Search
- Page Path
- HOME > Search
Review Article
- Recent topics on thyroid cytopathology: reporting systems and ancillary studies
- Mitsuyoshi Hirokawa, Ayana Suzuki
- J Pathol Transl Med. 2025;59(4):214-224. Published online June 30, 2025
- DOI: https://doi.org/10.4132/jptm.2025.04.18
- 359 View
- 34 Download
-
 Abstract
Abstract
 PDF
PDF - As fine-needle aspiration techniques and diagnostic methodologies for thyroid nodules have continued to evolve and reporting systems have been updated accordingly, we need to be up to date with the latest information to achieve accurate diagnoses. However, the diagnostic approaches and therapeutic strategies for thyroid nodules vary across laboratories and institutions. Several differences exist between Western and Eastern practices regarding thyroid fine-needle aspiration. This review describes the reporting systems for thyroid cytopathology and ancillary studies. Updated reporting systems enhance the accuracy, consistency, and clarity of cytology reporting, leading to improved patient outcomes and management strategies. Although a single global reporting system is optimal, reporting systems tailored to each country is acceptable. In such cases, compatibility must be ensured to facilitate data sharing. Ancillary methods include liquid-based cytology, immunocytochemistry, biochemical measurements, flow cytometry, molecular testing, and artificial intelligence, all of which improve diagnostic accuracy. These methods continue to evolve, and cytopathologists should actively adopt the latest methods and information to achieve more accurate diagnoses. We believe this review will be useful to practitioners of routine thyroid cytology.
Case Study
- Cytological features of atypical adenomatous hyperplasia and adenocarcinoma in situ of the lung: a case report
- Misa Takahashi, Seiya Homma, Chisato Setoguchi, Yoko Umezawa, Atsuhiko Sakamoto
- J Pathol Transl Med. 2025;59(3):195-200. Published online May 9, 2025
- DOI: https://doi.org/10.4132/jptm.2025.04.09
- 944 View
- 103 Download
-
 Abstract
Abstract
 PDF
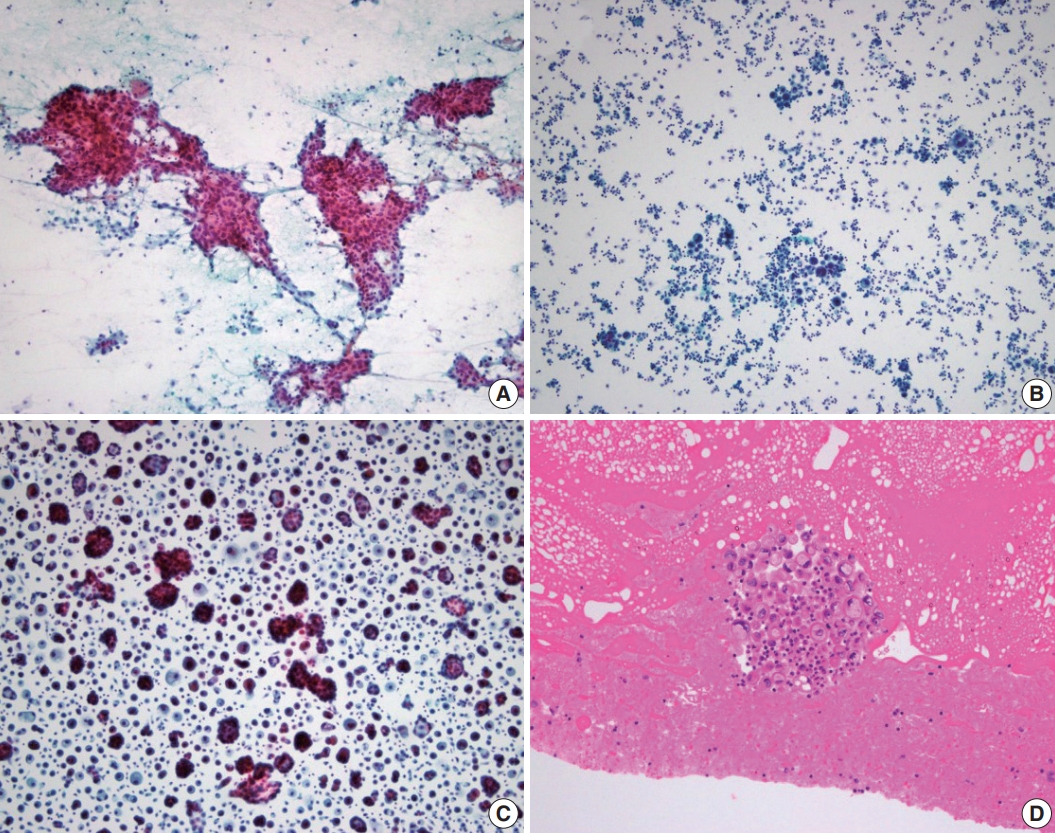
PDF - Atypical adenomatous hyperplasia (AAH) and adenocarcinoma in situ (AIS) are generally treated as different lesions, depending on the differences in lesion size and histological findings. However, these differences are not absolute; thus, AAH and AIS are often difficult to distinguish. Moreover, whether AAH and AIS can be regarded as different lesions remains unknown because cytological specimens, especially those of AAH, are rare. In this study, we examined these uncommon cytological specimens and compared the cytological findings between AAH and AIS. We observed many common cytological features with no obvious differences between AAH and AIS. These findings suggest that these two distinct lesions can be grouped into a single category. Therefore, we propose creating a new cytological category.
Reviews
- Breast fine-needle aspiration cytology in the era of core-needle biopsy: what is its role?
- Ahrong Kim, Hyun Jung Lee, Jee Yeon Kim
- J Pathol Transl Med. 2025;59(1):26-38. Published online January 15, 2025
- DOI: https://doi.org/10.4132/jptm.2024.11.01
- Correction in: J Pathol Transl Med 2025;59(2):147
- 3,437 View
- 265 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Fine-needle aspiration cytology (FNAC) has long been recognized as a minimally invasive, cost-effective, and reliable diagnostic tool for breast lesions. However, with the advent of core-needle biopsy (CNB), the role of FNAC has diminished in some clinical settings. This review aims to re-evaluate the diagnostic value of FNAC in the current era, focusing on its complementary use alongside CNB, the adoption of new approaches such as the International Academy of Cytology Yokohama System, and the implementation of rapid on-site evaluation to reduce inadequate sample rates. Advances in liquid-based cytology, receptor expression testing, molecular diagnostics, and artificial intelligence are discussed, highlighting their potential to enhance the diagnostic accuracy of FNAC. Despite challenges, FNAC remains a valuable diagnostic method, particularly in low-resource settings and specific clinical scenarios, and its role continues to evolve with technology.
-
Citations
Citations to this article as recorded by- Bulk-lysis protocols as a sensitive method for investigation of circulating CK19 cells in the peripheral blood of patients with breast cancer by flow cytometry
Daniella Serafin Couto Vieira, Laura Otto Walter, Maria Eduarda Cunha da Silva, Lisandra de Oliveira Silva, Heloísa Zorzi Costa, Chandra Chiappin Cardoso, Fernando Carlos de Lander Schmitt, Maria Cláudia Santos-Silva
Analytical Methods.2025; 17(23): 4771. CrossRef
- Bulk-lysis protocols as a sensitive method for investigation of circulating CK19 cells in the peripheral blood of patients with breast cancer by flow cytometry
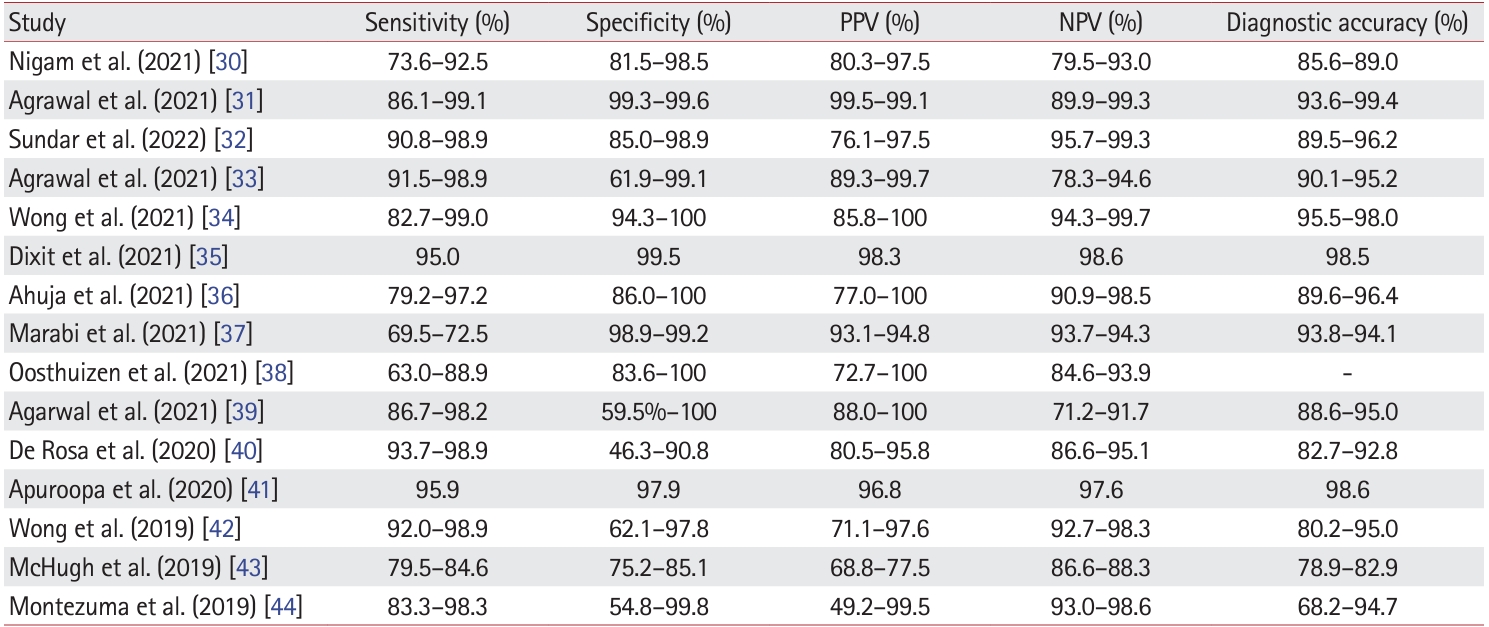
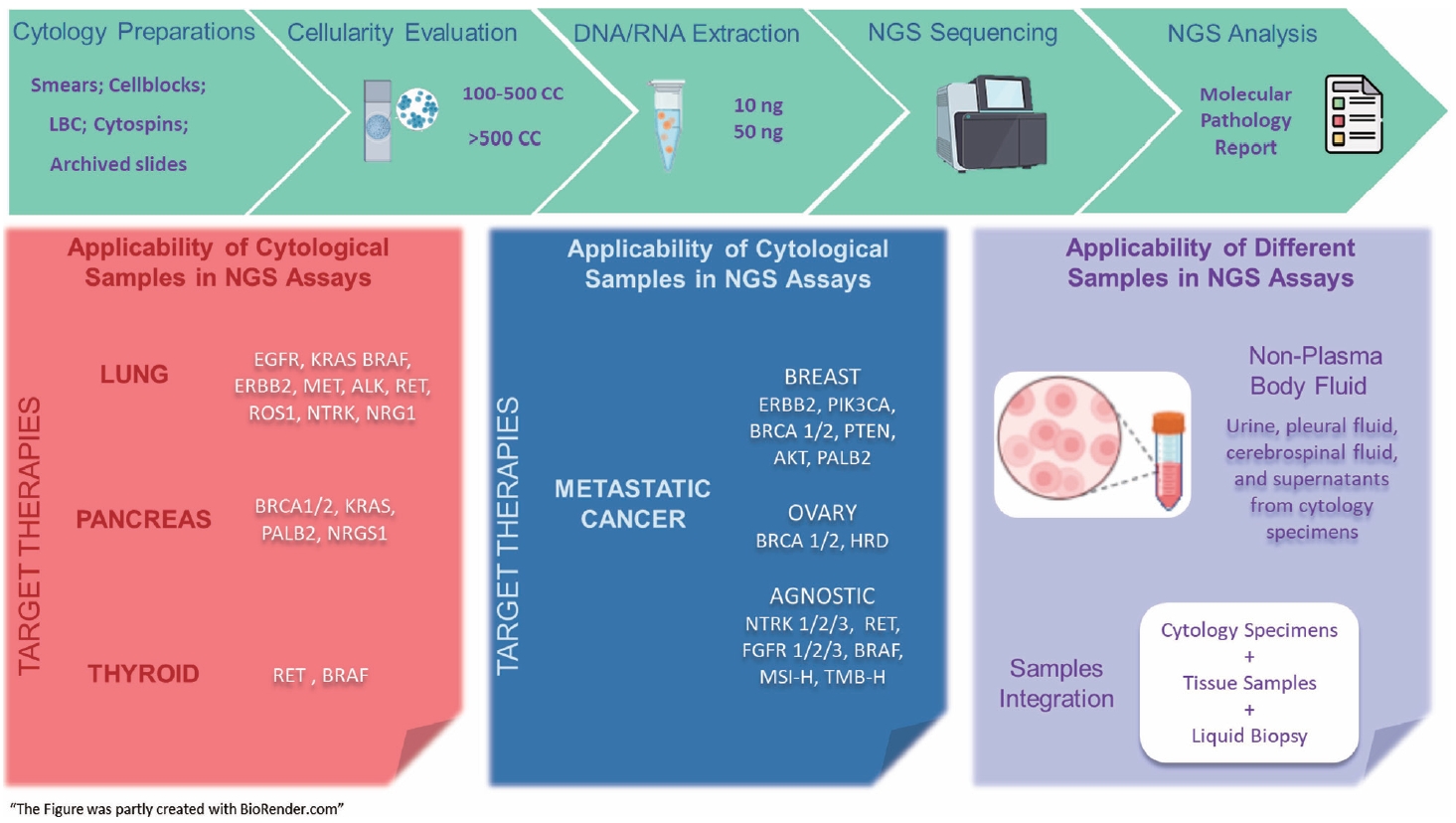
- Next step of molecular pathology: next-generation sequencing in cytology
- Ricella Souza da Silva, Fernando Schmitt
- J Pathol Transl Med. 2024;58(6):291-298. Published online November 7, 2024
- DOI: https://doi.org/10.4132/jptm.2024.10.22
- 2,100 View
- 290 Download
-
 Abstract
Abstract
 PDF
PDF - The evolving landscape of precision oncology underscores the pivotal shift from morphological diagnosis to treatment decisions driven by molecular profiling. Recent guidelines from the European Society for Medical Oncology recomend the use of next-generation sequencing (NGS) across a broader range of cancers, reflecting its superior efficiency and clinical value. NGS not only updates oncology testing by offering quicker, sample-friendly, and sensitive analysis but also reduces the need for multiple individual tests. Cytology samples, often obtained through less invasive methods, can yield high-quality genetic material suitable for molecular analysis. This article focuses on optimizing the use of cytology samples in NGS, and outlines their potential benefits in identifying actionable molecular alterations for targeted therapies across various solid tumors. It also addresses the need for validation studies and the strategies to incorporate or combine different types of samples into routine clinical practice. Integrating cytological and liquid biopsies into routine clinical practice, alongside conventional tissue biopsies, offers a comprehensive approach to tumor genotyping, early disease detection, and monitoring of therapeutic responses across various solid tumor types. For comprehensive biomarker characterization, all patient specimens, although limited, is always valuable.
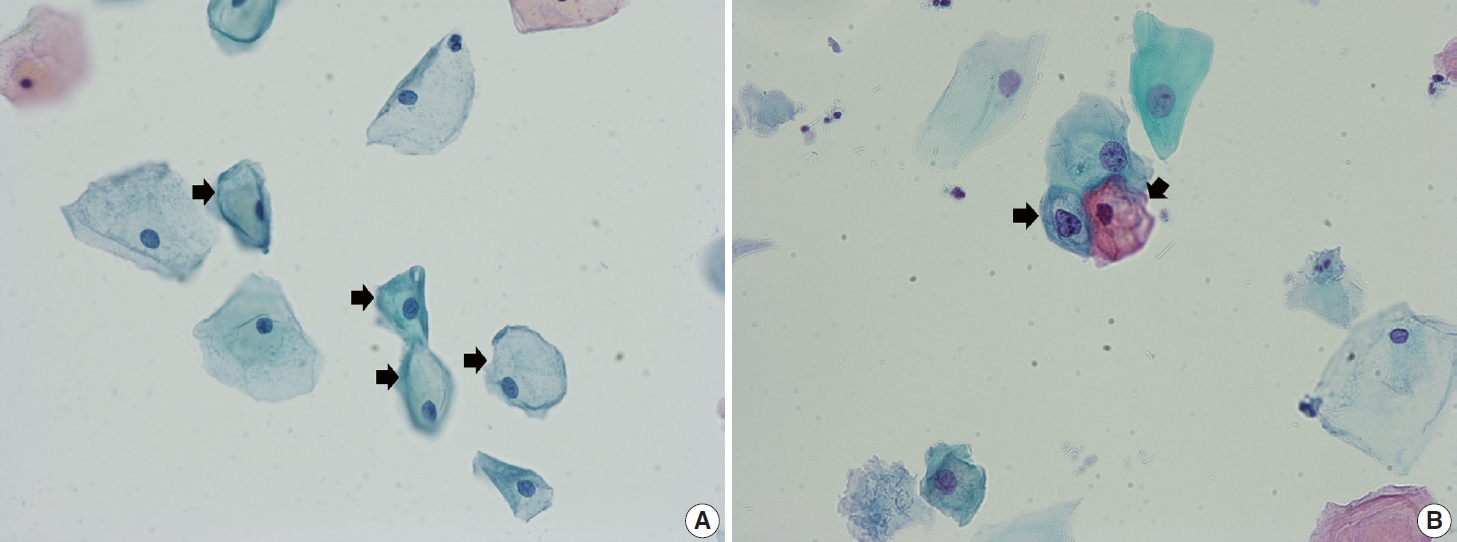
- Cervical intraepithelial neoplasia and cervical cytology in pregnancy
- Ji-Young Kim, Jeong Yun Shim
- J Pathol Transl Med. 2024;58(6):283-290. Published online November 7, 2024
- DOI: https://doi.org/10.4132/jptm.2024.10.17
- 3,695 View
- 312 Download
-
 Abstract
Abstract
 PDF
PDF - Cervical cancer screening during pregnancy presents unique challenges for cytologic interpretation. This review focuses on pregnancy-associated cytomorphological changes and their impact on diagnosis of cervical intraepithelial neoplasia (CIN) and cervical cancer. Pregnancy-induced alterations include navicular cells, hyperplastic endocervical cells, immature metaplastic cells, and occasional decidual cells or trophoblasts. These changes can mimic abnormalities such as koilocytosis, adenocarcinoma in situ, and high-grade squamous intraepithelial lesions, potentially leading to misdiagnosis. Careful attention to nuclear features and awareness of pregnancy-related changes are crucial for correct interpretation. The natural history of CIN during pregnancy shows higher regression rates, particularly for CIN 2, with minimal risk of progression. Management of abnormal cytology follows modified risk-based guidelines to avoid invasive procedures, with treatment typically deferred until postpartum. The findings reported in this review emphasize the importance of considering pregnancy status in cytological interpretation, highlight potential problems, and provide guidance on differentiating benign pregnancy-related changes from true abnormalities. Understanding these nuances is essential for accurate diagnosis and proper management of cervical abnormalities in pregnant women.
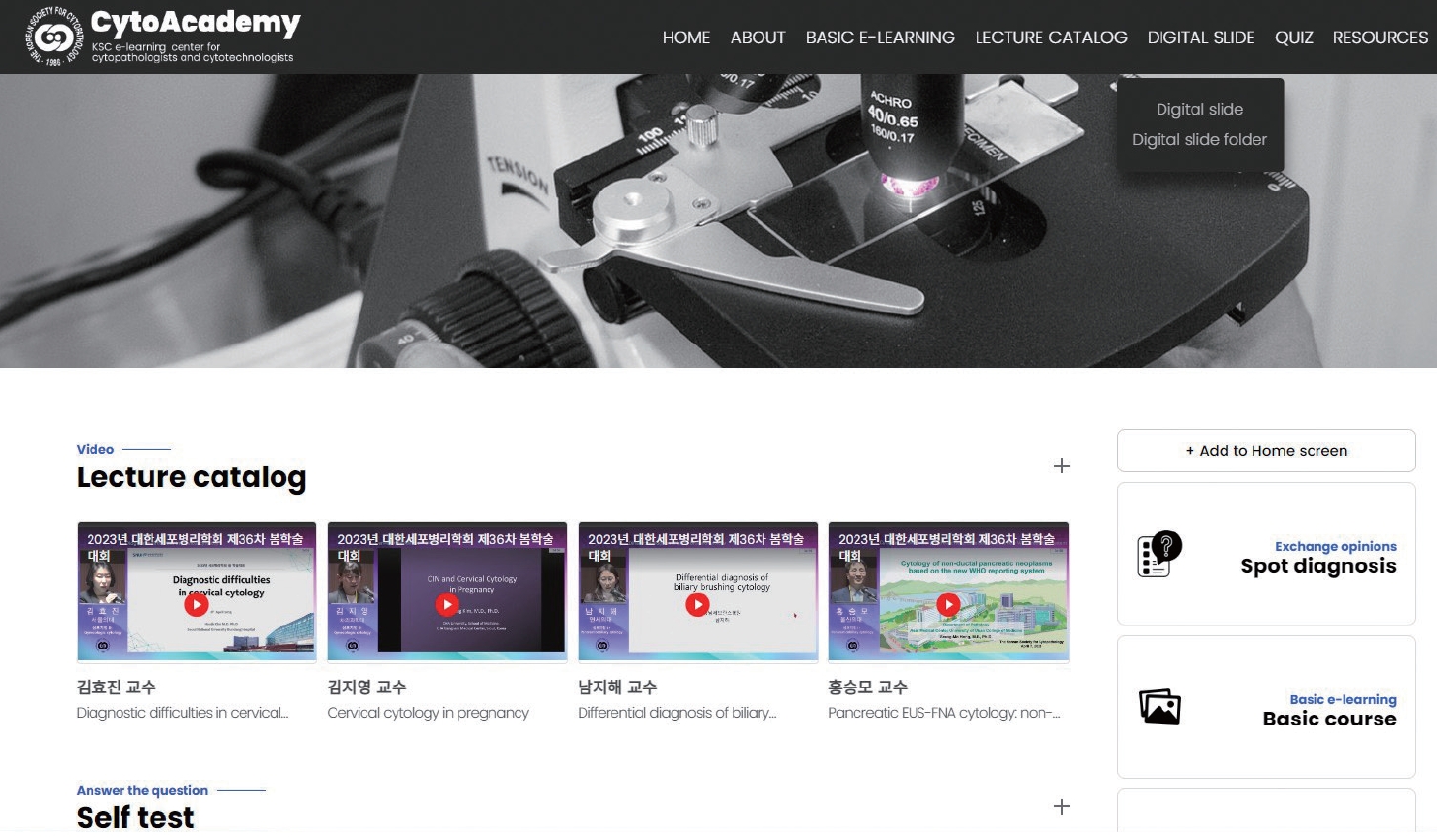
- Development of CytoAcademy: a new web- and mobile-based E-learning platform for cytopathologists and cytotechnologists by the Korean Society for Cytopathology in the post-pandemic era
- Ran Hong, Yosep Chong, Seung Wan Chae, Seung-Sook Lee, Gyungyub Gong
- J Pathol Transl Med. 2024;58(6):261-264. Published online November 7, 2024
- DOI: https://doi.org/10.4132/jptm.2024.10.02
- 3,061 View
- 264 Download
-
 Abstract
Abstract
 PDF
PDF - Since the late 1990s, online e-learning has offered unparalleled convenience and affordability, becoming increasingly popular among pathologists. Traditional learning theories have been successfully applied to web/mobile-based learning systems, with mobile technologies even enhancing conventional offline education. In cytopathology, hands-on microscope training has traditionally been paramount, complemented by real-case presentations and lectures. However, the coronavirus disease 2019 (COVID-19) pandemic disrupted regular academic activities, making online e-learning platforms essential. We designed a web/mobile-based learning platform to enhance continued medical education in cytopathology at various levels, particularly during the era of COVID-19 and beyond. Since 2021, we have integrated curriculum materials, virtual education files, and whole-slide images (WSIs) of cytopathology, submitted from over 200 institutions across Korea, with the support of numerous instructors. We develop a new e-learning platform named “CytoAcademy” composed of a basic session for each organ and level across the range of morphologic findings; on-demand lectures to enhance cytopathologic knowledge; WSI archives that allow users to explore various histologically confirmed cases; and a self-assessment test to help organize diagnostic knowledge acquired through the web/mobile-friendly learning system. The platform provides not just an opportunity to achieve a correct diagnosis, but also a learning experience based on problem-solving point. Members interact, identify their deficiencies, and focus on specific educational materials. In this manner, all participants can actively engage in creating and maintaining knowledge and foster a proactive approach to learning.
Original Article
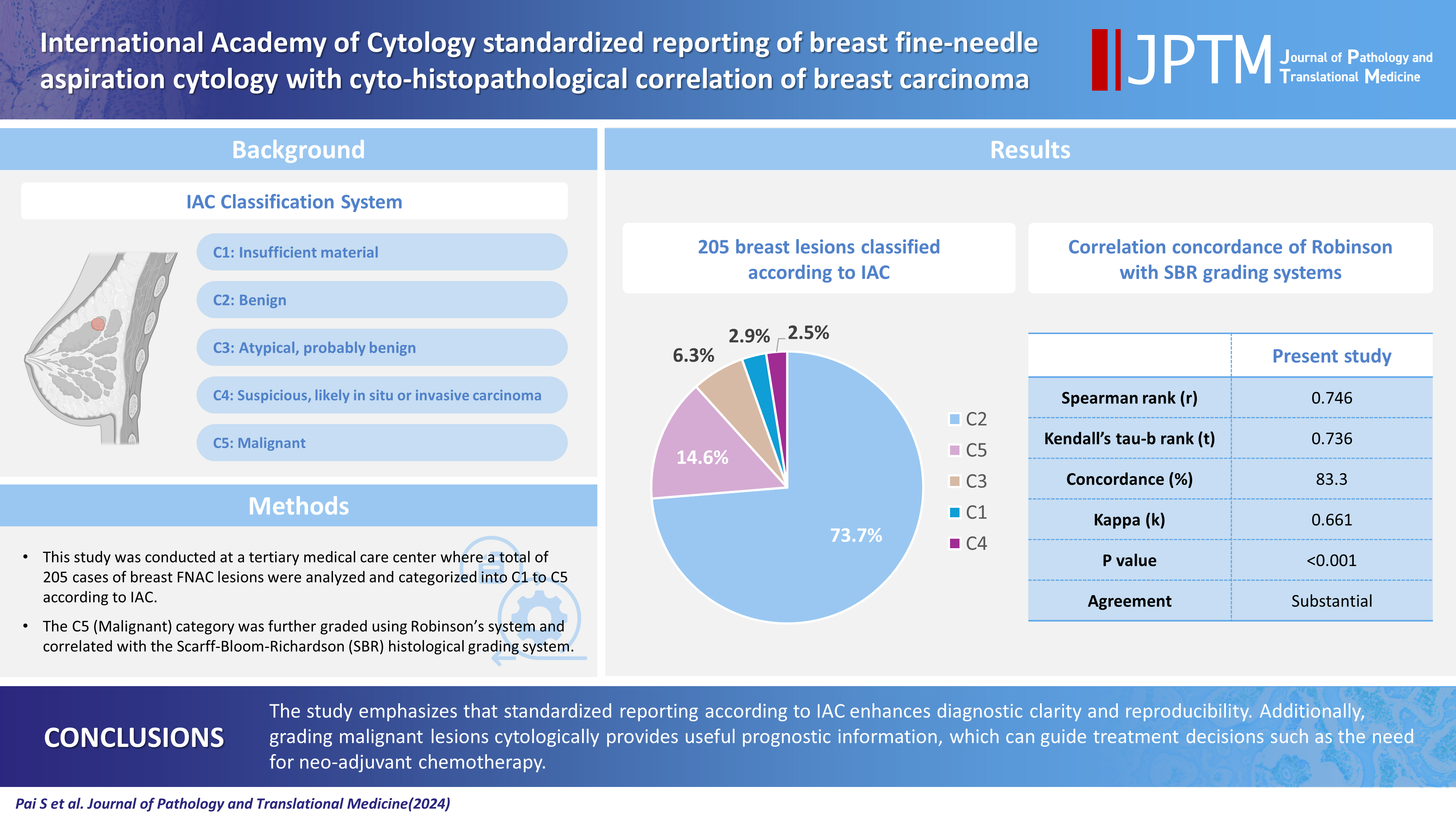
- International Academy of Cytology standardized reporting of breast fine-needle aspiration cytology with cyto-histopathological correlation of breast carcinoma
- Shweta Pai
- J Pathol Transl Med. 2024;58(5):241-248. Published online September 13, 2024
- DOI: https://doi.org/10.4132/jptm.2024.07.14
- 2,235 View
- 251 Download
-
 Abstract
Abstract
 PDF
PDF - Background
The International Academy of Cytology (IAC) has developed a standardized approach for reporting the findings of breast fine-needle aspiration cytology (FNAC). Accordingly, there are five chief categories of breast lesions, C1 (insufficient material), C2 (benign), C3 (atypical), C4 (suspicious), and C5 (malignant). The prognostication and management of breast carcinoma can be performed readily on the basis of this classification system. The aim of this study was to classify various breast lesions into one of the above-named categories and to further grade the C5 lesions specifically using the Robinson system. The latter grades were then correlated with modified Scarff-Bloom-Richardson (SBR) grades.
Methods
This retrospective study was undertaken in the pathology department of a hospital located in the urban part of the city of Bangalore. All FNAC procedures performed on breast lumps spanning the year 2020 were included in the study.
Results
A total of 205 breast lesions was classified according to the IAC guidelines into C1 (6 cases, 2.9%), C2 (151 cases, 73.7%), C3 (13 cases, 6.3%), C4 (5 cases, 2.5%), and C5 (30 cases, 14.6%) groups. The C5 cases were further graded using Robinson’s system. The latter showed a significant correlation with the SBR system (concordance=83.3%, Spearman correlation=0.746, Kendall’s tau-b=0.736, kappa=0.661, standard error=0.095, p≤.001).
Conclusions
A standardized approach for FNAC reporting of breast lesions, as advocated for by the IAC, improves the quality and clarity of the reports and assures diagnostic reproducibility on a global scale. Further, the cytological grading of C5 lesions provides reliable cyto-prognostic scores that can help assess a tumor’s aggressiveness and predict its histological grade.
Case Study
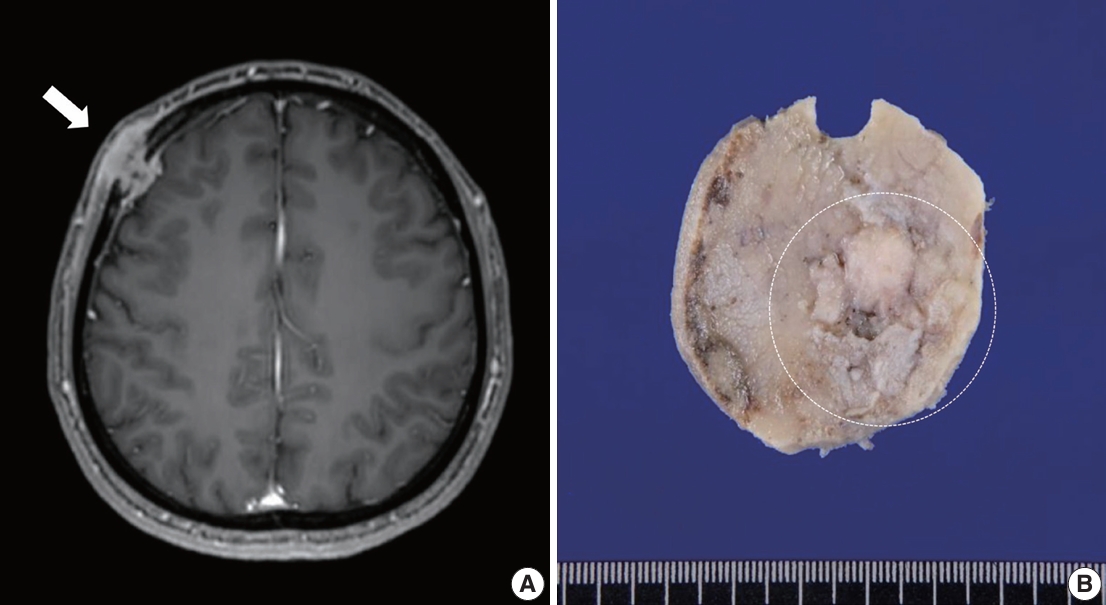
- Rhabdomyosarcoma of the skull with EWSR1 fusion and ALK and cytokeratin expression: a case report
- Hyeong Rok An, Kyung-Ja Cho, Sang Woo Song, Ji Eun Park, Joon Seon Song
- J Pathol Transl Med. 2024;58(5):255-260. Published online September 5, 2024
- DOI: https://doi.org/10.4132/jptm.2024.08.15
- 1,842 View
- 201 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Rhabdomyosarcoma (RMS) comprises of heterogeneous group of neoplasms that occasionally express epithelial markers on immunohistochemistry (IHC). We herein report the case of a patient who developed RMS of the skull with EWSR1 fusion and anaplastic lymphoma kinase (ALK) and cytokeratin expression as cytomorphologic features. A 40-year-old man presented with a mass in his forehead. Surgical resection was performed, during which intraoperative frozen specimens were obtained. Squash cytology showed scattered or clustered spindle and epithelioid cells. IHC revealed that the resected tumor cells were positive for desmin, MyoD1, cytokeratin AE1/ AE3, and ALK. Although EWSR1 rearrangement was identified on fluorescence in situ hybridization, ALK, and TFCP2 rearrangement were not noted. Despite providing adjuvant chemoradiation therapy, the patient died of tumor progression 10 months after diagnosis. We emphasize that a subset of RMS can express cytokeratin and show characteristic histomorphology, implying the need for specific molecular examination.
-
Citations
Citations to this article as recorded by
Review
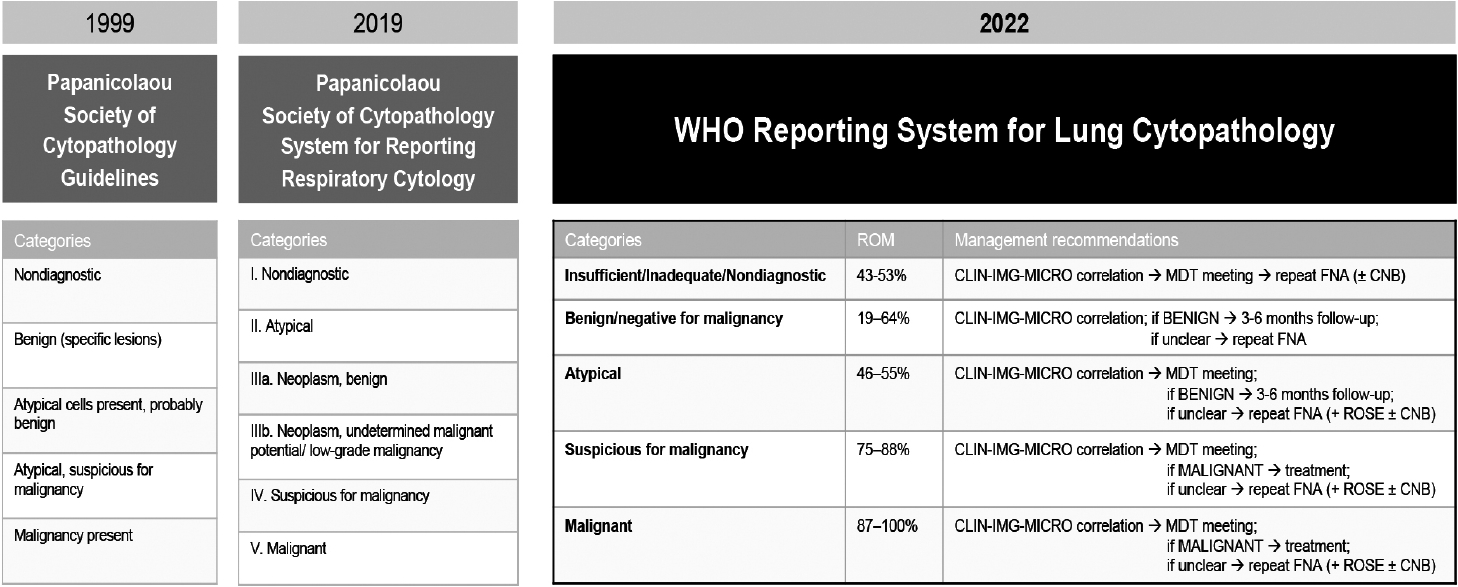
- Welcoming the new, revisiting the old: a brief glance at cytopathology reporting systems for lung, pancreas, and thyroid
- Rita Luis, Balamurugan Thirunavukkarasu, Deepali Jain, Sule Canberk
- J Pathol Transl Med. 2024;58(4):165-173. Published online July 15, 2024
- DOI: https://doi.org/10.4132/jptm.2024.06.11
- 1,934 View
- 249 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - This review addresses new reporting systems for lung and pancreatobiliary cytopathology as well as the most recent edition of The Bethesda Reporting System for Thyroid Cytopathology. The review spans past, present, and future aspects within the context of the intricate interplay between traditional morphological assessments and cutting-edge molecular diagnostics. For lung and pancreas, the authors discuss the evolution of reporting systems, emphasizing the bridge between past directives and more recent collaborative efforts of the International Academy of Cytology and the World Health Organization in shaping universal reporting systems. The review offers a brief overview of the structure of these novel systems, highlighting their strengths and pinpointing areas that require further refinement. For thyroid, the authors primarily focus on the third edition of The Bethesda System for Reporting Thyroid Cytopathology, also considering the two preceding editions. This review serves as an invaluable resource for cytopathologists, offering a panoramic view of the evolving landscape of cytopathology reporting and pointing out the integrative role of the cytopathologist in an era of rapid diagnostic and therapeutic advancements.
-
Citations
Citations to this article as recorded by- WHO Reporting System for Lung Cytopathology: Insights Into the Insufficient/Inadequate/Non‐Diagnostic, Atypical and Suspicious for Malignancy Categories and How to Use Them
Zahra Maleki, Sule Canberk, Andrew Field
Cytopathology.2025;[Epub] CrossRef - Reproducibility of the Bethesda system for reporting thyroid cytopathology (TBSRTC): An observational study of 100 patients
Kishori Moni Panda, Reena Naik, Mohd Ghouse Mohiddin
Indian Journal of Pathology and Oncology.2024; 11(4): 385. CrossRef
- WHO Reporting System for Lung Cytopathology: Insights Into the Insufficient/Inadequate/Non‐Diagnostic, Atypical and Suspicious for Malignancy Categories and How to Use Them
Original Articles
- Liquid-based cytology features of pancreatic acinar cell carcinoma: comparison with other non-ductal neoplasms of the pancreas
- Minji Kwon, Seung-Mo Hong, Kyoungbun Lee, Haeryoung Kim
- J Pathol Transl Med. 2024;58(4):182-190. Published online July 9, 2024
- DOI: https://doi.org/10.4132/jptm.2024.06.25
- 1,669 View
- 230 Download
-
 Abstract
Abstract
 PDF
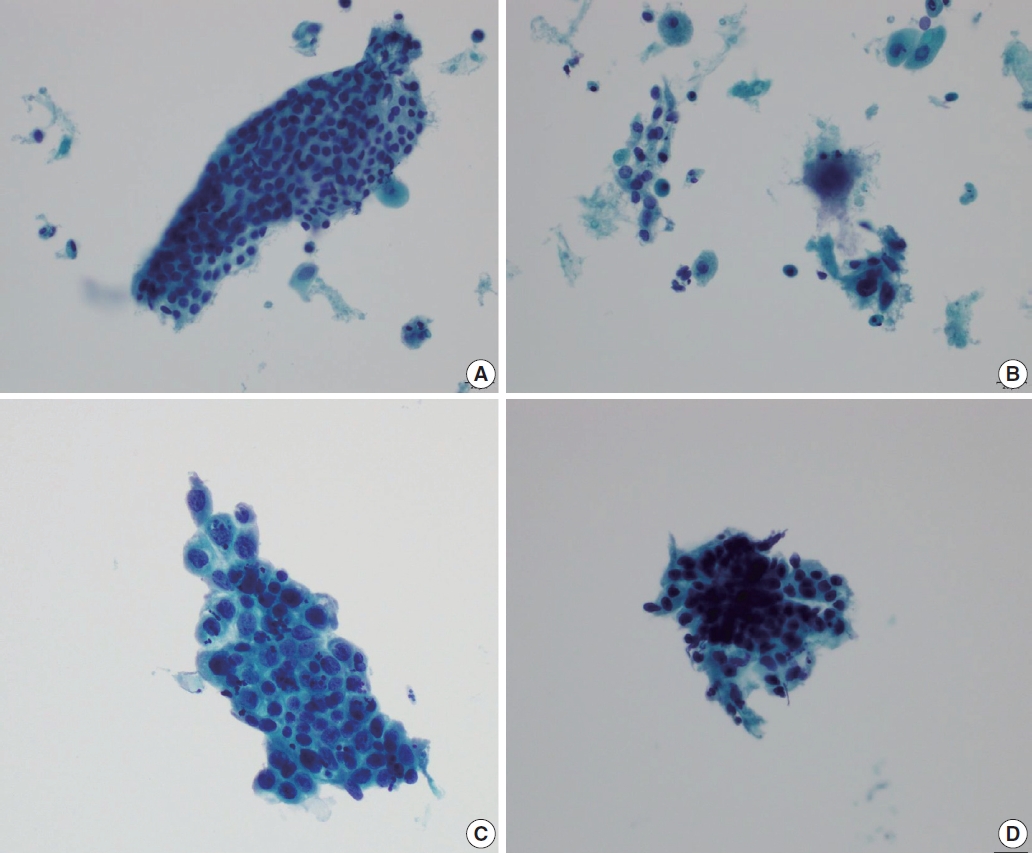
PDF - Background
Acinar cell carcinoma (ACC) is a rare malignant epithelial neoplasm, which shares many cytomorphological features with other non-ductal pancreatic neoplasms such as pancreatic neuroendocrine neoplasm (PanNEN) and solid-pseudopapillary neoplasm (SPN). Due to the relative rarity of these tumors, pathologists are less familiar with the cytological features, especially on liquid-based cytology (LBC) which has been relatively recently introduced for endoscopic ultrasound-guided fine needle aspiration specimens.
Methods
We evaluated the detailed cytological features of 15 histologically confirmed ACC (7 conventional smears [CS], 8 LBC), and compared them with the LBC features of SPN (n = 9) and PanNEN (n = 9).
Results
Compared with CS, LBCs of ACC demonstrated significantly less bloody background. All ACCs demonstrated prominent nucleoli and macronucleoli on LBC. On comparison with the LBC features of SPN and PanNEN, most ACCs demonstrated a necrotic background with apoptotic debris while PanNEN and SPN did not show these features. Acinar structures were predominantly observed in ACC, while frequent pseudopapillary structures were seen only in SPN. Prominent nucleoli and macronucleoli were only seen in ACC.
Conclusions
ACC had characteristic cytological features that could be observed on LBC preparations, such as high cellularity, necrotic/apoptotic background, nuclear tangles, acinar arrangement of cells, and macronucleoli. These findings also help distinguish ACC from PanNEN and SPN on LBC. It is important to be familiar with these features, as an accurate diagnosis on endoscopic ultrasound–guided fine needle aspiration cytology would have impact on the management of the patient.
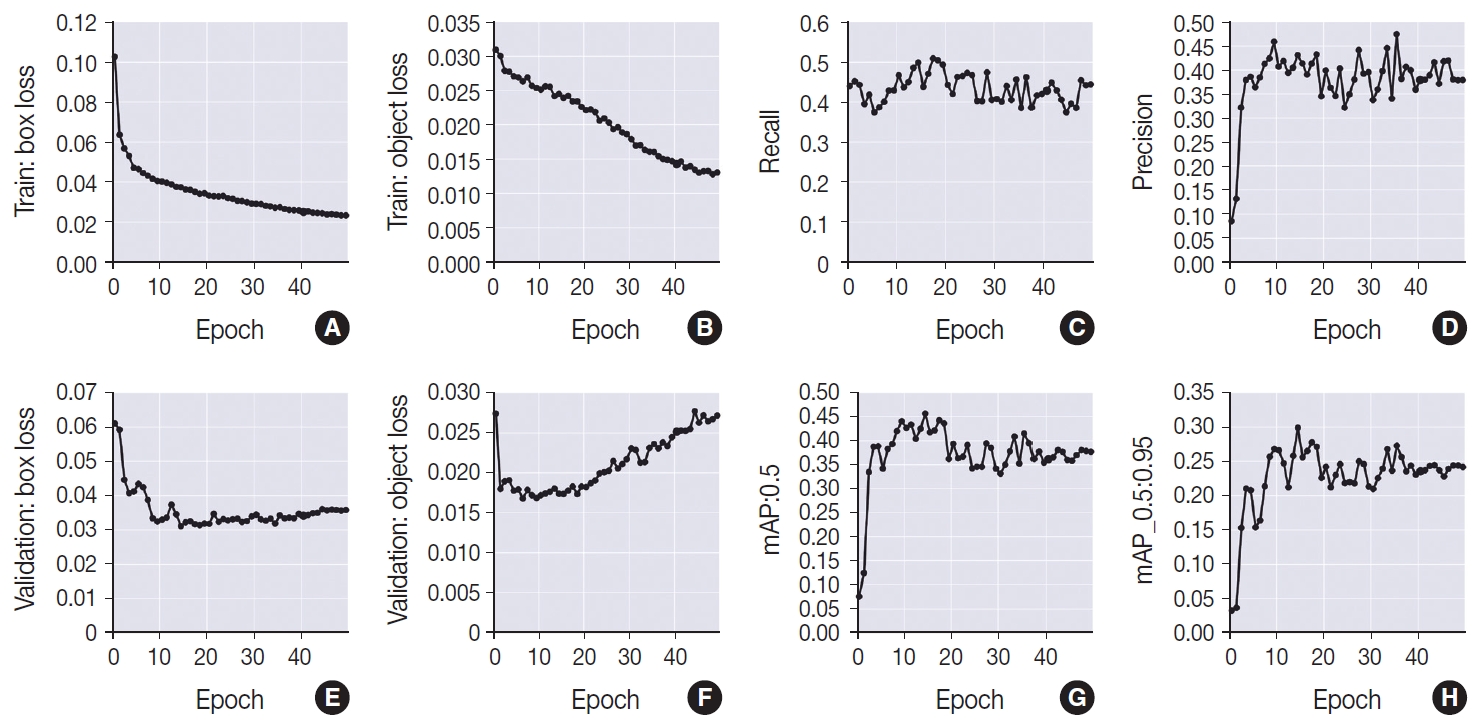
- Revisiting the utility of identifying nuclear grooves as unique nuclear changes by an object detector model
- Pedro R. F. Rende, Joel Machado Pires, Kátia Sakimi Nakadaira, Sara Lopes, João Vale, Fabio Hecht, Fabyan E. L. Beltrão, Gabriel J. R. Machado, Edna T. Kimura, Catarina Eloy, Helton E. Ramos
- J Pathol Transl Med. 2024;58(3):117-126. Published online April 30, 2024
- DOI: https://doi.org/10.4132/jptm.2024.03.07
- 2,751 View
- 262 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Among other structures, nuclear grooves are vastly found in papillary thyroid carcinoma (PTC). Considering that the application of artificial intelligence in thyroid cytology has potential for diagnostic routine, our goal was to develop a new supervised convolutional neural network capable of identifying nuclear grooves in Diff-Quik stained whole-slide images (WSI) obtained from thyroid fineneedle aspiration.
Methods
We selected 22 Diff-Quik stained cytological slides with cytological diagnosis of PTC and concordant histological diagnosis. Each of the slides was scanned, forming a WSI. Images that contained the region of interest were obtained, followed by pre-formatting, annotation of the nuclear grooves and data augmentation techniques. The final dataset was divided into training and validation groups in a 7:3 ratio.
Results
This is the first artificial intelligence model based on object detection applied to nuclear structures in thyroid cytopathology. A total of 7,255 images were obtained from 22 WSI, totaling 7,242 annotated nuclear grooves. The best model was obtained after it was submitted 15 times with the train dataset (14th epoch), with 67% true positives, 49.8% for sensitivity and 43.1% for predictive positive value.
Conclusions
The model was able to develop a structure predictor rule, indicating that the application of an artificial intelligence model based on object detection in the identification of nuclear grooves is feasible. Associated with a reduction in interobserver variability and in time per slide, this demonstrates that nuclear evaluation constitutes one of the possibilities for refining the diagnosis through computational models.
- Diagnostic proficiency test using digital cytopathology and comparative assessment of whole slide images of cytologic samples for quality assurance program in Korea
- Yosep Chong, Soon Auck Hong, Hoon Kyu Oh, Soo Jin Jung, Bo-Sung Kim, Ji Yun Jeong, Ho-Chang Lee, Gyungyub Gong
- J Pathol Transl Med. 2023;57(5):251-264. Published online August 24, 2023
- DOI: https://doi.org/10.4132/jptm.2023.07.17
- 4,857 View
- 320 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
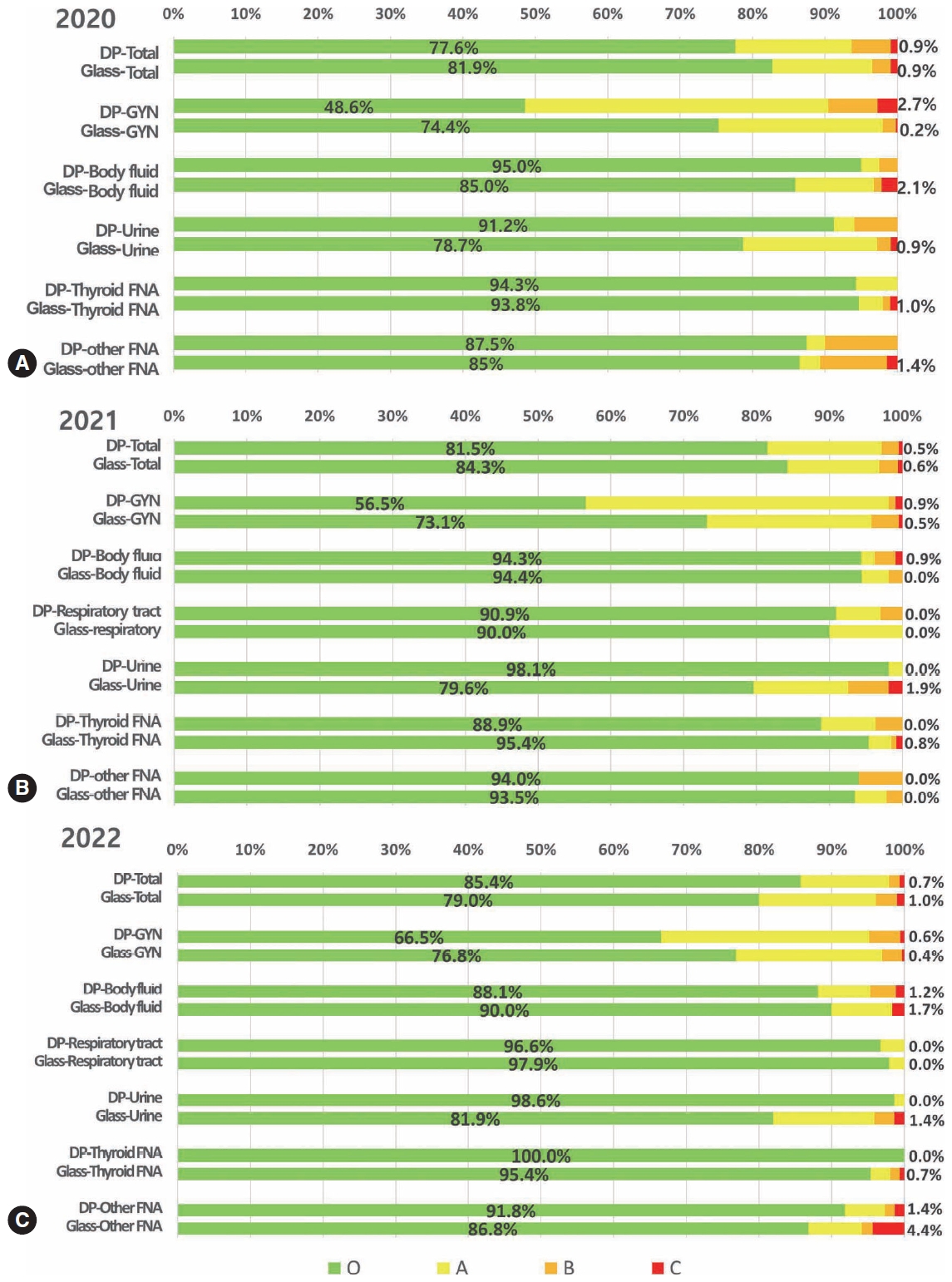
Supplementary Material - Background
The Korean Society for Cytopathology introduced a digital proficiency test (PT) in 2021. However, many doubtful opinions remain on whether digitally scanned images can satisfactorily present subtle differences in the nuclear features and chromatin patterns of cytological samples.
Methods
We prepared 30 whole-slide images (WSIs) from the conventional PT archive by a selection process for digital PT. Digital and conventional PT were performed in parallel for volunteer institutes, and the results were compared using feedback. To assess the quality of cytological assessment WSIs, 12 slides were collected and scanned using five different scanners, with four cytopathologists evaluating image quality through a questionnaire.
Results
Among the 215 institutes, 108 and 107 participated in glass and digital PT, respectively. No significant difference was noted in category C (major discordance), although the number of discordant cases was slightly higher in the digital PT group. Leica, 3DHistech Pannoramic 250 Flash, and Hamamatsu NanoZoomer 360 systems showed comparable results in terms of image quality, feature presentation, and error rates for most cytological samples. Overall satisfaction was observed with the general convenience and image quality of digital PT.
Conclusions
As three-dimensional clusters are common and nuclear/chromatin features are critical for cytological interpretation, careful selection of scanners and optimal conditions are mandatory for the successful establishment of digital quality assurance programs in cytology. -
Citations
Citations to this article as recorded by- Sensitivity, Specificity, and Cost–Benefit Effect Between Primary Human Papillomavirus Testing, Primary Liquid‐Based Cytology, and Co‐Testing Algorithms for Cervical Lesions
Chang Gok Woo, Seung‐Myoung Son, Hye‐Kyung Hwang, Jung‐Sil Bae, Ok‐Jun Lee, Ho‐Chang Lee
Diagnostic Cytopathology.2025; 53(1): 35. CrossRef - Integration of AI‐Assisted in Digital Cervical Cytology Training: A Comparative Study
Yihui Yang, Dongyi Xian, Lihua Yu, Yanqing Kong, Huaisheng Lv, Liujing Huang, Kai Liu, Hao Zhang, Weiwei Wei, Hongping Tang
Cytopathology.2025; 36(2): 156. CrossRef - Validation of digital image slides for diagnosis in cervico-vaginal cytology
Francisco Tresserra, Gemma Fabra, Olga Luque, Miriam Castélla, Carla Gómez, Carmen Fernández-Cid, Ignacio Rodríguez
Revista Española de Patología.2024; 57(3): 182. CrossRef - Improved Diagnostic Accuracy of Thyroid Fine-Needle Aspiration Cytology with Artificial Intelligence Technology
Yujin Lee, Mohammad Rizwan Alam, Hongsik Park, Kwangil Yim, Kyung Jin Seo, Gisu Hwang, Dahyeon Kim, Yeonsoo Chung, Gyungyub Gong, Nam Hoon Cho, Chong Woo Yoo, Yosep Chong, Hyun Joo Choi
Thyroid®.2024; 34(6): 723. CrossRef
- Sensitivity, Specificity, and Cost–Benefit Effect Between Primary Human Papillomavirus Testing, Primary Liquid‐Based Cytology, and Co‐Testing Algorithms for Cervical Lesions
Reviews
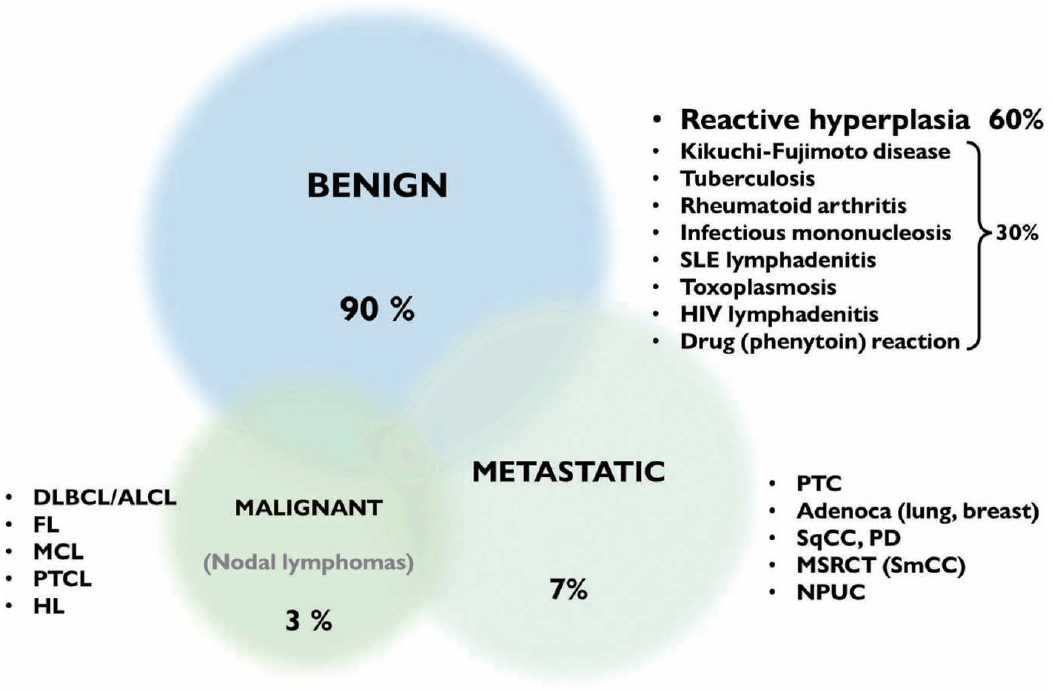
- A stepwise approach to fine needle aspiration cytology of lymph nodes
- Yosep Chong, Gyeongsin Park, Hee Jeong Cha, Hyun-Jung Kim, Chang Suk Kang, Jamshid Abdul-Ghafar, Seung-Sook Lee
- J Pathol Transl Med. 2023;57(4):196-207. Published online July 11, 2023
- DOI: https://doi.org/10.4132/jptm.2023.06.12
- 31,012 View
- 1,879 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - The cytological diagnosis of lymph node lesions is extremely challenging because of the diverse diseases that cause lymph node enlargement, including both benign and malignant or metastatic lymphoid lesions. Furthermore, the cytological findings of different lesions often resemble one another. A stepwise diagnostic approach is essential for a comprehensive diagnosis that combines: clinical findings, including age, sex, site, multiplicity, and ultrasonography findings; low-power reactive, metastatic, and lymphoma patterns; high-power population patterns, including two populations of continuous range, small monotonous pattern and large monotonous pattern; and disease-specific diagnostic clues including granulomas and lymphoglandular granules. It is also important to remember the histological features of each diagnostic category that are common in lymph node cytology and to compare them with cytological findings. It is also essential to identify a few categories of diagnostic pitfalls that often resemble lymphomas and easily lead to misdiagnosis, particularly in malignant small round cell tumors, poorly differentiated squamous cell carcinomas, and nasopharyngeal undifferentiated carcinoma. Herein, we review a stepwise approach for fine needle aspiration cytology of lymphoid diseases and suggest a diagnostic algorithm that uses this approach and the Sydney classification system.
-
Citations
Citations to this article as recorded by- Development and Validation of Explainable Artificial Intelligence System for Automatic Diagnosis of Cervical Lymphadenopathy From Ultrasound Images
Ming Xu, Yubiao Yue, Zhenzhang Li, Yinhong Li, Guoying Li, Haihua Liang, Di Liu, Xiaohong Xu, Mohamadreza (Mohammad) Khosravi
International Journal of Intelligent Systems.2025;[Epub] CrossRef - Immunocytochemical markers, molecular testing and digital cytopathology for aspiration cytology of metastatic breast carcinoma
Joshua J. X. Li, Gary M. Tse
Cytopathology.2024; 35(2): 218. CrossRef - Response to comment on “A stepwise approach to fine needle aspiration cytology of lymph nodes”
Yosep Chong, Gyeongsin Park, Hee Jeong Cha, Hyun-Jung Kim, Chang Suk Kang, Jamshid Abdul-Ghafar, Seung-Sook Lee
Journal of Pathology and Translational Medicine.2024; 58(1): 43. CrossRef - Comment on “A stepwise approach to fine needle aspiration cytology of lymph nodes”
Elisabetta Maffei, Valeria Ciliberti, Pio Zeppa, Alessandro Caputo
Journal of Pathology and Translational Medicine.2024; 58(1): 40. CrossRef - The Incidence of Thyroid Cancer in Bethesda III Thyroid Nodules: A Retrospective Analysis at a Single Endocrine Surgery Center
Iyad Hassan, Lina Hassan, Nahed Balalaa, Mohamad Askar, Hussa Alshehhi, Mohamad Almarzooqi
Diagnostics.2024; 14(10): 1026. CrossRef - Efficiency of Fine-Needle Aspiration (FNA) in Relation to Tru-Cut Biopsy of Lateral Neck Swellings
Mohammed S Al Olaimat, Fahad S Al Qooz, Zaid R Alzoubi, Elham M Alsharaiah, Ali S Al Murdif, Mohammad O Alanazi
Cureus.2024;[Epub] CrossRef - Pitfalls in the Cytological Diagnosis of Nodal Hodgkin Lymphoma
Uma Handa, Rasheeda Mohamedali, Rajpal Singh Punia, Simrandeep Singh, Ranjeev Bhagat, Phiza Aggarwal, Manveen Kaur
Diagnostic Cytopathology.2024; 52(12): 715. CrossRef - Rapid 3D imaging at cellular resolution for digital cytopathology with a multi-camera array scanner (MCAS)
Kanghyun Kim, Amey Chaware, Clare B. Cook, Shiqi Xu, Monica Abdelmalak, Colin Cooke, Kevin C. Zhou, Mark Harfouche, Paul Reamey, Veton Saliu, Jed Doman, Clay Dugo, Gregor Horstmeyer, Richard Davis, Ian Taylor-Cho, Wen-Chi Foo, Lucas Kreiss, Xiaoyin Sara J
npj Imaging.2024;[Epub] CrossRef
- Development and Validation of Explainable Artificial Intelligence System for Automatic Diagnosis of Cervical Lymphadenopathy From Ultrasound Images
- Trouble-makers in cytologic interpretation of the uterine cervix
- Eunah Shin, Jaeeun Yu, Soon Won Hong
- J Pathol Transl Med. 2023;57(3):139-146. Published online May 15, 2023
- DOI: https://doi.org/10.4132/jptm.2023.04.25
- 6,393 View
- 420 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - The development and standardization of cytologic screening of the uterine cervix has dramatically decreased the prevalence of squamous cell carcinoma of the uterine cervix. Advances in the understanding of biology of human papillomavirus have contributed to upgrading the histologic diagnosis of the uterine cervix; however, cytologic screening that should triage those that need further management still poses several difficulties in interpretation. Cytologic features of high grade intraepithelial squamous lesion (HSIL) mimics including atrophy, immature metaplasia, and transitional metaplasia, and glandular lesion masquerades including tubal metaplasia and HSIL with glandular involvement are described with accentuation mainly on the differential points. When the cytologic features lie in a gray zone between the differentials, the most important key to the more accurate interpretation is sticking to the very basics of cytology; screening the background and cellular architecture, and then scrutinizing the nuclear and cytoplasmic details.
-
Citations
Citations to this article as recorded by- Risk of cervical stenosis after cervical excision in postmenopausal patients
Eva Hauge, Line Winther Gustafson, Mette Tranberg, Pinar Bor
European Journal of Obstetrics & Gynecology and Reproductive Biology.2025; 308: 208. CrossRef - Pitfalls in Gynecological Cytology: Review of the Common and Less Frequent Entities in Pap Test
Danijela Vrdoljak-Mozetič, Snježana Štemberger-Papić, Damjana Verša Ostojić, Roberta Rubeša, Marko Klarić, Senija Eminović
Acta Cytologica.2024; 68(3): 281. CrossRef - Cytological features of human papillomavirus‐infected immature squamous metaplastic cells from cervical intraepithelial neoplasia grade 2
Mitsuaki Okodo, Kaori Okayama, Koji Teruya, Ruku Shinohara, Shuichi Mizuno, Rei Settsu, Yasuyoshi Ishii, Masahiko Fujii, Hirokazu Kimura, Mizue Oda
Journal of Medical Virology.2023;[Epub] CrossRef
- Risk of cervical stenosis after cervical excision in postmenopausal patients
- Biomarker testing of cytology specimens in personalized medicine for lung cancer patients
- Hyojin Kim, Jin-Haeng Chung
- J Pathol Transl Med. 2022;56(6):326-333. Published online November 9, 2022
- DOI: https://doi.org/10.4132/jptm.2022.10.17
- 4,136 View
- 159 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - Every patient with advanced non–small cell lung cancer (NSCLC) should be tested for targetable driver mutations and gene arrangements that may open avenues for targeted therapy. As most patients with NSCLC in the advanced stage of the disease are not candidates for surgery, these tests have to be performed on small biopsies or cytology samples. A growing number of other genetic changes with targetable mutations may be treatable in the near future. To identify patients who might benefit from novel targeted therapy, relevant markers should be tested in an appropriate context. In addition, immunotherapy of lung cancer is guided by the status of programmed death-ligand 1 expression in tumor cells. The variety and versatility of cytological specimen preparations offer significant advantages for molecular testing; however, they frequently remain underused. Therefore, evaluating the utility and adequacy of cytologic specimens is important, not only from a lung cancer diagnosis, but also for the large number of ancillary studies that are necessary to provide appropriate clinical management. A large proportion of lung cancers is diagnosed by aspiration or exfoliative cytology specimens; thus, optimizing strategies to triage and best use the tissue for diagnosis and biomarker studies forms a critical component of lung cancer management. In this review, we discuss the opportunities and challenges of using cytologic specimens for biomarker testing of lung cancer and the role of cytopathology in the molecular era.
-
Citations
Citations to this article as recorded by- Proposal of real-world solutions for the implementation of predictive biomarker testing in patients with operable non-small cell lung cancer
Paul Hofman, Petros Christopoulos, Nicky D’Haene, John Gosney, Nicola Normanno, Ed Schuuring, Ming-Sound Tsao, Christine Quinn, Jayne Russell, Katherine E Keating, Fernando López-Ríos
Lung Cancer.2025; 201: 108107. CrossRef - Molecular testing of cytology specimens: Issues in specimen adequacy and clinical utility
Ghulam Ghous, Komal Ijaz, Magda Esebua, Lester J. Layfield
Diagnostic Cytopathology.2024; 52(2): 123. CrossRef - The updated College of American Pathologists principles of analytic validation of immunohistochemical assays: A step forward for cytopathology
Sinchita Roy‐Chowdhuri
Cancer Cytopathology.2024; 132(9): 547. CrossRef - Best-Practice Biomarker Testing of Oesophago-Gastric Cancer in the UK: Expert Consensus Recommendations Developed Using a Modified Delphi
N.P. West, W. Mansoor, P. Taniere, E. Smyth, M. Rodriguez-Justo, A. Oniscu, P. Carter
Clinical Oncology.2024; 36(11): 701. CrossRef - Next step of molecular pathology: next-generation sequencing in cytology
Ricella Souza da Silva, Fernando Schmitt
Journal of Pathology and Translational Medicine.2024; 58(6): 291. CrossRef
- Proposal of real-world solutions for the implementation of predictive biomarker testing in patients with operable non-small cell lung cancer

 E-submission
E-submission



 First
First Prev
Prev



