Search
- Page Path
- HOME > Search
- Correlations and prognostic impacts of tumor spread through airspaces in surgically resected non–small cell lung cancer: a retrospective study from Jordan
- Ola Abu Al Karsaneh, Amani Al-Rousan, Sofian Al Shboul, Mohammed El-Sadoni, Anas Hayajneh, Moath Alrjoub, Sura Al-Rawabdeh, Tareq Saleh
- J Pathol Transl Med. 2026;60(1):92-106. Published online January 9, 2026
- DOI: https://doi.org/10.4132/jptm.2025.10.15
- 1,669 View
- 85 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Spread through air spaces (STAS) has been identified as an invasion pattern in non–small cell lung cancer (NSCLC). This study evaluated the association between tumor STAS and various clinicopathological parameters of NSCLC, with emphasis on the prognostic role of STAS. Methods: We evaluated 96 cases of NSCLC for STAS. STAS-positive cases were graded according to the distance between the edge of the primary tumor and the furthest STAS, in millimeters, or the number of alveoli separating STAS from the tumor. Results: STAS was observed in 33 patients (34.4%). In 28 cases, STAS was located in airspaces >3 alveoli away from the primary tumor. In 18 cases, STAS was found in airspaces > 2.5 mm away from the edge of the primary tumor. Morphologically, 18 cases of STAS demonstrated a solid nest pattern, eight showed a micropapillary cluster pattern, and seven exhibited a single-cell pattern. In multivariate analysis, only high tumor grade (p = .001) was independently associated with STAS in NSCLC. The presence of STAS (p = .047), lymphovascular invasion (p = .001), positive surgical margin (p = .021), adenocarcinoma histology (p = .020), and postoperative therapy (p = .049) showed a statistically significant lower overall survival (OS). However, multivariate analyses showed that STAS is not an independent predictor of OS in NSCLC. In addition, STAS-positive cases with an extension of >2.5 mm had significantly lower disease-free survival (DFS) (p = .018). Conclusions: The findings demonstrated that STAS is independently associated with a higher tumor grade and appears to have an adverse impact on OS and DFS in the examined subpopulation.
- Biomarker testing of cytology specimens in personalized medicine for lung cancer patients
- Hyojin Kim, Jin-Haeng Chung
- J Pathol Transl Med. 2022;56(6):326-333. Published online November 9, 2022
- DOI: https://doi.org/10.4132/jptm.2022.10.17
- 6,702 View
- 177 Download
- 8 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Every patient with advanced non–small cell lung cancer (NSCLC) should be tested for targetable driver mutations and gene arrangements that may open avenues for targeted therapy. As most patients with NSCLC in the advanced stage of the disease are not candidates for surgery, these tests have to be performed on small biopsies or cytology samples. A growing number of other genetic changes with targetable mutations may be treatable in the near future. To identify patients who might benefit from novel targeted therapy, relevant markers should be tested in an appropriate context. In addition, immunotherapy of lung cancer is guided by the status of programmed death-ligand 1 expression in tumor cells. The variety and versatility of cytological specimen preparations offer significant advantages for molecular testing; however, they frequently remain underused. Therefore, evaluating the utility and adequacy of cytologic specimens is important, not only from a lung cancer diagnosis, but also for the large number of ancillary studies that are necessary to provide appropriate clinical management. A large proportion of lung cancers is diagnosed by aspiration or exfoliative cytology specimens; thus, optimizing strategies to triage and best use the tissue for diagnosis and biomarker studies forms a critical component of lung cancer management. In this review, we discuss the opportunities and challenges of using cytologic specimens for biomarker testing of lung cancer and the role of cytopathology in the molecular era.
-
Citations
Citations to this article as recorded by- Proposal of real-world solutions for the implementation of predictive biomarker testing in patients with operable non-small cell lung cancer
Paul Hofman, Petros Christopoulos, Nicky D’Haene, John Gosney, Nicola Normanno, Ed Schuuring, Ming-Sound Tsao, Christine Quinn, Jayne Russell, Katherine E Keating, Fernando López-Ríos
Lung Cancer.2025; 201: 108107. CrossRef - Validation of ancillary procedures on formalin liquid fixed aspiration cytologic samples: from minimum to maximum
Orsolya Rideg, Tímea Dergez, Arnold Tóth, Tamás Tornóczky, Gábor Pavlovics, Endre Kálmán
American Journal of Clinical Pathology.2025; 164(6): 924. CrossRef - Molecular testing of cytology specimens: Issues in specimen adequacy and clinical utility
Ghulam Ghous, Komal Ijaz, Magda Esebua, Lester J. Layfield
Diagnostic Cytopathology.2024; 52(2): 123. CrossRef - The updated College of American Pathologists principles of analytic validation of immunohistochemical assays: A step forward for cytopathology
Sinchita Roy‐Chowdhuri
Cancer Cytopathology.2024; 132(9): 547. CrossRef - Best-Practice Biomarker Testing of Oesophago-Gastric Cancer in the UK: Expert Consensus Recommendations Developed Using a Modified Delphi
N.P. West, W. Mansoor, P. Taniere, E. Smyth, M. Rodriguez-Justo, A. Oniscu, P. Carter
Clinical Oncology.2024; 36(11): 701. CrossRef - Next step of molecular pathology: next-generation sequencing in cytology
Ricella Souza da Silva, Fernando Schmitt
Journal of Pathology and Translational Medicine.2024; 58(6): 291. CrossRef
- Proposal of real-world solutions for the implementation of predictive biomarker testing in patients with operable non-small cell lung cancer
- Programmed death-ligand 1 expression and tumor-infiltrating lymphocytes in non-small cell lung cancer: association with clinicopathologic parameters
- Gaurav Garg, Kuruswamy Thurai Prasad, Navneet Singh, Parul Gupta, Valliappan Muthu, Ashim Das, Amanjit Bal
- J Pathol Transl Med. 2021;55(6):398-405. Published online October 6, 2021
- DOI: https://doi.org/10.4132/jptm.2021.08.08
- 5,556 View
- 167 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Data on the prevalence of programmed death-ligand 1 (PD-L1) expression and tumor-infiltrating lymphocytes (TILs) in non–small cell lung cancer (NSCLC) and their clinical significance in Indian patients are limited.
Methods
Newly diagnosed NSCLC cases (adenocarcinoma or squamous cell carcinoma [SqCC] histology) were included in the present study. The TILs were evaluated based on morphology on hematoxylin and eosin–stained slides. PD-L1 expression in tumors was assessed using immunohistochemistry with rabbit monoclonal antibody (SP263) on the Ventana automated immunostainer. Tumors with PD-L1 expression > 50% on tumor cells were considered PD-L1–positive. Tumors in which TILs occupy > 25% of stroma were considered to have high TILs. The association of PD-L1 expression and TILs with various clinical parameters including overall survival (OS) was investigated.
Results
The present study included 128 cases of NSCLC (67 adenocarcinoma, 61 SqCC). PD-L1 positivity was observed in 17.2% of the patients with NSCLC. Baseline characteristics of PD-L1–positive subjects were similar to PD-L1–negative subjects except for a higher prevalence of liver metastasis (18.2% vs. 2.8%; p = .018) and a higher probability of diagnosis from extrapulmonary biopsies. High TILs were observed in 26.6% of the subjects. However, PD-L1 expression and high TIL did not affect OS.
Conclusions
PD-L1 positivity and high TILs were observed in 20% and 25% of the patients with NSCLC, respectively, however, neither were predictors of survival in SqCC. -
Citations
Citations to this article as recorded by- PDL1 and IDO‐2 Immunohistochemistry in Bronchoalveolar Lavage Versus Bronchoscopic Biopsy of Non‐Small Cell Lung Cancer
Menna Allah Hesham Mohammed Fekry, Yosria Mohammed El‐Gohary, Hesham Radwan Abd‐Elaziz, Tarek Hamdy Hassan, Mona Mostafa Ahmed
Cytopathology.2026; 37(2): 151. CrossRef - Multiplex plasma protein assays as a diagnostic tool for lung cancer
Mohammad Tanvir Ahamed, Jenny Forshed, Adrian Levitsky, Janne Lehtiö, Amanj Bajalan, Maria Pernemalm, Lars E. Eriksson, Björn Andersson
Cancer Science.2024; 115(10): 3439. CrossRef - Real-world prevalence of PD-L1 expression in non-small cell lung cancer: an Australia-wide multi-centre retrospective observational study
Prudence A. Russell, Alexandra L. Farrall, Sarita Prabhakaran, Khashayar Asadi, Wade Barrett, Caroline Cooper, Wendy Cooper, Samuel Cotton, Edwina Duhig, Matthew Egan, Stephen Fox, David Godbolt, Shilpa Gupta, Aniza Hassan, Connull Leslie, Trishe Leong, D
Pathology.2023; 55(7): 922. CrossRef
- PDL1 and IDO‐2 Immunohistochemistry in Bronchoalveolar Lavage Versus Bronchoscopic Biopsy of Non‐Small Cell Lung Cancer
- Robust home brew fragment sizing assay for detection of MET exon 14 skipping mutation in non–small cell lung cancer patients in resource constrained community hospitals
- Anurag Mehta, Shrinidhi Nathany, Aanchal Chopra, Sakshi Mattoo, Dushyant Kumar, Manoj Kumar Panigrahi
- J Pathol Transl Med. 2021;55(5):324-329. Published online September 2, 2021
- DOI: https://doi.org/10.4132/jptm.2021.07.15
- 6,419 View
- 132 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
A mutation/deletion involving donor or acceptor sites for exon 14 results in splicing out of exon 14 of the mesenchymal epithelial transition (MET) gene and is known as “MET exon 14 skipping” (ΔMET14). The two recent approvals with substantial objective responses and improved progression-free survival to MET inhibitors namely capmatinib and tepotinib necessitate the identification of this alteration upfront. We herein describe our experience of ΔMET14 detection by an mRNA-based assay using polymerase chain reaction followed by fragment sizing.
Methods
This is a home brew assay which was developed with the concept that the transcripts from true ΔMET14 will be shorter by ~140 bases than their wild type counterparts. The cases which were called MET exon 14 skipping positive on next-generation sequencing (NGS) were subjected to this assay, along with 13 healthy controls in order to establish the validity for true negatives.
Results
Thirteen cases of ΔMET14 mutation were detected on NGS using RNA-based sequencing. Considering NGS as a gold standard, the sizing assay using both gel and capillary electrophoresis that showed 100% specificity for both with concordance rates of 84.6% and 88.2% with NGS, respectively, were obtained.
Conclusions
Owing to the cost-effective nature and easy to use procedures, this assay will prove beneficial for small- and medium-sized laboratories where skilled technical personnel and NGS platforms are unavailable. -
Citations
Citations to this article as recorded by
- Peripheral type squamous cell carcinoma of the lung: clinicopathologic characteristics in comparison to the central type
- Yeoun Eun Sung, Uiju Cho, Kyo Young Lee
- J Pathol Transl Med. 2020;54(4):290-299. Published online June 17, 2020
- DOI: https://doi.org/10.4132/jptm.2020.05.04
- 11,156 View
- 209 Download
- 13 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Squamous cell carcinomas (SqCCs) of the lung are known to arise more often in a central area but reports of peripheral SqCCs have increased, with a pathogenesis that is obscured. In this study, the clinicopathologic characteristics of peripheral lung SqCCs were studied and compared with those of the central type.
Methods
This study included 63 peripheral lung SqCCs and 48 randomly selected central cases; hematoxylin and eosin-stained slides of surgically resected specimens were reviewed in conjunction with radiologic images and clinical history. Cytokeratin-7 immunohistochemical staining of key slides and epidermal growth factor receptor (EGFR)/KRAS mutations tested by DNA sequencing were also included.
Results
Stages of peripheral SqCCs were significantly lower than central SqCCs (p=.016). Cystic change of the mass (p=.007), presence of interstitial fibrosis (p=0.007), and anthracosis (p=.049) in the background lung were significantly associated with the peripheral type. Cytokeratin-7 positivity was also higher in peripheral SqCCs with cutoffs of both 10% and 50% (p=.011). Pathogenic mutations in EGFR and KRAS were observed in only one case out of the 72 evaluated. The Cox proportional hazard model indicated a significantly better disease-free survival (p=.009) and the tendency of better overall survival (p=.106) in the peripheral type.
Conclusions
In peripheral type, lower stage is a favorable factor for survival but more frequent interstitial fibrosis and older age are unfavorable factors. Multivariate Cox analysis revealed that peripheral type is associated with better disease-free survival. The pathogenesis of peripheral lung SqCCs needs further investigation, together with consideration of the background lung conditions. -
Citations
Citations to this article as recorded by- Assessing the performance of chest x‐ray screening in detecting early‐stage lung cancer in the general population
Choy‐Lye Chei, Sho Nakamura, Kaname Watanabe, Takashi Mizutani, Hiroto Narimatsu
International Journal of Cancer.2025; 156(11): 2127. CrossRef - Whole lung radiomic features are associated with overall survival in patients with locally advanced non-small cell lung cancer treated with definitive radiotherapy
Meng Yan, Zhen Zhang, Jia Tian, Jiaqi Yu, Andre Dekker, Dirk de Ruysscher, Leonard Wee, Lujun Zhao
Radiation Oncology.2025;[Epub] CrossRef - Imaging appearances, CT evolution patterns, and surgical prognosis of stage I lung squamous cell carcinoma
Wei-hua Zhao, Tian-you Luo, Fa-jin Lv, Qi Li
Cancer Imaging.2025;[Epub] CrossRef - Pulmonary squamous cell carcinoma and lymphoepithelial carcinoma – morphology, molecular characteristics and differential diagnosis
Sabina Berezowska, Marie Maillard, Mark Keyter, Bettina Bisig
Histopathology.2024; 84(1): 32. CrossRef - Assessment of seasonal variability of PM, BC and UFP levels at a highway toll stations and their associated health risks
Nazneen, Aditya Kumar Patra, Soma Sekhara Rao Kolluru, Abhishek Penchala, Sachidanand Kumar, Namrata Mishra, Naragam Bhanu Sree, Samrat Santra, Ravish Dubey
Environmental Research.2024; 245: 118028. CrossRef - Association between Airport Ultrafine Particles and Lung Cancer Risk: The Multiethnic Cohort Study
Arthur Bookstein, Justine Po, Chiuchen Tseng, Timothy V. Larson, Juan Yang, Sung-shim L. Park, Jun Wu, Salma Shariff-Marco, Pushkar P. Inamdar, Ugonna Ihenacho, Veronica W. Setiawan, Mindy C. DeRouen, Loïc Le Marchand, Daniel O. Stram, Jonathan Samet, Bea
Cancer Epidemiology, Biomarkers & Prevention.2024; 33(5): 703. CrossRef - Clinical and Bronchoscopy Assessment in Diagnosing the Histopathology Type of Primary Central Lung Tumors
Mia Elhidsi, Jamal Zaini, Lisnawati Rachmadi, Asmarinah Asmarinah, Aria Kekalih, Noni Soeroso, Menaldi Rasmin
The Open Respiratory Medicine Journal.2024;[Epub] CrossRef - Possible thoracic metastasis from squamous cell carcinoma of the external auditory canal: A case report
Hiroshi Takehara, Ken Kodama, Toru Momozane, Masashi Takeda, Kaichi Shigetsu, Hiroki Kishima
Clinical Case Reports.2024;[Epub] CrossRef - Radiological precursor lesions of lung squamous cell carcinoma: Early progression patterns and divergent volume doubling time between hilar and peripheral zones
Haruto Sugawara, Yasushi Yatabe, Hirokazu Watanabe, Hiroyuki Akai, Osamu Abe, Shun-ichi Watanabe, Masahiko Kusumoto
Lung Cancer.2023; 176: 31. CrossRef - Loss of GSTO2 contributes to cell growth and mitochondria function via the p38 signaling in lung squamous cell carcinoma
Ryusuke Sumiya, Masayoshi Terayama, Teruki Hagiwara, Kazuaki Nakata, Keigo Sekihara, Satoshi Nagasaka, Hideki Miyazaki, Toru Igari, Kazuhiko Yamada, Yuki I. Kawamura
Cancer Science.2022; 113(1): 195. CrossRef - Primary tumor location in lung cancer: the evaluation and administration
Xueqi Xie, Xiaolin Li, Wenjie Tang, Peng Xie, Xuefen Tan
Chinese Medical Journal.2022; 135(2): 127. CrossRef - Pulmonary squamous cell carcinoma with a lepidic-pagetoid growth pattern
Claudio Guerrieri, Mark Lindner, Joanna Sesti, Abhishek Chakraborti, Rachel Hudacko
Pathologica.2022; 114(4): 304. CrossRef - Deposition modeling of ambient particulate matter in the human respiratory tract
Salman Khan, Bhola Ram Gurjar, Veerendra Sahu
Atmospheric Pollution Research.2022; 13(10): 101565. CrossRef - Selection of the surgical approach for patients with cStage IA lung squamous cell carcinoma: A population-based propensity score matching analysis
Shengteng Shao, Guisong Song, Yuanyong Wang, Tengfei Yi, Shuo Li, Fuhui Chen, Yang Li, Xiaotong Liu, Bin Han, Yuhong Liu
Frontiers in Oncology.2022;[Epub] CrossRef - Virus Nanoparticles & Different Nanoparticles Affect Lung Cancer- A New Approach
Ranajit Nath, Ratna Roy, Soubhik bhattacharyya, Sourav Datta
International Journal of Scientific Research in Science and Technology.2021; : 867. CrossRef
- Assessing the performance of chest x‐ray screening in detecting early‐stage lung cancer in the general population
- Gene variant profiles and tumor metabolic activity as measured by FOXM1 expression and glucose uptake in lung adenocarcinoma
- Ashley Goodman, Waqas Mahmud, Lela Buckingham
- J Pathol Transl Med. 2020;54(3):237-245. Published online March 4, 2020
- DOI: https://doi.org/10.4132/jptm.2020.02.08
- 7,308 View
- 120 Download
- 2 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Cancer cells displaying aberrant metabolism switch energy production from oxidative phosphorylation to glycolysis. Measure of glucose standardized uptake value (SUV) by positron emission tomography (PET), used for staging of adenocarcinoma in high-risk patients, can reflect cellular use of the glycolysis pathway. The transcription factor, FOXM1 plays a role in regulation of glycolytic genes. Cancer cell transformation is driven by mutations in tumor suppressor genes such as TP53 and STK11 and oncogenes such as KRAS and EGFR. In this study, SUV and FOXM1 gene expression were compared in the background of selected cancer gene mutations.
Methods
Archival tumor tissue from cases of lung adenocarcinoma were analyzed. SUV was collected from patient records. FOXM1 gene expression was assessed by quantitative reverse transcriptase polymerase chain reaction (qRT-PCR). Gene mutations were detected by allele-specific PCR and gene sequencing.
Results
SUV and FOXM1 gene expression patterns differed in the presence of single and coexisting gene mutations. Gene mutations affected SUV and FOXM1 differently. EGFR mutations were found in tumors with lower FOXM1 expression but did not affect SUV. Tumors with TP53 mutations had increased SUV (p = .029). FOXM1 expression was significantly higher in tumors with STK11 mutations alone (p < .001) and in combination with KRAS or TP53 mutations (p < .001 and p = .002, respectively).
Conclusions
Cancer gene mutations may affect tumor metabolic activity. These observations support consideration of tumor cell metabolic state in the presence of gene mutations for optimal prognosis and treatment strategy. -
Citations
Citations to this article as recorded by- Prognostic value of combining clinical factors, 18F-FDG PET-based intensity, volumetric features, and deep learning predictor in patients with EGFR-mutated lung adenocarcinoma undergoing targeted therapies: a cross-scanner and temporal validation study
Kun-Han Lue, Yu-Hung Chen, Sung-Chao Chu, Chih-Bin Lin, Tso-Fu Wang, Shu-Hsin Liu
Annals of Nuclear Medicine.2024; 38(8): 647. CrossRef
- Prognostic value of combining clinical factors, 18F-FDG PET-based intensity, volumetric features, and deep learning predictor in patients with EGFR-mutated lung adenocarcinoma undergoing targeted therapies: a cross-scanner and temporal validation study
- MicroRNA-374a Expression as a Prognostic Biomarker in Lung Adenocarcinoma
- Yeseul Kim, Jongmin Sim, Hyunsung Kim, Seong Sik Bang, Seungyun Jee, Sungeon Park, Kiseok Jang
- J Pathol Transl Med. 2019;53(6):354-360. Published online October 24, 2019
- DOI: https://doi.org/10.4132/jptm.2019.10.01
- 6,782 View
- 130 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Lung cancer is the most common cause of cancer-related death, and adenocarcinoma is the most common histologic subtype. MicroRNA is a small non-coding RNA that inhibits multiple target gene expression at the post-transcriptional level and is commonly dysregulated in malignant tumors. The purpose of this study was to analyze the expression of microRNA-374a (miR-374a) in lung adenocarcinoma and correlate its expression with various clinicopathological characteristics.
Methods
The expression level of miR-374a was measured in 111 formalin-fixed paraffin-embedded lung adenocarcinoma tissues using reverse transcription-quantitative polymerase chain reaction assays. The correlation between miR-374a expression and clinicopathological parameters, including clinical outcome, was further analyzed.
Results
High miR-374 expression was correlated with advanced pT category (chi-square test, p=.004) and pleural invasion (chi-square test, p=.034). Survival analysis revealed that patients with high miR-374a expression had significantly shorter disease-free survival relative to those with low miR-374a expression (log-rank test, p=.032).
Conclusions
miR-374a expression may serve as a potential prognostic biomarker for predicting recurrence in early stage lung adenocarcinoma after curative surgery. -
Citations
Citations to this article as recorded by- Upregulated miR-374a-5p drives psoriasis pathogenesis through WIF1 downregulation and Wnt5a/NF-κB activation
Jing Ma, Lu Gan, Hongying Chen, Lihao Chen, Yu Hu, Chao Luan, Kun Chen, Jiaan Zhang
Cellular Signalling.2024; 119: 111171. CrossRef - Association between the expression level of miRNA‑374a and TGF‑β1 in patients with colorectal cancer
Noha El Din, Reem El‑Shenawy, Rehab Moustafa, Ahmed Khairy, Sally Farouk
World Academy of Sciences Journal.2024;[Epub] CrossRef - Cell-free plasma miRNAs analysis for low invasive lung cancer diagnostics
M. Yu. Konoshenko, P. P. Laktionov, Yu. A. Lancuhaj, S. V. Pak, S. E. Krasilnikov, O. E. Bryzgunova
Advances in Molecular Oncology.2023; 10(2): 78. CrossRef - MicroRNA‑mediated regulation in lung adenocarcinoma: Signaling pathways and potential therapeutic implications (Review)
Jiye Liu, Fei Zhang, Jiahe Wang, Yibing Wang
Oncology Reports.2023;[Epub] CrossRef - Dysregulation of miR-374a is involved in the progression of diabetic retinopathy and regulates the proliferation and migration of retinal microvascular endothelial cells
Zhanhong Wang, Xiao Zhang, Yanjun Wang, Dailing Xiao
Clinical and Experimental Optometry.2022; 105(3): 287. CrossRef - MicroRNA Profile for Diagnostic and Prognostic Biomarkers in Thyroid Cancer
Jong-Lyul Park, Seon-Kyu Kim, Sora Jeon, Chan-Kwon Jung, Yong-Sung Kim
Cancers.2021; 13(4): 632. CrossRef
- Upregulated miR-374a-5p drives psoriasis pathogenesis through WIF1 downregulation and Wnt5a/NF-κB activation
- p40 Immunohistochemistry Is an Excellent Marker in Primary Lung Squamous Cell Carcinoma
- Khairunisa Ahmad Affandi, Nur Maya Sabrina Tizen, Muaatamarulain Mustangin, Reena Rahayu MdReena Rahayu Md Zin
- J Pathol Transl Med. 2018;52(5):283-289. Published online August 31, 2018
- DOI: https://doi.org/10.4132/jptm.2018.08.14
- 26,443 View
- 347 Download
- 37 Web of Science
- 39 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Lung cancer is the third most common cancer worldwide. With major advances in the molecular testing of lung cancers and the introduction of targeted therapies, the distinction between adenocarcinoma and squamous cell carcinoma as well as pathologic subtyping has become important. Recent studies showed that p40 is highly specific for squamous and basal cells and is superior to p63 for diagnosing lung squamous cell carcinoma. The aim of this study was to evaluate the use of p40 immunohistochemical stain in the diagnosis of non-small cell lung carcinoma and its potential to replace current p63 antibody as the best immunohistochemical squamous marker.
Methods
Seventy formalin-fixed paraffin-embedded cases previously diagnosed as primary lung squamous cell carcinoma (n = 35) and lung adenocarcinoma (n = 35) from January 2008 to December 2016 were retrieved. The results of tumour cell immunoreactivity for p40 and p63 antibodies in lung squamous cell carcinoma and lung adenocarcinoma were compared.
Results
p40 was expressed in 27 cases of lung squamous cell carcinoma (77.1%). All cases of lung adenocarcinoma (35/35, 100%) were negative for p40. p63 expression was positive in 30 cases of lung squamous cell carcinoma (85.7%) and 13 cases of lung adenocarcinoma (37.1%). Reactivity for both p40 and p63 in lung squamous cell carcinoma was strong and diffuse, whereas variable reactivity was observed in lung adenocarcinoma.
Conclusions
p40 is an excellent marker for distinguishing lung squamous cell carcinoma from adenocarcinoma, and p40 expression is equivalent to p63 expression in lung squamous cell carcinoma. -
Citations
Citations to this article as recorded by- Immunohistochemical expression of ΔNp63 versus pan-p63 in normal and neoplastic feline tissues
Igor R. Santos, Carolina B. Brunner, Milena C. Paz, Gabriela Hartmann, Gabrielle Z. Tres, Luciana Sonne, Welden Panziera, David Driemeier, Marcele B. Bandinelli, Saulo P. Pavarini
Veterinary Pathology.2026;[Epub] CrossRef - Partial Response to Repotrectinib in ROS1-Rearranged Lung Squamous Cell Carcinoma: A Brief Report
Yukiko Yoshida, Hajime Asahina, Ken Kuwahara, Hidenori Mizugaki, Noriyuki Yamada, Hiroshi Yokouchi, Naohiro Nomura, Yoshihiro Matsuno, Satoshi Oizumi
Clinical Lung Cancer.2026; 27(2): 80. CrossRef - Morphologic and immunohistochemical study of HPV-related cervical adenosquamous carcinoma: Reappraisal of a poorly defined entity
Zhenwei Zhang, M. Ruhul Quddus, C James Sung, Kamaljeet Singh
Human Pathology.2026; 170: 106052. CrossRef - Analysis of a two-marker immunohistochemistry panel (TTF-1 and p40) for distinguishing lung adenocarcinoma from squamous cell carcinoma on destained direct cytologic smears
S.A. Deepa Adiga, Harsha Kunar, Anusha S. Bhatt, Surbhi Patel, Daksha D. Shetty
Annals of Diagnostic Pathology.2026; : 152617. CrossRef - Cancer of Unknown Primary With Squamous Cell Carcinoma Phenotype Presenting as Isolated Axillary Mass
Nicole Liang, Mohamed Alshal, Lynne J Goebel
Cureus.2025;[Epub] CrossRef - A critical appraisal of the clinico-radiological, histopathological and immunohistochemical profile of CT-guided and bronchoscopy-guided biopsies in lung lesions
Mukta Pujani, Ruchi Arora Sachdeva, S. Zafar Abbas, Charu Agarwal, Minakshi Bhardwaj, Varsha Chauhan, Jyoti Rajpoot, Dipti Sidam, Aniruna Dey
Lung India.2025; 42(3): 218. CrossRef - An Organoid Model for Translational Cancer Research Recapitulates Histoarchitecture and Molecular Hallmarks of Non-Small-Cell Lung Cancer
Camilla T. Ekanger, Maria P. Ramnefjell, Maren S. F. Guttormsen, Joakim Hekland, Kristin Dahl-Michelsen, Maria L. Lotsberg, Ning Lu, Linda E. B. Stuhr, Laurence Hoareau, Pirjo-Riitta Salminen, Fabian Gärtner, Marianne Aanerud, Lars A. Akslen, James B. Lor
Cancers.2025; 17(11): 1873. CrossRef - Accessing utility of immunohistochemistry, PD-L1 correlation with stage of cancer and EGFR mutation with disease survival in primary lung carcinoma
Kartavya Kumar Verma, Amit Bugalia, Ajoy Kumar behera, Nighat Hussain
Surgical and Experimental Pathology.2025;[Epub] CrossRef - Small intestinal SMARCA4‑deficient undifferentiated carcinoma with intussusception: A case report
Xiaoshan Cai, Shanshan Liu, Linqian Li, Yuming Zhang, Qin Guo, Ze Chen, Meihua Qu, Yubing Wang, Ben Yang, Xianwen Yue
Oncology Letters.2025; 31(2): 1. CrossRef - Clinicopathological and molecular perspectives on thoracic SMARCA4-deficient undifferentiated tumors and SMARCA4-deficient non-small cell lung carcinomas
Sumanta Das, Pallavi Mishra, Sunita Ahlawat
Pathologica.2025; 117(5): 455. CrossRef - Clinico-Pathological Profile of Non-Small Cell Lung Carcinoma with Emphasis on Diagnostic Immunohistochemistry – An Institutional Experience
Shubhika Rao Sachdeva, Bhavna Nayal, Ananth Pai
Medical Journal of Dr. D.Y. Patil Vidyapeeth.2025; 18(Suppl 2): S288. CrossRef - Lack of imbalance between the master regulators TTF1/NKX2-1 and ΔNp63/p40 implies adverse prognosis in non-small cell lung cancer
Martina Vescio, Matteo Bulloni, Giuseppe Pelosi, Linda Pattini
Scientific Reports.2024;[Epub] CrossRef - Adeno-to-squamous transition drives resistance to KRAS inhibition in LKB1 mutant lung cancer
Xinyuan Tong, Ayushi S. Patel, Eejung Kim, Hongjun Li, Yueqing Chen, Shuai Li, Shengwu Liu, Julien Dilly, Kevin S. Kapner, Ningxia Zhang, Yun Xue, Laura Hover, Suman Mukhopadhyay, Fiona Sherman, Khrystyna Myndzar, Priyanka Sahu, Yijun Gao, Fei Li, Fuming
Cancer Cell.2024; 42(3): 413. CrossRef - Common practice issues in pulmonary cytology/small biopsy: Diagnostic pitfalls and appropriate use of immunohistochemical stains
Jessie Xiong, Erik Polsdofer, Jian Jing
Human Pathology Reports.2024; 36: 300735. CrossRef - Integrating AI-Powered Digital Pathology and Imaging Mass Cytometry Identifies Key Classifiers of Tumor Cells, Stroma, and Immune Cells in Non–Small Cell Lung Cancer
Alessandra Rigamonti, Marika Viatore, Rebecca Polidori, Daoud Rahal, Marco Erreni, Maria Rita Fumagalli, Damiano Zanini, Andrea Doni, Anna Rita Putignano, Paola Bossi, Emanuele Voulaz, Marco Alloisio, Sabrina Rossi, Paolo Andrea Zucali, Armando Santoro, V
Cancer Research.2024; 84(7): 1165. CrossRef - Advances in combined neuroendocrine carcinoma of lung cancer
Zesen Han, Fujun Yang, Fang Wang, Huayu Zheng, Xiujian Chen, Hongyu Meng, Fenglei Li
Pathology and Oncology Research.2024;[Epub] CrossRef - Evolving Precision First-Line Systemic Treatment for Patients with Unresectable Non-Small Cell Lung Cancer
Tianhong Li, Weijie Ma, Ebaa Al-Obeidi
Cancers.2024; 16(13): 2350. CrossRef - Antibody-Conjugated Nanodiamond Enzyme for Targeted Non-Small-Cell Lung Cancer by Regulating Oxidative Stress
Xiaoying Guan, Jingwen Yang, Ziying Liu, Guowei Yang, Xiumei Tian
ACS Applied Nano Materials.2024; 7(20): 23670. CrossRef - Multifocal Pulmonary Opacities in an Elderly Smoker
Patton C McClelland, Zachary Jarrett, Christian C Lamb, Mateo Houle
Cureus.2024;[Epub] CrossRef - Clonal dynamics and Stereo-seq resolve origin and phenotypic plasticity of adenosquamous carcinoma
Ruiying Zhao, Yunhua Xu, Yedan Chen, Jiajun Zhang, Fei Teng, Sha Liao, Shengnan Chen, Qian Wu, Chan Xiang, Jiaohui Pang, Zhanxian Shang, Jikai Zhao, Hairong Bao, Hua Bao, Yang Shao, Shun Lu, Yuchen Han
npj Precision Oncology.2023;[Epub] CrossRef - Keratin 5 in Lung Cancer Specimens: Comparison of Four Antibody Clones and KRT5 mRNA-ISH
Christian Thomsen, Laura Blok-Husum, Jeanette Bæhr Georgsen, Torben Steiniche, Mogens Vyberg
Applied Immunohistochemistry & Molecular Morphology.2023; 31(6): 347. CrossRef - Carcinoma of unknown primary (CUP): an update for histopathologists
Katie Beauchamp, Bruce Moran, Timothy O’Brien, Donal Brennan, John Crown, Kieran Sheahan, Maura Bríd Cotter
Cancer and Metastasis Reviews.2023; 42(4): 1189. CrossRef - Advances in Genomic Data and Biomarkers: Revolutionizing NSCLC Diagnosis and Treatment
Juan Carlos Restrepo, Diana Dueñas, Zuray Corredor, Yamil Liscano
Cancers.2023; 15(13): 3474. CrossRef - Kallikrein-related peptidase 13 expression and clinicopathological features in lung squamous cell carcinoma
Ryusuke Sumiya, Kazuhiko Yamada, Teruki Hagiwara, Satoshi Nagasaka, Hideki Miyazaki, Toru Igari, Yuki Kawamura
Molecular and Clinical Oncology.2023;[Epub] CrossRef - Pre-clinical lung squamous cell carcinoma mouse models to identify novel biomarkers and therapeutic interventions
Priyanka Sahu, Chantal Donovan, Keshav Raj Paudel, Sophie Pickles, Vrushali Chimankar, Richard Y. Kim, Jay C. Horvart, Kamal Dua, Antonio Ieni, Francesco Nucera, Helle Bielefeldt-Ohmann, Sarah Mazilli, Gaetano Caramori, J. Guy Lyons, Philip M. Hansbro
Frontiers in Oncology.2023;[Epub] CrossRef - Intraosseous clear cell mucoepidermoid carcinoma: A case report and evaluation
Adesh S. Manchanda, Ramandeep S. Narang, Komaldeep K. Sandhu
Journal of Oral and Maxillofacial Pathology.2023; 27(4): 780. CrossRef - A targeted expression panel for classification, gene fusion detection and PD-L1 measurements – Can molecular profiling replace immunohistochemistry in non-small cell lung cancer?
Anita Tranberg Simonsen, Amalie Utke, Johanne Lade-Keller, Lasse Westphal Thomsen, Torben Steiniche, Magnus Stougaard
Experimental and Molecular Pathology.2022; 125: 104749. CrossRef - Basal cell carcinoma arising in association with maxillary odontogenic keratocyst in a patient with Gorlin-Goltz syndrome
Mutsuki Kawabe, Yoshitane Tsukamoto, Shohei Matuo, Shuji Kanda, Susumu Hashitani
Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology.2022; 34(3): 333. CrossRef - Cutaneous Metastases from Thymic Carcinoma Primary Tumor: A Rare Case
Eva Krishna Sutedja, Trustia Rizqandaru, Kartika Ruchiatan, Endang Sutedja
International Medical Case Reports Journal.2022; Volume 15: 293. CrossRef - Primary nonkeratinizing squamous cell carcinoma of the scapular bone: A case report
Yang Li, Jian-Lin Zuo, Jin-Shuo Tang, Xian-Yue Shen, Sheng-Hao Xu, Jian-Lin Xiao
World Journal of Clinical Cases.2021; 9(4): 976. CrossRef - Survival-associated N6-adenosine methyltransferase signatures in lung squamous cell carcinoma and clinical verification
Jialin Qu, Li Wang, Man Jiang, Zhimin Wei, Guangming Fu, Xiaochun Zhang
BMC Cancer.2021;[Epub] CrossRef - Pulmonary adenomyoma presenting as a right cardiophrenic angle mass
Osigbemhe Iyalomhe, Sam Sadigh, Charuhas Deshpande, Leslie Litzky, Anna Moran, Scott Simpson
Radiology Case Reports.2020; 15(5): 502. CrossRef - Head-to-Head Comparison of p63 and p40 in Non-Neuroendocrine Carcinomas of the Tubal Gut
Ahmed M. Bakhshwin, Ilyssa O. Gordon, Kathryn Bock Brown, Xiuli Liu, Daniela S. Allende
International Journal of Surgical Pathology.2020; 28(8): 835. CrossRef - Greater specificity of p40 compared with p63 in distinguishing squamous cell carcinoma from adenocarcinoma in effusion cellblocks
Nah Ihm Kim, Ji Shin Lee
Cytojournal.2020; 17: 13. CrossRef - Incidental Thyroid Mass in a Patient With Oropharyngeal Squamous Cell Carcinoma
Kinneri Mehta, Misha Movahed-Ezazi, Akshay V. Patel
JAMA Otolaryngology–Head & Neck Surgery.2020; 146(9): 859. CrossRef - Three dimensional texture analysis of noncontrast chest CT in differentiating solitary solid lung squamous cell carcinoma from adenocarcinoma and correlation to immunohistochemical markers
Rui Han, Roshan Arjal, Jin Dong, Hong Jiang, Huan Liu, Dongyou Zhang, Lu Huang
Thoracic Cancer.2020; 11(11): 3099. CrossRef - The role of the immunohistochemical marker p40 in the differential diagnosis of adenocarcinoma and nonkeratinizing squamous cell cancer of the lung
E.M. Olyushina, M.M. Byakhova, L.E. Zavalishina, Yu.Yu. Andreeva, A.B. Semenova, G.A. Frank
Arkhiv patologii.2020; 82(5): 50. CrossRef - Role of Immunocytochemistry in the Cytological Diagnosis of Pulmonary Tumors
Jasna Metovic, Luisella Righi, Luisa Delsedime, Marco Volante, Mauro Papotti
Acta Cytologica.2020; 64(1-2): 16. CrossRef - Subtyping Lung Cancer Using DNA Methylation in Liquid Biopsies
Sandra P. Nunes, Francisca Diniz, Catarina Moreira-Barbosa, Vera Constâncio, Ana Victor Silva, Júlio Oliveira, Marta Soares, Sofia Paulino, Ana Luísa Cunha, Jéssica Rodrigues, Luís Antunes, Rui Henrique, Carmen Jerónimo
Journal of Clinical Medicine.2019; 8(9): 1500. CrossRef
- Immunohistochemical expression of ΔNp63 versus pan-p63 in normal and neoplastic feline tissues
- Differential MicroRNA Expression between EGFR T790M and L858R Mutated Lung Cancer
- Ji Yeon Kim, Woo Jeong Lee, Ha Young Park, Ahrong Kim, Dong Hoon Shin, Chang Hun Lee
- J Pathol Transl Med. 2018;52(5):275-282. Published online August 16, 2018
- DOI: https://doi.org/10.4132/jptm.2018.07.29
- 8,556 View
- 129 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
MicroRNAs (miRNAs) are short, non-coding RNAs that mediate post-transcriptional gene regulation. They are commonly deregulated in human malignancies, including non-small cell lung cancer (NSCLC). The aim of this study is to investigate miRNA expression in T790M-mutated NSCLC resistant to epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors.
Methods
Six cases of resected NSCLC harboring the T790M mutation were examined. We performed miRNA time polymerase chain reaction (PCR) array profiling using EGFR T790M-mutated NSCLC and L858R-mutated NSCLC. Once identified, miRNAs that were differentially expressed between the two groups were validated by quantitative real-time polymerase chain reaction (qRT-PCR).
Results
miRNA PCR array profiling revealed three up-regulated miRNAs whose expression levels were altered 4.0-fold or more in the EGFR T790M mutation group than in the L858R group: miR-1 (fold change, 4.384), miR-196a (fold change, 4.138), and miR-124 (fold change, 4.132). The three differentially expressed miRNAs were validated by qRT-PCR, and they were found to be overexpressed in the T790M group relative to L858R group. In particular, expression levels of miR-1 and miR-124 were significantly higher in the T790M group (p-value of miR-1 = .004, miR-124 = .007, miR-196a = .096).
Conclusions
MiR-1, miR-124, and miR-196a are overexpressed in EGFR T790M mutated NSCLC. -
Citations
Citations to this article as recorded by- Whole exome sequencing and MicroRNA profiling of lung adenocarcinoma identified risk prediction features for tumors at stage I and its substages
Hao Ho, Sung-Liang Yu, Hsuan-Yu Chen, Shin-Sheng Yuan, Kang-Yi Su, Yi-Chiung Hsu, Chung-Ping Hsu, Cheng-Yen Chuang, Ya-Hsuan Chang, Yu-Cheng Li, Chiou-Ling Cheng, Gee-Chen Chang, Pan-Chyr Yang, Ker-Chau Li
Lung Cancer.2023; 184: 107352. CrossRef - Dynamic Evaluation of Circulating miRNA Profile in EGFR-Mutated NSCLC Patients Treated with EGFR-TKIs
Alessandro Leonetti, Mjriam Capula, Roberta Minari, Giulia Mazzaschi, Alessandro Gregori, Btissame El Hassouni, Filippo Papini, Paola Bordi, Michela Verzè, Amir Avan, Marcello Tiseo, Elisa Giovannetti
Cells.2021; 10(6): 1520. CrossRef - Generation of osimertinib-resistant cells from epidermal growth factor receptor L858R/T790M mutant non-small cell lung carcinoma cell line
Nalini Devi Verusingam, Yi-Chen Chen, Heng-Fu Lin, Chao-Yu Liu, Ming-Cheng Lee, Kai-Hsi Lu, Soon-Keng Cheong, Alan Han-Kiat Ong, Shih-Hwa Chiou, Mong-Lien Wang
Journal of the Chinese Medical Association.2021; 84(3): 248. CrossRef - Cell Behavior of Non-Small Cell Lung Cancer Is at EGFR and MicroRNAs Hands
Sarah Sayed Hassanein, Sherif Abdelaziz Ibrahim, Ahmed Lotfy Abdel-Mawgood
International Journal of Molecular Sciences.2021; 22(22): 12496. CrossRef - The Roles of MicroRNA in Lung Cancer
Kuan-Li Wu, Ying-Ming Tsai, Chi-Tun Lien, Po-Lin Kuo, Jen-Yu Hung
International Journal of Molecular Sciences.2019; 20(7): 1611. CrossRef
- Whole exome sequencing and MicroRNA profiling of lung adenocarcinoma identified risk prediction features for tumors at stage I and its substages
- WITHDRAWN:A Clinicopathologic Study of 220 Cases of Pulmonary Sclerosing Pneumocytoma in Korea: A Nationwide Survey
- Myunghee Kang, Seung Yeon Ha, Joung Ho Han, Mee Sook Roh, Se Jin Jang, Hee Jin Lee, Heae Surng Park, Geon Kook Lee, Kyo Young Lee, Jin-Haeng Chung, Yoo Duk Choi, Chang Hun Lee, Lucia Kim, Myoung Ja Chung, Soon Hee Jung, Gou Young Kim, Wan-Seop Kim
- Received April 4, 2018 Accepted July 9, 2018 Published online July 16, 2018
- DOI: https://doi.org/10.4132/jptm.2018.07.10 [Accepted]
- 5,698 View
- 63 Download
- Molecular Testing of Lung Cancers
- Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
- J Pathol Transl Med. 2017;51(3):242-254. Published online April 21, 2017
- DOI: https://doi.org/10.4132/jptm.2017.04.10
- 18,153 View
- 617 Download
- 28 Web of Science
- 28 Crossref
-
 Abstract
Abstract
 PDF
PDF - Targeted therapies guided by molecular diagnostics have become a standard treatment of lung cancer. Epidermal growth factor receptor (EGFR) mutations and anaplastic lymphoma kinase (ALK) rearrangements are currently used as the best predictive biomarkers for EGFR tyrosine kinase inhibitors and ALK inhibitors, respectively. Besides EGFR and ALK, the list of druggable genetic alterations has been growing, including ROS1 rearrangements, RET rearrangements, and MET alterations. In this situation, pathologists should carefully manage clinical samples for molecular testing and should do their best to quickly and accurately identify patients who will benefit from precision therapeutics. Here, we grouped molecular biomarkers of lung cancers into three categories—mutations, gene rearrangements, and amplifications—and propose expanded guidelines on molecular testing of lung cancers.
-
Citations
Citations to this article as recorded by- Association between PD-L1 expression with EGFR, ALK, and ROS1 driver oncogene mutations in non-small cell lung cancer
Dülger Onur, Yaylım İlhan, Öz Büge
Indian Journal of Pathology and Microbiology.2025; 68(1): 36. CrossRef - Evidence-based Approach to Transthoracic Needle Biopsy: Procedural Techniques, Risks, and Controversies
Shravan Sridhar, Hannah G. Ahn, Sayedomid Ebrahimzadeh, Felicia Tang, Brett Elicker
RadioGraphics.2025;[Epub] CrossRef - Enhancing Lung Cancer Care in Portugal: Bridging Gaps for Improved Patient Outcomes
Raquel Ramos, Conceição Souto Moura, Mariana Costa, Nuno Jorge Lamas, Renato Correia, Diogo Garcez, José Miguel Pereira, Carlos Sousa, Nuno Vale
Journal of Personalized Medicine.2024; 14(5): 446. CrossRef - Evolution of therapy for ALK-positive lung carcinomas: Application of third-generation ALK inhibitors in real clinical practice
A. F. Nasretdinov, A. V. Sultanbaev, Sh. I. Musin, K. V. Menshikov, R. T. Ayupov, A. A. Izmailov, G. A. Serebrennikov, V. E. Askarov, D. V. Feoktistov
Meditsinskiy sovet = Medical Council.2024; (10): 74. CrossRef - Cost-effectiveness of next-generation sequencing for advanced EGFR/ALK-negative non-small cell lung cancer
Dong-Won Kang, Sun-Kyeong Park, Sokbom Kang, Eui-Kyung Lee
Lung Cancer.2024; 197: 107970. CrossRef - miR-92a-3p regulates cisplatin-induced cancer cell death
Romain Larrue, Sandy Fellah, Nihad Boukrout, Corentin De Sousa, Julie Lemaire, Carolane Leboeuf, Marine Goujon, Michael Perrais, Bernard Mari, Christelle Cauffiez, Nicolas Pottier, Cynthia Van der Hauwaert
Cell Death & Disease.2023;[Epub] CrossRef - Diagnostic Approach of Lung Cancer: A Literature Review
Jesi Hana, Novia Nurul Faizah
Jurnal Respirasi.2023; 9(2): 141. CrossRef - Molecular Pathology of Lung Cancer
James J. Saller, Theresa A. Boyle
Cold Spring Harbor Perspectives in Medicine.2022; 12(3): a037812. CrossRef - Landscape of EGFR mutations in lung adenocarcinoma: a single institute experience with comparison of PANAMutyper testing and targeted next-generation sequencing
Jeonghyo Lee, Yeon Bi Han, Hyun Jung Kwon, Song Kook Lee, Hyojin Kim, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2022; 56(5): 249. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - TM4SF4 and LRRK2 Are Potential Therapeutic Targets in Lung and Breast Cancers through Outlier Analysis
Kyungsoo Jung, Joon-Seok Choi, Beom-Mo Koo, Yu Jin Kim, Ji-Young Song, Minjung Sung, Eun Sol Chang, Ka-Won Noh, Sungbin An, Mi-Sook Lee, Kyoung Song, Hannah Lee, Ryong Nam Kim, Young Kee Shin, Doo-Yi Oh, Yoon-La Choi
Cancer Research and Treatment.2021; 53(1): 9. CrossRef - The promises and challenges of early non‐small cell lung cancer detection: patient perceptions, low‐dose CT screening, bronchoscopy and biomarkers
Lukas Kalinke, Ricky Thakrar, Sam M. Janes
Molecular Oncology.2021; 15(10): 2544. CrossRef - Cost-effectiveness analyses of targeted therapy and immunotherapy for advanced non-small cell lung cancer in the United States: a systematic review
Anthony Yu, Eva Huang, Momoka Abe, Kang An, Sun-Kyeong Park, Chanhyun Park
Expert Review of Pharmacoeconomics & Outcomes Research.2021; 21(3): 381. CrossRef - The expanding capability and clinical relevance of molecular diagnostic technology to identify and evaluate EGFR mutations in advanced/metastatic NSCLC
Parth Shah, Jacob Sands, Nicola Normanno
Lung Cancer.2021; 160: 118. CrossRef - Testing for EGFR Mutations and ALK Rearrangements in Advanced Non-Small-Cell Lung Cancer: Considerations for Countries in Emerging Markets
Mercedes L Dalurzo, Alejandro Avilés-Salas, Fernando Augusto Soares, Yingyong Hou, Yuan Li, Anna Stroganova, Büge Öz, Arif Abdillah, Hui Wan, Yoon-La Choi
OncoTargets and Therapy.2021; Volume 14: 4671. CrossRef - Treatment of Patients With Non–Small-Cell Lung Cancer Harboring Rare Oncogenic Mutations
Melina E. Marmarelis, Corey J. Langer
Clinical Lung Cancer.2020; 21(5): 395. CrossRef - Detection of Targetable Genetic Alterations in Korean Lung Cancer Patients: A Comparison Study of Single-Gene Assays and Targeted Next-Generation Sequencing
Eunhyang Park, Hyo Sup Shim
Cancer Research and Treatment.2020; 52(2): 543. CrossRef - High prevalence of ROS1 gene rearrangement detected by FISH in EGFR and ALK negative lung adenocarcinoma
Yuyin Xu, Heng Chang, Lijing Wu, Xin Zhang, Ling Zhang, Jing Zhang, Yuan Li, Lei Shen, Xiaoli Zhu, Xiaoyan Zhou, Qianming Bai
Experimental and Molecular Pathology.2020; 117: 104548. CrossRef - An All-In-One Transcriptome-Based Assay to Identify Therapy-Guiding Genomic Aberrations in Nonsmall Cell Lung Cancer Patients
Jiacong Wei, Anna A. Rybczynska, Pei Meng, Martijn Terpstra, Ali Saber, Jantine Sietzema, Wim Timens, Ed Schuuring, T. Jeroen N. Hiltermann, Harry. J.M. Groen, Anthonie van der Wekken, Anke van den Berg, Klaas Kok
Cancers.2020; 12(10): 2843. CrossRef - Immunotherapy in EGFR-Mutant and ALK-Positive Lung Cancer
Alexander Gavralidis, Justin F. Gainor
The Cancer Journal.2020; 26(6): 517. CrossRef - Role of Immunocytochemistry in the Cytological Diagnosis of Pulmonary Tumors
Jasna Metovic, Luisella Righi, Luisa Delsedime, Marco Volante, Mauro Papotti
Acta Cytologica.2020; 64(1-2): 16. CrossRef - Molecular Diagnostic Assays and Clinicopathologic Implications of MET Exon 14 Skipping Mutation in Non–small-cell Lung Cancer
Eun Kyung Kim, Kyung A. Kim, Chang Young Lee, Sangwoo Kim, Sunhee Chang, Byoung Chul Cho, Hyo Sup Shim
Clinical Lung Cancer.2019; 20(1): e123. CrossRef - PD‐L1 expression in ROS1‐rearranged non‐small cell lung cancer: A study using simultaneous genotypic screening of EGFR, ALK, and ROS1
Jongmin Lee, Chan Kwon Park, Hyoung‐Kyu Yoon, Young Jo Sa, In Sook Woo, Hyo Rim Kim, Sue Youn Kim, Tae‐Jung Kim
Thoracic Cancer.2019; 10(1): 103. CrossRef - Human Leukocyte Antigen Class I and Programmed Death-Ligand 1 Coexpression Is an Independent Poor Prognostic Factor in Adenocarcinoma of the Lung
Yeon Bi Han, Hyun Jung Kwon, Soo Young Park, Eun-Sun Kim, Hyojin Kim, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2019; 53(2): 86. CrossRef - Molecular testing for advanced non-small cell lung cancer in Malaysia: Consensus statement from the College of Pathologists, Academy of Medicine Malaysia, the Malaysian Thoracic Society, and the Malaysian Oncological Society
Pathmanathan Rajadurai, Phaik Leng Cheah, Soon Hin How, Chong Kin Liam, Muhammad Azrif Ahmad Annuar, Norhayati Omar, Noriah Othman, Nurhayati Mohd Marzuki, Yong Kek Pang, Ros Suzanna Ahmad Bustamam, Lye Mun Tho
Lung Cancer.2019; 136: 65. CrossRef - Somatic mutations and immune checkpoint biomarkers
Brielle A. Parris, Eloise Shaw, Brendan Pang, Richie Soong, Kwun Fong, Ross A. Soo
Respirology.2019; 24(3): 215. CrossRef - Adverse Event Management in Patients with BRAF V600E-Mutant Non-Small Cell Lung Cancer Treated with Dabrafenib plus Trametinib
Anna Chalmers, Laura Cannon, Wallace Akerley
The Oncologist.2019; 24(7): 963. CrossRef - Genetic and clinicopathologic characteristics of lung adenocarcinoma with tumor spread through air spaces
Jae Seok Lee, Eun Kyung Kim, Moonsik Kim, Hyo Sup Shim
Lung Cancer.2018; 123: 121. CrossRef
- Association between PD-L1 expression with EGFR, ALK, and ROS1 driver oncogene mutations in non-small cell lung cancer
- Transformation to Small Cell Lung Cancer of Pulmonary Adenocarcinoma: Clinicopathologic Analysis of Six Cases
- Soomin Ahn, Soo Hyun Hwang, Joungho Han, Yoon-La Choi, Se-Hoon Lee, Jin Seok Ahn, Keunchil Park, Myung-Ju Ahn, Woong-Yang Park
- J Pathol Transl Med. 2016;50(4):258-263. Published online May 10, 2016
- DOI: https://doi.org/10.4132/jptm.2016.04.19
- 14,609 View
- 253 Download
- 54 Web of Science
- 49 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors (TKIs) are considered the first line treatment for a subset of EGFR-mutated non-small cell lung cancer (NSCLC) patients. Although transformation to small cell lung cancer (SCLC) is one of the known mechanisms of resistance to EGFR TKIs, it is not certain whether transformation to SCLC is exclusively found as a mechanism of TKI resistance in EGFR-mutant tumors.
Methods
We identified six patients with primary lung adenocarcinoma that showed transformation to SCLC on second biopsy (n = 401) during a 6-year period. Clinicopathologic information was analyzed and EGFR mutation results were compared between initial and second biopsy samples.
Results
Six patients showed transformation from adenocarcinoma to SCLC, of which four were pure SCLCs and two were combined adenocarcinoma and SCLCs. Clinically, four cases were EGFR-mutant tumors from non-smoking females who underwent TKI treatment, and the EGFR mutation was retained in the transformed SCLC tumors. The remaining two adenocarcinomas were EGFR wild-type, and one of these patients received EGFR TKI treatment.
Conclusions
NSCLC can acquire a neuroendocrine phenotype with or without EGFR TKI treatment. -
Citations
Citations to this article as recorded by- Small cell lung cancer transdifferentiation: not a negligible phenomenon
Lilla Horvath, Kristiina Boettiger, Zsolt Megyesfalvi, Balázs Döme, Clemens Aigner, Anita Horváth-Rózsás, Judit Berta
Current Opinion in Oncology.2026; 38(1): 39. CrossRef - Patients outcomes in lung adenocarcinoma transforming to small-cell lung cancer after tyrosine kinase inhibitor therapy
Shuai Wang, Yongsen Wang, Xuan Wu, Li Yang, Xiaoju Zhang
World Journal of Surgical Oncology.2025;[Epub] CrossRef - Baseline retinoblastoma transcriptional corepressor 1 (Rb1) functional inactivation is a pre-requisite but not sufficient for small-cell histological transformation in epidermal growth factor receptor (EGFR) mutant lung adenocarcinomas post-tyrosine kinas
Aruna Nambirajan, Amber Rathor, Hemavathi Baskarane, Anju GS, Sachin Khurana, Somagattu Sushmitha, Aparna Sharma, Prabhat Singh Malik, Deepali Jain
Virchows Archiv.2025; 487(3): 639. CrossRef - Case Report: Transforming small cell lung cancer: two cases report and literature review
Jinlong Liu, Jing Ai, Lize Zhao, Yimeng Qian, Qingxin Zhao, Chunling Ma, Yu Zhao, Jing Zhao
Frontiers in Oncology.2025;[Epub] CrossRef - Exploration of CT-based discrimination and diagnosis of various pathological types of ground glass nodules in the lungs
Haihui Wu, Xiong Zhang, Zheng Zhong
BMC Medical Imaging.2025;[Epub] CrossRef - Correlation between treatments and outcomes of patients with EGFR-mutated non-small-cell lung cancer that transitioned into small-cell lung cancer: an international retrospective study
C. Catania, S.V. Liu, M. Garassino, A. Delmonte, V. Scotti, F. Cappuzzo, C. Genova, A. Russo, M. Russano, C. Bennati, I. Colantonio, S. Martini, M. Pino, F. Conforti, L. Pala, G. Minuti, F. Citarella, E. Olmetto, A. Esposito, P. Cascetta, A. Di Lello, T.
ESMO Open.2025; 10(7): 105326. CrossRef - TPM3–NTRK1 fusion confers resistance to osimertinib in lung adenocarcinoma: a model in a continuous cell line
Fang Cao, Jiayin Dai, Kun Dong, Zhenli Yang, Yanli Zhu, Changsong Qi, Dongmei Lin, Xiaocui Bian, Yuqin Liu
Human Cell.2025;[Epub] CrossRef - Transformation to small cell lung cancer is irrespective of EGFR and accelerated by SMAD4-mediated ASCL1 transcription independently of RB1 in non-small cell lung cancer
Xi Ding, Min-xing Shi, Di Liu, Jing-xue Cao, Kai-xuan Zhang, Run-dong Zhang, Li-ping Zhang, Kai-xing Ai, Bo Su, Jie Zhang
Cell Communication and Signaling.2024;[Epub] CrossRef - The study of primary and acquired resistance to first-line osimertinib to improve the outcome of EGFR-mutated advanced Non-small cell lung cancer patients: the challenge is open for new therapeutic strategies
Alessandra Ferro, Gian Marco Marinato, Cristiana Mulargiu, Monica Marino, Giulia Pasello, Valentina Guarneri, Laura Bonanno
Critical Reviews in Oncology/Hematology.2024; 196: 104295. CrossRef - Comprehensive molecular and clinical insights into non-small cell lung cancer transformation to small cell lung cancer with an illustrative case report
Kresimir Tomic, Kristina Krpina, Lara Baticic, Miroslav Samarzija, Semir Vranic
Journal of Drug Targeting.2024; 32(5): 499. CrossRef - Transcriptomic Heterogeneity of EGFR-Mutant Non–Small Cell Lung Cancer Evolution Toward Small-Cell Lung Cancer
Songji Oh, Jaemoon Koh, Tae Min Kim, Soyeon Kim, Jeonghwan Youk, Miso Kim, Bhumsuk Keam, Yoon Kyung Jeon, Ja-Lok Ku, Dong-Wan Kim, Doo Hyun Chung, Dae Seog Heo
Clinical Cancer Research.2024; 30(20): 4729. CrossRef - Transformation of lung adenocarcinoma into small cell lung cancer after treatment with epidermal growth factor receptor tyrosine kinase inhibitors
Linwu Kuang, Yangkai Li
Oncology and Translational Medicine.2024; 10(6): 286. CrossRef - Exon-18-EGFR Mutated Transformed Small-Cell Lung Cancer: A Case Report and Literature Review
Nunzio Digiacomo, Tommaso De Pas, Giovanna Rossi, Paola Bossi, Erika Stucchi, Fabio Conforti, Emilia Cocorocchio, Daniele Laszlo, Laura Pala, Emma Zattarin, Chiara Catania
Current Oncology.2023; 30(3): 3494. CrossRef - Current knowledge of small cell lung cancer transformation from non-small cell lung cancer
Giuseppe Giaccone, Yongfeng He
Seminars in Cancer Biology.2023; 94: 1. CrossRef - Targeting the EGFR signaling pathway in cancer therapy: What’s new in 2023?
Sushanta Halder, Soumi Basu, Shobhit P. Lall, Apar K. Ganti, Surinder K. Batra, Parthasarathy Seshacharyulu
Expert Opinion on Therapeutic Targets.2023; 27(4-5): 305. CrossRef - Outcomes in Patients With Lung Adenocarcinoma With Transformation to Small Cell Lung Cancer After EGFR Tyrosine Kinase Inhibitors Resistance: A Systematic Review and Pooled Analysis
Jinhe Xu, Lihuan Xu, Baoshan Wang, Wencui Kong, Ying Chen, Zongyang Yu
Frontiers in Oncology.2022;[Epub] CrossRef - Small cell lung cancer transformation: From pathogenesis to treatment
Xiaomeng Yin, Yueyi Li, Hang Wang, Tingting Jia, Enli Wang, Yuling Luo, Yuhao Wei, Zeyi Qin, Xuelei Ma
Seminars in Cancer Biology.2022; 86: 595. CrossRef - Small Cell Lung Cancer Transformation following Treatment in EGFR-Mutated Non-Small Cell Lung Cancer
Isa Mambetsariev, Leonidas Arvanitis, Jeremy Fricke, Rebecca Pharaon, Angel R. Baroz, Michelle Afkhami, Marianna Koczywas, Erminia Massarelli, Ravi Salgia
Journal of Clinical Medicine.2022; 11(5): 1429. CrossRef - Morphologic-Molecular Transformation of Oncogene Addicted Non-Small Cell Lung Cancer
Fiorella Calabrese, Federica Pezzuto, Francesca Lunardi, Francesco Fortarezza, Sofia-Eleni Tzorakoleftheraki, Maria Vittoria Resi, Mariaenrica Tiné, Giulia Pasello, Paul Hofman
International Journal of Molecular Sciences.2022; 23(8): 4164. CrossRef - Genomic and Gene Expression Studies Helped to Define the Heterogeneity of Small-Cell Lung Cancer and Other Lung Neuroendocrine Tumors and to Identify New Therapeutic Targets
Ugo Testa, Elvira Pelosi, Germana Castelli
Onco.2022; 2(3): 186. CrossRef - Neuroendocrine transformation from EGFR/ALK-wild type or TKI-naïve non-small cell lung cancer: An under-recognized phenomenon
Xiao Chu, Yuyin Xu, Ye Li, Yue Zhou, Li Chu, Xi Yang, Jianjiao Ni, Yida Li, Tiantian Guo, Zhiqin Zheng, Qiang Zheng, Qianlan Yao, Yuan Li, Xiaoyan Zhou, Zhengfei Zhu
Lung Cancer.2022; 169: 22. CrossRef - Three Third-Generation Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors in Non-Small Cell Lung Cancer: Similarities and Differences
Ling Chen, Yangqingqing Zhou, Chaosheng Gan, XiaoLi Wang, Yihui Liu, Chunhui Dong, Ruiyuan He, Jin Yang
Cancer Investigation.2022; 40(7): 590. CrossRef - Histomorphological transformation from non-small cell lung carcinoma to small cell lung carcinoma after targeted therapy or immunotherapy: A report of two cases
Hao Liu, Li-Hong Chen, Zhi-Hui Zhang, Ning Wang, Si-Hui Zhuang, Hao Chen, Jin Du, Li-Juan Pang, Yan Qi
Frontiers in Oncology.2022;[Epub] CrossRef - Impressive response to dabrafenib, trametinib, and osimertinib in a metastatic EGFR-mutant/BRAF V600E lung adenocarcinoma patient
Maurício Fernando Silva Almeida Ribeiro, Franciele Hinterholz Knebel, Fabiana Bettoni, Rodrigo Saddi, Karina Perez Sacardo, Felipe Sales Nogueira Amorim Canedo, João Victor Machado Alessi, Andrea Kazumi Shimada, José Flávio Gomes Marin, Anamaria Aranha Ca
npj Precision Oncology.2021;[Epub] CrossRef - Histological transformation of non-small cell lung cancer: Clinical analysis of nine cases
Cai-Bao Jin, Ling Yang
World Journal of Clinical Cases.2021; 9(18): 4617. CrossRef - Lamellarin 14, a derivative of marine alkaloids, inhibits the T790M/C797S mutant epidermal growth factor receptor
Naoyuki Nishiya, Yusuke Oku, Chie Ishikawa, Tsutomu Fukuda, Shingo Dan, Tetsuo Mashima, Masaru Ushijima, Yoko Furukawa, Yuka Sasaki, Keishi Otsu, Tomoko Sakyo, Masanori Abe, Honami Yonezawa, Fumito Ishibashi, Masaaki Matsuura, Akihiro Tomida, Hiroyuki Sei
Cancer Science.2021; 112(5): 1963. CrossRef - Case Report: Transformation From Non-Small Cell Lung Cancer to Small Cell Lung Cancer During Anti-PD-1 Therapy: A Report of Two Cases
Qian Shen, Jingjing Qu, Lingyan Sheng, Qiqi Gao, Jianying Zhou
Frontiers in Oncology.2021;[Epub] CrossRef - Exploring the resistance mechanisms of second-line osimertinib and their prognostic implications using next-generation sequencing in patients with non-small-cell lung cancer
Kyoungmin Lee, Deokhoon Kim, Shinkyo Yoon, Dae Ho Lee, Sang-We Kim
European Journal of Cancer.2021; 148: 202. CrossRef - Comprehensive analysis of treatment modes and clinical outcomes of small cell lung cancer transformed from epidermal growth factor receptor mutant lung adenocarcinoma
Shouzheng Wang, Tongji Xie, Xuezhi Hao, Yan Wang, Xingsheng Hu, Lin Wang, Yan Li, Junling Li, Puyuan Xing
Thoracic Cancer.2021; 12(19): 2585. CrossRef - EGFR-Mutant SCLC Exhibits Heterogeneous Phenotypes and Resistance to Common Antineoplastic Drugs
Chih-An Lin, Sung-Liang Yu, Hsuan-Yu Chen, Huei-Wen Chen, Shr-Uen Lin, Chia-Ching Chang, Chong-Jen Yu, Pan-Chyr Yang, Chao-Chi Ho
Journal of Thoracic Oncology.2019; 14(3): 513. CrossRef - The clinicopathologic of pulmonary adenocarcinoma transformation to small cell lung cancer
Haiyan Yang, Li Liu, Chunhua Zhou, Yi Xiong, Yijuan Hu, Nong Yang, Jingjing Qu
Medicine.2019; 98(12): e14893. CrossRef - Chemistry and pharmacological diversity of quinoxaline motifs as anticancer agents
Olayinka O. Ajani, Martins T. Nlebemuo, Joseph A. Adekoya, Kehinde O. Ogunniran, Tolutope O. Siyanbola, Christiana O. Ajanaku
Acta Pharmaceutica.2019; 69(2): 177. CrossRef - Resistance to EGFR inhibitors in non-small cell lung cancer: Clinical management and future perspectives
Chiara Tomasello, Cinzia Baldessari, Martina Napolitano, Giulia Orsi, Giulia Grizzi, Federica Bertolini, Fausto Barbieri, Stefano Cascinu
Critical Reviews in Oncology/Hematology.2018; 123: 149. CrossRef - Small cell lung cancer transformation from EGFR-mutated lung adenocarcinoma: A case report and literatures review
Yangyang Liu
Cancer Biology & Therapy.2018; 19(6): 445. CrossRef - Anaplastic lymphoma kinase (ALK)-expressing Lung Adenocarcinoma with Combined Neuroendocrine Component or Neuroendocrine Transformation: Implications for Neuroendocrine Transformation and Response to ALK-tyrosine Kinase Inhibitors
Jongmin Sim, Hyunjin Kim, Jiyeon Hyeon, Yoon-La Choi, Joungho Han
Journal of Korean Medical Science.2018;[Epub] CrossRef - Assessment of Resistance Mechanisms and Clinical Implications in Patients WithEGFRT790M–Positive Lung Cancer and Acquired Resistance to Osimertinib
Geoffrey R. Oxnard, Yuebi Hu, Kathryn F. Mileham, Hatim Husain, Daniel B. Costa, Philip Tracy, Nora Feeney, Lynette M. Sholl, Suzanne E. Dahlberg, Amanda J. Redig, David J. Kwiatkowski, Michael S. Rabin, Cloud P. Paweletz, Kenneth S. Thress, Pasi A. Jänne
JAMA Oncology.2018; 4(11): 1527. CrossRef - Clinicopathological and genomic comparisons between different histologic components in combined small cell lung cancer and non-small cell lung cancer
Mong-Wei Lin, Kang-Yi Su, Te-Jen Su, Chia-Ching Chang, Jing-Wei Lin, Yi-Hsuan Lee, Sung-Liang Yu, Jin-Shing Chen, Min-Shu Hsieh
Lung Cancer.2018; 125: 282. CrossRef - Transformation to small‑cell lung cancer following treatment with icotinib in a patient with lung adenocarcinoma
Hongyang Lu, Bo Chen, Jing Qin, Fajun Xie, Na Han, Zhiyu Huang
Oncology Letters.2018;[Epub] CrossRef - Histological transformation of adenocarcinoma to small cell carcinoma lung as a rare mechanism of resistance to epidermal growth factor receptor-tyrosine kinase inhibitors: Report of a case with review of literature
Monalisa Hui, ShantveerG Uppin, BalaJoseph Stalin, G Sadashivudu
Lung India.2018; 35(2): 160. CrossRef - A rare case of squamous cell carcinoma lung with multiple locoregional recurrences and histological transformation
Ram Niwas, Shibdas Chakrabarti, Viswesvaran Balasubramanian, ManasKamal Sen, JagdishChander Suri
Lung India.2018; 35(6): 511. CrossRef - Small cell lung cancer transformation during immunotherapy with nivolumab: A case report
Takuma Imakita, Kohei Fujita, Osamu Kanai, Tsuyoshi Terashima, Tadashi Mio
Respiratory Medicine Case Reports.2017; 21: 52. CrossRef - Pulmonary neuroendocrine tumor in a female wolf (Canis lupus lupus)
Ayako SHIRAKI, Toshinori YOSHIDA, Masahi KAWASHIMA, Hirotada MURAYAMA, Rei NAGAHARA, Nanao ITO, Makoto SHIBUTANI
Journal of Veterinary Medical Science.2017; 79(3): 588. CrossRef - Secondary biopsy of non‐oncogenic‐driven lung cancer may reveal a clinically sensible histologic change. A brief report of two paradigmatic cases
Maria C. Mengoli, Giulia Orsi, Filippo Lococo, Giulia Grizzi, Fausto Barbieri, Federica Bertolini, Giulio Rossi, Silvia Novello
Thoracic Cancer.2017; 8(4): 359. CrossRef - Small-cell lung cancer in never smokers: The clinicopathological features including the prognosis
Masahiro Yamasaki, Naomi Saito, Wakako Daido, Sayaka Ishiyama, Naoko Deguchi, Masaya Taniwaki, Akio Sakatani, Megumu Fujihara, Nobuyuki Ohashi, Ken-ichi Arita
Cancer Treatment and Research Communications.2017; 12: 1. CrossRef - Clonal History and Genetic Predictors of Transformation Into Small-Cell Carcinomas From Lung Adenocarcinomas
June-Koo Lee, Junehawk Lee, Sehui Kim, Soyeon Kim, Jeonghwan Youk, Seongyeol Park, Yohan An, Bhumsuk Keam, Dong-Wan Kim, Dae Seog Heo, Young Tae Kim, Jin-Soo Kim, Se Hyun Kim, Jong Seok Lee, Se-Hoon Lee, Keunchil Park, Ja-Lok Ku, Yoon Kyung Jeon, Doo Hyun
Journal of Clinical Oncology.2017; 35(26): 3065. CrossRef - Australian recommendations for EGFR T790M testing in advanced non-small cell lung cancer
Thomas John, Jeffrey J Bowden, Stephen Clarke, Stephen B Fox, Kerryn Garrett, Keith Horwood, Christos S Karapetis
Asia-Pacific Journal of Clinical Oncology.2017; 13(4): 296. CrossRef - Metastatic Squamous Cell Carcinoma from Lung Adenocarcinoma after Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor Therapy
Hyung Kyu Park, Youjeong Seo, Yoon-La Choi, Myung-Ju Ahn, Joungho Han
Journal of Pathology and Translational Medicine.2017; 51(4): 441. CrossRef - Sequential occurrence of small cell and non-small lung cancer in a male patient: Is it a transformation?
Ahsan Wahab, Kavitha Kesari, Siddique Chaudhary, Mahin Khan, Hafiz Khan, Susan Smith, Yanis Boumber
Cancer Biology & Therapy.2017; 18(12): 940. CrossRef - The expression of S100B protein in serum of patients with brain metastases from small-cell lung cancer and its clinical significance
Shanling Mu, Hong Ma, Jun Shi, Dezhi Zhen
Oncology Letters.2017;[Epub] CrossRef
- Small cell lung cancer transdifferentiation: not a negligible phenomenon
- Sclerosing Perivascular Epithelioid Cell Tumor of the Lung: A Case Report with Cytologic Findings
- Ha Yeon Kim, Jin Hyuk Choi, Hye Seung Lee, Yoo Jin Choi, Aeree Kim, Han Kyeom Kim
- J Pathol Transl Med. 2016;50(3):238-242. Published online April 11, 2016
- DOI: https://doi.org/10.4132/jptm.2016.02.19
- 10,372 View
- 109 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF - Benign perivascular epithelioid cell tumor (PEComa) of the lung is a rare benign neoplasm, a sclerosing variant of which is even rarer. We present a case of 51-year-old man who was diagnosed with benign sclerosing PEComa by percutaneous fine needle aspiration cytology and biopsy. The aspirate revealed a few cell clusters composed of bland-looking polygonal or spindle cells with fine granular or clear cytoplasm. Occasional fine vessel-like structures with surrounding hyalinized materials were seen. The patient later underwent wedge resection of the lung. The histopathological study of the resected specimen revealed sheets of polygonal cells with clear vacuolated cytoplasm, variably sized thin blood vessels, and densely hyalinized stroma. In immunohistochemical studies, reactivity of tumor cells for human melanoma black 45 and Melan-A further supported the diagnosis of benign sclerosing PEComa. To the best of our knowledge, this is the first case of benign sclerosing PEComa described in lung.
-
Citations
Citations to this article as recorded by- Renal sclerosing AML/PEComa in a male - A case report and literature review
Zoe Williams, Paul Kim, James Kovacic, Andrew Shepherd, Krishan Rasiah, Ankur Dhar, Kathleen Young
Urology Case Reports.2026; 65: 103326. CrossRef - Robotic Treatment of Adrenal Sclerosing PEComa: A Case Report with 13 Years of Follow-Up and a Literature Review
Alessio Paladini, Raffaele La Mura, Michele Del Zingaro, Luca Lepri, Andrea Vitale, Jessica Pagnotta, Matteo Mearini, Guido Massa, Ettore Mearini, Giovanni Cochetti
Applied Sciences.2025; 15(16): 9161. CrossRef - A rare case of pulmonary perivascular epithelioid cell neoplasm
Maolin Xu, Xiaofang Guo
Asian Journal of Surgery.2025;[Epub] CrossRef - Cytopathology of rare gastric mesenchymal neoplasms: A series of 25 cases and review of literature
Carla Saoud, Peter B. Illei, Momin T. Siddiqui, Syed Z. Ali
Cytopathology.2023; 34(1): 15. CrossRef - Retroperitoneal Sclerosing Angiomyolipoma with Long-Term Follow up: A Case Report with Unique Clinicopathologic and Genomic Profile
Liwei Jia, Vandana Panwar, Michelle Parmley, Elena Lucas, Ivan Pedrosa, Payal Kapur
International Journal of Surgical Pathology.2022; 30(1): 86. CrossRef - Perivascular epithelioid cell tumor of the lung: A case report and literature review
Shaofu Yu, Shasha Zhai, Qian Gong, Xiaoping Hu, Wenjuan Yang, Liyu Liu, Yi Kong, Lin Wu, Xingxiang Pu
Thoracic Cancer.2022; 13(17): 2542. CrossRef - Cytopathology of extra-renal perivascular epithelioid cell tumor (PEComa): a series of 7 cases and review of the literature
Sintawat Wangsiricharoen, Tatianna C. Larman, Paul E. Wakely, Momin T. Siddiqui, Syed Z. Ali
Journal of the American Society of Cytopathology.2021; 10(2): 175. CrossRef - Clear cell sugar tumour: a rare tumour of the lung
Sarah Page, Matthew S. Yong, Alka Sinha, Pankaj Saxena
ANZ Journal of Surgery.2020;[Epub] CrossRef - Perivascular Epithelioid Cell Tumors (PEComas) of the Orbit
Panagiotis Paliogiannis, Giuseppe Palmieri, Francesco Tanda, Antonio Cossu
Journal of Pathology and Translational Medicine.2017; 51(1): 7. CrossRef
- Renal sclerosing AML/PEComa in a male - A case report and literature review
- Analysis of Mutations in Epidermal Growth Factor Receptor Gene in Korean Patients with Non-small Cell Lung Cancer: Summary of a Nationwide Survey
- Sang Hwa Lee, Wan Seop Kim, Yoo Duk Choi, Jeong Wook Seo, Joung Ho Han, Mi Jin Kim, Lucia Kim, Geon Kook Lee, Chang Hun Lee, Mee Hye Oh, Gou Young Kim, Sun Hee Sung, Kyo Young Lee, Sun Hee Chang, Mee Sook Rho, Han Kyeom Kim, Soon Hee Jung, Se Jin Jang, The Cardiopulmonary Pathology Study Group of Korean Society of Pathologists
- J Pathol Transl Med. 2015;49(6):481-488. Published online October 13, 2015
- DOI: https://doi.org/10.4132/jptm.2015.09.14
- 12,866 View
- 108 Download
- 22 Web of Science
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Analysis of mutations in the epidermal growth factor receptor gene (EGFR) is important for predicting response to EGFR tyrosine kinase inhibitors. The overall rate of EGFR mutations in Korean patients is variable. To obtain comprehensive data on the status of EGFR mutations in Korean patients with lung cancer, the Cardiopulmonary Pathology Study Group of the Korean Society of Pathologists initiated a nationwide survey. Methods: We obtained 1,753 reports on EGFR mutations in patients with lung cancer from 15 hospitals between January and December 2009. We compared EGFR mutations with patient age, sex, history of smoking, histologic diagnosis, specimen type, procurement site, tumor cell dissection, and laboratory status. Results: The overall EGFR mutation rate was 34.3% in patients with non-small cell lung cancer (NSCLC) and 43.3% in patients with adenocarcinoma. EGFR mutation rate was significantly higher in women, never smokers, patients with adenocarcinoma, and patients who had undergone excisional biopsy. EGFR mutation rates did not differ with respect to patient age or procurement site among patients with NSCLC. Conclusions: EGFR mutation rates and statuses were similar to those in published data from other East Asian countries. -
Citations
Citations to this article as recorded by- Projected cancer burden attributable to population aging: Insight from a rapidly aging society
Minh‐Thao Tu, Hoejun Kwon, Yoon‐Jung Choi, Hyunsoon Cho
International Journal of Cancer.2026; 158(4): 951. CrossRef - Assessing mutation-clinical correlations and treatment outcomes in Vietnamese non-small cell lung cancer patients
Hoang-Bac Nguyen, Bang-Suong Nguyen-Thi, Huu-Huy Nguyen, Minh-Khoi Le, Quoc-Trung Lam, Tuan-Anh Nguyen
Practical Laboratory Medicine.2025; 45: e00477. CrossRef - Gradual Increase in Lung Cancer Risk Due to Particulate Matter Exposure in Patients With Pulmonary Function Impairments: A Nationwide Korean Database Analysis
Jongin Lee, Joon Young Choi, Jeong Uk Lim
Journal of Korean Medical Science.2025;[Epub] CrossRef - Real-world treatment outcomes in South Korean patients with epidermal growth factor receptor-mutant non-small cell lung cancer
Young Saing Kim, Eun Young Lee, Hyun Woo Lee, Jin-Hyuk Choi, Tae-Hwan Kim, Yong Won Choi, Mi Sun Ahn
The Korean Journal of Internal Medicine.2025; 40(6): 1029. CrossRef - The role of oncogenes and tumor suppressor genes in determining survival rates of lung cancer patients in the population of North Sumatra, Indonesia
Noni Novisari Soeroso, Fannie Rizki Ananda, Johan Samuel Sitanggang, Noverita Sprinse Vinolina
F1000Research.2023; 11: 853. CrossRef - Comprehensive analysis of NGS and ARMS-PCR for detecting EGFR mutations based on 4467 cases of NSCLC patients
Changlong He, Chengcheng Wei, Jun Wen, Shi Chen, Ling Chen, Yue Wu, Yifan Shen, Huili Bai, Yangli Zhang, Xueping Chen, Xiaosong Li
Journal of Cancer Research and Clinical Oncology.2022; 148(2): 321. CrossRef - Unique characteristics of G719X and S768I compound double mutations of epidermal growth factor receptor (EGFR) gene in lung cancer of coal-producing areas of East Yunnan in Southwestern China
Jun-Ling Wang, Yu-Dong Fu, Yan-Hong Gao, Xiu-Ping Li, Qian Xiong, Rui Li, Bo Hou, Ruo-Shan Huang, Jun-Feng Wang, Jian-Kun Zhang, Jia-Ling Lv, Chao Zhang, Hong-Wei Li
Genes and Environment.2022;[Epub] CrossRef - Continuous Vaginal Bleeding Induced By EGFR-TKI in Premenopausal Female Patients With EGFR Mutant NSCLC
Min Yu, Xiaoyu Li, Xueqian Wu, Weiya Wang, Yanying Li, Yan Zhang, Shuang Zhang, Yongsheng Wang
Frontiers in Oncology.2022;[Epub] CrossRef - The role of oncogenes and tumor suppressor genes in determining survival rates of lung cancer patients in the population of North Sumatra, Indonesia
Noni Novisari Soeroso, Fannie Rizki Ananda, Johan Samuel Sitanggang, Noverita Sprinse Vinolina
F1000Research.2022; 11: 853. CrossRef - Adverse Event Profiles of Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors in Adenocarcinoma Lung Patients in North Sumatera Population
Moh. Ramadhani Soeroso, Noni Novisari Soeroso, Setia Putra Tarigan, Elisna Syahruddin
Open Access Macedonian Journal of Medical Sciences.2022; 10(T7): 134. CrossRef - Landscape of EGFR mutations in lung adenocarcinoma: a single institute experience with comparison of PANAMutyper testing and targeted next-generation sequencing
Jeonghyo Lee, Yeon Bi Han, Hyun Jung Kwon, Song Kook Lee, Hyojin Kim, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2022; 56(5): 249. CrossRef - Traditional Chinese Medicine Syndromes are Associated with Driver Gene Mutations and Clinical Characteristics in Patients with Lung Adenocarcinoma
Jili Yang, Haiyan Lu, Niancai Jing, Bo Wang, Huanyu Guo, Shoukun Sun, Yue Zhang, Chan-Yen Kuo
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Exosome-based detection of EGFR T790M in plasma and pleural fluid of prospectively enrolled non-small cell lung cancer patients after first-line tyrosine kinase inhibitor therapy
Yoonjung Kim, Saeam Shin, Kyung-A Lee
Cancer Cell International.2021;[Epub] CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Osimertinib in Patients with T790M-Positive Advanced Non-small Cell Lung Cancer: Korean Subgroup Analysis from Phase II Studies
Myung-Ju Ahn, Ji-Youn Han, Dong-Wan Kim, Byoung Chul Cho, Jin-Hyoung Kang, Sang-We Kim, James Chih-Hsin Yang, Tetsuya Mitsudomi, Jong Seok Lee
Cancer Research and Treatment.2020; 52(1): 284. CrossRef - Long non-coding RNA ATB promotes human non-small cell lung cancer proliferation and metastasis by suppressing miR-141-3p
Guojie Lu, Yaosen Zhang, Klaus Roemer
PLOS ONE.2020; 15(2): e0229118. CrossRef - Prognostic Role of S100A8 and S100A9 Protein Expressions in Non-small Cell Carcinoma of the Lung
Hyun Min Koh, Hyo Jung An, Gyung Hyuck Ko, Jeong Hee Lee, Jong Sil Lee, Dong Chul Kim, Jung Wook Yang, Min Hye Kim, Sung Hwan Kim, Kyung Nyeo Jeon, Gyeong-Won Lee, Se Min Jang, Dae Hyun Song
Journal of Pathology and Translational Medicine.2019; 53(1): 13. CrossRef - Epidermal growth factor receptor T790M mutations in non-small cell lung cancer (NSCLC) of Yunnan in southwestern China
Yongchun Zhou, Yuhui Ma, Hutao Shi, Yaxi Du, Yunchao Huang
Scientific Reports.2018;[Epub] CrossRef - Does the efficacy of epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor differ according to the type of EGFR mutation in non-small cell lung cancer?
Yong Won Choi, Jin-Hyuk Choi
The Korean Journal of Internal Medicine.2017; 32(3): 422. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - MET Exon 14 Skipping Mutations in Lung Adenocarcinoma: Clinicopathologic Implications and Prognostic Values
Geun Dong Lee, Seung Eun Lee, Doo-Yi Oh, Dan-bi Yu, Hae Min Jeong, Jooseok Kim, Sungyoul Hong, Hun Soon Jung, Ensel Oh, Ji-Young Song, Mi-Sook Lee, Mingi Kim, Kyungsoo Jung, Jhingook Kim, Young Kee Shin, Yoon-La Choi, Hyeong Ryul Kim
Journal of Thoracic Oncology.2017; 12(8): 1233. CrossRef - Epidermal growth factor receptor (EGFR) mutations in non-small cell lung cancer (NSCLC) of Yunnan in southwestern China
Yongchun Zhou, Yanlong Yang, Chenggang Yang, Yunlan Chen, Changshao Yang, Yaxi Du, Guangqiang Zhao, Yinjin Guo, Lianhua Ye, Yunchao Huang
Oncotarget.2017; 8(9): 15023. CrossRef - Detection of EGFR and KRAS Mutation by Pyrosequencing Analysis in Cytologic Samples of Non-Small Cell Lung Cancer
Seung Eun Lee, So-Young Lee, Hyung-Kyu Park, Seo-Young Oh, Hee-Joung Kim, Kye-Young Lee, Wan-Seop Kim
Journal of Korean Medical Science.2016; 31(8): 1224. CrossRef - MassARRAY, pyrosequencing, and PNA clamping for EGFR mutation detection in lung cancer tissue and cytological samples: a multicenter study
Kyueng-Whan Min, Wan-Seop Kim, Se Jin Jang, Yoo Duk Choi, Sunhee Chang, Soon Hee Jung, Lucia Kim, Mee-Sook Roh, Choong Sik Lee, Jung Weon Shim, Mi Jin Kim, Geon Kook Lee
Journal of Cancer Research and Clinical Oncology.2016; 142(10): 2209. CrossRef - Clinicopathologic characteristics of EGFR, KRAS, and ALK alterations in 6,595 lung cancers
Boram Lee, Taebum Lee, Se-Hoon Lee, Yoon-La Choi, Joungho Han
Oncotarget.2016; 7(17): 23874. CrossRef
- Projected cancer burden attributable to population aging: Insight from a rapidly aging society
- The Utilization of Cytologic Fine-Needle Aspirates of Lung Cancer for Molecular Diagnostic Testing
- Michael H. Roh
- J Pathol Transl Med. 2015;49(4):300-309. Published online June 16, 2015
- DOI: https://doi.org/10.4132/jptm.2015.06.16
- 17,077 View
- 173 Download
- 35 Web of Science
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF - In this era of precision medicine, our understanding and knowledge of the molecular landscape associated with lung cancer pathogenesis continues to evolve. This information is being increasingly exploited to treat advanced stage lung cancer patients with tailored, targeted therapy. During the management of these patients, minimally invasive procedures to obtain samples for tissue diagnoses are desirable. Cytologic fine-needle aspirates are often utilized for this purpose and are important not only for rendering diagnoses to subtype patients’ lung cancers, but also for ascertaining molecular diagnostic information for treatment purposes. Thus, cytologic fine-needle aspirates must be utilized and triaged judiciously to achieve both objectives. In this review, strategies in utilizing fine-needle aspirates will be discussed in the context of our current understanding of the clinically actionable molecular aberrations underlying non-small cell lung cancer and the molecular assays applied to these samples in order to obtain treatment-relevant molecular diagnostic information.
-
Citations
Citations to this article as recorded by- The Bridge: Supernatant Derived From Cytological Sample Preparations
Sinchita Roy‐Chowdhuri
Cytopathology.2025; 36(3): 222. CrossRef - Optimizing cytology and small biopsy specimen processing for ancillary studies: recommendations from the American Society of Cytopathology taskforce
Sinchita Roy-Chowdhuri, Christine N. Booth, Jonas J. Heymann, Elizabeth Jenkins, Joshua R. Menke, Sara E. Monaco, Ritu Nayar, Michiya Nishino, Roberto Ruiz-Cordero, Donna K. Russell, Anjali Saqi, Kaitlin E. Sundling, Michael J. Thrall, Vanda F. Torous, Ch
Journal of the American Society of Cytopathology.2025; 14(5): 285. CrossRef - Utility of Cell Block Preparation From CT-Guided FNAC with Immunohistochemistry in Diagnosing Primary Lung Carcinoma: A Prospective Study in A Tertiary Care Hospital
Subhargha Mandal, Abhishek Chowdhury, Riju Bhattacharyya, Palas Bhattacharyya
National Journal of Medical Research.2025; 15(04): 286. CrossRef - The American Cancer Society National Lung Cancer Roundtable strategic plan: Methods for improving turnaround time of comprehensive biomarker testing in non–small cell lung cancer
Sinchita Roy‐Chowdhuri, Haresh Mani, Adam H. Fox, Anne Tsao, Lynette M. Sholl, Farhood Farjah, Bruce E. Johnson, Raymond U. Osarogiagbon, M. Patricia Rivera, Gerard A. Silvestri, Robert A. Smith, Ignacio I. Wistuba
Cancer.2024; 130(24): 4200. CrossRef - Endobronchial ultrasound bronchoscopy Franseen fine needle biopsy tool versus standard fine needle aspiration needle: Impact on diagnosis and tissue adequacy
Matthew C. Aboudara, Timothy Saettele, Ossama Tawfik
Respiratory Medicine.2023; 208: 107131. CrossRef - Adequacy of small biopsy and cytology specimens for comprehensive genomic profiling of patients with non-small-cell lung cancer to determine eligibility for immune checkpoint inhibitor and targeted therapy
Erin Faber, Horiana Grosu, Sharjeel Sabir, Francis Anthony San Lucas, Bedia A Barkoh, Roland L Bassett, Rajyalakshmi Luthra, John Stewart, Sinchita Roy-Chowdhuri
Journal of Clinical Pathology.2022; 75(9): 612. CrossRef - Biomarker testing of cytology specimens in personalized medicine for lung cancer patients
Hyojin Kim, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2022; 56(6): 326. CrossRef - Formalin fixation for optimal concordance of programmed death‐ligand 1 immunostaining between cytologic and histologic specimens from patients with non–small cell lung cancer
Bregje M. Koomen, Jose van der Starre‐Gaal, Judith M. Vonk, Jan H. von der Thüsen, Jacqueline J. C. van der Meij, Kim Monkhorst, Stefan M. Willems, Wim Timens, Nils A. ’t Hart
Cancer Cytopathology.2021; 129(4): 304. CrossRef - Collection and Handling of Thoracic Small Biopsy and Cytology Specimens for Ancillary Studies: Guidelines from the College of American Pathologists (CAP)
Sinchita Roy-Chowdhuri
Journal of Molecular Pathology.2021; 2(1): 23. CrossRef - A decade of change: Trends in the practice of cytopathology at a tertiary care cancer centre
Peyman Dinarvand, Chinhua Liu, Sinchita Roy‐Chowdhuri
Cytopathology.2021; 32(5): 604. CrossRef - False‐negative programmed death‐ligand 1 immunostaining in ethanol‐fixed endobronchial ultrasound‐guided transbronchial needle aspiration specimens of non‐small‐cell lung cancer patients
Bregje M Koomen, Willem Vreuls, Mirthe de Boer, Emma J de Ruiter, Juergen Hoelters, Aryan Vink, Stefan M Willems
Histopathology.2021; 79(4): 480. CrossRef - Influence of preanalytical variables on performance of delta-like protein 3 (DLL3) predictive immunohistochemistry
Teodora Radonic, S. Duin, W. Vos, P. Kortman, Aeilko H. Zwinderman, Erik Thunnissen
Virchows Archiv.2021; 478(2): 293. CrossRef - Comparison of the SuperARMS and ARMS for detecting EGFR mutations in liquid-based cytology specimens from NSCLC patients
Wei Wu, Ziyang Cao, Wei Zhang, Liping Zhang, Likun Hou, Chunyan Wu
Diagnostic Pathology.2020;[Epub] CrossRef - Tumor cell representation by an improvised technique of fine-needle aspiration specimen acquisition and cell block preparation: Our experience in lung cancer cases in a peripheral center of eastern India
AnupKr Boler, Shreosee Roy, Arghya Bandyopadhyay, Abhishek Bandyopadhyay, MrinalKanti Ghosh
Journal of Cytology.2020; 37(2): 87. CrossRef - A new guideline from the College of American Pathologists to improve the adequacy of thoracic small specimens for ancillary studies
Sinchita Roy‐Chowdhuri
Cancer Cytopathology.2020; 128(10): 690. CrossRef - The utilization of cytologic and small biopsy samples for ancillary molecular testing
Michael H. Roh
Modern Pathology.2019; 32: 77. CrossRef - Diff-Quik Cytology Smears from Endobronchial Ultrasound Transbronchial Needle Aspiration Lymph Node Specimens as a Source of DNA for Next-Generation Sequencing Instead of Cell Blocks
David Fielding, Andrew J. Dalley, Farzad Bashirzadeh, Mahendra Singh, Lakshmy Nandakumar, Amy E. McCart Reed, Debra Black, Stephen Kazakoff, John V. Pearson, Katia Nones, Nicola Waddell, Sunil R. Lakhani, Peter T. Simpson
Respiration.2019; 97(6): 525. CrossRef - Molecular testing on endobronchial ultrasound (EBUS) fine needle aspirates (FNA): Impact of triage
Simon Sung, John P. Crapanzano, David DiBardino, David Swinarski, William A. Bulman, Anjali Saqi
Diagnostic Cytopathology.2018; 46(2): 122. CrossRef - Salvaging the supernatant: next generation cytopathology for solid tumor mutation profiling
Sinchita Roy-Chowdhuri, Meenakshi Mehrotra, Ana Maria Bolivar, Rashmi Kanagal-Shamanna, Bedia A. Barkoh, Brette Hannigan, Stephanie Zalles, Wenrui Ye, Dzifa Duose, Russell Broaddus, Gregg Staerkel, Ignacio Wistuba, L. Jeffrey Medeiros, Rajyalakshmi Luthra
Modern Pathology.2018; 31(7): 1036. CrossRef - Fluorescence in situ hybridization analysis on cytologic smears: An accurate and efficient method in the diagnosis of melanotic Xp11 translocation renal cancer
Alia Gupta, Mark Micale, Kurt D. Bernacki
Diagnostic Cytopathology.2018; 46(9): 786. CrossRef - Comprehensive Validation of Cytology Specimens for Next-Generation Sequencing and Clinical Practice Experience
Agnes Balla, Ken J. Hampel, Mukesh K. Sharma, Catherine E. Cottrell, Nikoletta Sidiropoulos
The Journal of Molecular Diagnostics.2018; 20(6): 812. CrossRef - Advances in Molecular Testing Techniques in Cytologic Specimens
Sinchita Roy-Chowdhuri
Surgical Pathology Clinics.2018; 11(3): 669. CrossRef - Next-generation molecular diagnosis: single-cell sequencing from bench to bedside
Wanjun Zhu, Xiao-Yan Zhang, Sadie L. Marjani, Jialing Zhang, Wengeng Zhang, Shixiu Wu, Xinghua Pan
Cellular and Molecular Life Sciences.2017; 74(5): 869. CrossRef - Big data from small samples: Informatics of next‐generation sequencing in cytopathology
Sinchita Roy‐Chowdhuri, Somak Roy, Sara E. Monaco, Mark J. Routbort, Liron Pantanowitz
Cancer Cytopathology.2017; 125(4): 236. CrossRef - Next‐generation sequencing of liquid‐based cytology non–small cell lung cancer samples
Jordan P. Reynolds, Yaolin Zhou, Maureen A. Jakubowski, Zhen Wang, Jennifer A. Brainard, Roger D. Klein, Carol F. Farver, Francisco A. Almeida, Yu‐Wei Cheng
Cancer Cytopathology.2017; 125(3): 178. CrossRef - Concurrent fine needle aspirations and core needle biopsies: a comparative study of substrates for next-generation sequencing in solid organ malignancies
Sinchita Roy-Chowdhuri, Hui Chen, Rajesh R Singh, Savitri Krishnamurthy, Keyur P Patel, Mark J Routbort, Jawad Manekia, Bedia A Barkoh, Hui Yao, Sharjeel Sabir, Russell R Broaddus, L Jeffrey Medeiros, Gregg Staerkel, John Stewart, Rajyalakshmi Luthra
Modern Pathology.2017; 30(4): 499. CrossRef - Diagnosis of anaplastic lymphoma kinase rearrangement in cytological samples through a fluorescence in situ hybridization–based assay: Cytological smears versus cell blocks
Federica Zito Marino, Giulio Rossi, Matteo Brunelli, Maria Gabriella Malzone, Giuseppina Liguori, Giuseppe Bogina, Alessandro Morabito, Gaetano Rocco, Renato Franco, Gerardo Botti
Cancer Cytopathology.2017; 125(5): 303. CrossRef - Next‐generation sequencing of cytologic preparations: An analysis of quality metrics
David H. Hwang, Elizabeth P. Garcia, Matthew D. Ducar, Edmund S. Cibas, Lynette M. Sholl
Cancer Cytopathology.2017; 125(10): 786. CrossRef - Recent advances in the pathology and molecular genetics of lung cancer: A practical review for cytopathologists
Erika F. Rodriguez, Sara E. Monaco
Journal of the American Society of Cytopathology.2016; 5(5): 252. CrossRef - Utilization of ancillary studies in the cytologic diagnosis of respiratory lesions: The papanicolaou society of cytopathology consensus recommendations for respiratory cytology
Lester J. Layfield, Sinchita Roy‐Chowdhuri, Zubair Baloch, Hormoz Ehya, Kim Geisinger, Susan J. Hsiao, Oscar Lin, Neal I. Lindeman, Michael Roh, Fernando Schmitt, Nikoletta Sidiropoulos, Paul A. VanderLaan
Diagnostic Cytopathology.2016; 44(12): 1000. CrossRef - Inflammatory myofibroblastic tumour
Michael McDermott
Seminars in Diagnostic Pathology.2016; 33(6): 358. CrossRef - Preanalytic Variables in Cytology: Lessons Learned From Next-Generation Sequencing—The MD Anderson Experience
Sinchita Roy-Chowdhuri, John Stewart
Archives of Pathology & Laboratory Medicine.2016; 140(11): 1191. CrossRef - Biomarker Testing in Lung Carcinoma Cytology Specimens: A Perspective From Members of the Pulmonary Pathology Society
Sinchita Roy-Chowdhuri, Dara L. Aisner, Timothy Craig Allen, Mary Beth Beasley, Alain Borczuk, Philip T. Cagle, Vera Capelozzi, Sanja Dacic, Gilda da Cunha Santos, Lida P. Hariri, Keith M. Kerr, Sylvie Lantuejoul, Mari Mino-Kenudson, Andre Moreira, Kirtee
Archives of Pathology & Laboratory Medicine.2016; 140(11): 1267. CrossRef - Identification of a novel partner gene, KIAA1217, fused to RET: Functional characterization and inhibitor sensitivity of two isoforms in lung adenocarcinoma
Mi-Sook Lee, Ryong Nam Kim, Hoseok I, Doo-Yi Oh, Ji-Young Song, Ka-Won Noh, Yu-Jin Kim, Jung Wook Yang, Maruja E. Lira, Chang Hun Lee, Min Ki Lee, Yeoung Dae Kim, Mao Mao, Joungho Han, Jhingook Kim, Yoon-La Choi
Oncotarget.2016; 7(24): 36101. CrossRef
- The Bridge: Supernatant Derived From Cytological Sample Preparations
KRAS Mutation Detection in Non-small Cell Lung Cancer Using a Peptide Nucleic Acid-Mediated Polymerase Chain Reaction Clamping Method and Comparative Validation with Next-Generation Sequencing- Boram Lee, Boin Lee, Gangmin Han, Mi Jung Kwon, Joungho Han, Yoon-La Choi
- Korean J Pathol. 2014;48(2):100-107. Published online April 28, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.2.100
- 14,279 View
- 104 Download
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF Background KRAS is one of commonly mutated genetic "drivers" in non-small cell lung cancers (NSCLCs). Recent studies indicate that patients withKRAS -mutated tumors do not benefit from adjuvant chemotherapy, so there is now a focus on targetingKRAS -mutated NSCLCs. A feasible mutation detection method is required in order to accurately test forKRAS status.Methods We compared direct Sanger sequencing and the peptide nucleic acid (PNA)-mediated polymerase chain reaction (PCR) clamping method in 134 NSCLCs and explored associations with clinicopathological factors. Next-generation sequencing (NGS) was used to validate the results of discordant cases. To increase the resolution of low-level somatic mutant molecules, PNA-mediated PCR clamping was used for mutant enrichment prior to NGS.
Results Twenty-one (15.7%) cases were found to have the
KRAS mutations using direct sequencing, with two additional cases by the PNA-mediated PCR clamping method. The frequencies ofKRAS mutant alleles were 2% and 4%, respectively, using conventional NGS, increasing up to 90% and 89%, using mutant-enriched NGS. TheKRAS mutation occurs more frequently in the tumors of smokers (p=.012) and in stage IV tumors (p=.032).Conclusions Direct sequencing can accurately detect mutations, but, it is not always possible to obtain a tumor sample with sufficient volume. The PNA-mediated PCR clamping can rapidly provide results with sufficient sensitivity.
-
Citations
Citations to this article as recorded by- KRAS mutated Non‐Small Lung Carcinoma: A Real World Context from the Indian subcontinent
Ullas Batra, Shrinidhi Nathany, Mansi Sharma, Amrith BP, Joslia T. Jose, Harkirat Singh, Sakshi Mattoo, Anurag Mehta
Cancer Medicine.2023; 12(3): 2869. CrossRef - Mechanism exploration and prognosis study of Astragali Radix-Spreading hedyotis herb for the treatment of lung adenocarcinoma based on bioinformatics approaches and molecular dynamics simulation
Junfeng Guo, Yuting Zhao, Xuanyu Wu, Ganggang Li, Yuwei Zhang, Yang Song, Quanyu Du
Frontiers in Chemistry.2023;[Epub] CrossRef - PEAC: An Ultrasensitive and Cost-Effective MRD Detection System in Non-small Cell Lung Cancer Using Plasma Specimen
Jianping Xu, Yue Pu, Rui Lin, Shanshan Xiao, Yingxue Fu, Tao Wang
Frontiers in Medicine.2022;[Epub] CrossRef - Potential applications of peptide nucleic acid in biomedical domain
Kshitij RB Singh, Parikipandla Sridevi, Ravindra Pratap Singh
Engineering Reports.2020;[Epub] CrossRef - A Highly Sensitive Next-Generation Sequencing-Based Genotyping Platform for EGFR Mutations in Plasma from Non-Small Cell Lung Cancer Patients
Jung-Young Shin, Jeong-Oh Kim, Mi-Ran Lee, Seo Ree Kim, Kyongmin Sarah Beck, Jin Hyoung Kang
Cancers.2020; 12(12): 3579. CrossRef - Association with PD-L1 Expression and Clinicopathological Features in 1000 Lung Cancers: A Large Single-Institution Study of Surgically Resected Lung Cancers with a High Prevalence of EGFR Mutation
Seung Eun Lee, Yu Jin Kim, Minjung Sung, Mi-Sook Lee, Joungho Han, Hong Kwan Kim, Yoon-La Choi
International Journal of Molecular Sciences.2019; 20(19): 4794. CrossRef - Peptide Nucleic Acid Clamping and Direct Sequencing in the Detection of Oncogenic Alterations in Lung Cancer: Systematic Review and Meta-Analysis
Jae-Uk Song, Jonghoo Lee
Yonsei Medical Journal.2018; 59(2): 211. CrossRef - Comparative analysis of Adam33 mutations in murine lung cancer cell lines by droplet digital PCR, real-time PCR and Insight Onco™ NGS
Soo-Jin Kim, Eunhee Kim, Kyung-Taek Rim
Molecular & Cellular Toxicology.2018; 14(2): 221. CrossRef - KRAS mutation analysis by next‐generation sequencing in endoscopic ultrasound‐guided sampling for solid liver masses
Hyun Jong Choi, Jong Ho Moon, Hee Kyung Kim, Yun Nah Lee, Tae Hoon Lee, Sang‐Woo Cha, Young Deok Cho, Sang‐Heum Park
Journal of Gastroenterology and Hepatology.2017; 32(1): 154. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - Peptide nucleic acids: Advanced tools for biomedical applications
Anjali Gupta, Anuradha Mishra, Nidhi Puri
Journal of Biotechnology.2017; 259: 148. CrossRef - Application of Peptide Nucleic Acid-based Assays Toward Detection of Somatic Mosaicism
Christopher S Hong, Chunzhang Yang, Zhengping Zhuang
Molecular Therapy - Nucleic Acids.2016; 5: e314. CrossRef - Detecting Primary KIT Mutations in Presurgical Plasma of Patients with Gastrointestinal Stromal Tumor
Guhyun Kang, Byeong Seok Sohn, Jung-Soo Pyo, Jung Yeon Kim, Boram Lee, Kyoung-Mee Kim
Molecular Diagnosis & Therapy.2016; 20(4): 347. CrossRef - Transformation to Small Cell Lung Cancer of Pulmonary Adenocarcinoma: Clinicopathologic Analysis of Six Cases
Soomin Ahn, Soo Hyun Hwang, Joungho Han, Yoon-La Choi, Se-Hoon Lee, Jin Seok Ahn, Keunchil Park, Myung-Ju Ahn, Woong-Yang Park
Journal of Pathology and Translational Medicine.2016; 50(4): 258. CrossRef - Clinicopathologic characteristics of EGFR, KRAS, and ALK alterations in 6,595 lung cancers
Boram Lee, Taebum Lee, Se-Hoon Lee, Yoon-La Choi, Joungho Han
Oncotarget.2016; 7(17): 23874. CrossRef - Detection of KIT and PDGFRA mutations in the plasma of patients with gastrointestinal stromal tumor
Guhyun Kang, Byung Noe Bae, Byeong Seok Sohn, Jung-Soo Pyo, Gu Hyum Kang, Kyoung-Mee Kim
Targeted Oncology.2015; 10(4): 597. CrossRef - Low Frequency of KRAS Mutation in Pancreatic Ductal Adenocarcinomas in Korean Patients and Its Prognostic Value
Mi Jung Kwon, Jang Yong Jeon, Hye-Rim Park, Eun Sook Nam, Seong Jin Cho, Hyung Sik Shin, Ji Hyun Kwon, Joo Seop Kim, Boram Han, Dong Hoon Kim, Yoon-La Choi
Pancreas.2015; 44(3): 484. CrossRef
- KRAS mutated Non‐Small Lung Carcinoma: A Real World Context from the Indian subcontinent
- Usual Interstitial Pneumonia with Lung Cancer: Clinicopathological Analysis of 43 Cases
- Dae Hyun Song, In Ho Choi, Sang Yun Ha, Kang Min Han, Jae Jun Lee, Min Eui Hong, Kyeongman Jeon, Man Pyo Chung, Jhingook Kim, Joungho Han
- Korean J Pathol. 2014;48(1):10-16. Published online February 25, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.1.10
- 11,268 View
- 79 Download
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Previous studies have suggested an association between usual interstitial pneumonia (UIP) and lung cancer (Ca). However, clinical and histological information is not enough to determine such an association, due to the low incidence and short survival time of patients with both conditions.
Methods We retrospectively reviewed the clinical and histological records of Ca patients with UIP between January 1999 and August 2013 at the Samsung Medical Center, Seoul, Korea. We found 43 patients who had Ca with UIP (UIP-Ca). Previously reported data of eighty-four patients with UIP-only were included as a comparison group.
Results Smoking is related to poor prognosis in patients with UIP-Ca, and the number of patients with a high smoking index of more than 30 pack-years significantly increased in UIP-Ca patients compared with UIP-only patients. There is no significant prognostic differentiation between UIP-Ca patients and UIP-only patients. Microscopically, UIP-Ca patients showed characteristically heterogeneous histological patterns and degrees of differentiation. There were many foci of squamous metaplasia or dysplasia at the peripheral area of squamous cell carcinomas.
Conclusions We report 43 cases of UIP-Ca. Our results suggest that smoking is related to cancer occurrence in UIP patients and poor prognosis in UIP-Ca patients.
-
Citations
Citations to this article as recorded by- Treatable traits in interstitial lung disease: a narrative review
Megan Harrison, Chloe Lawler, Fiona Lake, Vidya Navaratnam, Caitlin Fermoyle, Yuben Moodley, Tamera J. Corte
Therapeutic Advances in Respiratory Disease.2025;[Epub] CrossRef - Usual Interstitial Pneumonia and Lung Cancer
Lamiyae Senhaji, Meryem Karhate, Abir Bouhamdi, Mounia Serraj, Mohamed ElBiaze, Mohammed Chakib Benjelloun, Badreddine Alami, Bouchra Amara
Cureus.2025;[Epub] CrossRef - Prognosis of idiopathic pulmonary fibrosis without anti-fibrotic therapy: a systematic review
Yet H. Khor, Yvonne Ng, Hayley Barnes, Nicole S.L. Goh, Christine F. McDonald, Anne E. Holland
European Respiratory Review.2020; 29(157): 190158. CrossRef - Linfoma difuso de células B grandes pulmonar en paciente con neumonía intersticial no específica
Luis Gorospe Sarasúa, Paola Arrieta, Anabelle Chinea-Rodríguez, Carlos de la Puente-Bujidos
Reumatología Clínica.2019; 15(6): e151. CrossRef - Diffuse Large B-cell Lymphoma of the Lung in a Patient With Nonspecific Interstitial Pneumonia
Luis Gorospe Sarasúa, Paola Arrieta, Anabelle Chinea-Rodríguez, Carlos de la Puente-Bujidos
Reumatología Clínica (English Edition).2019; 15(6): e151. CrossRef - Characteristics of lung cancer among patients with idiopathic pulmonary fibrosis and interstitial lung disease – analysis of institutional and population data
Joo Heung Yoon, Mehdi Nouraie, Xiaoping Chen, Richard H Zou, Jacobo Sellares, Kristen L Veraldi, Jared Chiarchiaro, Kathleen Lindell, David O Wilson, Naftali Kaminski, Timothy Burns, Humberto Trejo Bittar, Samuel Yousem, Kevin Gibson, Daniel J Kass
Respiratory Research.2018;[Epub] CrossRef - Genomic profiles of lung cancer associated with idiopathic pulmonary fibrosis
Ji An Hwang, Deokhoon Kim, Sung‐Min Chun, SooHyun Bae, Joon Seon Song, Mi Young Kim, Hyun Jung Koo, Jin Woo Song, Woo Sung Kim, Jae Cheol Lee, Hyeong Ryul Kim, Chang‐Min Choi, Se Jin Jang
The Journal of Pathology.2018; 244(1): 25. CrossRef - Survival after repeated surgery for lung cancer with idiopathic pulmonary fibrosis: a retrospective study
Seijiro Sato, Yuki Shimizu, Tatsuya Goto, Akihiko Kitahara, Terumoto Koike, Hiroyuki Ishikawa, Takehiro Watanabe, Masanori Tsuchida
BMC Pulmonary Medicine.2018;[Epub] CrossRef - Alveolar Squamous Cell Metaplasia: Preneoplastic Lesion?
Adriana Handra-Luca
Journal of Pathology and Translational Medicine.2018; 52(6): 355. CrossRef - Low expression of long noncoding RNA CDKN2B-AS1 in patients with idiopathic pulmonary fibrosis predicts lung cancer by regulating the p53-signaling pathway
Yufeng Du, Xiaoyan Hao, Xuejun Liu
Oncology Letters.2018;[Epub] CrossRef - A clinicopathological study of surgically resected lung cancer in patients with usual interstitial pneumonia
Yasutaka Watanabe, Yoshinori Kawabata, Nobuyuki Koyama, Tomohiko Ikeya, Eishin Hoshi, Noboru Takayanagi, Shinichiro Koyama
Respiratory Medicine.2017; 129: 158. CrossRef - Risk of the preoperative underestimation of tumour size of lung cancer in patients with idiopathic interstitial pneumonias
Mariko Fukui, Kazuya Takamochi, Takeshi Matsunaga, Shiaki Oh, Katsutoshi Ando, Kazuhiro Suzuki, Atsushi Arakawa, Toshimasa Uekusa, Kenji Suzuki
European Journal of Cardio-Thoracic Surgery.2016; 50(3): 428. CrossRef - The Idiopathic Interstitial Pneumonias: Histology and Imaging
Diane C. Strollo, Teri J. Franks, Jeffrey R. Galvin
Seminars in Roentgenology.2015; 50(1): 8. CrossRef - Do Chest Expansion Exercises Aid Re‐shaping the Diaphragm Within the First 72 Hours Following Lung Transplantation in a Usual Interstitial Pneumonia Patient?
Massimiliano Polastri, Erika Venturini, Saverio Pastore, Andrea Dell'Amore
Physiotherapy Research International.2015; 20(3): 191. CrossRef - Scrotal wall metastasis from a primary lung adenocarcinoma
Marie-Louise M. Coussa-Koniski, Pia A. Maalouf, Nehme E. Raad, Noha A. Bejjani
Respiratory Medicine Case Reports.2015; 15: 77. CrossRef - The Ratio KL-6 to SLX in Serum for Prediction of the Occurrence of Drug-Induced Interstitial Lung Disease in Lung Cancer Patients with Idiopathic Interstitial Pneumonias Receiving Chemotherapy
Kosuke Kashiwabara, Hiroshi Semba, Shinji Fujii, Shinsuke Tsumura, Ryota Aoki
Cancer Investigation.2015; 33(10): 516. CrossRef - Idiopathic pulmonary fibrosis will increase the risk of lung cancer
Li Junyao, Yang Ming, Li Ping, Su Zhenzhong, Gao Peng, Zhang Jie
Chinese Medical Journal.2014; 127(17): 3142. CrossRef
- Treatable traits in interstitial lung disease: a narrative review
- Guideline Recommendations for Testing of
ALK Gene Rearrangement in Lung Cancer: A Proposal of the Korean Cardiopulmonary Pathology Study Group - Hyojin Kim, Hyo Sup Shim, Lucia Kim, Tae-Jung Kim, Kun Young Kwon, Geon Kook Lee, Jin-Haeng Chung
- Korean J Pathol. 2014;48(1):1-9. Published online February 25, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.1.1
- 16,410 View
- 131 Download
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF Rearrangement of anaplastic lymphoma kinase (
ALK ) gene is the best predictor of response to crizotinib, an ALK tyrosine kinase inhibitor. However, the prevalence of theALK fusion is low, so accurate patient identification is crucial for successful treatment using ALK inhibitors. Furthermore, most patients with lung cancer present with advanced-stage disease at the time of diagnosis, so it is important for pathologists to detectALK -rearranged patients while effectively maximizing small biopsy or cytology specimens. In this review, we propose a guideline recommendation for ALK testing approved by the Cardiopulmonary Pathology Study Group of the Korean Society of Pathologists.-
Citations
Citations to this article as recorded by- Molecular Characteristics of Radon Associated Lung Cancer Highlights MET Alterations
Gabriele Gamerith, Marcel Kloppenburg, Finn Mildner, Arno Amann, Sabine Merkelbach-Bruse, Carina Heydt, Janna Siemanowski, Reinhard Buettner, Michael Fiegl, Claudia Manzl, Georg Pall
Cancers.2022; 14(20): 5113. CrossRef -
ALK Translocation in ALK-Positive Mesenchymal Tumors: Diagnostic and Therapeutic Insights
Minsun Jung, Kyung Chul Moon, Jeongmo Bae, Tae Min Kim, Miso Kim, Yoon Kyung Jeon, Cheol Lee
Archives of Pathology & Laboratory Medicine.2022; 146(12): 1460. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Testing for EGFR Mutations and ALK Rearrangements in Advanced Non-Small-Cell Lung Cancer: Considerations for Countries in Emerging Markets
Mercedes L Dalurzo, Alejandro Avilés-Salas, Fernando Augusto Soares, Yingyong Hou, Yuan Li, Anna Stroganova, Büge Öz, Arif Abdillah, Hui Wan, Yoon-La Choi
OncoTargets and Therapy.2021; Volume 14: 4671. CrossRef - Molecular testing for advanced non-small cell lung cancer in Malaysia: Consensus statement from the College of Pathologists, Academy of Medicine Malaysia, the Malaysian Thoracic Society, and the Malaysian Oncological Society
Pathmanathan Rajadurai, Phaik Leng Cheah, Soon Hin How, Chong Kin Liam, Muhammad Azrif Ahmad Annuar, Norhayati Omar, Noriah Othman, Nurhayati Mohd Marzuki, Yong Kek Pang, Ros Suzanna Ahmad Bustamam, Lye Mun Tho
Lung Cancer.2019; 136: 65. CrossRef - Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors
Neal I. Lindeman, Philip T. Cagle, Dara L. Aisner, Maria E. Arcila, Mary Beth Beasley, Eric H. Bernicker, Carol Colasacco, Sanja Dacic, Fred R. Hirsch, Keith Kerr, David J. Kwiatkowski, Marc Ladanyi, Jan A. Nowak, Lynette Sholl, Robyn Temple-Smolkin, Benj
Journal of Thoracic Oncology.2018; 13(3): 323. CrossRef - Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors
Neal I. Lindeman, Philip T. Cagle, Dara L. Aisner, Maria E. Arcila, Mary Beth Beasley, Eric H. Bernicker, Carol Colasacco, Sanja Dacic, Fred R. Hirsch, Keith Kerr, David J. Kwiatkowski, Marc Ladanyi, Jan A. Nowak, Lynette Sholl, Robyn Temple-Smolkin, Benj
The Journal of Molecular Diagnostics.2018; 20(2): 129. CrossRef - Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors: Guideline From the College of American Pathologists, the International Association for the Study of Lung Cancer, and the
Neal I. Lindeman, Philip T. Cagle, Dara L. Aisner, Maria E. Arcila, Mary Beth Beasley, Eric H Bernicker, Carol Colasacco, Sanja Dacic, Fred R. Hirsch, Keith Kerr, David J. Kwiatkowski, Marc Ladanyi, Jan A. Nowak, Lynette Sholl, Robyn Temple-Smolkin, Benja
Archives of Pathology & Laboratory Medicine.2018; 142(3): 321. CrossRef - 5′/ 3′ imbalance strategy to detect ALK fusion genes in circulating tumor RNA from patients with non-small cell lung cancer
Yongqing Tong, Zhijun Zhao, Bei Liu, Anyu Bao, Hongyun Zheng, Jian Gu, Mary McGrath, Ying Xia, Bihua Tan, Chunhua Song, Yan Li
Journal of Experimental & Clinical Cancer Research.2018;[Epub] CrossRef - Molecular testing and treatment patterns for patients with advanced non-small cell lung cancer: PIvOTAL observational study
Dae Ho Lee, Ming-Sound Tsao, Karl-Otto Kambartel, Hiroshi Isobe, Ming-Shyan Huang, Carlos H. Barrios, Adnan Khattak, Filippo de Marinis, Smita Kothari, Ashwini Arunachalam, Xiting Cao, Thomas Burke, Amparo Valladares, Javier de Castro, Aamir Ahmad
PLOS ONE.2018; 13(8): e0202865. CrossRef - Microfluidics-based immunofluorescence for fast staining of ALK in lung adenocarcinoma
Saška Brajkovic, Benjamin Pelz, Maria-Giuseppina Procopio, Anne-Laure Leblond, Grégoire Repond, Ariane Schaub-Clerigué, Diego G Dupouy, Alex Soltermann
Diagnostic Pathology.2018;[Epub] CrossRef - Expanded Circulating Tumor Cells from a Patient with ALK- Positive Lung Cancer Present with EML4-ALK Rearrangement Along with Resistance Mutation and Enable Drug Sensitivity Testing: A Case Study
Zhuo Zhang, Hiroe Shiratsuchi, Nallasivam Palanisamy, Sunitha Nagrath, Nithya Ramnath
Journal of Thoracic Oncology.2017; 12(2): 397. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - Novel ALK fusion partners in lung cancer
Aglaya G. Iyevleva, Grigory A. Raskin, Vladislav I. Tiurin, Anna P. Sokolenko, Natalia V. Mitiushkina, Svetlana N. Aleksakhina, Aigul R. Garifullina, Tatiana N. Strelkova, Valery O. Merkulov, Alexandr O. Ivantsov, Ekatherina Sh. Kuligina, Kazimir M. Pozha
Cancer Letters.2015; 362(1): 116. CrossRef - Strategic management of transthoracic needle aspirates for histological subtyping and EGFR testing in patients with peripheral lung cancer: An institutional experience
Choonhee Son, Eun‐Ju Kang, Mee Sook Roh
Diagnostic Cytopathology.2015; 43(7): 532. CrossRef - Current and future molecular diagnostics in non-small-cell lung cancer
Chun Man Li, Wing Ying Chu, Di Lun Wong, Hin Fung Tsang, Nancy Bo Yin Tsui, Charles Ming Lok Chan, Vivian Wei Wen Xue, Parco Ming Fai Siu, Benjamin Yat Ming Yung, Lawrence Wing Chi Chan, Sze Chuen Cesar Wong
Expert Review of Molecular Diagnostics.2015; 15(8): 1061. CrossRef - Role of biopsy sampling for diagnosis of early and progressed hepatocellular carcinoma
Haeryoung Kim, Young Nyun Park
Best Practice & Research Clinical Gastroenterology.2014; 28(5): 813. CrossRef - Molecular Pathology of Lung Cancer: Current Status and Future Directions
Mee Sook Roh
Tuberculosis and Respiratory Diseases.2014; 77(2): 49. CrossRef - Epidermal growth factor receptor mutations and anaplastic lymphoma kinase rearrangements in lung cancer with nodular ground-glass opacity
Sung-Jun Ko, Yeon Joo Lee, Jong Sun Park, Young-Jae Cho, Ho Il Yoon, Jin-Haeng Chung, Tae Jung Kim, Kyung Won Lee, Kwhanmien Kim, Sanghoon Jheon, Hyojin Kim, Jae Ho Lee, Choon-Taek Lee
BMC Cancer.2014;[Epub] CrossRef
- Molecular Characteristics of Radon Associated Lung Cancer Highlights MET Alterations
- Comparison of Direct Sequencing, PNA Clamping-Real Time Polymerase Chain Reaction, and Pyrosequencing Methods for the Detection of
EGFR Mutations in Non-small Cell Lung Carcinoma and the Correlation with Clinical Responses to EGFR Tyrosin - Hyun Ju Lee, Xianhua Xu, Hyojin Kim, Yan Jin, Pingli Sun, Ji Eun Kim, Jin-Haeng Chung
- Korean J Pathol. 2013;47(1):52-60. Published online February 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.1.52
- 12,918 View
- 93 Download
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The aims of this study were to evaluate the abilities of direct sequencing (DS), peptide nucleic acid (PNA) clamping, and pyrosequencing methods to detect epidermal growth factor receptor (
EGFR ) mutations in formalin-fixed paraffin-embedded (FFPE) non-small cell lung carcinoma (NSCLC) samples and to correlateEGFR mutational status as determined by each method with the clinical response toEGFR tyrosine kinase inhibitors (TKIs).Methods Sixty-one NSCLC patients treated with EGFR TKIs were identified to investigate somatic mutations in the
EGFR gene (exons 18-21).Results Mutations in the
EGFR gene were detected in 38 of the 61 patients (62%) by DS, 35 (57%) by PNA clamping and 37 (61%) by pyrosequencing. A total of 44 mutations (72%) were found by at least one of the three methods, and the concordances among the results were relatively high (82-85%; kappa coefficient, 0.713 to 0.736). There were 15 discordant cases (25%) among the three different methods.Conclusions All three
EGFR mutation tests had good concordance rates (over 82%) for FFPE samples. These results suggest that if the DNA quality and enrichment of tumor cells are assured, then DS, PNA clamping, and pyrosequencing are appropriate methods for the detection ofEGFR mutations.-
Citations
Citations to this article as recorded by- Recent Trends of Lung Cancer in Korea
Jae Guk Lee, Ho Cheol Kim, Chang-Min Choi
Tuberculosis and Respiratory Diseases.2021; 84(2): 89. CrossRef - Predictive value of KRAS mutation and excision repair cross-complementing 1 (ERCC1) protein overexpression in patients with colorectal cancer administered FOLFOX regimen
Sun Min Park, Sung Bong Choi, Yoon Suk Lee, In Kyu Lee
Asian Journal of Surgery.2021; 44(5): 715. CrossRef - Recent advances in diagnostic technologies in lung cancer
Hye Jung Park, Sang Hoon Lee, Yoon Soo Chang
The Korean Journal of Internal Medicine.2020; 35(2): 257. CrossRef - Afatinib is effective in the treatment of lung adenocarcinoma with uncommon EGFR p.L747P and p.L747S mutations
Sheng-Kai Liang, Jen-Chung Ko, James Chih-Hsin Yang, Jin-Yuan Shih
Lung Cancer.2019; 133: 103. CrossRef - Biomarker Testing for Patients With Advanced Non–Small Cell Lung Cancer: Real-World Issues and Tough Choices
Nathan A. Pennell, Maria E. Arcila, David R. Gandara, Howard West
American Society of Clinical Oncology Educational Book.2019; (39): 531. CrossRef - Evaluation of EGFR mutations in NSCLC with highly sensitive droplet digital PCR assays
Xi‑Wen Jiang, Wei Liu, Xiao‑Ya Zhu, Xiao‑Xie Xu
Molecular Medicine Reports.2019;[Epub] CrossRef - Peptide Nucleic Acid Clamping and Direct Sequencing in the Detection of Oncogenic Alterations in Lung Cancer: Systematic Review and Meta-Analysis
Jae-Uk Song, Jonghoo Lee
Yonsei Medical Journal.2018; 59(2): 211. CrossRef - Distribution of KRAS, DDR2, and TP53 gene mutations in lung cancer: An analysis of Iranian patients
Zahra Fathi, Seyed Ali Javad Mousavi, Raheleh Roudi, Farideh Ghazi, Sumitra Deb
PLOS ONE.2018; 13(7): e0200633. CrossRef - EGFR T790M mutation testing within the osimertinib AURA Phase I study
Simon Dearden, Helen Brown, Suzanne Jenkins, Kenneth S. Thress, Mireille Cantarini, Rebecca Cole, Malcolm Ranson, Pasi A. Jänne
Lung Cancer.2017; 109: 9. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - Mutations of the Epidermal Growth Factor Receptor Gene in Triple-Negative Breast Cancer
Aeri Kim, Min Hye Jang, Soo Jung Lee, Young Kyung Bae
Journal of Breast Cancer.2017; 20(2): 150. CrossRef - Double primary lung adenocarcinoma diagnosed by epidermal growth factor receptor mutation status
Oh Jung Kwon, Min Hyeok Lee, Sung Ju Kang, Seul Gi Kim, In Beom Jeong, Ji Yun Jeong, Eun Jung Cha, Do Yeun Cho, Young Jin Kim, Ji Woong Son
Yeungnam University Journal of Medicine.2017; 34(2): 270. CrossRef - Generation of lung cancer cell lines harboring EGFR T790M mutation by CRISPR/Cas9-mediated genome editing
Mi-Young Park, Min Hee Jung, Eun Young Eo, Seokjoong Kim, Sang Hoon Lee, Yeon Joo Lee, Jong Sun Park, Young Jae Cho, Jin Haeng Chung, Cheol Hyeon Kim, Ho Il Yoon, Jae Ho Lee, Choon-Taek Lee
Oncotarget.2017; 8(22): 36331. CrossRef - Comparison of EGFR mutation detection between the tissue and cytology using direct sequencing, pyrosequencing and peptide nucleic acid clamping in lung adenocarcinoma: Korean multicentre study
Kyueng-Whan Min, Wan-Seop Kim, Se Jin Jang, Yoo Duk Choi, Sunhee Chang, Soon Hee Jung, Lucia Kim, Mee Sook Roh, Choong Sik Lee, Jung Weon Shim, Mi Jin Kim, Geon Kook Lee
QJM.2016; 109(3): 167. CrossRef - Epidermal Growth Factor Receptor Mutation and Anaplastic Lymphoma Kinase Gene Fusion: Detection in Malignant Pleural Effusion by RNA or PNA Analysis
Yi-Lin Chen, Chung-Ta Lee, Cheng-Chan Lu, Shu-Ching Yang, Wan-Li Chen, Yang-Cheng Lee, Chung-Hsien Yang, Shu-Ling Peng, Wu-Chou Su, Nan-Haw Chow, Chung-Liang Ho, Javier S Castresana
PLOS ONE.2016; 11(6): e0158125. CrossRef - IDH Mutation Analysis in Ewing Sarcoma Family Tumors
Ki Yong Na, Byeong-Joo Noh, Ji-Youn Sung, Youn Wha Kim, Eduardo Santini Araujo, Yong-Koo Park
Journal of Pathology and Translational Medicine.2015; 49(3): 257. CrossRef - Immunohistochemical demonstration of alteration of β-catenin during tumor metastasis by different mechanisms according to histology in lung cancer
XIANHUA XU, JI EUN KIM, PING-LI SUN, SEOL BONG YOO, HYOJIN KIM, YAN JIN, JIN-HAENG CHUNG
Experimental and Therapeutic Medicine.2015; 9(2): 311. CrossRef - Detection of EGFR-TK Domain–activating Mutations in NSCLC With Generic PCR-based Methods
Rajendra B. Shahi, Sylvia De Brakeleer, Jacques De Grève, Caroline Geers, Peter In’t Veld, Erik Teugels
Applied Immunohistochemistry & Molecular Morphology.2015; 23(3): 163. CrossRef - Frequent aerogenous spread with decreased E-cadherin expression of ROS1- rearranged lung cancer predicts poor disease-free survival
Yan Jin, Ping-Li Sun, Soo Young Park, Hyojin Kim, Eunhyang Park, Gilhyang Kim, Sukki Cho, Kwhanmien Kim, Choon-Taek Lee, Jin-Haeng Chung
Lung Cancer.2015; 89(3): 343. CrossRef - Membranous Insulin-like Growth Factor-1 Receptor (IGF1R) Expression Is Predictive of Poor Prognosis in Patients with Epidermal Growth Factor Receptor (EGFR)-Mutant Lung Adenocarcinoma
Eunhyang Park, Soo Young Park, Hyojin Kim, Ping-Li Sun, Yan Jin, Suk Ki Cho, Kwhanmien Kim, Choon-Taek Lee, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2015; 49(5): 382. CrossRef - Peptide Nucleic Acid Clamping Versus Direct Sequencing for the Detection of EGFR Gene Mutation in Patients with Non-small Cell Lung Cancer
Seong-Hoon Yoon, Yoo-Duk Choi, In-Jae Oh, Kyu-Sik Kim, Hayoung Choi, Jinsun Chang, Hong-Joon Shin, Cheol-Kyu Park, Young-Chul Kim
Cancer Research and Treatment.2015; 47(4): 661. CrossRef - Analysis of Mutations in Epidermal Growth Factor Receptor Gene in Korean Patients with Non-small Cell Lung Cancer: Summary of a Nationwide Survey
Sang Hwa Lee, Wan Seop Kim, Yoo Duk Choi, Jeong Wook Seo, Joung Ho Han, Mi Jin Kim, Lucia Kim, Geon Kook Lee, Chang Hun Lee, Mee Hye Oh, Gou Young Kim, Sun Hee Sung, Kyo Young Lee, Sun Hee Chang, Mee Sook Rho, Han Kyeom Kim, Soon Hee Jung, Se Jin Jang
Journal of Pathology and Translational Medicine.2015; 49(6): 481. CrossRef - Novel EGFR mutation-specific antibodies for lung adenocarcinoma: Highly specific but not sensitive detection of an E746_A750 deletion in exon 19 and an L858R mutation in exon 21 by immunohistochemistry
An Na Seo, Tae-In Park, Yan Jin, Ping-Li Sun, Hyojin Kim, Hyun Chang, Jin-Haeng Chung
Lung Cancer.2014; 83(3): 316. CrossRef - Simultaneous diagnostic platform of genotyping EGFR, KRAS, and ALK in 510 Korean patients with non‐small‐cell lung cancer highlights significantly higher ALK rearrangement rate in advanced stage
Tae‐Jung Kim, Chan Kwon Park, Chang Dong Yeo, Kihoon Park, Chin Kook Rhee, Jusang Kim, Seung Joon Kim, Sang Haak Lee, Kyo‐Young Lee, Hyoung‐Kyu Yoon
Journal of Surgical Oncology.2014; 110(3): 245. CrossRef - Epidermal growth factor receptor mutations and anaplastic lymphoma kinase rearrangements in lung cancer with nodular ground-glass opacity
Sung-Jun Ko, Yeon Joo Lee, Jong Sun Park, Young-Jae Cho, Ho Il Yoon, Jin-Haeng Chung, Tae Jung Kim, Kyung Won Lee, Kwhanmien Kim, Sanghoon Jheon, Hyojin Kim, Jae Ho Lee, Choon-Taek Lee
BMC Cancer.2014;[Epub] CrossRef - Cytoplasmic YAP Expression is Associated with Prolonged Survival in Patients with Lung Adenocarcinomas and Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor Treatment
Ping-Li Sun, Ji Eun Kim, Seol Bong Yoo, Hyojin Kim, Yan Jin, Sanghoon Jheon, Kwhanmien Kim, Choon Taek Lee, Jin-Haeng Chung
Annals of Surgical Oncology.2014; 21(S4): 610. CrossRef - Sensitive methods for detection of the S768R substitution in exon 18 of the DDR2 gene in patients with central nervous system metastases of non-small cell lung cancer
Marcin Nicoś, Tomasz Powrózek, Paweł Krawczyk, Bożena Jarosz, Beata Pająk, Marek Sawicki, Krzysztof Kucharczyk, Tomasz Trojanowski, Janusz Milanowski
Medical Oncology.2014;[Epub] CrossRef - Clinicopathologic and prognostic significance of c-MYC copy number gain in lung adenocarcinomas
A N Seo, J M Yang, H Kim, S Jheon, K Kim, C T Lee, Y Jin, S Yun, J-H Chung, J H Paik
British Journal of Cancer.2014; 110(11): 2688. CrossRef - KRASMutation Detection in Non-small Cell Lung Cancer Using a Peptide Nucleic Acid-Mediated Polymerase Chain Reaction Clamping Method and Comparative Validation with Next-Generation Sequencing
Boram Lee, Boin Lee, Gangmin Han, Mi Jung Kwon, Joungho Han, Yoon-La Choi
Korean Journal of Pathology.2014; 48(2): 100. CrossRef - Guideline Recommendations forEGFRMutation Testing in Lung Cancer: Proposal of the Korean Cardiopulmonary Pathology Study Group
Hyo Sup Shim, Jin-Haeng Chung, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Geon Kook Lee, Soon-Hee Jung, Se Jin Jang
Korean Journal of Pathology.2013; 47(2): 100. CrossRef - Immunohistochemical Classification of Primary and Secondary Glioblastomas
Kyu Sang Lee, Gheeyoung Choe, Kyung Han Nam, An Na Seo, Sumi Yun, Kyung Ju Kim, Hwa Jin Cho, Sung Hye Park
Korean Journal of Pathology.2013; 47(6): 541. CrossRef
- Recent Trends of Lung Cancer in Korea
- Alteration of the E-Cadherin/β-Catenin Complex Is an Independent Poor Prognostic Factor in Lung Adenocarcinoma
- Hyojin Kim, Seol Bong Yoo, Pingli Sun, Yan Jin, Sanghoon Jheon, Choon Taek Lee, Jin-Haeng Chung
- Korean J Pathol. 2013;47(1):44-51. Published online February 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.1.44
- 12,161 View
- 63 Download
- 36 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Epithelial-mesenchymal transition (EMT) is an important step in the invasion and progression of cancer and in the development of chemoresistance by cancer cells.
Methods To address the clinical significance of the EMT pathway in lung adenocarcinoma and the association of the pathway with histological subtype, we examined 193 surgically resected lung adenocarcinoma samples for the expression of representative EMT-related proteins (E-cadherin, β-catenin, and vimentin) by immunohistochemistry. Histological subtypes were classified according to the 2011 International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification. The results for EMT-related protein expression were analyzed for correlation with clinicopathological features and with survival.
Results The loss of E-cadherin expression and aberrant β-catenin expression were significantly associated with larger tumor size, pleural invasion, lymphatic/vascular invasion, and advanced pathological stage (p<0.05). The alteration of the E-cadherin/β-catenin complex was least frequently observed in the lepidic-predominant group, but these associations were not statistically significant. In the multivariate analysis, altered E-cadherin/β-catenin complex expression was found to be an independent poor prognostic factor (p=0.017; hazard ratio, 1.926; 95% confidence interval, 1.119 to 3.314).
Conclusions The alteration of the expression of the E-cadherin/β-catenin complex was associated with aggressive tumor behavior in lung adenocarcinoma.
-
Citations
Citations to this article as recorded by- Prognostic significance of stem cell-related marker expression and its correlation with histologic subtypes in lung adenocarcinoma
Eunhyang Park, Soo Young Park, Ping-Li Sun, Yan Jin, Ji Eun Kim, Sanghoon Jheon, Kwhanmien Kim, Choon Taek Lee, Hyojin Kim, Jin-Haeng Chung
Oncotarget.2106; 7(27): 42502. CrossRef - E-cadherin–Driven Adherens Junction Reinforcement Promotes Spheroid-Mediated Invasion and Progression In ALK-Rearranged Lung Cancer Chemoresistance
Dawon Hong, Hyun Jung Kwon, Jiwon Jeong, Seokhyun Yoon, Jin-Haeng Chung, Sunjoo Jeong
Molecules and Cells.2026; : 100329. CrossRef - Epigenetic Alterations of DNA Methylation and miRNA Contribution to Lung Adenocarcinoma
Wenhan Cai, Miao Jing, Jiaxin Wen, Hua Guo, Zhiqiang Xue
Frontiers in Genetics.2022;[Epub] CrossRef - Clinicopathological significance and prognostic value of E-cadherin expression in non-small cell lung cancer
Dong Chao, Gawei Hu, Qingxin Li
Medicine.2021; 100(7): e24748. CrossRef - Aberrant Expression of β-Catenin Correlates with Infiltrating Immune Cells and Prognosis in NSCLC
Hongmei Zheng, Yue Ning, Yang Yang, Yuting Zhan, Haihua Wang, Qiuyuan Wen, Jinwu Peng, Songqing Fan
Pathology and Oncology Research.2021;[Epub] CrossRef - Prognostic Significance of Wnt1, Wnt2, E-Cadherin, and β-catenin Expression in Operable Non-small Cell Lung Cancer
Anna Wrona, Aleksandra Sejda, Rafał Dziadziuszko, Jacek Jassem
Journal of Histochemistry & Cytochemistry.2021; 69(11): 711. CrossRef - Analysis of genes associated with prognosis of lung adenocarcinoma based on GEO and TCGA databases
Ye Yu, Xuemei Tian
Medicine.2020; 99(19): e20183. CrossRef - The roles of TG-interacting factor in cadmium exposure-promoted invasion and migration of lung cancer cells
Yadong Wang, Li Shi, Jiangmin Li, Haiyu Wang, Haiyan Yang
Toxicology in Vitro.2019; 61: 104630. CrossRef - Pizotifen inhibits the proliferation and invasion of gastric cancer cells
Ying Jiang, Wei Wang, Xi Wu, Jihua Shi
Experimental and Therapeutic Medicine.2019;[Epub] CrossRef - SNAI2 and TWIST1 in lymph node progression in early stages of NSCLC patients
Camille Emprou, Pauline Le Van Quyen, Jérémie Jégu, Nathalie Prim, Noëlle Weingertner, Eric Guérin, Erwan Pencreach, Michèle Legrain, Anne‐Claire Voegeli, Charlotte Leduc, Bertrand Mennecier, Pierre‐Emmanuel Falcoz, Anne Olland, Nicolas Santelmo, Elisabet
Cancer Medicine.2018; 7(7): 3278. CrossRef - E-Cadherin Loss Accelerates Tumor Progression and Metastasis in a Mouse Model of Lung Adenocarcinoma
Kerstin W. Sinkevicius, Kelly J. Bellaria, Juliana Barrios, Patrizia Pessina, Manav Gupta, Christine Fillmore Brainson, Roderick T. Bronson, Carla F. Kim
American Journal of Respiratory Cell and Molecular Biology.2018; 59(2): 237. CrossRef - Downregulation of peroxiredoxin II suppresses the proliferation and metastasis of gastric cancer cells
Linjun Niu, Ang Liu, Wei Xu, Liang Yang, Wugang Zhu, Yuming Gu
Oncology Letters.2018;[Epub] CrossRef - Implications of NOVA1 suppression within the microenvironment of gastric cancer: association with immune cell dysregulation
Eun Kyung Kim, Sun Och Yoon, Woon Yong Jung, Hyunjoo Lee, Youngran Kang, You-Jin Jang, Soon Won Hong, Seung Ho Choi, Woo Ick Yang
Gastric Cancer.2017; 20(3): 438. CrossRef - High FDG uptake on PET is associated with negative cell-to-cell adhesion molecule E-cadherin expression in lung adenocarcinoma
Kotaro Higashi, Yoshimichi Ueda, Miyako Shimasaki, Yasuhito Ishigaki, Yuka Nakamura, Manabu Oguchi, Tsutomu Takegami, Naoto Watanabe
Annals of Nuclear Medicine.2017; 31(8): 590. CrossRef - MicroRNA expression profiles and clinicopathological implications in lung adenocarcinoma according to EGFR, KRAS, and ALK status
Hyojin Kim, Jeong Mi Yang, Yan Jin, Sanghoon Jheon, Kwhanmien Kim, Choon Taek Lee, Jin-Haeng Chung, Jin Ho Paik
Oncotarget.2017; 8(5): 8484. CrossRef - A meta-analysis of abnormal β-catenin immunohistochemical expression as a prognostic factor in lung cancer: location is more important
Y. Yang, J. Shen, Jiaxi He, Jianxing He, G. Jiang
Clinical and Translational Oncology.2016; 18(7): 685. CrossRef - Aquaporin 1 Is an Independent Marker of Poor Prognosis in Lung Adenocarcinoma
Sumi Yun, Ping-Li Sun, Yan Jin, Hyojin Kim, Eunhyang Park, Soo Young Park, Kyuho Lee, Kyoungyul Lee, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2016; 50(4): 251. CrossRef - Prognostic Values of Vimentin Expression and Its Clinicopathological Significance in Non-Small Cell Lung Cancer: A Meta-Analysis of Observational Studies with 4118 Cases
Zhihua Ye, Xin Zhang, Yihuan Luo, Shikang Li, Lanshan Huang, Zuyun Li, Ping Li, Gang Chen, Aamir Ahmad
PLOS ONE.2016; 11(9): e0163162. CrossRef - Myoferlin expression in non-small cell lung cancer: Prognostic role and correlation with VEGFR-2 expression
DAE HYUN SONG, GYUNG HYUCK KO, JEONG HEE LEE, JONG SIL LEE, GYEONG-WON LEE, HYEON CHEOL KIM, JUNG WOOK YANG, ROK WON HEO, GU SEOB ROH, SUN-YOUNG HAN, DONG CHUL KIM
Oncology Letters.2016; 11(2): 998. CrossRef - Short hairpin RNA silencing of TGF-βRII and FZD-7 synergistically suppresses proliferation and metastasis of hepatocellular carcinoma cells
CONG CHEN, YUYANG XUE, DEJUN ZHANG, WEI XU, HAO XU, HONG YAO, DONGSHENG PEI, YUMING GU
Oncology Letters.2016; 11(3): 2039. CrossRef - NOVA1 inhibition by miR-146b-5p in the remnant tissue microenvironment defines occult residual disease after gastric cancer removal
Sun Och Yoon, Eun Kyung Kim, Mira Lee, Woon Yong Jung, Hyunjoo Lee, Youngran Kang, You-Jin Jang, Soon Won Hong, Seung Ho Choi, Woo Ick Yang
Oncotarget.2016; 7(3): 2475. CrossRef - Immunohistochemical demonstration of alteration of β-catenin during tumor metastasis by different mechanisms according to histology in lung cancer
XIANHUA XU, JI EUN KIM, PING-LI SUN, SEOL BONG YOO, HYOJIN KIM, YAN JIN, JIN-HAENG CHUNG
Experimental and Therapeutic Medicine.2015; 9(2): 311. CrossRef - FRK Inhibits Migration and Invasion of Human Glioma Cells by Promoting N-cadherin/β-catenin Complex Formation
Qiong Shi, Xu Song, Jun Wang, Jia Gu, Weijian Zhang, Jinxia Hu, Xiuping Zhou, Rutong Yu
Journal of Molecular Neuroscience.2015; 55(1): 32. CrossRef - Dissociation of E-cadherin/β-catenin complex by MG132 and bortezomib enhances CDDP induced cell death in oral cancer SCC-25 cells
Lanhai Lü, Xiqiang Liu, Cheng Wang, Fengchun Hu, Jianning Wang, Hongzhang Huang
Toxicology in Vitro.2015; 29(8): 1965. CrossRef - Epigallocatechin-3-gallate inhibits nicotine-induced migration and invasion by the suppression of angiogenesis and epithelial-mesenchymal transition in non-small cell lung cancer cells
JINGLI SHI, FEI LIU, WENZHANG ZHANG, XIN LIU, BIHUA LIN, XUDONG TANG
Oncology Reports.2015; 33(6): 2972. CrossRef - Clinicopathologic and prognostic significance of c-MYC copy number gain in lung adenocarcinomas
A N Seo, J M Yang, H Kim, S Jheon, K Kim, C T Lee, Y Jin, S Yun, J-H Chung, J H Paik
British Journal of Cancer.2014; 110(11): 2688. CrossRef - The Clinicopathological Significance of Epithelial Mesenchymal Transition Associated Protein Expression in Head and Neck Squamous Cell Carcinoma
Kyu Ho Kim, Lucia Kim, Suk Jin Choi, Jee Young Han, Joon Mee Kim, Young Chae Chu, Young-Mo Kim, In Suh Park, Joo Han Lim
Korean Journal of Pathology.2014; 48(4): 263. CrossRef - Adenoid dysplasia of the oral mucosa
Belinda Bunn, Keith Hunter, Syed Ali Khurram, W.F.P. van Heerden
Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2014; 118(5): 586. CrossRef - FGFR1 amplification is associated with poor prognosis and smoking in non-small-cell lung cancer
An Na Seo, Yan Jin, Hee Jin Lee, Ping-Li Sun, Hyojin Kim, Sanghoon Jheon, Kwhanmien Kim, Choon-Taek Lee, Jin-Haeng Chung
Virchows Archiv.2014; 465(5): 547. CrossRef - FNC, a Novel Nucleoside Analogue, Blocks Invasion of Aggressive Non-Hodgkin Lymphoma Cell Lines Via Inhibition of the Wnt/β-Catenin Signaling Pathway
Yan Zhang, Chen-Ping Wang, Xi-Xi Ding, Ning Wang, Fang Ma, Jin-Hua Jiang, Qing-Duan Wang, Jun-Biao Chang
Asian Pacific Journal of Cancer Prevention.2014; 15(16): 6829. CrossRef - β-Catenin overexpression is associated with gefitinib resistance in non-small cell lung cancer cells
Xia Fang, Pan Gu, Caicun Zhou, Aibin Liang, Shenxiang Ren, Fang Liu, Yu Zeng, Yunjin Wu, Yinmin Zhao, Binbin Huang, Zongmei Zhang, Xianghua Yi
Pulmonary Pharmacology & Therapeutics.2014; 28(1): 41. CrossRef - Tumor‐size‐based morphological features of metastatic lymph node tumors from primary lung adenocarcinoma
Eiji Yamada, Genichiro Ishii, Nao Aramaki, Keiju Aokage, Tomoyuki Hishida, Junji Yoshida, Motohiro Kojima, Kanji Nagai, Atsushi Ochiai
Pathology International.2014; 64(12): 591. CrossRef - Prognostic and Clinicopathological Significance of Downregulated E-Cadherin Expression in Patients with Non-Small Cell Lung Cancer (NSCLC): A Meta-Analysis
Yan-Long Yang, Ming-Wu Chen, Lei Xian, Alfons Navarro
PLoS ONE.2014; 9(6): e99763. CrossRef - Hepatic Stellate Cells Secreted Hepatocyte Growth Factor Contributes to the Chemoresistance of Hepatocellular Carcinoma
Guofeng Yu, Yingying Jing, Xingrui Kou, Fei Ye, Lu Gao, Qingmin Fan, Yang Yang, Qiudong Zhao, Rong Li, Mengchao Wu, Lixin Wei, Xin-Yuan Guan
PLoS ONE.2013; 8(9): e73312. CrossRef - A Comprehensive Comparative Analysis of the Histomorphological Features of ALK-Rearranged Lung Adenocarcinoma Based on Driver Oncogene Mutations: Frequent Expression of Epithelial-Mesenchymal Transition Markers than Other Genotype
Hyojin Kim, Se Jin Jang, Doo Hyun Chung, Seol Bong Yoo, Pingli Sun, Yan Jin, Kyung Han Nam, Jin-Ho Paik, Jin-Haeng Chung, Alfredo Fusco
PLoS ONE.2013; 8(10): e76999. CrossRef - Non-small cell lung cancer cells survived ionizing radiation treatment display cancer stem cell and epithelial-mesenchymal transition phenotypes
Roberto Gomez-Casal, Chitralekha Bhattacharya, Nandita Ganesh, Lisa Bailey, Per Basse, Michael Gibson, Michael Epperly, Vera Levina
Molecular Cancer.2013;[Epub] CrossRef
- Prognostic significance of stem cell-related marker expression and its correlation with histologic subtypes in lung adenocarcinoma
- Diffuse Pulmonary Meningotheliomatosis: A Case Report.
- Jungsuk An, Heejung Park, Joungho Han, Tae Sung Kim, Yong Soo Choi, Moon Seok Choi, Sang Won Um
- Korean J Pathol. 2011;45:S32-S35.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.S1.S32
- 5,238 View
- 43 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Diffuse pulmonary meningotheliomatosis (DPM) is an extremely rare condition. We herein report a unique case of DPM in a 54-year-old woman with a previous history of hepatocellular carcinoma. A chest computed tomography showed diffuse bilateral nodular infiltration, suggesting miliary spread of metastatic hepatocellular carcinoma. The patient underwent a video-assisted thoracoscopic surgery for diagnostic purposes. The cut surface of the lung specimen showed multiple dispersed small nodules, consisting of variably sized nests or whorls of bland epithelioid cells often along the walls of alveolar septa or in a perivascular network within the alveolar interstitium. The tumor cells showed immunoreactivity for epithelial membrane antigen, vimentin, and progesterone receptor. DPM should be included in the differential diagnosis of diffuse multiple small nodules or a reticular pattern in the radiologic studies.
-
Citations
Citations to this article as recorded by- Minute Pulmonary Meningothelial-Like Nodules Simulating Hematogenous Lung Metastasis: A Case Report
Sang Kook Lee, Gi Jeong Kim, Young Jae Kim, Ah Young Leem, Eu Dong Hwang, Se Kyu Kim, Joon Chang, Young Ae Kang, Song Yee Kim
Tuberculosis and Respiratory Diseases.2013; 75(2): 67. CrossRef
- Minute Pulmonary Meningothelial-Like Nodules Simulating Hematogenous Lung Metastasis: A Case Report
- Mucoepidermoid Carcinoma of Tracheobronchial Tree: Clinicopathological Study of 31 Cases.
- Sang Yun Ha, Joungho Han, Jae Jun Lee, Young Eun Kim, Yoon La Choi, Hong Kwan Kim
- Korean J Pathol. 2011;45(2):175-181.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.2.175
- 5,271 View
- 33 Download
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
All aspects of mucoepidermoid carcinoma (MEC) of the lung including histologic grading, clinical behavior and its differentiation from adenosquamous cell carcinoma are still not fully understood.
METHODS
We reviewed the hematoxylin-eosin stained slides and medical records of 31 cases of MEC of the lungs. The cases were classified as low and high grade according to the quantitative grading system formulated for MEC. High grade tumors were tested for an epidermal growth factor receptor (EGFR) mutation.
RESULTS
Twenty eight cases were classified as low grade and 3 cases as high grade. Histologically, lower glandular component, cellular atypia, necrosis, mitoses >4/10 high power fields, and endolymphatic tumor emboli were typical characteristics of a high grade tumor. Although some tumors showed histologic features mimicking high grade tumors, they were classified as low grade tumors according to this quantitative grading system. Low grade tumors showed no recurrence or metastasis. However, among three patients with a high grade tumor, two had distant metastases and one died of disease. Additionally, an EGFR mutation was not detected.
CONCLUSIONS
A high grade MEC was consistently different from a low grade tumor with regard to malignant histologic features and poor prognosis. Therefore, correct histologic grading is important in predicting the prognosis to avoid unnecessary treatment. -
Citations
Citations to this article as recorded by- A rare case of endobronchial mucoepidermoid carcinoma of the lung presenting as non-resolving pneumonia
Toolsie Omesh, Ranjan Gupta, Anjali Saqi, Joshua Burack, Misbahuddin Khaja
Respiratory Medicine Case Reports.2018; 25: 154. CrossRef - Cutaneous Involvement by Nasal Mucoepidermoid Carcinoma: The Tip of the Iceberg Phenomenon
Ge Zhao, Oliver Chang, John Streidl, Amit Bhrany, Kyle Garton, Timothy H. McCalmont, Paul E. Swanson, Zsolt Argenyi, Michi M. Shinohara
Journal of Cutaneous Pathology.2017; 44(2): 113. CrossRef - Surgical outcomes of pulmonary mucoepidermoid carcinoma: A review of 41 cases
Chih-Cheng Hsieh, Yung-Han Sun, Shih-Wei Lin, Yi-Chen Yeh, Mei-Lin Chan, Pei-Yi Chu
PLOS ONE.2017; 12(5): e0176918. CrossRef - Clinicopathologic characteristics of EGFR, KRAS, and ALK alterations in 6,595 lung cancers
Boram Lee, Taebum Lee, Se-Hoon Lee, Yoon-La Choi, Joungho Han
Oncotarget.2016; 7(17): 23874. CrossRef - Metastatic Pulmonary Mucoepidermoid Carcinoma with Fulminant Clinical Course
Yong Won Park, Seon Bin Yoon, Mi Ju Cheon, Young Min Koh, Hyeon Sik Oh, Se Joong Kim, Seung Hyeun Lee
The Ewha Medical Journal.2015; 38(2): 85. CrossRef - Lung cancer in never-smoker Asian females is driven by oncogenic mutations, most often involving EGFR
Sang Yun Ha, So-Jung Choi, Jong Ho Cho, Hye Joo Choi, Jinseon Lee, Kyungsoo Jung, Darry Irwin, Xiao Liu, Maruja E. Lira, Mao Mao, Hong Kwan Kim, Yong Soo Choi, Young Mog Shim, Woong Yang Park, Yoon-La Choi, Jhingook Kim
Oncotarget.2015; 6(7): 5465. CrossRef - Bronchoscopic Resection of an Exophytic Endoluminal Tracheal Mass
Russell J. Miller, Septimiu D. Murgu
Annals of the American Thoracic Society.2013; 10(6): 697. CrossRef - EGFR mutations and mucoepidermoid carcinoma: Putative significance in differing populations
Iain D. O’Neill
Lung Cancer.2012; 78(1): 125. CrossRef
- A rare case of endobronchial mucoepidermoid carcinoma of the lung presenting as non-resolving pneumonia
- The Fine Needle Aspiration Cytology of a Metastatic Pulmonary Adrenocortical Carcinoma Mimicking Primary Large Cell Carcinoma of the Lung.
- Na Rae Kim, Dong Hae Chung, Jae Ik Lee, Seung Yeon Ha
- Korean J Pathol. 2010;44(5):558-563.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.5.558
- 3,332 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Adrenocortical carcinoma is a rare neoplasm and it has an invariably lethal prognosis. We report here on the fine needle aspiration cytologic findings of a solitary metastatic pulmonary adrenocortical carcinoma in a 24-year-old woman. The aspirate smears were very cellular and they were composed of a monomorphic population of large polyhedral cells with abundant granular or vacuolated cytoplasm, and the cells were predominantly singly scattered in a necrotic background. Multinucleated pleomorphic tumor cells were also found. Pleomorphic nuclei with thickened nuclear membranes were impinging on the cell membranes. Mitotic activity was occasionally seen. The cytologic findings of pleomorphic cells with microvacuolated cytoplasm and the presence of vague gland-like sheets, as well as the patient's history of undergoing adrenalectomy for primary adrenocortical carcinoma helped the pathologist reach the diagnosis of metastatic adrenocortical carcinoma. Here, we focus on the cytologic differential points of metastastic pulmonary adrenocortical carcinoma and primary pulmonary carcinoma, especially large cell carcinoma.
- Differential Expression of Glut1 in Pulmonary Neuroendocrine Tumors: Correlation with Histological Grade.
- Hyun Ju Lee, Seol Bong Yoo, Won Woo Lee, Doo Hyun Chung, Jeong Wook Seo, Jin Haeng Chung
- Korean J Pathol. 2009;43(3):201-205.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.3.201
- 5,031 View
- 39 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Increased glucose uptake, a process that is mediated by glucose transporter (Glut1) proteins, is an important metabolic feature in a variety of cancer cells. The overexpression of Glut1 in human cancers is known to be related to a variety of histopathological parameters, including histological grade, proliferation rate, and lymphatic invasion. The principal objective of this study was to evaluate Glut1 expression in the spectrum of pulmonary neuroendocrine (NE) tumors including typical carcinoid tumor (TC), atypical carcinoid tumor (AC), large cell neuroendocrine carcinoma (LCNEC), and small cell carcinoma (SCC), and to characterize the relationship between Glut1 expression and the histologic grade of NE tumors.
METHODS
19 TC, 7 AC, 13 LCNEC, and 6 SCC patients were included in this study. The percentages of Glut1-positive tumor cells in these patients were determined. For statistical analysis, Glut1 expression was subdivided into a Glut1-low expression group (0-30%) and a Glut1-high expression group (31-90%).
RESULTS
In our subgroup analyses, the histological grade of pulmonary neuroendocrine (NE) tumors was significantly correlated with Glut1 expression; TC (n=19, 3.6+/-4.2%), AC (n=7, 20.0+/-4.9%), LCNEC (n=13, 60.0+/-21.1%), and SCC (n=6, 74.2+/-16.9%). Glut1-high expression was significantly associated with high-grade NE tumors such as LCNEC and SCC (n=19, 62.6+/-21.0%) (p=0.000).
CONCLUSIONS
The results of this study appear to indicate that Glut1 overexpression is a consistent feature of high-grade NE lung tumors. -
Citations
Citations to this article as recorded by- GLUT1: A novel tool reflecting proliferative activity of lung neuroendocrine tumors?
Nazim Benzerdjeb, Pascal Berna, Henri Sevestre
Pathology International.2017; 67(1): 32. CrossRef - Oncocytic carcinoid tumor of the lung with intense F-18 fluorodeoxyglucose (FDG) uptake in positron emission tomography–computed tomography (PET/CT)
Yuki Tanabe, Yoshifumi Sugawara, Rieko Nishimura, Kohei Hosokawa, Makoto Kajihara, Teruhiko Shimizu, Tadaaki Takahashi, Shinya Sakai, Shigeki Sawada, Motohiro Yamashita, Haruhiko Ohtani
Annals of Nuclear Medicine.2013; 27(8): 781. CrossRef
- GLUT1: A novel tool reflecting proliferative activity of lung neuroendocrine tumors?
- Fine Needle Aspiration Cytologic Findings of Pulmonary Neuroendocrine Tumors.
- Jae Soo Koh
- J Pathol Transl Med. 2008;19(1):9-15.
- DOI: https://doi.org/10.3338/kjc.2008.19.1.9
- 2,800 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - The major categories of neuroendocrine tumors of lung are typical carcinoid, atypical carcinoid, large cell neuroendocrine carcinoma, and small cell carcinoma. The histologic classification criteria of neuroendocrine tumors are well documented in the "WHO Classification of Tumors" based on mitotic figures and necrosis. Cytologic characteristics of neuroendocrine tumors are trabecular, acinar, and solid arrangement of tumor cells and occasional rosette formation. Nuclear chromatin patterns are characteristically described as "salt and pepper chromatin pattern". Many of cytologic classifications documented in the literature are before the "WHO Classification". In this review, the cytologic features of pulmonary neuroendocrine tumors are documented according to the WHO classification, and recent concepts of neuroendocrine tumors of lung are discussed.
- Expression of bcl-2, p53 and VEGF in Non-Small Cell Lung Carcinomas: Their Relation with the Microvascular Density and Prognosis.
- Jinyoung Yoo, Ji Han Jung, Hyun Joo Choi, Seok Jin Kang, Chang Suk Kang
- Korean J Pathol. 2005;39(2):74-80.
- 2,182 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The aim of this study was to investigate the expression of bcl-2, p53 and vascular endothelial growth factor (VEGF) in non-small cell lung cancer (NSCLC), and to examine the relationship between those protein expressions and neovascularization. We also analyzed the prognostic impact of these biological parameters on the patients' overall survival rate.
METHODS
The archival tumor tissues from 147 previously untreated patients with NSCLC were examined by immunohistochemistry for bcl-2, p53 and VEGF proteins. The vascularity was measured by the average microvascular density (MVD) of the CD34-positive vessels. Clinical information was obtained through the computerized retrospective database from the tumor registry.
RESULTS
Immunoreactivity for bcl-2 was detected in 17% (25/147), p53 in 72% (106/147) and VEGF in 75% (110/147) of the tumors. An inverse association was found between bcl-2 expression and VEGF expression (p=0.012). There was a significant correlation between the bcl-2 expression and the MVD (p=0.009), and also between the p53 expression and the MVD (p=0.045). The mean survival time was associated with the patients' age (p=0.032), the T status (p=0.038), the tumor stage (p=0.009), and expressions of bcl-2 (p=0.016) and VEGF (p=0.039). On multivariate analysis, only the tumor stage and VEGF expression maintained their prognostic influence.
CONCLUSIONS
Our data suggest that bcl-2 and p53 alterations are involved in the angiogenesis of NSCLC, and are either dependent on or independent of VEGF. It is further noteworthy that the tumor stage and VEGF expression may be useful in predicting patients' survival.
- Emphysematous Cystic Pulmonary Metastasis of Angiosarcoma.
- Tae Heon Kim, Ji Sun Song, Soon Hee Jung, Ki Jun Sung, Eun Gi Kim
- Korean J Pathol. 2001;35(6):544-546.
- 2,059 View
- 10 Download
-
 Abstract
Abstract
- Pulmonary metastatic angiosarcoma usually reveals multiple nodular lesions associated with parenchymal hemorrhage. It is presented, in rare cases, as multiple emphysematous cystic lesions, complicated by pneumothorax. We experienced a case of pulmonary metastastasis from angiosarcoma of the scalp in a 58-year-old male showing multiple thin-walled emphysematous cystic lesions. The tumor cells spread along the subpleural and interlobular septa, focally surrounding the cystic lesions. This case suggests that a rare metastatic pattern seen in angiosarcoma of the scalp should be considered as a differential diagnosis of bullous emphysematous lesion.
- Pulmonary Lymphangioleiomyomatosis and Micronodular Pneumocyte Hyperplasia associated with Tuberous Sclerosis: A Case Report.
- Gou Young Kim, Juhie Lee, Yong Koo Park, Youn Wha Kim, Jae Hoon Park, Moon Ho Yang
- Korean J Pathol. 2002;36(1):51-54.
- 2,203 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Lymphangioleiomyomatosis (LAM) is characterized by a hamartomatous proliferation of smooth muscle cells in the lung, mediastium, and abdomen. In the lung, an abnormal proliferation of smooth muscle is seen along the airways, blood vessels, and lymphatics, resulting in honeycombing of the lung. It occurs in 0.1-1% of tuberous sclerosis (TSC) patients. Micronodular pneumocyte hyperplasia (MNPH) is a rare but distinctive pulmonary manifestation of TSC, and appears to be a hamartomatous proliferation of the type II pneumocytes. We report a case of pulmonary LAM and MNPH associated with TSC and bilateral renal angiomyolipoma in a 26-year-old woman. Immunohistochemically, the spindle cells of LAM were positive for HMB-45, but the type II pneumocytes of MNPH were negative.
- Loss of PTEN Expression in Primary Lung Cancer.
- Mee Sook Roh
- Korean J Pathol. 2002;36(5):286-291.
- 1,941 View
- 12 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The phosphatase and tensin homolog deleted on chromosome 10 (PTEN) gene, a candidate tumor suppressor, is localized to chromosome 10q23 and shares extensive homology with cytoskeletal proteins auxilin and tensin. It appears to have multifunctional roles involved in cell proliferation, migration, and invasion. The role of PTEN alteration in the lung cancer and its relationship with other suppressor genes are not well established.
METHODS
Formalin-fixed, paraffin-embedded tissues from 105 patients with diagnosed with primary lung cancer were evaluated for PTEN and p53 protein expression using immunohistochemical methods. The results of the expression pattern of PTEN were compared with clinicopathological parameters and the expression pattern of p53.
RESULTS
Forty-seven (44.8%) of 105 cases had loss of PTEN expression. Loss of PTEN expression was significantly associated with histologic type (p<0.05), but did not correlate with tumor size, lymph node metastasis, and stage. There was no significant relationship between loss of PTEN expression and p53 expression, and no significant difference in clinicopathologic characteristics between particular groups of patterns with the four possible tumor carrying PTEN/p53 phenotypes.
CONCLUSION
It is suggested that loss of PTEN expression occurs commonly in primary lung cancers and correlates with histologic type. Our results also support the proposed role of PTEN as a candidate tumor suppressor in lung cancer, and we suggest that there is a need for further study of this gene.
- Expression of Thymidylate Synthase in Non-Small Cell Lung Cancer.
- Jinyoung Yoo, Suzi Kim, Byoung Yong Shim, Sung Hwan Kim, So Hyang Song, Deog Gon Cho, Meyung Im Ahn, Chi Hong Kim, Kyu Do Cho, Seok Jin Kang, Hoon Kyo Kim
- Korean J Pathol. 2005;39(6):412-417.
- 2,245 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Thymidylate synthase (TS) catalyzes the methylation of deoxyuridine monophosphate (dUMP) to deoxythymidine monophosphate (dTMP), and this is an essential step in DNA biosynthesis. The present investigation was designed to determine the expression of TS in the patients with non-small cell lung cancer (NSCLC) and to assess the possible associations between the TS status and the p53 or proliferative index (PI).
METHODS
The archival tumor tissues from 56 previously untreated NSCLC patients were examined by immunohistochemistry for TS, p53 and Ki-67.
RESULTS
Forty-one men and 15 women (age range: 35 to 79 years, mean age: 62 years) were included in this study. The TS expression was high in 40 patients (71.4%) and low in 16 patients (28.6%). The aberrant expression of p53 was detected in 35 patients (62.5%). The mean PI for all the patients was 31.4+/-12.1. The TS-high tumors tended to be more poorly differentiated (p=0.069). The TS expression by a semiquantitative fourscale grading system was significantly correlated with the PIs (p=0.003). No correlation was established between the TS expression and the p53 status (p=0.806) or survival (p=0.951). CONCLUSIONS: TS was not confirmed to be a useful marker for determining the prognosis of NSCLC patients. However, our data suggest that the tumor cells with higher TS expression have a higher proliferative activity.

 E-submission
E-submission

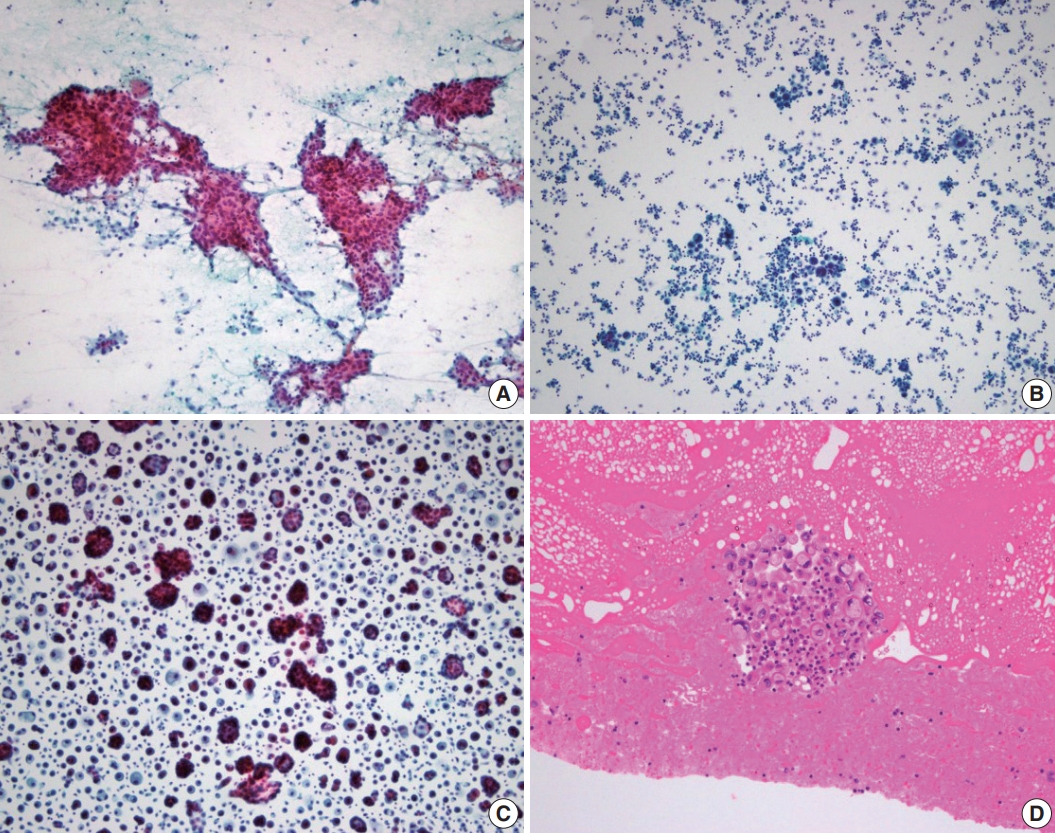

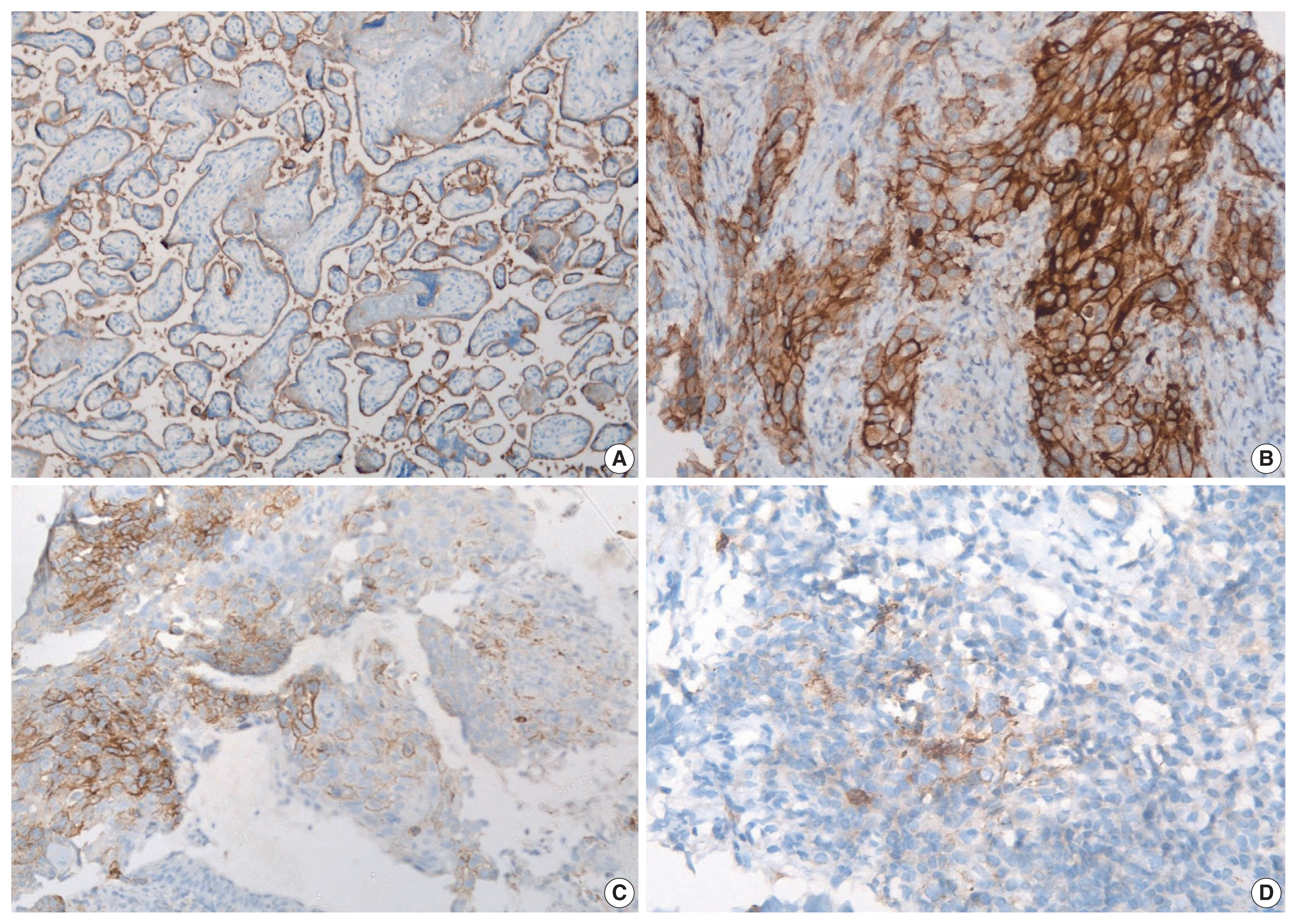

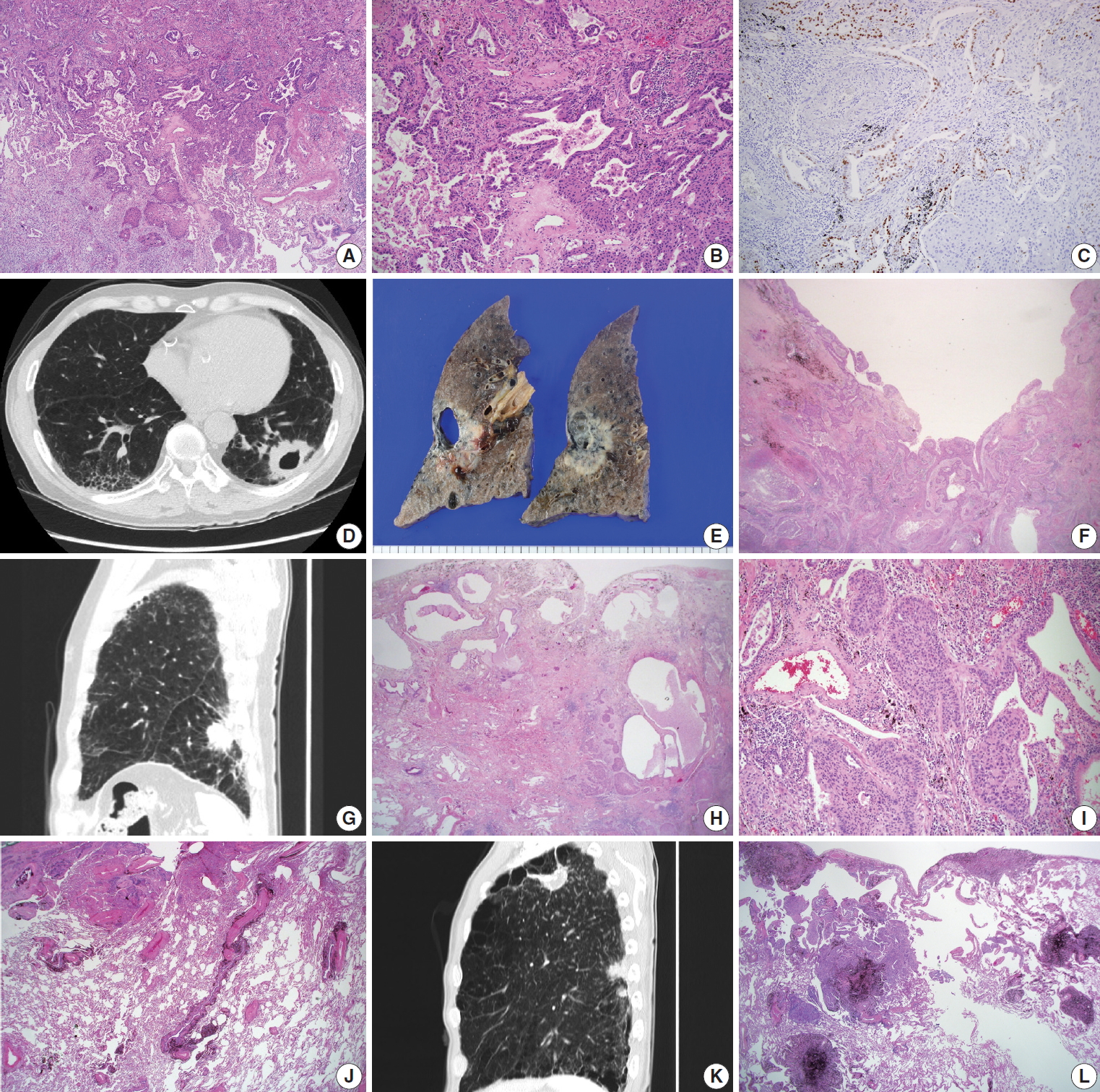
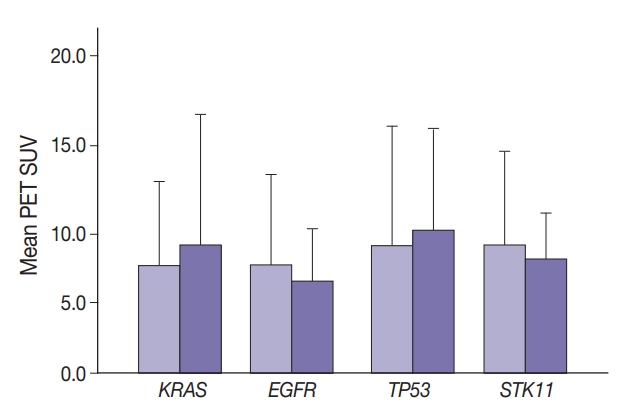
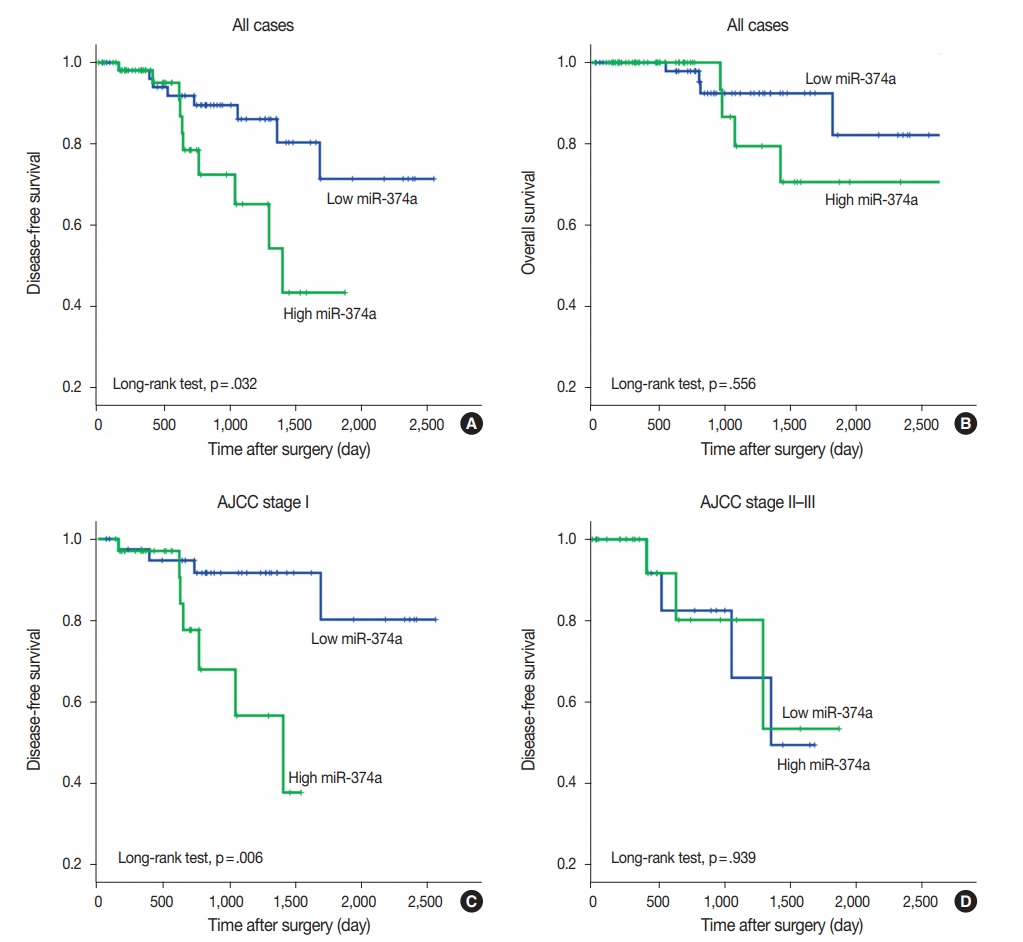
 First
First Prev
Prev



