Search
- Page Path
- HOME > Search
- Diagnostic yield of fine needle aspiration with simultaneous core needle biopsy for thyroid nodules
- Mohammad Ali Hasannia, Ramin Pourghorban, Hoda Asefi, Amir Aria, Elham Nazar, Hojat Ebrahiminik, Alireza Mohamadian
- J Pathol Transl Med. 2025;59(3):180-187. Published online April 16, 2025
- DOI: https://doi.org/10.4132/jptm.2025.03.04
- 10,875 View
- 235 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Fine needle aspiration (FNA) is a widely utilized technique for assessing thyroid nodules; however, its inherent non-diagnostic rate poses diagnostic challenges. The present study aimed to evaluate and compare the diagnostic efficacy of FNA, core needle biopsy (CNB), and their combined application in the assessment of thyroid nodules.
Methods
A total of 56 nodules from 50 patients was analyzed using both FNA and simultaneous CNB. The ultrasound characteristics were categorized according to the American College of Radiology Thyroid Imaging Reporting and Data Systems classification system. The study compared the sensitivity, specificity, and accuracy of FNA, CNB, and the combination of the two techniques.
Results
The concordance between FNA and CNB was notably high, with a kappa coefficient of 0.837. The sensitivity for detecting thyroid malignancy was found to be 25.0% for FNA, 66.7% for CNB, and 83.3% for the combined FNA/CNB approach, with corresponding specificities of 84.6%, 97.4%, and 97.4%. The accuracy of the FNA/CNB combination was the highest at 94.1%.
Conclusions
The findings of this study indicate that both CNB and the FNA/CNB combination offer greater diagnostic accuracy for thyroid malignancy compared to FNA alone, with no significant complications reported. Integrating CNB with FNA findings may enhance management strategies and treatment outcomes for patients with thyroid nodules.
- Educational exchange in thyroid core needle biopsy diagnosis: enhancing pathological interpretation through guideline integration and peer learning
- Agnes Stephanie Harahap, Chan Kwon Jung
- J Pathol Transl Med. 2024;58(5):205-213. Published online July 24, 2024
- DOI: https://doi.org/10.4132/jptm.2024.06.24
- 5,011 View
- 297 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
While fine needle aspiration cytology (FNAC) plays an essential role in the screening of thyroid nodules, core needle biopsy (CNB) acts as an alternative method to address FNAC limitations. However, diagnosing thyroid CNB samples can be challenging due to variations in background and levels of experience. Effective training is indispensable to mitigate this challenge. We aim to evaluate the impact of an educational program on improving the accuracy of CNB diagnostics.
Methods
The 2-week observational program included a host mentor pathologist with extensive experience and a visiting pathologist. The CNB classification by The Practice Guidelines Committee of the Korean Thyroid Association was used for the report. Two rounds of reviewing the case were carried out, and the level of agreement between the reviewers was analyzed.
Results
The first-round assessment showed a concordance between two pathologists for 247 thyroid CNB specimens by 84.2%, with a kappa coefficient of 0.74 (indicating substantial agreement). This finding was attributed to the discordance in the use of categories III and V. After peer learning, the two pathologists evaluated 30 new cases, which showed an overall improvement in the level of agreement. The percentage of agreement between pathologists on thyroid CNB diagnosis was 86.7%, as measured by kappa coefficient of 0.80.
Conclusions
This educational program, consisting of guided mentorship and peer learning, can substantially enhance the diagnostic accuracy of thyroid CNB. It is useful in promoting consistent diagnostic standards and contributes to the ongoing development of global pathology practices. -
Citations
Citations to this article as recorded by- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
Agnes Stephanie Harahap, Maria Francisca Ham, Retno Asti Werdhani, Erwin Danil Julian, Rafi Ilmansyah, Chloe Indira Arfelita Mangunkusumso, Tri Juli Edi Tarigan
Journal of Pathology and Translational Medicine.2025; 59(3): 149. CrossRef
- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
- Concurrent intestinal plasmablastic lymphoma and diffuse large B-cell lymphoma with a clonal relationship: a case report and literature review
- Nao Imuta, Kosuke Miyai, Motohiro Tsuchiya, Mariko Saito, Takehiro Sone, Shinichi Kobayashi, Sho Ogata, Fumihiko Kimura, Susumu Matsukuma
- J Pathol Transl Med. 2024;58(4):191-197. Published online June 25, 2024
- DOI: https://doi.org/10.4132/jptm.2024.05.14
- 4,900 View
- 223 Download
-
 Abstract
Abstract
 PDF
PDF - Herein, we report a case of plasmablastic lymphoma (PBL) and diffuse large B-cell lymphoma (DLBCL) that occurred concurrently in the large intestine. An 84-year-old female presented with a palpable rectal tumor and ileocecal tumor observed on imaging analyses. Endoscopic biopsy of both lesions revealed lymphomatous round cells. Hartmann’s operation and ileocecal resection were performed for regional control. The ileocecal lesion consisted of a proliferation of CD20/CD79a-positive lymphoid cells, indicative of DLBCL. In contrast, the rectal tumor showed proliferation of atypical cells with pleomorphic nuclei and abundant amphophilic cytoplasm, with immunohistochemical findings of CD38/CD79a/MUM1/MYC (+) and CD20/CD3/CD138/PAX5 (–). Tumor cells were positive for Epstein-Barr virus– encoded RNA based on in situ hybridization and MYC rearrangement in fluorescence in situ hybridization analysis. These findings indicated the rectal tumor was most likely a PBL. Sequencing analysis for immunoglobulin heavy variable genes indicated a common B-cell origin of the two sets of lymphoma cells. This case report and literature review provide new insights into PBL tumorigenesis.
- Fibrin-associated large B-cell lymphoma arising in an endovascular graft: first case report in Korea
- Min Gyoung Pak, Mee Sook Roh
- J Pathol Transl Med. 2024;58(2):87-90. Published online January 24, 2024
- DOI: https://doi.org/10.4132/jptm.2023.12.28
- 4,175 View
- 267 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Fibrin-associated large B-cell lymphoma (FA-LBCL) is an extremely rare subtype of LBCL that consists of microscopic aggregates of atypical large B cells in the background of fibrin. Here, we report the first case of FA-LBCL in Korea. A 57-year-old male presented with a large amount of thrombus in the thoracic aorta during follow-up for graft replacement of the thoracoabdominal aorta 8 years prior. The removed thrombus, measuring 4.3 × 3.1 cm, histologically exhibited eosinophilic fibrinous material with several small clusters of atypical lymphoid cells at the periphery. The atypical cells were positive for CD20 by immunohistochemistry and for Epstein-Barr virus by in situ hybridization. The Ki-67 proliferation rate was 85%. The patient was still alive with no recurrence at the 7-year follow-up after thrombectomy. Although the diagnosis can be very difficult and challenging due to its paucicellular features, pathologists should be aware of FALBCL, which has likely been underestimated in routine evaluations of thrombi.
-
Citations
Citations to this article as recorded by- Acute Lower Limb Arterial Occlusion Due to Malignant Lymphoma: A Case Report
Hana Isokawa, Hiroshi Abe, Dai Ozaki, Hiroyuki Isogai, Tetsuro Miyazaki, Takashi Tokano, Tohru Minamino
Internal Medicine.2026;[Epub] CrossRef
- Acute Lower Limb Arterial Occlusion Due to Malignant Lymphoma: A Case Report
- Tumor-infiltrating T lymphocytes evaluated using digital image analysis predict the prognosis of patients with diffuse large B-cell lymphoma
- Yunjoo Cho, Jiyeon Lee, Bogyeong Han, Sang Eun Yoon, Seok Jin Kim, Won Seog Kim, Junhun Cho
- J Pathol Transl Med. 2024;58(1):12-21. Published online January 10, 2024
- DOI: https://doi.org/10.4132/jptm.2023.11.02
- 5,267 View
- 271 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The implication of the presence of tumor-infiltrating T lymphocytes (TIL-T) in diffuse large B-cell lymphoma (DLBCL) is yet to be elucidated. We aimed to investigate the effect of TIL-T levels on the prognosis of patients with DLBCL.
Methods
Ninety-six patients with DLBCL were enrolled in the study. The TIL-T ratio was measured using QuPath, a digital pathology software package. The TIL-T ratio was investigated in three foci (highest, intermediate, and lowest) for each case, resulting in TIL-T–Max, TIL-T–Intermediate, and TIL-T–Min. The relationship between the TIL-T ratios and prognosis was investigated.
Results
When 19% was used as the cutoff value for TIL-T–Max, 72 (75.0%) and 24 (25.0%) patients had high and low TIL-T–Max, respectively. A high TIL-T–Max was significantly associated with lower serum lactate dehydrogenase levels (p < .001), with patient group who achieved complete remission after RCHOP therapy (p < .001), and a low-risk revised International Prognostic Index score (p < .001). Univariate analysis showed that patients with a low TIL-T–Max had a significantly worse prognosis in overall survival compared to those with a high TIL-T–Max (p < .001); this difference remained significant in a multivariate analysis with Cox proportional hazards (hazard ratio, 7.55; 95% confidence interval, 2.54 to 22.42; p < .001).
Conclusions
Patients with DLBCL with a high TIL-T–Max showed significantly better prognosis than those with a low TIL-T–Max, and the TIL-T–Max was an independent indicator of overall survival. These results suggest that evaluating TIL-T ratios using a digital pathology system is useful in predicting the prognosis of patients with DLBCL. -
Citations
Citations to this article as recorded by- Do Pre‐Treatment Biopsy Characteristics Predict Early Tumour Progression in Feline Diffuse Large B Cell Nasal Lymphoma Treated With Radiotherapy?
Valerie J. Poirier, Valeria Meier, Michelle Turek, Neil Christensen, Jacqueline Bowal, Matthew D. Ponzini, Stefan M. Keller
Veterinary and Comparative Oncology.2025; 23(1): 82. CrossRef - Comprehensive Analysis of Tumor Microenvironment and PD-L1 Expression Associations with Clinicopathological Features and Prognosis in Diffuse Large B-Cell Lymphoma
Yun-Li Xie, Long-Feng Ke, Wen-Wen Zhang, Fu Kang, Shu-Yi Lu, Chen-Yu Wu, Huan-Huan Zhu, Jian-Chao Wang, Gang Chen, Yan-Ping Chen
Blood and Lymphatic Cancer: Targets and Therapy.2025; Volume 15: 167. CrossRef - Metabolic-immune axis in the tumor microenvironment: a new strategy for prognostic assessment and precision therapy in DLBCL and FL
Chengqian Chen, Wei Guo, Haotian Wang, Luming Cao, Ou Bai
Frontiers in Immunology.2025;[Epub] CrossRef - Integrative analysis of a novel immunogenic PANoptosis‑related gene signature in diffuse large B-cell lymphoma for prognostication and therapeutic decision-making
Ming Xu, Ming Ruan, Wenhua Zhu, Jiayue Xu, Ling Lin, Weili Li, Weirong Zhu
Scientific Reports.2024;[Epub] CrossRef
- Do Pre‐Treatment Biopsy Characteristics Predict Early Tumour Progression in Feline Diffuse Large B Cell Nasal Lymphoma Treated With Radiotherapy?
- Metallic implant-associated lymphoma: ALK-negative anaplastic large cell lymphoma associated with total knee replacement arthroplasty
- Jai-Hyang Go
- J Pathol Transl Med. 2023;57(1):75-78. Published online January 10, 2023
- DOI: https://doi.org/10.4132/jptm.2022.10.30
- 5,225 View
- 116 Download
- 2 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Metallic implant-associated lymphomas are extremely rare. Only seven cases have been reported in association with knee joint arthroplasty, and all tumors were large B-cell lymphomas. This report is the first case of anaplastic large cell lymphoma occurring after total knee replacement arthroplasty. An 80‑year‑old female patient was admitted because of right knee pain for 2 years. She had undergone total knee replacement arthroplasty 10 years prior. Computed tomography showed an irregular osteolytic lesion in the right lateral femoral condyle, adjacent to the metallic prosthesis. Histologic findings reveal sheets of anaplastic tumor cells that were positive for CD2, CD4, CD5, CD43, and CD30 but negative for CD3, CD20, CD15, and anaplastic lymphoma kinase. Epstein-Barr encoding region in situ hybridization was negative. Analysis of T-cell receptor γ gene rearrangement studies using BIOMED-2–based multiplex polymerase chain reaction confirmed monoclonal T cell proliferation. The woman was finally diagnosed with ALK-negative anaplastic large cell lymphoma.
-
Citations
Citations to this article as recorded by- Clinical and microscopic evidence of biofilm formation on titanium miniplates applied in maxillofacial surgery: a case series analysis
Bramasto Purbo Sejati, Ahmad Kusumaatmaja, Maria Goreti Widiastuti, Tetiana Haniastuti
Case Reports in Plastic Surgery and Hand Surgery.2025;[Epub] CrossRef - Granulomatous Mycosis Fungoides Associated with Knee Prostheses: A Case Report and Literature Review
Belloso Rosa Izu, Rodriguez Blandon Jurvist Stee, Peña Nekane Martinez, Colunga Barbara Lada, Izaguirre Ane Lobato, Apraiz Isabel Gainza, Ponsa Carla Valenti
International Journal of Dermatology and Clinical Research.2025; 11(1): 022. CrossRef - Primary bone diffuse large B‐cell lymphoma (PB‐DLBCL): a distinct extranodal lymphoma of germinal centre origin, with a common EZB‐like mutational profile and good prognosis
Vanesa‐Sindi Ivanova, John Davies, Thomas Menter, Damian Wild, Anne Müller, Fatime Krasniqi, Frank Stenner, Alexandros Papachristofilou, Stefan Dirnhofer, Alexandar Tzankov
Histopathology.2024; 84(3): 525. CrossRef - Osteosarcoma After Total Knee Arthroplasty
Pablo Martínez-Collado, Oriol Pujol, Andrés Bustos, Martí Plomer, María G. Carrasco, Tulio Silva, Roberto Vélez, Joan Minguell
JBJS Case Connector.2024;[Epub] CrossRef
- Clinical and microscopic evidence of biofilm formation on titanium miniplates applied in maxillofacial surgery: a case series analysis
- Prognostic significance of BLK expression in R-CHOP treated diffuse large B-cell lymphoma
- Soyeon Choi, Yoo Jin Lee, Yunsuk Choi, Misung Kim, Hyun-Jung Kim, Ji Eun Kim, Sukjoong Oh, Seoung Wan Chae, Hee Jeong Cha, Jae-Cheol Jo
- J Pathol Transl Med. 2022;56(5):281-288. Published online September 13, 2022
- DOI: https://doi.org/10.4132/jptm.2022.07.26
- 5,296 View
- 107 Download
- 3 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The aim of the present study was to evaluate the prognostic significance of B-cell lymphocyte kinase (BLK) expression for survival outcomes in diffuse large B-cell lymphoma (DLBCL) patients treated with R-CHOP.
Methods
We retrospectively analyzed the medical records of 89 patients from two tertiary referral hospitals. The expression of BLK, SYK, and CDK1 were evaluated in a semiquantitative method using an H-score, and the proportions of BCL2 and C-MYC were evaluated.
Results
A total of 89 patients received R-CHOP chemotherapy as a first-line chemotherapy. The expression rates of BLK in tumor cells was 39.2% (n = 34). BLK expression status was not significantly associated with clinical variables; however, BLK expression in tumor cells was significantly associated with the expression of both C-MYC and BCL2 (p = .003). With a median follow-up of 60.4 months, patients with BLK expression had significantly lower 5-year progression-free survival (PFS) and overall survival rates (49.8% and 60.9%, respectively) than patients without BLK expression (77.3% and 86.7%, respectively). In multivariate analysis for PFS, BLK positivity was an independent poor prognostic factor (hazard ratio, 2.208; p = .040).
Conclusions
Here, we describe the clinicopathological features and survival outcome according to expression of BLK in DLBCL. Approximately 39% of DLBCL patients showed BLK positivity, which was associated as a predictive marker for poor prognosis in patients who received R-CHOP chemotherapy. -
Citations
Citations to this article as recorded by- Exploring the cell-free total RNA transcriptome in diffuse large B-cell lymphoma and primary mediastinal B-cell lymphoma patients as biomarker source in blood plasma liquid biopsies
Philippe Decruyenaere, Edoardo Giuili, Kimberly Verniers, Jasper Anckaert, Katrien De Grove, Malaïka Van der Linden, Dries Deeren, Jo Van Dorpe, Fritz Offner, Jo Vandesompele
Frontiers in Oncology.2023;[Epub] CrossRef
- Exploring the cell-free total RNA transcriptome in diffuse large B-cell lymphoma and primary mediastinal B-cell lymphoma patients as biomarker source in blood plasma liquid biopsies
- An unusual case of microsatellite instability–high/deficient mismatch repair (MSI-H/dMMR) diffuse large B-cell lymphoma revealed by targeted gene sequencing
- Bogyeong Han, Sehui Kim, Jiwon Koh, Jeong Mo Bae, Hongseok Yun, Yoon Kyung Jeon
- J Pathol Transl Med. 2022;56(2):92-96. Published online November 16, 2021
- DOI: https://doi.org/10.4132/jptm.2021.10.15
- 9,238 View
- 263 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Microsatellite instability-high/deficient mismatch repair (MSI-H/dMMR) status has been approved as a tissue-agnostic biomarker for immune checkpoint inhibitor therapy in patients with solid tumors. We report the case of an MSI-H/dMMR diffuse large B-cell lymphoma (DLBCL) identified by targeted gene sequencing (TGS). A 90-year-old female who presented with vaginal bleeding and a large mass in the upper vagina was diagnosed with germinal center-B-cell-like DLBCL, which recurred at the uterine cervix at 9 months after chemotherapy. Based on TGS of 121 lymphoma-related genes and the LymphGen algorithm, the tumor was classified genetically as DLBCL of EZB subtype. Mutations in multiple genes, including frequent frameshift mutations, were detected by TGS and further suggested MSI. The MSI-H/dMMR and loss of MLH1 and PMS2 expression were determined in MSI-fragment analysis, MSI real-time polymerase chain reaction, and immunohistochemical tests. This case demonstrates the potential diagnostic and therapeutic utility of lymphoma panel sequencing for DLBCL with MSI-H/dMMR.
-
Citations
Citations to this article as recorded by- Shared genomic features of HIV+ diffuse large B-cell lymphoma in two African cohorts
Sophia M. Roush, Mishalan Moodley, Jenny Coelho, Samantha Beck, Amon Chirwa, Edwards Kasonkanji, Marriam Mponda, Maurice Mulenga, Tamiwe Tomoka, Hanri van Zijl, Katherine Hodkinson, Arshad Ismail, Senzo Mtshali, Jonathan Featherston, Satish Gopal, Matthew
Scientific Reports.2025;[Epub] CrossRef - Chimeric and mutant CARD9 constructs enable analyses of conserved and diverged autoinhibition mechanisms in the CARD‐CC protein family
Jens Staal, Yasmine Driege, Femke Van Gaever, Jill Steels, Rudi Beyaert
The FEBS Journal.2024; 291(6): 1220. CrossRef - PD-L1+diffuse large B-cell lymphoma with extremely high mutational burden and microsatellite instability due to acquiredPMS2mutation
Andrew W. Allbee, James Gerson, Guang Yang, Adam Bagg
Molecular Case Studies.2023; 9(4): a006318. CrossRef
- Shared genomic features of HIV+ diffuse large B-cell lymphoma in two African cohorts
- Clinicopathologic implication of PD-L1 gene alteration in primary adrenal diffuse large B cell lymphoma
- Ki Rim Lee, Jiwon Koh, Yoon Kyung Jeon, Hyun Jung Kwon, Jeong-Ok Lee, Jin Ho Paik
- J Pathol Transl Med. 2022;56(1):32-39. Published online November 16, 2021
- DOI: https://doi.org/10.4132/jptm.2021.10.05
- 5,508 View
- 169 Download
- 1 Web of Science
-
 Abstract
Abstract
 PDF
PDF - Background
Primary adrenal (PA) diffuse large B cell lymphoma (DLBCL) was previously reported as an aggressive subset of DLBCL, but its genetic features were not sufficiently characterized. From our previous study of DLBCL with programmed death-ligand 1 (PD-L1) gene alterations, we focused on PD-L1 gene alterations in PA-DLBCL with clinicopathologic implications.
Methods
We performed fluorescence in situ hybridization for PD-L1 gene translocation and amplification in PA-DLBCL (n = 18) and comparatively analyzed clinicopathologic characteristics with systemic non-adrenal (NA)-DLBCL (n = 90).
Results
PA-DLBCL harbored distinctive features (vs. NADLBCL), including high international prognostic index score (3–5) (72% [13/18] vs. 38% [34/90], p = .007), poor Eastern Cooperative Oncology Group performance score (≥ 2) (47% [7/15] vs. 11% [10/90], p = .003), elevated serum lactate dehydrogenase (LDH) (78% [14/18] vs. 51% [44/87], p = .035) and MUM1 expression (87% [13/15] vs. 60% [54/90], p = .047). Moreover, PA-DLBCL showed frequent PD-L1 gene alterations (vs. NA-DLBCL) (39% [7/18] vs. 6% [5/86], p = .001), including translocation (22% [4/18] vs. 3% [3/87], p = .016) and amplification (17% [3/18] vs. 2% [2/87], p = .034). Within the PA-DLBCL group, PD-L1 gene–altered cases (vs. non-altered cases) tended to have B symptoms (p = .145) and elevated LDH (p = .119) but less frequent bulky disease (≥ 10 cm) (p = .119). In the survival analysis, PA-DLBCL had a poor prognosis for overall survival (OS) and progression-free survival (PFS) (vs. NA-DLBCL; p = .014 and p = .004). Within the PA-DLBCL group, PD-L1 translocation was associated with shorter OS and PFS (p < .001 and p = .012).
Conclusions
PA-DLBCL is a clinically aggressive and distinct subset of DLBCL with frequent PD-L1 gene alterations. PD-L1 gene translocation was associated with poor prognosis in PA-DLBCL.
- Renal intravascular large B cell lymphoma: the first case report in Korea and a review of the literature
- Moonsik Kim, Haerim Chung, Woo Ick Yang, Hyeon Joo Jeong
- J Pathol Transl Med. 2020;54(5):426-431. Published online August 13, 2020
- DOI: https://doi.org/10.4132/jptm.2020.06.18
- 6,323 View
- 121 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Herein, we describe the first case of renal intravascular large B cell lymphoma in Korea occurring in a 66-year-old female. She presented with mild fever and dyspnea. On physical and laboratory evaluations, hemophagocytic lymphohistiocytosis was suspected, but the bone marrow biopsy results were unremarkable. During the work-up, massive proteinuria developed, which led to a renal biopsy. The renal architecture was relatively well-preserved, but the glomeruli were hypercellular with the infiltration of atypical, large lymphoid cells with increased nucleus-cytoplasm ratio and clumped chromatin. Similar cells were also present in the peritubular capillaries. The tumor cells exhibited membranous staining for CD20 and CD79a. After the diagnosis of intravascular large B cell lymphoma, the patient received rituximab-based chemotherapy under close follow-up.
-
Citations
Citations to this article as recorded by- Intravascular large B-cell lymphoma of the central nervous system with renal involvement: a case report and literature review
Jun Li, Zhaojiao Li, Yifeng Shi, Jiajie Chen, Heng Zhao, Xueye Mao, Shan Li, Huiying Wang, Qiang Meng, Lingchun Liu
Frontiers in Oncology.2025;[Epub] CrossRef - EBV-Positive Intravascular Large B-Cell Lymphoma of the Small Intestine: A Case Report and Literature Review
Chenglong Pan, Xiaoling Ma, Yanfei Yao, Chunyan Wang
International Journal of Surgical Pathology.2024; 32(3): 586. CrossRef - Intravascular large B‐cell lymphoma in renal cell carcinoma incidentally detected by robot‐assisted partial nephrectomy
Michio Noda, Yutaka Enomoto, Yukari Shirasugi, Sumiyo Ando, Yukimasa Matsuzawa, Haruki Kume
IJU Case Reports.2022; 5(3): 191. CrossRef - Case Report: Intravascular Large B-Cell Lymphoma: A Clinicopathologic Study of Four Cases With Review of Additional 331 Cases in the Literature
Yingying Han, Qingjiao Li, Dan Wang, Lushan Peng, Tao Huang, Chunlin Ou, Keda Yang, Junpu Wang
Frontiers in Oncology.2022;[Epub] CrossRef - Renal Involvement of CD20-Negative Intravascular Large B Cell Lymphoma with Neurological Manifestations
Faten Aqeel, Serena M. Bagnasco, Duvuru Geetha, Yoshihide Fujigaki
Case Reports in Nephrology.2022; 2022: 1. CrossRef
- Intravascular large B-cell lymphoma of the central nervous system with renal involvement: a case report and literature review
- Combined Adenosquamous and Large Cell Neuroendocrine Carcinoma of the Gallbladder
- Jiyoon Jung, Yang-Seok Chae, Chul Hwan Kim, Youngseok Lee, Jeong Hyeon Lee, Dong-Sik Kim, Young-Dong Yu, Joo Young Kim
- J Pathol Transl Med. 2018;52(2):121-125. Published online October 5, 2017
- DOI: https://doi.org/10.4132/jptm.2017.08.20
- 8,962 View
- 155 Download
- 12 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Large cell neuroendocrine carcinoma (LCNEC) of the gallbladder is extremely rare and usually combined with other type of malignancy, mostly adenocarcinoma. We report an unusual case of combined adenosquamous carcinoma and LCNEC of the gallbladder in a 54-year-old woman. A radical cholecystectomy specimen revealed a 4.3×4.0 cm polypoid mass in the fundus with infiltration of adjacent liver parenchyma. Microscopically, the tumor consisted of two distinct components. Adenosquamous carcinoma was predominant and abrupt transition from adenocarcinoma to squamous cell carcinoma was observed. LCNEC showed round cells with large, vesicular nuclei, abundant mitotic figures, and occasional pseudorosette formation. The patient received adjuvant chemotherapy. However, multiple liver metastases were identified at 3-month follow-up. Metastatic nodules were composed of LCNEC and squamous cell carcinoma components. Detecting LCNEC component is important in gallbladder cancer, because the tumor may require a different chemotherapy regimen and show early metastasis and poor prognosis.
-
Citations
Citations to this article as recorded by- Postoperative gastric cancer accompanied by large-cell neuroendocrine carcinoma: A case report
Zhiqin Chen, Jiang Liu, Jin Liu, Yinhang Wu, Jian Liu
Medicine.2025; 104(41): e44367. CrossRef - Does the size of the neuroendocrine-carcinoma component determine the prognosis of gallbladder cancer?
Ya-Fei Hu, Jun-Ke Wang, Wen-Jie Ma, Hai-Jie Hu, Han-Fei Gu, Fei Liu, Tian-Run Lv, Si-Qi Yang, Yu-Shi Dai, Rui-Qi Zou, Yan-Wen Jin, Fu-Yu Li
Frontiers in Endocrinology.2024;[Epub] CrossRef - Az epehólyag adenosquamosus daganata
Fanni Hegedűs, Anita Sejben
Orvosi Hetilap.2024; 165(49): 1945. CrossRef - Comparison of Metastatic Patterns Among Neuroendocrine Tumors, Neuroendocrine Carcinomas, and Nonneuroendocrine Carcinomas of Various Primary Organs
Hyung Kyu Park, Ghee Young Kwon
Journal of Korean Medical Science.2023;[Epub] CrossRef - Clinical features and outcomes analysis of Gallbladder neuroendocrine carcinoma
Man Jiang, Yijing Zhang
Journal of Cancer Research and Therapeutics.2023; 19(4): 910. CrossRef - Primary mixed large cell neuroendocrine carcinoma and adenocarcinoma of the gallbladder: A case report and literature review
Tingting Yu, Shike Li, Zhuo Zhang
Asian Journal of Surgery.2022; 45(11): 2336. CrossRef - Mixed neuroendocrine-non-neuroendocrine neoplasm of the gallbladder: case report and literature review
Xu Ren, Hong Jiang, Kan Sun, Xufu Qin, Yongping Qu, Tian Xia, Yan Chen
Diagnostic Pathology.2022;[Epub] CrossRef - Neuroendocrine Neoplasms of the Gallbladder: A Clinicopathological Analysis of 13 Patients and a Review of the Literature
Pengyan Wang, Jingci Chen, Ying Jiang, Congwei Jia, Junyi Pang, Shan Wang, Xiaoyan Chang, Oronzo Brunetti
Gastroenterology Research and Practice.2021; 2021: 1. CrossRef - Gallbladder Mixed Neuroendocrine-Non-neuroendocrine Neoplasm (MiNEN) Arising in Intracholecystic Papillary Neoplasm: Clinicopathologic and Molecular Analysis of a Case and Review of the Literature
Amedeo Sciarra, Edoardo Missiaglia, Mounir Trimech, Emmanuel Melloul, Jean-Philippe Brouland, Christine Sempoux, Stefano La Rosa
Endocrine Pathology.2020; 31(1): 84. CrossRef - Mixed neuroendocrine-non-neuroendocrine carcinoma of gallbladder: case report
Adam Skalický, Lucie Vištejnová, Magdaléna Dubová, Tomáš Malkus, Tomáš Skalický, Ondřej Troup
World Journal of Surgical Oncology.2019;[Epub] CrossRef
- Postoperative gastric cancer accompanied by large-cell neuroendocrine carcinoma: A case report
- A Small Case Series of Intravascular Large B-Cell Lymphoma with Unexpected Findings: Subset of Cases with Concomitant Extravascular Central Nervous System (CNS) Involvement Mimicking Primary CNS Lymphoma
- Kate Poropatich, Dave Dittmann, Yi-Hua Chen, Kirtee Raparia, Kristy Wolniak, Juehua Gao
- J Pathol Transl Med. 2017;51(3):284-291. Published online April 17, 2017
- DOI: https://doi.org/10.4132/jptm.2017.02.16
- 13,029 View
- 226 Download
- 11 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Intravascular large B-cell lymphoma (IVLBCL) is a rare type of extranodal lymphoma with growth mainly in the lumina of vessels. We studied a small series of IVLBCL and focused on its central nervous system (CNS) involvement.
Methods
Searching the medical records of Northwestern Memorial Hospital, we identified five cases of IVLBCL from January 2007 to January 2015. Clinical information, hematoxylin and eosin stained histologic slides and immunohistochemistry studies were reviewed for all cases. Polymerase chain reaction (PCR) analysis for the immunoglobulin (Ig) heavy and light chain gene rearrangement was performed on all five cases.
Results
Three of the five cases of IVLBCL were autopsies. Patients’ age ranged from 56 to 84. CNS involvement was present in two cases—in both patients, the CNS involvement showed an extravascular pattern with confluent sheet-like formation. PCR analysis confirmed that in one case the systemic intravascular and CNS extravascular components were clonally identical.
Conclusions
In a small case series of IVLBCL, we observed that CNS involvement by IVLBCL often has an extravascular morphology, but is clonally identical to the intravascular counterpart by PCR analysis. As IVLBCL can have a rapidly progressing poor outcome, it should be kept in the differential diagnoses for patients presenting with lymphoma of the CNS. The presence of extravascular growth patterns in the CNS should not exclude IVLBCL as a diagnosis. -
Citations
Citations to this article as recorded by- Clinical manifestations and outcomes of patients with intravascular large B-cell lymphoma with neurological involvement: highlighting longitudinally extensive myelopathy as a distinct feature
Ekdanai Uawithya, Palakorn Lertsakworakul, Weerapat Owatthanapanich, Jiraporn Jitprapaikulsan
BMJ Neurology Open.2025; 7(1): e000915. CrossRef - Intravascular large B-cell lymphoma of the central nervous system with renal involvement: a case report and literature review
Jun Li, Zhaojiao Li, Yifeng Shi, Jiajie Chen, Heng Zhao, Xueye Mao, Shan Li, Huiying Wang, Qiang Meng, Lingchun Liu
Frontiers in Oncology.2025;[Epub] CrossRef - A single institution series of intravascular lymphoma: Neurological manifestations and neuroimaging findings
J. Corroza, C. Alburquerque, L. Martínez-Martínez, I. Gastón, L. Torné, M.C. Gil-Alzueta, J. Oteiza, T. Cabada, M.C. Viguria, A. Panizo, M.E. Erro
Neurología.2025; 40(8): 768. CrossRef - A Rare Case of Adrenal Intravascular Large B-Cell Lymphoma Diagnosed via Percutaneous Needle Biopsy
Jiafei Zeng, Jin Li, Shuai Luo, Jinjing Wang
World Journal of Surgical Oncology.2025;[Epub] CrossRef - Intravascular Lymphoma: A Unique Pattern Underlying a Protean Disease
Mario Della Mura, Joana Sorino, Filippo Emanuele Angiuli, Gerardo Cazzato, Francesco Gaudio, Giuseppe Ingravallo
Cancers.2025; 17(14): 2355. CrossRef - A single institution series of intravascular lymphoma: Neurological manifestations and neuroimaging findings
J. Corroza, C. Alburquerque, L. Martínez-Martínez, I. Gastón, L. Torné, M.C. Gil-Alzueta, J. Oteiza, T. Cabada, M.C. Viguria, A. Panizo, M.E. Erro
Neurología (English Edition).2025; 40(8): 768. CrossRef - Intravascular Large B-Cell Lymphoma Presenting as Migraine with Aura: A Case Report
Sydney Moseley, Robert Fekete
Case Reports in Neurology.2025; 17(1): 176. CrossRef - A case report and literature review of cutaneous intravascular large B-cell lymphoma presenting clinically as panniculitis: a difficult diagnosis, but a good prognosis
Deniz Bayçelebi, Levent Yıldız, Nilgün Şentürk
Anais Brasileiros de Dermatologia.2021; 96(1): 72. CrossRef - Diffuse large B-cell lymphoma (DLBCL) with significant intravascular invasion. Close resemblance of its clinicopathological features to intravascular large B-cell lymphoma, but not to DLBCL-not otherwise specified
Hiroe Itami, Hirokazu Nakamine, Masayuki Kubo, Kohei Ogawa, Rina Tani, Shinji Nakamura, Maiko Takeda, Yuji Nitta, Tomoko Uchiyama, Tomomi Fujii, Kinta Hatakeyama, Chiho Ohbayashi
Journal of Clinical and Experimental Hematopathology.2021; 61(3): 152. CrossRef - Unusual and Fatal Case of an Undiagnosed Intravascular Large B‐cell Lymphoma: The Oncologist’s Great Imitator†
Rosario Barranco, Fiorella Caputo, Davide Bedocchi, Francesca Maria Elena Frigiolini, Lara Castelletti, Giulio Fraternali Orcioni, Francesco Ventura
Journal of Forensic Sciences.2020; 65(1): 314. CrossRef - Pituitary Gland and Neurological Involvement in a Case of Hemophagocytic Syndrome Revealing an Intravascular Large B-Cell Lymphoma
Sylvain Raoul Simeni Njonnou, Bruno Couturier, Yannick Gombeir, Sylvain Verbanck, France Devuyst, Georges El Hachem, Ivan Theate, Anne-Laure Trepant, Virginie De Wilde, Frédéric-Alain Vandergheynst
Case Reports in Hematology.2019; 2019: 1. CrossRef - Accurate Detection of Tumor Infiltration by 11C-Methionine Positron Emission Tomography in a Patient with Central Nervous System Intravascular Lymphoma: A Case Report
Shoji Yomo, Keiji Tsutsumi, Takehiro Yako, Hiromasa Sato, Takao Hashimoto, Kazuhiro Oguchi
Case Reports in Oncology.2018; 11(2): 577. CrossRef
- Clinical manifestations and outcomes of patients with intravascular large B-cell lymphoma with neurological involvement: highlighting longitudinally extensive myelopathy as a distinct feature
- Long Non-coding RNA HOTAIR Expression in Diffuse Large B-Cell Lymphoma: In Relation to Polycomb Repressive Complex Pathway Proteins and H3K27 Trimethylation
- Eun Ji Oh, Soo Hee Kim, Woo Ick Yang, Young Hyeh Ko, Sun Och Yoon
- J Pathol Transl Med. 2016;50(5):369-376. Published online August 22, 2016
- DOI: https://doi.org/10.4132/jptm.2016.06.06
- 11,060 View
- 174 Download
- 27 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
A long non-coding RNA hox transcript antisense intergenic RNA (HOTAIR) is involved in epigenetic regulation through chromatin remodeling by recruiting polycomb repressive complex 2 (PRC2) proteins (EZH2, SUZ12, and EED) that induce histone H3 trimethylation at lysine 27 (H3K27me3). Deregulation of c-MYC and interaction between c-MYC and EZH2 are well known in lymphomagenesis; however, little is known about the expression status of HOTAIR in diffuse large B-cell lymphomas (DLBCLs).
Methods
The expression status of PRC2 (EZH2, SUZ12, and EED), H3K27me3, c-MYC, and BCL2 was analyzed using immunohistochemistry (n = 231), and HOTAIR was investigated by a quantification real-time polymerase chain reaction method (n = 164) in DLBCLs.
Results
The present study confirmed the positive correlation among PRC2 proteins, H3K27me3, and c-MYC in DLBCLs. Expression level of HOTAIR was also positively correlated to EZH2 (p < .05, respectively). Between c-MYC and HOTAIR, and between c- MYC/BCL2 co-expression and HOTAIR, however, negative correlation was observed in DLBCLs (p < .05, respectively). High level of H3K27me3 was determined as an independent prognostic marker in poor overall survival (hazard ratio, 2.0; p = .023) of DLBCL patients. High expression of HOTAIR, however, was associated with favorable overall survival (p = .004) in the univariate analysis, but the impact was not significant in the multivariate analysis. The favorable outcome of DLBCL with HOTAIR high expression levels may be related to the negative correlation with c- MYC expression or c-MYC/BCL2 co-expression.
Conclusions
HOTAIR expression could be one of possible mechanisms for inducing H3K27me3 via EZH2-related PRC2 activation, and induced H3K27me3 may be strongly related to aggressive DLBCLs which show poor patient outcome. -
Citations
Citations to this article as recorded by- EZH2 Dysregulation and Its Oncogenic Role in Human Cancers
Shiv Verma, Nikita Goyal, Suhani Goyal, Parminder Kaur, Sanjay Gupta
Cancers.2025; 17(19): 3111. CrossRef - HOTAIR in cancer: diagnostic, prognostic, and therapeutic perspectives
Majid Nazari, Emad Babakhanzadeh, Arghavan Mollazadeh, Mohadese Ahmadzade, Elham Mohammadi Soleimani, Elnaz Hajimaqsoudi
Cancer Cell International.2024;[Epub] CrossRef - Long noncoding RNAs (lncRNAs) in human lymphomas
Ali Gholami, Khosro Farhadi, Fatemeh Sayyadipour, Masoud Soleimani, Fakhredin Saba
Genes & Diseases.2022; 9(4): 900. CrossRef - Long noncoding RNAs (lncRNAs) in HIV-mediated carcinogenesis: Role in cell homeostasis, cell survival processes and drug resistance
Lilian Makgoo, Salerwe Mosebi, Zukile Mbita
Non-coding RNA Research.2022; 7(3): 184. CrossRef - Biomedical impact of the expression of HOX locus-associated LncRNAs HOTAIR and HOTTIP in diffuse large B cell lymphoma
Mona Salah Eldin Habieb, Suzy Fawzy Goher, Abd-Elmonem Abd-Elkader El-Torgman, Ibrahim El Tantawy El Sayed, Najlaa Zanati Ali Abd-Elfattah
Human Gene.2022; 34: 201112. CrossRef - Mechanism of LncHOTAIR Regulating Proliferation, Apoptosis, and Autophagy of Lymphoma Cells through hsa-miR-6511b-5p/ATG7 Axis
Fu Gui, Xinyi Yu, Yemeng Wu, Chao Wu, Yulan Zhang, Peng-Yue Zhang
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef -
Circulating RNA biomarkers in diffuse large B-cell lymphoma: a systematic review
Philippe Decruyenaere, Fritz Offner, Jo Vandesompele
Experimental Hematology & Oncology.2021;[Epub] CrossRef - Circulating long non-coding RNAs HOTAIR, Linc-p21, GAS5 and XIST expression profiles in diffuse large B-cell lymphoma: association with R-CHOP responsiveness
Mahmoud A. Senousy, Aya M. El-Abd, Raafat R. Abdel-Malek, Sherine M. Rizk
Scientific Reports.2021;[Epub] CrossRef - An immunotherapeutic approach to decipher the role of long non-coding RNAs in cancer progression, resistance and epigenetic regulation of immune cells
Krishnapriya M. Varier, Hemavathi Dhandapani, Wuling Liu, Jialei Song, Chunlin Wang, Anling Hu, Yaacov Ben-David, Xiangchun Shen, Yanmei Li, Babu Gajendran
Journal of Experimental & Clinical Cancer Research.2021;[Epub] CrossRef - Cancer‑associated fibroblast‑derived CCL5 contributes to cisplatin resistance in A549 NSCLC cells partially through upregulation of lncRNA HOTAIR expression
Xiangjun Sun, Zhijie Chen
Oncology Letters.2021;[Epub] CrossRef - Competitive Endogenous RNA Network Involving miRNA and lncRNA in Non-Hodgkin Lymphoma: Current Advances and Clinical Perspectives
Mara Fernandes, Herlander Marques, Ana Luísa Teixeira, Rui Medeiros
Biomedicines.2021; 9(12): 1934. CrossRef - EZH2 expression is dependent on MYC and TP53 regulation in diffuse large B‐cell lymphoma
Eduardo Henrique Neves Filho, Carlos Gustavo Hirth, Igor Allen Frederico, Rommel Mario Burbano, Thiago Carneiro, Silvia Helena Rabenhorst
APMIS.2020; 128(4): 308. CrossRef Long Noncoding RNAs in Diffuse Large B-Cell Lymphoma: Current Advances and Perspectives
Xianbo Huang, Wenbin Qian, Xiujin Ye
OncoTargets and Therapy.2020; Volume 13: 4295. CrossRef- Lnc SMAD5-AS1 as ceRNA inhibit proliferation of diffuse large B cell lymphoma via Wnt/β-catenin pathway by sponging miR-135b-5p to elevate expression of APC
Chen-Chen Zhao, Yang Jiao, Yi-Yin Zhang, Jie Ning, Yi-Ruo Zhang, Jing Xu, Wei Wei, Gu Kang-Sheng
Cell Death & Disease.2019;[Epub] CrossRef - H3K18Ac as a Marker of Cancer Progression and Potential Target of Anti-Cancer Therapy
Marta Hałasa, Anna Wawruszak, Alicja Przybyszewska, Anna Jaruga, Małgorzata Guz, Joanna Kałafut, Andrzej Stepulak, Marek Cybulski
Cells.2019; 8(5): 485. CrossRef - HOTAIR as a Prognostic Predictor for Diverse Human Cancers: A Meta- and Bioinformatics Analysis
Halil Ibrahim Toy, Didem Okmen, Panagiota I. Kontou, Alexandros G. Georgakilas, Athanasia Pavlopoulou
Cancers.2019; 11(6): 778. CrossRef - Long Noncoding RNA HOTAIR Promotes Endometrial Carcinoma Cell Proliferation by Binding to PTEN via the Activating Phosphatidylinositol 3-Kinase/Akt Signaling Pathway
Xiao-Hui Zhang, Pin Hu, Yang-Qin Xie, Yong-Jun Kang, Min Li
Molecular and Cellular Biology.2019;[Epub] CrossRef - EZH2 abnormalities in lymphoid malignancies: underlying mechanisms and therapeutic implications
Boheng Li, Wee-Joo Chng
Journal of Hematology & Oncology.2019;[Epub] CrossRef - The prognostic impact of long noncoding RNA HOTAIR in leukemia and lymphoma: a meta-analysis
Yun Lin, Zhihong Fang, Zhijuan Lin, Zhifeng Li, Jintao Zhao, Yiming Luo, Bing Xu
Hematology.2018; 23(9): 600. CrossRef - Retracted: Downregulation of Long Noncoding RNA HOTAIR and EZH2 Induces Apoptosis and Inhibits Proliferation, Invasion, and Migration of Human Breast Cancer Cells
Lu Han, Hai-Chao Zhang, Li Li, Cai-Xia Li, Xu Di, Xin Qu
Cancer Biotherapy and Radiopharmaceuticals.2018; 33(6): 241. CrossRef - Long Non-Coding RNAs Guide the Fine-Tuning of Gene Regulation in B-Cell Development and Malignancy
Mette Dahl, Lasse Sommer Kristensen, Kirsten Grønbæk
International Journal of Molecular Sciences.2018; 19(9): 2475. CrossRef - HOTAIR, a long noncoding RNA, is a marker of abnormal cell cycle regulation in lung cancer
Minghui Liu, Hongyi Zhang, Ying Li, Rui Wang, Yongwen Li, Hongbing Zhang, Dian Ren, Hongyu Liu, Chunsheng Kang, Jun Chen
Cancer Science.2018; 109(9): 2717. CrossRef - The evolving concept of cancer stem-like cells in thyroid cancer and other solid tumors
Heather Hardin, Ranran Zhang, Holly Helein, Darya Buehler, Zhenying Guo, Ricardo V Lloyd
Laboratory Investigation.2017; 97(10): 1142. CrossRef - Emerging roles for long noncoding RNAs in B-cell development and malignancy
M. Winkle, J.L. Kluiver, A. Diepstra, A. van den Berg
Critical Reviews in Oncology/Hematology.2017; 120: 77. CrossRef
- EZH2 Dysregulation and Its Oncogenic Role in Human Cancers
- Prognostic Implication of Semi-quantitative Immunohistochemical Assessment of CD20 Expression in Diffuse Large B-Cell Lymphoma
- Chang Hwan Choi, Young Hoon Park, Joo Han Lim, Suk Jin Choi, Lucia Kim, In Suh Park, Jee Young Han, Joon Mee Kim, Young Chae Chu
- J Pathol Transl Med. 2016;50(2):96-103. Published online February 15, 2016
- DOI: https://doi.org/10.4132/jptm.2016.01.12
- 11,682 View
- 135 Download
- 11 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Immunohistochemical demonstration of CD20 in diffuse large B-cell lymphoma (DLBCL) is prerequisite not only for the diagnosis but also for assigning patients to rituximab-containing chemotherapy. However, little is known about the impact of abundance of CD20 expression assessed by immunohistochemistry on the clinical outcome of DLBCL. We performed a semi-quantitative immunohistochemical analysis of CD20 expression in DLBCL to examine the prognostic implication of the level of CD20 expression. Methods: Pre-treatment diagnostic tissue samples from 48 DLBCL patients who were treated with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) regimen were represented in a tissue microarray and immunostained for CD20. The relative abundance of CD20 expression was semi-quantitatively scored using a web-based ImmunoMembrane plug-in. Receiver operating characteristic curve analysis was used to determine a prognostically relevant cut-off score in order to dichotomize the patients into CD20-high versus CD20-low groups. Results: The levels of CD20 expression were heterogeneous among the patients, with a wide and linear distribution of scores. Patients in CD20-low group showed significantly poor clinical outcome. Conclusions: The levels of CD20 expression in DLBCL are heterogeneous among the patients with DLBCL. A subgroup of the patients with CD20 expression levels below the cut-off score showed poor clinical outcome. -
Citations
Citations to this article as recorded by- The Expression Levels of CD20 as a Prognostic Value in Feline B-Cell Nasal Lymphoma: A Pilot Study
Kravee Chaipoca, Theerapol Sirinarumitr, Supreeya Srisampan, Charuwan Wongsali, Attawit Kovitvadhi, Tassanee Jaroensong
Animals.2024; 14(7): 1043. CrossRef - Prognostic molecular biomarkers in diffuse large B-cell lymphoma in the rituximab era and their therapeutic implications
Sotirios G. Papageorgiou, Thomas P. Thomopoulos, Ioannis Katagas, Anthi Bouchla, Vassiliki Pappa
Therapeutic Advances in Hematology.2021;[Epub] CrossRef - Novel tumour–infiltrating lymphocyte-related risk stratification based by flow cytometry for patients with de novo angioimmunoblastic T cell lymphoma
Qiqi Zhu, Xueqin Deng, Wenqing Yao, Zihang Chen, Yunxia Ye, Limin Gao, Wenyan Zhang, Weiping Liu, Sha Zhao
Annals of Hematology.2021; 100(3): 715. CrossRef - Induced CD20 Expression on B-Cell Malignant Cells Heightened the Cytotoxic Activity of Chimeric Antigen Receptor Engineered T Cells
Yingxi Xu, Saisai Li, Ying Wang, Jia Liu, Xinhe Mao, Haiyan Xing, Zheng Tian, Kejing Tang, Xiaolong Liao, Qing Rao, Dongsheng Xiong, Min Wang, Jianxiang Wang
Human Gene Therapy.2019; 30(4): 497. CrossRef - Characterization of head and neck squamous cell carcinoma arising in young patients: Particular focus on molecular alteration and tumor immunity
Hyang Joo Ryu, Eun Kyung Kim, Byoung Chul Cho, Sun Och Yoon
Head & Neck.2019; 41(1): 198. CrossRef - Immunoglobulin D (IgD) and IgD receptor expression in diffuse large B-cell lymphoma
Xing Dai, Yu-Jing Wu, Xiao-Yi Jia, Yan Chang, Hua-Xun Wu, Chun Wang, Wei Wei
Hematology.2019; 24(1): 544. CrossRef - The implications of TrkA and MET aberrations in de novo salivary duct carcinoma
Hyang Joo Ryu, Yoon Woo Koh, Sun Och Yoon
Human Pathology.2018; 81: 18. CrossRef - Prognostic stratification improvement by integrating ID1/ID3/IGJ gene expression signature and immunophenotypic profile in adult patients with B-ALL
Nataly Cruz-Rodriguez, Alba L. Combita, Leonardo J. Enciso, Lauren F. Raney, Paula L. Pinzon, Olga C. Lozano, Alba M. Campos, Niyireth Peñaloza, Julio Solano, Maria V. Herrera, Jovanny Zabaleta, Sandra Quijano
Journal of Experimental & Clinical Cancer Research.2017;[Epub] CrossRef - Implications of infiltrating immune cells within bone marrow of patients with diffuse large B-cell lymphoma
Juhyeon Jeong, Eun Ji Oh, Woo Ick Yang, Soo Jeong Kim, Sun Och Yoon
Human Pathology.2017; 64: 222. CrossRef - Architectural patterns of p16 immunohistochemical expression associated with cancer immunity and prognosis of head and neck squamous cell carcinoma
Hyang Joo Ryu, Eun Kyung Kim, Su Jin Heo, Byoung Chul Cho, Hye Ryun Kim, Sun Och Yoon
APMIS.2017; 125(11): 974. CrossRef - New developments in the pathology of malignant lymphoma. A review of the literature published from January–April 2016
J. Han van Krieken
Journal of Hematopathology.2016; 9(2): 73. CrossRef - Diffuse large B-cell lymphoma: R-CHOP failure—what to do?
Bertrand Coiffier, Clémentine Sarkozy
Hematology.2016; 2016(1): 366. CrossRef
- The Expression Levels of CD20 as a Prognostic Value in Feline B-Cell Nasal Lymphoma: A Pilot Study
- Analysis of Histologic Features Suspecting Anaplastic Lymphoma Kinase (ALK)-Expressing Pulmonary Adenocarcinoma
- In Ho Choi, Dong Won Kim, Sang Yun Ha, Yoon-La Choi, Hee Jeong Lee, Joungho Han
- J Pathol Transl Med. 2015;49(4):310-317. Published online June 22, 2015
- DOI: https://doi.org/10.4132/jptm.2015.05.13
- 12,270 View
- 93 Download
- 20 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Since 2007 when anaplastic lymphoma kinase (ALK) rearrangements were discovered in non-small cell lung cancer, the ALK gene has received attention due to ALK-targeted therapy, and a notable treatment advantage has been observed in patients harboring the EML4/ALK translocation. However, using ALK-fluorescence in situ hybridization (FISH) as the standard method has demerits such as high cost, a time-consuming process, dependency on interpretation skill, and tissue preparation. We analyzed the histologic findings which could complement the limitation of ALK-FISH test for pulmonary adenocarcinoma. Methods: Two hundred five cases of ALK-positive and 101 of ALK-negative pulmonary adenocarcinoma from January 2007 to May 2013 were enrolled in this study. The histologic findings and ALK immunohistochemistry results were reviewed and compared with the results of ALK-FISH and EGFR/KRAS mutation status. Results: Acinar, cribriform, and solid growth patterns, extracellular and intracellular mucin production, and presence of signet-ring-cell element, and psammoma body were significantly more often present in ALK-positive cancer. In addition, the presence of goblet cell-like cells and presence of nuclear inclusion and groove resembling papillary thyroid carcinoma were common in the ALK-positive group. Conclusions: The above histologic parameters can be helpful in predicting ALK rearranged pulmonary adenocarcinoma, leading to rapid FISH analysis and timely treatment. -
Citations
Citations to this article as recorded by- Evidential deep learning-based ALK-expression screening using H&E-stained histopathological images
Sai Chandra Kosaraju, Sai Phani Parsa, Dae Hyun Song, Hyo Jung An, Yoon-La Choi, Joungho Han, Jung Wook Yang, Mingon Kang
npj Digital Medicine.2025;[Epub] CrossRef - Clinicopathological significances of cribriform pattern in lung adenocarcinoma
Jung-Soo Pyo, Byoung-Hoon Lee, Kyueng-Whan Min, Nae Yu Kim
Pathology - Research and Practice.2024; 253: 155035. CrossRef - Clinicopathological features and prognostic significance of pulmonary adenocarcinoma with signet ring cell components: meta-analysis and SEER analysis
Yang Tan, Ying-he Huang, Jia-wen Xue, Rui Zhang, Run Liu, Yan Wang, Zhen-Bo Feng
Clinical and Experimental Medicine.2023; 23(8): 4341. CrossRef - Lung-Cancer Risk in Mice after Exposure to Gamma Rays, Carbon Ions or Neutrons: Egfr Pathway Activation and Frequent Nuclear Abnormality
Kenshi Suzuki, Shunsuke Yamazaki, Ken-ichi Iwata, Yutaka Yamada, Takamitsu Morioka, Kazuhiro Daino, Mutsumi Kaminishi, Mari Ogawa, Yoshiya Shimada, Shizuko Kakinuma
Radiation Research.2022;[Epub] CrossRef - Pathological cytomorphologic features and the percentage of ALK FISH-positive cells predict pulmonary adenocarcinoma prognosis: a prospective cohort study
Fenge Jiang, Congcong Wang, Ping Yang, Ping Sun, Jiannan Liu
World Journal of Surgical Oncology.2021;[Epub] CrossRef - Cribriform pattern in lung invasive adenocarcinoma correlates with poor prognosis in a Chinese cohort
Yang Qu, Haifeng Lin, Chen Zhang, Kun Li, Haiqing Zhang
Pathology - Research and Practice.2019; 215(2): 347. CrossRef - Incidence of brain metastasis in lung adenocarcinoma at initial diagnosis on the basis of stage and genetic alterations
Bumhee Yang, Hyun Lee, Sang-Won Um, Kyunga Kim, Jae Il Zo, Young Mog Shim, O Jung Kwon, Kyung Soo Lee, Myung-Ju Ahn, Hojoong Kim
Lung Cancer.2019; 129: 28. CrossRef - Qualitative and quantitative cytomorphological features of primary anaplastic lymphoma kinase‐positive lung cancer
Ryuko Tsukamoto, Hiroyuki Ohsaki, Sho Hosokawa, Yasunori Tokuhara, Shingo Kamoshida, Toshiko Sakuma, Tomoo Itoh, Chiho Ohbayashi
Cytopathology.2019; 30(3): 295. CrossRef - Double Trouble: A Case Series on Concomitant Genetic Aberrations in NSCLC
Nele Van Der Steen, Yves Mentens, Marc Ramael, Leticia G. Leon, Paul Germonpré, Jose Ferri, David R. Gandara, Elisa Giovannetti, Godefridus J. Peters, Patrick Pauwels, Christian Rolfo
Clinical Lung Cancer.2018; 19(1): 35. CrossRef - Update on the potential significance of psammoma bodies in lung adenocarcinoma from a modern perspective
Akio Miyake, Koji Okudela, Mai Matsumura, Mitsui Hideaki, Hiromasa Arai, Shigeaki Umeda, Shoji Yamanaka, Yoshihiro Ishikawa, Michihiko Tajiri, Kenichi Ohashi
Histopathology.2018; 72(4): 609. CrossRef - Integrin β3 Inhibition Enhances the Antitumor Activity of ALK Inhibitor in ALK-Rearranged NSCLC
Ka-Won Noh, Insuk Sohn, Ji-Young Song, Hyun-Tae Shin, Yu-Jin Kim, Kyungsoo Jung, Minjung Sung, Mingi Kim, Sungbin An, Joungho Han, Se-Hoon Lee, Mi-Sook Lee, Yoon-La Choi
Clinical Cancer Research.2018; 24(17): 4162. CrossRef - An anaplastic lymphoma kinase-positive lung cancer microlesion: A case report
Tetsuo Kon, Youichiro Baba, Ichiro Fukai, Gen Watanabe, Tomoko Uchiyama, Tetsuya Murata
Human Pathology: Case Reports.2017; 7: 11. CrossRef - The prevalence of ALK rearrangement in pulmonary adenocarcinomas in an unselected Caucasian population from a defined catchment area: impact of smoking
Birgit G Skov, Paul Clementsen, Klaus R Larsen, Jens B Sørensen, Anders Mellemgaard
Histopathology.2017; 70(6): 889. CrossRef - Ciliated muconodular papillary tumor of the lung harboring ALK gene rearrangement: Case report and review of the literature
Yan Jin, Xuxia Shen, Lei Shen, Yihua Sun, Haiquan Chen, Yuan Li
Pathology International.2017; 67(3): 171. CrossRef - Molecular breakdown: a comprehensive view of anaplastic lymphoma kinase (ALK)‐rearranged non‐small cell lung cancer
Ka‐Won Noh, Mi‐Sook Lee, Seung Eun Lee, Ji‐Young Song, Hyun‐Tae Shin, Yu Jin Kim, Doo Yi Oh, Kyungsoo Jung, Minjung Sung, Mingi Kim, Sungbin An, Joungho Han, Young Mog Shim, Jae Ill Zo, Jhingook Kim, Woong‐Yang Park, Se‐Hoon Lee, Yoon‐La Choi
The Journal of Pathology.2017; 243(3): 307. CrossRef - Anaplastic lymphoma kinase immunohistochemistry in lung adenocarcinomas: Evaluation of performance of standard manual method using D5F3 antibody
D Jain, K Jangra, PS Malik, S Arulselvi, K Madan, S Mathur, MC Sharma
Indian Journal of Cancer.2017; 54(1): 209. CrossRef - Clinicopathological Features and Therapeutic Responses of Chinese Patients with Advanced Lung Adenocarcinoma Harboring an Anaplastic Lymphoma Kinase Rearrangement
Danxia Lin, De Zeng, Chen Chen, Xiao Wu, Miaojun Wang, Jiongyu Chen, Hui Lin, Xihui Qiu
Oncology Research and Treatment.2017; 40(1-2): 27. CrossRef - A Validation Study for the Use of ROS1 Immunohistochemical Staining in Screening for ROS1 Translocations in Lung Cancer
Patrizia Viola, Manisha Maurya, James Croud, Jana Gazdova, Nadia Suleman, Eric Lim, Tom Newsom-Davis, Nick Plowman, Alexandra Rice, M. Angeles Montero, David Gonzalez de Castro, Sanjay Popat, Andrew G. Nicholson
Journal of Thoracic Oncology.2016; 11(7): 1029. CrossRef - Non-small Cell Lung Cancer with Concomitant EGFR, KRAS, and ALK Mutation: Clinicopathologic Features of 12 Cases
Taebum Lee, Boram Lee, Yoon-La Choi, Joungho Han, Myung-Ju Ahn, Sang-Won Um
Journal of Pathology and Translational Medicine.2016; 50(3): 197. CrossRef - ALK gene rearranged lung adenocarcinomas: molecular genetics and morphology in cohort of patients from North India
Amanjit Bal, Navneet Singh, Parimal Agarwal, Ashim Das, Digambar Behera
APMIS.2016; 124(10): 832. CrossRef
- Evidential deep learning-based ALK-expression screening using H&E-stained histopathological images
- Accuracy of Core Needle Biopsy Versus Fine Needle Aspiration Cytology for Diagnosing Salivary Gland Tumors
- In Hye Song, Joon Seon Song, Chang Ohk Sung, Jong-Lyel Roh, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim, Jeong Hyun Lee, Jung Hwan Baek, Kyung-Ja Cho
- J Pathol Transl Med. 2015;49(2):136-143. Published online March 12, 2015
- DOI: https://doi.org/10.4132/jptm.2015.01.03
- 17,616 View
- 238 Download
- 79 Web of Science
- 82 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Core needle biopsy is a relatively new technique used to diagnose salivary gland lesions, and its role in comparison with fine needle aspiration cytology needs to be refined. Methods: We compared the results of 228 ultrasound-guided core needle biopsy and 371 fine needle aspiration procedures performed on major salivary gland tumors with their postoperative histological diagnoses. Results: Core needle biopsy resulted in significantly higher sensitivity and more accurate tumor subtyping, especially for malignant tumors, than fine needle aspiration. No patient developed major complications after core needle biopsy. Conclusions: We recommend ultrasoundguided core needle biopsy as the primary diagnostic tool for the preoperative evaluation of patients with salivary gland lesions, especially when malignancy is suspected. -
Citations
Citations to this article as recorded by- Fine-needle aspiration or core needle biopsy? A meta-analysis of diagnostic accuracy and procedural outcomes in salivary gland tumors
Kenan Kassem, Alaa Safia, Uday Abd Elhadi, Shlomo Merchavy
European Journal of Radiology.2026; 194: 112532. CrossRef - Controversial issues in core needle biopsy for diagnosing parotid neoplasms
N. V. Vishneva, P. A. Demenchuk, O. Yu. Petropavlovskaya, E. I. Selifanova, A. N. Lanina, N. V. Kalakutsky, A. I. Yaremenko
Parodontologiya.2026; 30(4): 407. CrossRef - Frozen Section Analysis in Submandibular Gland Tumors: Optimizing Intraoperative Decision-Making
Amir Bolooki, Felix Johnson, Anna Stenzl, Zhaojun Zhu, Benedikt Gabriel Hofauer
Cancers.2025; 17(5): 895. CrossRef - The Myriad Spectrum of Salivary Gland Lesions: Cytohistological Correlation on Fine Needle Aspiration Cytology, Core Needle Biopsy, and Resections in a 5‐Year Single Institutional Experience of North India
Zachariah Chowdhury, Pallavi Majumdar, Sumeet Narain, Komal Lamba
Diagnostic Cytopathology.2025; 53(8): 391. CrossRef - Salivary Duct Carcinoma: A 12-Year Single Center Experience
Hyowon Ahn, Dongbin Ahn, Ji Hye Kwak
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2025; 68(6): 232. CrossRef - Cytological Spectrum of Salivary Gland Lesions Using the Milan System and their Histopathological Correlation: Retrospective Study in a Peripheral Medical College of Eastern India
Ujjwal Bandyopadhyay, Sarmila Guha Banerjee, Sirshak Dutta
Indian Journal of Otolaryngology and Head & Neck Surgery.2025; 77(11): 4887. CrossRef - Parotid Secretory Carcinoma: A Distinct Entity from Acinic Cell Carcinoma
Muhammad Adzha Musa, Muhamad Arif Ahmad Radzi, Moharzudi Mohamed, Ikram Hakim
Indian Journal of Otolaryngology and Head & Neck Surgery.2025;[Epub] CrossRef - Diagnostic performance of ultrasound guided salivary gland core needle biopsy and fine needle aspiration in children
Vicente Oliveira, Anthea Lafrenière, Nikolaus Wolter, Joao Amaral, Alessandro Gasparetto, Dimitri Parra Rojas
Pediatric Radiology.2025; 56(2): 393. CrossRef - Giant Pleomorphic Adenoma of Submandibular Gland
Harendra Kumar, Qazi Saquib Rizwan, Mayank Gupta, Tarun Kumar
Indian Journal of Otolaryngology and Head & Neck Surgery.2024; 76(1): 1361. CrossRef - CT-guided core needle biopsies of head and neck tumors: a comprehensive monocenter analysis of safety and outcomes
Thomas Joseph Vogl, Heinrich Johannes Ketelsen, Scherwin Mahmoudi, Jan-Erik Scholtz, Vitali Koch, Leon David Grünewald, Peter Wild, Timo Stoever, Simon Bernatz
European Radiology.2024; 34(8): 5370. CrossRef - Indications for Submandibulectomy Within a 20-Year Period
Amir Bolooki, Anna Stenzl, Christopher Weusthof, Benedikt Hofauer
Ear, Nose & Throat Journal.2024;[Epub] CrossRef - Treatment of Warthin’s Tumors of the Parotid Gland With Radiofrequency Ablation: A Systematic Review of the Current Literature
Kenny Do, Eric Kawana, Sisi Tian, Jo-Lawrence Bigcas
Ear, Nose & Throat Journal.2024;[Epub] CrossRef - Evaluation of the anterior processes of the parotid gland: an ultrasonographic study
Tarık Ali Uğur, Hümeyra Tercanlı
Surgical and Radiologic Anatomy.2024; 46(6): 915. CrossRef - Salivary Gland Fine-Needle Aspiration
Federica Policardo, Antonino Mule’, Esther Diana Rossi
Surgical Pathology Clinics.2024; 17(3): 347. CrossRef - Implementation of the Milan System for Reporting Salivary Gland Cytology: A Two-Year Outcome Cytopathology Data of a Tertiary Care Center
Soudamini Mahapatra, Chinmaya Sundar Ray, Aparajita Mishra, Dileswari Pradhan
Cureus.2024;[Epub] CrossRef - Preoperative cytopathological investigatory aids in the diagnosis of salivary gland lesions
S Vidyalakshmi, K Shanmugasamy
Journal of Oral and Maxillofacial Pathology.2024; 28(2): 172. CrossRef - Machine Learning on Ultrasound Texture Analysis Data for Characterizing of Salivary Glandular Tumors: A Feasibility Study
Li-Jen Liao, Ping-Chia Cheng, Feng-Tsan Chan
Diagnostics.2024; 14(16): 1761. CrossRef - Association of Membranous Basal Cell Adenoma and Basal Cell Adenocarcinoma With Brooke-Spiegler Syndrome
Lexi Goehring, Debby Rampisela, Jordan L Pleitz
Cureus.2024;[Epub] CrossRef - A Retrospective 8‐Year Single Institutional Study in Germany Regarding Diagnosis, Treatment, and Outcome of Malignant Parotid Tumors
S. Andrianopoulou, L. S. Fiedler, B. M. Lippert, O. C. Bulut, Mohamed Rahouma
International Journal of Surgical Oncology.2024;[Epub] CrossRef - High Field MRI in Parotid Gland Tumors: A Diagnostic Algorithm
Chiara Gaudino, Andrea Cassoni, Martina Lucia Pisciotti, Resi Pucci, Chiara Veneroso, Cira Rosaria Tiziana Di Gioia, Francesca De Felice, Patrizia Pantano, Valentino Valentini
Cancers.2024; 17(1): 71. CrossRef - Nationwide Incidence Trends of Pediatric Parotid Malignancy in Korea and a Retrospective Analysis of Single-Institution Surgical Experience of Parotidectomy
Hyun Seong Kim, Seo Young Kim, Eun-Jae Chung, Seong Keun Kwon, Soon-Hyun Ahn, Yuh-Seog Jung, Jungirl Seok
Korean Society of Head and Neck Oncology.2024; 40(2): 7. CrossRef - The Usefulness of Ultrasound-Guided Core Needle Biopsy Compared to Fine Needle Aspiration in Pre-Operative Diagnosis of Cystic-Predominant Parotid Tumors
Youn Jin Cho, Young Rok Jo, Hyun Jun Hong, Hye Ran Lee
Korean Journal of Otorhinolaryngology-Head and Neck Surgery.2023; 66(8): 532. CrossRef - The Value of Ultrasound-guided Core Needle Biopsy in Differentiating Benign from Malignant Salivary Gland Lesions
Mohammad Ali Kazemi, Farzaneh Amini, Bita Kargar, Maryam Lotfi, Keyvan Aghazadeh, Hashem Sharifian, Behnaz Moradi, Javid Azadbakht
Indian Journal of Otolaryngology and Head & Neck Surgery.2023; 75(2): 266. CrossRef - Schnellschnittdiagnostik bei Tumoren des Trigonum submandibulare
S. Riemann, A. Knopf
HNO.2023; 71(3): 164. CrossRef - Myoepithelial Carcinoma Ex Pleomorphic Adenoma of the Submandibular Gland: A Case Report
Georgia Syrnioti, Antonia Syrnioti, Alharith Abdullah, Xuehui Lui, Ernesto Mendoza
Cureus.2023;[Epub] CrossRef - Intraductal Carcinoma: The Carcinoma In Situ of the Salivary Gland
Rhema Thomas, Tijjani Umar, Farzad Borumandi
Journal of Craniofacial Surgery.2023; 34(5): e432. CrossRef - Fine-Needle Aspiration Cytology for Parotid Tumors
Masataka Taniuchi, Tetsuya Terada, Ryo Kawata
Life.2022; 12(11): 1897. CrossRef - Utility of the Milan System for Reporting Salivary Gland Cytology, with focus on the incidence and histologic correlates of atypia of undetermined significance (AUS) and salivary gland neoplasm of uncertain malignant potential (SUMP): A 3‐year institution
Christopher M. Cormier, Shweta Agarwal
Cancer Cytopathology.2022; 130(4): 303. CrossRef - Percutaneous CT-Guided Core Needle Biopsies of Head and Neck Masses: Review of 184 Cases at a Single Academic Institution, Common and Special Techniques, Diagnostic Yield, and Safety
R.W. Jordan, D.P. Shlapak, J.C. Benson, F.E. Diehn, D.K. Kim, V.T. Lehman, G.B. Liebo, A.A. Madhavan, J.M. Morris, P.P. Morris, J.T. Verdoorn, C.M. Carr
American Journal of Neuroradiology.2022; 43(1): 117. CrossRef - Nodular fasciitis of the submandibular gland
Ting Suen Wong, Richard Wei Chern Gan, Laszlo Karsai, Bun Yin Winson Wong
BMJ Case Reports.2022; 15(4): e245584. CrossRef - Validation of the Milan system for reporting salivary gland cytopathology: a single institution’s 10-year experience
Christopher Felicelli, Joseph Reznicek, Yevgen Chornenkyy, Lucy Jager, Daniel Johnson
Journal of the American Society of Cytopathology.2022; 11(5): 264. CrossRef - Application of the Milan system for reporting salivary gland cytopathology using cell blocks
Grégoire B. Morand, Raihanah Alsayegh, Alex M. Mlynarek, Marianne Plourde, Tiffany Mach, Marco A. Mascarella, Michael P. Hier, Livia Florianova, Marc P. Pusztaszeri
Virchows Archiv.2022; 481(4): 575. CrossRef - Comparisons among the Ultrasonography Prediction Model, Real-Time and Shear Wave Elastography in the Evaluation of Major Salivary Gland Tumors
Ping-Chia Cheng, Wu-Chia Lo, Chih-Ming Chang, Ming-Hsun Wen, Po-Wen Cheng, Li-Jen Liao
Diagnostics.2022; 12(10): 2488. CrossRef - A Novel Sonographic Scoring Model in the Prediction of Major Salivary Gland Tumors
Wu‐Chia Lo, Chih‐Ming Chang, Chi‐Te Wang, Po‐Wen Cheng, Li‐Jen Liao
The Laryngoscope.2021;[Epub] CrossRef - Assessing the diagnostic accuracy for pleomorphic adenoma and Warthin tumor by employing the Milan System for Reporting Salivary Gland Cytopathology: An international, multi‐institutional study
Derek B. Allison, Alexander P. Smith, Daniel An, James Adam Miller, Khurram Shafique, Sharon Song, Kartik Viswanathan, Elizabeth Eykman, Rema A. Rao, Austin Wiles, Güliz A. Barkan, Ritu Nayar, Guido Fadda, Celeste N. Powers, Esther Diana Rossi, Momin T. S
Cancer Cytopathology.2021; 129(1): 43. CrossRef - Magnetic resonance imaging of salivary gland tumours: Key findings for imaging characterisation
Davide Maraghelli, Michele Pietragalla, Cesare Cordopatri, Cosimo Nardi, Anna Julie Peired, Giandomenico Maggiore, Stefano Colagrande
European Journal of Radiology.2021; 139: 109716. CrossRef - The Milan System, from Its Introduction to Its Current Adoption in the Diagnosis of Salivary Gland Cytology
Esther Diana Rossi
Journal of Molecular Pathology.2021; 2(2): 114. CrossRef - Utility of the Milan system for reporting salivary gland cytopathology during rapid on‐site evaluation (ROSE) of salivary gland aspirates
Aanchal Kakkar, Mukin Kumar, Priyadarsani Subramanian, Arshad Zubair, Rajeev Kumar, Alok Thakar, Deepali Jain, Sandeep R. Mathur, Venkateswaran K. Iyer
Cytopathology.2021; 32(6): 779. CrossRef - Contribution of small tissue biopsy and flow cytometry to preoperative cytological categorization of salivary gland fine needle aspirates according to the Milan System: Single center experience on 287 cases
Tolga Bağlan, Serpil Dizbay Sak, Cevriye Cansız Ersöz, Koray Ceyhan
Diagnostic Cytopathology.2021; 49(4): 509. CrossRef - Is Milan for kids?: The Milan System for Reporting Salivary Gland Cytology in pediatric patients at an academic children's hospital with cytologic‐histologic correlation
Swati P. Satturwar, Maren Y. Fuller, Sara E. Monaco
Cancer Cytopathology.2021; 129(11): 884. CrossRef - Radiographic Interpretation in Oral Medicine and Hospital Dental Practice
Katherine France, Anwar A.A.Y. AlMuzaini, Mel Mupparapu
Dental Clinics of North America.2021; 65(3): 509. CrossRef - Carcinoma ex pleomorphic adenoma of major salivary glands: CT and MR imaging findings
Can Wang, Qiang Yu, Siyi Li, Jingjing Sun, Ling Zhu, Pingzhong Wang
Dentomaxillofacial Radiology.2021; 50(7): 20200485. CrossRef - Salivary gland carcinoma in children and adolescents: The EXPeRT/PARTNER diagnosis and treatment recommendations
Aurore Surun, Dominik T. Schneider, Andrea Ferrari, Teresa Stachowicz‐Stencel, Jelena Rascon, Anna Synakiewicz, Abbas Agaimy, Kata Martinova, Denis Kachanov, Jelena Roganovic, Ewa Bien, Gianni Bisogno, Ines B. Brecht, Frédéric Kolb, Juliette Thariat, Anto
Pediatric Blood & Cancer.2021;[Epub] CrossRef - A Call for Universal Acceptance of the Milan System for Reporting Salivary Gland Cytopathology
Eric Barbarite, Sidharth V. Puram, Adeeb Derakhshan, Esther D. Rossi, William C. Faquin, Mark A. Varvares
The Laryngoscope.2020; 130(1): 80. CrossRef - Preoperative biopsy in parotid malignancies: Variation in use and impact on surgical margins
Liliya Benchetrit, Sina J. Torabi, Elliot Morse, Saral Mehra, Rahmatullah Rahmati, Heather A. Osborn, Benjamin L. Judson
The Laryngoscope.2020; 130(6): 1450. CrossRef - α‐Synuclein Real‐Time Quaking‐Induced Conversion in the Submandibular Glands of Parkinson's Disease Patients
Sireesha Manne, Naveen Kondru, Huajun Jin, Vellareddy Anantharam, Xuemei Huang, Arthi Kanthasamy, Anumantha G. Kanthasamy
Movement Disorders.2020; 35(2): 268. CrossRef - The Accessory Parotid Gland and its Clinical Significance
Mateusz A. Rosa, Dominik P. Łazarz, Jakub R. Pękala, Bendik Skinningsrud, Sigurd S. Lauritzen, Bernard Solewski, Przemysław A. Pękala, Jerzy A. Walocha, Krzysztof A. Tomaszewski
Journal of Craniofacial Surgery.2020; 31(3): 856. CrossRef - Comparison of core needle biopsy and fine‐needle aspiration in diagnosis of ma lignant salivary gland neoplasm: Systematic review and meta‐analysis
Jungheum Cho, Junghoon Kim, Ji Sung Lee, Choong Guen Chee, Youngjune Kim, Sang Il Choi
Head & Neck.2020; 42(10): 3041. CrossRef - The Milan system for reporting salivary gland cytopathology: The clinical impact so far. Considerations from theory to practice
Esther Diana Rossi, William C. Faquin
Cytopathology.2020; 31(3): 181. CrossRef - The role of core needle biopsy in parotid glands lesions with inconclusive fine needle aspiration
Farrokh Heidari, Firouzeh Heidari, Benyamin Rahmaty, Neda Jafari, Kayvan Aghazadeh, Saeed Sohrabpour, Ebrahim Karimi
American Journal of Otolaryngology.2020; 41(6): 102718. CrossRef - Role of Fine Needle Aspiration Cytology in the Diagnosis of Parotid Gland Tumors: Analysis of 193 Cases
Rahim Dhanani, Haissan Iftikhar, Muhammad Sohail Awan, Nida Zahid, Sehrish Nizar Ali Momin
International Archives of Otorhinolaryngology.2020; 24(04): e508. CrossRef - Cytohistological correlation of salivary gland tumours with emphasis on Milan system for reporting: A novel step towards internal quality assurance
Anandraj Vaithy.K, ATM Venkat Raghava, E S Keerthika Sri, K R Umadevi
IP Archives of Cytology and Histopathology Research.2020; 5(4): 283. CrossRef - Diagnosing Recently Defined and Uncommon Salivary Gland Lesions in Limited Cellularity Specimens: Cytomorphology and Ancillary Studies
Esther Diana Rossi, Zubair Baloch, William Faquin, Liron Pantanowitz
AJSP: Reviews and Reports.2020; 25(5): 210. CrossRef - Peripheral T Cell Lymphoma of Parotid Gland: A Diagnostic Challenge
J. G. Aishwarya, Satish Nair, C. N. Patil, Swarna Shivakumar, N. Shrivalli, Ashish Shah
Indian Journal of Otolaryngology and Head & Neck Surgery.2019; 71(S1): 533. CrossRef - Potential utility of core needle biopsy in the diagnosis of IgG4-related dacryoadenitis and sialadenitis
Kenichi Takano, Tsuyoshi Okuni, Keisuke Yamamoto, Ryuta Kamekura, Ryoto Yajima, Motohisa Yamamoto, Hiroki Takahashi, Tetsuo Himi
Modern Rheumatology.2019; 29(2): 393. CrossRef - Retrospective assessment of the effectiveness of the Milan system for reporting salivary gland cytology: A systematic review and meta‐analysis of published literature
Sahar J Farahani, Zubair Baloch
Diagnostic Cytopathology.2019; 47(2): 67. CrossRef - Values of fine‐needle aspiration cytology of parotid gland tumors: A review of 996 cases at a single institution
Manabu Suzuki, Ryo Kawata, Masaaki Higashino, Shuji Nishikawa, Tetsuya Terada, Shin‐Ichi Haginomori, Yoshitaka Kurisu, Yoshinobu Hirose
Head & Neck.2019; 41(2): 358. CrossRef - Positive Surgical Margins in Submandibular Malignancies: Facility and Practice Variation
Liliya Benchetrit, Elliot Morse, Benjamin L. Judson, Saral Mehra
Otolaryngology–Head and Neck Surgery.2019; 161(4): 620. CrossRef - The growth rate and the positive prediction of needle biopsy of clinically diagnosed Warthin’s tumor
Jungirl Seok, Woo-Jin Jeong, Soon-Hyun Ahn, Young Ho Jung
European Archives of Oto-Rhino-Laryngology.2019; 276(7): 2091. CrossRef - The Difference in the Clinical Features Between Carcinoma ex Pleomorphic Adenoma and Pleomorphic Adenoma
Jungirl Seok, Se Jin Hyun, Woo-Jin Jeong, Soon-Hyun Ahn, Hyojin Kim, Young Ho Jung
Ear, Nose & Throat Journal.2019; 98(8): 504. CrossRef - Fine‐needle aspiration cytology and radiological imaging in parotid gland tumours: Our experience in 103 patients
Clare Perkins, Edward Toll, Philip Reece
Clinical Otolaryngology.2019; 44(6): 1124. CrossRef - Application of the Milan system of reporting salivary cytopathology – A retrospective cytohistological correlation study
Ramya Katta, Devi Padmavathi Chaganti
Journal of Dr. NTR University of Health Sciences.2019; 8(1): 11. CrossRef - Ultrasound‐guided core needle biopsy in salivary glands: A meta‐analysis
Hee Joon Kim, Jong Seung Kim
The Laryngoscope.2018; 128(1): 118. CrossRef - Accuracy and effectiveness of ultrasound-guided core-needle biopsy in the diagnosis of focal lesions in the salivary glands
Jose Luis del Cura, Gloria Coronado, Rosa Zabala, Igone Korta, Ignacio López
European Radiology.2018; 28(7): 2934. CrossRef - The Milan System for Reporting Salivary Gland Cytopathology (MSRSGC): an ASC-IAC–sponsored system for reporting salivary gland fine-needle aspiration
Esther Diana Rossi, Zubair Baloch, Marc Pusztaszeri, William C. Faquin
Journal of the American Society of Cytopathology.2018; 7(3): 111. CrossRef - Routine and Advanced Ultrasound of Major Salivary Glands
Kunwar Suryaveer Singh Bhatia, Yuk-Ling Dai
Neuroimaging Clinics of North America.2018; 28(2): 273. CrossRef - The Milan System for Reporting Salivary Gland Cytopathology (MSRSGC): An ASC-IAC-Sponsored System for Reporting Salivary Gland Fine-Needle Aspiration
Esther Diana Rossi, Zubair W. Baloch, Marc Pusztaszeri, William C. Faquin
Acta Cytologica.2018; 62(3): 157. CrossRef - Evaluation and diagnosis of salivary gland neoplasms
Erica Jackson Mayland, Anna M. Pou
Operative Techniques in Otolaryngology-Head and Neck Surgery.2018; 29(3): 129. CrossRef - Feasibility and Safety of Multicenter Tissue and Biofluid Sampling for α-Synuclein in Parkinson’s Disease: The Systemic Synuclein Sampling Study (S4)
Lana M. Chahine, Thomas G. Beach, Nicholas Seedorff, Chelsea Caspell-Garcia, Christopher S. Coffey, Michael Brumm, Charles H. Adler, Geidy E. Serrano, Carly Linder, Sherri Mosovsky, Tatiana Foroud, Holly Riss, Dixie Ecklund, John Seibyl, Danna Jennings, V
Journal of Parkinson’s Disease.2018; 8(4): 517. CrossRef - Preoperative diagnostic of parotid gland neoplasms: fine-needle aspiration cytology or core needle biopsy?
Peter Zbären, Asterios Triantafyllou, Kenneth O. Devaney, Vincent Vander Poorten, Henrik Hellquist, Alessandra Rinaldo, Alfio Ferlito
European Archives of Oto-Rhino-Laryngology.2018; 275(11): 2609. CrossRef - A comparison study of the reporting systems for salivary gland fine needle aspirations: Are they really different?
Diana Montezuma, Sule Canberk, Ozlem Aydın, Mehmet Polat Dermirhas, André F. Vieira, Süha Goksel, Ümit İnce, Fernando Schmitt
Diagnostic Cytopathology.2018; 46(10): 859. CrossRef - Pediatric salivary gland carcinomas: Diagnostic and therapeutic management
Céleste Rebours, Vincent Couloigner, Louise Galmiche, Odile Casiraghi, Cécile Badoual, Sabah Boudjemaa, Anthony Chauvin, Monique Elmaleh, Brice Fresneau, Sylvie Fasola, Erea‐Noël Garabédian, Thierry Van Den Abeele, Daniel Orbach
The Laryngoscope.2017; 127(1): 140. CrossRef - Agreement between rapid on‐site evaluation and the final cytological diagnosis of salivary gland specimens
S. Wangsiricharoen, S. Lekawanvijit, S. Rangdaeng
Cytopathology.2017; 28(4): 321. CrossRef - Mesenchymal neoplasms of the head and neck: a cytopathologic analysis on fine needle aspiration
James Lee, Samia Kazmi, Christopher J. VandenBussche, Syed Z. Ali
Journal of the American Society of Cytopathology.2017; 6(3): 105. CrossRef - Clinical Results of Surgical Treatment in Parotid Tumors
Ahmet Kara
Journal of Otolaryngology-ENT Research.2017;[Epub] CrossRef - Parotid gland metastases of distant primary tumours: A diagnostic challenge
Achim M. Franzen, Thomas Günzel, Anja Lieder
Auris Nasus Larynx.2016; 43(2): 187. CrossRef - Modern Radiology in the Management of Head and Neck Cancer
G.J.C. Burkill, R.M. Evans, V.V. Raman, S.E.J. Connor
Clinical Oncology.2016; 28(7): 440. CrossRef - Fine‐needle aspiration and core needle biopsy: An update on 2 common minimally invasive tissue sampling modalities
Paul A. VanderLaan
Cancer Cytopathology.2016; 124(12): 862. CrossRef - Staging and follow-up of high-grade malignant salivary gland tumours: The role of traditional versus functional imaging approaches – A review
Nicole Freling, Flavio Crippa, Roberto Maroldi
Oral Oncology.2016; 60: 157. CrossRef - Biopsy of parotid masses: Review of current techniques
Sananda Haldar, Joseph D Sinnott, Kemal M Tekeli, Samuel S Turner, David C Howlett
World Journal of Radiology.2016; 8(5): 501. CrossRef - Review on the applications of ultrasonography in dentomaxillofacial region
Şehrazat Evirgen
World Journal of Radiology.2016; 8(1): 50. CrossRef - Comprehensive Cytomorphologic Analysis of Pulmonary Adenoid Cystic Carcinoma: Comparison to Small Cell Carcinoma and Non-pulmonary Adenoid Cystic Carcinoma
Seokhwi Kim, Jinah Chu, Hojoong Kim, Joungho Han
Journal of Pathology and Translational Medicine.2015; 49(6): 511. CrossRef
- Fine-needle aspiration or core needle biopsy? A meta-analysis of diagnostic accuracy and procedural outcomes in salivary gland tumors
- Diffuse Large B-Cell Lymphoma Arising in Warthin's Tumor: Case Study and Review of the Literature
- Güliz Özkök, Funda Taşlı, Nazan Özsan, Rafet Öztürk, Hakan Postacı
- Korean J Pathol. 2013;47(6):579-582. Published online December 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.6.579
- 8,878 View
- 55 Download
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Warthin's tumor is the second most common type of salivary gland tumor. Microscopically, Warthin's tumor displays a proliferative epithelial component and lymphoid stroma. Carcinomas arising from the epithelial component are well known, but malignant transformations of the lymphoid stroma are rare. When they do occur, they are most commonly B-cell type non-Hodgkin lymphomas. A 60-year-old male patient underwent surgical resection of a parotid mass. After superficial parotidectomy, microscopic examination indicated that the tumor was of epithelial components with basaloid and oncocytic columns of cells neighboring lymphoid components. In addition to the lymphoid follicles with distinct germinal centers, there were large, bizarre and extremely atypical neoplastic cells seen in the lymphoid component. Large neoplastic cells were diffusely CD20 and CD30 positive. The patient was diagnosed with "Warthin's tumor and diffuse large B-cell lymphoma with expression of CD30." The histopathologic and clinical features are discussed along with a review of the literature.
-
Citations
Citations to this article as recorded by- From the archives of MD Anderson Cancer Center: Small lymphocytic lymphoma/chronic lymphocytic leukemia diagnosed in Warthin tumor
Jing Zhou, L. Jeffrey Medeiros
Annals of Diagnostic Pathology.2025; 79: 152533. CrossRef - Warthin’s Tumor Involved by Monoclonal B-Cell Lymphocytosis: A Case Report
Alexie Kindy, Ziang Wang, Robin Gautam, Robert Bennett, Zijian Wang
Cureus.2025;[Epub] CrossRef - Warthin tumor concomitant with mantle cell lymphoma: a case report and review of literature
Hai-Chao Tong, Shuang Ma, Lan Chen, Xiangyun Meng, Ying-Chun Li, Le-Yao Li, Lingyun Dong, Wan-Lin Zhang, Tyler Wildes, Lian-He Yang, Endi Wang
Diagnostic Pathology.2024;[Epub] CrossRef - A Rare Diagnosis of Parotid Gland Follicular Lymphoma Arising in Warthin Tumor: Case Report and Literature Review
Ido Vaknin, Irit Allon, Shirley Zafrir-Haver, Alex Abramson
Medicina.2024; 60(12): 2086. CrossRef - Warthin’s Tumor of the Parotid Gland With Degeneration to Diffuse Large B-cell Lymphoma: A Case Report and Review of Literature
Mauricio Gutierrez-Alvarez, Cynthia Martinez, Ana Priscila Campollo Lopez, Kevin Fuentes, Jorge Alberto Robles Aviña
Cureus.2023;[Epub] CrossRef - Pathogenesis Analysis of Salivary Gland Tumors Through the Expression of Programmed Death-Ligand 1 (PD-L1)
Aisyah Izzatul Muna, Maria Evata Krismawati Surya, Meiske Margaretha, Jane Kosasih, Mei Syafriadi
Indian Journal of Otolaryngology and Head & Neck Surgery.2023; 75(4): 3098. CrossRef - Role of cytotoxic T-lymphocyte antigen 4 (CTLA-4) expression in the pathogenesis of Warthin’s tumor growth
Alvionika Nadyah Qotrunnada, Tecky Indriana, Jane Kosasih, Meiske Margaretha, Mei Syafriadi
Dental Journal (Majalah Kedokteran Gigi).2022; 55(4): 194. CrossRef - Lymphoepithelial Carcinoma of Salivary Glands
Lester D.R. Thompson, Rumeal D. Whaley
Surgical Pathology Clinics.2021; 14(1): 75. CrossRef - Follicular Lymphoma Diagnosed in Warthin Tumor: A Case Report and Review of the Literature
Fnu Alnoor, Jatin S. Gandhi, Matthew K. Stein, Joel F. Gradowski
Head and Neck Pathology.2020; 14(2): 386. CrossRef - Prevalence of Lymphoid Neoplasia in a Retrospective Analysis of Warthin Tumor: A Single Institution Experience
F. N. U. Alnoor, Jatin S. Gandhi, Matthew K. Stein, Jorge Solares, Joel F. Gradowski
Head and Neck Pathology.2020; 14(4): 944. CrossRef - A Case of Diffuse Large B Cell Lymphoma in Submandibular Gland
Sang Hoo Park, Min Gyoung Pak, Dong Kun Lee
Journal of Clinical Otolaryngology Head and Neck Surgery.2020; 31(1): 111. CrossRef - Analysis of the Clinical Relevance of Histological Classification of Benign Epithelial Salivary Gland Tumours
Henrik Hellquist, António Paiva-Correia, Vincent Vander Poorten, Miquel Quer, Juan C. Hernandez-Prera, Simon Andreasen, Peter Zbären, Alena Skalova, Alessandra Rinaldo, Alfio Ferlito
Advances in Therapy.2019; 36(8): 1950. CrossRef - Diffuse large B-cell lymphoma arising from follicular lymphoma with warthin’s tumor of the parotid gland - immunophenotypic and genetic features: A case report
Chang-Song Wang, Xia Chu, Di Yang, Lei Ren, Nian-Long Meng, Xue-Xia Lv, Tian Yun, Yan-Sha Cao
World Journal of Clinical Cases.2019; 7(22): 3895. CrossRef - Presentation of Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma in a Warthin Tumor: Case Report and Literature Review
Hadeel Jawad, Peter McCarthy, Gerard O’Leary, Cynthia C. Heffron
International Journal of Surgical Pathology.2018; 26(3): 256. CrossRef - Bilateral Warthin tumor in psoriatic patients in therapy with multiple immunosuppressive therapy
M Burlando, E Cozzani, C Chinazzo, M larosa, M Boggio, A Parodi
International Journal of Immunopathology and Pharmacology.2015; 28(1): 138. CrossRef - Nodular Lymphocyte-Predominant Hodgkin Lymphoma in a Warthin Tumor of the Parotid Gland
Arianna Di Napoli, Giuseppe Mallel, Armando Bartolazzi, Elena Cavalieri, Roberto Becelli, Claudia Cippitelli, Luigi Ruco
International Journal of Surgical Pathology.2015; 23(5): 419. CrossRef
- From the archives of MD Anderson Cancer Center: Small lymphocytic lymphoma/chronic lymphocytic leukemia diagnosed in Warthin tumor
- Morphologic Analysis of Pulmonary Neuroendocrine Tumors
- Seung Seok Lee, Myunghee Kang, Seung Yeon Ha, Jungsuk An, Mee Sook Roh, Chang Won Ha, Jungho Han
- Korean J Pathol. 2013;47(1):16-20. Published online February 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.1.16
- 7,915 View
- 52 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Few studies on how to diagnose pulmonary neuroendocrine tumors through morphometric analysis have been reported. In this study, we measured and analyzed the characteristic parameters of pulmonary neuroendocrine tumors using an image analyzer to aid in diagnosis.
Methods Sixteen cases of typical carcinoid tumor, 5 cases of atypical carcinoid tumor, 15 cases of small cell carcinoma, and 51 cases of large cell neuroendocrine carcinoma were analyzed. Using an image analyzer, we measured the nuclear area, perimeter, and the major and minor axes.
Results The mean nuclear area was 0.318±0.101 µm2 in typical carcinoid tumors, 0.326±0.119 µm2 in atypical carcinoid tumors, 0.314±0.107 µm2 in small cell carcinomas, and 0.446±0.145 µm2 in large cell neuroendocrine carcinomas. The mean nuclear circumference was 2.268±0.600 µm in typical carcinoid tumors, 2.408±0.680 µm in atypical carcinoid tumors, 2.158±0.438 µm in small cell carcinomas, and 3.247±1.276 µm in large cell neuroendocrine carcinomas. All parameters were useful in distinguishing large cell neuroendocrine carcinoma from other tumors (p=0.001) and in particular, nuclear circumference was the most effective (p=0.001).
Conclusions Pulmonary neuroendocrine tumors showed nuclear morphology differences by subtype. Therefore, evaluation of quantitative nuclear parameters improves the accuracy and reliability of diagnosis.
-
Citations
Citations to this article as recorded by- Clinical Significance of Persistent Tumor in Bone Marrow during Treatment of High-risk Neuroblastoma
Young Bae Choi, Go Eun Bae, Na Hee Lee, Jung-Sun Kim, Soo Hyun Lee, Keon Hee Yoo, Ki Woong Sung, Hong Hoe Koo
Journal of Korean Medical Science.2015; 30(8): 1062. CrossRef - Morphologic Alteration of Metastatic Neuroblastic Tumor in Bone Marrow after Chemotherapy
Go Eun Bae, Yeon-Lim Suh, Ki Woong Sung, Jung-Sun Kim
Korean Journal of Pathology.2013; 47(5): 433. CrossRef
- Clinical Significance of Persistent Tumor in Bone Marrow during Treatment of High-risk Neuroblastoma
- Interobserver Variability in Diagnosing High-Grade Neuroendocrine Carcinoma of the Lung and Comparing It with the Morphometric Analysis
- Seung Yeon Ha, Joungho Han, Wan-Seop Kim, Byung Seong Suh, Mee Sook Roh
- Korean J Pathol. 2012;46(1):42-47. Published online February 23, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.1.42
- 9,654 View
- 48 Download
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Distinguishing small cell lung carcinoma (SCLC) and large cell neuroendocrine carcinoma (LCNEC) of the lung is difficult with little information about interobserver variability.
Methods One hundred twenty-nine cases of resected SCLC and LCNEC were independently evaluated by four pathologists and classified according to the 2004 World Health Organization criteria. Agreement was regarded as "unanimous" if all four pathologists agreed on the classification. The kappa statistic was calculated to measure the degree of agreement between pathologists. We also measured cell size using image analysis, and receiver-operating-characteristic curve analysis was performed to evaluate cell size in predicting the diagnosis of high-grade neuroendocrine (NE) carcinomas in 66 cases.
Results Unanimous agreement was achieved in 55.0% of 129 cases. The kappa values ranged from 0.35 to 0.81. Morphometric analysis reaffirmed that there was a continuous spectrum of cell size from SCLC to LCNEC and showed that tumors with cells falling in the middle size range were difficult to categorize and lacked unanimous agreement.
Conclusions Our results provide an objective explanation for considerable interobserver variability in the diagnosis of high-grade pulmonary NE carcinomas. Further studies would need to define more stringent and objective definitions of cytologic and architectural characteristics to reliably distinguish between SCLC and LCNEC.
-
Citations
Citations to this article as recorded by- Case report: A patient with EGFR L861Q positive adenosquamous lung carcinoma transforming into large cell neuroendocrine cancer after treatment with Almonertinib
Kele Cheng, Yong Zhu, Ran Sang, Zhongsheng Kuang, Yang Cao
Frontiers in Oncology.2025;[Epub] CrossRef - Deep Learning–Based Retinoblastoma Protein Subtyping of Pulmonary Large-Cell Neuroendocrine Carcinoma on Small Hematoxylin and Eosin–Stained Specimens
Teodora E. Trandafir, Frank W.J. Heijboer, Farhan Akram, Jules L. Derks, Yunlei Li, Lisa M. Hillen, Ernst-Jan M. Speel, Zsolt Megyesfalvi, Balazs Dome, Andrew P. Stubbs, Anne-Marie C. Dingemans, Jan H. von der Thüsen
Laboratory Investigation.2025; 105(9): 104192. CrossRef - Treatment outcomes in patients with stage IV large cell neuroendocrine carcinoma: a nationwide registry study
Frank W.J. Heijboer, Jules L. Derks, Francien H. van Nederveen, Lisa M. Hillen, Michael A. den Bakker, Teodora Radonic, Ronald A.M. Damhuis, Ernst-Jan M. Speel, Jan H. von der Thüsen, Anne-Marie C. Dingemans
Lung Cancer.2025; 210: 108830. CrossRef - Updates on lung neuroendocrine neoplasm classification
Giulia Vocino Trucco, Luisella Righi, Marco Volante, Mauro Papotti
Histopathology.2024; 84(1): 67. CrossRef - Recent advancement of HDAC inhibitors against breast cancer
Syed Abdulla Mehmood, Kantrol Kumar Sahu, Sounok Sengupta, Sangh Partap, Rajshekhar Karpoormath, Brajesh Kumar, Deepak Kumar
Medical Oncology.2023;[Epub] CrossRef - Genomic Feature of a Rare Case of Mix Small-Cell and Large-Cell Neuroendocrine Lung Carcinoma: A Case Report
Youcai Zhu, Feng Zhang, Dong Yu, Fang Wang, Manxiang Yin, Liangye Chen, Chun Xiao, Yueyan Huang, Feng Ding
Frontiers in Oncology.2022;[Epub] CrossRef - Small-Cell Carcinoma of the Lung: What We Learned about It?
Luisella Righi, Marco Volante, Mauro Papotti
Acta Cytologica.2022; 66(4): 257. CrossRef - Hierarchical identification of a transcriptional panel for the histological diagnosis of lung neuroendocrine tumors
Juxuan Zhang, Jiaxing Deng, Xiao Feng, Yilong Tan, Xin Li, Yixin Liu, Mengyue Li, Haitao Qi, Lefan Tang, Qingwei Meng, Haidan Yan, Lishuang Qi
Frontiers in Genetics.2022;[Epub] CrossRef - Immunohistochemical Staining With Neuroendocrine Markers is Essential in the Diagnosis of Neuroendocrine Neoplasms of the Esophagogastric Junction
Dea N.M. Jepsen, Anne-Marie K. Fiehn, Rajendra S. Garbyal, Ulla Engel, Jakob Holm, Birgitte Federspiel
Applied Immunohistochemistry & Molecular Morphology.2021; 29(6): 454. CrossRef - Improving differential diagnosis of pulmonary large cell neuroendocrine carcinoma and small cell lung cancer via a transcriptomic, biological pathway-based machine learning model
Junhong Guo, Likun Hou, Wei Zhang, Zhengwei Dong, Lei Zhang, Chunyan Wu
Translational Oncology.2021; 14(12): 101222. CrossRef - Are Neuroendocrine Negative Small Cell Lung Cancer and Large Cell Neuroendocrine Carcinoma with WT RB1 two Faces of the Same Entity?
Dmitriy Sonkin, Anish Thomas, Beverly A Teicher
Lung Cancer Management.2019;[Epub] CrossRef - Ki-67 labeling index of neuroendocrine tumors of the lung has a high level of correspondence between biopsy samples and surgical specimens when strict counting guidelines are applied
Alessandra Fabbri, Mara Cossa, Angelica Sonzogni, Mauro Papotti, Luisella Righi, Gaia Gatti, Patrick Maisonneuve, Barbara Valeri, Ugo Pastorino, Giuseppe Pelosi
Virchows Archiv.2017; 470(2): 153. CrossRef - The Use of Immunohistochemistry Improves the Diagnosis of Small Cell Lung Cancer and Its Differential Diagnosis. An International Reproducibility Study in a Demanding Set of Cases
Erik Thunnissen, Alain C. Borczuk, Douglas B. Flieder, Birgit Witte, Mary Beth Beasley, Jin-Haeng Chung, Sanja Dacic, Sylvie Lantuejoul, Prudence A. Russell, Michael den Bakker, Johan Botling, Elisabeth Brambilla, Erienne de Cuba, Kim R. Geisinger, Kenzo
Journal of Thoracic Oncology.2017; 12(2): 334. CrossRef - Reply to Letter “The Use of Immunohistochemistry Improves the Diagnosis of Small Cell Lung Cancer and Its Differential Diagnosis. An International Reproducibility Study in a Demanding Set of Cases.”
Erik Thunnissen, Birgit I. Witte, Masayuki Noguchi, Yasushi Yatabe
Journal of Thoracic Oncology.2017; 12(6): e70. CrossRef - What clinicians are asking pathologists when dealing with lung neuroendocrine neoplasms?
Giuseppe Pelosi, Alessandra Fabbri, Mara Cossa, Angelica Sonzogni, Barbara Valeri, Luisella Righi, Mauro Papotti
Seminars in Diagnostic Pathology.2015; 32(6): 469. CrossRef - Unraveling Tumor Grading and Genomic Landscape in Lung Neuroendocrine Tumors
Giuseppe Pelosi, Mauro Papotti, Guido Rindi, Aldo Scarpa
Endocrine Pathology.2014; 25(2): 151. CrossRef - Grading the neuroendocrine tumors of the lung: an evidence-based proposal
G Rindi, C Klersy, F Inzani, G Fellegara, L Ampollini, A Ardizzoni, N Campanini, P Carbognani, T M De Pas, D Galetta, P L Granone, L Righi, M Rusca, L Spaggiari, M Tiseo, G Viale, M Volante, M Papotti, G Pelosi
Endocrine-Related Cancer.2014; 21(1): 1. CrossRef - Controversial issues and new discoveries in lung neuroendocrine tumors
Giuseppe Pelosi, Kenzo Hiroshima, Mari Mino-Kenudson
Diagnostic Histopathology.2014; 20(10): 392. CrossRef - BAI3, CDX2 and VIL1: a panel of three antibodies to distinguish small cell from large cell neuroendocrine lung carcinomas
Muhammad F Bari, Helen Brown, Andrew G Nicholson, Keith M Kerr, John R Gosney, William A Wallace, Irshad Soomro, Salli Muller, Danielle Peat, Jonathan D Moore, Lesley A Ward, Maxim B Freidin, Eric Lim, Manu Vatish, David R J Snead
Histopathology.2014; 64(4): 547. CrossRef - Neuroendocrine tumours—challenges in the diagnosis and classification of pulmonary neuroendocrine tumours
M A den Bakker, F B J M Thunnissen
Journal of Clinical Pathology.2013; 66(10): 862. CrossRef - Morphologic Analysis of Pulmonary Neuroendocrine Tumors
Seung Seok Lee, Myunghee Kang, Seung Yeon Ha, Jungsuk An, Mee Sook Roh, Chang Won Ha, Jungho Han
Korean Journal of Pathology.2013; 47(1): 16. CrossRef - Altered expression of microRNA miR‐21, miR‐155, and let‐7a and their roles in pulmonary neuroendocrine tumors
Hyoun Wook Lee, Eun Hee Lee, Seung Yeon Ha, Chang Hun Lee, Hee Kyung Chang, Sunhee Chang, Kun Young Kwon, Il Seon Hwang, Mee Sook Roh, Jeong Wook Seo
Pathology International.2012; 62(9): 583. CrossRef
- Case report: A patient with EGFR L861Q positive adenosquamous lung carcinoma transforming into large cell neuroendocrine cancer after treatment with Almonertinib
- CD44s and CD44v6 Are Predominantly Expressed in the Non-germinal Center B-Cell-like Type of Diffuse Large B-Cell Lymphomas.
- Kyueng Whan Min, Young Ha Oh, Chan Kum Park, So Dug Lim, Wan Seop Kim
- Korean J Pathol. 2011;45(6):589-595.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.6.589
- 4,171 View
- 29 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
CD44 protein is known as a homing cellular adhesion molecule that is linked to diverse cellular functions such as adhesion, migration and invasion, which are all important in cancer progression and metastasis. The expression of CD44 standard and variant isoforms (CD44 standard isoform [CD44s] and CD44 splice variants containing exon v6 [CD44v6], respectively) is associated with an unfavorable clinical outcome in various neoplasms.
METHODS
Forty patients who were diagnosed with diffuse large B-cell lymphoma (DLBCL) through biopsy at Hanyang University Hospital between 1996 and 2003 were included in this study. CD44 proteins expression was analyzed by immunohistochemical staining on a tissue microarray and the correlation of CD44 with the types of DLBCL and clinical parameters, including the factors defined by the International Prognostic Index, was evaluated.
RESULTS
A high CD44s and intermediate to strong CD44v6 expression, including cytoplasmic membranous staining patterns, was present in 35% (14/40) and 25% (10/40) of DLBCL patients, respectively. High CD44s expression was correlated significantly with non-germinal center B-cell-like types (non-GCB, p=0.004) and patients with old age (p=0.041).
CONCLUSIONS
High CD44s expression may be significantly associated with the non-GCB type compared to the GCB type and may be essential to the prediction of disease outcome in tumor stage III in DLBCL patients.
- Prognostic Implication of Programmed Death-1-Positive Tumor-infiltrating Lymphocytes in Diffuse Large B-Cell Lymphoma.
- Young Sin Ko, Young Ha Oh, Chan Kum Park, Wook Youn Kim, Hye Seung Han, So Dug Lim, Tae Sook Hwang, Wan Seop Kim
- Korean J Pathol. 2011;45(6):573-581.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.6.573
- 4,509 View
- 42 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Programmed death-1 (PD-1) is physiologically expressed by germinal center-associated helper T-cells and has an inhibitory effect on T-cell activity.
METHODS
We examined 63 cases of diffuse large B-cell lymphoma (DLBCL) and determined the number of PD-1-positive helper T-cells in a representative tumor area after immunohistochemical staining using a monoclonal antibody against PD-1. The PD-1-positive cells were counted in 3 high-power fields (HPFs; 400x).
RESULTS
Patients were divided into 2 groups: one with a high number of PD-1-positive cells (>20/HPF, n=33) and one with a low number of PD-1-positive cells (< or =20/HPF, n=30). The former group showed decreased overall survival, but at a statistically non-significant level (p=0.073). A high number of PD-1-positive cells was more common in patients at an advanced clinical stage and with high international prognostic index score (p=0.025 and p=0.026, respectively). The number of extranodal sites also somewhat correlated with the PD-1 staining status (p=0.071). However, the number of PD-1-positive cells was not associated with patient age, serum lactate dehydrogenase level, and Eastern Cooperative Oncology Group performance score.
CONCLUSIONS
The high number of PD-1-positive cells might be associated with an unfavorable outcome in DLBCL patients. -
Citations
Citations to this article as recorded by- Mechanisms of PD-1/PD-L1 expression and prognostic relevance in non-Hodgkin lymphoma: a summary of immunohistochemical studies
Pauline Gravelle, Barbara Burroni, Sarah Péricart, Cédric Rossi, Christine Bezombes, Marie Tosolini, Diane Damotte, Pierre Brousset, Jean-Jacques Fournié, Camille Laurent
Oncotarget.2017; 8(27): 44960. CrossRef - Expression of programmed cell death ligand 1 (PD-L1) in advanced stage EBV-associated extranodal NK/T cell lymphoma is associated with better prognosis
Wook Youn Kim, Ho Young Jung, Soo Jeong Nam, Tae Min Kim, Dae Seog Heo, Chul-Woo Kim, Yoon Kyung Jeon
Virchows Archiv.2016; 469(5): 581. CrossRef
- Mechanisms of PD-1/PD-L1 expression and prognostic relevance in non-Hodgkin lymphoma: a summary of immunohistochemical studies
- Childhood Asymmetry Labium Majus Enlargement.
- Mi Jin Gu, Sang Yoon Kim
- Korean J Pathol. 2011;45(5):529-531.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.5.529
- 5,696 View
- 72 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Childhood asymmetry labium majus enlargement (CALME) is a disctinctive clinicopathologic entity of pre- and early puberty first described in 2005. It is defined as an expansion of normal soft tissues of the vulva. Although CALME is not a rare lesion, it has been called lipoma, fibroma, hamartoma, and fibrous hyperplasia. CALME is not a true neoplasm and is a physiologic growth in response to hormone. It may tend to resolve spontaneously and recur after surgical resection. We report four cases of CALME with a review of the literature. To the best of the knowledge, this is the first Korean report.
-
Citations
Citations to this article as recorded by- Keep CALME (childhood asymmetry labium majus enlargement) and follow up
Andrea Sechi, Annalisa Patrizi, Giulio Vara, Rita Golfieri, Iria Neri
JDDG: Journal der Deutschen Dermatologischen Gesellschaft.2021; 19(9): 1276. CrossRef - Bei CALME (childhood asymmetry labium majus enlargement): die Ruhe bewahren und nachverfolgen
Andrea Sechi, Annalisa Patrizi, Giulio Vara, Rita Golfieri, Iria Neri
JDDG: Journal der Deutschen Dermatologischen Gesellschaft.2021; 19(9): 1276. CrossRef - Childhood Asymmetry Labium Majus Enlargement (CALME): Description of Two Cases
Cristina Salvatori, Ilaria Testa, Marco Prestipino, Maria Elena Laurenti, Sara Riccioni, Giuseppe Di Cara, Nicola Principi, Susanna Esposito, Mirko Bertozzi
International Journal of Environmental Research and Public Health.2018; 15(7): 1525. CrossRef - Childhood asymmetrical labium majus enlargement sonographic and MR imaging appearances
Ami Gokli, Jeremy Neuman, Ruby Lukse, June Koshy, Fanyi Kong, Tal Laor
Pediatric Radiology.2016; 46(5): 674. CrossRef
- Keep CALME (childhood asymmetry labium majus enlargement) and follow up
- Ovarian Large Cell Neuroendocrine Carcinoma Associated with Endocervical-like Mucinous Borderline Tumor: A Case Report and Literature Review.
- Jun Mo Kim, Hyeong Chan Shin, Mi Jin Kim
- Korean J Pathol. 2011;45(5):523-528.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.5.523
- 5,100 View
- 34 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Ovarian large cell neuroendocrine carcinoma is a rare tumor that is usually associated with surface epithelial tumors. Mucinous tumors are most common surface epithelial component identified in reported cases. Ovarian mucinous tumor associated with large cell neuroendocrine carcinoma is almost always an intestinal type. However, large cell neuroendocrine carcinoma associated with pure mucinous borderline tumor of endocervical-like type has not been described previously. The present case report describes a large cell neuroendocrine carcinoma associated with endocervical-like mucinous borderline tumor of the ovary in a 35-year-old woman. The tumor was confirmed by histopathology and immunohistochemistry. A review of the pertinent literature is included.
-
Citations
Citations to this article as recorded by- The puzzle of gynecologic neuroendocrine carcinomas: State of the art and future directions
Giuseppe Caruso, Carolina Maria Sassu, Federica Tomao, Violante Di Donato, Giorgia Perniola, Margherita Fischetti, Pierluigi Benedetti Panici, Innocenza Palaia
Critical Reviews in Oncology/Hematology.2021; 162: 103344. CrossRef - Pathological features, clinical presentations and prognostic factors of ovarian large cell neuroendocrine carcinoma: a case report and review of published literature
Xiaohang Yang, Junyu Chen, Ruiying Dong
Journal of Ovarian Research.2019;[Epub] CrossRef - Primary pure large cell neuroendocrine carcinoma of the ovary
Chen-Hsien Lin, Yu-Chieh Lin, Mu-Hsien Yu, Her-Young Su
Taiwanese Journal of Obstetrics and Gynecology.2014; 53(3): 413. CrossRef - Pure Large Cell Neuroendocrine Carcinoma of Ovary: A Rare Clinical Entity and Review of Literature
P. N. Shakuntala, K. Uma Devi, K. Shobha, U. D. Bafna, M. Geetashree
Case Reports in Oncological Medicine.2012; 2012: 1. CrossRef
- The puzzle of gynecologic neuroendocrine carcinomas: State of the art and future directions
- Diffuse Large B-Cell Lymphoma Associated with Chronic Inflammation Manifested as a Soft Tissue Mass: Incidental Discovery on Histological Examination.
- Sang Yun Ha, Yoon La Choi, Sung Joo Kim, Young Hye Ko
- Korean J Pathol. 2011;45(4):417-422.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.4.417
- 5,385 View
- 39 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - We report an extraordinary case of diffuse large B-cell lymphoma arising in a cystic necrotic mass in a 35-year-old man who presented with a soft tissue mass at the site of previous surgery. A benign mass was surgically removed 17 years ago, after which a cystic lesion gradually developed at the same site. The resected mass appeared as a thick-walled cyst filled with brown necrotic and hemorrhagic material. On microscopic examination, the cyst wall was primarily necrotic tissue with some aggregates of large atypical lymphoid cells. These atypical cells were diffusely positive for CD20 and showed a high proliferation index, Epstein-Barr virus positivity, and clonal rearrangement of the immunoglobulin gene. His present condition was diagnosed as Epstein-Barr virus-associated diffuse large B-cell lymphoma arising from chronic inflammation. It is important to be aware of the clinical manifestations and histological features of this rare disease in light of diagnosis and treatment.
-
Citations
Citations to this article as recorded by- EBV-negative Fibrin-Associated Large B-Cell Lymphoma Arising in Thyroid Hyperplastic Nodule: Report of a Case and Literature Review
Tin Wai Ho, Wah Cheuk, John K.C. Chan
International Journal of Surgical Pathology.2023; 31(7): 1420. CrossRef - Diffuse Large B Cell Lymphoma in a Prosthetic Aortic Graft
David Bell, David Marshman
Heart, Lung and Circulation.2017; 26(2): e4. CrossRef - Fibrin-associated EBV-positive Large B-Cell Lymphoma
Daniel F. Boyer, Penelope A. McKelvie, Laurence de Leval, Kerstin L. Edlefsen, Young-Hyeh Ko, Zachary A. Aberman, Alexandra E. Kovach, Aneal Masih, Ha T. Nishino, Lawrence M. Weiss, Alan K. Meeker, Valentina Nardi, Maryknoll Palisoc, Lina Shao, Stefania P
American Journal of Surgical Pathology.2017; 41(3): 299. CrossRef - Malignant Lymphoma Mimicking an Infection After Shoulder Surgery
Jabari Ian Justin Martin, Jasmine Bauknight, Vincent Desiderio, Bahman Sadr
Journal of the American Academy of Orthopaedic Surgeons.2017; 25(4): 314. CrossRef - Current Concepts in Primary Effusion Lymphoma and Other Effusion-Based Lymphomas
Yoonjung Kim, Chan Jeong Park, Jin Roh, Jooryung Huh
Korean Journal of Pathology.2014; 48(2): 81. CrossRef
- EBV-negative Fibrin-Associated Large B-Cell Lymphoma Arising in Thyroid Hyperplastic Nodule: Report of a Case and Literature Review
- Association of CD57+ Natural Killer Cells with Better Overall Survival in DLBCL Patients.
- Jeong Hyeon Lee, Yoon Jin Kwak, Chul Hwan Kim, Insun Kim
- Korean J Pathol. 2011;45(4):361-370.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.4.361
- 3,673 View
- 27 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Malignant tumor cells may evoke the innate and adaptive immune systems. Various immune cells are involved in this immune reaction, and tumor infiltrating lymphocytes, macrophages, natural killer (NK) cells are associated with patient prognosis for solid tumors.
METHODS
Seventy-eight patients who were diagnosed with diffuse large B cell lymphoma (DLBCL) between 2001 and 2009 were selected. CD57+ NK cells, CD68+ tumor associated macrophages (TAMs), and CD4+ and CD8+ T cells were evaluated in tissue sections using immunohistochemical staining and compared with clinical parameters including age, gender, performance status, clinical stage, serum lactic dehydrogenase level, number of extranodal sites, international prognostic index score, chemotherapy response, and survival.
RESULTS
Patients with high numbers of CD57+ NK cells had a significantly higher overall survival rate than patients with low numbers of CD57+ NK cells. However, no significant difference was observed between the number of CD57+ NK cells and other prognostic parameters. The number of CD68+ TAMs and CD4+ or CD8+ T cells was not significantly correlated with prognostic factors in patients with DLBCL.
CONCLUSIONS
An evaluation of tumor infiltrating CD57+ NK cells is recommended as a prognostic indicator in patients with DLBCL. -
Citations
Citations to this article as recorded by- The prognostic value of tumor-associated macrophages detected by immunostaining in diffuse large B cell lymphoma: A meta-analysis
Mei Lin, Shupei Ma, Lingling Sun, Zhiqiang Qin
Frontiers in Oncology.2023;[Epub] CrossRef
- The prognostic value of tumor-associated macrophages detected by immunostaining in diffuse large B cell lymphoma: A meta-analysis
- Distinction of Pulmonary Large Cell Neuroendocrine Carcinoma from Small Cell Lung Carcinoma Using a Panel of Bcl-2, p63, and 34betaE12.
- Jun Zhe Li, Chan Choi, Yoo Duk Choi, Kook Joo Na
- Korean J Pathol. 2011;45(2):170-174.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.2.170
- 3,931 View
- 33 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Making the distinction between large cell neuroendocrine carcinoma (LCNEC) and small cell lung carcinoma (SCLC) is difficult in some samples of biopsy tissues, but we have to separate LCNEC from SCLC because the two types of cancer may need different therapy and they have different prognostic implications. Thus far, there are no specific immunohistochemical markers that allow distinguishing these two kinds of tumors.
METHODS
We performed an immunohistochemical analysis to study the expressions of p63, Bcl-2, and 34betaE12 and to investigate whether these 3 molecules have correlations in LCNEC and SCLC. We also evaluated the expression of the neuroendocrine markers chromogranin, synaptophysin and CD56.
RESULTS
A statistical analysis was performed for p63, Bcl-2, and 34betaE12 in separate and combined panels. According to the combinations of p63, Bcl-2, and 34betaE12, there were frequent expressions of p63-/Bcl-2+ or Bcl-2+/34betaE12- in the SCLC, and there was a superior proportion of them in the SCLC rather than that in the LCNEC. The p63-/Bcl-2+ and Bcl-2+/34betaE12- antibody combinations showed higher specificities compared to any single antibody for diagnosing SCLC.
CONCLUSIONS
Bcl-2 and selective p63 or 34betaE12 made up a most useful panel of markers for making the differential diagnosis of LCNEC and SCLC. -
Citations
Citations to this article as recorded by- Evaluation of Serum LDH, p53 and BCL2 in Lung Cancer Patients
Pawar Komal, Rajvik Kruti, Vora Hemangini
Gujarat Cancer Society Research Journal.2020; 22(2): 22. CrossRef
- Evaluation of Serum LDH, p53 and BCL2 in Lung Cancer Patients
- Newly Formed Hepatic Masses in Children with Biliary Atresia after Kasai Hepatic Portoenterostomy.
- Hye Jong Song, Yeon Lim Suh
- Korean J Pathol. 2011;45(2):160-169.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.2.160
- 4,811 View
- 30 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
This report describes the clinicopathologic findings of six hepatic masses that developed after Kasai hepatic portoenterostomy (HPE) in six patients with longstanding biliary atresia (BA).
METHODS
Hepatic masses were found in six of 55 pediatric patients who underwent liver transplantation for BA after Kasai HPE from 1997 to 2009. Clinicopathologic analysis was performed and immunohistochemical staining was carried out for CD34, smooth muscle actin (SMA) and cytokeratin 7.
RESULTS
Of the six hepatic masses, two were diagnosed as focal nodular hyperplasia (FNH)-like lesions, two were large regenerative nodules (LRN), one was a mesenchymal hamartoma (MH) and one was a cholangiocarcinoma. The immunohistochemical staining findings for SMA and CD34 were more prominent for the FNH-like nodules than for the cirrhotic background liver. Dysplastic biliary epithelium arising from intestinal metaplasia was found in the cholangiocarcinoma.
CONCLUSIONS
Our findings suggest that FNH-like lesions, LRNs and MH are the results of vascular hemodynamic changes after Kasai HPE and that cholangiocarcinoma is due to recurrent cholangitis after BA. All the lesions in this series must be included in the differential diagnosis of a newly formed hepatic mass in patients after portoenterostomy. -
Citations
Citations to this article as recorded by- Imaging Findings and Management Strategies for Liver Masses in Children with Predisposition Disorders: A Review by the Pediatric LI-RADS Group
Amy B. Kolbe, Michael R. Acord, Geetika Khanna, Cara E. Morin, HaiThuy N. Nguyen, Mitchell A. Rees, Esther Ro, Gary R. Schooler, Judy H. Squires, Ali B. Syed, Elizabeth R. Tang, Alexander J. Towbin, Adina Alazraki
RadioGraphics.2025;[Epub] CrossRef - Features of Nodules in Explants of Children Undergoing Liver Transplantation for Biliary Atresia
Ana M. Calinescu, Anne-Laure Rougemont, Mehrak Anooshiravani, Nathalie M. Rock, Valerie A. McLin, Barbara E. Wildhaber
Journal of Clinical Medicine.2022; 11(6): 1578. CrossRef - Biliary Atresia Patients With Successful Kasai Portoenterostomy Can Present With Features of Obliterative Portal Venopathy
Kalyani R. Patel, Sanjiv Harpavat, Zahida Khan, Sadhna Dhingra, Norma Quintanilla, Mihail Firan, John Goss
Journal of Pediatric Gastroenterology and Nutrition.2020; 71(1): 91. CrossRef
- Imaging Findings and Management Strategies for Liver Masses in Children with Predisposition Disorders: A Review by the Pediatric LI-RADS Group
- The Fine Needle Aspiration Cytology of a Metastatic Pulmonary Adrenocortical Carcinoma Mimicking Primary Large Cell Carcinoma of the Lung.
- Na Rae Kim, Dong Hae Chung, Jae Ik Lee, Seung Yeon Ha
- Korean J Pathol. 2010;44(5):558-563.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.5.558
- 3,321 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Adrenocortical carcinoma is a rare neoplasm and it has an invariably lethal prognosis. We report here on the fine needle aspiration cytologic findings of a solitary metastatic pulmonary adrenocortical carcinoma in a 24-year-old woman. The aspirate smears were very cellular and they were composed of a monomorphic population of large polyhedral cells with abundant granular or vacuolated cytoplasm, and the cells were predominantly singly scattered in a necrotic background. Multinucleated pleomorphic tumor cells were also found. Pleomorphic nuclei with thickened nuclear membranes were impinging on the cell membranes. Mitotic activity was occasionally seen. The cytologic findings of pleomorphic cells with microvacuolated cytoplasm and the presence of vague gland-like sheets, as well as the patient's history of undergoing adrenalectomy for primary adrenocortical carcinoma helped the pathologist reach the diagnosis of metastatic adrenocortical carcinoma. Here, we focus on the cytologic differential points of metastastic pulmonary adrenocortical carcinoma and primary pulmonary carcinoma, especially large cell carcinoma.
- Expression of P-glycoprotein and Apoptosis in Diffuse Large B-cell Lymphoma.
- Ji Eun Kim, Young A Kim, Mee Soo Chang, Yunkyeong Jeon, JinHo Paik, Seon Og Yoon
- Korean J Pathol. 2009;43(4):317-320.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.4.317
- 3,905 View
- 74 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Diffuse large B-cell lymphoma (DLBCL) is the most common type of malignant lymphoma which responds well to conventional chemotherapy. However, quite a few patients have a recurrence with more aggressive forms after completion of therapy. Multidrug resistance proteins (MRP) are related to this process in several ways such as cell cycle alteration and modulation of apoptosis. METHODS: We investigated the expression of P-glycoprotein (Gp), one of the well-known MRP, as well as apoptosis associated proteins in DLBCL. Immunohistochemical staining for Gp, p53, Bcl-2, Ki-67, active caspase 3 and FADD was done in forty DLBCL cases. The association between MRP and apoptosis associated proteins to clinical findings was also tested. RESULTS: Twenty-nine patients out of 40 (73%) with DLBCL were positive for Gp, and 26 cases (65%) had a strong positive for Gp. Gp expression was stronger in high-grade lesions than in low-grade lesions and was associated to Bcl-2 expression. However, we could not find an adverse impact of Gp expression on patients' overall survival or relapse free survival rate. CONCLUSIONS: Our study revealed a high frequency of expression for Gp in DLBCL with a possible relationship between the expressions of Gp to apoptosis associated proteins.
- Large Cell Neuroendocrine Carcinoma of the Lung 2 cases including one presented as an ovarian mass.
- Yun Jung Kim, Jung Weon Shim, Hye Kyung Ahn, Young Euy Park
- Korean J Pathol. 1997;31(3):257-262.
- 2,181 View
- 12 Download
-
 Abstract
Abstract
 PDF
PDF - Pulmonary tumors exhibiting neuroendocrine differentiation are classified as typical carcinoid, atypical carcinoid, and small cell lung carcinoma(SCLC). Travis et al. proposed a fourth category of large cell neuroendocrine carcinoma, which is characterized by light microscopic neuroendocrine appearance, cells of large size, polygonal shape, low nuclear cytoplasmic ratio, coarse nuclear chromatin, with prominent nucleoli high mitotic rate and frequent necrosis; and neuroendocrine features by immunohistochemistry or electron microscopy. High grade neuroendocrine carcinoma (LCAC-NE) revealed aggressive clinical course. We report two cases of neuroendocrine tumors of the lung characterized by a trabecular pattern of large pleomorphic cells with frequent mitoses and wide necrosis. The frequent metastatic sites of atypical carcinoid were liver, bone and brain. One of our case is presented, at first, as an ovarian mass, which shows multifocal rosettes and revealed metastasis from lung. Both cases expressed neuroendocrine differentiation by light microscopy and immunohistochemistry. However clinical neuroendocrine symptom were not present.
- Large Cell Neuroendocrine Carcinoma of the Lung: Report of three cases.
- Jai Hyang Go, Sun Ree Jung, Dong Hwan Shin, Woo Hee Jung
- Korean J Pathol. 1995;29(4):511-516.
- 2,087 View
- 12 Download
-
 Abstract
Abstract
 PDF
PDF - We report three cases of neuroendocrine tumors of the lung characterized by large pleomorphic cell with frequent mitosis, which show neuroendocrine differentiation by both light microscopy or electron microscopy and iminunohistochemistry. These tumors have been categorized as large cell neuroendocrine carcinoma by Travis et al.(1991) in contrast with non-small cell lung cancer with neuroendocrine differentiation. In the latter, neuroendocrine differentiation is not evident by light microscopy and must be demonstrated by imunohistochemstry or by electron microscopy. The prognosis of large cell neuroendocrine carcinoma, together with non-small cell lung cancer with neuroendocrine differentiation, appears to be worse than cancer without neuroendocrine differentiation and intermediate between atypical carcinoid and small cell lung cancer. Larger numbers of patients will be needed to demonstrate significant differences in survival.
- Correlation between Clinical Outcome and Proliferation Index in Diffuse Large B-Cell Lymphoma.
- Sung Shin Park, Joo ryung Huh, Seung Sook Lee, Yun Koo Kang, Dae Seog Heo, Chul Woo Kim
- Korean J Pathol. 1999;33(7):475-482.
- 2,404 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - The diffuse large B-cell lymphoma category of the Revised European American Classification of Lymphoid Neoplasms (REAL) encompasses different morphologic lymphoma subtypes in a single entity, especially the diffuse large cell (DLC) and the immunoblastic (IBL) subtypes by Working Formulation (WF). The aim of this study is to determine the influence of the morphologic subdivision within this category with respect to clinical outcome and proliferative index using Ki-67 immunostainig combined with image analysis. We retrospectively reviewed 74 patients from 1990 to 1996, who were diagnosed with diffuse large B-cell lymphoma. All cases were reclassified according to REAL and Working Formulation (WF), and Ki-67 immunostaining was performed in all the cases. Fifty-eight cases (78.4%) were classified as DLC and 16 cases (21.6%) as IBL, according to WF. Twenty one cases (28.4%) showed nodal involvement and 53 cases (71.6%), extranodal involvement. All cases were found to display a variable degree of nuclear Ki-67 staining. A proliferative index of 50% or higher identified a group of patients (77%) who had poor clinical results. Overall survival was significantly reduced in these patients displaying high Ki-67 associated proliferative index compared to those with a low proliferative index (p=0.007). 5-year survival estimates were 93% in the low proliferative index group and 55% in the high proliferative index group. A multivariate regression analysis incorporating commonly used clinical prognostic factors confirmed the independent effect of proliferation index on survival. Moreover, all of the 16 IBL cases showed Ki-67 positivity of 50% or higher, which correlates with the poor clinical outcome compared to 70.7% of DLC (p=0.014). We conclude that subdivision of the diffuse large B-cell lymphoma category of the REAL classification is necessary in terms of prognostic significance in correlation with Ki-67 proliferative index.
- Clonality of Large Regenerative Nodule Accompanied by Hepatocellular Carcinoma.
- Zhe Piao, Bong Kyun Chun, Woo Jung Lee, Young Nyun Park, Ho guen Kim, Chanil Park
- Korean J Pathol. 1997;31(9):884-890.
- 2,023 View
- 15 Download
-
 Abstract
Abstract
 PDF
PDF - In order to clarify the preneoplastic nature of large regenerative nodules without dysplastic change, we analysed the clonality of hepatocellular carcinomas (HCCs) and large nodules, diameter > or =0.5 cm, of cirrhotic liver by X-linked human androgen receptor (HUMARA) gene assay, using the principle of random X chromosome methylation and inactivation in female. Ten cases of HCC and 5 cases of large nodules without dysplasia from 9 female patients were selected. All the tumors, large nodules and paired normal control cells were selectively microdissected from deparaffinized hematoxylin and eosin stained slides. Genomic DNA was isolated and digested with HhaI. Polymerase chain reaction(PCR) amplication of the HUMARA locus was performed using 32P-a-dCTP containing PCR mixtures. The PCR amplified products were separated by gel electrophoresis and analysed by autoradiography. Nine HCCs from 8 patients were monoclonal and 1 case was polyclonal and the remaining 1 case was not polymorphic at the HUMARA locus. The HCC case which showed polyclonality contained many inflammatory cells. All the large nodules were polyclonal by HUMARA assay. These results suggest that all or most of the cells composing the large regenerative nodules without dysplasia are polyclonal. This assay may be informative for the differentiation between regenerative and preneoplastic nodules in cirrhotic liver and the size of nodule may be not important in hepatocarcinogenesis.
- Large-Cell Acanthoma: A case report.
- Yu Hoon Kim, Seong Jin Cho, Ae ree Kim, Nam Hee Won, Kye Yong Song
- Korean J Pathol. 1996;30(2):161-163.
- 2,373 View
- 43 Download
-
 Abstract
Abstract
 PDF
PDF - Large-cell acanthoma is a generally hyperkeratotic, sharply demarcated patch on sun-exposed skin with the outstanding pathologic feature being composed of large, relatively uniform keratinocytes. We describe a case of large-cell acanthoma that involved the skin of the nasal bridge. Patient was a 56-year-old women with a tannish brown patch, 2 cm in size and of 5 years' duration. Controversial issues about nosologic entity of large cell acanthoma are discussed.
- Galactocele in a Male Child: A case report.
- Yoon Mi Jeen, Yoon Jeong Choi, Dong Wha Lee, Chan Il Park
- Korean J Pathol. 1996;30(2):164-165.
- 2,452 View
- 122 Download
-
 Abstract
Abstract
 PDF
PDF - We investigated a unilocular mammary cyst occurring in a two and a half year old male baby. The cyst was lined by simple columnar epithelium and filled with a milky secretory material. These histologic features were consistent with galactocele. The child had enlarged left breast since birth, but it seemed to be noncontributory as the child had neither endocrine abnormalities nor perinatal disorders. Galactocele is an uncommon breast lesion usually occuring in females following lactation. It is rarely a cause of breast enlargement.
- Uterine Cervical Large Cell Neuroendocrine Carcinoma Concurrent with High Grade Squamous Intraepithelial Neoplasia: A Case Report.
- Yun Kyung Kang, Jae Whoan Koh
- Korean J Pathol. 2008;42(6):389-392.
- 2,198 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - Large cell neuroendocrine carcinoma (LCNEC) of the uterine cervix is a rare and aggressive malignancy. We report a case of uterine cervical LCNEC concurrent with high grade squamous intraepithelial neoplasia (HG-SIN). The LCNEC expressed chromogranin A and thyroid transcription factor 1 (TTF1). The HG-SIN was negative for these markers. Human papillomavirus (HPV) type 18 was positive in LCNEC whereas both type 16 and 18 were positive in HG-SIN by nested polymerase chain reaction. This case showed TTF1 positivity nonetheless diagnosed as a primary uterine cervical LCNEC confirmed by the detection of HPV genome within the tumor. It is critical to recognize LCNEC of the uterine cervix even in the small biopsy specimen because it is a distinctive clinicopathological entity with highly aggressive behavior and unfavorable outcome.
- Immunohistochemical Study for Ki-1 and EMA Antigens in Large Cell Lymphoma including Anaplastic Large Cell Lymphoma.
- Soon Ae Oak, Young Hyeh Ko, Jung Dal Lee
- Korean J Pathol. 1994;28(2):135-143.
- 2,069 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - To evaluate the frequency of EM A and Ki-I antigen expression in the large cell lymphoma and to define the histologic characteristics of Ki-1 positive anaplastic large cell lymphoma, 40 cases of malignant lymphoma, diffuse large cell type were immunostained by Ki-I and EMA monoclonal antibodies. Eight cases of large cell lymphomas expressed EMA, among which 4 cases were positive for Ki-I antibody as well. The positive rate for EMA was much higher in T cell lymphomas than in B cell lymphomas. Among 4 cases of Ki-I positive lymphomas, 2 cases showing membrane staining of Ki-1 with prototypic histologic feature of anaplastic large cell lymphoma were classified as Ki-1 positive anaplastic large cell lymphoma(ALCL). Ki-I positive ALCL were T-cell in one and non-T, non-B cell type in the other, respectively. The remaining 2 cases of Ki-1 positive lymphomas showing cytoplasmic staining were classified as both B-cell centroblastic/centrocytic lymphoma and T-cell pleomorphic large cell lymphoma.
- Immunohistochemical Study of Primary Large Cell Undifferentiated Carcinoma of the Lung.
- Hye Seung Han, Jeong Wook Seo, Eui Keun Ham
- Korean J Pathol. 1996;30(5):417-426.
- 2,213 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - We performed a histopathologic and immunohistochemical study of 23 cases of surgically resected large cell undifferentiated carcinoma(LCUC) of the lung. The relative incidence of LCUC was 7.6% among the total resected cases of primary lung cancer over 7 years(1987-1993). The mean age of the patients was 56 years and 21 cases were male. The mean size of the mass was 5 cm and 11 cases were located peripherally. According to the histologic features, LCUC could be divided into three groups: squamous cell carcinoma-like(6 cases), adenocarcinoma-like(13 cases), and small cell carcinoma-like(4 cases) groups. The histologic differences were related to the variations of the immunohistochemical properties, but there were no differences in prognosis among these groups. Immunoreactivity to cytokeratin(CAM 5.2) was demonstrated in 22/23(96%). Carcinoembryonic antigen was positive in 13/23(57%). Neuron specific enolase and chromogranin were positive in 11/23(48%) and 5/23(22%), respectively. Vimentin was seen in 11/23(48%). From these observations, we could subclassify them by their immunologic phenotypes; exocrine features in 6/23(26%), neuroendocrine(NE) features in 4/23(17%), both exocrine and NE phenotypes in 7/23(30%), and 6 cases(26%) showed neither phenotype. The group with NE features showed a worse prognosis(P<0.05) and immunoreactivity for vimentin was also related to a worse prognosis(P<0.05). These findings imply that the immunohistochemical properties of LCUC are closely related to the histopathologic features. The groups, subdivided by histology and immunoreactivity, showed no prognostic difference except for the NE differentiation and reaction for vimentin.
- Uterine Low Grade Endometrial Stromal Sarcoma Presented as Extrauterine Masses: A Case Report.
- Sun Young Jun, Hongil Ha, In Ae Park, Kyu Rae Kim
- Korean J Pathol. 2002;36(4):262-265.
- 2,394 View
- 37 Download
-
 Abstract
Abstract
 PDF
PDF - Endometrial stromal sarcoma (ESS) is a mesenchymal neoplasm that usually occurs as a primary tumor of the uterine corpus, but rarely arises in other sites, such as the ovary, the pelvic cavity, mesentery, omentum, and serosal or intramural portions of the large intestine. We present a case in which multiple nodules of ESS involving the taenia coli of the ascending colon were accompanied by grossly and radiologically unrecognized small, endometrial stromal lesions (less than 0.5 cm in the greatest dimension) with only focal marginal irregularities in the subsequent hysterectomy specimen. Whether this small sized endometrial stromal tumor is an incidentally associated endometrial stromal nodule (ESN) or a small sized, low grade ESS that was preceded by metastatic lesion is debatable. However, endometrial stromal tumors with tongue-like protrusions and associated fibroblastic stromal reaction around the tumor strongly favored these nodules being the small uterine ESS mimicking ESN. We propose that meticulous search for the detection of uterine ESS is mandatory before making a diagnosis of primary extrauterine ESS even in cases having a grossly or radiologically normal uterus and that the extent of focal irregularities of ESN should be more clearly defined for the correct diagnosis of ESS and ESN.
- Effusion Cytology of Ki - 1 Positive Anaplastic Large Cell Lymphoma: A Case Report.
- Mi Sook Lee, Mi Ja Lee, Yu Kyung Jeong, Sung Chul Lim, Keun Hong Kee, Ho Jong Jeon
- J Pathol Transl Med. 1995;6(2):163-168.
- 2,085 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - Ki-1 positive anaplastic large cell lymphoma is a newly described high-grade lymphoma and is defined by histopathological and immunologic criteria. We experienced a case of systemically involving Ki-1 positive anaplastic large cell lymphoma in a 44 year-old female which initially manifested as pleural effusion. Abdominopelvic CT scan showed the evidence of marked lymphadenopathy in retroperitoneal and both external and inguinal lymph nodes. On cytologic examination of pleural fluid tumor cells revealed pleomorphic large isolated cells with prominent nucleoli and abundant cytoplasms. The nuclei were large with irregular profiles including some deep invaginations. Also. occasional multilobed/multinucleated and binucleated nuclei were seen. Immunohistochemical examination was performed to differentiate from the undifferentiated adenocarcinoma. Hodgkin's disease, non-Hodgkin's lymphoma and malignant histiocytosis. The neoplastic cells were positive for leukocyte common antigen. CD3 CD30(ki-1) but negative for cytokeratin. epithelial membrane antigen. and CD15. A histologic diagnosis of Ki-1 positive anaplastic lymphoma was made by biopsies of the inguinal lymph node, polypoid lesion of the stomach and cecum.
- Cytomorphologic Comparison of Hodgkin Lymphoma and Anaplastic Large cell Lymphoma in Fine Needle Aspiration Cytology.
- Seung Sook Lee, Jae Soo Koh, Sunhoo Park, Min Suk Kim, Soo Youn Cho, Soo Young Chung, Han Suk Ryu, Jung Soon Kim, Hwa Jung Ha, Baek Youl Ryoo
- J Pathol Transl Med. 2006;17(2):126-135.
- 2,964 View
- 63 Download
-
 Abstract
Abstract
 PDF
PDF - To study the differentiating cytomorphological features of Hodgkin lymphoma (HL) and anaplastic large cell lymphoma (ALCL) using fine needle aspiration cytology (FNAC), cytomorphological features of 16 patients with HL (n=8) or ALCL (n=8) were analyzed. In the initial cytological diagnosis prior to biopsy, HLs were properly diagnosed in 4 out of 8 cases (4 HL, 2 atypical, 2 benign), whereas all ALCL were diagnosed as malignancies. However, correct diagnosis of non-Hodgkin lymphoma (NHL) was made in only two ALCL patients (2 NHL, 1 HL, 1 sarcoma, 4 malignancy without specific type). Overall, the percentage of large abnormal cells ranged from 30% to 90% in ALCL except for one case, whereas it was less than 5% in all 8 HL. A spectrum of atypical cells was more characteristic of ALCL. In contrast, HL showed an sharp difference between reactive lymphoid cells and neoplastic ones (bimorphic pattern). Moreover, the emergence of kidney-shaped abnormal cells or wreath-like multinucleated cells was helpful in diagnosing ALCL. The combination of thesefeatures would be useful in differentiating HL and ALCL. Nevertheless, these two types of lymphomas cannot be definitely distinguished based on cytomorphological features alone. Therefore, the aim of FNAC would be to suggest a specific diagnosis and indicate the need for a biopsy.
- Polypoid Ganglioneuromatosis of Colon: A case report.
- Jin Ja Park, Kyung Chan Choi, Young Hee Choi, Young Euy Park
- Korean J Pathol. 1998;32(5):388-390.
- 2,003 View
- 10 Download
-
 Abstract
Abstract
- Gastrointestinal ganglioneuromatosis is an extremely rare lesion which typically occurs with a significant systemic syndrome. It is known to be a major component of multiple endocrine neoplasia, type 2b. We presented a case of polypoid ganglioneuromatosis of the colon in a 3-year-old female with abdominal pain and diarrhea. She had no clinical evidence of the systemic syndrome or von Recklinghausen's neurofibromatosis, conditions in which intestinal ganglioneuromatosis can occur. Gross examination showed diffuse polypoid masses in ascending and transverse colons with normal-appearing mucosa. Microscopic examination revealed a proliferation of spindle-shaped neuronal cells containing multiple clusters of mature ganglion cells in the mucosa, submucosa and proper muscle. We describe a case of colonic ganglioneuromatosis without any component of multiple endocrine neoplasia or family history.
- High-grade Transformation of Primary Nodal Marginal Zone B-Cell Lymphoma: A Case Report.
- Joo Heon Kim, Dong Wook Kang, Mee Ja Park, Jin Man Kim
- Korean J Pathol. 2003;37(4):282-286.
- 2,453 View
- 49 Download
-
 Abstract
Abstract
 PDF
PDF - Primary nodal marginal zone B-cell lymphoma (MZBCL) is recognized as a rare and distinct entity. The rate of histologic transformation into diffuse large B-cell lymphoma (DLBCL) seems lower than the rate of transformation in follicular lymphoma. We herein report a rare case ofnodal MZBCL showing transformation into DLBCL. The patient was a 73-year-old female withcervical lymphadenopathy. On the initial biopsy, the lymph node architecture was diffuselyeffaced with an extensive interfollicular and parafollicular infiltrate of monocytoid B-cells. Therewere scattered large blastic B-cells without formations of compact sheets. The diagnosis ofnodal MZBCL was made. The patient did not receive chemotherapy and was treated with aconservatively supportive regimen. Forty two months later, the patient developed a new cervicallymphadenopathy and a biopsy was performed. Histologically, the lymph node revealeddiffuse sheets of transformed large B-cells showing prominent nucleoli. The diagnosis ofDLBCL transformed from nodal MZBCL was made. The patient was treated with 3 cycles ofcombined CHOP chemotherapy and she showed clinical improvement. These observationssuggest that an untreated primary nodal MZBCL may undergo high-grade transformation.
- Clinicopathological Analysis of Systemic Anaplastic Large Cell Lymphoma.
- Soo Young Chung, Han Suk Ryu, Jae Soo Ko, Baek Youl Ryoo, Seung Sook Lee
- Korean J Pathol. 2006;40(6):399-405.
- 2,161 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Several studies from western countries have reported variable prognoses for patients with systemic anaplastic large cell lymphoma (ALCL) depending strongly on the expression of anaplastic lymphoma kinase (ALK). However, no prognostic significance of ALK expression in Koreans was reported in a single report regarding these patients, although the number of cases was limited in that study.
METHODS
We analyzed the clinicopathological features of ALK+ ALCL and ALK- ALCL in 30 Korean patients diagnosed with primary systemic ALCL.
RESULTS
ALK expression was detected in 60% of all ALCL patients (18/30), and there was no statistical significance to ALK expression in overall survival. Patients with ALK+ ALCL were younger in age and had negative bcl-2 expression; these differences were statistically significant. Tumors positive for ALK protein and granzyme B expression, and negative for bcl-2 expression with a null-cell phenotype tended to have better survival outcomes, althought this trend failed to reach statistical significance (p<0.2), probably due to the limited number of cases in this study.
CONCLUSION
ALK protein expression and the absence of bcl-2 in tumor cells tend to result in better survival despite the failure of this trend to achieve statistical significance. Further studies that examine potential pathologic prognostic factors combined with the expression of ALK and apoptotic factors such as bcl-2 are needed. Additional larger-scale studies are also needed to conclude that ALK expression has no prognostic significance among Koreans.
- Prognostic Significance of P53, BCL-2 and PCNA in Diffuse Large B-Cell Lymphoma: Correlation with International Prognostic Index.
- Dong chul Kim, Gyeongsin Park, Ahwon Lee, Kyo Young Lee, Sang In Shim, Chang Suk Kang
- Korean J Pathol. 2003;37(6):407-412.
- 1,932 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Diffuse large B-cell lymphoma (DLBCL) represents a diverse spectrum of clinical presentation, morphology, and genetic and molecular alterations, and shows variable prognoses and responses to therapy. The International Prognosis Index (IPI) is widely used to predict prognosis but is not precise.
METHODS
Thirty-nine cases of DLBCL were classified into low- and high-risk groups according to IPI and were analyzed for their p53, BCL-2, BCL-6 and PCNA expression profile by immunohistochemical staining and overall survival rate.
RESULTS
The mean age of the 39 patients, 23 males and 16 females, was 52.6 years. There were 23 cases (59.0%) in the low-risk group and 16 (41.0%) in the high-risk group. p53, BCL-2, BCL-6 and PCNA expression was higher in the high-risk group than in the low-risk group, but only the differences in p53 and BCL-2 expression were statistically significant (p < 0.05).
CONCLUSION
The p53 and BCL-2 protein expression in DLBCL may supplement IPI in predicting the prognosis of DLBCL patients.
- Primary Diffuse Large B-cell Lymphoma of the Prostate: A Case Report.
- Dong chul Kim, Gyeongsin Park, Ahwon Lee, Kyungja Han, Chang Suk Kang
- Korean J Pathol. 2003;37(6):432-434.
- 2,250 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Primary lymphomas of the prostate are extremely rare and can mimic other more common prostatic lesions clinically. We report a case of primary diffuse large B-cell lymphoma of the prostate in an 81-year-old man. The patient presented with voiding difficulty as an initial symptom and enlargement of the prostate on rectal digital examination. Transurethral prostatic resection was performed. On microscopic examination, atypical lymphoid cells infiltrated and replaced the prostatic parenchyma. The tumor cells had large nuclei with irregular nuclear membrane and vesicular clumped chromatin. Nucleoli were not distinct and the cells had scanty cytoplasm. Immunohistochemically, the tumor cells were immunoreactive for CD20 and CD79a but not reactive for CD5, BCL-2 and BCL-6. Histopathological diagnosis was diffuse large B-cell lymphoma of the prostate. The patient received 5 cycles of chemotherapy after histologic diagnosis but died from pulmonary and scrotal metastases 6 months later.
- Fine Needle Aspiration Cytology of Anaplastic Large Cell Lymphoma: A case mimicking malignant fibrous histiocytoma.
- Jung Won Lee, Young Lyun Oh, Young Hyeh Ko
- J Pathol Transl Med. 1998;9(1):99-104.
- 2,066 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Anaplastic large cell lymphoma(ALCL) is an uncommon type of non-Hodgkin's lymphoma(NHL) populated with anaplastic, often bizarre cells that express CD30 (Ki-1) antigen. The unusual histologic and cytologic features may cause confusion with other neoplasms, such as poorly differentiated carcinoma, melanoma, Hodgkin's disease, or true histiocytic lymphoma. Although the cytologic features of ALCL have been well described, there are few reports about cytologic findings of the sarcomatoid variant of ALCL. We experienced a case of fine needle aspiration(FNA) cytologic findings of ALCL which mimicks malignant fibrous histiocytoma. FNA cytology of chest wall mass in a 62-year-old female with a history of peripheral T-cell lymphoma(Lennert lymphoma) revealed a heterogeneous population of single cells and poorly cohesive cells with large, pleomorphic nuclei and spindle cells gathering around vascular structures within an inflammatory background. Additional features of the neoplastic cells were eccentric, multilobated nuclei with occasional "wreath-like" configuration; abundant cytoplasm with vacuolization; and prominent nucleoli. The cytologic features suggested sarcoma, especially malignant fibrous histiocytoma. The diagnosis was made retrospectively with an aid of immunocytochemical staining.

 E-submission
E-submission

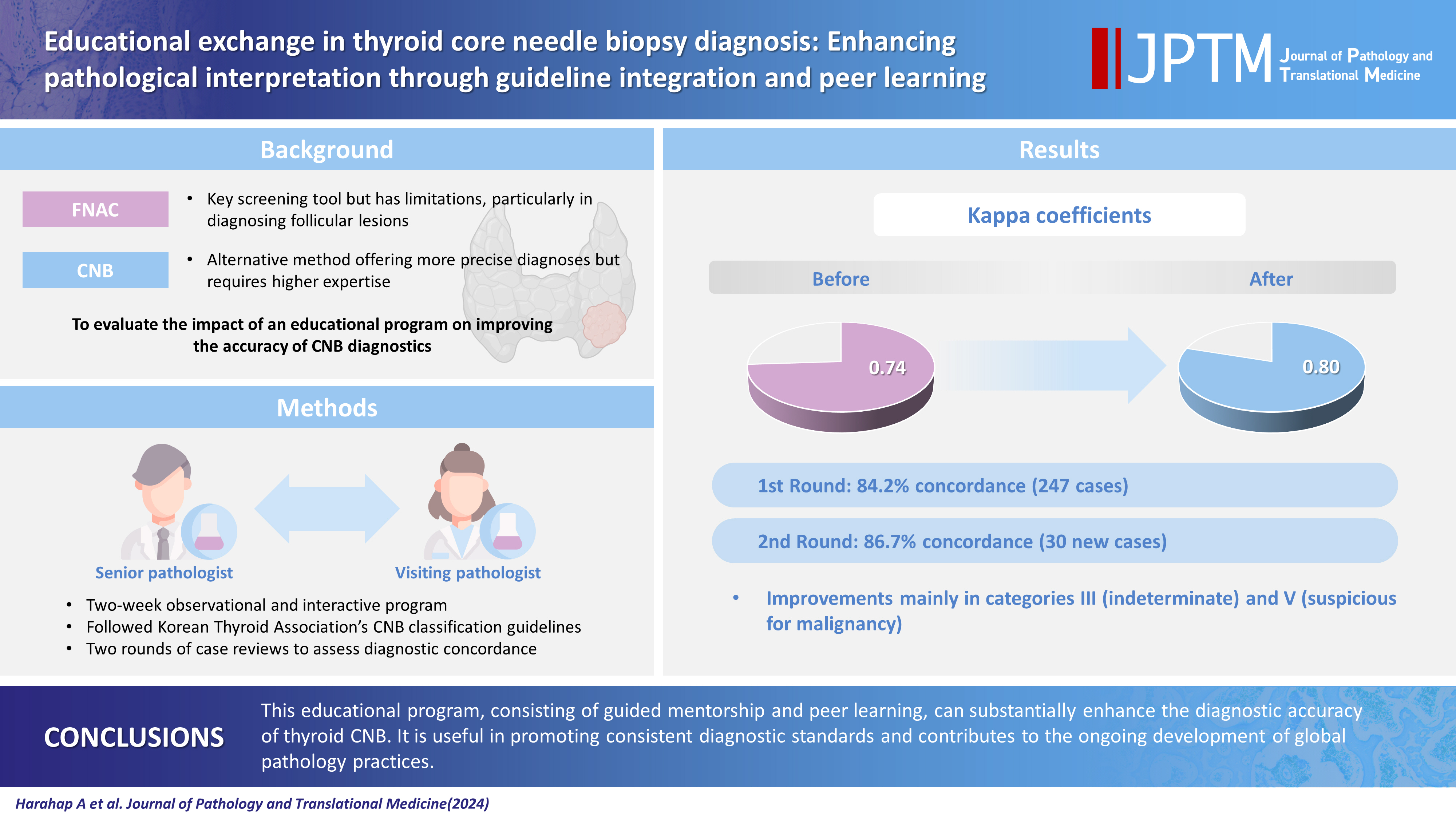

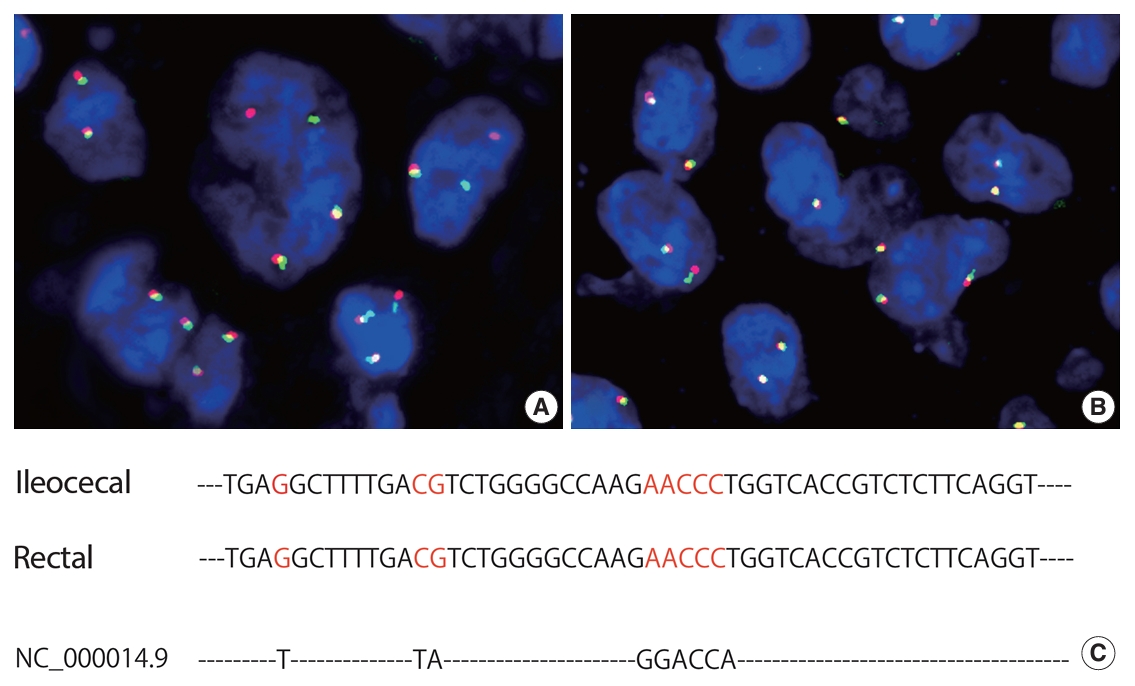
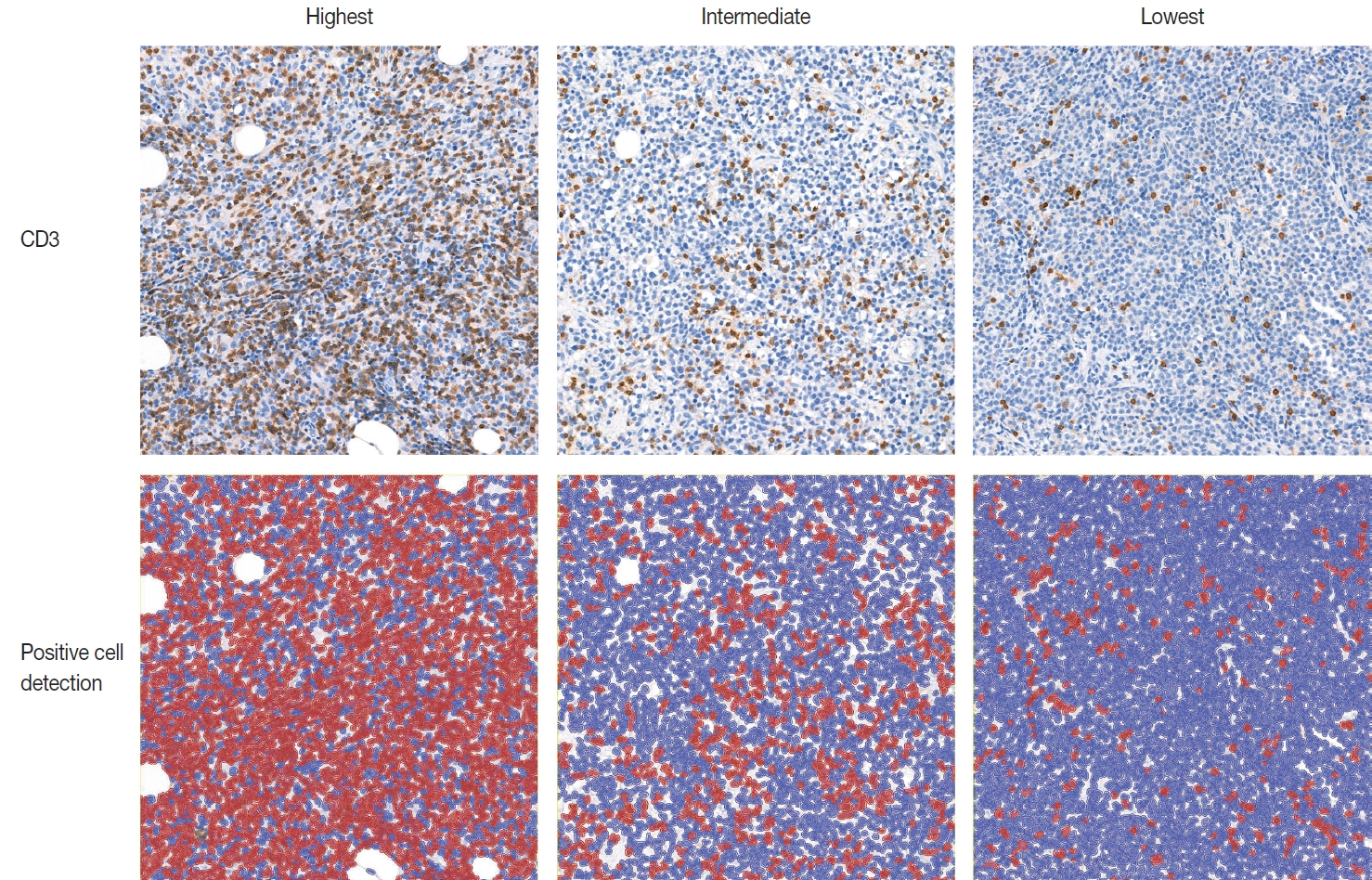

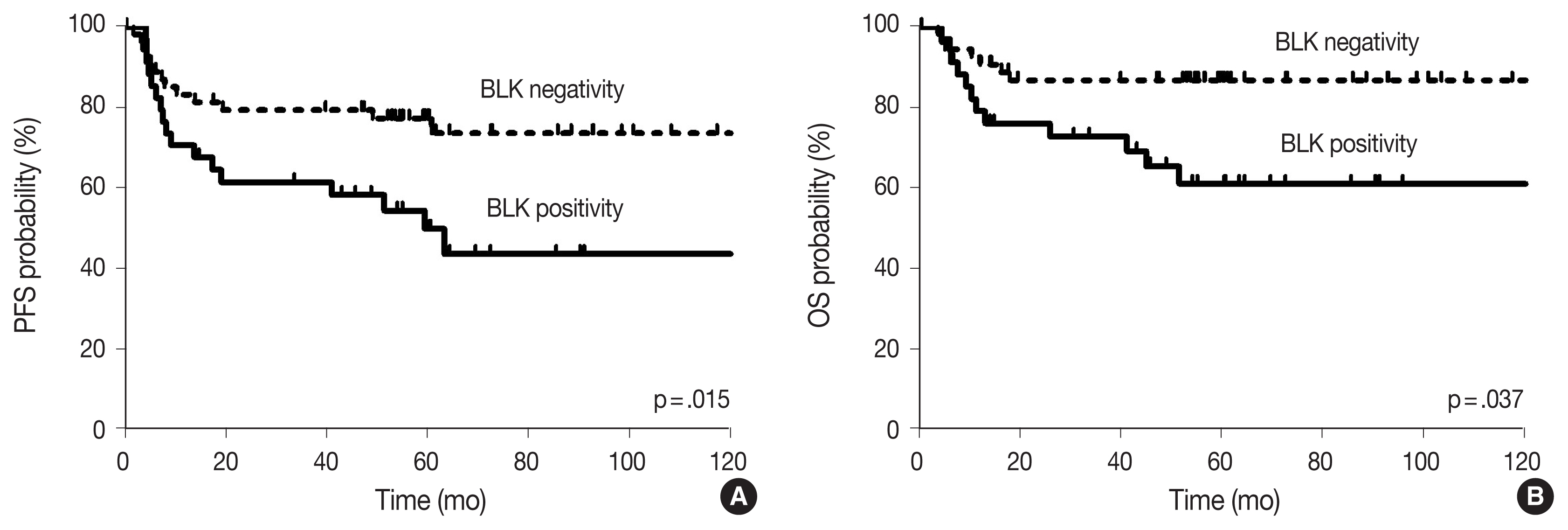
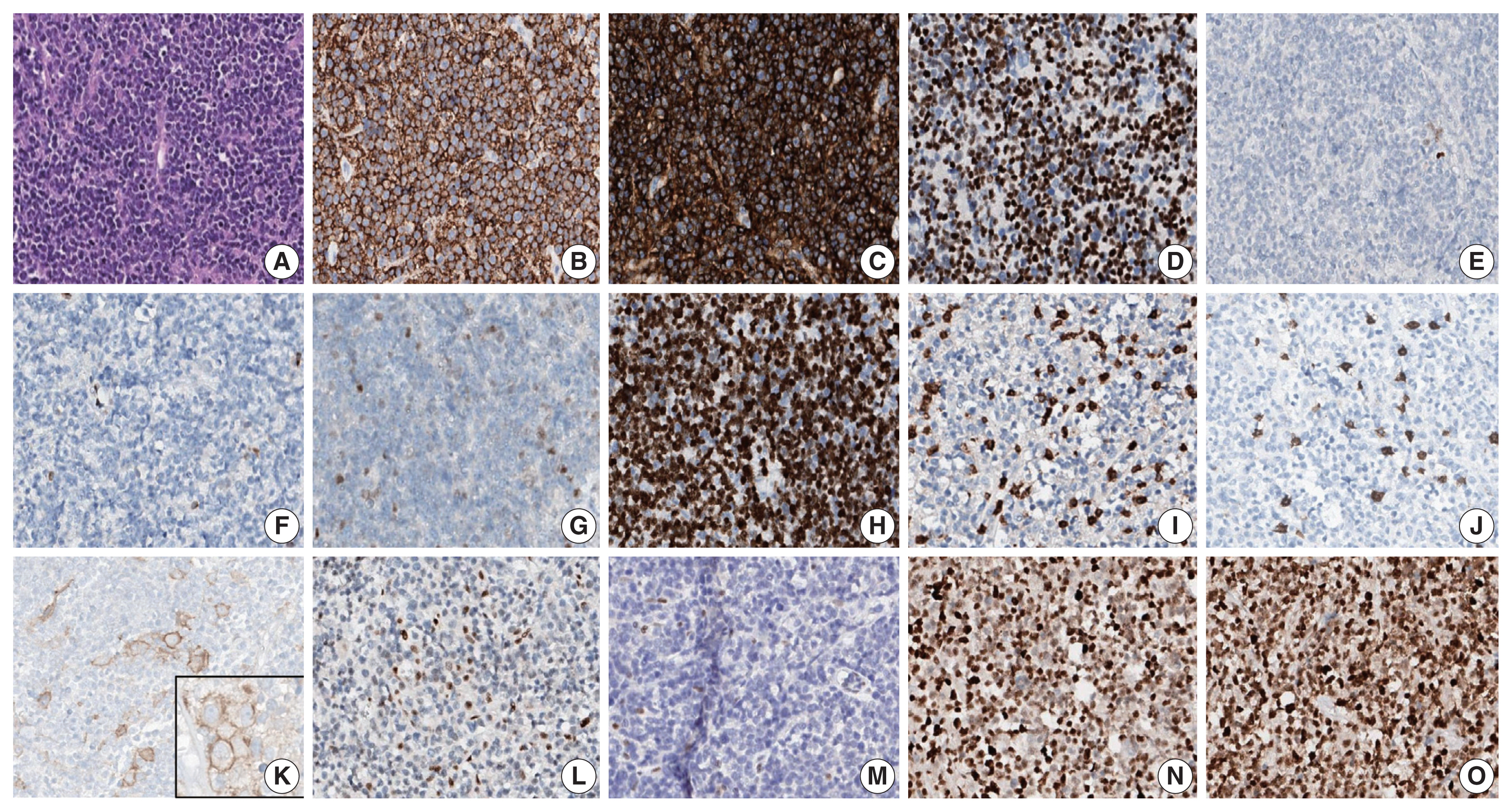
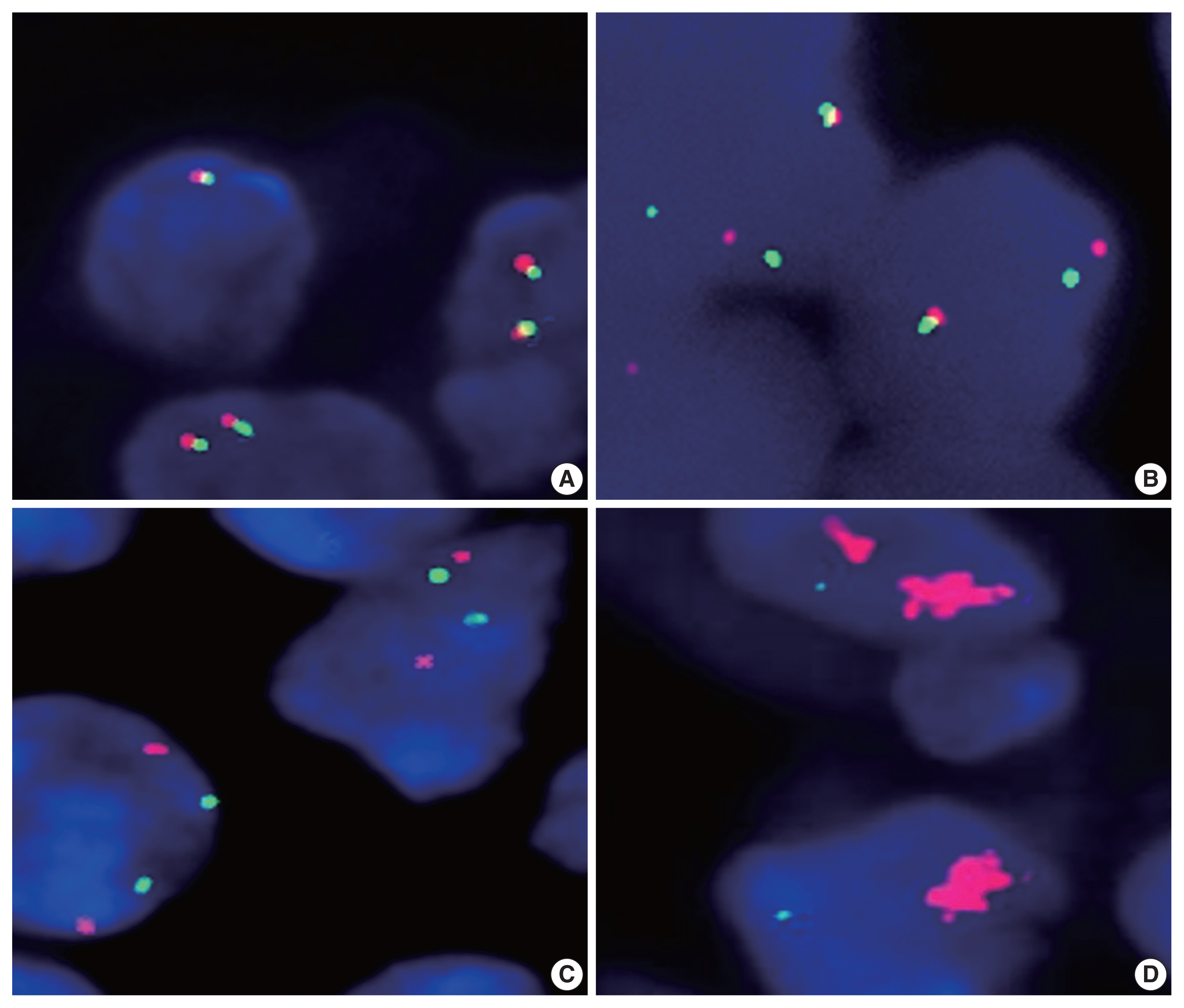
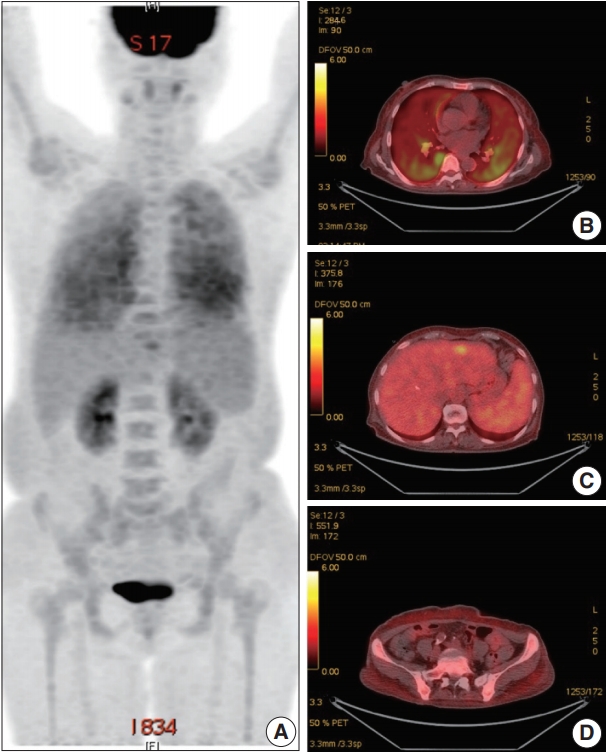
 First
First Prev
Prev



