Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(1); 2012 > Article
-
Case Report
Metaplastic Thymoma: Report of 4 Cases - Guhyun Kang, Nara Yoon, Joungho Han, Young Eun Kim, Tae Sung Kim1, Kwhanmien Kim2
-
Korean Journal of Pathology 2012;46(1):92-95.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.1.92
Published online: February 23, 2012
Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
2Department of Thoracic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- Corresponding Author: Joungho Han, M.D. Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, 50 Irwon-dong, Gangnam-gu, Seoul 135-710, Korea. Tel: +82-2-3410-2800, Fax: +82-2-3410-0025, hanjho@skku.edu
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Metaplastic thymoma (MT), accepted in the World Health Organization 2004 scheme, is a circumscribed tumor of the thymus exhibiting biphasic morphology. We herein describe the clinicopathologic features of four MTs and the differential diagnoses of this unusual tumor. There were three women and one man with mean age of 49.5 years. The patients were found to have mediastinal masses, and underwent surgical excision. One exhibited symptoms of myasthenia gravis, and the serum titer for anti-acetylcholine receptor antibody was positive. Grossly, the tumors were encapsulated, and showed vaguely multinodular, solid, tan-white to yellow cut surfaces. Histologically, they comprised epithelial islands intertwining with bundles of delicate spindle cells. The patients remained well after surgical excision at 5-55 months. Because of the distinctive histological appearance and benign clinical course, MT should be distinguished from other more aggressive mediastinal neoplasms displaying biphasic feature.
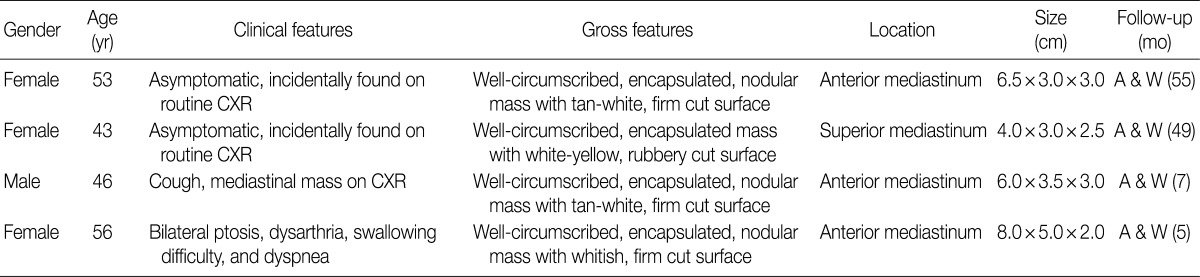
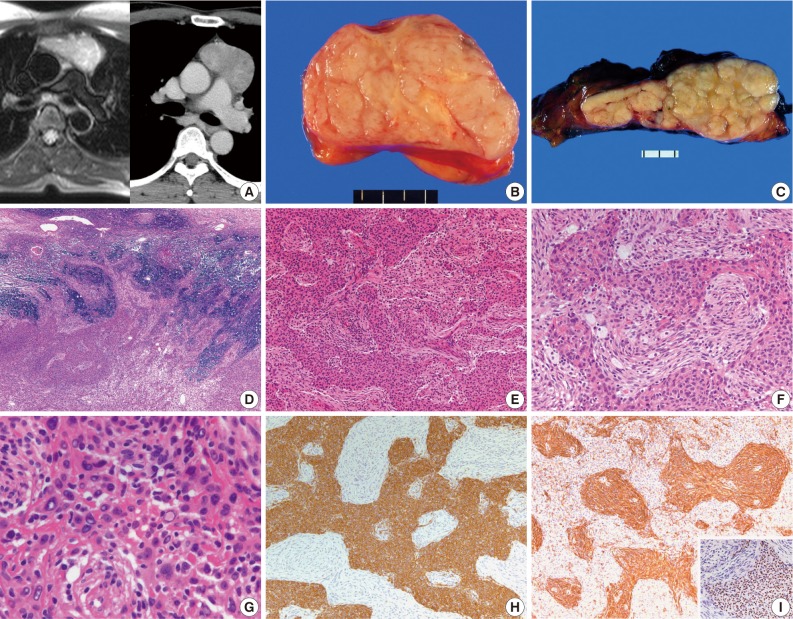
- The clinicopathologic features of 4 patients are summarized in Table 1. There were 3 women and one man, and the mean age of diagnosis was 49.5 years. Two patients were asymptomatic, and one, who had smoked for 10 pack-years, complained of cough. A 56-year-old woman had manifested the symptoms of MG, such as ptosis, dysarthria and difficulty in swallowing, and the serum level of anti-acetylcholine receptor antibody was 12.52 nmol/L. The patients were found to have an anterior or superior mediastinal mass on routine chest radiograph, and were further evaluated with computed tomography or magnetic resonance imaging (Fig. 1A). None of the patients had other autoimmune disorders and clinical evidence of tumor elsewhere. The masses were treated with complete surgical excision. All the patients were alive and well without local recurrence at 5-55 months.
- The tumors were variably encapsulated, and measured 4.0-8.0 cm in the greatest diameter. The cut surfaces were vaguely multinodular, firm or rubbery and tan-white to yellow (Fig. 1B, C). All the cases revealed essentially similar histologic features. They were well circumscribed with a thin rim of residual thymic tissue in the peripheral portions. One case showed focal invasion of the surrounding thymic tissue (Fig. 1D). The tumors were composed of anastomosing islands or broad trabeculae of epithelial cells disposed among delicate spindle cells (Fig. 1E). The two components were sharply delineated or gradually merged, and were present in variable proportions from area to area (Fig. 1F). The epithelial cells were oval to polygonal with vesicular nuclei and small prominent nucleoli. Some of the cells exhibited enlarged hyperchromatic or empty-looking nuclei, but mitotic figure was not observed in 30 consecutive high-power fields (Fig. 1G). The spindle cells showed a short fascicular or storiform growth pattern, and were bland-looking with fine nuclear chromatin and bipolar processes. Immunohistochemically, the epithelial cells were strongly positive for cytokeratin (1:130, clone AE1/AE3, Dako, Carpinteria, CA, USA) and p63 protein (1:400, clone 4A4, Dako), and were negative for vimentin (1:200, clone Vim 3B4, Dako). While the spindle cells were strongly positive for viementin, and were negative or focally, weakly positive for cytokeratin (Fig. 1H, I).
CASE REPORTS
- MT has been reported in the literatures under the designations 'thymoma with pseudosarcomatous stroma,' 'low-grade metaplastic carcinoma' or 'biphasic thymoma, mixed polygonal and spindle cell type'.7 Suster et al.5 suggested that the spindle cell component was reactive fibroblastic/myofibroblastic cells rather than the neoplastic proliferation of stromal elements arising from connective tissue in the thymus. On the other hand, Yoneda et al.4 considered the spindle cell component, which gradually merged with the epithelial islands at least at some foci, to be a deviation of the neoplastic precursor (i.e., mesenchymal metaplasia of tumor cells), and suggested both components arose from the same stem cells with the capacity of multidirectional differentiation.
- All cases in our series had been submitted for intraoperative frozen section evaluation, and the diagnosis was rendered as 'consistent with MT.' Grossly, the tumors were well-circumscribed or encapsulated, and lacked distinct fibrous septation or cystic change that can be seen in conventional thymomas. Some areas showed marked predominance of one component to the exclusion of the other. If only areas composed of spindle cells are sampled, the constituent cells can mimic those of a type A thymoma.6 A diagnosis of such cases can be made by additional section to identify the typical biphasic pattern. The epithelial cells form lobules that are separated by acellular fibrous band in type B thymomas, while the epithelial component is intertwined with spindle cells and small amounts of loose collagenous tissue in MTs. Despite some epithelial cells exhibit enlarged atypical nuclei and may be similar to those of type B3 thymoma, MTs lack the perivascular spaces.4,5 The differential diagnosis of biphasic thymic tumor includes biphasic mesothelioma, synovial sarcoma, teratoma and ectopic hamartomatous thymoma (EHT). It is noteworthy that EHT is a benign tumor of the lower neck showing an admixture of epithelial islands with spindle and adipose cells. This tumor is not deep-seated, and cytokeratin is positive in both epithelial and spindle cell component with at least focal glandular differentiation.10-12 In contrast to EHT, MT exhibits alternating areas of epithelial and spindle cell component, which is highlighted by immunostaining for cytokeratin and vimentin, respectively.
- The age range of reported MTs was 28 to 71 years (mean, 50.9 years), and the tumor tended to prevail in men.4,5,7 In our series, the male to female ratio was 1:3 with mean age of 49.5 years (range, 43 to 56 years). It seems that MT usually occurs in adult patients of both genders as thymomas and thymic carcinomas.7 Molecular studies on a limited number of cases have shown few genetic alterations, and favor interpretation of this tumor as a thymoma.7 However, MG and paraneoplastic autoimmune phenomena that are common in other types of thymoma have not been observed in MTs. All the 4 tumors had the same histologic and immunohistochemical features as other cases described in the literatures, but one of the patients reported herein was associated with MG, further supporting a closer relationship with thymoma than with thymic carcinoma. MT differs from SC in showing good circumscription and bland-looking spindle cells, even though squamoid epithelial islands may show nuclear polymorphism.4,5 Recently, 2 cases of SC arising in MT have been reported.8,9 The tumors had foci with marked atypical spindle cells, frequent mitotic figures and necrosis, but the follow-up was too short to assess behavior. Only one patient with MT was reported to have developed local recurrence at 14 months, and died at 6 years.4-6,8,9
- We report 4 cases of an unusual morphologic variant of thymoma, characterized by a biphasic epithelial and spindle cell morphology. Because of the distinctive histologic appearance and indolent clinical behavior, MT should be distinguished from other more aggressive mediastinal neoplasms which display a biphasic pattern.
DISCUSSION
- 1. Strobel P, Marx A, Zettl A, Müller-Hermelink HK. Thymoma and thymic carcinoma: an update of the WHO Classification 2004. Surg Today 2005; 35: 805-811. ArticlePubMedPDF
- 2. Suster S, Rosai J. Thymic carcinoma: a clinicopathologic study of 60 cases. Cancer 1991; 67: 1025-1032. ArticlePubMed
- 3. Suster S. Thymic carcinoma: update of current diagnostic criteria and histologic types. Semin Diagn Pathol 2005; 22: 198-212. ArticlePubMed
- 4. Yoneda S, Marx A, Heimann S, Shirakusa T, Kikuchi M, Müller-Hermelink HK. Low-grade metaplastic carcinoma of the thymus. Histopathology 1999; 35: 19-30. ArticlePubMedPDF
- 5. Suster S, Moran CA, Chan JK. Thymoma with pseudosarcomatous stroma: report of an unusual histologic variant of thymic epithelial neoplasm that may simulate carcinosarcoma. Am J Surg Pathol 1997; 21: 1316-1323. ArticlePubMed
- 6. Noh TW, Kim SH, Lim BJ, Yang WI, Chung KY. Thymoma with pseudosarcomatous stroma. Yonsei Med J 2001; 42: 571-575. ArticlePubMed
- 7. Travis WD, Brambilla E, Müller-Hermelink HK, Harris CC. Pathology and genetics of tumours of the lung, pleura, thymus and heart. 2004; Lyon: IARC Press, 152-181.
- 8. Lu HS, Gan MF, Zhou T, Wang SZ. Sarcomatoid thymic carcinoma arising in metaplastic thymoma: a case report. Int J Surg Pathol 2011; 19: 677-680. ArticlePubMedPDF
- 9. Moritani S, Ichihara S, Mukai K, et al. Sarcomatoid carcinoma of the thymus arising in metaplastic thymoma. Histopathology 2008; 52: 409-411. ArticlePubMed
- 10. Fetsch JF, Laskin WB, Michal M, et al. Ectopic hamartomatous thymoma: a clinicopathologic and immunohistochemical analysis of 21 cases with data supporting reclassification as a branchial anlage mixed tumor. Am J Surg Pathol 2004; 28: 1360-1370. PubMed
- 11. Rosai J, Limas C, Husband EM. Ectopic hamartomatous thymoma: a distinctive benign lesion of lower neck. Am J Surg Pathol 1984; 8: 501-513. PubMed
- 12. Roth JA, Enzinger FM, Tannenbaum M. Synovial sarcoma of the neck: a followup study of 24 cases. Cancer 1975; 35: 1243-1253. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Giant Metaplastic Thymoma With Extensive Calcification
Keisuke Todoroki, Satoshi Kawakami, Keiya Nagata, Kentaro Miura, Momoko Takizawa, Yasunari Fujinaga
Journal of Thoracic Imaging.2025;[Epub] CrossRef - A Rare Case of Metaplastic Thymoma Presenting With Myasthenia Gravis
Ilianne Vega Prado, John Shymansky, Anisha Apte, Keith Mortman, Henry J. Kaminski, Stephanie Barak
International Journal of Surgical Pathology.2024; 32(1): 155. CrossRef - Thymic epithelial tumours: histopathological classification and differential diagnosis
Jan von der Thüsen
Histopathology.2024; 84(1): 196. CrossRef - Epigenetics of Thymic Epithelial Tumors
Vanessa Nicolì, Fabio Coppedè
Cancers.2023; 15(2): 360. CrossRef - Expanding the Clinicopathologic Spectrum of YAP1::MAML2–Rearranged Thymic Neoplasm
Eric Eunshik Kim, Ye Yoon Suh, Sang Won Lee, Jeong Mo Bae, Kyoungbun Lee, Sungyoung Lee, Hongseok Yun, Kyeong Cheon Jung, Jiwon Koh
Modern Pathology.2023; 36(2): 100048. CrossRef -
Significance of
YAP1–MAML2
rearrangement and
GTF2I
mutation in the diagnosis and differential diagnosis of metaplastic thymoma
Minghao Wang, Hongtao Xu, Qiang Han, Liang Wang
Annals of Medicine.2023;[Epub] CrossRef - Loss of YAP1 C‐terminus expression as an ancillary marker for metaplastic thymoma: a potential pitfall in detecting YAP1::MAML2 gene rearrangement
Xuan Wang, Lei‐lei Liu, Qing Li, Qiu‐yuan Xia, Rui Li, Sheng‐bing Ye, Ru‐song Zhang, Ru Fang, Hui Chen, Nan Wu, Qiu Rao
Histopathology.2023; 83(5): 798. CrossRef - A Case of Metaplastic Thymoma
Ryoichi TAKENAKA, Kenji NEZU, Daijiro TAKEMOTO, Tatsuya HAYASHI, Hisato YAMAMOTO, Shoichi MATSUKAGE
Nihon Rinsho Geka Gakkai Zasshi (Journal of Japan Surgical Association).2023; 84(4): 538. CrossRef - Malignant Transformation of Metaplastic Thymoma into High-Grade Sarcomatoid Carcinoma: A Case Report
Zheng Hua Piao, Jin Ping Chen, Hai Ren Chen, Xin Cheng Zhou
International Journal of Surgical Pathology.2022; 30(5): 564. CrossRef - YAP1-MAML2 Fusion as a Diagnostic Biomarker for Metaplastic Thymoma
Jikai Zhao, Ruiying Zhao, Chan Xiang, Jinchen Shao, Lianying Guo, Yuchen Han
Frontiers in Oncology.2021;[Epub] CrossRef - Metaplastic thymoma: a distinctive thymic neoplasm characterized by YAP1-MAML2 gene fusions
Marina Vivero, Phani Davineni, Valentina Nardi, John K.C. Chan, Lynette M. Sholl
Modern Pathology.2020; 33(4): 560. CrossRef - Metaplastic thymoma: Report of two cases
Yoshikazu Shinohara, Mariko Tanaka, Kentaro Kitano, Kazuhiro Nagayama, Masaaki Sato, Jun Nakajima
The Journal of the Japanese Association for Chest Surgery.2020; 34(7): 733. CrossRef - Type AB thymoma is not a mixed tumor of type A and type B thymomas, but a distinct type of thymoma
Yukari Miki, Kana Hamada, Tadashi Yoshino, Katsuya Miyatani, Kiyoshi Takahashi
Virchows Archiv.2014; 464(6): 725. CrossRef - Potential Role of Adjuvant Radiation Therapy in Cervical Thymic Neoplasm Involving Thyroid Gland or Neck
Jae Myoung Noh, Sang Yun Ha, Yong Chan Ahn, Dongryul Oh, Seung Won Seol, Young Lyun Oh, Joungho Han
Cancer Research and Treatment.2014; 47(3): 436. CrossRef - A Case of Metaplastic Thymoma
Eiji MIYAHARA, Tomoko ITAGAKI, Masaki KUWAHARA, Akira KAMEDA, Yoshihiro MIYATA, Kazuhiro SENTANI, Wataru YASUI
Nihon Rinsho Geka Gakkai Zasshi (Journal of Japan Surgical Association).2014; 75(2): 360. CrossRef
 PubReader
PubReader-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
- Related articles
Fig. 1
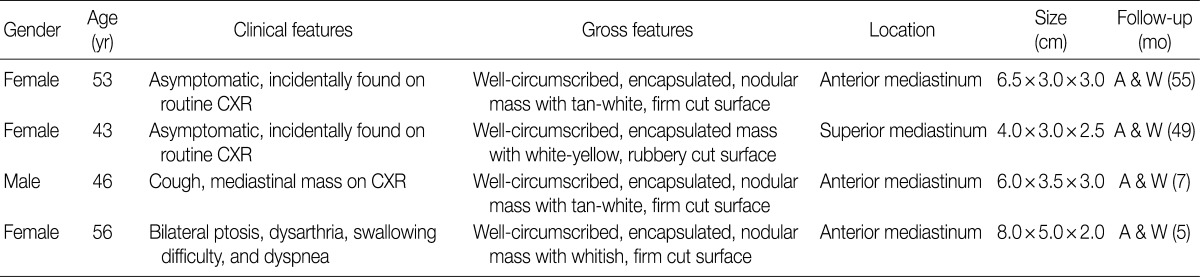
CXR, chest x-ray; A & W, alive and well with no disease.

 E-submission
E-submission