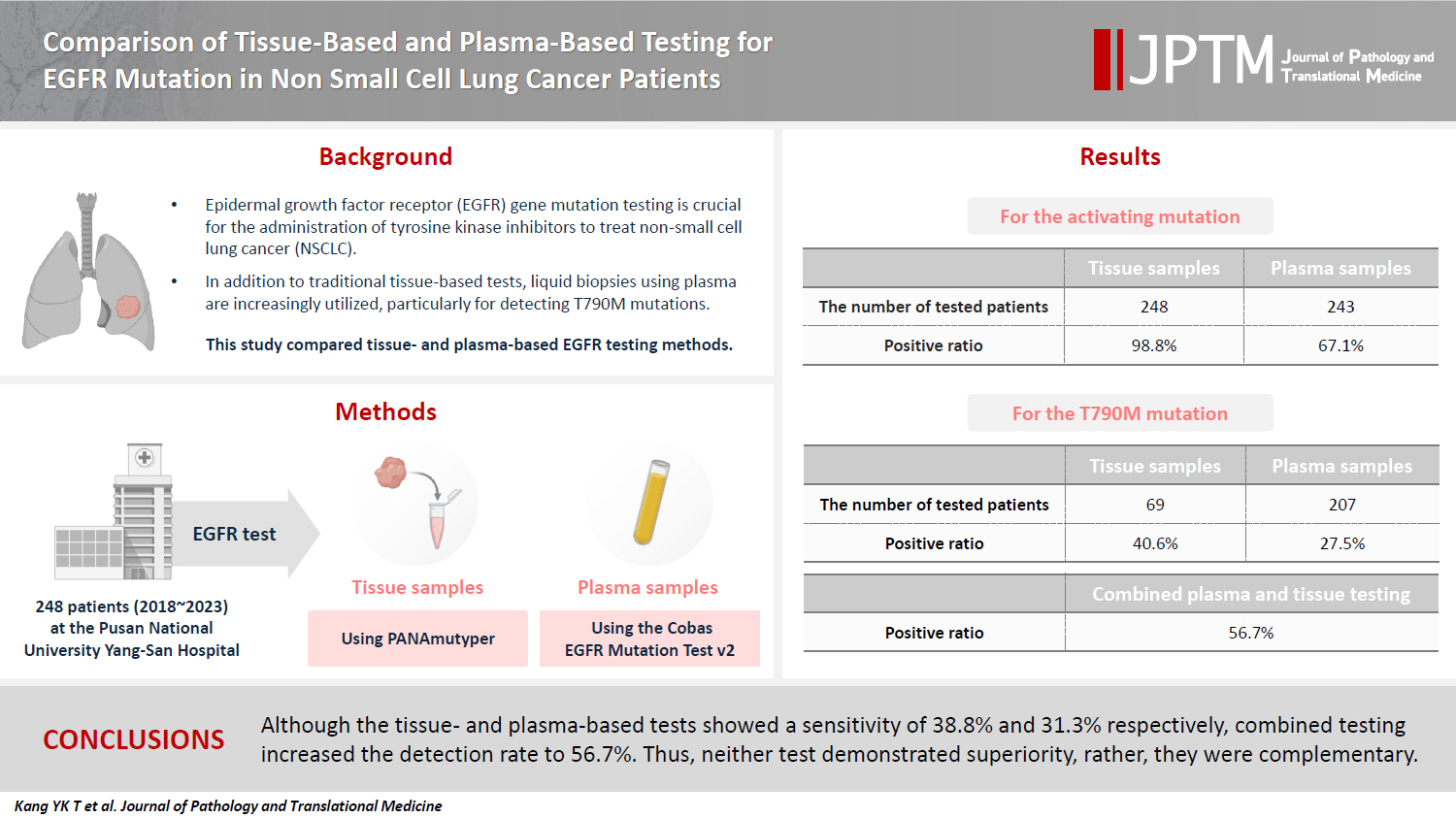
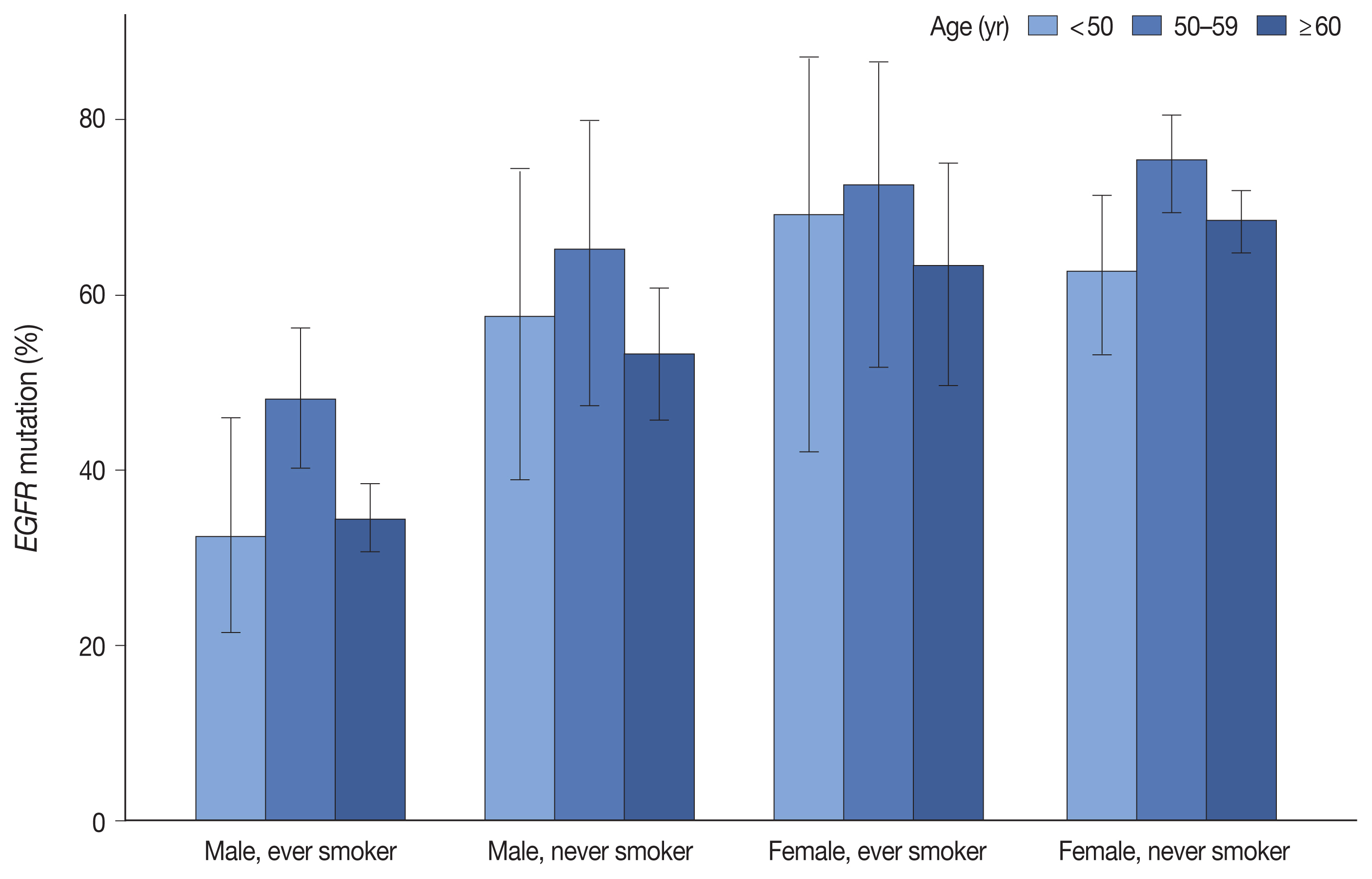

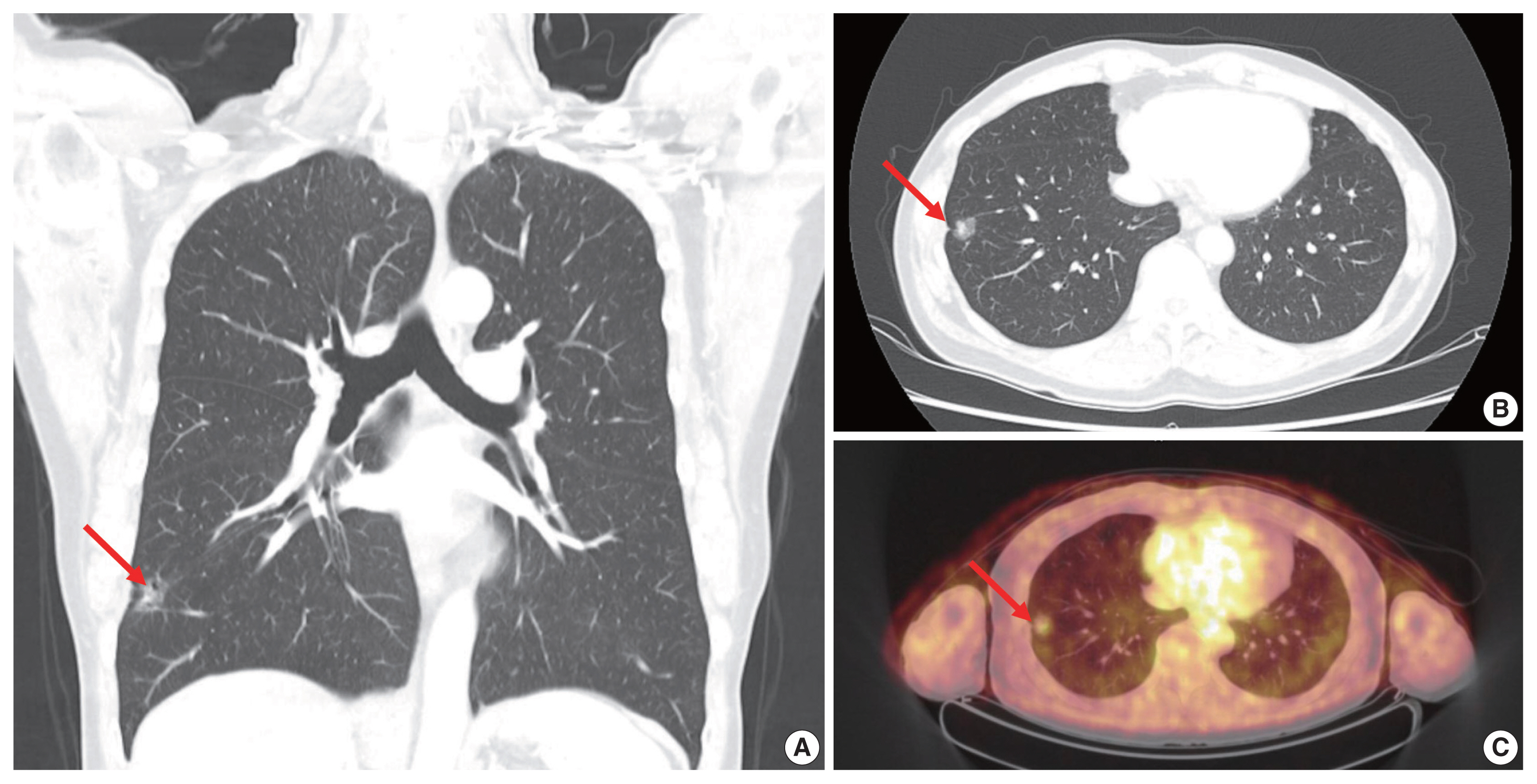
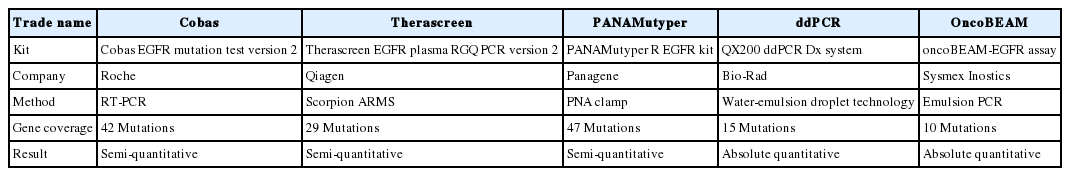
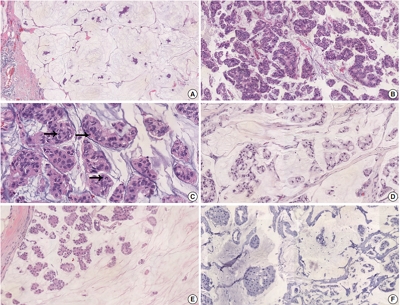
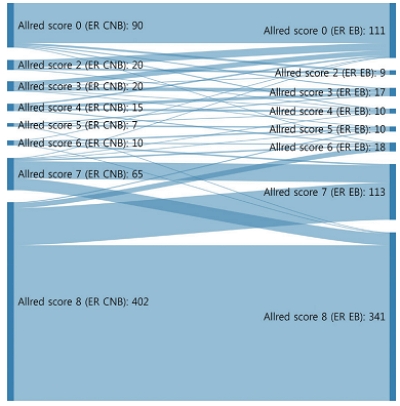
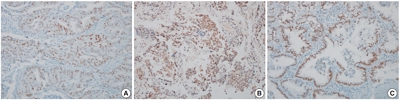
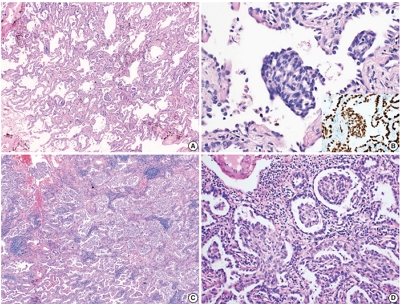
 First
First Prev
Prev



