Previous issues
- Page Path
- HOME > Articles and issues > Previous issues
Original Articles
- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
- Agnes Stephanie Harahap, Maria Francisca Ham, Retno Asti Werdhani, Erwin Danil Julian, Rafi Ilmansyah, Chloe Indira Arfelita Mangunkusumso, Tri Juli Edi Tarigan
- J Pathol Transl Med. 2025;59(3):149-160. Published online April 25, 2025
- DOI: https://doi.org/10.4132/jptm.2025.02.19
- 3,480 View
- 183 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Core needle biopsy (CNB) improves diagnostic accuracy by providing precise tissue sampling for histopathological evaluation, overcoming the limitation of inconclusive fine-needle aspiration results. This study evaluated the diagnostic performance of CNB in assessing thyroid nodules, with additional analysis of the benefits of BRAF V600E and RAS Q61R immunohistochemical (IHC) markers.
Methods
This retrospective study enrolled patients with thyroid nodules who underwent CNB at Dr. Cipto Mangunkusumo Hospital, Jakarta, from July 2022 to July 2024. CNB diagnoses were classified using the Korean Thyroid Association Criteria. Diagnostic efficacy was evaluated for neoplastic and malignant lesions, both independently and with BRAF V600E and RAS Q61R IHC. The correlation between nodule size and postoperative diagnosis was also analyzed.
Results
A total of 338 thyroid nodule samples was included, and 52.7% were classified as CNB category II. In the 104 samples with postoperative diagnoses, category IV was the most prevalent (39.4%). CNB demonstrated a sensitivity of 74% and a specificity of 100% for neoplastic lesions and 23.8% sensitivity and 100% specificity for malignant lesions. Combining CNB with BRAF V600E and RAS Q1R IHC increased the sensitivity to 77% for neoplastic lesions and 28.8% for malignant lesions. Larger nodules (>3 cm) were significantly associated with neoplastic (p = .005) and malignant lesions (p = .004).
Conclusions
CNB performs well in identifying neoplastic lesions, with or without BRAF V600E and RAS Q61R IHC, but its low sensitivity for malignant lesions warrants caution. While CNB categories V–VI indicate malignancy, the possibility of malignancy in categories I–IV should not be overlooked.
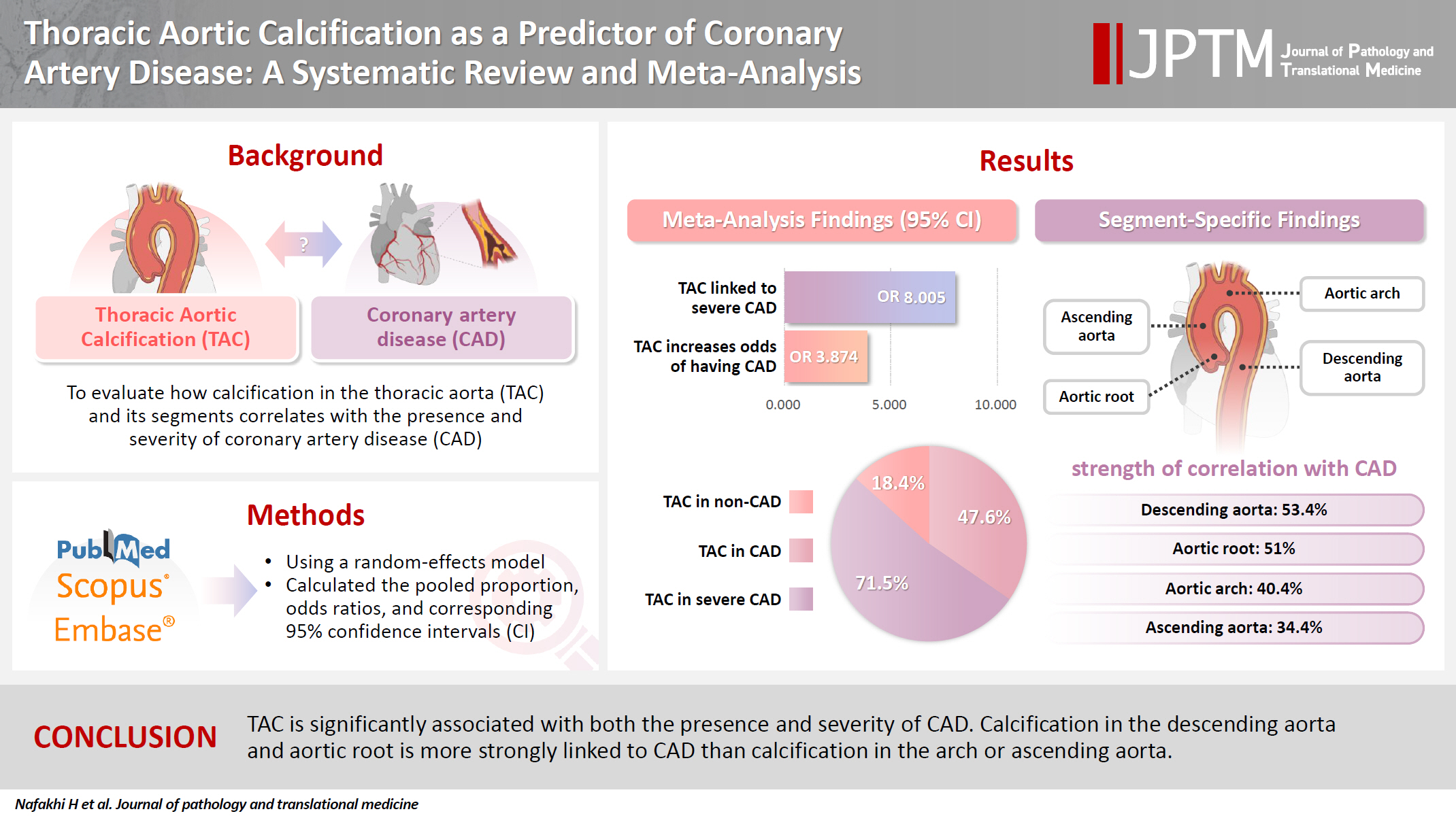
- Thoracic aortic calcification as a predictor of coronary artery disease: a systematic review and meta-analysis
- Hussein Nafakhi, Alaa Salah Jumaah, Akeel Abed Yasseen
- J Pathol Transl Med. 2025;59(3):161-170. Published online April 30, 2025
- DOI: https://doi.org/10.4132/jptm.2025.03.05
- 6,238 View
- 163 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
The relationship between coronary atherosclerosis (progression, outcome) and calcification in the thoracic aorta (TAC), particularly across its various segments, is complex and often shows conflicting associations in the literature. To address this debated and complex relationship, we aimed to evaluate how TAC and its segments correlate with the presence and severity of coronary artery disease (CAD).
Methods
We reviewed all articles published between January 1990 and September 2024 that examined the link between TAC and CAD and were indexed in PubMed, Scopus, or EMBASE. Using a random-effects model, we calculated pooled proportions, odds ratios, and corresponding 95% confidence intervals (CIs) to evaluate the association between TAC and CAD, with consideration of severity.
Results
The study included 17 studies with 8,187 participants, 2,775 of whom had CAD (1,059 with severe CAD), and 5,412 of whom did not. The pooled odds ratio of TAC in patients with CAD compared to that in those without was 3.874 (95% CI, 2.789 to 5.381). For severe CAD versus mild CAD, the odds ratio was 8.005 (95% CI, 2.611 to 24.542). Calcification of the aortic root (pooled proportion, 51%; 95% CI, 0.282 to 0.733) or descending aorta (pooled proportion, 53.4%; 95% CI, 0.341 to 0.718) had the strongest association with CAD compared to calcification of the arch or ascending aorta.
Conclusions
TAC is significantly associated with both the presence and severity of CAD. Calcification in the descending aorta and aortic root is more strongly linked to CAD than calcification in the arch or ascending aorta. -
Citations
Citations to this article as recorded by- International Liver Transplantation Society/Liver Intensive Care Group of Europe guidelines for cardiovascular assessment before liver transplantation
Emmanuel Weiss, Gonzalo Crespo, Alexandra Anderson, Gianni Biancofiore, Ryan Chadha, Jacek B. Cywinski, Andrea De Gasperi, James Findlay, Marc Giménez-Milà, Constantine Karvellas, Michael Kaufman, Ashish Malik, Marina Moguilevitch, Sher-Lu Pai, Koen Reynt
American Journal of Transplantation.2025;[Epub] CrossRef
- International Liver Transplantation Society/Liver Intensive Care Group of Europe guidelines for cardiovascular assessment before liver transplantation
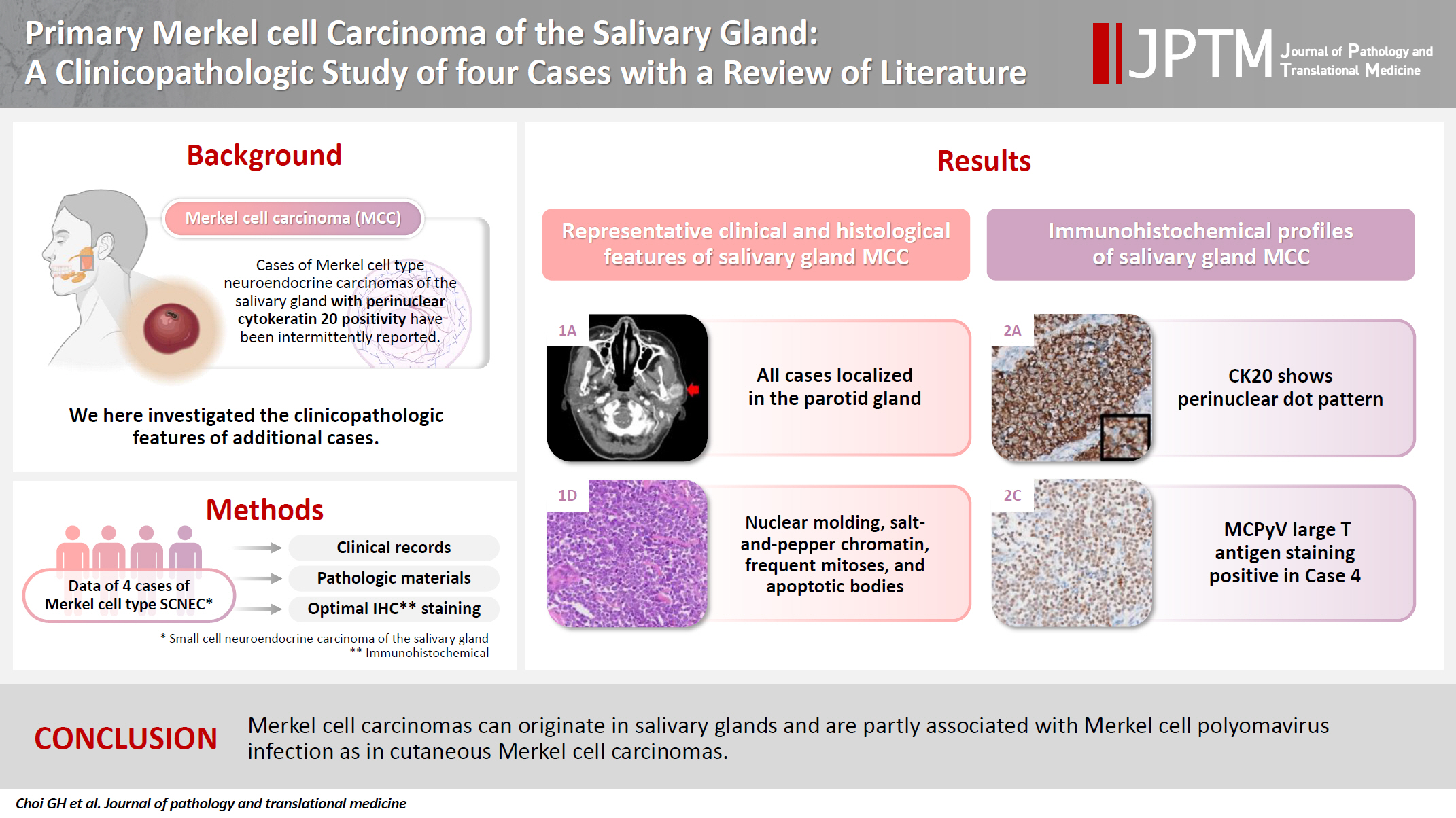
- Primary Merkel cell carcinoma of the salivary gland: a clinicopathologic study of four cases with a review of literature
- Gyuheon Choi, Joon Seon Song, Hee Jin Lee, Gi Hwan Kim, Young Ho Jung, Yoon Se Lee, Kyung-Ja Cho
- J Pathol Transl Med. 2025;59(3):171-179. Published online April 30, 2025
- DOI: https://doi.org/10.4132/jptm.2025.03.25
- 3,381 View
- 151 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Primary Merkel cell carcinoma of the salivary gland is currently not listed in the World Health Organization classification. However, cases of Merkel cell type neuroendocrine carcinomas of the salivary gland with perinuclear cytokeratin 20 positivity have been intermittently reported. We here investigated the clinicopathologic features of additional cases.
Methods
Data of four cases of Merkel cell type small cell neuroendocrine carcinoma of the salivary gland were retrieved. To confirm the tumors’ primary nature, clinical records and pathologic materials were reviewed. Optimal immunohistochemical staining was performed to support the diagnosis.
Results
All tumors were located in the parotid gland. Possibilities of metastasis were excluded in all cases through a meticulous clinicopathological review. Tumor histology was consistent with the diagnosis of small cell neuroendocrine carcinoma. Tumors’ immunohistochemical phenotypes were consistent with Merkel cell carcinoma, including Merkel cell polyomavirus large T antigen positivity in two of the four cases.
Conclusions
Merkel cell carcinomas can originate in salivary glands and are partly associated with Merkel cell polyomavirus infection as in cutaneous Merkel cell carcinomas. -
Citations
Citations to this article as recorded by- Parotid intranodal metastasis of Merkel cell carcinoma: a rare case report
Tong Gao, Dengshun Wang, Hongwei Yu, Yu’e Wang, Haibin Lu
BMC Oral Health.2025;[Epub] CrossRef
- Parotid intranodal metastasis of Merkel cell carcinoma: a rare case report
- Diagnostic yield of fine needle aspiration with simultaneous core needle biopsy for thyroid nodules
- Mohammad Ali Hasannia, Ramin Pourghorban, Hoda Asefi, Amir Aria, Elham Nazar, Hojat Ebrahiminik, Alireza Mohamadian
- J Pathol Transl Med. 2025;59(3):180-187. Published online April 16, 2025
- DOI: https://doi.org/10.4132/jptm.2025.03.04
- 9,519 View
- 219 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Fine needle aspiration (FNA) is a widely utilized technique for assessing thyroid nodules; however, its inherent non-diagnostic rate poses diagnostic challenges. The present study aimed to evaluate and compare the diagnostic efficacy of FNA, core needle biopsy (CNB), and their combined application in the assessment of thyroid nodules.
Methods
A total of 56 nodules from 50 patients was analyzed using both FNA and simultaneous CNB. The ultrasound characteristics were categorized according to the American College of Radiology Thyroid Imaging Reporting and Data Systems classification system. The study compared the sensitivity, specificity, and accuracy of FNA, CNB, and the combination of the two techniques.
Results
The concordance between FNA and CNB was notably high, with a kappa coefficient of 0.837. The sensitivity for detecting thyroid malignancy was found to be 25.0% for FNA, 66.7% for CNB, and 83.3% for the combined FNA/CNB approach, with corresponding specificities of 84.6%, 97.4%, and 97.4%. The accuracy of the FNA/CNB combination was the highest at 94.1%.
Conclusions
The findings of this study indicate that both CNB and the FNA/CNB combination offer greater diagnostic accuracy for thyroid malignancy compared to FNA alone, with no significant complications reported. Integrating CNB with FNA findings may enhance management strategies and treatment outcomes for patients with thyroid nodules.
Case Studies
- Histopathological characteristics of Epstein-Barr virus (EBV)–associated encephalitis and colitis in chronic active EBV infection
- Betty A Kasimo, James J Yahaya, Sun Och Yoon, Se Hoon Kim, Minsun Jung
- J Pathol Transl Med. 2025;59(3):188-194. Published online April 16, 2025
- DOI: https://doi.org/10.4132/jptm.2025.02.21
- 3,786 View
- 161 Download
-
 Abstract
Abstract
 PDF
PDF - Chronic active Epstein-Barr virus (CAEBV) can induce complications in various organs, including the brain and gastrointestinal tract. A 3-year-old boy was referred to the hospital with a history of fever and seizures for 15 days. A diagnosis of encephalitis based on computed tomography (CT) and magnetic resonance imaging findings and clinical correlation was made. Laboratory tests showed positive serology for Epstein-Barr virus (EBV) and negative for Rotavirus antigen and IgG and IgM antibodies for cytomegalovirus, herpes simplex virus, and varicella zoster virus, respectively. Abdominal CT showed diffuse wall thickening with fluid distension of small bowel loops, lower abdomen wall thickening, and a small amount of ascites. The biopsy demonstrated positive Epstein-Barr encoding region in situ hybridization in cells within the crypts and lamina propria. The patient was managed with steroids and hematopoietic stem cell transplantation (HSCT). This case showed histopathological characteristics of concurrent EBV-associated encephalitis and colitis in CAEBV infection. The three-step strategy of immunosuppressive therapy, chemotherapy, and allogeneic HSCT should be always be considered for prevention of disease progression.
- Cytological features of atypical adenomatous hyperplasia and adenocarcinoma in situ of the lung: a case report
- Misa Takahashi, Seiya Homma, Chisato Setoguchi, Yoko Umezawa, Atsuhiko Sakamoto
- J Pathol Transl Med. 2025;59(3):195-200. Published online May 9, 2025
- DOI: https://doi.org/10.4132/jptm.2025.04.09
- 3,696 View
- 124 Download
-
 Abstract
Abstract
 PDF
PDF - Atypical adenomatous hyperplasia (AAH) and adenocarcinoma in situ (AIS) are generally treated as different lesions, depending on the differences in lesion size and histological findings. However, these differences are not absolute; thus, AAH and AIS are often difficult to distinguish. Moreover, whether AAH and AIS can be regarded as different lesions remains unknown because cytological specimens, especially those of AAH, are rare. In this study, we examined these uncommon cytological specimens and compared the cytological findings between AAH and AIS. We observed many common cytological features with no obvious differences between AAH and AIS. These findings suggest that these two distinct lesions can be grouped into a single category. Therefore, we propose creating a new cytological category.
Correspondence
- Erratum: Diagnostic challenges in the assessment of thyroid neoplasms using nuclear features and vascular and capsular invasion: a multi-center interobserver agreement study
- Agnes Stephanie Harahap, Mutiah Mutmainnah, Maria Francisca Ham, Dina Khoirunnisa, Abdillah Hasbi Assadyk, Husni Cangara, Aswiyanti Asri, Diah Prabawati Retnani, Fairuz Quzwain, Hasrayati Agustina, Hermawan Istiadi, Indri Windarti, Krisna Murti, Muhammad Takbir, Ni Made Mahastuti, Nila Kurniasari, Nungki Anggorowati, Pamela Abineno, Yulita Pundewi Setyorini, Kennichi Kakudo
- J Pathol Transl Med. 2025;59(3):201-201. Published online March 31, 2025
- DOI: https://doi.org/10.4132/jptm.2024.07.25.r
- Corrects: J Pathol Transl Med 2024;58(6):299
- 2,285 View
- 56 Download

 E-submission
E-submission







 First
First Prev
Prev



