Search
- Page Path
- HOME > Search
- Evaluation of the characteristics of multiple human papillomavirus (HPV) infections identified using the BD Onclarity HPV assay and comparison with those of single HPV infection
- Jinhee Kim, Moonsik Kim, Ji Young Park
- J Pathol Transl Med. 2022;56(5):289-293. Published online September 13, 2022
- DOI: https://doi.org/10.4132/jptm.2022.08.02
- 7,883 View
- 136 Download
- 10 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Human papillomavirus (HPV) infection is a major cause of cervical cancer and associated precursor lesions. Multiple HPV genotype infections have been reported. However, their clinicopathological characteristics still remain elusive.
Methods
For this study, 814 consecutive patients who had undergone colposcopy and HPV genotyping test using BD Onclarity HPV assay were retrospectively selected. Clinicopathological parameters of multiple HPV infections were compared with those of single HPV infection.
Results
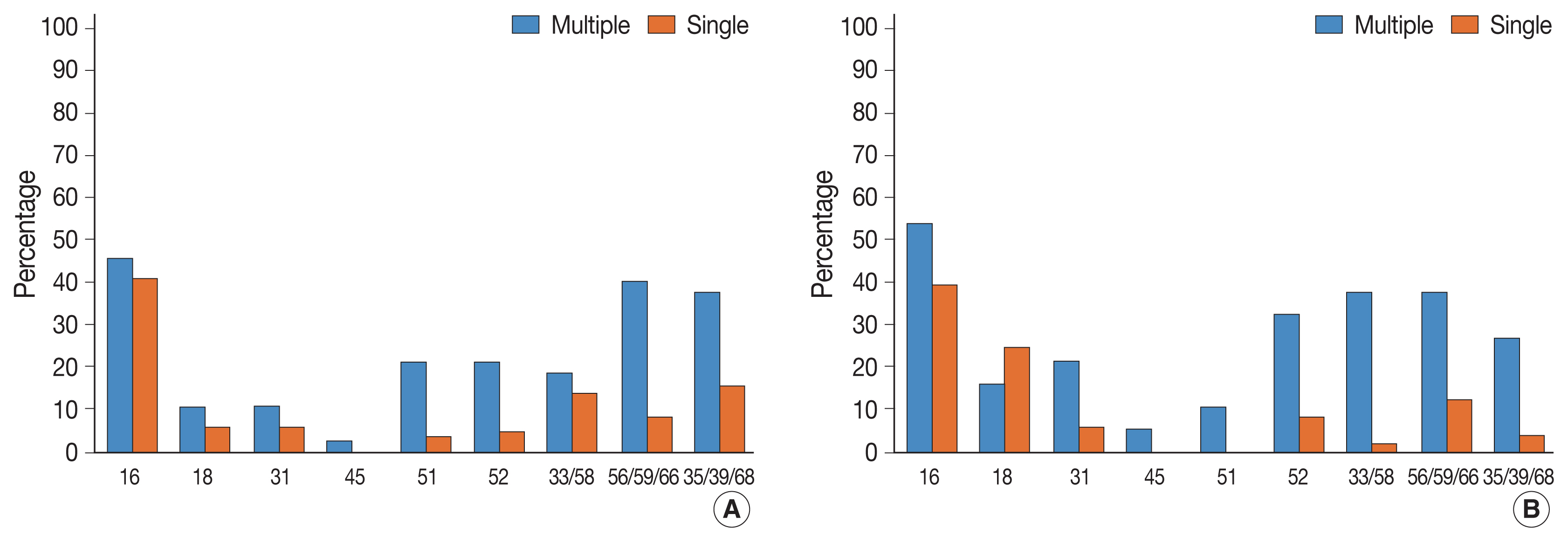
Multiple HPV infections were found in 110 out of 814 cases (13.5%). Multiple HPV infections were associated with a significantly higher incidence of high-grade intraepithelial lesions (HSILs) compared with single HPV infection. Other high-risk HPV genotypes, in addition to HPV 16, were found more frequently in the multiple HPV infections group; these included HPV 51, 52, 33/58, 56/59/66, and 35/39/68. No specific coinfection pattern was not identified. Additionally, the number of HPV genotypes in multiple HPV infections was not associated with the progression to HSIL or squamous cell carcinoma.
Conclusions
Multiple HPV infections have distinct clinicopathological characteristics (compared with single HPV infection). As their biological behavior is uncertain, close and frequent follow-up is warranted. -
Citations
Citations to this article as recorded by- The Prevalence of Multi-Type Infections Among Human Papillomavirus Types in Korean Women
Jang Mook Kim, Hee Seung Song, Jieun Hwang, Jae Kyung Kim
Pathogens.2025; 14(4): 369. CrossRef - Multiple high-risk human papillomavirus infections exacerbate cervical lesion risk: epidemiological evidence from suining, Sichuan
Yaling Jing, Jianhui Chen, Fang Lin, Xiaonan Huang, Yulin Liu, Mingcai Zhao, Chuan Ye, Lianfang Zhao, Xiaofang Liu, Jiayan Yang
Virology Journal.2025;[Epub] CrossRef - The cervical cancer related distribution, coinfection and risk of 15 HPV types in Baoan, Shenzhen, in 2017–2023
Rukai Li, Weiwei Meng, Yunhai Zuo, Yanli Xu, Shaonan Wu
Virology Journal.2024;[Epub] CrossRef - Molecular findings and virological assessment of bladder papillomavirus infection in cattle
Francesca De Falco, Anna Cutarelli, Francesca Luisa Fedele, Cornel Catoi, Sante Roperto
Veterinary Quarterly.2024; 44(1): 1. CrossRef - Patterns of single and multiple HPV infections in female: A systematic review and meta-analysis
Dan Zhou, Jing Xue, Yaqiong Sun, Liling Zhu, Ming Zhao, Meimei Cui, Min Zhang, Jingjing Jia, Limei Luo
Heliyon.2024; 10(17): e35736. CrossRef - Age distribution of patients with multiple High-Risk Human Papilloma Virus (HR-HPV) genotypes and HPV vaccine recommendations by age
Gülçin Çetin Uysal, Nil Tekin
Family Practice and Palliative Care.2024; 9(3): 80. CrossRef - Relative distribution of HPV genotypes in histological cervical samples and associated grade lesion in a women population over the last 16 years in Burgundy, France
Christelle Auvray, Serge Douvier, Odile Caritey, Jean-Baptiste Bour, Catherine Manoha
Frontiers in Medicine.2023;[Epub] CrossRef - Epidemiologic characteristics of high-risk HPV and the correlation between multiple infections and cervical lesions
Qinli Luo, Xianghua Zeng, Hanyi Luo, Ling Pan, Ying Huang, Haiyan Zhang, Na Han
BMC Infectious Diseases.2023;[Epub] CrossRef
- The Prevalence of Multi-Type Infections Among Human Papillomavirus Types in Korean Women
- Human Papillomavirus Serologic Profiles of Selected Filipinos with Head and Neck Squamous Cell Carcinoma
- Pia Marie Albano, Christianne Salvador, Jose Orosa, Sheryl Racelis, Modesty Leaño, Angelika Michel, John Donnie Ramos, Dana Holzinger, Michael Pawlita
- J Pathol Transl Med. 2019;53(5):273-279. Published online May 30, 2019
- DOI: https://doi.org/10.4132/jptm.2019.05.12
- 8,386 View
- 196 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The low prevalence of human papillomavirus (HPV) DNA and mRNA in biopsy samples of Filipinos with head and neck squamous cell carcinoma (HNSCC) has been reported previously. Here, the HPV serologic profiles of HNSCC cases were analyzed and associated with life-style and sexual practices.
Methods
Serum samples were collected between May 2012 and September 2013 from HNSCC patients (n = 22) in the northwest region of the Philippines, and age- and sex-matched clinically healthy controls. Antibodies to capsid and early oncoproteins of HPV16, 18, 31, 33, 45, 52, 58, 6, and 11 were analyzed using multiplex serology.
Results
Most of the cases were males with tumors of the oral cavity or larynx. Two of the cases tested positive for at least one of the early oncoproteins (E6, E7, E1, and/or E2) of HPV16, and 11 did not display reactivity to any HPV early or late oncoproteins. Of the controls, four tested positive for at least one of the HPV16 early oncoproteins, and 10 were non-reactive to all HPV types. Titers to HPV16 E6 or E7 of the seropositive cases and controls were considerably lower than those typically observed in economically developed countries.
Conclusions
The low HPV titers seen here are consistent with the results of molecular analyses for this population. Hence, the seropositivity of some of the HNSCC cases is likely an indication of prior exposure to the virus and not the presence of HPV-driven tumors. -
Citations
Citations to this article as recorded by- Social determinants of sex disparities in cancer in Southeast Asia
Ma. Veronica Pia N. Arevalo, Ethan Angelo S. Maslog, Katherine Donatela Manlongat, Eric David B. Ornos, Imjai Chitapanarux, Michelle Ann B. Eala, Edward Christopher Dee
iScience.2023; 26(7): 107110. CrossRef
- Social determinants of sex disparities in cancer in Southeast Asia
- Distribution of Human Papillomavirus 52 and 58 Genotypes, and Their Expression of p16 and p53 in Cervical Neoplasia
- Tae Eun Kim, Hwal Woong Kim, Kyung Eun Lee
- Korean J Pathol. 2014;48(1):24-29. Published online February 25, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.1.24
- 10,810 View
- 64 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Background This study investigates the prevalence of human papillomavirus (HPV) 52 and 58 genotypes among women residing in Busan, and the expression of p16 and p53 proteins in cervical neoplasia with HPV 52 and 58 infections.
Methods A total of three hundred fifteen cases were analyzed using the HPV DNA chip test for HPV genotypes, and of these, we retrospectively examined p16 and p53 expression in 62 cases of cervical tissues infected with HPV 52 and 58 using immunohistochemistry.
Results HPV 52 and 58 genotypes were identified in 62 (54.9%) out of 113 high-risk, HPV-infected cases. Of the cases examined, there were 19 single HPV 52 infections (16.8%), 23 single HPV 58 infections (20.4%), 4 multiple HPV 52 infections (3.5%), and 16 multiple HPV-58 infections (14.2%). Immunoreactivity of p16 and p53 was observed in 41 (66.1%) and 23 (37.1%) of the 62 cases of cervical neoplasia infected with HPV 52 and 58 genotypes, respectively.
Conclusions This study demonstrates a high prevalence of HPV 52 and 58 genotypes, in addition to HPV 16, among high-risk strains of cervical neoplasia in Korea. These findings suggest that development of more vaccines would be beneficial for the prevention of the various HPV genotypes.
-
Citations
Citations to this article as recorded by- Screening for High-Risk Human Papillomavirus Reveals HPV52 and HPV58 among Pediatric and Adult Patient Saliva Samples
Hunter Hinton, Lorena Herrera, Sofia Valenzuela, Katherine M. Howard, Karl Kingsley
Dentistry Journal.2024; 12(3): 56. CrossRef - Usefulness Analysis of Urine Samples for Early Screening of Human Papilloma Virus Infection
Yoon Sung Choi, Hyunwoo Jin, Kyung Eun Lee
Journal of Cancer Prevention.2019; 24(4): 240. CrossRef - Relationship between Expression of P16 and Ki-67 and Persistent Infection of HPV in Cervical Carcinoma Patients
群欢 黄
Advances in Clinical Medicine.2018; 08(08): 776. CrossRef - Analysis of Sequence Variation and Risk Association of Human Papillomavirus 52 Variants Circulating in Korea
Youn Jin Choi, Eun Young Ki, Chuqing Zhang, Wendy C. S. Ho, Sung-Jong Lee, Min Jin Jeong, Paul K. S. Chan, Jong Sup Park, Xuefeng Liu
PLOS ONE.2016; 11(12): e0168178. CrossRef
- Screening for High-Risk Human Papillomavirus Reveals HPV52 and HPV58 among Pediatric and Adult Patient Saliva Samples
- Primary Squamous Cell Carcinoma of the Upper Genital Tract: Utility of p16INK4a Expression and HPV DNA Status in its Differential Diagnosis from Extended Cervical Squamous Cell Carcinoma
- Su Hyun Yoo, Eun-Mi Son, Chang Okh Sung, Kyu-Rae Kim
- Korean J Pathol. 2013;47(6):549-556. Published online December 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.6.549
- 8,861 View
- 66 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Primary squamous cell carcinoma (SCC) of the upper genital tract, including the endometrium, fallopian tubes, and ovaries, is extremely rare. It must be distinguished from the mucosal extension of primary cervical SCC because determination of the primary tumor site is important for tumor staging. However, patients with SCC of the fallopian tubes or ovarian surface have often undergone prior hysterectomy with inadequate examination of the cervix, making it difficult to determine the primary site.
Methods We compared histologic findings, p16INK4a expression, and human papillomavirus (HPV) DNA status in four patients with primary SCC of the upper genital tract and five patients with primary cervical SCC extending to the mucosa of the upper genital tract.
Results All five SCCs of cervical origin showed strong expression of p16INK4a, whereas all four SCCs of the upper genital tract were negative, although one showed weak focal staining. Three of the five cervical SCCs were positive for HPV16 DNA, whereas all four primary SCCs of the upper genital tract were negative for HPV DNA.
Conclusions Although a thorough histological examination is important, immunonegativity for p16INK4a and negative for HPV DNA may be useful adjuncts in determining primary SCCs of the upper genital tract.
-
Citations
Citations to this article as recorded by- A Case of Squamous Cell Carcinoma Clinically Thought to be Arising From Bursa of Knee Joint
Shoichi Sakamoto, Yuki Yamamoto, Michihiro Takiwaki, Yumi Nakantani, Seiji Kanno, Yoshimasa Mera, Masazumi Tanigami, Yusuke Inada, Yutaka Inaba, Kayo Kunimoto, Hiroshi Yamada, Yoshifumi Iwahashi, Shin‐ichi Murata, Masatoshi Jinnin
Australasian Journal of Dermatology.2025; 66(3): 175. CrossRef - PAX8 Positivity, Abnormal p53 Expression, and p16 Negativity in a Primary Endometrial Squamous Cell Carcinoma: A Case Report and Review of the Literature
Daniela Fanni, Michele Peiretti, Valerio Mais, Elena Massa, Clara Gerosa, Francesca Ledda, Maria Luisa Fais, Gavino Faa, Stefano Angioni
International Journal of Gynecological Pathology.2022; 41(4): 431. CrossRef - Molecular Analysis of HPV-independent Primary Endometrial Squamous Cell Carcinoma Reveals TP53 and CDKN2A Comutations
Mark R. Hopkins, Doreen N. Palsgrove, Brigitte M. Ronnett, Russell Vang, Jeffrey Lin, Tricia A. Murdock
American Journal of Surgical Pathology.2022; 46(12): 1611. CrossRef - Primary squamous cell carcinoma of the endometrium—Case report with cytological characteristics in direct and indirect endometrial samples
Sanda Rajhvajn, Ana Barišić, Lada Škopljanac‐Mačina, Danijela Jurič, Vesna Mahovlić
Cytopathology.2021; 32(6): 823. CrossRef - Überraschung in der Abradatdiagnostik
U. Kellner, A. Kellner, U. Cirkel
Der Pathologe.2015; 36(3): 317. CrossRef - Retropharyngeal Lymph Node Metastasis in 54 Patients with Oropharyngeal Squamous Cell Carcinoma Who Underwent Surgery-Based Treatment
Eun-Jae Chung, Go-Woon Kim, Bum-Ki Cho, Sung-Jin Cho, Dae-Young Yoon, Young-Soo Rho
Annals of Surgical Oncology.2015; 22(9): 3049. CrossRef
- A Case of Squamous Cell Carcinoma Clinically Thought to be Arising From Bursa of Knee Joint
- Cytological Evaluation and REBA HPV-ID HPV Testing of Newly Developed Liquid-Based Cytology, EASYPREP: Comparison with SurePath
- Youn Soo Lee, Gyungyub Gong, Jin Hee Sohn, Ki Sung Ryu, Jung Hun Lee, Shin Kwang Khang, Kyung-Ja Cho, Yong-Man Kim, Chang Suk Kang
- Korean J Pathol. 2013;47(3):265-274. Published online June 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.3.265
- 11,954 View
- 98 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The objective of this study was to evaluate a newly-developed EASYPREP liquid-based cytology method in cervicovaginal specimens and compare it with SurePath.
Methods Cervicovaginal specimens were prospectively collected from 1,000 patients with EASYPREP and SurePath. The specimens were first collected by brushing for SurePath and second for EASYPREP. The specimens of both methods were diagnosed according to the Bethesda System. Additionally, we performed to REBA HPV-ID genotyping and sequencing analysis for human papillomavirus (HPV) on 249 specimens.
Results EASYPREP and SurePath showed even distribution of cells and were equal in cellularity and staining quality. The diagnostic agreement between the two methods was 96.5%. Based on the standard of SurePath, the sensitivity, specificity, positive predictive value, and negative predictive value of EASYPREP were 90.7%, 99.2%, 94.8%, and 98.5%, respectively. The positivity of REBA HPV-ID was 49.4% and 95.1% in normal and abnormal cytological samples, respectively. The result of REBA HPV-ID had high concordance with sequencing analysis.
Conclusions EASYPREP provided comparable results to SurePath in the diagnosis and staining quality of cytology examinations and in HPV testing with REBA HPV-ID. EASYPREP could be another LBC method choice for the cervicovaginal specimens. Additionally, REBA HPV-ID may be a useful method for HPV genotyping.
-
Citations
Citations to this article as recorded by- Virome capture sequencing for comprehensive HPV genotyping in cervical samples
Thanayod Sasivimolrattana, Sasiprapa Liewchalermwong, Wasun Chantratita, Insee Sensorn, Arkom Chaiwongkot, Parvapan Bhattarakosol
Science Progress.2025;[Epub] CrossRef - High-Risk Human Papillomavirus Detection via Cobas® 4800 and REBA HPV-ID® Assays
Sasiprapa Liewchalermwong, Shina Oranratanaphan, Wichai Termrungruanglert, Surang Triratanachat, Patou Tantbirojn, Nakarin Kitkumthorn, Parvapan Bhattarakosol, Arkom Chaiwongkot
Viruses.2022; 14(12): 2713. CrossRef - Evaluation of nuclear chromatin using grayscale intensity and thresholded percentage area in liquid‐based cervical cytology
Hyekyung Lee, Myungein Han, Taejo Yoo, Chanho Jung, Hyun‐Jin Son, Migyung Cho
Diagnostic Cytopathology.2018; 46(5): 384. CrossRef - Comparison of EASYPREP® and SurePath® in thyroid fine‐needle aspiration
Yosep Chong, Ki Hyun Baek, Jee Young Kim, Tae‐Jung Kim, Eun Jung Lee, Chang Suk Kang
Diagnostic Cytopathology.2016; 44(4): 283. CrossRef
- Virome capture sequencing for comprehensive HPV genotyping in cervical samples
- Expression of CHOP in Squamous Tumor of the Uterine Cervix
- Hyun Hee Chu, Jun Sang Bae, Kyoung Min Kim, Ho Sung Park, Dong Hyu Cho, Kyu Yun Jang, Woo Sung Moon, Myoung Jae Kang, Dong Geun Lee, Myoung Ja Chung
- Korean J Pathol. 2012;46(5):463-469. Published online October 25, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.5.463
- 9,407 View
- 40 Download
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Background High-risk human papillomavirus (HR-HPV) infection and abnormal p53 expression are closely involved in carcinogenesis of squamous cell carcinoma (SqCC) of uterine cervix. Recent studies have suggested that virus-induced endoplasmic reticulum (ER) stress modulates various cell survival and cell death signaling pathways. The C/EBP homologous protein (CHOP) is associated with ER stress-mediated apoptosis and is also involved in carcinogenesis of several human cancers. We hypothesized that CHOP is involved in the carcinogenesis of uterine cervical cancer in association with HR-HPV and/or p53.
Methods Immunohistochemistry was used to analyze CHOP and p53 protein expression of tissue sections from 191 patients with invasive cancer or preinvasive lesions of the uterine cervix (61 cases of SqCC, 66 cases of cervical intraepithelial neoplasia [CIN] III, and 64 cases of CIN I).
Results CHOP was expressed in 59.4% of CIN I, 48.5% of CIN III, and 70.5% of SqCC cases. It was also significantly more frequent in invasive SqCC than in preinvasive lesions (p=0.042). Moreover, CHOP expression significantly correlated with HR-HPV infection and p53 expression (p=0.009 and p=0.038, respectively).
Conclusions Our results suggest that CHOP is involved in the carcinogenesis of the uterine cervix SqCC via association with HR-HPV and p53.
-
Citations
Citations to this article as recorded by- Interplay between the cellular stress pathway, stemness markers, and Helicobacter pylori infection in gastric cancer
Mehran Gholamin, Atena Mansouri, Mohammad Reza Abbaszadegan, Mohammad Ali Karimi, Hossein Barzegar, Fatemeh Fardi Golyan, Hanie Mahaki, Hamid Tanzadehpanah, Reihaneh Alsadat Mahmoudian
Gene Reports.2025; 40: 102263. CrossRef - Role of C-reactive protein in cervical intraepithelial neoplasia/cancer
Adriana Pedreañez, Yenddy Carrero, Renata Vargas, Juan P.Hernández Fonseca, Jesús Mosquera
Pathology - Research and Practice.2025; 276: 156274. CrossRef - Expression of GRP78 and its copartners in HEK293 and pancreatic cancer cell lines (BxPC-3/PANC-1) exposed to MRI and CT contrast agents
Ali Ahmed Azzawri, Ibrahim Halil Yildirim, Zeynep Yegin, Abdurrahim Dusak
Nucleosides, Nucleotides & Nucleic Acids.2024; 43(5): 391. CrossRef - Endoplasmic Reticulum Stress and Homeostasis in Reproductive Physiology and Pathology
Elif Guzel, Sefa Arlier, Ozlem Guzeloglu-Kayisli, Mehmet Tabak, Tugba Ekiz, Nihan Semerci, Kellie Larsen, Frederick Schatz, Charles Lockwood, Umit Kayisli
International Journal of Molecular Sciences.2017; 18(4): 792. CrossRef - Endoplasmic reticulum stress pathway PERK‐eIF2α confers radioresistance in oropharyngeal carcinoma by activating NF‐κB
Qiao Qiao, Chaonan Sun, Chuyang Han, Ning Han, Miao Zhang, Guang Li
Cancer Science.2017; 108(7): 1421. CrossRef - Curcumin induces ER stress-mediated apoptosis through selective generation of reactive oxygen species in cervical cancer cells
Boyun Kim, Hee Seung Kim, Eun-Ji Jung, Jung Yun Lee, Benjamin K. Tsang, Jeong Mook Lim, Yong Sang Song
Molecular Carcinogenesis.2016; 55(5): 918. CrossRef - Down-regulation of C/EBP homologous protein (CHOP) expression in gastric cardia adenocarcinoma: Their relationship with clinicopathological parameters and prognostic significance
Xiao-Juan Zhu, She-Gan Gao, San-Qiang Li, Zhen-Guo Shi, Zhi-Kun Ma, Shan-Shan Zhu, Xiao-Shan Feng
Clinics and Research in Hepatology and Gastroenterology.2015; 39(3): 391. CrossRef - MG289 in <i>Mycoplasma genitalium</i> Enhances Microbial Invasion and Bacterial Persistence in Benign Human Prostate Cells
Wasia Rizwani, Leticia Reyes, Jeongsoon Kim, Steve Goodison, Charles J. Rosser
Open Journal of Urology.2013; 03(06): 232. CrossRef
- Interplay between the cellular stress pathway, stemness markers, and Helicobacter pylori infection in gastric cancer
- Cytomorphologic Features According to HPV DNA Type in Histologically Proven Cases of the Uterine Cervix.
- In Ho Choi, So Young Jin, Dong Wha Lee, Dong Won Kim, Yoon Mi Jeen
- Korean J Pathol. 2011;45(6):612-620.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.6.612
- 4,902 View
- 37 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
This study investigated whether human papillomavirus (HPV) genotype is related to koilocytic changes in cervical cytology and histology, and what factors cause discrepancies among cytology, HPV DNA chip tests, and biopsies.
METHODS
We examined 174 of 949 cases histologically confirmed by both cytology and HPV DNA chip testing. We analyzed koilocytic changes in cytology and biopsies according to HPV genotype.
RESULTS
HPV-16 significantly coincided with nuclear size variation and hyperchromasia, although the cytomorphologic features correlated with other HPV genotypes were not statistically significant. By analyzing 68 cases in which there were discrepancies between the HPV DNA chip test and histological results, we confirmed that artifacts or glycogen acanthosis resulted in the over-diagnoses of four HPV-negative cases with normal cytology. Four diagnostic errors and four sampling errors were present in eight HPV-positive cases. The degree of nuclear size variation significantly influenced the cytologically under-diagnosed cases (p=0.006).
CONCLUSIONS
Other than HPV-16, HPV genotype exhibited no cytological or histological differences. The discrepancy between the results of HPV DNA chip test and histology was created by glycogen acanthosis, immature squamous metaplasia, artifacts, and sampling errors. -
Citations
Citations to this article as recorded by- Koilocytic changes are not elicited by human papillomavirus genotypes with higher oncogenic potential
Mitsuaki Okodo, Kaori Okayama, Koji Teruya, Hirokazu Kimura, Natsumi Noji, Yasuyoshi Ishii, Masahiko Fujii, Mizue Oda, Toshiyuki Sasagawa
Journal of Medical Virology.2020; 92(12): 3766. CrossRef - Analysis of Sequence Variation and Risk Association of Human Papillomavirus 52 Variants Circulating in Korea
Youn Jin Choi, Eun Young Ki, Chuqing Zhang, Wendy C. S. Ho, Sung-Jong Lee, Min Jin Jeong, Paul K. S. Chan, Jong Sup Park, Xuefeng Liu
PLOS ONE.2016; 11(12): e0168178. CrossRef - Uncommon and Rare Human Papillomavirus Genotypes Relating to Cervical Carcinomas
Na Rae Kim, Myunghee Kang, Soon Pyo Lee, Hyunchul Kim, Jungsuk An, Dong Hae Chung, Seung Yeon Ha, Hyun Yee Cho
Korean Journal of Pathology.2014; 48(1): 43. CrossRef - Distribution of Human Papillomavirus 52 and 58 Genotypes, and Their Expression of p16 and p53 in Cervical Neoplasia
Tae Eun Kim, Hwal Woong Kim, Kyung Eun Lee
Korean Journal of Pathology.2014; 48(1): 24. CrossRef
- Koilocytic changes are not elicited by human papillomavirus genotypes with higher oncogenic potential
- The Usefulness of p16INK4a Immunocytochemical Staining in ASC-H Patients.
- Kwang Il Yim, Yeo Ju Kang, Tae Eun Kim, Gyeongsin Park, Eun Sun Jung, Yeong Jin Choi, Kyo Young Lee, Chang Seok Kang, Ahwon Lee
- Korean J Pathol. 2011;45(3):290-295.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.3.290
- 4,666 View
- 26 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The grey zone of cervical cytology, and in particular atypical squamous cells, cannot exclude HSIL (ASC-H) causes diagnostic difficulties and increases medical expenses. We analyzed p16INK4a expression in ASC-H liquid-based cytology specimens (LBCS) to develop more effective methods for the management of ASC-H patients.
METHODS
We carried out p16INK4a immunostaining with 57 LBCS of ASC-H diagnostic categories, all of which were histologically cofirmed and 43 cases of which were compared with the results of a human papillomavirus (HPV) chip test.
RESULTS
p16INK4a immunostaining with ASC-H LBCS was positive in 20% (3/15) of cervicitis, 25.0% (3/12) of tissue-low-grade squamous intraepithelial lesion, 75.0% (18/24) of tissue-high grade squamous intraepithelial lesion (HSIL), and 100% (6/6) of invasive cancer cases. The positivity of p16INK4a in LBCS was correlated with higher grade of histologic diagnosis (r=0.578, p=0.000). The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of p16INK4a immunostaining for the prediction of tissue-HSIL+ were 80.0%, 77.8%, 80.0%, and 77.8%, respectively. The sensitivity, specificity, PPV, and NPV of p16INK4a immunostaining plus HPV chip test for predicting tissue-HSIL+ were 71.2%, 86.4%, 84.2%, and 79.2%.
CONCLUSIONS
p16INK4a immunostaining as well as HPV chip testing with remaining LBCS with ASC-H are useful objective markers for the prediction of tissue-HSIL+. -
Citations
Citations to this article as recorded by- Usefulness of p16INK4a Immunocytochemical staining for the Differentiation between Atrophy and ASCUS in Diagnosis of Uterine Cervical Cancer
Hye Ryoung Shin, Taekil Eom, Wan-Su Choi
Biomedical Science Letters.2023; 29(3): 144. CrossRef
- Usefulness of p16INK4a Immunocytochemical staining for the Differentiation between Atrophy and ASCUS in Diagnosis of Uterine Cervical Cancer
- Evaluation of the HPV ISH Assay in Cervical Cancer.
- Jung Uee Lee, Jung Ha Shin, Jong Ok Kim, Yeong Jin Choi, Kyo Young Lee, Jong Sup Park, Won Chul Lee, Ahwon Lee
- Korean J Pathol. 2010;44(5):513-520.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.5.513
- 5,506 View
- 116 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Human papillomavirus (HPV) infection can be detected by in situ hybridization (ISH), in which a punctate signal pattern indicates integrated HPV DNA and a diffuse pattern denotes the presence of episomal viral DNA. This study was conducted to evaluate the usefulness of an HPV ISH assay for invasive cervical cancer.
METHODS
The HPV ISH assay for high-risk HPV and immunohistochemical staining for p16(INK4a), p53, bcl-2, and Ki-67 were performed in a tissue microarray of 279 cervical cancers.
RESULTS
High-risk HPV ISH was positive in 194 (69.5%) of the samples. Punctate, diffuse, and mixed signal patterns were observed in 157 (56.3%), one (0.4%), and 36 cases (12.9%), respectively. Positive results in high-risk HPV ISH were associated with p16 and bcl-2 expression (p = 0.01 and p < 0.01, respectively). According to a Cox regression analysis, HPV infection and its surrogate immunohistochemical markers such as p16, bcl-2, and Ki-67 were not independent prognostic factors, but stage and grade were independent prognostic factors.
CONCLUSIONS
Our results confirm that an HPV ISH assay is reasonably sensitive for HPV infection and that it might be useful to identify integrated HPV DNA in formalin-fixed and paraffin-embedded specimens. Further study encompassing HPV type, E2/E6 ratio, and therapeutic modality is necessary to understand the clinical meaning of HPV status in cervical cancer. -
Citations
Citations to this article as recorded by- Prevalence of human papillomavirus in eyelid carcinoma among Koreans: a clinicopathological study
Min Kyu Yang, Namju Kim, Hokyung Choung, Ji Eun Kim, Sang In Khwarg
BMC Ophthalmology.2023;[Epub] CrossRef - Cervical cancer screening by molecular Pap‐transformation of gynecologic cytology
Shaikhali M Barodawala, Kirti Chadha, Vikas Kavishwar, Anuradha Murthy, Shamma Shetye
Diagnostic Cytopathology.2019; 47(5): 374. CrossRef - Prognostic Significance of Amplification of thec-MYCGene in Surgically Treated Stage IB-IIB Cervical Cancer
Tae-Jung Kim, Ahwon Lee, Sung-Jong Lee, Won-Chul Lee, Yeong-Jin Choi, Kyo-Young Lee, Chang Suk Kang
The Korean Journal of Pathology.2011; 45(6): 596. CrossRef
- Prevalence of human papillomavirus in eyelid carcinoma among Koreans: a clinicopathological study
- HPV Genotyping in Squamous Cell Carcinoma of Upper Aerodigestive Tract.
- Young Kim, Eun Hui Jeong, Byung Woo Min, Sung Sun Kim, Yoo Duk Choi, Woon Jae Jung, Jong Hee Nam, Chang Soo Park
- Korean J Pathol. 2010;44(5):483-487.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.5.483
- 4,063 View
- 23 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Smoking and alcohol consumption are the main risk factors for squamous cell carcinoma of the upper aerodigestive tract (SCCUAT). However, human papillomavirus (HPV) has been etiologically linked with tonsillar squamous cell carcinoma (TSCC). Therefore, we investigated the etiologic role of HPV in the context of SCCUAT in Korea.
METHODS
Archival paraffin block samples from 136 cases previously diagnosed as SCCUAT were randomly selected. A commercial HPV DNA chip was used for HPV genotyping.
RESULTS
One hundred and seventeen cases were available after checking beta-globin (47 cases of tonsil and 70 of non-tonsil). A HPV-positive result (HPV 16 and 18) occurred in 13 cases of SCCUAT, and 12 cases were tonsil (25.5%, 12/47). Among the 12 HPV-positive patients with TSCC, nine were non-smokers and non-drinkers. Most HPV-negative patients with TSCC had a history of alcohol drinking and smoking (32/35, 91.4%). HPV infection status was not significantly associated with histological grade, clinical stage, or survival in patients with TSCC.
CONCLUSIONS
HPV infection was significantly higher in patients with TSCC among those with SCCUAT. HPV may be independent risk factor in development of TSCC, such as smoking and alcohol drinking. -
Citations
Citations to this article as recorded by- Prevalence of high-risk human papillomavirus and its genotype distribution in head and neck squamous cell carcinomas
Yuil Kim, Young-Hoon Joo, Min-Sik Kim, Youn Soo Lee
Journal of Pathology and Translational Medicine.2020; 54(5): 411. CrossRef
- Prevalence of high-risk human papillomavirus and its genotype distribution in head and neck squamous cell carcinomas
- Comparison of Clinical Efficacy between an HPV DNA Chip and a Hybrid-Capture II Assay in a Patient with Abnormal Colposcopic Findings.
- Tae Jung Kim, Chan Kwon Jung, Ahwon Lee, Eun Sun Jung, Young Jin Choi, Kyo Young Lee, Jong Sup Park
- J Pathol Transl Med. 2008;19(2):119-125.
- DOI: https://doi.org/10.3338/kjc.2008.19.2.119
- 3,245 View
- 13 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - This study was performed to compare the efficacy between a DNA chip method and a Hybrid-Capture II assay (HC-II) for detecting human papillomavirus in patients with intraepithelial lesions of the uterine cervix. From May, 2005, to June, 2006, 192 patients with abnormal colposcopic findings received cervical cytology, HC-II and HPV DNA chip tests, and colposcopic biopsy or conization. We compared the results of HC-II and HPV DNA chip in conjunction with liquid based cervical cytology (LBCC) and confirmed the results of biopsy or conization. The sensitivity of the HPV DNA chip test was higher than HC-II or LBCC. The HPV DNA chip in conjunction with LBCC showed higher sensitivity than any single method and higher sensitivity than HC-II with LBCC. We confirmed that the HPV DNA chip test was more sensitive for detecting HPV in cervical lesions than HC-II, and that it would provide more useful clinical information about HPV type and its multiple infections.
-
Citations
Citations to this article as recorded by- Comparison of Analytical and Clinical Performance of HPV 9G DNA Chip, PANArray HPV Genotyping Chip, and Hybrid-Capture II Assay in Cervicovaginal Swabs
Ho Young Jung, Hye Seung Han, Hyo Bin Kim, Seo Young Oh, Sun-Joo Lee, Wook Youn Kim
Journal of Pathology and Translational Medicine.2016; 50(2): 138. CrossRef
- Comparison of Analytical and Clinical Performance of HPV 9G DNA Chip, PANArray HPV Genotyping Chip, and Hybrid-Capture II Assay in Cervicovaginal Swabs
- The Usefulness of Cervicovaginal Cytology as a Primary Screening Test.
- Jae Hong Park, Seung Yeon Ha, Hyun Yee Cho, Dong Hae Chung, Na Rae Kim, Sanghui Park
- J Pathol Transl Med. 2008;19(2):107-110.
- DOI: https://doi.org/10.3338/kjc.2008.19.2.107
- 2,942 View
- 15 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - We evaluated the usefulness of cervicovaginal cytology as a primary screening test by analyzing the cytologic and histological diagnoses of 2,254 women. Cervicovaginal cytology had 93.0% sensitivity, 86.1% specificity, 88.2% positive predictive value, and 91.7% of negative predictive value. Cervicovaginal cytology as a primary screening test showed much higher specificity but slightly lower sensitivity than HPV DNA testing. However, the sensitivity of cervicovaginal cytology will be improved continuously due to the development of liquid-based cytology. We regard cervicovaginal cytology as a good primary screening test for cervical intraepithelial neoplasia or carcinoma.
-
Citations
Citations to this article as recorded by- Working Conditions that Impact the Workload of Cytotechnologists: A Study Calculating the Actual Man Power Required
Soo Il Jee, Yong Ho Ahn, Hwa-Jeong Ha, Jeong Eun Kang, Jun Ho Won
The Korean Journal of Clinical Laboratory Science.2021; 53(2): 174. CrossRef
- Working Conditions that Impact the Workload of Cytotechnologists: A Study Calculating the Actual Man Power Required
- Evaluation of Self-collected Pad Sampling for the Detection of HPV In Cervicovaginal Secretion.
- Seong Rim Kim, Sang Yong Song, Dae Shick Kim, Jung Won Lee, Chang Soo Park, Duk Soo Bae, Hyen Ji Lee, Kyung Tae Kim, Oh Joong Kwon, Eun Seop Song, Hee Jae Joo, Gheungwhan Ahn
- Korean J Pathol. 2004;38(4):258-264.
- 2,415 View
- 46 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Self-collection of secretion samples for HPV testing is a feasible alternative method for women who would decline to participate in population based cervical cancer programs. The purpose of this study was to determine the sensitivity and specificity of self-sampling for HPV in determining high grade squamous intraepithelial lesion (HSIL) using the pad, and we also wished to compare the results from samples collected by women themselves and those results from samples collected by physicians.
METHODS
Fifty patients voluntarily participated in the sensitivity and specificity study at the university hospitals and 290 volunteers participated in the agreement study at local clinics. DNA was extracted and amplified using HPV L1 consensus primers for the direct sequencing of the pad samples.
RESULTS
For the detection of HSIL, self-collected pad sampling showed good sensitivity (75.0%) and excellent specificity (100%). Two hundreds eighty-six samples from the pads and concurrent physicians?samples showed the agreement at 98.6% with the Kappa, 0.9622 (p=0.0000).
CONCLUSIONS
A self-sampling method using the pad for the detection of HPV DNA is suggested to be an efficient method to access many women for screening easily, rapidly and conveniently. Testing the pad method? utility for a country- or large area-based mass screening study will be necessary in the future.
- Detection of Human Papillomavirus DNA by In Situ Hybridization using Biotinylated DNA Probes in Cervical Intraepithelial Neoplasias and Squamous Cell Carcinomas.
- Sang Sook Lee, Ki Kwon Kim, Chai Hong Chung, Seung Won Jin, U Ik Sohn
- Korean J Pathol. 1990;24(1):16-26.
- 2,262 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - The authors examined 9 condylomas, 26 cervical intraepithelial neoplasms(CIN) and 22 invasive squamous cell carcinomas for the presence of human papillomavirus(HPV) DNA sequences by DNA-DNA in situ hybridization. In situ hybridization revealed target HPV DNA sequences mostly in the nuclei of the superficial cells from epithelium which contained either maturation or koilocytotic atypias. With the use of biotinylated HPV DNA probes 6/11, 16/18 and 31/33/35, 42 of the 57(73.7%) were positive with HPV-6/11, 23 with HPV-16/18, 32 with HPV-31/33/35 and 18 with two or more mixed probes. HPV-31/33/35 was wht most prevalent in CIN and invasive squamous cell carcinomas, follwed by HPV-16/18. The incidence of HPV DNA increased from 66.7% to 86.4% with increasing severity of the lesions from condylomas to invasive squamous cell carcinomas. Flat condyloma was most freuently accompanied by CIN.
- Expression of ras Oncogene Product, MHC class II Antigen and Human Papillomavirus 16/18 DNA in Carcinomas of the Uterine Cervix.
- K J Cho, Ja June Jang
- Korean J Pathol. 1993;27(5):485-490.
- 1,957 View
- 10 Download
-
 Abstract
Abstract
 PDF
PDF - Immunohistochemical study for ras oncogene product(p21) and MHC class II(HLA-DR) antigen, and in situ hybridization for human papillomavirus(HPV) type 16/18 were performed on 50 squamous cell carcinomas of the uterine cervix. Activated ras and aberrant DR expression were noted in 26 cases(52%) and 11 cases(22%), respectively, without a difference between keratinizing and non-keratinizing types. No direct correlation between ras and DR expression was histologically found. p21 was diffusely distributed with a finely granular pattern in the cytoplasm. Aberrant DR expression was also diffuse, with linear staining along the cell membrane. In situ hybridization revealed HPV type 16/18 DNAs in superficial koilocytotic cells of 4 cases, in which ras or DR expression was not correlated with the presence of HPV DNA.
- Relationship between HPV Infection and bcl-2 Protein Expression and Apoptosis in Invasive and In Situ Squamous Cell Carcinoma of the Uterine Cervix.
- Myoung Ja Chung, Kyu Yun Jang, Woo Sung Moon, Myoung Jae Kang, Dong Geun Lee
- Korean J Pathol. 1999;33(9):702-708.
- 2,289 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - Human papillomavirus (HPV) 16/18 is a causative agent of uterine cervical carcinoma. HPV 16/18 can alter cell cycle regulation through apoptosis. Bcl-2 is an important regulatory gene of apoptosis. A study was done to evaluate the relation between HPV 16/18 and bcl-2 and apoptosis in 21 cases of carcinoma in-situ (CIS), 5 cases of microinvasive carcinoma and 23 cases of invasive squamous cell carcinoma. HPV 16/18 was detected by hybrid capture system (HCS), bcl-2 protein by immunohistochemical method and apoptosis by using the hematoxylin-eosin stained slide. The results were as follows: Expression of the bcl-2 protein was 43% (9/21) in CIS and 26% (6/23) in invasive carcinoma. Expression of the bcl-2 protein was 42% (5/12) in CIS with HPV 16/18 infection, 44% in CIS without HPV 16/18 infection, 20% (2/10) in invasive carcinoma with HPV 16/18 infection and 31% (4/13) in invasive carcinoma without HPV 16/18 infection. Mean apoptotic index (mAI) was 3.36 in CIS, 5.23 in microinvasive and 6.25 in invasive carcinoma. mAI was 3.66 in CIS with HPV 16/18 infection, 2.86 in CIS without HPV 16/18 infection, 6.18 in invasive carcinoma with HPV 16/18 infection and 6.30 in invasive carcinoma without HPV 16/18 infection. Based on these results, we conclude that there are no correlation between HPV infection and bcl-2, and between HPV infection and apoptosis in invasive and in situ carcinoma of the uterine cervix, and apoptosis is increased according to tumor progression.
- Correlation Of Human Papillomavirus Infection and Postmenopausal Squamous Atypia in Cervical Cytology.
- Yi Kyeong Chun, In Gul Moon, Sung Ran Hong, Hye Sun Kim, Jong Sun Choi, Ji Young Park, Jong Sook Park, Tae Jin Kim, Hy Sook Kim
- J Pathol Transl Med. 2004;15(2):81-85.
- 2,276 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - Postmenopausal squamous atypia (PSA) is a phenomenon characterized by cellular alterations mimicking condyloma in the uterine cervix of postmenopausal women. It is not associated with human papillomavirus (HPV) infection. The aim of this study is to correlate findings with HPV infection and the cytohistologic findings of PSA. Eighty-three smears from postmenopausal women, initially interpreted as ASCUS and low-grade squamous intraepithelial lesions(LSIL), were reviewed according to the criteria of PSA. Fifty-eight cases were subsequently reclassified as PSA. Forty cases categorized as PSA were available for HPV-DNA detection by a nested polymerase chain reaction. Eight of these 40 cases(20%) showed biopsy-proven LSIL lesions. The HPV-DNA was detected in 42.5%(17/40), compared to 25%(5/20) of control cases. The HPV-DNA detection rate of biopsy-proven LSIL was 62.5%(5/8). It has been concluded that cytologic differential diagnosis of PSA from LSIL is difficult due to because of poor histologic and viral correlation.
- Polymerase Chain Reaction Analysis of Human Papillomavirus in Esophageal Squamous Cell Carcinoma with its Correlation to p53 mutation.
- Wan Seop Kim, Eun Kyung Hong, In Kyu Kim, Moon Hyang Park, Jung Dal Lee
- Korean J Pathol. 1996;30(11):1018-1026.
- 1,847 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - HPV infection has been implicated strongly in the pathogenesis of human squamous cell carcinoma(SCC). We analysed a series of 28 surgically removed, invasive squamous cell carcinoma of the esophagus by polymerase chain reaction to detect HPV DNA using consensus primers and 8 type-specific primers of HPV (6, 11, 16, 18, 31, 33, 35, 51). HPV 6, 31, 35 or 51 DNA were detected in 20 out of 28 cases (71.4%) of the esophageal SCCs. HPV 51 was the most frequently detected type, occuring in 13 out of 28 cases (46.4%). p53 immunohistochemical staining was also performed to demonstrate any relationship to HPV DNA positivity. It showed positivity in 16 out of 28(57.1%) esophageal SCCs, and HPV DNA and p53 positivity were concurrently detected in 11 out of 28 cases of SCCs. There was no significant inverse relation between HPV DNA positivity and p53 expression(p>0.05). Our results supported HPV involvement in esophageal squamous cell carcinoma, and suggested there may be another pathway not related to the p53-binding pathway in the carcinogenesis of esophageal SCCs by HPV.
- Characterization of Human Papillomavirus Types in Cervical Epithelial Neoplasia by in Situ Hybridization.
- Chan Kum Park, Moon Hyang Park
- Korean J Pathol. 1992;26(5):436-444.
- 1,949 View
- 12 Download
-
 Abstract
Abstract
 PDF
PDF - An in situ DNA hybridization technique was applied to detect human papillomavirus(HPV) DNA, HPV types 6/11 and 16/18, on paraffin sections of 36 cervical condylomatous lesions associated with cervical intraepithelial neoplasia and invasive squamous cell carcinoma. 1) HPV DNA sequences were identified in 14 of 36 cervical condylomatous lesions(39.0%); HPV 6/11 in 7 cases(19.0%) and HPV 16/18 in 7 cases(19.0%). 2) With the use of biotinylated HPV 6/11 DNA probes, 5 of 5 condyloma acuminata(100%), 1 of 5 flat condylomata(20%), and 1 of 7 mild dysplasias(14.3%) were positive. 3) With the use of HPV 16/18 DNA probes, 1 of 7 mild dysplasias(14.3%), 2 of 5 moderate dysplasias(40%), 2 of 4 severe dysplasias(50%), and 2 of 5 invasive squamous cell carcinomas(40%) were positive. 4) The positive stainings to HPV DNA probes were primarily detected in koilocytotic nuclei of the superficial epithelium. No positive signals were found in the normal, dysplastic or carcinoma cells. 5) The numbers positively stained cells were decreased with increasing severity of the lesions from benign condylomas to invasive squamous cell carcinomas. In conclusion, HPV types 6/11 were more commonly identified in benign condylomatous and low grade intraepithelial lesions than high grade lesions. However, HPV types 16/18 were identified in high grade CIN and invasive squamous cell carcinomas. The present results while supporting the concept on HPV 16/18 as the high risk of HPV types in cerivical carcinogenesis also emphasize the applicability of the situ DNA hybridization as a tool in analysis of the specific HPV DNA sequences in routine biopsies of these lesions.

 E-submission
E-submission

 First
First Prev
Prev



