Search
- Page Path
- HOME > Search
- Primary Merkel cell carcinoma of the salivary gland: a clinicopathologic study of four cases with a review of literature
- Gyuheon Choi, Joon Seon Song, Hee Jin Lee, Gi Hwan Kim, Young Ho Jung, Yoon Se Lee, Kyung-Ja Cho
- J Pathol Transl Med. 2025;59(3):171-179. Published online April 30, 2025
- DOI: https://doi.org/10.4132/jptm.2025.03.25
- 3,563 View
- 153 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Primary Merkel cell carcinoma of the salivary gland is currently not listed in the World Health Organization classification. However, cases of Merkel cell type neuroendocrine carcinomas of the salivary gland with perinuclear cytokeratin 20 positivity have been intermittently reported. We here investigated the clinicopathologic features of additional cases.
Methods
Data of four cases of Merkel cell type small cell neuroendocrine carcinoma of the salivary gland were retrieved. To confirm the tumors’ primary nature, clinical records and pathologic materials were reviewed. Optimal immunohistochemical staining was performed to support the diagnosis.
Results
All tumors were located in the parotid gland. Possibilities of metastasis were excluded in all cases through a meticulous clinicopathological review. Tumor histology was consistent with the diagnosis of small cell neuroendocrine carcinoma. Tumors’ immunohistochemical phenotypes were consistent with Merkel cell carcinoma, including Merkel cell polyomavirus large T antigen positivity in two of the four cases.
Conclusions
Merkel cell carcinomas can originate in salivary glands and are partly associated with Merkel cell polyomavirus infection as in cutaneous Merkel cell carcinomas. -
Citations
Citations to this article as recorded by- Parotid intranodal metastasis of Merkel cell carcinoma: a rare case report
Tong Gao, Dengshun Wang, Hongwei Yu, Yu’e Wang, Haibin Lu
BMC Oral Health.2025;[Epub] CrossRef
- Parotid intranodal metastasis of Merkel cell carcinoma: a rare case report
- Intravascular schwannoma as an extremely unusual cause of vein obstruction: a case report
- Luis Miguel Chinchilla-Tábora, Beatriz Segovia Blázquez, José María Sayagués, Marta Rodríguez González, Joaquín González-Rivero, José Antonio Muñoz León, Andrea Beatriz Jiménez Pérez, Idalia González Morais, Diego Bueno-Sacristán, María Dolores Ludeña
- J Pathol Transl Med. 2024;58(5):249-254. Published online July 3, 2024
- DOI: https://doi.org/10.4132/jptm.2024.05.15
- 4,149 View
- 282 Download
-
 Abstract
Abstract
 PDF
PDF - The blood vessel lumen is an extremely rare location for a benign peripheral nerve sheath tumor like schwannoma. Less than 10 cases have been previously reported. In this report, we present a case of a 68-year-old woman who had a soft tissue nodule at the posterior calf of her left leg during a physical examination. Pathological examination was performed after complete surgical excision. The patient underwent follow-up for 12 months after surgery without evidence of recurrence or any other complication. This is the first case of intravascular schwannoma reported as a cause of vein obstruction. Microscopically, the tumor was composed of Schwann spindle cells that were immunoreactive for S100 protein and SOX10. This tumor was surrounded by a well-defined vascular smooth muscle wall. Prospective series are required to improve the knowledge on the underlying mechanisms of intravascular schwannoma development.
- Malignant potential of neuroendocrine microtumor of the pancreas harboring high-grade transformation: lesson learned from a patient with von Hippel-Lindau syndrome
- Jongwon Lee, Kyung Jin Lee, Dae Wook Hwang, Seung-Mo Hong
- J Pathol Transl Med. 2024;58(2):91-97. Published online March 13, 2024
- DOI: https://doi.org/10.4132/jptm.2024.02.13
- 4,609 View
- 211 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pancreatic neuroendocrine microtumor (PNEMT) is a neuroendocrine tumor (NET) < 0.5 cm in diameter, and it is considered benign. We report a PNEMT with high-grade transformation (HGT). A man in his 60s with von Hippel-Lindau syndrome underwent surgical resection of a NET. A second sub-centimeter nodule with a nodule-in-nodule pattern was discovered. The 0.4 cm outer nodule contained clear columnar cells with round nuclei and indistinct nucleoli, while the 0.1 cm inner nodule had eosinophilic cells with an increased nuclear to cytoplasmic ratio, vesicular nuclei, and prominent nucleoli. Tumor cells in the outer and inner nodules were synaptophysin and chromogranin positive. Only the inner nodule was p53 positive, while the outer nodule was exclusively positive for carbonic anhydrase 9 and vimentin. The Ki-67 labeling indices for the outer and inner nodules were 2.1% (grade 1) and 44.3% (grade 3), respectively. This nodule was determined to be a PNEMT with HGT. Our findings suggest that a PNEMT may not always be benign and can undergo HGT.
-
Citations
Citations to this article as recorded by- Decoding Pancreatic Neuroendocrine Tumors: Molecular Profiles, Biomarkers, and Pathways to Personalized Therapy
Linda Galasso, Federica Vitale, Gabriele Giansanti, Giorgio Esposto, Raffaele Borriello, Irene Mignini, Alberto Nicoletti, Lorenzo Zileri Dal Verme, Antonio Gasbarrini, Maria Elena Ainora, Maria Assunta Zocco
International Journal of Molecular Sciences.2025; 26(16): 7814. CrossRef - Pancreatic neuroendocrine microtumors in the elderly: A retrospective study using cadaveric pancreatic tissue
Ting Yang, Ke Ren, Xiang-Quan Chen, Taku Toriumi, Yutaro Natsuyama, Jun Li, Aoi Sukeda, Toshitaka Nagao, Shuang-Qin Yi
World Journal of Gastrointestinal Oncology.2025;[Epub] CrossRef - Molecular Basis of Pancreatic Neuroendocrine Tumors
Alesia Maluchenko, Denis Maksimov, Zoia Antysheva, Julia Krupinova, Ekaterina Avsievich, Olga Glazova, Natalia Bodunova, Nikolay Karnaukhov, Ilia Feidorov, Diana Salimgereeva, Mark Voloshin, Pavel Volchkov
International Journal of Molecular Sciences.2024; 25(20): 11017. CrossRef
- Decoding Pancreatic Neuroendocrine Tumors: Molecular Profiles, Biomarkers, and Pathways to Personalized Therapy
- Immunohistochemical expression of anaplastic lymphoma kinase in neuroblastoma and its relations with some clinical and histopathological features
- Thu Dang Anh Phan, Thao Quyen Nguyen, Nhi Thuy To, Thien Ly Thanh, Dat Quoc Ngo
- J Pathol Transl Med. 2024;58(1):29-34. Published online January 10, 2024
- DOI: https://doi.org/10.4132/jptm.2023.12.07
- 5,258 View
- 289 Download
- 3 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Anaplastic lymphoma kinase (ALK) mutations have been identified as a prominent cause of some familial and sporadic neuroblastoma (NB). ALK expression in NB and its relationship with clinical and histopathological features remains controversial. This study investigated ALK expression and its potential relations with these features in NB.
Methods
Ninety cases of NB at the Department of Pathology, University of Medicine and Pharmacy at Ho Chi Minh City, Viet Nam from 01/01/2018 to 12/31/2021, were immunohistochemically stained with ALK (D5F3) antibody. The ALK expression and its relations with some clinical and histopathological features were investigated.
Results
The rate of ALK expression in NB was 91.1%. High ALK expression (over 50% of tumor cells were positive with moderate-strong intensity) accounted for 65.6%, and low ALK expression accounted for 34.4%. All the MYCN-amplified NB patients had ALK immunohistochemistry positivity, most cases had high ALK protein expression. The undifferentiated subtype of NB had a lower ALK-positive rate than the poorly differentiated and differentiated subtype. The percentages of ALK positivity were significantly higher in more differentiated histological types of NB (p = .024). There was no relation between ALK expression and: age group, sex, primary tumor location, tumor stage, MYCN status, clinical risk, Mitotic-Karyorrhectic Index, prognostic group, necrosis, and calcification.
Conclusions
ALK was highly expressed in NB. ALK expression was not related to several clinical and histopathological features. More studies are needed to elucidate the association between ALK expression and ALK gene status and to investigate disease progression, especially the oncogenesis of ALK-positive NB. -
Citations
Citations to this article as recorded by- A humanized anaplastic lymphoma kinase (ALK)-directed antibody-drug conjugate with pyrrolobenzodiazepine payload demonstrates efficacy in ALK-expressing cancers
Alberto D. Guerra, Smita Matkar, Christina Acholla, Colleen Casey, Grant Li, Martina Mazzeschi, Khushbu Patel, Kateryna Krytska, Chuan Chen, Skye Balyasny, Joshua Kalna, Paul Kamitsuka, Mark Gerelus, Grace Polkosnik, David Groff, Apratim Mukherje, Cynthia
Nature Communications.2025;[Epub] CrossRef - Integration of ALK gene mutations and targeted therapies in pediatric high-risk neuroblastoma: advancements in precision oncology
Bhumika Bheemavarapu, Mohammad Khalil, Aseef Rehman, Saman Javid, FNU Cyrus, Sardar Noman Qayyum, Aasvi Gohil, Siraj Ul Muneer, Samim Noori
Annals of Medicine & Surgery.2025; 87(10): 6470. CrossRef
- A humanized anaplastic lymphoma kinase (ALK)-directed antibody-drug conjugate with pyrrolobenzodiazepine payload demonstrates efficacy in ALK-expressing cancers
- Diagnosis of interstitial lung diseases: from Averill A. Liebow to artificial intelligence
- Eunhee S. Yi, Paul Wawryko, Jay H. Ryu
- J Pathol Transl Med. 2024;58(1):1-11. Published online January 10, 2024
- DOI: https://doi.org/10.4132/jptm.2023.11.17
- 7,386 View
- 430 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Histopathologic criteria of usual interstitial pneumonia (UIP)/idiopathic pulmonary fibrosis (IPF) were defined over the years and endorsed by leading organizations decades after Dr. Averill A. Liebow first coined the term UIP in the 1960s as a distinct pathologic pattern of fibrotic interstitial lung disease. Novel technology and recent research on interstitial lung diseases with genetic component shed light on molecular pathogenesis of UIP/IPF. Two antifibrotic agents introduced in the mid-2010s opened a new era of therapeutic approaches to UIP/IPF, albeit contentious issues regarding their efficacy, side effects, and costs. Recently, the concept of progressive pulmonary fibrosis was introduced to acknowledge additional types of progressive fibrosing interstitial lung diseases with the clinical and pathologic phenotypes comparable to those of UIP/IPF. Likewise, some authors have proposed a paradigm shift by considering UIP as a stand-alone diagnostic entity to encompass other fibrosing interstitial lung diseases that manifest a relentless progression as in IPF. These trends signal a pendulum moving toward the tendency of lumping diagnoses, which poses a risk of obscuring potentially important information crucial to both clinical and research purposes. Recent advances in whole slide imaging for digital pathology and artificial intelligence technology could offer an unprecedented opportunity to enhance histopathologic evaluation of interstitial lung diseases. However, current clinical practice trends of moving away from surgical lung biopsies in interstitial lung disease patients may become a limiting factor in this endeavor as it would be difficult to build a large histopathologic database with correlative clinical data required for artificial intelligence models.
-
Citations
Citations to this article as recorded by- Identification of early genes in the pathophysiology of fibrotic interstitial lung disease in a new model of pulmonary fibrosis
Nathan Hennion, Corentin Bedart, Léonie Vandomber, Frédéric Gottrand, Sarah Humez, Cécile Chenivesse, Jean-Luc Desseyn, Valérie Gouyer
Cellular and Molecular Life Sciences.2025;[Epub] CrossRef - Radiological Insights into UIP Pattern: A Comparison Between IPF and Non-IPF Patients
Stefano Palmucci, Miriam Adorna, Angelica Rapisarda, Alessandro Libra, Sefora Fischetti, Gianluca Sambataro, Letizia Antonella Mauro, Emanuele David, Pietro Valerio Foti, Claudia Mattina, Corrado Spatola, Carlo Vancheri, Antonio Basile
Journal of Clinical Medicine.2025; 14(12): 4162. CrossRef
- Identification of early genes in the pathophysiology of fibrotic interstitial lung disease in a new model of pulmonary fibrosis
- Diagnostic conundrums of schwannomas: two cases highlighting morphological extremes and diagnostic challenges in biopsy specimens of soft tissue tumors
- Chankyung Kim, Yang-Guk Chung, Chan Kwon Jung
- J Pathol Transl Med. 2023;57(5):278-283. Published online August 24, 2023
- DOI: https://doi.org/10.4132/jptm.2023.07.13
- 5,386 View
- 265 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Schwannomas are benign, slow-growing peripheral nerve sheath tumors commonly occurring in the head, neck, and flexor regions of the extremities. Although most schwannomas are easily diagnosable, their variable morphology can occasionally create difficulty in diagnosis. Reporting pathologists should be aware that schwannomas can exhibit a broad spectrum of morphological patterns. Clinical and radiological examinations can show correlation and should be performed, in conjunction with ancillary tests, when appropriate. Furthermore, deferring a definitive diagnosis until excision may be necessary for small biopsy specimens and frozen sections. This report underscores these challenges through examination of two unique schwannoma cases, one predominantly cellular and the other myxoid, both of which posed significant challenges in histological interpretation.
-
Citations
Citations to this article as recorded by- Oral and maxillofacial schwannoma (OMSCH): An institutional study of 102 patients
Lingli Huang, Wenya Zhu, Qicheng Ye, Shengwen Liu, Hao Lu, Wenjun Yang, Wanlin Xu
Journal of Stomatology Oral and Maxillofacial Surgery.2026; 127(3): 102678. CrossRef - Plexiform Schwannoma Over the Anterior Chest Wall: A Clinicopathological Review
Debojyoti Sasmal, Saswata Barenya, Hinglaj Saha, Pankaj Kumar Halder
Amrita Journal of Medicine.2025; 21(2): 95. CrossRef - Giant Retroperitoneal Schwannoma: Case Report and Review of the Literature
Magdalena Alexieva, Evgeni V Mekov, Silvia Ivanova, Alexandrina Vlahova, Georgi Yankov
Cureus.2025;[Epub] CrossRef - Breast schwannoma: review of entity and differential diagnosis
Sandra Ixchel Sanchez, Ashley Cimino-Mathews
Journal of Pathology and Translational Medicine.2025; 59(6): 353. CrossRef
- Oral and maxillofacial schwannoma (OMSCH): An institutional study of 102 patients
- Aneurysmal bone cyst: a review
- Elham Nasri, John David Reith
- J Pathol Transl Med. 2023;57(2):81-87. Published online March 14, 2023
- DOI: https://doi.org/10.4132/jptm.2023.02.23
- 37,011 View
- 783 Download
- 28 Web of Science
- 32 Crossref
-
 Abstract
Abstract
 PDF
PDF - Aneurysmal bone cyst (ABC) is a benign locally destructive bone neoplasm composed of multi-loculated blood-filled cystic spaces. The most common sites of involvement are the meta-diaphysis of the long bones and posterior elements of the vertebrae. Secondary, ABC-like changes can complicate a variety of other benign and malignant primary bone neoplasms, including giant cell tumor, fibrous dysplasia, and osteosarcoma. About two-third of primary ABCs have a rearrangement of the USP6 gene, which is not present in the ABC-like changes that occur secondary to other primary bone tumors (i.e., secondary ABC). Primary ABC of bone carries a variable but generally high rate of local recurrence. This paper provides an overview of the pathophysiology, clinical presentation, radiographic and pathologic findings, treatment, and prognosis of ABC.
-
Citations
Citations to this article as recorded by- Polidocanol Sclerotherapy Plus Adjuvant Autogenous Bone Marrow Injection for Management of Aneurysmal Bone Cyst: A Prospective Study
Ehab Abdelfattah Elshal, Maysra Abdelhalim Mohamed Byoumy, Abdallah Mousa Elwany Hassan, Abdelaziz Monsef Ali, Mohammed Al-Saeed Abdo Abu Hatab, Ahmed Sayed Ismaeil Khashaba
Indian Journal of Orthopaedics.2026;[Epub] CrossRef - Long‐Term Outcomes of Temporal Bone Aneurysmal Bone Cysts: Ambispective Study With Systematic Review and Pooled Analysis
Nidhin Das K, Anant Mehrotra, Amit Keshri, Mohit Sinha, Nazrin Hameed, Kalyan Chidambaram, Mohd Aqib, Awadesh Kumar Jaiswal, Ravisankar Manogaran
Otolaryngology–Head and Neck Surgery.2025; 172(5): 1493. CrossRef - Assessment and management of periacetabular aneurysmal bone cysts—a series of four cases
Reagan S.H Beyer, Quinn Steiner, David W Hennessy, Humberto G Rosas, David C Goodspeed, Andrea M Spiker
Journal of Hip Preservation Surgery.2025; 12(1): 11. CrossRef - Angiomatoid fibrous histiocytoma with EWSR1-CREB1 gene fusion occurs in lungs and ribs with systemic multiple metastases: a case report and review of the literature
Dongmei Feng, Ying Li, Zhengjin Li, Yun Pan, Yixuan Gao, Jinyan Cha, Chunmei Zhang
Frontiers in Oncology.2025;[Epub] CrossRef - Complete remodelling post-intralesional resection of an aggressive proximal humerus aneurysmal bone cyst mimicking telangiectatic osteosarcoma
Harpreet Singh, Sze Jet Aw, Arjandas Mahadev, Mohammad Ashik Bin Zainuddin, Kenneth Pak Leung Wong
BMJ Case Reports.2025; 18(2): e263437. CrossRef - First insights into the safety and effectiveness of additional courses with cladribine tablets under real-world conditions
Christoph Kleinschnitz, Jelena Skuljec, Markus C. Kowarik, Michael Ernst, Lara Woitschach, Lukas Cepek, Daniela Rau, Benedicta Kühnler, Sylke Schlemilch-Paschen, Matthias Schwab, Refik Pul
Multiple Sclerosis and Related Disorders.2025; 97: 106398. CrossRef - Case Report: Giant cell lesions in the Maxillofacial region: diagnostic points and treatment strategies
Xiaohan Gao, Shuangyi Wang, Xiaohong Zhan, Yanshan Liu, Liqiang Chen, Jian Sun, Haoyue Xu
Frontiers in Oncology.2025;[Epub] CrossRef - Endoscopic Curettage of Aneurysmal Bone Cyst of the Distal Fibula
Tun Hing Lui, Ka Kin Cheung, Wun Kee Szeto
Arthroscopy Techniques.2025; 14(7): 103561. CrossRef - Reviewing superficial bone lesions: What the radiologist needs to know
Dâmaris Versiani Caldeira Gonçalves, Isabela Azevedo Nicodemos da Cruz, Marcelo Astolfi Caetano Nico, Alípio Gomes Ormond Filho, Júlio Brandão Guimarães
Clinical Imaging.2025; 123: 110493. CrossRef - Juvenile ossifying fibroma and aneurysmal bone cyst in the mandible: A case report and mini review of literature
Fatma Wageeh Attya, Walaa Hussein Abu El-Ela, Basma Abdelrahman Ahmed, Iman Mohamed Helmy
Pediatric Dental Journal.2025; 35(3): 100354. CrossRef - A clinical case of an aneurysmal bone cyst of the humerus
N.S. Lysenko, V.V. Bayev, І.О. Voronzhev, S.M. Palchyk, А.М. Hrytsenko
Український радіологічний та онкологічний журнал.2025; 33(2): 270. CrossRef - Aneurysmal bone cyst of the rib. Robotic resection of a rare lesion
Luis Arana-Bolaños, Xcaret Luna-Vargas, Amelia Fernández-Avendaño, Mónica Martínez-Ferman, Pablo Gomes-da Silva de Rosenzweig, Francina Bolaños-Morales
Journal of Surgical Case Reports.2025;[Epub] CrossRef - Musculoskeletal tumors and tumor-like lesions with “dark” signal intensity on T2-weighted MR images: A pictorial review
Jingkun Zhang, Fengyuan Luo, Juan Chen, Huijuan Yang, Qi Zhang
Medicine.2025; 104(41): e45179. CrossRef - Escleroterapia con alcohol al 90% previo a exéresis de quiste óseo aneurismático maxilar: Reporte de caso
Glenda Semanate Cajas
Arandu UTIC.2025; 12(3): 4306. CrossRef - Case Report: Adult proximal humeral aneurysmal bone cyst: radical resection and reconstruction with osteoconductive allograft & reverse arthroplasty—Ecuador's first reported case and functional outcomes
Gabriel Gamecho Arteaga, Henry Hernández, Chrystian X. Mestanza, Jaime Zurita, Marlon Arias-Intriago, Juan S. Izquierdo-Condoy
Frontiers in Surgery.2025;[Epub] CrossRef - Aggressive Aneurysmal Bone Cyst of the Mandible: A Rare Case of Rapid Expansion and Surgical Management
Fatemeh Mashhadiabbas, Sanaz Gholami Toghchi, Sara Alehossein, Hoorisa Norouzi, Mohammadreza Kashefi Baher
Clinical Case Reports.2025;[Epub] CrossRef - Management of aggressive recurrent thoracic spine aneurysmal bone cyst in a 7-year-old male: A case report and review of the literature
Pedram Jahangiri, Faramarz Roohollahi, Zohreh Habibi, Mohammad Hosein Mirbolouk, Mohsen Rostami
Surgical Neurology International.2024; 15: 30. CrossRef - Intraosseous hemangioma with aneurysmal bone cyst-like changes of the hyoid bone: Case report and literature review
Jeonghyun Oh, Song Iy Han, Sung-Chul Lim
Medicine.2024; 103(6): e37137. CrossRef - Fibrous dysplasia with aneurysmal bone cyst-like change occurring in pediatric orbit: case report and literature review
Xinyao Wang, Wenbin Guan, Haibo Zhang, Lei Bao, Xiaoqiang Wang
Oral and Maxillofacial Surgery.2024; 28(2): 999. CrossRef - Pathological Fractures in Aneurysmal Bone Cysts: A Systematic Review
Doriana Di Costa, Elena Gabrielli, Mariagrazia Cerrone, Emidio Di Gialleonardo, Giulio Maccauro, Raffaele Vitiello
Journal of Clinical Medicine.2024; 13(9): 2485. CrossRef - Quiste óseo aneurismático torácico, descompresión mediante costotransversectomía, corpectomía y caja telescópica expandible. Reporte de un caso y revisión de literatura
Karoll Ortíz-Guillén, José M García-De la Rosa, Everardo García, Adriana Vargas-Oviedo
Cirugía de Columna.2024; 2(3): 188. CrossRef - The Role of Denosumab Treatment in Recurrent Giant Cell Bone Tumor of the Orbit
Arjav Gupta, Bruce Colwell, David B. Clarke, Emad A. Massoud, Sidney Croul, Ahsen Hussain
Ophthalmic Plastic & Reconstructive Surgery.2024; 40(5): e161. CrossRef - Denosumab Re-Challenge and Long-Term Efficacy for Aneurysmal Bone Cyst of the Spine: Enhanced Treatment Algorithm
Gisberto Evangelisti, Franziska C. S. Altorfer, Luigi Falzetti, Emanuela Palmerini, Cristiana Griffoni, Riccardo Ghermandi, Stefano Boriani, Annalisa Monetta, Marilena Cesari, Toni Ibrahim, Alessandro Gasbarrini
Journal of Clinical Medicine.2024; 13(15): 4522. CrossRef - Rare Aneurysmal Bone Cyst Presentation in the Orbit: A Systematic Review of the Literature with an Illustrative Case Report
Sean O'Leary, Fakhar Hayat, Saketh Amasa, Muhammad Ammar Haider, Saad Akram Asbeutah, Usama AlDallal, Umaru Barrie, Mohamed Ismail
World Neurosurgery.2024; 191: 1. CrossRef - Primary osseous leiomyosarcoma of humerus misinterpreted as aneurysmal bone cyst: A case report and literature review
Yong Jin Cho, Young Kwon Koh, Sung-Chul Lim
Medicine.2024; 103(38): e39762. CrossRef - Recurrent Aneurysmal Bone Cyst Treated with Percutaneous Doxycycline Sclerotherapy
Cory Gall, Daniel C. Allison
JBJS Case Connector.2024;[Epub] CrossRef - Development and Printing of a Customized 3D Model of a Solitary Humeral Cyst as a Stage in Surgical Treatment of Bone Defects Using Orgignal Bone Replased Material
Bakhtiyar Makhatov, Berik Tuleubayev, Amina Koshanova
Journal of Clinical Medicine of Kazakhstan.2024; 21(6): 91. CrossRef - Diagnosis and management of bone cysts
Deepak C. D., Anitha Boregowdanapalya
International Journal of Research in Medical Sciences.2024; 13(1): 509. CrossRef - A rare case of cavitated Schmorl’s node in the cervical spine: imaging features of bone scan and magnetic resonance
Yung-Cheng Chang, Yu-Jing Kao, Ling Chun Sun, Wen-Hsuan Hsiao, Shin-Tsu Chang
MOJ Orthopedics & Rheumatology.2024; 16(5): 278. CrossRef - Metastatic patellar bone tumor due to gastric cancer resembling a primary or secondary aneurysmal bone cyst: A case report
T. Furuta, T. Sakuda, K. Yoshioka, K. Arihiro, N. Adachi
International Journal of Surgery Case Reports.2023; 108: 108379. CrossRef - Clear cell chondrosarcoma: a review of clinicopathologic characteristics, differential diagnoses, and patient management
Borislav A. Alexiev, Erica R. Vormittag-Nocito, Terrance D. Peabody, Jonathan Samet, William B. Laskin
Human Pathology.2023; 139: 126. CrossRef - Malignant transformation of an aneurysmal bone cyst of the femoral neck: A case report
Xiaoyang Song, Yongjie Qiao, Haoqiang Zhang, Lirong Sha, Jinpeng Lou, Xinyuan Yu, Hao Liu, Langfeng Zhu, Shenghu Zhou
Experimental and Therapeutic Medicine.2023;[Epub] CrossRef
- Polidocanol Sclerotherapy Plus Adjuvant Autogenous Bone Marrow Injection for Management of Aneurysmal Bone Cyst: A Prospective Study
- Significance of tumor-associated neutrophils, lymphocytes, and neutrophil-to-lymphocyte ratio in non-invasive and invasive bladder urothelial carcinoma
- Wael Abdo Hassan, Ahmed Kamal ElBanna, Noha Noufal, Mohamed El-Assmy, Hany Lotfy, Rehab Ibrahim Ali
- J Pathol Transl Med. 2023;57(2):88-94. Published online January 10, 2023
- DOI: https://doi.org/10.4132/jptm.2022.11.06
- 7,446 View
- 325 Download
- 15 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Tumor-infiltrating neutrophils and lymphocytes play essential roles in promoting or combating various neoplasms. This study aimed to investigate the association between tumor-infiltrating neutrophils and lymphocytes and the neutrophil-to-lymphocyte ratio in the progression of urothelial carcinoma.
Methods
A total of 106 patients diagnosed with urothelial carcinoma were was. Pathological examination for tumor grade and stage and for tumor-infiltrating neutrophils, both CD4 and CD8+ T lymphocytes, as well as the neutrophil- to-lymphocyte ratio were evaluated.
Results
The presence of neutrophils and the neutrophil-to-lymphocyte ratio correlated with high-grade urothelial neoplasms. In both low- and high-grade tumors, the lymphocytes increased during progression from a non-invasive neoplasm to an early-invasive neoplasm. CD8+ T lymphocytes increased in low-grade non–muscle-invasive tumors compared to non-invasive tumors. Additionally, there was a significant decrease in CD8+ T lymphocytes during progression to muscle-invasive tumors.
Conclusions
Our results suggest that tumor-infiltrating neutrophils and CD8+ T lymphocytes have a significant effect on tumor grade and progression. -
Citations
Citations to this article as recorded by- Prognostic role of the neutrophil/lymphocyte ratio in high‐risk BCG‐naïve non‐muscle‐invasive bladder cancer treated with intravesical gemcitabine/docetaxel
Mohamad Abou Chakra, Riitta Lassila, Nancy El Beayni, Sarah L. Mott, Michael A. O'Donnell
BJU International.2025; 135(1): 125. CrossRef - Understanding the Dual Role of Macrophages in Tumor Growth and Therapy: A Mechanistic Review
Muhammad Summer, Saima Riaz, Shaukat Ali, Qudsia Noor, Rimsha Ashraf, Rana Rashad Mahmood Khan
Chemistry & Biodiversity.2025;[Epub] CrossRef - Cross-Talk Between Cancer and Its Cellular Environment—A Role in Cancer Progression
Eliza Turlej, Aleksandra Domaradzka, Justyna Radzka, Dominika Drulis-Fajdasz, Julita Kulbacka, Agnieszka Gizak
Cells.2025; 14(6): 403. CrossRef - Global trends in tumor-associated neutrophil research: a bibliometric and visual analysis
Shaodong Li, Peng Dong, Xueliang Wu, Zhenhua Kang, Guoqiang Yan
Frontiers in Immunology.2025;[Epub] CrossRef - Tumor-associated neutrophils and neutrophil extracellular traps in lung cancer: antitumor/protumor insights and therapeutic implications
Milad Sheervalilou, Mostafa Ghanei, Masoud Arabfard
Medical Oncology.2025;[Epub] CrossRef - Construction of a column-line graphical model of poor outcome of neoadjuvant regimens for muscle-invasive bladder cancer based on NLR, dNLR and SII indicators
Bo Hu, Longsheng Wang, Shanna Qu, Tao Zhang
World Journal of Surgical Oncology.2025;[Epub] CrossRef - Machine Learning of Urine Cytology Highlights Increased Neutrophil Count in Muscle-Invasive Urothelial Carcinoma
Moe Kameda, Sayaka Kobayashi, Yoshimi Nishijima, Ryosuke Akuzawa, Rio Kaneko, Rio Shibanuma, Seiji Arai, Hayato Ikota, Kazuhiro Suzuki, Hideaki Yokoo, Masanao Saio
Journal of Cytology.2025; 42(3): 124. CrossRef - Tumor-Infiltrating Immune Cells in Non-Muscle-Invasive Bladder Cancer: Prognostic Implications, Predictive Value, and Future Perspectives
Roberta Mazzucchelli, Angelo Cormio, Magda Zanelli, Maurizio Zizzo, Andrea Palicelli, Andrea Benedetto Galosi, Francesca Sanguedolce
Applied Sciences.2025; 15(22): 12032. CrossRef - Immune cell networking in solid tumors: focus on macrophages and neutrophils
Irene Di Ceglie, Silvia Carnevale, Anna Rigatelli, Giovanna Grieco, Piera Molisso, Sebastien Jaillon
Frontiers in Immunology.2024;[Epub] CrossRef - Immunohistochemistry assessment of tissue neutrophil-to-lymphocyte ratio predicts outcomes in melanoma patients treated with anti-programmed cell death 1 therapy
Renan J. Teixeira, Vinícius G. de Souza, Bruna P. Sorroche, Victor G. Paes, Fabiana A. Zambuzi-Roberto, Caio A.D. Pereira, Vinicius L. Vazquez, Lidia M.R.B. Arantes
Melanoma Research.2024; 34(3): 234. CrossRef - Association between alteration of neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, cancer antigen-125 and surgical outcomes in advanced stage ovarian cancer patient who received neoadjuvant chemotherapy
Ponganun Tuntinarawat, Ratnapat Tangmanomana, Thannaporn Kittisiam
Gynecologic Oncology Reports.2024; 52: 101347. CrossRef - Prognostic value of neutrophil-to-lymphocyte ratio in patients with non–muscle-invasive bladder cancer with intravesical Bacillus Calmette–Guérin immunotherapy: a systematic review and meta-analysis
Jiaguo Huang, Li Lin, Dikai Mao, Runmiao Hua, Feifei Guan
Frontiers in Immunology.2024;[Epub] CrossRef - Update on the Mechanism of Action of Intravesical BCG Therapy to Treat Non-Muscle-Invasive Bladder Cancer
Mohamad Abou Chakra, Yi Luo, Igor Duquesne, Michael A O'Donnell
Frontiers in Bioscience-Landmark.2024;[Epub] CrossRef - Significant association between high neutrophil-lymphocyte ratio and poor prognosis in patients with hepatocellular carcinoma: a systematic review and meta-analysis
Chunhua Xu, Fenfang Wu, Lailing Du, Yeping Dong, Shan Lin
Frontiers in Immunology.2023;[Epub] CrossRef - Chitinase 3-like-1 Expression in the Microenvironment Is Associated with Neutrophil Infiltration in Bladder Cancer
Ling-Yi Xiao, Yu-Li Su, Shih-Yu Huang, Yi-Hua Chen, Po-Ren Hsueh
International Journal of Molecular Sciences.2023; 24(21): 15990. CrossRef
- Prognostic role of the neutrophil/lymphocyte ratio in high‐risk BCG‐naïve non‐muscle‐invasive bladder cancer treated with intravesical gemcitabine/docetaxel
- Neuropathologic features of central nervous system hemangioblastoma
- Rebecca A. Yoda, Patrick J. Cimino
- J Pathol Transl Med. 2022;56(3):115-125. Published online May 3, 2022
- DOI: https://doi.org/10.4132/jptm.2022.04.13
- 16,464 View
- 367 Download
- 18 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF - Hemangioblastoma is a benign, highly vascularized neoplasm of the central nervous system (CNS). This tumor is associated with loss of function of the VHL gene and demonstrates frequent occurrence in von Hippel-Lindau (VHL) disease. While this entity is designated CNS World Health Organization grade 1, due to its predilection for the cerebellum, brainstem, and spinal cord, it is still an important cause of morbidity and mortality in affected patients. Recognition and accurate diagnosis of hemangioblastoma is essential for the practice of surgical neuropathology. Other CNS neoplasms, including several tumors associated with VHL disease, may present as histologic mimics, making diagnosis challenging. We outline key clinical and radiologic features, pathophysiology, treatment modalities, and prognostic information for hemangioblastoma, and provide a thorough review of the gross, microscopic, immunophenotypic, and molecular features used to guide diagnosis.
-
Citations
Citations to this article as recorded by- Immunohistochemical Expression of PAX8 in Central Nervous System Hemangioblastomas: A Potential Diagnostic Pitfall for Neuropathologists
Giuseppe Broggi, Jessica Farina, Valeria Barresi, Francesco Certo, Giuseppe Maria Vincenzo Barbagallo, Gaetano Magro, Rosario Caltabiano
Applied Immunohistochemistry & Molecular Morphology.2025; 33(3): 160. CrossRef - Endolymphatic Sac Tumor. Post-Radiosurgery Evaluation Using Time-Resolved Imaging of Contrast Kinetics MR Angiography
Antonella Blandino, Allegra Romano, Chiara Filippi, Sofia Pizzolante, Andrea Romano, Giulia Moltoni, Edoardo Covelli, Maurizio Barbara, Alessandro Bozzao
Ear, Nose & Throat Journal.2025;[Epub] CrossRef - Stereotactic radiosurgery in the management of central nervous system hemangioblastomas: a systematic review and meta-analysis
Amirhossein Zare, Amirhessam Zare, Alireza Soltani Khaboushan, Bardia Hajikarimloo, Jason P. Sheehan
Neurosurgical Review.2025;[Epub] CrossRef - Cerebellar medullary cistern hemangioblastoma
Dahai Cao, Qiang Zhang
Asian Journal of Surgery.2025; 48(9): 5843. CrossRef - Navigating rare vascular brain tumors: A retrospective observational study
Sana Ahuja, Dipanker S Mankotia, Naveen Kumar, Vyomika Teckchandani, Sufian Zaheer
Cancer Research, Statistics, and Treatment.2025; 8(2): 92. CrossRef - A potential new entity pending further validation of pulmonary primary interstitial Tumor: Lymphangioleiomyomatosis-like
Lingyu Zhao, Xiaochen Shen, Yun Niu, Huang Chen, Dingrong Zhong
Respiratory Medicine Case Reports.2025; 57: 102241. CrossRef - Renal cell carcinoma with fibromyomatous stroma (RCC FMS) and with hemangioblastoma‐like areas is part of the RCC FMS spectrum in patients with tuberous sclerosis complex
Katherina Baranova, Jacob A Houpt, Deaglan Arnold, Andrew A House, Laura Lockau, Lindsay Ninivirta, Stephen Pautler, Haiying Chen, Madeleine Moussa, Rola Saleeb, Jose A Gomez, Asli Yilmaz, Farshid Siadat, Adrian Box, Douglas J Mahoney, Franz J Zemp, Manal
Histopathology.2025; 87(5): 687. CrossRef - Renal hemangioblastoma and renal cell carcinoma with fibromyomatous stroma and hemangioblastoma-like areas belong to the spectrum of one entity
Kiril Trpkov, Norel Salut, Inmaculada Ribera-Cortada, Elías Tasso Xipell, Isabel Trias Puigsureda, Asli Yilmaz, Arjumand Riyaz Husain, Erik Nohr, Adrian Box, Farshid Siadat, Katherina Baranova, Rola M. Saleeb, Robert Stoehr, Arndt Hartmann, Abbas Agaimy
Virchows Archiv.2025;[Epub] CrossRef - Primary hemangioblastoma of rectum: a rare case report and review of literature
Aiping Zheng, Shaojuan Zhang, Qiang Ma, Wenxu Yang, Hualiang Xiao, Xinyu Liang
Journal of Cancer Research and Clinical Oncology.2025;[Epub] CrossRef - Cerebellar Hemangioblastoma Resection Complicated by Postoperative Vasogenic Edema in the Setting of Concurrent Immunotherapy Treatment
Aashka Sheth, Nicholas Dietz, Andrea Becerril-Gaitan, Rahim Kasem, Akshitkumar Mistry, Brian J Williams, Dale Ding, Isaac Abecassis
Cureus.2025;[Epub] CrossRef - Familial Von Hippel–Lindau Disease: A Case Series of Cerebral Hemangioblastomas with MRI, Histopathological, and Genetic Correlations
Claudiu Matei, Ioana Boeras, Dan Orga Dumitriu, Cosmin Mutu, Adriana Popescu, Mihai Gabriel Cucu, Alexandru Calotă-Dobrescu, Bogdan Fetica, Diter Atasie
Life.2025; 15(11): 1649. CrossRef - Characterization of spinal hemangioblastomas in patients with and without von Hippel-Lindau, and YAP expression
Ana-Laura Calderón-Garcidueñas, Steven-Andrés Piña-Ballantyne, Eunice-Jazmín Espinosa-Aguilar, Rebeca de Jesús Ramos-Sánchez
Revista Española de Patología.2024; 57(3): 160. CrossRef - Patients With Hemangioblastoma: Mood Disorders and Sleep Quality
Ali Riazi, Yaser Emaeillou, Nima Najafi, Mohammad Hoseinimanesh, Mohammad Ibrahim Ashkaran, Donya Sheibani Tehrani
Brain Tumor Research and Treatment.2024; 12(2): 87. CrossRef - Radiosurgically Treated Recurrent Cerebellar Hemangioblastoma: A Case Report and Literature Review
François Fabi, Ève Chamberland, Myreille D’Astous, Karine Michaud, Martin Côté, Isabelle Thibault
Current Oncology.2024; 31(7): 3968. CrossRef - Dual manifestations: spinal and cerebellar hemangioblastomas indicative of von Hippel-Lindau syndrome
Nurhuda Hendra Setyawan, Rachmat Andi Hartanto, Rusdy Ghazali Malueka, Ery Kus Dwianingsih, Dito Pondra Dharma
Radiology Case Reports.2024; 19(11): 5000. CrossRef - Phenotypic and Genotypic Features of a Chinese Cohort with Retinal Hemangioblastoma
Liqin Gao, Feng Zhang, J. Fielding Hejtmancik, Xiaodong Jiao, Liyun Jia, Xiaoyan Peng, Kai Ma, Qian Li
Genes.2024; 15(9): 1192. CrossRef - Case report: Hemangioblastoma in the brainstem of a dog
Kirsten Landsgaard, Samantha St. Jean, Stephanie Lovell, Jonathan Levine, Christine Gremillion, Brian Summers, Raquel R. Rech
Frontiers in Veterinary Science.2023;[Epub] CrossRef - Intramedullary hemangioblastoma of the thoracic cord with a microsurgical approach: A case report and literature review
Eduardo Cattapan Piovesan, Werner Petry Silva, Adroaldo Baseggio Mallmann, Felipe Severo Lanzini, Bruna Zanatta de Freitas, Francisco Costa Beber Lemanski, Charles André Carazzo
Surgical Neurology International.2023; 14: 137. CrossRef - Secondary Holocord Syringomyelia Associated With Spinal Hemangioblastoma in a 29-Year-Old Female
Eric Chun-Pu Chu, Edouard Sabourdy, Benjamin Cheong
Cureus.2023;[Epub] CrossRef - Belzutifan in adults with VHL-associated central nervous system hemangioblastoma: a single-center experience
Bryan J. Neth, Mason J. Webb, Jessica White, Joon H. Uhm, Pavel N. Pichurin, Ugur Sener
Journal of Neuro-Oncology.2023; 164(1): 239. CrossRef - Resection of Intramedullary Hemangioblastoma: Timing of Surgery and Its Impact on Neurological Outcome and Quality of Life
Michael Schwake, Sarah Ricchizzi, Sophia Krahwinkel, Emanuele Maragno, Stephanie Schipmann, Walter Stummer, Marco Gallus, Markus Holling
Medicina.2023; 59(9): 1611. CrossRef
- Immunohistochemical Expression of PAX8 in Central Nervous System Hemangioblastomas: A Potential Diagnostic Pitfall for Neuropathologists
- Intraoperative frozen cytology of intraosseous cystic meningioma in the sphenoid bone
- Na Rae Kim, Gie-Taek Yie
- J Pathol Transl Med. 2020;54(6):508-512. Published online July 1, 2020
- DOI: https://doi.org/10.4132/jptm.2020.05.21
- 5,667 View
- 101 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Meningiomas in bone are rarely subjected to fine-needle aspiration diagnosis, and those arising in the skull bone with a cystic presentation are rare. A 24-year-old woman presented with subdural hemorrhage, and subsequent radiology depicted an osteolytic mass-like lesion in the sphenoid bone. Intraoperatively, a solid and cystic hemorrhagic lesion mimicking an aneurysmal bone cyst was observed in the sphenoid bone with dural tearing. Frozen cytology showed singly scattered or epithelioid clusters of round to elongated cells intermixed with many neutrophils. Tumor cells had bland-looking round nuclei with rare prominent nucleoli and nuclear inclusions and eosinophilic granular to globoid cytoplasm in capillary-rich fragments. Histology revealed intraosseous meningothelial and microcystic meningioma (World Health Organization grade 1) in right lesser wing of the sphenoid bone. Considering its unusual location and cytologic findings, differential diagnoses included chordoma, chondroma, chondrosarcoma, and aneurysmal bone cyst. The present case posed a diagnostic challenge due to possible confusion with these entities.
-
Citations
Citations to this article as recorded by- Purely cystic intraosseous meningioma of the skull: A radiologic conundrum and histologic challenge
Diego Rojas, Arman Kavoussi, Ashley Rose Ricciardelli, Alex Flores, Sricharan Gopakumar, Luis Carrete, Hsiang-Chih Lu, Alex W. Brenner, Akash J. Patel
Surgical Neurology International.2025; 16: 221. CrossRef - Middle ear adenoma: Cytohistologic features and differential diagnosis
Abdullah Almajnooni, Matthew Vega, Lin Cheng, Paolo Gattuso, Mary K. Allen‐Proctor
Diagnostic Cytopathology.2023;[Epub] CrossRef - Exploring the role of epidermal growth factor receptor variant III in meningeal tumors
Rashmi Rana, Vaishnavi Rathi, Kirti Chauhan, Kriti Jain, Satnam Singh Chhabra, Rajesh Acharya, Samir Kumar Kalra, Anshul Gupta, Sunila Jain, Nirmal Kumar Ganguly, Dharmendra Kumar Yadav, Timir Tripathi
PLOS ONE.2021; 16(9): e0255133. CrossRef
- Purely cystic intraosseous meningioma of the skull: A radiologic conundrum and histologic challenge
- Primary carcinoid tumor in the external auditory canal
- Dong Hae Chung, Gyu Cheol Han, Na Rae Kim
- J Pathol Transl Med. 2020;54(2):184-187. Published online November 13, 2019
- DOI: https://doi.org/10.4132/jptm.2019.11.07
- 9,004 View
- 167 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - A 39-year-old man visited the department of otolaryngology due to an ongoing hearing disturbance that had lasted for 1 year. Temporal bone computed tomography revealed soft tissue density nearly obliterating the left external auditory canal (EAC). The mass was composed of sheets of round tumor cells containing moderate amounts of fine granular cytoplasm and salt and pepper chromatin. Neither mitosis nor necrosis was found. The Ki-67 proliferation index was less than 2%. Cells were positive for CD56 and synaptophysin but negative for chromogranin, cytokeratin (CK) 20, and CK7. Based on these findings, the tumor was diagnosed as a carcinoid tumor, well differentiated neuroendocrine carcinoma, grade 1 (G1) according to current World Health Organization (WHO) classification of head and neck tumors; and a neuroendocrine tumor, G1 according to neuroendocrine neoplasm (NEN)-2018 WHO standard classification. He remained free of local recurrence and metastasis after 20 months of follow up. To date, only six cases of primary NENs in the EAC have been reported. Metastatic tumor should be included in the differential diagnoses. Because of its rarity, the prognosis and treatment have not yet been clarified.
-
Citations
Citations to this article as recorded by- First Report on a Rare Poorly Differentiated Neuroendocrine Tumour of the External Auditory Canal Involving Pinna
Akash Varshney, Amit Kumar Tyagi, Prashant Durgapal, Kajal Mahto, Akhilesh Chandra Yadav, Ankita Semwal
Indian Journal of Otolaryngology and Head & Neck Surgery.2025; 77(4): 1922. CrossRef - Incidental finding of a neuroendocrine neoplasm in a suspected ear canal exostosis
Alexander Wieck Fjaeldstad, Gerda Elisabeth Villadsen, Gitte Dam, Stephen Jacques Hamilton-Dutoit, Thomas Winther Frederiksen
Otolaryngology Case Reports.2022; 22: 100394. CrossRef - 68Ga-DOTATATE Uptake in Well-Differentiated Neuroendocrine Tumor of the External Auditory Canal
Özge Erol Fenercioğlu, Ediz Beyhan, Rahime Şahin, Mehmet Can Baloğlu, Tevfik Fikret Çermik
Clinical Nuclear Medicine.2022; 47(8): e552. CrossRef
- First Report on a Rare Poorly Differentiated Neuroendocrine Tumour of the External Auditory Canal Involving Pinna
- Serous Adenocarcinoma of Fallopian Tubes: Histological and Immunohistochemical Aspects
- Natalia Hyriavenko, Mykola Lyndin, Kateryna Sikora, Artem Piddubnyi, Ludmila Karpenko, Olha Kravtsova, Dmytrii Hyriavenko, Olena Diachenko, Vladyslav Sikora, Anatolii Romaniuk
- J Pathol Transl Med. 2019;53(4):236-243. Published online April 11, 2019
- DOI: https://doi.org/10.4132/jptm.2019.03.21
- 8,483 View
- 132 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Although primary cancer of the fallopian tubes is a relatively rare type of tumor in female reproductive organs, its mortality is quite high. It is important to identify molecular and biological markers of this malignancy that determine its specific phenotype.
Methods
The study was carried out on samples received from 71 female patients with primary cancer of the fallopian tubes. The main molecular and biological properties, including hormone status (estrogen receptor [ER], progesterone receptor [PR]), human epidermal growth factor receptor (HER2)/neu expression, proliferative potential (Ki-67), apoptosis (p53, Bcl-2), and pro-angiogenic (vascular endothelial growth factor) quality of serous tumors were studied in comparison with clinical and morphological characteristics.
Results
ER and PR expression is accompanied by low grade neoplasia, early clinical disease stage, and absence of lymphogenic metastasis (p < .001). HER2/neu expression is not typical for primary cancer of the fallopian tubes. Ki-67 expression is characterized by an inverse correlation with ER and PR (p < .05) and is associated with lymphogenic metastasis (p < .01). p53+ status correlates with high grade malignancy, tumor progression, metastasis, negative ER/PR (p < .001), and negative Bcl-2 status (p < .05). Positive Bcl-2 status is positively correlated with ER and PR expression and low grade malignancy.
Conclusions
Complex morphologic (histological and immunohistochemical) study of postoperative material allows estimation of the degree of malignancy and tumor spread to enable appropriate treatment for each case. -
Citations
Citations to this article as recorded by- Rare non-serous fallopian tube cancers: institutional experience and literature review
Dmitrii Sumtsov, Georgyi Sumtsov, Nataliia Hyriavenko, Mykola Lyndin, Kateryna Sikora, Nataliia Kalashnik, Svitlana Smiian, Igor Gladchuk
Wiener Medizinische Wochenschrift.2024; 174(9-10): 199. CrossRef - UŞAQLIQ BORULARININ BİRİNCİLİ XƏRÇƏNGİ: DİAQNOSTİKASI VƏ MÜALİCƏSİNİN NƏTİCƏLƏRİ
D.G. Sumtsov, G.O. Sumtsov, N.I. Hyriavenko, S.A. Smiian, N.V. Kalashnyk, K.O. Sikora, N.M. Rozhkovska, I.Z. Gladchuk
Azerbaijan Medical Journal.2023; (4): 75. CrossRef - FEATURES OF ENDOMETRIUM STRUCTURE IN ALCOHOL-ABUSING HIV-INFECTED INDIVIDUALS
M. Lytvynenko
Inter Collegas.2021; 8(1): 52. CrossRef - Concurrent Clostridial Enteritis and Oviductal Adenocarcinoma with Carcinomatosis in an Adult Alpaca (Vicugna pacos)
Mandy Womble, Megan E. Schreeg, Allison Hoch, Enoch B. de Souza Meira, Derek Foster, Christopher Premanandan, Tatiane T. Negrão Watanabe
Journal of Comparative Pathology.2021; 189: 52. CrossRef - Problems of primary fallopian tube cancer diagnostics during and after surgery
D.G. Sumtsov, I.Z. Gladchuk, G.O. Sumtsov, N.I. Hyriavenko, M.S. Lyndin, V.V. Sikora, V.M. Zaporozhan
REPRODUCTIVE ENDOCRINOLOGY.2021; (59): 66. CrossRef
- Rare non-serous fallopian tube cancers: institutional experience and literature review
- WITHDRAWN:A Clinicopathologic Study of 220 Cases of Pulmonary Sclerosing Pneumocytoma in Korea: A Nationwide Survey
- Myunghee Kang, Seung Yeon Ha, Joung Ho Han, Mee Sook Roh, Se Jin Jang, Hee Jin Lee, Heae Surng Park, Geon Kook Lee, Kyo Young Lee, Jin-Haeng Chung, Yoo Duk Choi, Chang Hun Lee, Lucia Kim, Myoung Ja Chung, Soon Hee Jung, Gou Young Kim, Wan-Seop Kim
- Received April 4, 2018 Accepted July 9, 2018 Published online July 16, 2018
- DOI: https://doi.org/10.4132/jptm.2018.07.10 [Accepted]
- 5,658 View
- 63 Download
- Combined Hepatocellular Carcinoma and Neuroendocrine Carcinoma with Ectopic Secretion of Parathyroid Hormone: A Case Report and Review of the Literature
- Hyun Jung Kwon, Ji-Won Kim, Haeryoung Kim, YoungRok Choi, Soomin Ahn
- J Pathol Transl Med. 2018;52(4):232-237. Published online May 25, 2018
- DOI: https://doi.org/10.4132/jptm.2018.05.17
- 8,692 View
- 159 Download
- 17 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF - Primary combined hepatocellular carcinoma (HCC) and neuroendocrine carcinoma is a rare entity, and so is hypercalcemia due to ectopic parathyroid hormone (PTH) secretion by tumor. A 44-year old man with hepatitis B virus associated chronic liver disease presented with a hepatic mass. Hemihepatectomy discovered the mass as combined HCC and poorly differentiated cholangiocarcinoma. During adjuvant chemoradiation therapy, he presented with nausea, and multiple systemic metastases were found. Laboratory tests revealed hypercalcemia with markedly elevated PTH and neuron specific enolase. Parathyroid scan showed normal uptake in parathyroid glands, suggestive of ectopic PTH secretion. Subsequently, immunohistochemistry of neuroendocrine marker was performed on the primary lesion, and confirmed the neuroendocrine differentiation in non-HCC component. The patient died 71 days after surgery. This report may suggest the possibility of ectopic PTH secretion by neuroendocrine carcinoma of hepatic origin causing hypercalcemia. Caution for neuroendocrine differentiation should be exercised when diagnosing poorly differentiated HCC.
-
Citations
Citations to this article as recorded by- Mixed glandular neuroendocrine carcinoma of the endometrium with hypercalcemic crisis
Mei Luo, Xiaoxia Yu, Zhongpei Chen, Zhenhan Li
The American Journal of the Medical Sciences.2025; 369(2): 281. CrossRef - Combined Neuroendocrine Carcinoma and Hepatocellular Carcinoma of the Liver: Systematic Literature Review Suggests Implementing Biological Characterization to Optimize Therapeutic Strategy
Daniela Sambataro, Sandro Bellavia, Paolo Di Mattia, Danilo Centonze, Carmela Emmanuele, Annalisa Bonasera, Giuseppe Caputo, Andrea Maria Onofrio Quattrocchi, Ernesto Vinci, Vittorio Gebbia, Maria Rosaria Valerio
Cancers.2025; 17(7): 1074. CrossRef - Surgical Resection of Primary Hepatic Mixed Neuroendocrine-Non-Neuroendocrine Neoplasm: A Report of Three Cases
Ryosuke Toyonaka, Osamu Aramaki, Nao Yoshida, Yusuke Mitsuka, Masanori Nakamura, Shu Inagaki, Kaiki Murai, Toshiyuki Ishige, Ryusuke Tsujimura, Sumie Ohni, Shinobu Masuda, Hiroharu Yamashita, Yukiyasu Okamura
The Japanese Journal of Gastroenterological Surgery.2025; 58(6): 331. CrossRef - Case report: mixed large-cell neuroendocrine and hepatocellular carcinoma of the liver
Xin Gao, Heng Wang, Zheyu Niu, Meng Liu, Xiaohan Kong, Hongrui Sun, Chaoqun Ma, Huaqiang Zhu, Jun Lu, Xu Zhou
Frontiers in Oncology.2024;[Epub] CrossRef - Mixed Primary Hepatocellular Carcinoma and Hepatic Neuroendocrine Carcinoma: Case Report and Literature Review
Woo Young Shin, Keon Young Lee, Kyeong Deok Kim
Medicina.2023; 59(2): 418. CrossRef - Comparison of Metastatic Patterns Among Neuroendocrine Tumors, Neuroendocrine Carcinomas, and Nonneuroendocrine Carcinomas of Various Primary Organs
Hyung Kyu Park, Ghee Young Kwon
Journal of Korean Medical Science.2023;[Epub] CrossRef - Immunohistochemical characterization of a steroid-secreting oncocytic adrenal carcinoma responsible for paraneoplastic hyperparathyroidism
Magalie Haissaguerre, Estelle Louiset, Christofer C Juhlin, Adam Stenman, Christophe Laurent, Hélène Trouette, Hervé Lefebvre, Antoine Tabarin
European Journal of Endocrinology.2023; 188(4): K11. CrossRef - Neuroendocrine neoplasms of the biliary tree, liver and pancreas: a pathological approach
Claudio Luchini, Giuseppe Pelosi, Aldo Scarpa, Paola Mattiolo, Deborah Marchiori, Roberta Maragliano, Fausto Sessa, Silvia Uccella
Pathologica.2021; 113(1): 28. CrossRef - Contrast-Enhanced Ultrasound Findings of Hepatocellular Carcinoma With Neuroendocrine Carcinoma: A Case Report
Hong Wang, Dan Yang, Zhenru Wu, Yan Luo, Wenwu Ling
Frontiers in Medicine.2021;[Epub] CrossRef - Combined primary hepatic neuroendocrine carcinoma and hepatocellular carcinoma: case report and literature review
Akira Nakano, Kenichi Hirabayashi, Hiroshi Yamamuro, Taro Mashiko, Yoshihito Masuoka, Seiichiro Yamamoto, Soji Ozawa, Toshio Nakagohri
World Journal of Surgical Oncology.2021;[Epub] CrossRef - Hepatocellular carcinoma in patients with renal dysfunction: Pathophysiology, prognosis, and treatment challenges
Hsuan Yeh, Chung-Cheng Chiang, Tzung-Hai Yen
World Journal of Gastroenterology.2021; 27(26): 4104. CrossRef - Severe hypercalcaemia from ectopic intact parathyroid hormone secretion treated with continuous renal replacement therapy in a patient with two malignancies
Nathaniel Hocker, Maria Story, Alysa Lerud, Sarat Kuppachi
BMJ Case Reports.2021; 14(6): e242172. CrossRef - Parathyroid Carcinoma and Ectopic Secretion of Parathyroid hormone
Filomena Cetani, Elena Pardi, Claudio Marcocci
Endocrinology and Metabolism Clinics of North America.2021; 50(4): 683. CrossRef - Primary hepatic neuroendocrine cancer coexisted with hepatocellular carcinoma: a case report
Chikara Ebisutani, Seitetsu Yoon, Toshiki Hyodo, Takafumi Watanabe, Hirofumi Okada, Yutaka Shirakawa, Yoshio Sakamoto, Shigeya Hirohata
Kanzo.2020; 61(3): 122. CrossRef - Two-in-one: A pooled analysis of primary hepatic neuroendocrine carcinoma combined/collided with hepatocellular carcinoma
Jia-Xi Mao, Fei Teng, Ke-Yan Sun, Cong Liu, Guo-Shan Ding, Wen-Yuan Guo
Hepatobiliary & Pancreatic Diseases International.2020; 19(4): 399. CrossRef - Primary hepatic neuroendocrine carcinoma coexisting with distal cholangiocarcinoma
Qi Xin, Rong Lv, Cheng Lou, Zhe Ma, Gui-Qiu Liu, Qin Zhang, Hai-Bo Yu, Chuan-Shan Zhang
Medicine.2020; 99(26): e20854. CrossRef - Mixed hepatocellular carcinoma-neuroendocrine carcinoma—A diagnostic and therapeutic challenge
Nusrat Jahan, Irfan Warraich, Edwin Onkendi, Sanjay Awasthi
Current Problems in Cancer: Case Reports.2020; 1: 100020. CrossRef
- Mixed glandular neuroendocrine carcinoma of the endometrium with hypercalcemic crisis
- Multiple Neuroendocrine Tumors in Stomach and Duodenum in a Multiple Endocrine Neoplasia Type 1 Patient
- Bohyun Kim, Han-Kwang Yang, Woo Ho Kim
- J Pathol Transl Med. 2018;52(2):126-129. Published online December 21, 2017
- DOI: https://doi.org/10.4132/jptm.2017.09.16
- 8,775 View
- 145 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - A 67-year-old woman with a history of subtotal parathyroidectomy, distal pancreatectomy, and total splenectomy 23 years prior underwent surgical gastric resection for neuroendocrine tumors of the stomach and duodenum. Meticulous examination of the entire stomach and duodenum revealed multiple scattered, minute neuroendocrine tumors. To the best of our knowledge, this is the first case report of a patient diagnosed with gastroduodenal neuroendocrine tumors associated with multiple endocrine neoplasia type 1 (MEN 1) in whom complete histologic mapping of the whole gastrectomy specimen was performed. The presence of MEN 1–associated neuroendocrine tumors in the stomach is very rare, but should be considered in patients diagnosed with MEN 1 who present with a new tumor in the stomach.
-
Citations
Citations to this article as recorded by- A Case of Asymptomatic Multiple Endocrine Neoplasia Type I with Thymic Carcinoid
Suk Ki Park, Moon Won Lee, In Sub Han, Young Joo Park, Sung Yong Han, Joon Woo Park, Bong Eun Lee, Gwang Ha Kim, Sang Soo Kim
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2019; 19(1): 65. CrossRef
- A Case of Asymptomatic Multiple Endocrine Neoplasia Type I with Thymic Carcinoid
- Extramural Perineural Invasion in pT3 and pT4 Gastric Carcinomas
- Alejandro España-Ferrufino, Leonardo S. Lino-Silva, Rosa A. Salcedo-Hernández
- J Pathol Transl Med. 2018;52(2):79-84. Published online November 9, 2017
- DOI: https://doi.org/10.4132/jptm.2017.11.01
- 10,165 View
- 143 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Perineural invasion (PNI) is widely studied in malignant tumors, and its prognostic significance is well demonstrated. Most studies have focused on evaluating the mural PNI (mPNI); however, extramural PNI (ePNI) may influence the prognosis in gastric cancer. We evaluated the prognostic value of ePNI compared with mPNI in gastric cancer in this observational comparative cross-sectional study.
Methods
Seventy-three pT3 and pT4 gastric carcinomas with PNI were evaluated. Forty-eight (65.7%) were in the mPNI group and the remaining in the ePNI group.
Results
Clinicopathologic characteristics between the two groups were similar, except for the outcomes. The 5-year disease-specific survival (DSS) rate was 64% for the mPNI group and 50% for the ePNI group (p=.039), a difference that did not remain significant in multivariate analysis. The only independent adverse prognostic factor in multivariate analysis was the presence of lymph node metastasis (hazard ratio, 1.757; 95% confidence interval, 1.082 to 2.854; p=.023).
Conclusions
We demonstrated the prognostic effect of ePNI for DSS in surgically resected pT3–pT4 gastric cancer patients. ePNI could be considered in the staging and prognostic systems of gastric cancer to stratify patients with a high risk of recurrence. -
Citations
Citations to this article as recorded by- Investigation of Conditioned Media-Mediated Communication between Pancreatic Cancer Cells and Neurons
Didem Karakaş
Acta Medica Nicomedia.2025; 8(1): 15. CrossRef - Innervating 3D in vitro models: bioengineering and design blueprints
Mariana-Tomás de Carvalho, Margarida Henriques-Pereira, Maria V. Monteiro, Meriem Lamghari, João F. Mano, Vítor M. Gaspar
Trends in Biotechnology.2025; 43(11): 2743. CrossRef - Development and validation of a preoperative CT-based risk score integrating morphological and body composition parameters to predict recurrence-free survival in gastric cancer patients following curative surgery
Ruochen Cong, Jialei Ming, Ruonan Xu, Liyu Zhu, Xinyue Wang, Zhengqi Zhu
European Journal of Radiology.2025; 191: 112318. CrossRef - Comparison of 2D and 3D measured iodine concentration of gastric adenocarcinoma on spectral-CT and their relationship with perineural invasion
Tianxia Bei, Xiaoqiang Yao, Xuejun Chen, Yue Wu, Jing Li, Jinrong Qu
BMC Medical Imaging.2025;[Epub] CrossRef - Neural control of tumor immunity
Burak Kizil, Francesco De Virgiliis, Christoph Scheiermann
The FEBS Journal.2024; 291(21): 4670. CrossRef - Spectral CT-based nomogram for preoperative prediction of perineural invasion in locally advanced gastric cancer: a prospective study
Jing Li, Shuning Xu, Yi Wang, Mengjie Fang, Fei Ma, Chunmiao Xu, Hailiang Li
European Radiology.2023; 33(7): 5172. CrossRef - Crosstalk between cancer cells and the nervous system
Meng Huang, Gu Gong, Yicheng Deng, Xinmiao Long, Wenyong Long, Qing Liu, Wei Zhao, Rufu Chen
Medicine Advances.2023; 1(3): 173. CrossRef - Targeting tumor innervation: premises, promises, and challenges
Xinyu Li, Xueqiang Peng, Shuo Yang, Shibo Wei, Qing Fan, Jingang Liu, Liang Yang, Hangyu Li
Cell Death Discovery.2022;[Epub] CrossRef - Cancer-Associated Neurogenesis and Nerve-Cancer Cross-talk
Deborah A. Silverman, Vena K. Martinez, Patrick M. Dougherty, Jeffrey N. Myers, George A. Calin, Moran Amit
Cancer Research.2021; 81(6): 1431. CrossRef - Perineural Invasion and Postoperative Adjuvant Chemotherapy Efficacy in Patients With Gastric Cancer
Qing Tao, Wen Zhu, Xiaohui Zhao, Mei Li, Yongqian Shu, Deqiang Wang, Xiaoqin Li
Frontiers in Oncology.2020;[Epub] CrossRef - Perineural invasion as a predictive factor for survival outcome in gastric cancer patients: a systematic review and meta-analysis
Bochao Zhao, Wu Lv, Di Mei, Rui Luo, Shiyang Bao, Baojun Huang, Jie Lin
Journal of Clinical Pathology.2020; 73(9): 544. CrossRef - Consensus-Expressed CXCL8 and MMP9 Identified by Meta-Analyzed Perineural Invasion Gene Signature in Gastric Cancer Microarray Data
Xiuzhi Jia, Minjia Lu, Chen Rui, Ying Xiao
Frontiers in Genetics.2019;[Epub] CrossRef
- Investigation of Conditioned Media-Mediated Communication between Pancreatic Cancer Cells and Neurons
- Combined Adenosquamous and Large Cell Neuroendocrine Carcinoma of the Gallbladder
- Jiyoon Jung, Yang-Seok Chae, Chul Hwan Kim, Youngseok Lee, Jeong Hyeon Lee, Dong-Sik Kim, Young-Dong Yu, Joo Young Kim
- J Pathol Transl Med. 2018;52(2):121-125. Published online October 5, 2017
- DOI: https://doi.org/10.4132/jptm.2017.08.20
- 8,853 View
- 155 Download
- 12 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Large cell neuroendocrine carcinoma (LCNEC) of the gallbladder is extremely rare and usually combined with other type of malignancy, mostly adenocarcinoma. We report an unusual case of combined adenosquamous carcinoma and LCNEC of the gallbladder in a 54-year-old woman. A radical cholecystectomy specimen revealed a 4.3×4.0 cm polypoid mass in the fundus with infiltration of adjacent liver parenchyma. Microscopically, the tumor consisted of two distinct components. Adenosquamous carcinoma was predominant and abrupt transition from adenocarcinoma to squamous cell carcinoma was observed. LCNEC showed round cells with large, vesicular nuclei, abundant mitotic figures, and occasional pseudorosette formation. The patient received adjuvant chemotherapy. However, multiple liver metastases were identified at 3-month follow-up. Metastatic nodules were composed of LCNEC and squamous cell carcinoma components. Detecting LCNEC component is important in gallbladder cancer, because the tumor may require a different chemotherapy regimen and show early metastasis and poor prognosis.
-
Citations
Citations to this article as recorded by- Postoperative gastric cancer accompanied by large-cell neuroendocrine carcinoma: A case report
Zhiqin Chen, Jiang Liu, Jin Liu, Yinhang Wu, Jian Liu
Medicine.2025; 104(41): e44367. CrossRef - Does the size of the neuroendocrine-carcinoma component determine the prognosis of gallbladder cancer?
Ya-Fei Hu, Jun-Ke Wang, Wen-Jie Ma, Hai-Jie Hu, Han-Fei Gu, Fei Liu, Tian-Run Lv, Si-Qi Yang, Yu-Shi Dai, Rui-Qi Zou, Yan-Wen Jin, Fu-Yu Li
Frontiers in Endocrinology.2024;[Epub] CrossRef - Az epehólyag adenosquamosus daganata
Fanni Hegedűs, Anita Sejben
Orvosi Hetilap.2024; 165(49): 1945. CrossRef - Comparison of Metastatic Patterns Among Neuroendocrine Tumors, Neuroendocrine Carcinomas, and Nonneuroendocrine Carcinomas of Various Primary Organs
Hyung Kyu Park, Ghee Young Kwon
Journal of Korean Medical Science.2023;[Epub] CrossRef - Clinical features and outcomes analysis of Gallbladder neuroendocrine carcinoma
Man Jiang, Yijing Zhang
Journal of Cancer Research and Therapeutics.2023; 19(4): 910. CrossRef - Primary mixed large cell neuroendocrine carcinoma and adenocarcinoma of the gallbladder: A case report and literature review
Tingting Yu, Shike Li, Zhuo Zhang
Asian Journal of Surgery.2022; 45(11): 2336. CrossRef - Mixed neuroendocrine-non-neuroendocrine neoplasm of the gallbladder: case report and literature review
Xu Ren, Hong Jiang, Kan Sun, Xufu Qin, Yongping Qu, Tian Xia, Yan Chen
Diagnostic Pathology.2022;[Epub] CrossRef - Neuroendocrine Neoplasms of the Gallbladder: A Clinicopathological Analysis of 13 Patients and a Review of the Literature
Pengyan Wang, Jingci Chen, Ying Jiang, Congwei Jia, Junyi Pang, Shan Wang, Xiaoyan Chang, Oronzo Brunetti
Gastroenterology Research and Practice.2021; 2021: 1. CrossRef - Gallbladder Mixed Neuroendocrine-Non-neuroendocrine Neoplasm (MiNEN) Arising in Intracholecystic Papillary Neoplasm: Clinicopathologic and Molecular Analysis of a Case and Review of the Literature
Amedeo Sciarra, Edoardo Missiaglia, Mounir Trimech, Emmanuel Melloul, Jean-Philippe Brouland, Christine Sempoux, Stefano La Rosa
Endocrine Pathology.2020; 31(1): 84. CrossRef - Mixed neuroendocrine-non-neuroendocrine carcinoma of gallbladder: case report
Adam Skalický, Lucie Vištejnová, Magdaléna Dubová, Tomáš Malkus, Tomáš Skalický, Ondřej Troup
World Journal of Surgical Oncology.2019;[Epub] CrossRef
- Postoperative gastric cancer accompanied by large-cell neuroendocrine carcinoma: A case report
- Loss of Progesterone Receptor Expression Is an Early Tumorigenesis Event Associated with Tumor Progression and Shorter Survival in Pancreatic Neuroendocrine Tumor Patients
- Sung Joo Kim, Soyeon An, Jae Hoon Lee, Joo Young Kim, Ki-Byung Song, Dae Wook Hwang, Song Cheol Kim, Eunsil Yu, Seung-Mo Hong
- J Pathol Transl Med. 2017;51(4):388-395. Published online June 8, 2017
- DOI: https://doi.org/10.4132/jptm.2017.03.19
- 9,009 View
- 138 Download
- 18 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Pancreatic neuroendocrine tumors (PanNETs) are the second most common pancreatic neoplasms and there is no well-elucidated biomarker to stratify their detection and prognosis. Previous studies have reported that progesterone receptor (PR) expression status was associated with poorer survival in PanNET patients.
Methods
To validate previous studies, PR protein expression was assessed in 21 neuroendocrine microadenomas and 277 PanNETs and compared with clinicopathologic factors including patient survival.
Results
PR expression was gradually decreased from normal islets (49/49 cases, 100%) to neuroendocrine microadenoma (14/21, 66.6%) to PanNETs (60/277, 21.3%; p < .001). PanNETs with loss of PR expression were associated with increased tumor size (p < .001), World Health Organization grade (p = .001), pT classification (p < .001), perineural invasion (p = .028), lymph node metastasis (p = .004), activation of alternative lengthening of telomeres (p = .005), other peptide hormonal expression (p < .001) and ATRX/DAXX expression (p = .015). PanNET patients with loss of PR expression (5-year survival rate, 64.1%) had significantly poorer recurrence-free survival outcomes than those with intact PR expression (90%) by univariate (p = .012) but not multivariate analyses. Similarly, PanNET patients with PR expression loss (5-year survival rate, 76%) had significantly poorer overall survival by univariate (p = .015) but not multivariate analyses.
Conclusions
Loss of PR expression was noted in neuroendocrine microadenomas and was observed in the majority of PanNETs. This was associated with increased grade, tumor size, and advanced pT and pN classification; and was correlated with decreased patient survival time by univariate but not multivariate analyses. Loss of PR expression can provide additional information on shorter disease-free survival in PanNET patients. -
Citations
Citations to this article as recorded by- Incidence and Prognostic Implications of Lymphovascular Invasion in Node‐Negative Pancreatic Neuroendocrine Tumors: Results From the US Neuroendocrine Study Group
Kota Sahara, Diamantis I. Tsilimigras, Yuki Homma, Jun Kawashima, Shishir K. Maithel, Flavio Rocha, Sharon Weber, Ryan Fields, Kamran Idrees, George A. Poultsides, Cliff Cho, Itaru Endo, Timothy M. Pawlik
Journal of Surgical Oncology.2025; 131(3): 465. CrossRef - Sex Differences in the Survival of Patients with Neuroendocrine Neoplasms: A Comparative Study of Two National Databases
Mohamed Mortagy, Marie Line El Asmar, Kandiah Chandrakumaran, John Ramage
Cancers.2024; 16(13): 2376. CrossRef - Association Between Female Sex and Better Survival in Gastroenteropancreatic Neuroendocrine Tumors
Jeremy Chang, Mohammed O. Suraju, Catherine G. Tran, Carlos H.F. Chan, Po Hien Ear, James R. Howe, Scott K. Sherman
Journal of Surgical Research.2024; 302: 53. CrossRef - Venous invasion and lymphatic invasion are correlated with the postoperative prognosis of pancreatic neuroendocrine neoplasm
Sho Kiritani, Junichi Arita, Yuichiro Mihara, Rihito Nagata, Akihiko Ichida, Yoshikuni Kawaguchi, Takeaki Ishizawa, Nobuhisa Akamatsu, Junichi Kaneko, Kiyoshi Hasegawa
Surgery.2023; 173(2): 365. CrossRef - Combined Infiltrative Macroscopic Growth Pattern and Infiltrative Microscopic Tumor Border Status Is a Novel Surrogate Marker of Poor Prognosis in Patients With Pancreatic Neuroendocrine Tumor
Bokyung Ahn, Joo Young Kim, Seung-Mo Hong
Archives of Pathology & Laboratory Medicine.2023; 147(1): 100. CrossRef - HORMONET: a phase II trial of tamoxifen for estrogen/progesterone receptor-positive neuroendocrine tumors
Milton J. Barros, Jonathan Strosberg, Taymeyah Al-Toubah, Victor Hugo F. de Jesus, Lais Durant, Celso A. Mello, Tiago C. Felismino, Louise De Brot, Rodrigo G. Taboada, Mauro D. Donadio, Rachel P. Riechelmann
Therapeutic Advances in Medical Oncology.2023;[Epub] CrossRef - Diagnostic and Prognostic Impact of Progesterone Receptor Immunohistochemistry: A Study Evaluating More Than 16,000 Tumors
Florian Viehweger, Lisa-Marie Tinger, David Dum, Natalia Gorbokon, Anne Menz, Ria Uhlig, Franziska Büscheck, Andreas M. Luebke, Claudia Hube-Magg, Andrea Hinsch, Doris Höflmayer, Christoph Fraune, Patrick Lebok, Sören Weidemann, Maximilian Lennartz, Frank
Analytical Cellular Pathology.2022; 2022: 1. CrossRef - Prognostic Nomograms to Predict Overall Survival and Cancer-Specific Survival of Patients With Pancreatic Neuroendocrine Tumors
Zuoli Song, Sumei Wang, Yujing Wu, Jinjuan Zhang, Shuye Liu
Pancreas.2021; 50(3): 414. CrossRef - Pancreatic High-Grade Neuroendocrine Neoplasms in the Korean Population: A Multicenter Study
Haeryoung Kim, Soyeon An, Kyoungbun Lee, Sangjeong Ahn, Do Youn Park, Jo-Heon Kim, Dong-Wook Kang, Min-Ju Kim, Mee Soo Chang, Eun Sun Jung, Joon Mee Kim, Yoon Jung Choi, So-Young Jin, Hee Kyung Chang, Mee-Yon Cho, Yun Kyung Kang, Myunghee Kang, Soomin Ahn
Cancer Research and Treatment.2020; 52(1): 263. CrossRef - Systemic distribution of progesterone receptor subtypes in human tissues
Teeranut Asavasupreechar, Ryoko Saito, Yasuhiro Miki, Dean P. Edwards, Viroj Boonyaratanakornkit, Hironobu Sasano
The Journal of Steroid Biochemistry and Molecular Biology.2020; 199: 105599. CrossRef - Progesteron receptor expression in insulin producing cells of neuroendocrine neoplasms
Tomoyoshi Tachibana, Atsuko Kasajima, Takeshi Aoki, Tomoaki Tabata, Keely McNamara, Samaneh Yazdani, Sato Satoko, Fumiyoshi Fujishima, Fuyuhiko Motoi, Michiaki Unno, Hironobu Sasano
The Journal of Steroid Biochemistry and Molecular Biology.2020; 201: 105694. CrossRef - Prognostic and predictive factors on overall survival and surgical outcomes in pancreatic neuroendocrine tumors: recent advances and controversies
Lingaku Lee, Tetsuhide Ito, Robert T Jensen
Expert Review of Anticancer Therapy.2019; 19(12): 1029. CrossRef - Immunohistochemistry, carcinomas of unknown primary, and incidence rates
Edward B. Stelow, Hadi Yaziji
Seminars in Diagnostic Pathology.2018; 35(2): 143. CrossRef - Carbonic anhydrase 9 expression in well-differentiated pancreatic neuroendocrine neoplasms might be associated with aggressive behavior and poor survival
Joo Young Kim, Sang Hwa Lee, Soyeon An, Sung Joo Kim, You-Na Sung, Ki-Byung Song, Dae Wook Hwang, Song Cheol Kim, Seung-Mo Hong
Virchows Archiv.2018; 472(5): 739. CrossRef - Prognostic value of progesterone receptor in solid pseudopapillary neoplasm of the pancreas: evaluation of a pooled case series
Feiyang Wang, Zibo Meng, Shoukang Li, Yushun Zhang, Heshui Wu
BMC Gastroenterology.2018;[Epub] CrossRef - Estrogens modulate progesterone receptor expression and may contribute to progesterone-mediated apoptotic β-cell death
Viviane Abreu Nunes
Endocrinology&Metabolism International Journal.2018;[Epub] CrossRef
- Incidence and Prognostic Implications of Lymphovascular Invasion in Node‐Negative Pancreatic Neuroendocrine Tumors: Results From the US Neuroendocrine Study Group
- Diagnostic Significance of Cellular Neuroglial Tissue in Ovarian Immature Teratoma
- Yun Chai, Chang Gok Woo, Joo-Young Kim, Chong Jai Kim, Shin Kwang Khang, Jiyoon Kim, In Ah Park, Eun Na Kim, Kyu-Rae Kim
- J Pathol Transl Med. 2017;51(1):49-55. Published online October 14, 2016
- DOI: https://doi.org/10.4132/jptm.2016.09.19
- 18,696 View
- 491 Download
- 6 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Immature teratoma (IT) is a tumor containing immature neuroectodermal tissue, primarily in the form of neuroepithelial tubules. However, the diagnosis of tumors containing only cellular neuroglial tissue (CNT) without distinct neuroepithelial tubules is often difficult, since the histological characteristics of immature neuroectodermal tissues remain unclear. Here, we examined the significance of CNT and tried to define immature neuroectodermal tissues by comparing the histological features of neuroglial tissues between mature teratoma (MT) and IT.
Methods
The histological features of neuroglial tissue, including the cellularity, border between the neuroglial and adjacent tissues, cellular composition, mitotic index, Ki-67 proliferation rate, presence or absence of tissue necrosis, vascularity, and endothelial hyperplasia, were compared between 91 MT and 35 IT cases.
Results
CNTs with a cellularity grade of ≥ 2 were observed in 96% of IT cases and 4% of MT cases (p < .001); however, CNT with a cellularity grade of 3 in MT cases was confined to the histologically distinct granular layer of mature cerebellar tissue. Moreover, CNT in IT exhibited significantly higher rates of Ki-67 proliferation, mitoses, and necrosis than those in MT (p < .001). Furthermore, an infiltrative border of neuroglial tissue and glomeruloid endothelial hyperplasia were significantly more frequent in IT cases than in MT cases (p < .001).
Conclusions
Our results suggest that if CNT with a cellularity grade of ≥ 2 is not a component of cerebellar tissue, such cases should be diagnosed as IT containing immature neuroectodermal tissue, particularly if they exhibit an infiltrative border, mitoses, necrosis, and increased Ki-67 proliferation. -
Citations
Citations to this article as recorded by- An Atypical Presentation of a Pediatric Mature Teratoma: A Case Report and Review of the Literature
Ahmed M Othman, Abdulaziz A Abu Alnasr, Reem E Kordi, Shahad A Abu Alnasr
Cureus.2024;[Epub] CrossRef - Immature Teratoma: Diagnosis and Management—A Review of the Literature
Liviu Moraru, Melinda-Ildiko Mitranovici, Diana Maria Chiorean, Marius Coroș, Raluca Moraru, Ioan Emilian Oală, Sabin Gligore Turdean
Diagnostics.2023; 13(9): 1516. CrossRef - Congenital Immature Grade ΙΙΙ Teratoma of the Neck: A Case Report
Nazneen Liaqat, Israr Ud Din, Zeeshan Ali, Majid Rashid, Afsheen Liaqat
Cureus.2023;[Epub] CrossRef - Benign ovarian teratoma in the dog with predominantly nervous tissue: A case report
P Makovicky, AV Makarevich, P Makovicky, A Seidavi, L Vannucci, K Rimarova
Veterinární medicína.2022; 67(2): 99. CrossRef - Fascin as a Useful Marker for Identifying Neural Components in Immature Teratomas of Human Ovary and Those Derived From Murine Embryonic Stem Cells
Ryunosuke Umehara, Atsushi Kurata, Masakatsu Takanashi, Hirotsugu Hashimoto, Koji Fujita, Toshitaka Nagao, Masahiko Kuroda
International Journal of Gynecological Pathology.2019; 38(4): 377. CrossRef - Cerebellar Differentiation in Ovarian Teratoma: A Report of 6 Cases
Colin J.R. Stewart, Maxine L. Crook
International Journal of Gynecological Pathology.2018; 37(4): 316. CrossRef - Mitotic activity of epithelia of ectoand entodermal types in spontaneous and experimental teratomas of mice
Pavel A. Dyban
Medical academic journal.2018; 18(4): 42. CrossRef - Ovarian cystectomy in the treatment of apparent early-stage immature teratoma
Ting Zhao, Yan Liu, Xiao Wang, Hao Zhang, Yuan Lu
Journal of International Medical Research.2017; 45(2): 771. CrossRef
- An Atypical Presentation of a Pediatric Mature Teratoma: A Case Report and Review of the Literature
- Overview of IgG4-Related Tubulointerstitial Nephritis and Its Mimickers
- Hyeon Joo Jeong, Su-Jin Shin, Beom Jin Lim
- J Pathol Transl Med. 2016;50(1):26-36. Published online December 14, 2015
- DOI: https://doi.org/10.4132/jptm.2015.11.09
- 14,149 View
- 233 Download
- 13 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF - Tubulointerstitial nephritis (TIN) is the most common form of renal involvement in IgG4-related disease. It is characterized by a dominant infiltrate of IgG4-positive plasma cells in the interstitium and storiform fibrosis. Demonstration of IgG4-positive plasma cells is essential for diagnosis, but the number of IgG4-positive cells and the ratio of IgG4-positive/IgG-positive plasma cells may vary from case to case and depending on the methods of tissue sampling even in the same case. IgG4-positive plasma cells can be seen in TIN associated with systemic lupus erythematosus, Sjögren syndrome, or anti-neutrophil cytoplasmic antibody–associated vasculitis, which further add diagnostic confusion and difficulties. To have a more clear view of IgG4-TIN and to delineate differential points from other TIN with IgG4-positive plasma cell infiltrates, clinical and histological features of IgG4-TIN and its mimickers were reviewed. In the rear part, cases suggesting overlap of IgG4-TIN and its mimickers and glomerulonephritis associated with IgG4-TIN were briefly described.
-
Citations
Citations to this article as recorded by- Glycosylation in kidney diseases
Yingying Ling, Fei Cai, Tao Su, Yi Zhong, Ling Li, Bo Meng, Guisen Li, Meng Gong, Hao Yang, Xinfang Xie, Zhenyu Sun, Yang Zhao, Fang Liu, Yong Zhang
Precision Clinical Medicine.2025;[Epub] CrossRef - IgG4-related kidney disease: Clinicopathologic features, differential diagnosis, and mimics
Sarwat I. Gilani, Alessia Buglioni, Lynn D. Cornell
Seminars in Diagnostic Pathology.2024; 41(2): 88. CrossRef - Utilizing Immunoglobulin G4 Immunohistochemistry for Risk Stratification in Patients with Papillary Thyroid Carcinoma Associated with Hashimoto Thyroiditis
Faridul Haq, Gyeongsin Park, Sora Jeon, Mitsuyoshi Hirokawa, Chan Kwon Jung
Endocrinology and Metabolism.2024; 39(3): 468. CrossRef - IgG4-assoziierte Nierenerkrankungen
Christina Thompson, Frank O. Henes, Oliver M. Steinmetz, Simon Melderis
Die Nephrologie.2023; 18(4): 249. CrossRef - Concurrent anti-neutrophil cytoplasmic antibody-associated glomerulonephritis and IgG4-associated tubulointerstitial nephritis with C3 glomerulonephritis
Jianan Feng, Jinyu Yu, Xueyao Wang, Yue Wang, Yang Liu, Zhonggao Xu, Weixia Sun
Medicine.2020; 99(5): e18857. CrossRef - A case of eosinophilic granulomatosis with polyangiitis as a mimicker of IgG4-related disease
Ryuichiro Kanda, Satoshi Kubo, Kazuhisa Nakano, Akio Kawabe, Aya Nawata, Kentaro Hanami, Shingo Nakayamada, Yoshiya Tanaka
Modern Rheumatology Case Reports.2020; 4(2): 278. CrossRef - Renal tubular acidosis as the initial presentation of Sjögren’s syndrome
Karen Ho, Pouneh Dokouhaki, Mark McIsaac, Bhanu Prasad
BMJ Case Reports.2019; 12(8): e230402. CrossRef - Hypocomplementemic interstitial nephritis with long-term follow-up
Alyssa Penning, Claire Kassakian, Donald C Houghton, Nicole K Andeen
Journal of Clinical Nephrology.2019; 3(1): 042. CrossRef - Immunoglobulin G4-related kidney diseases: An updated review
Maurizio Salvadori, Aris Tsalouchos
World Journal of Nephrology.2018; 7(1): 29. CrossRef - Systemic lupus erythematosus in a patient with an organic lesion of the central nervous system: practicaldifferential diagnosis
E. V. Lebedeva, M. V. Novoseltsev, A. N. Lvov, I. V. Khamaganova
Klinicheskaya dermatologiya i venerologiya.2018; 17(6): 21. CrossRef - Concurrent IgG4-related tubulointerstitial nephritis and IgG4 myeloperoxidase-anti-neutrophil cytoplasmic antibody positive crescentic glomerulonephritis
Tao Su, Li Yang, Zhao Cui, Su-xia Wang, Ming-hui Zhao
Medicine.2017; 96(20): e6707. CrossRef - IgG4-Related Kidney Disease: Report of a Case Presenting as a Renal Mass
Daniele Bianchi, Luca Topazio, Gabriele Gaziev, Valerio Iacovelli, Pierluigi Bove, Alessandro Mauriello, Enrico Finazzi Agrò
Case Reports in Surgery.2017; 2017: 1. CrossRef
- Glycosylation in kidney diseases
- Dysembryoplastic Neuroepithelial Tumors
- Yeon-Lim Suh
- J Pathol Transl Med. 2015;49(6):438-449. Published online October 23, 2015
- DOI: https://doi.org/10.4132/jptm.2015.10.05
- 16,468 View
- 294 Download
- 26 Web of Science
- 32 Crossref
-
 Abstract
Abstract
 PDF
PDF - Dysembryoplastic neuroepithelial tumor (DNT) is a benign glioneuronal neoplasm that most commonly occurs in children and young adults and may present with medically intractable, chronic seizures. Radiologically, this tumor is characterized by a cortical topography and lack of mass effect or perilesional edema. Partial complex seizures are the most common presentation. Three histologic subtypes of DNTs have been described. Histologically, the recognition of a unique, specific glioneuronal element in brain tumor samples from patients with medically intractable, chronic epilepsy serves as a diagnostic feature for complex or simple DNT types. However, nonspecific DNT has diagnostic difficulty because its histology is indistinguishable from conventional gliomas and because a specific glioneuronal element and/or multinodularity are absent. This review will focus on the clinical, radiographic, histopathological, and immunohistochemical features as well as the molecular genetics of all three variants of DNTs. The histological and cytological differential diagnoses for this lesion, especially the nonspecific variant, will be discussed.
-
Citations
Citations to this article as recorded by- A Case of Dysembryoplastic Neuroepithelial Tumor in an HIV-Positive Adult: Diagnostic Lessons for Clinicians
Mariana Lobo, Susana Viana, Andreia Sá Lima, Isabel Monteiro, Carolina M Cerqueira, Frederico Duarte, Luís M Ribeiro, Sara Camões
Cureus.2026;[Epub] CrossRef - An Imaging Review of Common Pediatric Brain Tumors
Joseph Yang, Brandon Collins, Matthew Beniuk, Alexandra Hodder, Dani Bahnam, Angela Pickles
Roentgen Ray Review.2025;[Epub] CrossRef - Ruptured intratumoral arteriovenous malformation in a patient with dysembryoplastic neuroepithelial tumor: A case report
Takashi Aoka, Masaaki Nishimoto, Hideki Ogiwara
Surgical Neurology International.2025; 16: 375. CrossRef - Pediatric Neuroglial Tumors: A Review of Ependymoma and Dysembryoplastic Neuroepithelial Tumor
Melissa Arfuso, Sandeepkumar Kuril, Harshal Shah, Derek Hanson
Pediatric Neurology.2024; 156: 139. CrossRef - From bedside to bench: New insights in epilepsy‐associated tumors based on recent classification updates and animal models on brain tumor networks
Silvia Cases‐Cunillera, Lea L. Friker, Philipp Müller, Albert J. Becker, Gerrit H. Gielen
Molecular Oncology.2024; 18(12): 2951. CrossRef - Imaging of pediatric glioneuronal and neuronal tumors
Vivek Pai, Suzanne Laughlin, Birgit Ertl-Wagner
Child's Nervous System.2024; 40(10): 3007. CrossRef - Dysembryoplastic Neuroepithelial Tumor: A Case Report of A Benign Intracranial Lesion Masquerading as Seizure Disorder
Garima S Agarwal, Anil K Agrawal, Daksh Singhal, Jayashree Bhawani
Cureus.2024;[Epub] CrossRef - Super T2-FLAIR mismatch sign: a prognostic imaging biomarker for non-enhancing astrocytoma, IDH-mutant
Iori Ozono, Shumpei Onishi, Ushio Yonezawa, Akira Taguchi, Novita Ikbar Khairunnisa, Vishwa Jeet Amatya, Fumiyuki Yamasaki, Yukio Takeshima, Nobutaka Horie
Journal of Neuro-Oncology.2024; 169(3): 571. CrossRef - Genotype-relevant neuroimaging features in low-grade epilepsy-associated tumors
Keiya Iijima, Hiroyuki Fujii, Fumio Suzuki, Kumiko Murayama, Yu-ichi Goto, Yuko Saito, Terunori Sano, Hiroyoshi Suzuki, Hajime Miyata, Yukio Kimura, Takuma Nakashima, Hiromichi Suzuki, Masaki Iwasaki, Noriko Sato
Frontiers in Neurology.2024;[Epub] CrossRef - Extra-temporal pediatric low-grade gliomas and epilepsy
José Hinojosa, Victoria Becerra, Santiago Candela-Cantó, Mariana Alamar, Diego Culebras, Carlos Valencia, Carlos Valera, Jordi Rumiá, Jordi Muchart, Javier Aparicio
Child's Nervous System.2024; 40(10): 3309. CrossRef - Atypical Presentation of Dysembryoplastic Neuroepithelial Tumor
Varis S. Khalilov, Aleksey N. Kislyakov, Natalia A. Medvedeva, Natalia S. Serova
Annals of Clinical and Experimental Neurology.2024; 18(3): 109. CrossRef - Unusual low-grade neuroepithelial tumour in a child
Leia Salongo, Ali Nael, Pournima Navalkele, John Ross Crawford
BMJ Case Reports.2024; 17(10): e262692. CrossRef - Glioneuronal and Neuronal Tumors: Who? When? Where? An Update Based on the 2021 World Health Organization Classification
A.S. Ayres, G.A. Bandeira, S.F. Ferraciolli, J.T. Takahashi, R.A. Moreno, L.F. de Souza Godoy, Y.R. Casal, L.G.C.A. de Lima, F.P. Frasseto, L.T. Lucato
Neurographics.2023; 13(1): 1. CrossRef - Biological functions of the Olig gene family in brain cancer and therapeutic targeting
Jenny I. Szu, Igor F. Tsigelny, Alexander Wojcinski, Santosh Kesari
Frontiers in Neuroscience.2023;[Epub] CrossRef - Aspekte der Bildgebung des Hippokampus
Isabela S. Alves, Artur M. N. Coutinho, Ana Vieira, Bruno P. Rocha, Ula L. Passos, Vinicius T. Gonçalves, Paulo D. S. Silva, Malia X. Zhan, Paula C. Pinho, Daniel S. Delgado, Marcos F. L. Docema, Hae W. Lee, Bruno A. Policeni, Claudia C. Leite, Maria G. M
Neuroradiologie Scan.2023; 13(03): 197. CrossRef - T2-FLAIR Mismatch Sign in Pediatric Low-Grade Glioma
M.W. Wagner, L. Nobre, K. Namdar, F. Khalvati, U. Tabori, C. Hawkins, B.B. Ertl-Wagner
American Journal of Neuroradiology.2023; 44(7): 841. CrossRef - Clinicopathological features of dysembryoplastic neuroepithelial tumor: a case series
Shabina Rahim, Nasir Ud Din, Jamshid Abdul-Ghafar, Qurratulain Chundriger, Poonum Khan, Zubair Ahmad
Journal of Medical Case Reports.2023;[Epub] CrossRef - Imaging Aspects of the Hippocampus
Isabela S. Alves, Artur M. N. Coutinho, Ana P. F. Vieira, Bruno P. Rocha, Ula L. Passos, Vinicius T. Gonçalves, Paulo D. S. Silva, Malia X. Zhan, Paula C. Pinho, Daniel S. Delgado, Marcos F. L. Docema, Hae W. Lee, Bruno A. Policeni, Claudia C. Leite, Mari
RadioGraphics.2022; 42(3): 822. CrossRef - Dysembryoplastic neuroepithelial tumors: A single-institutional series with special reference to glutamine synthetase expression
Chiara Caporalini, Mirko Scagnet, Selene Moscardi, Gioia Di Stefano, Gianna Baroni, Flavio Giordano, Federico Mussa, Carmen Barba, Iacopo Sardi, Lorenzo Genitori, Anna Maria Buccoliero
Annals of Diagnostic Pathology.2021; 54: 151774. CrossRef - Unusual case of occipital lobe dysembryoplastic neuroepithelial tumour with GNAi1-BRAF fusion
Jennifer H Yang, Denise M Malicki, Michael L Levy, John Ross Crawford
BMJ Case Reports.2021; 14(1): e241440. CrossRef - Malformations of Cortical Development, Cognitive Involvementand Epilepsy: A Single Institution Experience in 19 Young Patients
Valeria Venti, Maria Chiara Consentino, Pierluigi Smilari, Filippo Greco, Claudia Francesca Oliva, Agata Fiumara, Raffaele Falsaperla, Martino Ruggieri, Piero Pavone
Children.2021; 8(8): 637. CrossRef - A Case of Dysembryoplastic Neuroepithelial Tumor in an Adolescent Male
Marcel Yibirin, Diana De Oliveira, Isabella Suarez, Gabriela Lombardo, Carlos Perez
Cureus.2021;[Epub] CrossRef - Clinical and histopathological profile of dysembryoplastic neuroepithelial tumor
Pooja Gupta, Fouzia Siraj, Akanksha Malik, K. B. Shankar
Journal of Cancer Research and Therapeutics.2021; 17(4): 912. CrossRef - Neuroradiological and pathomorphological features of epilepsy associated brain tumors
V. S. Khalilov, A. A. Kholin, A. N. Kisyakov, N. A. Medvedeva, B. R. Bakaeva
Diagnostic radiology and radiotherapy.2021; 12(2): 7. CrossRef - Evaluación prequirúrgica mediante resonancia magnética funcional en pacientes con tumores neuroepiteliales disembrioplásicos: una serie de casos
Natalia García-Casares, Francisco Alfaro-Rubio, José Ramón Ramos-Rodríguez, Álvaro Ocaña-Ledesma, Bernarda Márquez-Márquez, Victoria E. Fernández-Sánchez, Guillermo Ibáñez-Botella, Miguel Ángel Arráez-Sánchez, Pedro J. Serrano-Castro
Neurocirugía.2020; 31(4): 158. CrossRef - Features of the neuroradiological picture of ganglioglioma on the example of 20 clinical cases
V.S. Khalilov, A.A. Kholin, Kh.Sh. Gazdieva, A.N. Kislyakov, N.N. Zavadenko
Zhurnal nevrologii i psikhiatrii im. S.S. Korsakova.2020; 120(11): 90. CrossRef - Malignant Glial Neuronal Tumors After West Nile Virus Neuroinvasive Disease: A Coincidence or a Clue?
Akanksha Sharma, Marie F. Grill, Scott Spritzer, A. Arturo Leis, Mark Anderson, Parminder Vig, Alyx B. Porter
The Neurohospitalist.2019; 9(3): 160. CrossRef - Particularities in differential diagnostics of epileptogenic brain malformations on the low-field MRI-device
V. S. Khalilov, A. A. Kholin, B. R. Bakaeva, M. Yu. Bobylova, Kh. Sh. Gazdieva
Russian Journal of Child Neurology.2019; 13(4): 23. CrossRef - Dysembryoplastic Neuroepithelial Tumors: What You Need to Know
Sabino Luzzi, Angela Elia, Mattia Del Maestro, Samer K. Elbabaa, Sergio Carnevale, Francesco Guerrini, Massimo Caulo, Patrizia Morbini, Renato Galzio
World Neurosurgery.2019; 127: 255. CrossRef - The miR‐139‐5p regulates proliferation of supratentorial paediatric low‐grade gliomas by targeting the PI3K/AKT/mTORC1 signalling
G. Catanzaro, Z. M. Besharat, E. Miele, M. Chiacchiarini, A. Po, A. Carai, C. E. Marras, M. Antonelli, M. Badiali, A. Raso, S. Mascelli, D. Schrimpf, D. Stichel, M. Tartaglia, D. Capper, A. von Deimling, F. Giangaspero, A. Mastronuzzi, F. Locatelli, E. Fe
Neuropathology and Applied Neurobiology.2018; 44(7): 687. CrossRef - Dysembryoplastic Neuroectodermal Tumor: An Analysis from the Surveillance, Epidemiology, and End Results Program, 2004–2013
Ha Son Nguyen, Ninh Doan, Michael Gelsomino, Saman Shabani
World Neurosurgery.2017; 103: 380. CrossRef - Common Histologically Benign Tumors of the Brain
Roy E. Strowd, Jaishri O. Blakeley
Continuum.2017; 23(6): 1680. CrossRef
- A Case of Dysembryoplastic Neuroepithelial Tumor in an HIV-Positive Adult: Diagnostic Lessons for Clinicians
- Neuroendocrine Tumors of the Female Reproductive Tract: A Literature Review
- Yi Kyeong Chun
- J Pathol Transl Med. 2015;49(6):450-461. Published online October 13, 2015
- DOI: https://doi.org/10.4132/jptm.2015.09.20
- 18,943 View
- 280 Download
- 28 Web of Science
- 29 Crossref
-
 Abstract
Abstract
 PDF
PDF - Neuroendocrine tumors of the female reproductive tract are a heterogeneous group of neoplasms that display various histologic findings and biologic behaviors. In this review, the classification and clinicopathologic characteristics of neuroendocrine tumors of the female reproductive tract are described. Differential diagnoses are discussed, especially for non-neuroendocrine tumors showing high-grade nuclei with neuroendocrine differentiation. This review also discusses recent advances in our pathogenetic understanding of these disorders.
-
Citations
Citations to this article as recorded by- Mixed neuroendocrine-non-neuroendocrine neoplasm (MiNEN) of the cervix in a 38-year-old female: a case report and review of literature
Josh Matthew B. Chen, Denise B. Andal, Benedict Jose P. Canora, Claire Anne Therese M. Hemedez
Human Pathology Reports.2026; 43: 300815. CrossRef - Neuroendocrine Neoplasms of the Gastrointestinal Tract: Morphology, WHO 2022 Grading, and Prognostic Perspectives
Hussein Qasim, Shaima' Dibian, Mohammad Abu Shugaer, Karis Khattab, Mudhaffer Touqan, Matteo Luigi Giuseppe Leoni , Giustino Varrassi
Cureus.2026;[Epub] CrossRef - A rare case report of primary ovarian carcinoid presenting with constipation
Xiaofeng Deng, Qian Huang, Bangfang Xie, Hailong Huang, Jianguo Chen
Frontiers in Oncology.2025;[Epub] CrossRef - Clinical, pathological characteristics, and therapeutic outcomes of primary ovarian carcinoid tumors: a case series of 15 cases
Xinyue Dai, Suidan Chen, Simeng Yang
World Journal of Surgical Oncology.2025;[Epub] CrossRef - Smart Red Blood Cell Carriers: A Nanotechnological Approach to Cancer Drug Delivery
Ioannis Tsamesidis, Georgios Dryllis, Sotirios P. Fortis, Andreas Sphicas, Vasiliki Konstantinidou, Maria Chatzidimitriou, Stella Mitka, Maria Trapali, Petros Skepastianos, Anastasios G. Kriebardis, Ilias Pessach
Current Issues in Molecular Biology.2025; 47(9): 711. CrossRef - Imaging of Gynecologic Neuroendocrine Tumors: A Case-Based Pictorial Essay
Ana Paula Bavaresco, Ulysses S. Torres, Mayara S. Cruz, Vitor V.C. Machado, Cynthia L.P. Borborema, Giovanna S. Torre, Jhonata Soares Da Silva, Tulio A. Kawai, Gustavo R.A. Focchi, Eduardo O. Pacheco, Aley Talans, Daniel Bekhor, Ana Paula C. Moura, Lucas
Seminars in Ultrasound, CT and MRI.2025;[Epub] CrossRef - Challenges in Diagnosis and Management of Ovarian Neuroendocrine Carcinoma: A Case of Aggressive Disease With Multimodal Treatment Approach
Javeria Haider, Humera Mahmood, Muhammad Faheem, Shaista Khurshid, Abdullah, Biruk Demisse Ayalew, Humza Saeed
Clinical Case Reports.2025;[Epub] CrossRef - Neuroendocrine Marker Expression in Primary Non-neuroendocrine Epithelial Tumors of the Ovary: A Study of 551 Cases
Michaela Kendall Bártů, Kristýna Němejcová, Romana Michálková, Quang Hiep Bui, Jana Drozenová, Pavel Fabian, Oluwole Fadare, Jitka Hausnerová, Jan Laco, Radoslav Matěj, Gábor Méhes, Adam Šafanda, Naveena Singh, Petr Škapa, Zuzana Špůrková, Simona Stolnicu
International Journal of Gynecological Pathology.2024; 43(2): 123. CrossRef - Diagnostic and therapeutic challenge of neuroendocrine endometrial carcinoma: a case report
Hariyono Winarto, David Calvin, Fitriyadi Kusuma, Kartiwa Hadi Nuryanto, Yuri Feharsal, Dewita Nilasari, Hartono Tjahjadi
The Pan African Medical Journal.2024;[Epub] CrossRef - Neuroendocrine carcinoma of ovary: Hitherto rare entity in primary ovarian tumors
Md A. Osama, Seema Rao, Punita Bhardwaj, Geeta Mediratta, Sunita Bhalla, Sonia Badwal
Indian Journal of Pathology and Microbiology.2023; 66(4): 855. CrossRef - Mixed neuroendocrine–non-neuroendocrine neoplasm with mucinous adenocarcinoma and amphicrine carcinoma components in the bile duct: an autopsy case
Toji Murabayashi, Yoshihide Kanno, Takashi Odaira, Shinsuke Koshita, Takahisa Ogawa, Hiroaki Kusunose, Toshitaka Sakai, Keisuke Yonamine, Kazuaki Miyamoto, Fumisato Kozakai, Kazuki Endo, Yutaka Noda, Takashi Sawai, Kei Ito
Clinical Journal of Gastroenterology.2023; 16(2): 310. CrossRef - Coexistence of Papillary Thyroid Carcinoma and Strumal Carcinoid Arising from Struma Ovarii in Pregnant Women: a Case Report and Review
Myungsoo Im, Doohwa Kim, Soree Ryang, Bo Hyun Kim
International Journal of Thyroidology.2023; 16(1): 134. CrossRef - Role of radiotherapy in the management of rare gynaecological cancers
R. Morcet-Delattre, S. Espenel, P. Tas, C. Chargari, A. Escande
Cancer/Radiothérapie.2023; 27(8): 778. CrossRef - Small cell carcinoma of the ovary, pulmonary type: A role for adjuvant radiotherapy after carboplatin and etoposide?
Anase S. Asom, Ricardo R. Lastra, Yasmin Hasan, Lori Weinberg, Gini F. Fleming, Katherine C. Kurnit
Gynecologic Oncology Reports.2022; 39: 100925. CrossRef - MicroRNA and Metabolic Profiling of a Primary Ovarian Neuroendocrine Carcinoma Pulmonary-Type Reveals a High Degree of Similarity with Small Cell Lung Cancer
Stefano Miglietta, Giulia Girolimetti, Lorena Marchio, Manuela Sollazzo, Noemi Laprovitera, Sara Coluccelli, Dario De Biase, Antonio De Leo, Donatella Santini, Ivana Kurelac, Luisa Iommarini, Anna Ghelli, Davide Campana, Manuela Ferracin, Anna Myriam Perr
Non-Coding RNA.2022; 8(5): 64. CrossRef - Neuroendocrine Carcinomas of the Uterine Cervix, Endometrium, and Ovary Show Higher Tendencies for Bone, Brain, and Liver Organotrophic Metastases
Hyung Kyu Park
Current Oncology.2022; 29(10): 7461. CrossRef - Uterine carcinoma admixed with neuroendocrine carcinoma
Maria Victoria Olinca, Anca Potecă, Elvira Brătilă, Mihai Mitran
Ginecologia.ro.2022; 4(38): 32. CrossRef - The puzzle of gynecologic neuroendocrine carcinomas: State of the art and future directions
Giuseppe Caruso, Carolina Maria Sassu, Federica Tomao, Violante Di Donato, Giorgia Perniola, Margherita Fischetti, Pierluigi Benedetti Panici, Innocenza Palaia
Critical Reviews in Oncology/Hematology.2021; 162: 103344. CrossRef - Pitfalls and challenges in managing neuroendocrine carcinoma of gynecological origin: A case series and brief review
Lauren E. Farmer, Rutmi U. Goradia, Nisha A. Lakhi
Clinical Case Reports.2021;[Epub] CrossRef - Primary mixed large cell neuroendocrine and high grade serous carcinoma of the endometrium
Liesel Elisabeth Hardy, Zia Chaudry, King Wan, Chloe Ayres
BMJ Case Reports.2020; 13(9): e234977. CrossRef - Neuroendocrine carcinoma of the endometrium: Disease course, treatment, and outcomes
Kathryn Schlechtweg, Ling Chen, Caryn M. St. Clair, Ana I. Tergas, Fady Khoury-Collado, June Y. Hou, Alexander Melamed, Alfred I. Neugut, Dawn L. Hershman, Jason D. Wright
Gynecologic Oncology.2019; 155(2): 254. CrossRef - Peritoneal Fluid Cytology of Disseminated Large Cell Neuroendocrine Carcinoma Combined with Endometrioid Adenocarcinoma of the Endometrium
Yong-Moon Lee, Min-Kyung Yeo, Song-Yi Choi, Kyung-Hee Kim, Kwang-Sun Suh
Journal of Pathology and Translational Medicine.2019; 53(6): 407. CrossRef - Pro-Gastrin Releasing Peptide: A New Serum Marker for Endometrioid Adenocarcinoma
Mine Kiseli, Gamze Sinem Caglar, Asli Yarci Gursoy, Tolga Tasci, Tuba Candar, Egemen Akincioglu, Emre Goksan Pabuccu, Nurettin Boran, Gokhan Tulunay, Haldun Umudum
Gynecologic and Obstetric Investigation.2018; 83(6): 540. CrossRef - Tumeur neuroendocrine à petite cellule de l’endomètre : prise en charge originale
E. Galmiche, N. Hudry, P. Sagot, P. Ginod, S. Douvier
Gynécologie Obstétrique Fertilité & Sénologie .2017; 45(6): 381. CrossRef - Twist on a classic: vitamin D and hypercalcaemia of malignancy
Juan C Osorio, Masha G Jones, Nina Schatz-Siemers, Stephanie J Tang
BMJ Case Reports.2017; 2017: bcr-2017-220819. CrossRef - Mixed Neuroendocrine-Nonneuroendocrine Neoplasms (MiNENs): Unifying the Concept of a Heterogeneous Group of Neoplasms
Stefano La Rosa, Fausto Sessa, Silvia Uccella
Endocrine Pathology.2016; 27(4): 284. CrossRef - Neuroendocrine tumours in rare sites: differences in nomenclature and diagnostics—a rare and ubiquitous histotype
Elia Guadagno, Gaetano De Rosa, Marialaura Del Basso De Caro
Journal of Clinical Pathology.2016; 69(7): 563. CrossRef - Primary ovarian neuroendocrine tumor arising in association with a mature cystic teratoma: A case report
Nicolas M. Orsi, Mini Menon
Gynecologic Oncology Reports.2016; 17: 83. CrossRef - Benign Endometrial Polyp and Primary Endometrial Small Cell Neuroendocrine Carcinoma Confined to the Polyp: A Rare Association
Pembe Oltulu, Ceyhan Uğurluoğlu, Ayşenur Uğur, Sıdıka Fındık, Lema Tavlı
Journal of Clinical and Experimental Investigations.2016;[Epub] CrossRef
- Mixed neuroendocrine-non-neuroendocrine neoplasm (MiNEN) of the cervix in a 38-year-old female: a case report and review of literature
- Clinical and Prognostic Significances of Cytokeratin 19 and KIT Expression in Surgically Resectable Pancreatic Neuroendocrine Tumors
- Eun-Mi Son, Joo Young Kim, Soyeon An, Ki-Byung Song, Song Cheol Kim, Eunsil Yu, Seung-Mo Hong
- J Pathol Transl Med. 2015;49(1):30-36. Published online January 15, 2015
- DOI: https://doi.org/10.4132/jptm.2014.10.23
- 13,125 View
- 102 Download
- 22 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Pancreatic neuroendocrine tumors (PanNETs) are malignant endocrine neoplasms that present diverse clinical behaviors. Therefore, identification of biomarkers of PanNETs is important for stratification of the prognosis of PanNET patients. Recently, cytokeratin 19 (CK19) and KIT expression were reported to have prognostic significance in PanNET patients. Methods: To identify their prognostic significance, CK19 and KIT protein expression were assessed in 182 surgically resected PanNETs and compared with clinicopathologic factors. Results: Of 182 PanNETs cases, CK19 and KIT expression was noted in 97 (53.3%) and 16 (8.8%) cases, respectively. PanNET patients with CK19 expression had larger tumors (p=.006), higher World Health Organization (WHO) grade (p=.002) and pT classification (p<.001), increased distant metastasis (p=.004), and lymphovascular (p=.012) and perineural (p=.019) invasion. Similarly, those with KIT expression had larger tumors (p=.030), higher WHO grade (p=.001), advanced pT classification (p<.001), distant metastasis (p=.001), and lymphovascular invasion (p=.014). The 5-year survival rate for PanNET patients with KIT expression was significantly lower (62%) than that of patients without KIT expression (77%, p=.011), as determined by univariate but not by multivariate analyses. Conclusions: CK19 and KIT expression correlate with higher metastatic potential and advanced disease stage, and KIT expression is associated with worse survival in PanNET patients. -
Citations
Citations to this article as recorded by- Case Report: Extra-adrenal retroperitoneal paraganglioma in a young adult cat diagnosed by imaging, pathology, and immunohistochemistry
Sang-June Sohn, Sohee Lim, Junghoon Park, Ulsoo Choi, Yeon-Jung Hong
Frontiers in Veterinary Science.2025;[Epub] CrossRef - Appendiceal mucinous tumour resulting in autoamputation of the appendix: A case report and literature review
Chenao Wang, Yufeng Liu, Yaqing Liu, Baicheng Li, Xingdong Hou, Bowei Lu, Zhao Chen, Shili Ning
Experimental and Therapeutic Medicine.2025; 31(2): 1. CrossRef - Expression profiles of cadherin 17 and claudin 18.2 in comparison with peptide hormonal expression in pancreatic neuroendocrine tumours: Implications for targeted immunotherapy
Kahoko Maeda, Takeshi Uehara, Waki Hosoda, Yasuhiro Kuraishi, Hiroyoshi Ota
Pathology - Research and Practice.2024; 262: 155537. CrossRef - Glypican-3 and Cytokeratin-19 Expression in Pancreatic Cancer in a Canadian Population
Carley Bekkers, Ravi Ramjeesingh, Thomas Arnason
Journal of Clinical Medicine.2024; 13(22): 6893. CrossRef - Combined Infiltrative Macroscopic Growth Pattern and Infiltrative Microscopic Tumor Border Status Is a Novel Surrogate Marker of Poor Prognosis in Patients With Pancreatic Neuroendocrine Tumor
Bokyung Ahn, Joo Young Kim, Seung-Mo Hong
Archives of Pathology & Laboratory Medicine.2023; 147(1): 100. CrossRef -
Tumor-associated nonmyelinating Schwann cell–expressed
PVT1
promotes pancreatic cancer kynurenine pathway and tumor immune exclusion
Chengcao Sun, Youqiong Ye, Zhi Tan, Yuan Liu, Yajuan Li, Wei Hu, Ke Liang, Sergey D. Egranov, Lisa Angela Huang, Zhao Zhang, Yaohua Zhang, Jun Yao, Tina K. Nguyen, Zilong Zhao, Andrew Wu, Jeffrey R. Marks, Abigail S. Caudle, Aysegul A. Sahin, Jianjun Gao,
Science Advances.2023;[Epub] CrossRef - Diagnostic and prognostic impact of cytokeratin 19 expression analysis in human tumors: a tissue microarray study of 13,172 tumors
Anne Menz, Rifka Bauer, Martina Kluth, Clara Marie von Bargen, Natalia Gorbokon, Florian Viehweger, Maximilian Lennartz, Cosima Völkl, Christoph Fraune, Ria Uhlig, Claudia Hube-Magg, Noémi De Wispelaere, Sarah Minner, Guido Sauter, Simon Kind, Ronald Simo
Human Pathology.2021; 115: 19. CrossRef - The molecular biology of pancreatic neuroendocrine neoplasms: Challenges and translational opportunities
Kate Young, Naureen Starling, Anguraj Sadanandam
Seminars in Cancer Biology.2020; 61: 132. CrossRef - Pancreatic acinar cell carcinomas and mixed acinar-neuroendocrine carcinomas are more clinically aggressive than grade 1 pancreatic neuroendocrine tumours
Joo Young Kim, Jacqueline A. Brosnan-Cashman, Jiyoon Kim, Soyeon An, Kyoung-Bun Lee, Haeryoung Kim, Do Youn Park, Kee-Taek Jang, Young-Ha Oh, Ralph H. Hruban, Christopher M. Heaphy, Seung-Mo Hong
Pathology.2020; 52(3): 336. CrossRef - Morphologic Variants of Pancreatic Neuroendocrine Tumors: Clinicopathologic Analysis and Prognostic Stratification
Yue Xue, Michelle D. Reid, Burcin Pehlivanoglu, Rebecca C. Obeng, Hongmei Jiang, Bahar Memis, Shu K. Lui, Juan Sarmiento, David Kooby, Shishir K. Maithel, Bassel El-Rayes, Olca Basturk, Volkan Adsay
Endocrine Pathology.2020; 31(3): 239. CrossRef - Histological grades and prognostic markers of well-differentiated pancreatic neuroendocrine tumor (WDPNET)
Yongchao Li, Daniel Rowan, Claire P. Williamson, Meiyun Fan, Ali G. Saad, Lizhi Zhang
Journal of Pancreatology.2020; 3(4): 188. CrossRef - Clinical and histopathologic prognostic implications of the expression of cytokeratins 8, 10, 13, 14, 16, 18 and 19 in oral and oropharyngeal squamous cell carcinoma
Rima A. Safadi, Niveen I. Abdullah, Rolla F. Alaaraj, Dima H. Bader, Darshan D. Divakar, Abed A. Hamasha, Maher A. Sughayer
Archives of Oral Biology.2019; 99: 1. CrossRef - Prognostic and predictive factors on overall survival and surgical outcomes in pancreatic neuroendocrine tumors: recent advances and controversies
Lingaku Lee, Tetsuhide Ito, Robert T Jensen
Expert Review of Anticancer Therapy.2019; 19(12): 1029. CrossRef - Carbonic anhydrase 9 expression in well-differentiated pancreatic neuroendocrine neoplasms might be associated with aggressive behavior and poor survival
Joo Young Kim, Sang Hwa Lee, Soyeon An, Sung Joo Kim, You-Na Sung, Ki-Byung Song, Dae Wook Hwang, Song Cheol Kim, Seung-Mo Hong
Virchows Archiv.2018; 472(5): 739. CrossRef - CD133 expression in well-differentiated pancreatic neuroendocrine tumors: a potential predictor of progressive clinical courses
Yasuhiro Sakai, Seung-Mo Hong, Soyeon An, Joo Young Kim, Denis Corbeil, Jana Karbanová, Kyoko Otani, Kohei Fujikura, Ki-Byung Song, Song Cheol Kim, Masayuki Akita, Yoshihide Nanno, Hirochika Toyama, Takumi Fukumoto, Yonson Ku, Takanori Hirose, Tomoo Itoh,
Human Pathology.2017; 61: 148. CrossRef - Prognostic and predictive biomarkers in neuroendocrine tumours
David L. Chan, Stephen J. Clarke, Connie I. Diakos, Paul J. Roach, Dale L. Bailey, Simron Singh, Nick Pavlakis
Critical Reviews in Oncology/Hematology.2017; 113: 268. CrossRef - Loss of Progesterone Receptor Expression Is an Early Tumorigenesis Event Associated with Tumor Progression and Shorter Survival in Pancreatic Neuroendocrine Tumor Patients
Sung Joo Kim, Soyeon An, Jae Hoon Lee, Joo Young Kim, Ki-Byung Song, Dae Wook Hwang, Song Cheol Kim, Eunsil Yu, Seung-Mo Hong
Journal of Pathology and Translational Medicine.2017; 51(4): 388. CrossRef - Prognostic significance of cytokeratin 19 expression in pancreatic neuroendocrine tumor: A meta-analysis
Dong Cen, Jiang Chen, Zheyong Li, Jie Zhao, Xiujun Cai, Aamir Ahmad
PLOS ONE.2017; 12(11): e0187588. CrossRef - A retrospective cohort study of pancreatic neuroendocrine tumors at single institution over 15 years: New proposal for low- and high-grade groups, validation of a nomogram for prognosis, and novel follow-up strategy for liver metastases
Liangtao Ye, Huilin Ye, Quanbo Zhou, Zhihua Li, Qing Lin, Langping Tan, Wenchao Gao, Zhiqiang Fu, Shangyou Zheng, Rufu Chen
International Journal of Surgery.2016; 29: 108. CrossRef - Correlating and Combining Genomic and Proteomic Assessment withIn VivoMolecular Functional Imaging: Will This Be the Future Roadmap for Personalized Cancer Management?
Bhakti Basu, Sandip Basu
Cancer Biotherapy and Radiopharmaceuticals.2016; 31(3): 75. CrossRef - Recent Updates on Neuroendocrine Tumors From the Gastrointestinal and Pancreatobiliary Tracts
Joo Young Kim, Seung-Mo Hong
Archives of Pathology & Laboratory Medicine.2016; 140(5): 437. CrossRef
- Case Report: Extra-adrenal retroperitoneal paraganglioma in a young adult cat diagnosed by imaging, pathology, and immunohistochemistry
- A Ciliated Cyst with Müllerian Differentiation Arising in the Posterior Mediastinum
- So Jung Lee, Chung Su Hwang, Do Youn Park, Gi Young Huh, Chang Hun Lee
- Korean J Pathol. 2014;48(5):401-404. Published online October 27, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.5.401
- 9,556 View
- 80 Download
- 10 Crossref
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Cyst of Hattori: literature review and case presentation
R. B. Berdnikov, K. A. Andryuschenko, N. S. Zavarov, E. M. Petrunina, A. V. Bazhenov, A. S. Romakhin
PULMONOLOGIYA.2025; 35(4): 553. CrossRef - Cyst of Hattori: A Rare Cyst in the Posterior Mediastinum
Matthew D. Turner, Elicia Goodale, Barry C. Gibney, Maria Cecilia D. Reyes
International Journal of Surgical Pathology.2023; 31(4): 431. CrossRef - A large retroperitoneal Mullerian cyst: case report and review of the literature
Elena Parmentier, Jody Valk, Paul Willemsen, Caroline Mattelaer
Acta Chirurgica Belgica.2021; 121(4): 278. CrossRef - A case of resected Mullerian cyst in posterior mediastinum
Yoshiyuki Susaki, Noriyoshi Sawabata
The Journal of the Japanese Association for Chest Surgery.2020; 34(2): 137. CrossRef - Serosal Inclusion Cysts and Arteriovenous Fistulas in Paraprostatic Area of a Dog
Daisuke KOJIMA, Kyoko KOJIMA, Kazumi OTA, Yoshihiko KOJIMA
Journal of the Japan Veterinary Medical Association.2020; 73(9): 511. CrossRef - A surgical case of Mullerian cyst in the posterior mediastinum
Yusuke Kita, Yoshimasa Tokunaga, Taku Okamoto
The Journal of the Japanese Association for Chest Surgery.2019; 33(1): 68. CrossRef - CT and MRI characteristics for differentiating mediastinal Müllerian cysts from bronchogenic cysts
M. Kawaguchi, H. Kato, A. Hara, N. Suzui, H. Tomita, T. Miyazaki, H. Iwata, M. Matsuo
Clinical Radiology.2019; 74(12): 976.e19. CrossRef - A case of Mullerian cyst arising in the posterior mediastinum
Masahiro Adachi, Isao Sano, Shintaro Hashimoto, Ryoichiro Doi, Hideki Taniguchi, Kazuto Shigematsu
The Journal of the Japanese Association for Chest Surgery.2018; 32(6): 713. CrossRef - Two resected cases of Mullerian cyst in the posterior mediastinum
Shotaro Hashimoto, Masato Hisano, Masato Morimoto
The Journal of the Japanese Association for Chest Surgery.2018; 32(7): 818. CrossRef - Posterior mediastinal Müllerian cyst: a rare cause of pain in a young woman
Rebecca Weedle, Keith Conway, Igor Saftic, Alan Soo
Asian Cardiovascular and Thoracic Annals.2017; 25(6): 466. CrossRef
- Cyst of Hattori: literature review and case presentation
- Altered Expression of PTEN and Its Major Regulator MicroRNA-21 in Pulmonary Neuroendocrine Tumors
- Hyoun Wook Lee, Seung Yeon Ha, Mee Sook Roh
- Korean J Pathol. 2014;48(1):17-23. Published online February 25, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.1.17
- 8,911 View
- 46 Download
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Phosphatase and tensin homolog on chromosome ten (PTEN) is one of the most frequently inactivated tumor suppressors in various tumor types. MicroRNA-21 (miR-21) may affect tumor progression by post-transcriptional repression of expression of tumor suppressors, such as PTEN. This study was conducted to evaluate the significance of PTEN expression in pulmonary neuroendocrine (NE) tumors and to analyze the relationship between PTEN and miR-21 expressions.
Methods Expressions of PTEN and miR-21 were investigated by immunohistochemistry and real time reverse transcription-polymerase chain reaction, respectively, in 75 resected pulmonary NE tumors (23 typical carcinoids [TCs], nine atypical carcinoids [ACs], 22 large cell NE carcinomas [LCNECs], and 21 small cell lung carcinomas [SCLCs]).
Results Loss of PTEN expression was observed in four of 23 TCs (17.4%), four of nine ACs (44.4%), 16 of 22 LCNECs (72.7%) and nine of 21 SCLCs (42.9%) (p=.025). The expression level of miR-21 was significantly higher in high-grade NE carcinomas than in carcinoid tumors (p<.001). PTEN expression was inversely correlated with miR-21 expression (p<.001).
Conclusions This study suggests that aberrant expression of PTEN in relation to miR-21 may represent an important step in the development and progression of pulmonary NE tumors.
-
Citations
Citations to this article as recorded by- Mechanisms of skin wound healing regulated by fibroblast-derived exosomes
Ye Qiu, Xingying Zhu, Xiaoqian Yang, Jiaming Wan
Biochemistry and Biophysics Reports.2025; 44: 102371. CrossRef - Role of microRNAs in regulating cell proliferation, metastasis and chemoresistance and their applications as cancer biomarkers in small cell lung cancer
Monu Pandey, Abhirup Mukhopadhyay, Surender K. Sharawat, Sachin Kumar
Biochimica et Biophysica Acta (BBA) - Reviews on Cancer.2021; 1876(1): 188552. CrossRef - Neuroendocrine Tumors Are Enriched in Cowden Syndrome
Alison Greidinger, Susan Miller-Samuel, Veda N. Giri, Michele Sue-Ann Woo, Saranya Akumalla, Charnita Zeigler-Johnson, Scott W. Keith, Daniel P. Silver
JCO Precision Oncology.2020; (4): 551. CrossRef - Prognostic and predictive role of the PI3K–AKT–mTOR pathway in neuroendocrine neoplasms
P. Gajate, T. Alonso-Gordoa, O. Martínez-Sáez, J. Molina-Cerrillo, E. Grande
Clinical and Translational Oncology.2018; 20(5): 561. CrossRef - Genetic and epigenetic drivers of neuroendocrine tumours (NET)
Annunziata Di Domenico, Tabea Wiedmer, Ilaria Marinoni, Aurel Perren
Endocrine-Related Cancer.2017; 24(9): R315. CrossRef - Expression of hsa-let-7b-5p, hsa-let-7f-5p, and hsa-miR-222-3p and their putative targets HMGA2 and CDKN1B in typical and atypical carcinoid tumors of the lung
Pietro Di Fazio, Moritz Maass, Silvia Roth, Christian Meyer, Joana Grups, Peter Rexin, Detlef K Bartsch, Andreas Kirschbaum
Tumor Biology.2017; 39(10): 101042831772841. CrossRef - The regulatory role of aberrant Phosphatase and Tensin Homologue and Liver Kinase B1 on AKT/mTOR/c-Myc axis in pancreatic neuroendocrine tumors
Tsung-Ming Chang, Yan-Shen Shan, Pei-Yi Chu, Shih Sheng Jiang, Wen-Chun Hung, Yu-Lin Chen, Hsiu-Chi Tu, Hui-You Lin, Hui-Jen Tsai, Li-Tzong Chen
Oncotarget.2017; 8(58): 98068. CrossRef - Pulmonary atypical carcinoid in a patient with Cowden syndrome
Hiroaki Tsunezuka, Kaori Abe, Junichi Shimada, Masayoshi Inoue
Interactive CardioVascular and Thoracic Surgery.2016; 22(6): 860. CrossRef - Differential miRNA-Expression as an Adjunctive Diagnostic Tool in Neuroendocrine Tumors of the Lung
Melanie Demes, Christoph Aszyk, Holger Bartsch, Joachim Schirren, Annette Fisseler-Eckhoff
Cancers.2016; 8(4): 38. CrossRef - microRNA-21 promotes osteogenic differentiation of mesenchymal stem cells by the PI3K/β-catenin pathway
Yu-Bin Meng, Xue Li, Zhao-Yang Li, Jin Zhao, Xu-Bo Yuan, Yu Ren, Zhen-Duo Cui, Yun-De Liu, Xian-Jin Yang
Journal of Orthopaedic Research.2015; 33(7): 957. CrossRef - Inhibition of NADPH oxidase protects against metastasis of human lung cancer by decreasing microRNA-21
Song Yan, Gang Liu, Changyan Pei, Wenqing Chen, Pei Li, Qiang Wang, Xintian Jin, Jiajia Zhu, Mengzhu Wang, Xiyu Liu
Anti-Cancer Drugs.2015; 26(4): 388. CrossRef
- Mechanisms of skin wound healing regulated by fibroblast-derived exosomes
- Morphologic Alteration of Metastatic Neuroblastic Tumor in Bone Marrow after Chemotherapy
- Go Eun Bae, Yeon-Lim Suh, Ki Woong Sung, Jung-Sun Kim
- Korean J Pathol. 2013;47(5):433-442. Published online October 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.5.433
- 8,748 View
- 49 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The aim of this study is to evaluate the histologic features of metastatic neuroblastic tumors (NTs) in bone marrow (BM) before and after chemotherapy in comparison with those of primary NTs.
Methods A total of 294 biopsies from 48 children diagnosed with NTs with BM metastasis were examined. There were 48 primary neoplasm biopsies, 48 BM biopsies before chemotherapy, 36 primary neoplasm excisional biopsies after chemotherapy, and 162 BM biopsies after chemotherapy.
Results Metastatic NTs in BM before chemotherapy were composed of undifferentiated and/or differentiating neuroblasts, but had neither ganglion cells nor Schwannian stroma. Metastatic foci of BM after chemotherapy were found to have differentiated into ganglion cells or Schwannian stroma, which became more prominent after further cycles of chemotherapy. Persistence of NTs or tumor cell types in BM after treatment did not show statistically significant correlation to patients' outcome. However, three out of five patients who newly developed poorly differentiated neuroblasts in BM after treatment expired due to disease progression.
Conclusions Metastatic NTs in BM initially consist of undifferentiated or differentiating neuroblasts regardless of the primary tumor subtype, and become differentiated after chemotherapy. Newly appearing poorly differentiated neuroblasts after treatment might be an indicator for poor prognosis.
-
Citations
Citations to this article as recorded by- Postchemotherapy gross residual tumor in non‐high‐risk neuroblastoma: Clinical significance and the role of adjuvant therapy
Eun Seop Seo, Hana Lim, Hee Won Cho, Hee Young Ju, Ji Won Lee, Keon Hee Yoo, Sanghoon Lee, Do Hoon Lim, Ki Woong Sung, Hong Hoe Koo
Pediatric Blood & Cancer.2022;[Epub] CrossRef
- Postchemotherapy gross residual tumor in non‐high‐risk neuroblastoma: Clinical significance and the role of adjuvant therapy
- A Giant Peritoneal Loose Body
- Hyun-Soo Kim, Ji-Youn Sung, Won Seo Park, Youn Wha Kim
- Korean J Pathol. 2013;47(4):378-382. Published online August 26, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.4.378
- 9,771 View
- 65 Download
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Peritoneal loose bodies (PLBs) are usually discovered incidentally during laparotomy or autopsy. A few cases of giant PLBs presenting with various symptoms have been reported in the literature. Here, we describe a case of a giant PLB incidentally found in the pelvic cavity of a 50-year-old man. Computed tomography revealed a free ovoid mass in the pelvic cavity that consisted of central dense, heterogeneous calcifications and peripheral soft tissue. The mass was an egg-shaped, hard, glistening concretion measuring 7.5×7.0×6.8 cm and weighing 160 g. This concretion consisted of central necrotic fatty tissue surrounded by concentrically laminated, acellular, fibrous material. Small PLBs usually do not require any specific treatment. However, if PLBs cause alimentary or urinary symptoms due to their large size, surgical removal may be recommended. It is essential for clinicians to be aware of this entity and its characteristic features to establish the correct diagnosis.
-
Citations
Citations to this article as recorded by- A giant peritoneal loose body: A case report and updated literature review and data synthesis
Guo-Le Nie, Shicheng Chu, Song Geng, Hong Jiang, Hao Zhan
Medicine.2025; 104(50): e45956. CrossRef - Unveiling the rarity: A case report of giant peritoneal loose body
Abdudin Heru Mehammed, Natnael Alemu Bezabih, Muluken Yifru Gebresilassie, Yohanna Aregawi Hailu, Mengistu Yismie Semahegn, Misganaw Yigletie Damtie
Radiology Case Reports.2024; 19(11): 5492. CrossRef - A Case of a Fixed Giant Peritoneal Loose Body outside the Peritoneum and near the Rectovesical Excavation
Kotaro Nanno, Seiichi Shinji, Takeshi Yamada, Akihisa Matsuda, Ryo Ohta, Hiromichi Sonoda, Takuma Iwai, Kohki Takeda, Kazuhide Yonaga, Koji Ueda, Sho Kuriyama, Toshimitsu Miyasaka, Hiromasa Komori, Yoshinobu Shioda, Hiroshi Yoshida
Journal of Nippon Medical School.2023; 90(3): 276. CrossRef - A Large Intraperitoneal Free Body in a 69-Year-Old Indian Man: a Case Study
Siddhartha Sankar Bhattacharjee, Promit Chakraborty
Indian Journal of Surgery.2022; 84(1): 206. CrossRef - Peritoneal loose body presenting as a hepatic mass: A case report and review of the literature
Yang Wen, Min-jie Shang, Yan-qing Ma, Song-hua Fang, Yuan Chen
Open Medicine.2021; 16(1): 1356. CrossRef - Peritoneal Loose Body in a Patient With Ampullary Adenocarcinoma
A.V. Pradeep, Abdul Razik, Ankur Goyal, Atin Kumar, Virinder Kumar Bansal, Asuri Krishna
ACG Case Reports Journal.2021; 8(11): e00680. CrossRef - Exploratory laparoscopy as first choice procedure for the diagnosis of giant peritoneal loose body: a case report
RuiBin Li, ZhiHeng Wan, HaoTian Li
Journal of International Medical Research.2020;[Epub] CrossRef - A rare peritoneal egg: Case report with literature review
Nilu Malpani Dhoot, Shivaraj Afzalpurkar, Usha Goenka, Vinay Mahendra, Enam Murshed Khan, Arpita Sutradhar, Mahesh Goenka
Radiology Case Reports.2020; 15(10): 1895. CrossRef - A giant peritoneal loose body impacted in the pelvic cavity, a rare and interesting finding during laparotomy
Ayad A. Mohammed
International Journal of Surgery: Global Health.2020; 3(6): e24. CrossRef - Giant Mobile Intraperitoneal Loose Body
Mohd Ilyas, Mohd Yaqoob Wani, Musaib Ahmad Dar, Feroze A. Shaheen
ACG Case Reports Journal.2019; 6(1): e00006. CrossRef - Giant peritoneal loose body in a patient with end-stage renal disease
Nadejda Cojocari, Leonard David
SAGE Open Medical Case Reports.2018;[Epub] CrossRef - Two giant peritoneal loose bodies were simultaneously found in one patient: A case report and review of the literature
Qingxing Huang, Aihong Cao, Jun Ma, Zhenhua Wang, Jianhong Dong
International Journal of Surgery Case Reports.2017; 36: 74. CrossRef - Laparoscopic extraction of a giant peritoneal loose body: Case report and review of literature
Keiso Matsubara, Yuji Takakura, Takashi Urushihara, Takashi Nishisaka, Toshiyuki Itamoto
International Journal of Surgery Case Reports.2017; 39: 188. CrossRef - Symptomatic giant peritoneal loose body in the pelvic cavity: A case report
Andreas Elsner, Mikolaj Walensi, Maya Fuenfschilling, Robert Rosenberg, Robert Mechera
International Journal of Surgery Case Reports.2016; 21: 32. CrossRef - A Case of a Peritoneal Loose Body with the Maximum Diameter of 50 mm
Yoshihiro MOCHIZUKI, Hiroshi IINO, Michio HARA, Syugo SHIBA, Makoto SUDO, Naoki OISHI, Tetsuo KONDO
Nihon Rinsho Geka Gakkai Zasshi (Journal of Japan Surgical Association).2016; 77(10): 2552. CrossRef - Giant peritoneal loose body in the pelvic cavity confirmed by laparoscopic exploration: a case report and review of the literature
Hong Zhang, Yun-zhi Ling, Ming-ming Cui, Zhi-xiu Xia, Yong Feng, Chun-sheng Chen
World Journal of Surgical Oncology.2015;[Epub] CrossRef
- A giant peritoneal loose body: A case report and updated literature review and data synthesis
- Bronchial Schwannomas: Clinicopathologic Analysis of 7 Cases
- Yoon Yang Jung, Min Eui Hong, Joungho Han, Tae Sung Kim, Jhingook Kim, Young-Mog Shim, Hojoong Kim
- Korean J Pathol. 2013;47(4):326-331. Published online August 26, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.4.326
- 9,634 View
- 68 Download
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF Background It has long been recognized that bronchial schwannomas are extremely rare. As such, diagnosing tumors in this extraordinary location can sometimes be problematic.
Methods We reviewed seven cases of bronchoscopically or surgically resected endobronchial schwannomas and evaluated their clinical and pathologic features.
Results The present study included five female and two male patients, with ages ranging from 16 to 81 years (mean age, 44.9 years). The clinical presentation varied according to tumor size and location. Patients with more centrally (trachea or main bronchus) located tumors experienced respiratory symptoms (80%) more often than patients with more peripherally (lobar or segmental bronchus) located tumors (0%). Histologically, the tumors were composed of spindle cells that stained with S100 protein. Some of the tumors showed typical Antoni A areas with Verocay body formation. Five of six patients (83.3%) underwent complete tumor removal by rigid bronchoscopy.
Conclusions Pathologists should consider endobronchial schwannoma in the differential diagnosis of a spindle cell tumor involving the bronchus. Additionally, our results showed that rigid bronchoscopy is an effective tool for tumor removal in endobronchial schwannoma patients.
-
Citations
Citations to this article as recorded by- Tracheal schwannoma: A pseudo-asthmatic syndrome with successful laser Nd-YAG resection as first-line therapy
Ranim Nakhal, Raneem Ahmad, Bassel Ibrahim, Sultaneh Haddad, Arabi Abbas, Nizar Abbas
International Journal of Surgery Case Reports.2025; 134: 111706. CrossRef - CT-Occult Primary Benign Tracheobronchial Neoplasms: A Single-Center 40-Case Clinicopathologic Series
Qiliang Liu, Yan Hu, Minhui Mei, Xuan Wang, Jun Li, Chao Quan, Peng Liu
International Journal of General Medicine.2025; Volume 18: 5765. CrossRef - Outcomes of Different Surgical Approaches in Tracheal Schwannoma: A Narrative Review
Hassan Fahmi Alkhars, Mohammad Almayouf, Majed Albarrak, Faisal Alzahrani, Naif Fnais, Mohammed Alessa, Khalid Alqahtani, Saleh Aldhahri
Ear, Nose & Throat Journal.2025;[Epub] CrossRef - Rare tracheal schwannoma in a child: successful resection via cervical incision
Hariharan Krishnamurthi, Vijayakumar Raju, Naveen Srinivasan, Kaushik Jothinath, Karthik Babu Murugesan, Antony Terance Benjamin, Nagarajan Muthialu
Indian Journal of Thoracic and Cardiovascular Surgery.2025;[Epub] CrossRef - Video-assisted thoracic surgery for an endobronchial ancient schwannoma obstructing the left main bronchus
Jiyeon Kang, Yeon Soo Kim, Ji-Ye Kim
Journal of Surgical Case Reports.2024;[Epub] CrossRef - Interventional treatment of right lower lobe bronchial schwannoma under bronchoscopy: A case report and literature review
Xiyue Li, Ximiao Yu, Ruiqi Luo, Xun Wang
Science Progress.2024;[Epub] CrossRef - Two cases of large tracheobronchial schwannomas completely resected by rigid bronchoscopy with multiple instruments
Changhwan Kim, Hae‐Seong Nam, Yousang Ko
Respirology Case Reports.2023;[Epub] CrossRef - Tracheobronchial schwannoma: a case report and literature review
Guo Lina, Hou Pengguo, Xiao Zhihua, Wang Jianxin, Bai Baoqin, Zhang Mingyue, Sun Junping
Journal of International Medical Research.2023;[Epub] CrossRef - Malignant and Benign Tracheobronchial Neoplasms: Comprehensive Review with Radiologic, Bronchoscopic, and Pathologic Correlation
Francis Girvin, Alexander Phan, Sharon Steinberger, Eugene Shostak, Jamie Bessich, Fang Zhou, Alain Borczuk, Geraldine Brusca-Augello, Margaret Goldberg, Joanna Escalon
RadioGraphics.2023;[Epub] CrossRef - Clinicopathological Characteristics and Pathogenesis of Granular Cell Tumours of the Airways
Jesús Machuca-Aguado, Fernando Cózar-Bernal, Enrique Rodríguez-Zarco, Juan José Ríos-Martin, Miguel Ángel Idoate Gastearena
Journal of Bronchology & Interventional Pulmonology.2023; 30(4): 390. CrossRef - Treatment of primary tracheal schwannoma with endoscopic resection: A case report
Yong-Shuai Shen, Xiang-Dong Tian, Yi Pan, Hua Li
World Journal of Clinical Cases.2022; 10(28): 10279. CrossRef - Primary bronchial schwannoma: A case report
Yosuke Aoyama, Atsushi Miyamoto, Takeshi Fujii, Sakashi Fujimori, Meiyo Tamaoka, Daiya Takai
Medicine.2022; 101(40): e31062. CrossRef - Endobronchial schwannoma in adult: A case report
Touil Imen, Boudaya Mohamed Sadok, Aloui Raoudha, Souhir Ksissa, Brahem Yosra, Ben Attig Yosr, Ksontini Meriem, Bouchareb Soumaya, Keskes Boudawara Nadia, Boussoffara Leila, Knani Jalel
Respiratory Medicine Case Reports.2021; 33: 101396. CrossRef - Primary intratracheal schwannoma misdiagnosed as severe asthma in an adolescent: A case report
Hui-Rong Huang, Pei-Qiang Li, Yi-Xin Wan
World Journal of Clinical Cases.2021; 9(17): 4388. CrossRef - PD‐1/PD‐L1 negative schwannoma mimicking obstructive bronchial malignancy: A case report
Daibing Zhou, Xiaoyan Xing, Jie Fan, Youzhi Zhang, Jie Liu, Yi Gong
Thoracic Cancer.2020; 11(8): 2335. CrossRef - Case report: A tracheobronchial schwannoma in a child
Li Zhang, Wen Tang, Qing-Shan Hong, Pei-feng Lv, Kui-Ming Jiang, Rui Du
Respiratory Medicine Case Reports.2020; 30: 101047. CrossRef - Recurrent transmural tracheal schwannoma resected by video-assisted thoracoscopic window resection
Huiguo Chen, Kai Zhang, Mingjun Bai, Haifeng Li, Jian Zhang, Lijia Gu, Weibin Wu
Medicine.2019; 98(51): e18180. CrossRef - Primary intratracheal schwannoma resected during bronchoscopy using argon plasma coagulation
Purva V Sharma, Yash B Jobanputra, Tatiana Perdomo Miquel, J Ryan Schroeder, Adam Wellikoff
BMJ Case Reports.2018; 2018: bcr-2018-225140. CrossRef - Dumbbell posterior mediastinal schwannoma invading trachea: Multidisciplinary management – weight off the chest
Abhijeet Singh, VallandramamR Pattabhiraman, Arjun Srinivasan, Sivaramakrishnan Mahadevan
Lung India.2018; 35(3): 269. CrossRef - Primary tracheal schwannoma a review of a rare entity: current understanding of management and followup
Shadi Hamouri, Nathan M. Novotny
Journal of Cardiothoracic Surgery.2017;[Epub] CrossRef - A Case of Primary Tracheal Schwannoma
Sung Min Choi, Ji Hong You, Sang Bae Lee, Seong Han Kim, Yon Soo Kim
Kosin Medical Journal.2017; 32(2): 258. CrossRef - Bronchial schwannoma: a singular lesion as a cause of obstructive pneumonia
Rui Caetano Oliveira, Tiago Nogueira, Vítor Sousa, Lina Carvalho
BMJ Case Reports.2016; 2016: bcr2016217300. CrossRef - Bronchoscopic and surgical management of rare endobronchial tumors
Kamlesh Pandey, Preyas J. Vaidya, Arvind H. Kate, Vinod B. Chavhan, Pruthviraj Jaybhaye, Kamlakar Patole, Ramakant K. Deshpande, Prashant N. Chhajed
Journal of Cancer Research and Therapeutics.2016; 12(2): 1093. CrossRef - Endobronchial Neurilemmoma Mimicking a Bronchial Polyp
Ryoung Eun Ko, Seung Yong Park, Yeong Hun Choe, So Ri Kim, Heung Bum Lee, Yong Chul Lee, Seoung Ju Park
Soonchunhyang Medical Science.2015; 21(2): 176. CrossRef - Optimal treatment for primary benign intratracheal schwannoma: A case report and review of the literature
XIAHUI GE, FENGFENG HAN, WENBIN GUAN, JINYUAN SUN, XUEJUN GUO
Oncology Letters.2015; 10(4): 2273. CrossRef
- Tracheal schwannoma: A pseudo-asthmatic syndrome with successful laser Nd-YAG resection as first-line therapy
- Proposal for a Standardized Pathology Report of Gastroenteropancreatic Neuroendocrine Tumors: Prognostic Significance of Pathological Parameters
- Mee-Yon Cho, Jin Hee Sohn, So Young Jin, Hyunki Kim, Eun Sun Jung, Mi-Jung Kim, Kyoung-Mee Kim, Woo Ho Kim, Joon Mee Kim, Yun Kyung Kang, Joon Hyuk Choi, Dae Young Kang, Youn Wha Kim, Eun Hee Choi
- Korean J Pathol. 2013;47(3):227-237. Published online June 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.3.227
- 15,321 View
- 148 Download
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Background There is confusion in the diagnosis and biological behaviors of gastroenteropancreatic neuroendocrine tumors (GEP-NETs), because of independently proposed nomenclatures and classifications. A standardized form of pathology report is required for the proper management of patients.
Methods We discussed the proper pathological evaluation of GEP-NET at the consensus conference of the subcommittee meeting for the Gastrointestinal Pathology Study Group of the Korean Society of Pathologists. We then verified the prognostic significance of pathological parameters from our previous nationwide collection of pathological data from 28 hospitals in Korea to determine the essential data set for a pathology report.
Results Histological classification, grading (mitosis and/or Ki-67 labeling index), T staging (extent, size), lymph node metastasis, and lymphovascular and perineural invasion were significant prognostic factors and essential for the pathology report of GEP-NET, while immunostaining such as synaptophysin and chromogranin may be optional. Furthermore, the staging system, either that of the 2010 American Joint Cancer Committee (AJCC) or the European Neuroendocrine Tumor Society (ENETS), should be specified, especially for pancreatic neuroendocrine neoplasms.
Conclusions A standardized pathology report is crucial for the proper management and prediction of prognosis of patients with GEP-NET.
-
Citations
Citations to this article as recorded by- Analysis of Prognostic Risk Factors of Endoscopic Submucosal Dissection (ESD) and Curative Resection of Gastrointestinal Neuroendocrine Neoplasms
Yuan Si, ChaoKang Huang, JingBin Yuan, XianHui Zhang, QingQiang He, ZhiJin Lin, Ling He, ZhongXin Liu, Yuvaraja Teekaraman
Contrast Media & Molecular Imaging.2022;[Epub] CrossRef - Standardization of the pathologic diagnosis of appendiceal mucinous neoplasms
Dong-Wook Kang, Baek-hui Kim, Joon Mee Kim, Jihun Kim, Hee Jin Chang, Mee Soo Chang, Jin-Hee Sohn, Mee-Yon Cho, So-Young Jin, Hee Kyung Chang, Hye Seung Han, Jung Yeon Kim, Hee Sung Kim, Do Youn Park, Ha Young Park, So Jeong Lee, Wonae Lee, Hye Seung Lee,
Journal of Pathology and Translational Medicine.2021; 55(4): 247. CrossRef - Preoperative diagnosis of well‐differentiated neuroendocrine tumor in common hepatic duct by brush cytology: A case report
Jiwoon Choi, Kyong Joo Lee, Sung Hoon Kim, Mee‐Yon Cho
Diagnostic Cytopathology.2019; 47(7): 720. CrossRef - Primary renal well-differentiated neuroendocrine tumors: report of six cases with an emphasis on the Ki-67 index and mitosis
Bohyun Kim, Han-Seong Kim, Kyung Chul Moon
Diagnostic Pathology.2019;[Epub] CrossRef - Primary low‐grade neuroendocrine carcinoma of the skin: An exceedingly rare entity
Tiffany Y. Chen, Annie O. Morrison, Joe Susa, Clay J. Cockerell
Journal of Cutaneous Pathology.2017; 44(11): 978. CrossRef - Prognostic Validity of the American Joint Committee on Cancer and the European Neuroendocrine Tumors Staging Classifications for Pancreatic Neuroendocrine Tumors
Jae Hee Cho, Ji Kon Ryu, Si Young Song, Jin-Hyeok Hwang, Dong Ki Lee, Sang Myung Woo, Young-Eun Joo, Seok Jeong, Seung-Ok Lee, Byung Kyu Park, Young Koog Cheon, Jimin Han, Tae Nyeun Kim, Jun Kyu Lee, Sung-Hoon Moon, Hyunjin Kim, Eun Taek Park, Jae Chul Hw
Pancreas.2016; 45(7): 941. CrossRef - Early diagnosis and treatment of gastrointestinal neuroendocrine tumors
Hong Shen, Zhuo Yu, Jing Zhao, Xiu-Zhen Li, Wen-Sheng Pan
Oncology Letters.2016; 12(5): 3385. CrossRef - Recent Updates on Neuroendocrine Tumors From the Gastrointestinal and Pancreatobiliary Tracts
Joo Young Kim, Seung-Mo Hong
Archives of Pathology & Laboratory Medicine.2016; 140(5): 437. CrossRef - Pancreatic neuroendocrine tumors: Correlation between the contrast-enhanced computed tomography features and the pathological tumor grade
Koji Takumi, Yoshihiko Fukukura, Michiyo Higashi, Junnichi Ideue, Tomokazu Umanodan, Hiroto Hakamada, Ichiro Kanetsuki, Takashi Yoshiura
European Journal of Radiology.2015; 84(8): 1436. CrossRef - Tumeurs neuroendocrines du tube digestif et du pancréas : ce que le pathologiste doit savoir et doit faire en 2014
Jean-Yves Scoazec, Anne Couvelard
Annales de Pathologie.2014; 34(1): 40. CrossRef - Spectrum of Gastroenteropancreatic NENs in Routine Histological Examinations of Bioptic and Surgical Specimen: A Study of 161 Cases Collected from 17 Departments of Pathology in the Czech Republic
Václav Mandys, Tomáš Jirásek
Gastroenterology Research and Practice.2014; 2014: 1. CrossRef - p27 Loss Is Associated with Poor Prognosis in Gastroenteropancreatic Neuroendocrine Tumors
Hee Sung Kim, Hye Seung Lee, Kyung Han Nam, Jiwoon Choi, Woo Ho Kim
Cancer Research and Treatment.2014; 46(4): 383. CrossRef
- Analysis of Prognostic Risk Factors of Endoscopic Submucosal Dissection (ESD) and Curative Resection of Gastrointestinal Neuroendocrine Neoplasms
- Peripheral Primitive Neuroectodermal Tumor with Osseous Component of the Small Bowel Mesentery: A Case Study
- Joon Mee Kim, Young Chae Chu, Chang Hwan Choi, Lucia Kim, Suk Jin Choi, In Suh Park, Jee Young Han, Kyung Rae Kim, Yoon-La Choi, Taeeun Kim
- Korean J Pathol. 2013;47(1):77-81. Published online February 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.1.77
- 11,111 View
- 49 Download
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF A case of peripheral primitive neuroectodermal tumor of the small bowel mesentery with osseous component is reported. A 23-year-old man was admitted to our hospital because of acute severe abdominal pain. Abdominal computed tomography revealed a large solid and cystic, oval shaped mass, measuring 11.0×6.0 cm in the pelvic cavity. Histologically the resected lesion consisted of sheets of undifferentiated small round cells forming Homer-Wright rosettes and perivascular pseudorosettes, and showed areas of osteoid and bone formation. Immunohistochemical studies revealed that tumor cells expressed positivity against CD99 (MIC2), CD57, neuron-specific enolase, and vimentin. Fluorescence
in situ hybridization study revealed Ewing sarcoma breakpoint region 1 (EWSR1 ) gene rearrangement on chromosome 22q12. To the authors' knowledge this is the first documentation of a peripheral neuroectodermal tumor with osteoid and bone formation of the small bowel mesentery.-
Citations
Citations to this article as recorded by- Undifferentiated small round cell sarcomas in the retroperitoneal space in a 12-year-old female: a rare case report
Dan Liu, Xiaoge Liu, Yan Deng, Ran Wu, Xin Li
Frontiers in Pediatrics.2025;[Epub] CrossRef - Primary Ewing’s sarcoma of the intestine: case report and literature review
Baofa Luo, Wei Gao, Ting Li, Xinran Yu, Fei Guo
Frontiers in Oncology.2024;[Epub] CrossRef - Primary Ewing’s sarcoma in a small intestine – a case report and review of the literature
Andrej Kolosov, Audrius Dulskas, Kastytis Pauza, Veslava Selichova, Dmitrij Seinin, Eugenijus Stratilatovas
BMC Surgery.2020;[Epub] CrossRef - Case report and literature review of Ewing's sarcoma in the gastrointestinal tract
Christopher Bong, Iain Thomson, Guy Lampe
Surgical Practice.2018; 22(2): 84. CrossRef - Pediatric Ewing’s Sarcoma/Primitive Neuroectodermal Tumor (ES/PNET) Developed in the Small Intestine: A Case Report
You Sun Kim, Hye Min Moon, Kyu Sang Lee, Young Suk Park, Hyun-Young Kim, Ji Young Kim, Jin Min Cho, Hyoung Soo Choi
Clinical Pediatric Hematology-Oncology.2017; 24(2): 162. CrossRef - Huge peripheral primitive neuroectodermal tumor of the small bowel mesentery at nonage: A case report and review of the literature
Zhe Liu, Yuan-Hong Xu, Chun-Lin Ge, Jin Long, Rui-Xia Du, Ke-Jian Guo
World Journal of Clinical Cases.2016; 4(9): 306. CrossRef - Primary primitive neuroectodermal tumor arising in the mesentery and ileocecum: A report of three cases and review of the literature
LIBO PENG, LIMIN YANG, NAN WU, BO WU
Experimental and Therapeutic Medicine.2015; 9(4): 1299. CrossRef - Une curieuse tumeur digestive à cellules rondes
Alia Zehani, Ines Chelly, Beya Chelly, Jean-Michel Coindre, Slim Haouet, Nidhameddine Kchir
Annales de Pathologie.2014; 34(2): 104. CrossRef
- Undifferentiated small round cell sarcomas in the retroperitoneal space in a 12-year-old female: a rare case report
- Morphologic Analysis of Pulmonary Neuroendocrine Tumors
- Seung Seok Lee, Myunghee Kang, Seung Yeon Ha, Jungsuk An, Mee Sook Roh, Chang Won Ha, Jungho Han
- Korean J Pathol. 2013;47(1):16-20. Published online February 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.1.16
- 7,814 View
- 52 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Few studies on how to diagnose pulmonary neuroendocrine tumors through morphometric analysis have been reported. In this study, we measured and analyzed the characteristic parameters of pulmonary neuroendocrine tumors using an image analyzer to aid in diagnosis.
Methods Sixteen cases of typical carcinoid tumor, 5 cases of atypical carcinoid tumor, 15 cases of small cell carcinoma, and 51 cases of large cell neuroendocrine carcinoma were analyzed. Using an image analyzer, we measured the nuclear area, perimeter, and the major and minor axes.
Results The mean nuclear area was 0.318±0.101 µm2 in typical carcinoid tumors, 0.326±0.119 µm2 in atypical carcinoid tumors, 0.314±0.107 µm2 in small cell carcinomas, and 0.446±0.145 µm2 in large cell neuroendocrine carcinomas. The mean nuclear circumference was 2.268±0.600 µm in typical carcinoid tumors, 2.408±0.680 µm in atypical carcinoid tumors, 2.158±0.438 µm in small cell carcinomas, and 3.247±1.276 µm in large cell neuroendocrine carcinomas. All parameters were useful in distinguishing large cell neuroendocrine carcinoma from other tumors (p=0.001) and in particular, nuclear circumference was the most effective (p=0.001).
Conclusions Pulmonary neuroendocrine tumors showed nuclear morphology differences by subtype. Therefore, evaluation of quantitative nuclear parameters improves the accuracy and reliability of diagnosis.
-
Citations
Citations to this article as recorded by- Clinical Significance of Persistent Tumor in Bone Marrow during Treatment of High-risk Neuroblastoma
Young Bae Choi, Go Eun Bae, Na Hee Lee, Jung-Sun Kim, Soo Hyun Lee, Keon Hee Yoo, Ki Woong Sung, Hong Hoe Koo
Journal of Korean Medical Science.2015; 30(8): 1062. CrossRef - Morphologic Alteration of Metastatic Neuroblastic Tumor in Bone Marrow after Chemotherapy
Go Eun Bae, Yeon-Lim Suh, Ki Woong Sung, Jung-Sun Kim
Korean Journal of Pathology.2013; 47(5): 433. CrossRef
- Clinical Significance of Persistent Tumor in Bone Marrow during Treatment of High-risk Neuroblastoma
- Collision of Adenocarcinoma and Schwannoma of the Stomach: A Case Report
- Jai Hyang Go
- Korean J Pathol. 2012;46(4):373-376. Published online August 23, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.4.373
- 8,422 View
- 36 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF The simultaneous occurrence of an adenocarcinoma and schwannoma is extremely rare in the stomach, and only one such case has been previously reported, which presented as two separate masses. Indeed, the collision of these tumors has never been reported. We report the case of a 61-year-old male patient who was diagnosed with the synchronous development of a schwannoma and advanced mucinous adenocarcinoma of the stomach, in which the carcinoma cells focally invaded the schwannoma.
-
Citations
Citations to this article as recorded by- What About Gastric Schwannoma? A Review Article
Sara Lauricella, Sergio Valeri, Gianluca Mascianà, Ida Francesca Gallo, Erica Mazzotta, Chiara Pagnoni, Saponaro Costanza, Lorenza Falcone, Domenico Benvenuto, Marco Caricato, Gabriella Teresa Capolupo
Journal of Gastrointestinal Cancer.2021; 52(1): 57. CrossRef - SYNCHRONOUS DEVELOPMENT OF SCHWANNOMA AND PRIMARY ADENOCARCINOMA IN THE STOMACH: A CASE REPORT
Algirdas Šlepavičius, Valdas Gasilionis, Alvydas Česas
Visuomenės sveikata.2019; 28(7): 75. CrossRef - Gastric Collision Tumors: An Insight into Their Origin and Clinical Significance
Adamantios Michalinos, Anastasia Constantinidou, Michael Kontos
Gastroenterology Research and Practice.2015; 2015: 1. CrossRef - Coexistence of gastrointestinal stromal tumor and inflammatory myofibroblastic tumor of the stomach presenting as a collision tumor: first case report and literature review
Hyeong Chan Shin, Mi Jin Gu, Se Won Kim, Jae Woon Kim, Joon Hyuk Choi
Diagnostic Pathology.2015;[Epub] CrossRef
- What About Gastric Schwannoma? A Review Article
- Clinicopathological Analysis of 21 Thymic Neuroendocrine Tumors
- Soomin Ahn, Jae Jun Lee, Sang Yun Ha, Chang Ohk Sung, Jhingook Kim, Joungho Han
- Korean J Pathol. 2012;46(3):221-225. Published online June 22, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.3.221
- 10,863 View
- 95 Download
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Thymic neuroendocrine carcinomas (NECs) are uncommon, for which there is no established information available because of a limited number of epidemiological study in Asia.
Methods We reviewed 21 cases of surgically resected thymic NECs, and evaluated their pathological and clinical features.
Results It showed male predominance (male/female ratio, 15/6) with wide age range from 20 to 72 years (mean age, 49 years). All 21 cases were divided into two types according to the World Health Organization criteria: atypical carcinoid (n=18) and large cell NEC (n=3). Three cases of atypical carcinoid (AC) were associated with ectopic Cushing's syndrome. All the patients (3/3) with large cell NEC (3/3) and 16.7% (3/18) of those with AC died of tumor progression. Common sites of metastasis included lung, lymph node, brain, lumbar spine, mediastinum, bone, and liver.
Conclusions In conclusion, thymic neuroendocrine tumors carry a poor prognosis. Regarding the tumor classification, our results showed that a vast majority of carcinoids in the thymus correspond to ACs. In addition, our results also indicate that typical carcinoid is a very rare entity. Some cases of AC exhibited a large size, solid pattern and they showed aggressive clinical behavior, which highlights the spectrum of histologic appearances of thymic NECs.
-
Citations
Citations to this article as recorded by- A Case of Stage IV Thymic Typical Carcinoid with Multiple Bone Metastases
Hisaya Chikaraishi, Tomohiro Maniwa, Hironobu Samejima, Masao Kobayashi, Julian Horiguchi, Ryu Kanzaki, Hidetoshi Satomi, Keiichiro Honma, Jiro Okami
Haigan.2025; 65(4): 286. CrossRef - Pathology, molecular biology, medical oncology, and radiotherapy implications of lung neuroendocrine neoplasm classification: a multidisciplinary perspective
Giuseppe Pelosi, Alice Laffi, Gianpiero Catalano, Antonino Bruno, Mauro Papotti, Barbara Bassani, Fabrizio Bianchi, Eleonora Duregon, Tommaso Martino De Pas, Chiara Catania, Riccardo Ricotta, Riccardo Papa, Sergio Harari, Angelica Sonzogni, Ilaria Guerrie
Expert Review of Anticancer Therapy.2025; : 1. CrossRef - Neuroendocrine neoplasms of the thymus
Paul D. Barone, Chen Zhang
Frontiers in Immunology.2024;[Epub] CrossRef - Thymic neuroendocrine tumours
Jan von der Thüsen
Diagnostic Histopathology.2023; 29(2): 114. CrossRef - The Utility of Fine Needle Aspiration (FNA) Biopsy in the Diagnosis of Mediastinal Lesions
Uma Kundu, Qiong Gan, Deepak Donthi, Nour Sneige
Diagnostics.2023; 13(14): 2400. CrossRef - Paediatric and adolescent ectopic Cushing's syndrome: systematic review
Chethan Yami Channaiah, Manjiri Karlekar, Vijaya Sarathi, Anurag Ranjan Lila, Shruthi Ravindra, Padma Vikram Badhe, Gaurav Malhotra, Saba Samad Memon, Virendra Ashokrao Patil, C S Pramesh, Tushar Bandgar
European Journal of Endocrinology.2023; 189(4): S75. CrossRef - Multiple endocrine neoplasia type 1 (MEN-1) and neuroendocrine neoplasms (NENs)
Grigoris Effraimidis, Ulrich Knigge, Maria Rossing, Peter Oturai, Åse Krogh Rasmussen, Ulla Feldt-Rasmussen
Seminars in Cancer Biology.2022; 79: 141. CrossRef - Multiple electrolyte disturbances as the presenting feature of multiple endocrine neoplasia type 1 (MEN-1)
Adrian Po Zhu Li, Sheela Sathyanarayan, Salvador Diaz-Cano, Sobia Arshad, Eftychia E Drakou, Royce P Vincent, Ashley B Grossman, Simon J B Aylwin, Georgios K Dimitriadis
Endocrinology, Diabetes & Metabolism Case Reports.2022;[Epub] CrossRef - Metastatic Thymic Carcinoid: Does Surgeon Have a Primary Role?
Kumud Gupta, Ravindra K. Dewan, Vinitha Viswambharan Nair, Rajat Saxena, Shaleen Prasad
The Indian Journal of Chest Diseases and Allied Sciences.2022; 56(4): 255. CrossRef - A resected case of large cell neuroendocrine carcinoma of the thymus
Masashi Umeda, Takahiko Misao, Tomoya Senoh, Yoshinobu Shikatani, Motoi Aoe
The Journal of the Japanese Association for Chest Surgery.2022; 36(7): 766. CrossRef - Treatment strategy and prognostic analysis of spinal metastases from thymomas: A retrospective study from a single center
Shuzhong Liu, Xi Zhou, An Song, Zhen Huo, Siyuan Yao, Yipeng Wang, Yong Liu
Clinical Neurology and Neurosurgery.2020; 196: 106056. CrossRef - Large Cell Neuroendocrine Carcinoma of the Mediastinum Successfully Treated with Systemic Chemotherapy after Palliative Radiotherapy
Takeaki Hidaka, Saki Okuzumi, Ako Matsuhashi, Hidenori Takahashi, Kazunori Hata, Seiichiro Shimizu, Yoshinobu Iwasaki
Internal Medicine.2019; 58(4): 563. CrossRef - Surgical management of spinal metastases of thymic carcinoma
Shuzhong Liu, Xi Zhou, An Song, Zhen Huo, William A. Li, Radhika Rastogi, Yipeng Wang, Yong Liu
Medicine.2019; 98(3): e14198. CrossRef - Resected thymic large cell neuroendocrine carcinoma: A case report and review of the literature
Shogo Ogata, Ryo Maeda, Masaki Tomita, Yuichiro Sato, Takanori Ayabe, Kunihide Nakamura
International Journal of Surgery Case Reports.2019; 60: 53. CrossRef - Metastatic or locally advanced mediastinal neuroendocrine tumours
Aadil Adnan, Shreyas Kudachi, Sudha Ramesh, Kumar Prabhash, Sandip Basu
Nuclear Medicine Communications.2019; 40(9): 947. CrossRef - Results of treatment for thymic neuroendocrine tumours: multicentre clinicopathological study†
Naoko Ose, Hajime Maeda, Masayoshi Inoue, Eiichi Morii, Yasushi Shintani, Hiroshi Matsui, Hirohito Tada, Tositeru Tokunaga, Kenji Kimura, Yasushi Sakamaki, Yukiyasu Takeuchi, Kenjiro Fukuhara, Hiroshi Katsura, Teruo Iwasaki, Meinoshin Okumura
Interactive CardioVascular and Thoracic Surgery.2018; 26(1): 18. CrossRef - Patterns of Failure Following Postoperative Radiation Therapy Based on “Tumor Bed With Margin” for Stage II to IV Type C Thymic Epithelial Tumor
Kyung Hwa Lee, Jae Myoung Noh, Yong Chan Ahn, Dongryul Oh, Jhingook Kim, Young Mog Shim, Jung-ho Han
International Journal of Radiation Oncology*Biology*Physics.2018; 102(5): 1505. CrossRef - Resected thymic large cell neuroendocrine carcinoma: report of a case
Hiromitsu Domen, Yasuhiro Hida, Masaaki Sato, Haruka Takahashi, Tatsuru Ishikawa, Yosuke Shionoya, Midori Hashimoto, Kaoru Nishiyama, Yuma Aoki, Kazuho Inoko, Syotaro Furukawa, Kazuomi Ichinokawa, Hidehisa Yamada
Surgical Case Reports.2018;[Epub] CrossRef - Successful treatment of malignant thymoma with sacrum metastases
Shuzhong Liu, Xi Zhou, An Song, Zhen Huo, William A. Li, Radhika Rastogi, Yipeng Wang, Yong Liu
Medicine.2018; 97(51): e13796. CrossRef - Incidental metastatic mediastinal atypical carcinoid in a patient with parathyroid adenoma: a case report
Zareen Kiran, Asma Ahmed, Owais Rashid, Saira Fatima, Faizan Malik, Saulat Fatimi, Mubassher Ikram
Journal of Medical Case Reports.2017;[Epub] CrossRef - Thymus neuroendocrine tumors with CTNNB1 gene mutations, disarrayed ß-catenin expression, and dual intra-tumor Ki-67 labeling index compartmentalization challenge the concept of secondary high-grade neuroendocrine tumor: a paradigm shift
Alessandra Fabbri, Mara Cossa, Angelica Sonzogni, Paolo Bidoli, Stefania Canova, Diego Cortinovis, Maria Ida Abbate, Fiorella Calabrese, Nazarena Nannini, Francesca Lunardi, Giulio Rossi, Stefano La Rosa, Carlo Capella, Elena Tamborini, Federica Perrone,
Virchows Archiv.2017; 471(1): 31. CrossRef - Thymic large cell neuroendocrine carcinoma – a rare and aggressive tumor: a case report
Efared Boubacar, Gabrielle Atsame-Ebang, Sani Rabiou, Ammor Fatimazahra, Asmae Mazti, Ibrahim S. Sidibé, Layla Tahiri, Nawal Hammas, Ouadnouni Yassine, Smahi Mohamed, Chbani Laila, El Fatemi Hinde
Journal of Medical Case Reports.2017;[Epub] CrossRef - Clinicopathological features of neoplasms with neuroendocrine differentiation occurring in the liver
Yoriko Nomura, Osamu Nakashima, Jun Akiba, Sachiko Ogasawara, Shogo Fukutomi, Rin Yamaguchi, Hironori Kusano, Masayoshi Kage, Koji Okuda, Hirohisa Yano
Journal of Clinical Pathology.2017; 70(7): 563. CrossRef - Retrosternal goiter and thymic carcinoid: A rare co-existence
Abdulsalam Yaseen Taha, Nezar A. Almahfooz, Hassanain H. Khudair
Journal of the Egyptian Society of Cardio-Thoracic Surgery.2017; 25(4): 369. CrossRef - A case of large-cell neuroendocrine carcinoma of the thymus involving a patient with long-term survival after surgery
Qiuming Kan, Kohei Tagawa, Teruaki Ishida, Mitsuyo Nishimura, Katsuhiko Aoyama
The Journal of the Japanese Association for Chest Surgery.2017; 31(7): 927. CrossRef - Neuroendokrine Neoplasien des Mediastinums
L. Brcic, M. Heidinger, H. Popper
Der Pathologe.2016; 37(5): 434. CrossRef - Outcome of primary neuroendocrine tumors of the thymus: A joint analysis of the International Thymic Malignancy Interest Group and the European Society of Thoracic Surgeons databases
Pier Luigi Filosso, Xiaopan Yao, Usman Ahmad, Yilei Zhan, James Huang, Enrico Ruffini, William Travis, Marco Lucchi, Andreas Rimner, Alberto Antonicelli, Francesco Guerrera, Frank Detterbeck
The Journal of Thoracic and Cardiovascular Surgery.2015; 149(1): 103. CrossRef - Clinical Significance of Persistent Tumor in Bone Marrow during Treatment of High-risk Neuroblastoma
Young Bae Choi, Go Eun Bae, Na Hee Lee, Jung-Sun Kim, Soo Hyun Lee, Keon Hee Yoo, Ki Woong Sung, Hong Hoe Koo
Journal of Korean Medical Science.2015; 30(8): 1062. CrossRef - Tumor genetics and survival of thymic neuroendocrine neoplasms: A multi‐institutional clinicopathologic study
Philipp Ströbel, Andreas Zettl, Konstantin Shilo, Wen‐Yu Chuang, Andrew G. Nicholson, Yoshihiro Matsuno, Anthony Gal, Rolf Hubert Laeng, Peter Engel, Carlo Capella, Mirella Marino, John Kwok-Cheung Chan, Andreas Rosenwald, William Travis, Teri J. Franks,
Genes, Chromosomes and Cancer.2014; 53(9): 738. CrossRef - Disseminated large cell neuroendocrine carcinoma associated with ectopic adrenocorticotropic hormone secretion
A Van der Walt, K Huddle, S Pather, A Korb
Journal of Endocrinology, Metabolism and Diabetes of South Africa.2014; 19(1): 40. CrossRef - Morphologic Alteration of Metastatic Neuroblastic Tumor in Bone Marrow after Chemotherapy
Go Eun Bae, Yeon-Lim Suh, Ki Woong Sung, Jung-Sun Kim
Korean Journal of Pathology.2013; 47(5): 433. CrossRef
- A Case of Stage IV Thymic Typical Carcinoid with Multiple Bone Metastases
- A Soft Tissue Perineurioma and a Hybrid Tumor of Perineurioma and Schwannoma
- Ji Young Park, Nam Jo Park, Sang Pyo Kim, Kun Young Kwon, Sang Sook Lee
- Korean J Pathol. 2012;46(1):75-78. Published online February 23, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.1.75
- 9,179 View
- 64 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Perineuriomas are composed of differentiated perineurial cells. Perineuriomas have been recently recognized by the immunoreactivity for epithelial membrane antigen (EMA). Microscopically, perineuriomas show proliferation of spindle cells with wavy nuclei and delicate elongated bipolar cytoplasmic processes. The tumor cells are usually negative for the S-100 protein. Ultrastructurally, perineurial cells reveal slender, nontapered processes containing pinocytic vesicles and discontinuous basal lamina. Interestingly, hybrid tumors of benign peripheral nerve sheath tumor (PNST) have been recently reported by using immunohistochemical and ultrastructural investigations. Herein, we report a case of soft tissue perineurioma arising in the skin of a 56-year-old female; another case of a hybrid tumor of perineurioma and schwannoma in the posterior mediastinum occurred in a 53-year-old male, which is the first case of the hybrid PNST tumor reported in Korea.
-
Citations
Citations to this article as recorded by- Plexiform Fibromyxoma of the Gastric Body: A Rare Benign Mesenchymal Tumor in an Unconventional Location
Anan Bseiso, Dalia Ibrahim
International Journal of Surgical Pathology.2025;[Epub] CrossRef - Neurogenic tumours of the posterior mediastinum and differential diagnosis considerations
Michael A den Bakker, Annikka Weissferdt
Histopathology.2024; 84(1): 238. CrossRef - Hybrid tumors with perineurioma components: a systematic review of the literature and illustrative case
Karina A. Lenartowicz, Dileep D. Monie, Kimberly K. Amrami, Christopher J. Klein, Caterina Giannini, Robert J. Spinner
Acta Neurochirurgica.2022; 165(4): 935. CrossRef - Hybrid Schwannoma/Perineurioma: Morphologic Variations and Genetic Profiles
Takanori Hirose, Anna Kobayashi, Sumihito Nobusawa, Naoe Jimbo
Applied Immunohistochemistry & Molecular Morphology.2021; 29(6): 433. CrossRef - Mesenchymal Tumors of the Mediastinum: An Update on Diagnostic Approach
Joon Hyuk Choi, Jae Y. Ro
Advances in Anatomic Pathology.2021; 28(5): 351. CrossRef - Neurogenic Tumors of the Mediastinum
Erika F. Rodriguez, Robert Jones, Daniel Miller, Fausto J. Rodriguez
Seminars in Diagnostic Pathology.2020; 37(4): 179. CrossRef - A Rare Perineurioma/Granular Cell Tumor Hybrid Peripheral Nerve Sheath Tumor
Koorosh Haghayeghi, Gladys Telang, Sonja Chen, Jack Bevivino, Shamlal Mangray, Yiang Hui, Leslie Robinson-Bostom
The American Journal of Dermatopathology.2020; 42(10): 762. CrossRef - Hybrid peripheral nerve sheath tumors
Emine KILIÇ BAĞIR, Arbil AÇIKALIN, Gülfiliz GÖNLÜŞEN, Suzan ZORLUDEMİR, Mehmet Ali DEVECİ
Cukurova Medical Journal.2019; 44(3): 804. CrossRef - Primary intraosseous hybrid epithelioid schwannoma/perineurioma in the proximal tibia: a case report of benign hybrid neoplasm with local hypercellularity
Yuejiao Lang, Dawei Liu, Pei Xiang, Jilin Wang, Yang Li
Diagnostic Pathology.2019;[Epub] CrossRef - Hybrid peripheral nerve sheath tumors: report of five cases and detailed review of literature
Nasir Ud Din, Zubair Ahmad, Jamshid Abdul-Ghafar, Rashida Ahmed
BMC Cancer.2017;[Epub] CrossRef - Primary intraosseous hybrid nerve sheath tumor of femur: A hitherto undescribed occurrence in bone with secondary aneurysmal bone cyst formation resulting in pathological fracture
Louis Tsun Cheung Chow
Pathology - Research and Practice.2015; 211(5): 409. CrossRef - Mesenchymal tumours of the mediastinum—part II
Michael A. den Bakker, Alexander Marx, Kiyoshi Mukai, Philipp Ströbel
Virchows Archiv.2015; 467(5): 501. CrossRef - Primary pleural hybrid cellular schwannoma/perineurioma: A case report
Danny Soria-Céspedes, Carlos Robles-Vidal, Arturo Gómez-González, Rosalinda Peñaloza-Ramírez, Carlos Ortiz-Hidalgo
Respiratory Investigation.2014; 52(4): 269. CrossRef - Hybrid peripheral nerve sheath tumour with intermingled perineuriomatous and schwannomatous areas reflected in skin ultrasonography image
H. Saeki, K. Ito, Y. Nobeyama, T. Ishiji, M. Fukunaga, H. Nakagawa
Clinical and Experimental Dermatology.2014; 39(6): 747. CrossRef - Périneuriome extraneural des tissus mous localisé au nez
A. Zaouak, R. Benmously, M. Belhadj Salah, W. Koubaa, A. Debbiche, I. Mokhtar
Annales de Dermatologie et de Vénéréologie.2013; 140(8-9): 540. CrossRef
- Plexiform Fibromyxoma of the Gastric Body: A Rare Benign Mesenchymal Tumor in an Unconventional Location
- Interobserver Variability in Diagnosing High-Grade Neuroendocrine Carcinoma of the Lung and Comparing It with the Morphometric Analysis
- Seung Yeon Ha, Joungho Han, Wan-Seop Kim, Byung Seong Suh, Mee Sook Roh
- Korean J Pathol. 2012;46(1):42-47. Published online February 23, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.1.42
- 9,570 View
- 48 Download
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Distinguishing small cell lung carcinoma (SCLC) and large cell neuroendocrine carcinoma (LCNEC) of the lung is difficult with little information about interobserver variability.
Methods One hundred twenty-nine cases of resected SCLC and LCNEC were independently evaluated by four pathologists and classified according to the 2004 World Health Organization criteria. Agreement was regarded as "unanimous" if all four pathologists agreed on the classification. The kappa statistic was calculated to measure the degree of agreement between pathologists. We also measured cell size using image analysis, and receiver-operating-characteristic curve analysis was performed to evaluate cell size in predicting the diagnosis of high-grade neuroendocrine (NE) carcinomas in 66 cases.
Results Unanimous agreement was achieved in 55.0% of 129 cases. The kappa values ranged from 0.35 to 0.81. Morphometric analysis reaffirmed that there was a continuous spectrum of cell size from SCLC to LCNEC and showed that tumors with cells falling in the middle size range were difficult to categorize and lacked unanimous agreement.
Conclusions Our results provide an objective explanation for considerable interobserver variability in the diagnosis of high-grade pulmonary NE carcinomas. Further studies would need to define more stringent and objective definitions of cytologic and architectural characteristics to reliably distinguish between SCLC and LCNEC.
-
Citations
Citations to this article as recorded by- Case report: A patient with EGFR L861Q positive adenosquamous lung carcinoma transforming into large cell neuroendocrine cancer after treatment with Almonertinib
Kele Cheng, Yong Zhu, Ran Sang, Zhongsheng Kuang, Yang Cao
Frontiers in Oncology.2025;[Epub] CrossRef - Deep Learning–Based Retinoblastoma Protein Subtyping of Pulmonary Large-Cell Neuroendocrine Carcinoma on Small Hematoxylin and Eosin–Stained Specimens
Teodora E. Trandafir, Frank W.J. Heijboer, Farhan Akram, Jules L. Derks, Yunlei Li, Lisa M. Hillen, Ernst-Jan M. Speel, Zsolt Megyesfalvi, Balazs Dome, Andrew P. Stubbs, Anne-Marie C. Dingemans, Jan H. von der Thüsen
Laboratory Investigation.2025; 105(9): 104192. CrossRef - Treatment outcomes in patients with stage IV large cell neuroendocrine carcinoma: a nationwide registry study
Frank W.J. Heijboer, Jules L. Derks, Francien H. van Nederveen, Lisa M. Hillen, Michael A. den Bakker, Teodora Radonic, Ronald A.M. Damhuis, Ernst-Jan M. Speel, Jan H. von der Thüsen, Anne-Marie C. Dingemans
Lung Cancer.2025; 210: 108830. CrossRef - Updates on lung neuroendocrine neoplasm classification
Giulia Vocino Trucco, Luisella Righi, Marco Volante, Mauro Papotti
Histopathology.2024; 84(1): 67. CrossRef - Recent advancement of HDAC inhibitors against breast cancer
Syed Abdulla Mehmood, Kantrol Kumar Sahu, Sounok Sengupta, Sangh Partap, Rajshekhar Karpoormath, Brajesh Kumar, Deepak Kumar
Medical Oncology.2023;[Epub] CrossRef - Genomic Feature of a Rare Case of Mix Small-Cell and Large-Cell Neuroendocrine Lung Carcinoma: A Case Report
Youcai Zhu, Feng Zhang, Dong Yu, Fang Wang, Manxiang Yin, Liangye Chen, Chun Xiao, Yueyan Huang, Feng Ding
Frontiers in Oncology.2022;[Epub] CrossRef - Small-Cell Carcinoma of the Lung: What We Learned about It?
Luisella Righi, Marco Volante, Mauro Papotti
Acta Cytologica.2022; 66(4): 257. CrossRef - Hierarchical identification of a transcriptional panel for the histological diagnosis of lung neuroendocrine tumors
Juxuan Zhang, Jiaxing Deng, Xiao Feng, Yilong Tan, Xin Li, Yixin Liu, Mengyue Li, Haitao Qi, Lefan Tang, Qingwei Meng, Haidan Yan, Lishuang Qi
Frontiers in Genetics.2022;[Epub] CrossRef - Immunohistochemical Staining With Neuroendocrine Markers is Essential in the Diagnosis of Neuroendocrine Neoplasms of the Esophagogastric Junction
Dea N.M. Jepsen, Anne-Marie K. Fiehn, Rajendra S. Garbyal, Ulla Engel, Jakob Holm, Birgitte Federspiel
Applied Immunohistochemistry & Molecular Morphology.2021; 29(6): 454. CrossRef - Improving differential diagnosis of pulmonary large cell neuroendocrine carcinoma and small cell lung cancer via a transcriptomic, biological pathway-based machine learning model
Junhong Guo, Likun Hou, Wei Zhang, Zhengwei Dong, Lei Zhang, Chunyan Wu
Translational Oncology.2021; 14(12): 101222. CrossRef - Are Neuroendocrine Negative Small Cell Lung Cancer and Large Cell Neuroendocrine Carcinoma with WT RB1 two Faces of the Same Entity?
Dmitriy Sonkin, Anish Thomas, Beverly A Teicher
Lung Cancer Management.2019;[Epub] CrossRef - Ki-67 labeling index of neuroendocrine tumors of the lung has a high level of correspondence between biopsy samples and surgical specimens when strict counting guidelines are applied
Alessandra Fabbri, Mara Cossa, Angelica Sonzogni, Mauro Papotti, Luisella Righi, Gaia Gatti, Patrick Maisonneuve, Barbara Valeri, Ugo Pastorino, Giuseppe Pelosi
Virchows Archiv.2017; 470(2): 153. CrossRef - The Use of Immunohistochemistry Improves the Diagnosis of Small Cell Lung Cancer and Its Differential Diagnosis. An International Reproducibility Study in a Demanding Set of Cases
Erik Thunnissen, Alain C. Borczuk, Douglas B. Flieder, Birgit Witte, Mary Beth Beasley, Jin-Haeng Chung, Sanja Dacic, Sylvie Lantuejoul, Prudence A. Russell, Michael den Bakker, Johan Botling, Elisabeth Brambilla, Erienne de Cuba, Kim R. Geisinger, Kenzo
Journal of Thoracic Oncology.2017; 12(2): 334. CrossRef - Reply to Letter “The Use of Immunohistochemistry Improves the Diagnosis of Small Cell Lung Cancer and Its Differential Diagnosis. An International Reproducibility Study in a Demanding Set of Cases.”
Erik Thunnissen, Birgit I. Witte, Masayuki Noguchi, Yasushi Yatabe
Journal of Thoracic Oncology.2017; 12(6): e70. CrossRef - What clinicians are asking pathologists when dealing with lung neuroendocrine neoplasms?
Giuseppe Pelosi, Alessandra Fabbri, Mara Cossa, Angelica Sonzogni, Barbara Valeri, Luisella Righi, Mauro Papotti
Seminars in Diagnostic Pathology.2015; 32(6): 469. CrossRef - Unraveling Tumor Grading and Genomic Landscape in Lung Neuroendocrine Tumors
Giuseppe Pelosi, Mauro Papotti, Guido Rindi, Aldo Scarpa
Endocrine Pathology.2014; 25(2): 151. CrossRef - Grading the neuroendocrine tumors of the lung: an evidence-based proposal
G Rindi, C Klersy, F Inzani, G Fellegara, L Ampollini, A Ardizzoni, N Campanini, P Carbognani, T M De Pas, D Galetta, P L Granone, L Righi, M Rusca, L Spaggiari, M Tiseo, G Viale, M Volante, M Papotti, G Pelosi
Endocrine-Related Cancer.2014; 21(1): 1. CrossRef - Controversial issues and new discoveries in lung neuroendocrine tumors
Giuseppe Pelosi, Kenzo Hiroshima, Mari Mino-Kenudson
Diagnostic Histopathology.2014; 20(10): 392. CrossRef - BAI3, CDX2 and VIL1: a panel of three antibodies to distinguish small cell from large cell neuroendocrine lung carcinomas
Muhammad F Bari, Helen Brown, Andrew G Nicholson, Keith M Kerr, John R Gosney, William A Wallace, Irshad Soomro, Salli Muller, Danielle Peat, Jonathan D Moore, Lesley A Ward, Maxim B Freidin, Eric Lim, Manu Vatish, David R J Snead
Histopathology.2014; 64(4): 547. CrossRef - Neuroendocrine tumours—challenges in the diagnosis and classification of pulmonary neuroendocrine tumours
M A den Bakker, F B J M Thunnissen
Journal of Clinical Pathology.2013; 66(10): 862. CrossRef - Morphologic Analysis of Pulmonary Neuroendocrine Tumors
Seung Seok Lee, Myunghee Kang, Seung Yeon Ha, Jungsuk An, Mee Sook Roh, Chang Won Ha, Jungho Han
Korean Journal of Pathology.2013; 47(1): 16. CrossRef - Altered expression of microRNA miR‐21, miR‐155, and let‐7a and their roles in pulmonary neuroendocrine tumors
Hyoun Wook Lee, Eun Hee Lee, Seung Yeon Ha, Chang Hun Lee, Hee Kyung Chang, Sunhee Chang, Kun Young Kwon, Il Seon Hwang, Mee Sook Roh, Jeong Wook Seo
Pathology International.2012; 62(9): 583. CrossRef
- Case report: A patient with EGFR L861Q positive adenosquamous lung carcinoma transforming into large cell neuroendocrine cancer after treatment with Almonertinib
- Nuclear Image Analysis Study of Neuroendocrine Tumors
- Meeja Park, Taehwa Baek, Jongho Baek, Hyunjin Son, Dongwook Kang, Jooheon Kim, Hyekyung Lee
- Korean J Pathol. 2012;46(1):38-41. Published online February 23, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.1.38
- 8,071 View
- 41 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Background There is a subjective disagreement about nuclear chromatin in the field of pathology. Objective values of red, green, and blue (RGB) light intensities for nuclear chromatin can be obtained through a quantitative analysis using digital images.
Methods We examined 10 cases of well differentiated neuroendocrine tumors of the rectum, small cell lung carcinomas, and moderately differentiated squamous cell lung carcinomas respectively. For each case, we selected 30 representative cells and captured typical microscopic findings. Using an image analyzer, we determined the longest nuclear line profiles and obtained graph files and Excel data on RGB light intensities. We assessed the meaningful differences in graph files and Excel data among the three different tumors.
Results The nucleus of hematoxylin and eosin-stained tumor cells was expressed as a combination of RGB light sources. The highest intensity was from blue, whereas the lowest intensity was from green. According to the graph files, green showed the most noticeable change in the light intensity, which is consistent with the difference in standard deviations.
Conclusions The change in the light intensity for green has an important implication for differentiating between tumors. Specific features of the nucleus can be expressed in specific values of RGB light intensities.
-
Citations
Citations to this article as recorded by- Difference of the Nuclear Green Light Intensity between Papillary Carcinoma Cells Showing Clear Nuclei and Non-neoplastic Follicular Epithelia in Papillary Thyroid Carcinoma
Hyekyung Lee, Tae Hwa Baek, Meeja Park, Seung Yun Lee, Hyun Jin Son, Dong Wook Kang, Joo Heon Kim, Soo Young Kim
Journal of Pathology and Translational Medicine.2016; 50(5): 355. CrossRef - Comparison of diagnostic accuracy between CellprepPlus® and ThinPrep® liquid‐based preparations in effusion cytology
Yong‐Moon Lee, Ji‐Yong Hwang, Seung‐Myoung Son, Song‐Yi Choi, Ho‐Chang Lee, Eun‐Joong Kim, Hye‐Suk Han, Jin young An, Joung‐Ho Han, Ok‐Jun Lee
Diagnostic Cytopathology.2014; 42(5): 384. CrossRef
- Difference of the Nuclear Green Light Intensity between Papillary Carcinoma Cells Showing Clear Nuclei and Non-neoplastic Follicular Epithelia in Papillary Thyroid Carcinoma
- Composite Tumor of Adenocarcinoma and Small Cell Neuroendocrine Carcinoma of the Uterine Cervix: A Case Report.
- Hye Rim Park, Yong Woo Lee, Young Euy Park
- J Pathol Transl Med. 1990;1(1):111-120.
- 2,122 View
- 45 Download
-
 Abstract
Abstract
 PDF
PDF - Small cell neuroendocrine carcinoma of the uterine cervix is a distinct subtype of cervical cancer that appears analogous to oat cell carcinoma and carcinoid tumors of the lung. It has been assumed to be derived from the neural crest via argyrophilic cells in the normal endocervix. We have recently encountered a case of small cell neuroendocrine carcinoma of the uterine cervix coexisting with adenocarcinoma which was argyrophil negative. A 66-year-old multiparous woman was admitted because of vaginal bleeding for 2 months. Cervicovaginal smear revealed several scattered clusters and sheets of monotonous small cells with some peripheral palisading in the background of hemorrhage and necrosis. Radical hysterectomy specimen revealed and ulcerofungating tumor on endocervical canal which was composed of two components. Major component of the tumor was made up of monomorphic population of small oval-shaped tumor cells arranged in sheets and partly in acinar structeres or trabecular fashion. Other component was adenocarcinoma, endocervical well-differentiated type. Argyropilia was present on the Grimelius stain and immunohistochemical studies revealed diffuse positivity to neuron-specific enolase and carcinoembryonic antigen. Electron microscopic examination showed clusters of small round to oval cells, which had a few well-formed desmosomes and several membrane-bound, dense-core neurosectetory granules.
- Fine needle aspiration cytology of malignant epithelial mesothelioma of the peritoneum.
- Sun Hee Sung, Kwang Gil Lee
- J Pathol Transl Med. 1991;2(1):43-50.
- 1,968 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - A case of malignant epithelial mesothelioma of the peritoneum diagnosed by fine needle aspiration cytology is described. The smear showed many individually scattered or clustered large round malignant epithelial cells intermingled with relatively small nonneoplastic mesothelial and mesenchymal cells. Papillary configurations with thick fibrous core were also seen. The malignant cells were virtually reminiscent of reactive mesothelial cells but they were larger in size and had more prominent nucleoli and more frequent binucleated or multinucleated cell formations than reactive mesothelial cells. The characteristic features of malignant cell of mesothelioma compared with the metastatic adenocarcinoma were relatively uniform cellular size, prominent round nucleoli, large round vesicular nuclei with finely granular chromatin pattern, smooth nuclear membrane, abundant glassy cytoplasm rather than bubbly mucin-containing cytoplasm and fuzzy cell border.
- Bilateral Frontal Polymicrogyria: An Autopsy Case Report.
- Yi Kyeong Chun, Jong Sun Choi, Je G Chi
- Korean J Pathol. 2011;45:S62-S65.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.S1.S62
- 3,516 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - Bilateral frontal polymicrogyria is a recently recognized syndrome characterized by symmetric polymicrogyria of both frontal lobes that presents with delayed motor and language development, spastic quadriparesis, and variable mental retardation. However, the postmortem findings of this syndrome are not fully elaborated. Here we describe an autopsy case of bilateral frontal polymicrogyria in a male fetus delivered at 22 weeks gestation due to extensive chorioamnionitis. The microscopic findings included a thinned cortical plate with fair neuronal maturation. There were no signs of neuronal damage and the white matter was unremarkable.
- Mixed Endocrine-Exocrine Carcinoma of Gallbladder Derived from Dysplasia.
- Min Jin Lhee, Ji Young Woo
- Korean J Pathol. 2011;45(5):537-541.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.5.537
- 3,446 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - A rare case of multiple mixed endocrine-exocrine carcinoma (MEEC) of gallbladder in a 68-year-old man is described. The lesions were two separate nodules (17x13x7 mm and 17 mm in length) on the mucosa, which were composed of predominant neuroendocrine carcinoma (NEC) infiltrating into the adventitia and minor portion of adenocarcinoma (AC) or high grade dysplasia (HGD) on the surface. Surrounding mucosa showed areas of low grade dysplasia (LGD). Two nodal metastases out of 16 nodes were found containing NEC component. By immunohistochemistry, human mutL homolog 1 (hMLH1), p53, human mutS homolog 2 (hMSH2) and human mutS homolog 6 (hMSH6) showed diffuse strong positive reaction in HGD, AC and NEC, contrasting with weak positive reaction in LGD. On genetic analysis, all lesions of HGD, AC, and NEC except for LGD showed positive loss of heterozygosity in D5S346 locus. For microsatellite instability and K-ras mutation tests, all lesions showed negative results. Common immunophenotypes and molecular results among HGD, AC, and NEC suggested that NEC of this MEEC was derived from the dysplasia-AC sequence.
- Ovarian Large Cell Neuroendocrine Carcinoma Associated with Endocervical-like Mucinous Borderline Tumor: A Case Report and Literature Review.
- Jun Mo Kim, Hyeong Chan Shin, Mi Jin Kim
- Korean J Pathol. 2011;45(5):523-528.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.5.523
- 5,049 View
- 34 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Ovarian large cell neuroendocrine carcinoma is a rare tumor that is usually associated with surface epithelial tumors. Mucinous tumors are most common surface epithelial component identified in reported cases. Ovarian mucinous tumor associated with large cell neuroendocrine carcinoma is almost always an intestinal type. However, large cell neuroendocrine carcinoma associated with pure mucinous borderline tumor of endocervical-like type has not been described previously. The present case report describes a large cell neuroendocrine carcinoma associated with endocervical-like mucinous borderline tumor of the ovary in a 35-year-old woman. The tumor was confirmed by histopathology and immunohistochemistry. A review of the pertinent literature is included.
-
Citations
Citations to this article as recorded by- The puzzle of gynecologic neuroendocrine carcinomas: State of the art and future directions
Giuseppe Caruso, Carolina Maria Sassu, Federica Tomao, Violante Di Donato, Giorgia Perniola, Margherita Fischetti, Pierluigi Benedetti Panici, Innocenza Palaia
Critical Reviews in Oncology/Hematology.2021; 162: 103344. CrossRef - Pathological features, clinical presentations and prognostic factors of ovarian large cell neuroendocrine carcinoma: a case report and review of published literature
Xiaohang Yang, Junyu Chen, Ruiying Dong
Journal of Ovarian Research.2019;[Epub] CrossRef - Primary pure large cell neuroendocrine carcinoma of the ovary
Chen-Hsien Lin, Yu-Chieh Lin, Mu-Hsien Yu, Her-Young Su
Taiwanese Journal of Obstetrics and Gynecology.2014; 53(3): 413. CrossRef - Pure Large Cell Neuroendocrine Carcinoma of Ovary: A Rare Clinical Entity and Review of Literature
P. N. Shakuntala, K. Uma Devi, K. Shobha, U. D. Bafna, M. Geetashree
Case Reports in Oncological Medicine.2012; 2012: 1. CrossRef
- The puzzle of gynecologic neuroendocrine carcinomas: State of the art and future directions
- Primary Hepatic Neuroblastoma: A Case Report.
- Geunyoung Jung, Jihun Kim
- Korean J Pathol. 2011;45(4):423-427.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.4.423
- 4,822 View
- 32 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Neuroblastoma is a malignant tumor of primordial neural crest origin. It usually develops along the sympathetic nervous system, such as the adrenal glands or paramedian sympathetic chain and metastasizes to the liver most frequently. However, a primary hepatic neuroblastoma has not been reported yet. Here, we report a case of 29-year-old woman who presented with a solitary hepatic mass. Grossly, the mass was large, creamy, rubbery firm, and showed focal hemorrhage and central cavitation. Microscopically, the tumor cells were arranged in small nests of spindle to ovoid cells with abundant neuropil. The neuroblastic nature of the tumor was confirmed by immunohistochemistry and electron microscopy. No extrahepatic mass was found, despite a thorough systemic survey such as chest and abdominopelvic computed tomography (CT) scans and a whole body positron emission tomography-CT study. To the best of our knowledge, this is the first report of a bona fide primary hepatic neuroblastoma.
-
Citations
Citations to this article as recorded by- Primary hepatic neuroblastoma in a 19-month-old child: A case report
Jovana Dimić, Dejan Skorić, Aleksandar Sretenović, Slaviša Đuričić
Medicinska istrazivanja.2022; 55(2): 41. CrossRef - Morphologic Alteration of Metastatic Neuroblastic Tumor in Bone Marrow after Chemotherapy
Go Eun Bae, Yeon-Lim Suh, Ki Woong Sung, Jung-Sun Kim
Korean Journal of Pathology.2013; 47(5): 433. CrossRef
- Primary hepatic neuroblastoma in a 19-month-old child: A case report
- Composite Pheochromocytoma or Paraganglioma of Adrenal Gland: A Case Report with Immunohistochemical Studies and Electron Microscopic Examination.
- Hyeyoon Chang, Hoiseon Jeong, Younghye Kim, Sung Hye Park, Aeree Kim
- Korean J Pathol. 2011;45(3):306-310.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.3.306
- 4,659 View
- 38 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Composite pheochromocytoma or paraganglioma of the adrenal gland is a well-recognized, yet extremely rare tumor with only one case reported in Korea. We report a case of incidentally found composite pheochromocytoma and ganglioneuroma of the adrenal gland in a 44-year-old female composed of intermingled components of pheochromocytom, ganglioneuroma, and cells with intermediate features. On immunohistochemical staining, the pheochromocytoma component was positive for synaptophysin and chromogranin, but negative for S-100 protein. Staining for the S-100 protein revealed sustentacular cells which formed a peripheral coat around the "Zellballen" and Schwann cells. The Fontana-Masson stain defined neuromelanin granules of ganglion cells and the ganglion cells expressed neural markers such as neurofilament proteins. Ultrastructural findings revealed pheochromocytes with a round or ovoid nucleus and occasionally prominent nucleolus containing numerous adrenaline and noradrenaline granules.
-
Citations
Citations to this article as recorded by- Bilateral pheochromocytoma with ganglioneuroma component associated with multiple neuroendocrine neoplasia type 2A: a case report
Boubacar Efared, Gabrielle Atsame-Ebang, Soufiane Tahirou, Khalid Mazaz, Nawal Hammas, Hinde El Fatemi, Laila Chbani
Journal of Medical Case Reports.2017;[Epub] CrossRef
- Bilateral pheochromocytoma with ganglioneuroma component associated with multiple neuroendocrine neoplasia type 2A: a case report
- SSTR2A Protein Expression in Neuroendocrine Neoplasms of the Colorectum.
- Young Eun Kim, Jeeyun Lee, Young Suk Park, Kyoung Mee Kim
- Korean J Pathol. 2011;45(3):276-280.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.3.276
- 4,185 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Expression studies of somatostatin receptor type 2A (SSTR2A) in neuroendocrine neoplasms (NENs) led to the development of clinically relevant diagnostic and therapeutic strategies. However, most of these strategies used in-house-developed antibodies and were focused on lung tumors. We evaluated commercially available SSTR2A antibodies in NENs of the colorectum to observe their subcellular localization and distribution within the resected tumor.
METHODS
The immunohistochemistry of 77 NENs located in the colorectum were studied using a commercially available antibody against SSTR2A.
RESULTS
Most neuroendocrine tumors (NET) grade (G)1 and G2 expressed the SSTR2A in the cytoplasm with apical or luminal localization. However, all neuroendocrine carcinomas (NEC) G3 were negative for SSTR2A.
CONCLUSIONS
Our data indicate that SSTR2A immunohistochemistry shows cytoplasmic staining with distinct subcellular localization in most NET G1 in the colorectum using a commercially available antibody. Low or no expression of SSTR2A in NET G2 and NEC G3 raises the possibility that SSTR2A may correlate with histologic differentiation and proliferative activity. Further validation studies in large case series are needed.
- Distinction of Pulmonary Large Cell Neuroendocrine Carcinoma from Small Cell Lung Carcinoma Using a Panel of Bcl-2, p63, and 34betaE12.
- Jun Zhe Li, Chan Choi, Yoo Duk Choi, Kook Joo Na
- Korean J Pathol. 2011;45(2):170-174.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.2.170
- 3,868 View
- 33 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Making the distinction between large cell neuroendocrine carcinoma (LCNEC) and small cell lung carcinoma (SCLC) is difficult in some samples of biopsy tissues, but we have to separate LCNEC from SCLC because the two types of cancer may need different therapy and they have different prognostic implications. Thus far, there are no specific immunohistochemical markers that allow distinguishing these two kinds of tumors.
METHODS
We performed an immunohistochemical analysis to study the expressions of p63, Bcl-2, and 34betaE12 and to investigate whether these 3 molecules have correlations in LCNEC and SCLC. We also evaluated the expression of the neuroendocrine markers chromogranin, synaptophysin and CD56.
RESULTS
A statistical analysis was performed for p63, Bcl-2, and 34betaE12 in separate and combined panels. According to the combinations of p63, Bcl-2, and 34betaE12, there were frequent expressions of p63-/Bcl-2+ or Bcl-2+/34betaE12- in the SCLC, and there was a superior proportion of them in the SCLC rather than that in the LCNEC. The p63-/Bcl-2+ and Bcl-2+/34betaE12- antibody combinations showed higher specificities compared to any single antibody for diagnosing SCLC.
CONCLUSIONS
Bcl-2 and selective p63 or 34betaE12 made up a most useful panel of markers for making the differential diagnosis of LCNEC and SCLC. -
Citations
Citations to this article as recorded by- Evaluation of Serum LDH, p53 and BCL2 in Lung Cancer Patients
Pawar Komal, Rajvik Kruti, Vora Hemangini
Gujarat Cancer Society Research Journal.2020; 22(2): 22. CrossRef
- Evaluation of Serum LDH, p53 and BCL2 in Lung Cancer Patients
- Vascular Endothelial Growth Factor Bioactivity and Its Receptors in Patients with Acute Respiratory Distress Syndrome.
- Simona Gurzu, Ioan Jung, Leonard Azamfirei, Bong Young Shin, Raluca Solomon, Daria Demian, Judith Kovacs, Han Kyeom Kim
- Korean J Pathol. 2011;45(2):139-145.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.2.139
- 4,539 View
- 26 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Pathogenesis of acute respiratory distress syndrome (ARDS) is a controversial issue. Few studies have analyzed the possible role of vascular endothelial growth factor (VEGF) and its receptors in this lesion.
METHODS
We compared the immunohistochemical expression of VEGF, its receptors (VEGFR1, VEGFR2) and CD68, in normal lungs and lungs with ARDS. Fifty necropsy cases and 12 lung biopsies with ARDS were analyzed. In total, eight cases were in the early stage and 54 cases were in late stage of ARDS. In addition, the serum level of VEGF165 was also determined.
RESULTS
In normal lungs, all antibodies marked the endothelial cells (EC) and pneumocytes (PC), except for CD68, which was expressed in the alveolar macrophages. In early ARDS, the intensity of VEGF165 and VEGFR2 decreased in both EC and PC. VEGF121 was absent in PC but its expression increased in bronchial epithelium. VEGFR1 was expressed in the integral PC. In late ARDS, VEGF165 down-regulation was more significant in PC and EC but its intensity increased in hyaline membranes (HM). In some cases, HM were CD68 positive. The serum level of VEGF165 was up-regulated, while VEGF165 intensity in PC decreased and the HM appeared in alveolar spaces.
CONCLUSIONS
Sporadic positivity of HM for CD68 and decreasing of VEGF165 expression in EC proved that VEGF165 is produced by PC, destroyed macrophages, and extravasated serum. -
Citations
Citations to this article as recorded by- Hallazgos similares al COVID-19 en un caso fatal de neumonía intersticial descamativa asociada con glomerulonefritis por IgA en una niña de 13 meses de edad
Simona Gurzu, Catalin-Bogdan Satala, Lorena Elena Melit, Adrian Streinu-Cercel, Dan Otelea, Brandusa Capalna, Claudiu Ioan Puiac, Janos Szederjesi, Ioan Jung
Kompass Neumología.2021; 3(2): 69. CrossRef - COVID-19 Like Findings in a Fatal Case of Idiopathic Desquamative Interstitial Pneumonia Associated With IgA Glomerulonephritis in a 13-Month-Old Child
Simona Gurzu, Catalin Bogdan Satala, Lorena Elena Melit, Adrian Streinu-Cercel, Dan Otelea, Brandusa Capalna, Claudiu Ioan Puiac, Janos Szederjesi, Ioan Jung
Frontiers in Pediatrics.2020;[Epub] CrossRef
- Hallazgos similares al COVID-19 en un caso fatal de neumonía intersticial descamativa asociada con glomerulonefritis por IgA en una niña de 13 meses de edad
- Use of Calretinin, CD56, and CD34 for Differential Diagnosis of Schwannoma and Neurofibroma.
- Ji Young Park, Hoon Park, Nam Jo Park, June Sik Park, Hyun Jung Sung, Sang Sook Lee
- Korean J Pathol. 2011;45(1):30-35.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.1.30
- 6,362 View
- 174 Download
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It is important to differentiate between schwannomas and neurofibromas for the cases in which the histopathologic features overlap. Depending on the tumor type, surgeons can decide on a treatment method and whether to preserve or sacrifice the nerve; the possibility of malignant transformation in the case of neurofibromas also needs to be considered.
METHODS
We studied 101 cases of schwannoma and 103 cases of neurofibroma. All the hematoxylin and eosin slides for these cases were reviewed, and tissue microarrays were prepared from the representative areas. Immunohistochemical analysis was performed using antibodies for S-100 protein, calretinin, CD56 and CD34.
RESULTS
All the tumors except 3 neurofibromas were positive for the S-100 protein. Calretinin was found in 26.7% of the schwannomas (27/101), but it was not found in any of the neurofibromas. CD56 was positive in 77.2% of the schwannomas (78/101) and in 9.8% of the neurofibromas (10/102). CD34 was positive in 42.5% of the schwannomas (43/101) and in 80.2% of the neurofibromas (81/101). Statistically, calretinin was significantly specific for schwannomas (p<0.001) and CD56 was also sensitive for these tumors (p<0.001). On the other hand, a CD34 expression seemed highly sensitive (p<0.001) for neurofibromas.
CONCLUSIONS
We concluded that combined immunohistochemical analysis for calretinin, CD56, and CD34 may be very useful for differentiating schwannomas from neurofibromas. -
Citations
Citations to this article as recorded by- Microcystic Pseudoglandular Cutaneous Neurofibroma: The First Japanese Case of a Rare Neurofibroma Variant
Shinichi Nakazato, Yasuyuki Fujita, Takashi Anan
The Journal of Dermatology.2025;[Epub] CrossRef - A rare case of giant intercostal nerve schwannoma
Bandari A. Ahmed, Ashley I. Simpson
International Surgery Journal.2025; 12(7): 1142. CrossRef - HISTOMORPHOLOGICAL SPECTRUM AND IMMUNOHISTOCHEMICAL EXPRESSION OF S100 AND CD56 AMONG TUMORS OF PERIPHERAL NERVES-A CROSS-SECTIONAL STUDY
KARTHIK SIGAMANI, SHOBANA B, NAYANA CHANDRAN
Asian Journal of Pharmaceutical and Clinical Research.2025; : 142. CrossRef - Histomorphological Spectrum and Diagnostic Utility of S100, SOX10, CD34, Calretinin, and Ki67 in the Evaluation of Schwannomas: A Retrospective Study of 26 Cases in a Tertiary Health Institute, Zaria-Nigeria
Zainab Ali Adamu, Mikhail O. Buhari, Abdullahi Mohammed
Journal of West African College of Surgeons.2025;[Epub] CrossRef - The skin's secret script: fingerprints of CD34 and the dolphin dance of Schwann cells
Vijay Joshi, Ketki Bhoite, Vidya Kharkar, Rajiv Joshi, Surupa Das
International Journal of Research in Dermatology.2025; 11(6): 541. CrossRef - Breast schwannoma: review of entity and differential diagnosis
Sandra Ixchel Sanchez, Ashley Cimino-Mathews
Journal of Pathology and Translational Medicine.2025; 59(6): 353. CrossRef - Primary Pulmonary Neurofibroma: Diagnostic Approach to a Common Tumor at an Uncommon Site – A Case Report
Rakesh Kumar Gupta, Bhoomika Kaushik, Shaurya Vijayran, Ranganath Ganga, Mudalsha Ravina
SN Comprehensive Clinical Medicine.2025;[Epub] CrossRef - Ancient cervical vagal schwannoma and an interposition great auricular to vagus nerve graft
Nicholas Figaro, Rickhi Ramoutar, David Richards, Rodolfo Arozarena, Mala Geelal, Solaiman Juman
Edorium Journal of Otolaryngology.2024; 5(2): 1. CrossRef - Lung schwannomas, an unusual entity
Nazia M. Walvir, Rumana H. Makhdoomi, Meesa Zargar, Aiffa Aiman, Shadab Maqsood
Lung India.2023; 40(1): 70. CrossRef - A Spectrum of Histomorphological and Immunohistochemical Expression Profiles of S-100, CD56 and Calretinin in Benign Peripheral Nerve Sheath Tumours
Poornima Jaiswal, Anand CD, Jaison Jacob John
Cureus.2023;[Epub] CrossRef - An unusual diffuse CD34 staining in an olfactory groove cellular schwannoma: Case report
Marios Theologou, Jorge D. Perez Ruiz, Panagiotis Varoutis, Nicolaos Flaris, Nikolaos `Skoulios
Archivos de Neurociencias.2023;[Epub] CrossRef - An unusual diffuse CD34 staining in an olfactory groove cellular schwannoma: Case report
Marios Theologou, Jorge D. Perez Ruiz, Panagiotis Varoutis, Nicolaos Flaris, Nikolaos `Skoulios
Archivos de Neurociencias.2023;[Epub] CrossRef - Intranodal Neurofibroma: A Case Report and Literature Review
Steven H. Adams, Tara L. Huston, Daniel Lozeau
The American Journal of Dermatopathology.2022; 44(4): 306. CrossRef - A rare case of pseudoglandular schwannoma
Fadime Eda GÖKALP SATICI, Hamide SAYAR
Journal of Surgery and Medicine.2022; 6(4): 1. CrossRef - Gastric Schwannoma as an Important and Infrequent Differential Diagnosis of Gastric Mesenchymal Tumours: A Case Report and Review of Literature
Abdalla Saad Abdalla Al-Zawi, Salma Lahmadi, Saman Jalilzadeh Afshari, Ipshita Kak, Salem Alowami
Cureus.2022;[Epub] CrossRef - Spindle cell proliferations of the sigmoid colon, rectum and anus: a review with emphasis on perineurioma
Patrice Grech, John B Schofield
Histopathology.2020; 76(3): 342. CrossRef - Large retroperitoneal schwannoma: a rare cause of chronic back pain
Milan Radojkovic, Dragan Mihailovic, Miroslav Stojanovic, Danijela Radojković
Journal of International Medical Research.2018; 46(8): 3404. CrossRef - Nasal Septal Schwannoma
Hyun Jin Min, Seok Chan Hong, Kyung Soo Kim
Journal of Craniofacial Surgery.2017; 28(1): e97. CrossRef - Neurofibroma of the Colon: A Diagnostic Mimicker of Gastrointestinal Stromal Tumor
Soomin Ahn, Choon Sik Chung, Kyoung-Mee Kim
Case Reports in Gastroenterology.2016; 10(3): 674. CrossRef - Solitary Epibulbar Neurofibroma in Older Adult Patients
Thais Shiota Tanaka, Victor M. Elner, Hakan Demirci
Cornea.2015; 34(4): 475. CrossRef - Syncytial nuclear aggregates in normal placenta show increased nuclear condensation, but apoptosis and cytoskeletal redistribution are uncommon
S.J. Coleman, L. Gerza, C.J.P. Jones, C.P. Sibley, J.D. Aplin, A.E.P. Heazell
Placenta.2013; 34(5): 449. CrossRef - Analysis of syncytial nuclear aggregates in preeclampsia shows increased sectioning artefacts and decreased inter-villous bridges compared to healthy placentas
S.J. Calvert, C.J.P. Jones, C.P. Sibley, J.D. Aplin, A.E.P. Heazell
Placenta.2013; 34(12): 1251. CrossRef
- Microcystic Pseudoglandular Cutaneous Neurofibroma: The First Japanese Case of a Rare Neurofibroma Variant
- Immunohistochemical Identification of Pneumocystis jirovecii in Liquid-based Cytology of Bronchoalveolar Lavage: Nine Cases Report.
- Jeong Hyeon Lee, Ji Young Lee, Mi Ran Shin, Hyeong Kee Ahn, Chul Whan Kim, Insun Kim
- Korean J Pathol. 2011;45(1):115-118.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.1.115
- 4,792 View
- 48 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pneumocystis pneumonia (PCP) is caused by the yeast-like fungus Pneumocystis jirovecii, which is specific to humans. PCP could be a source of opportunistic infection in adults that are immunosuppressed and children with prematurity or malnutrition. The diagnosis should be confirmed by identification of the causative organism, by analysis of the sputum, a bronchoalveolar lavage or a tissue biopsy. In both histologic and cytologic specimens, the cysts are contained within frothy exudates, which form aggregated clumps. The cysts often collapse forming crescent-shaped bodies that resemble ping-pong balls. We recently diagnosed nine cases of PCP using an immunohistochemical stain for Pneumocystis. The patients consisted of five human immunodeficiency virus positive individuals, two renal transplant recipients, and two patients with a malignant disease. All nine patients were infected with P. jirovecii, which was positive for monoclonal antibody 3F6. In conclusion, the immunohistochemical stain used in this report is a new technique for the detection of P. jirovecii infection.
-
Citations
Citations to this article as recorded by- Metabolic Changes in Serum Metabolome of Beagle Dogs Fed Black Ginseng
Dahye Yoon, Ye Jin Kim, Wan Kyu Lee, Bo Ram Choi, Seon Min Oh, Young Seob Lee, Jae Kwang Kim, Dae Young Lee
Metabolites.2020; 10(12): 517. CrossRef - Effects of Red or Black Ginseng Extract in a Rat Model of Inflammatory Temporomandibular Joint Pain
Hyeon-Jeong Lee, Yun-Kyung Kim, Ja-Hyeong Choi, Jung-Hwa Lee, Hye-Jin Kim, Mi-Gyung Seong, Min-Kyung Lee
Journal of Dental Hygiene Science.2017; 17(1): 65. CrossRef - Value of Bronchoalveolar Lavage Fluid Cytology in the Diagnosis ofPneumocystis jiroveciiPneumonia: A Review of 30 Cases
Ji-Youn Sung, Joungho Han, Young Lyun Oh, Gee Young Suh, Kyeongman Jeon, Taeeun Kim
Tuberculosis and Respiratory Diseases.2011; 71(5): 322. CrossRef
- Metabolic Changes in Serum Metabolome of Beagle Dogs Fed Black Ginseng
- CK20 Negative and CK7 Positive Merkel Cell Carcinoma of the Conjunctiva: Brief Case Report.
- Jung Ha Shin, Jae Young Park, Hyun Seung Kim, Ok Ran Shin, Kyo Young Lee
- Korean J Pathol. 2010;44(6):675-678.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.6.675
- 6,413 View
- 57 Download
-
 Abstract
Abstract
 PDF
PDF - Merkel cell carcinoma (MCC) is an uncommon but potentially aggressive neuroendocrine carcinoma of the skin. It typically develops on sun-exposed areas of the head and neck, particularly the eyelid, periorbital region, and extremities. We report a case of unusually located MCC, presenting as a conjunctival mass, which has only been reported once in the English literature. An 83-year-old male presented with a 0.8 x 0.7 cm sized mass protruding from the lower fornix of the right conjunctiva. The mass was excised. The tumor was located in the submucosa without connection to the overlying mucosa. Light microscopic findings showed a carcinoma with undifferentiated small round cells and the presence of cytokeratin (CK AE1/3, CK7) and neuroendocrine markers. We established a diagnosis of MCC. As reported in the literature, the majority of MCCs are positive for CK20 but negative for CK7. But, this case showed an uncommon cytokeratin immunohistochemical profile of positive for CK7 and negative for CK20, suggesting a new immunophenotypic MCC variant.
- A Case of Endocrine Mucin-Producing Sweat Gland Carcinoma Co-existing with Mucinous Carcinoma: A Case Report.
- Sunhee Chang, Sang Hwa Shim, Mee Joo, Hanseong Kim, Yong Kyu Kim
- Korean J Pathol. 2010;44(1):97-100.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.1.97
- 5,514 View
- 51 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF - An endocrine mucin-producing sweat gland carcinoma (EMPSGC) is a rare skin tumor that most commonly occurs on the eyelids of elderly women. This tumor is morphologically analogous to endocrine ductal carcinoma in situ and solid papillary carcinoma of the breast. We describe one case of a 51-year-old male with an EMPSGC co-existing with mucinous carcinoma of the eyelid. The tumor was composed of dilated ducts with a smooth border and was partially filled with a papillary proliferation. Tumor cells were uniform, small-to-medium in size, and oval-to-polygonal with light eosinophilic cytoplasm. Nuclei were bland with diffusely stippled chromatin and inconspicuous nucleoli. Tumor cells expressed chromogranin, synaptophysin, estrogen and progesterone receptors, cytokeratin 7, and epithelial membrane antigen.
-
Citations
Citations to this article as recorded by- A Case of Endocrine Mucin-Producing Sweat Gland Carcinoma of the Eyelid
Ji Eon Kang, Sung Eun Kim, Suk-Woo Yang
Journal of the Korean Ophthalmological Society.2023; 64(2): 149. CrossRef - Endocrine mucin-producing sweat gland carcinoma: a systematic review and meta-analysis
Michael H. Froehlich, Keith R. Conti, Ivy I. Norris, Jordan J. Allensworth, Nicole A. Ufkes, Shaun A. Nguyen, Evelyn T. Bruner, Joel Cook, Terry A. Day
Journal of Dermatological Treatment.2022; 33(4): 2182. CrossRef - Next-generation sequencing analysis suggests varied multistep mutational pathogenesis for endocrine mucin-producing sweat gland carcinoma with comments on INSM1 and MUC2 suggesting a conjunctival origin
Joseph G. Mathew, Anita S. Bowman, Jad Saab, Klaus J. Busam, Kishwer Nehal, Melissa Pulitzer
Journal of the American Academy of Dermatology.2022; 86(5): 1072. CrossRef - Endocrine mucin‐producing sweat gland carcinoma and associated primary cutaneous mucinous carcinoma: Review of the literature
Rebecca Tian Mei Au, Manish M. Bundele
Journal of Cutaneous Pathology.2021; 48(9): 1156. CrossRef - An Update on Endocrine Mucin-producing Sweat Gland Carcinoma
Meghana Agni, Meisha L. Raven, Randy C. Bowen, Nora V. Laver, Patricia Chevez-Barrios, Tatyana Milman, Charles G. Eberhart, Steven Couch, Daniel D. Bennett, Daniel M. Albert, R. Nick Hogan, Paul O. Phelps, Hillary Stiefel, Norberto Mancera, Martin Hyrcza,
American Journal of Surgical Pathology.2020; 44(8): 1005. CrossRef - A Case of Endocrine Mucin-Producing Sweat Gland Carcinoma: Is it Still an Under-Recognized Entity?
Khaled A. Murshed, Mohamed Ben-Gashir
Case Reports in Dermatology.2020; 12(3): 255. CrossRef - Endocrine Mucin-Producing Sweat Gland Carcinoma, a Histological Challenge
Mary Anne Brett, Samih Salama, Gabriella Gohla, Salem Alowami
Case Reports in Pathology.2017; 2017: 1. CrossRef - Endocrine mucin‐producing sweat gland carcinoma occurring on extra‐facial site: a case report
Jia‐Huei Tsai, Tzu‐Lin Hsiao, Yi‐Ying Chen, Cheng‐Hsiang Hsiao, Jau‐Yu Liau
Journal of Cutaneous Pathology.2014; 41(6): 544. CrossRef - Endocrine Mucin-Producing Sweat Gland Carcinoma
Catharine A. Dhaliwal, Antonia Torgersen, Jonathan J. Ross, James W. Ironside, Asok Biswas
The American Journal of Dermatopathology.2013; 35(1): 117. CrossRef
- A Case of Endocrine Mucin-Producing Sweat Gland Carcinoma of the Eyelid

 E-submission
E-submission
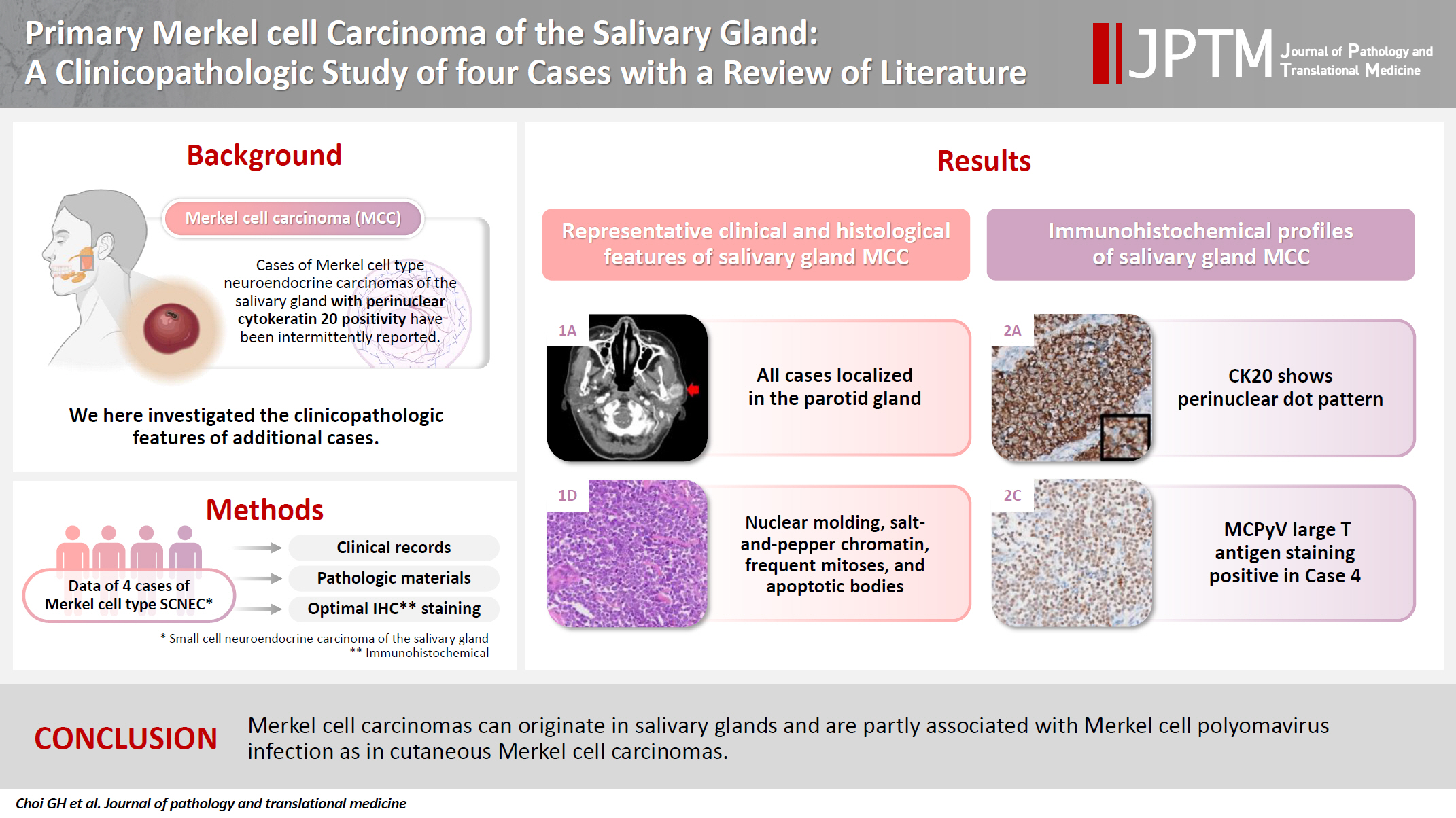

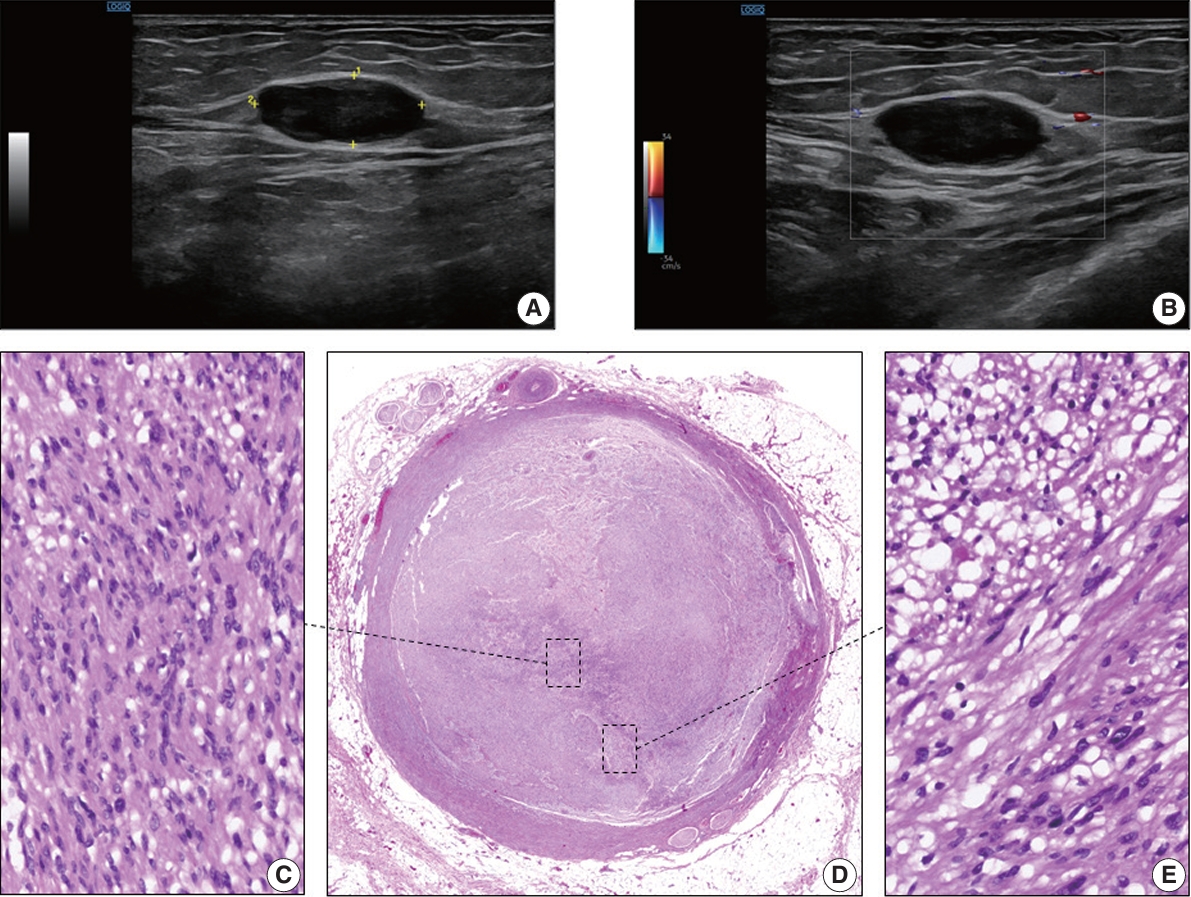
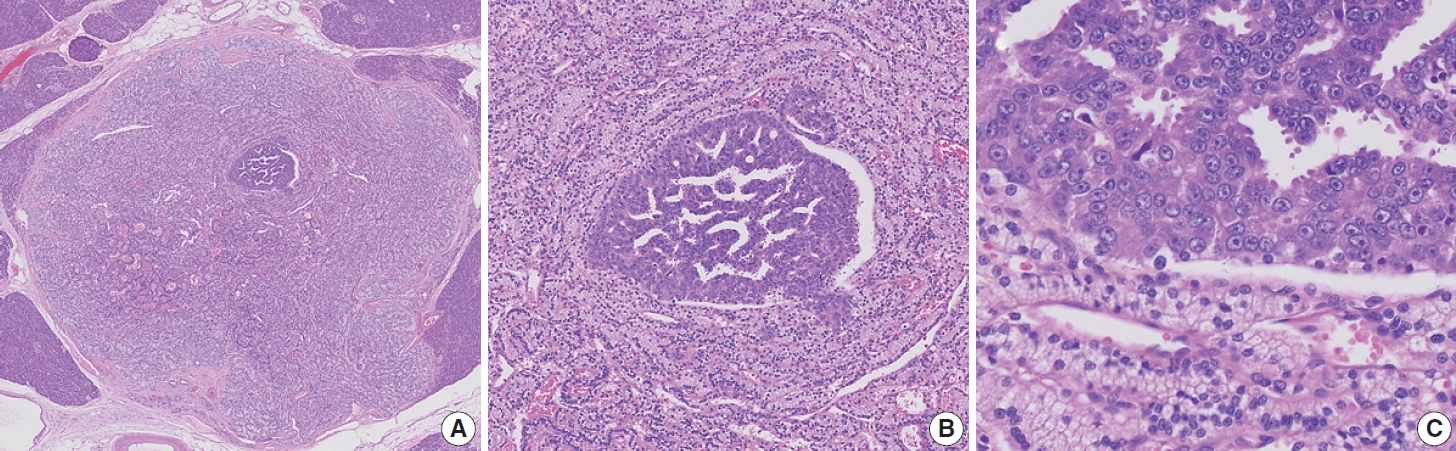
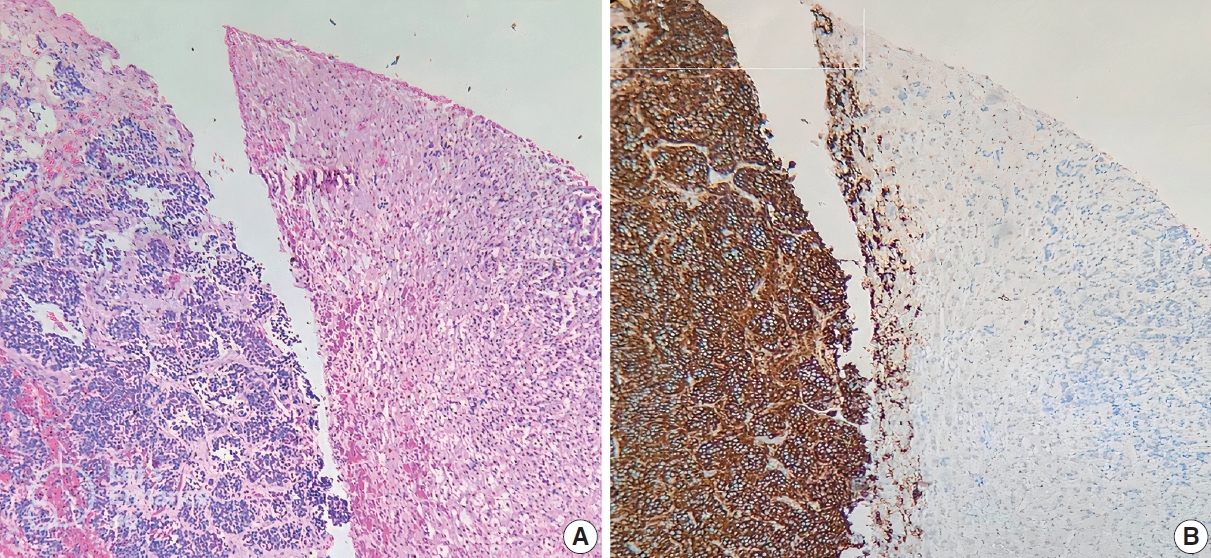
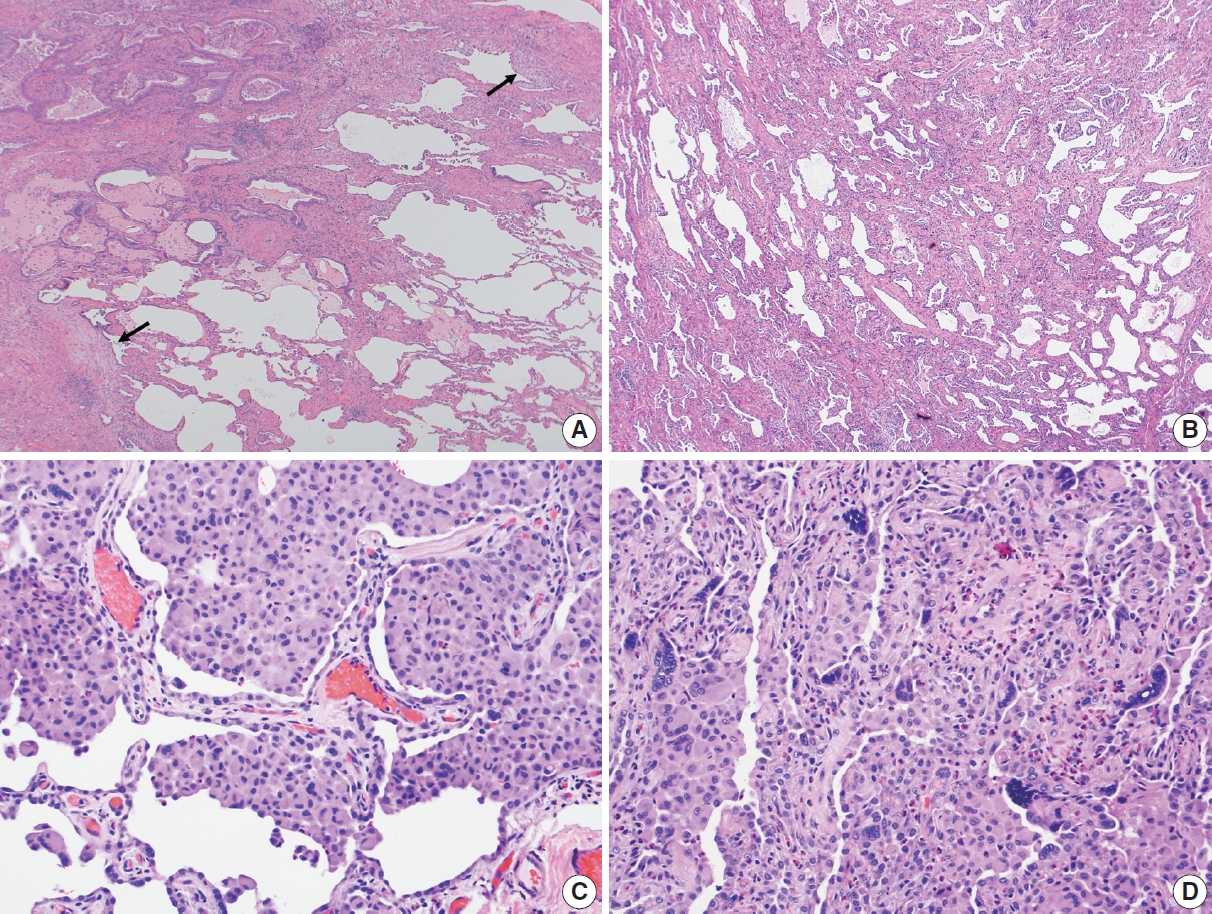
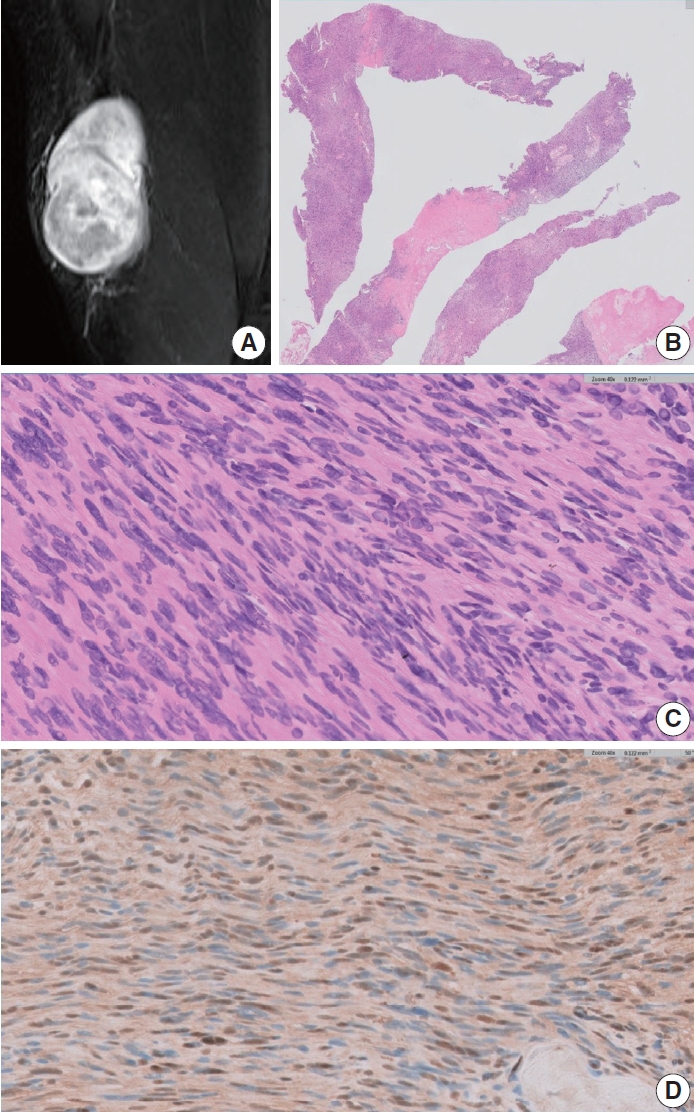

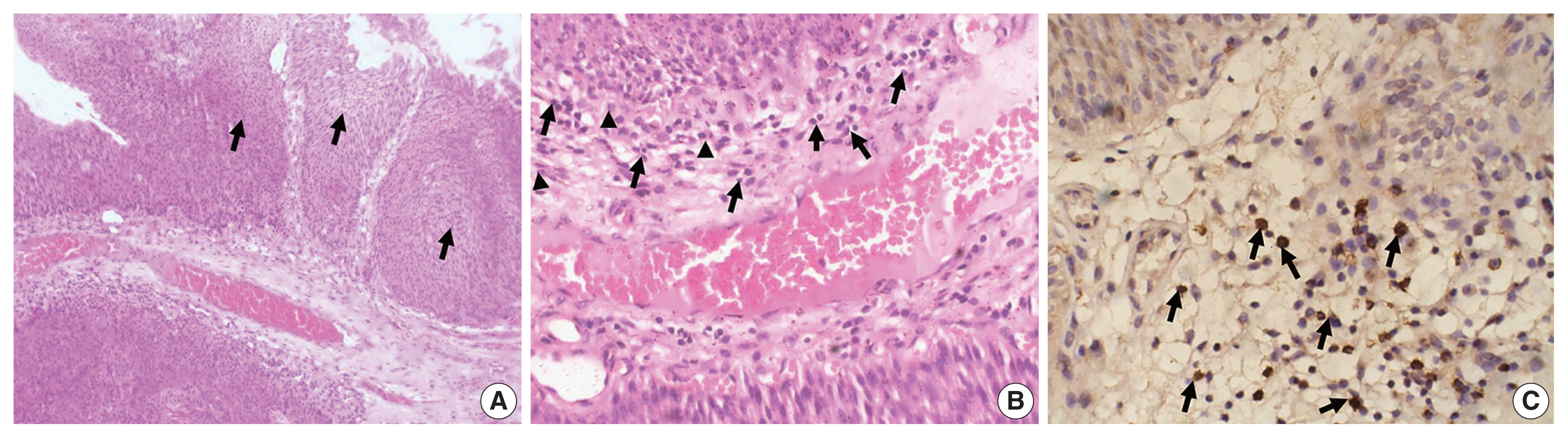
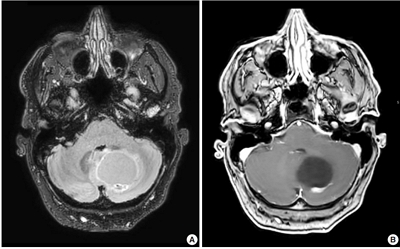
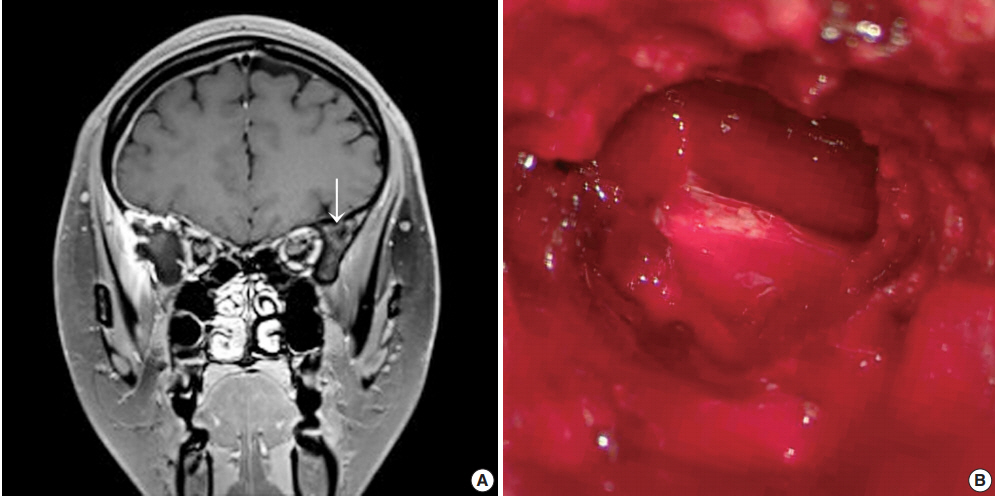
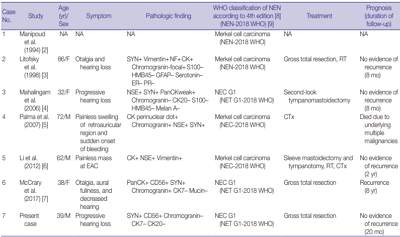
 First
First Prev
Prev



