Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(1); 2012 > Article
-
Case Report
Mimicry of Minute Pulmonary Meningothelial-like Nodules to Metastatic Deposits in a Patient with Infiltrating Lobular Carcinoma: A Case Report and Review of the Literature - Hala Kfoury, Maria A. Arafah, Maha M. Arafah, Sami Alnassar1, Waseem Hajjar1
-
Korean Journal of Pathology 2012;46(1):87-91.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.1.87
Published online: February 23, 2012
Department of Pathology, College of Medicine, King Saud University, Riyadh, Saudi Arabia.
1Department of Surgery, Division of Thoracic Surgery, College of Medicine, King Saud University, Riyadh, Saudi Arabia.
- Corresponding Author: Maria A. Arafah, M.D. Department of Pathology, College of Medicine, King Saud University, P.O. Box 2925, Riyadh 11461, Saudi Arabia. Tel: +966-14670862, Fax: +966-14671888, marafah83@gmail.com
• Received: August 23, 2011 • Revised: September 22, 2011 • Accepted: September 29, 2011
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Minute pulmonary meningothelial-like nodules (MPMNs) are incidentally found lesions in lung resection specimens and autopsies. MPMNs have been associated with neoplastic and non-neoplastic pulmonary conditions and occasionally with extrapulmonary diseases. We report a case of a female patient presenting with invasive lobular carcinoma of the breast and MPMNs, masquerading as metastatic deposits. We describe the morphological, immunohistochemical and ultrastructural features of MPMNs and emphasize the importance of their recognition for proper staging and treatment of patients. To our knowledge, this is the first case in the English literature describing this coexistence.
- A 65-year-old diabetic and hypertensive female patient was referred to our hospital for an open lung excisional biopsy for nodules in the right lower and middle lobes. The patient had a history of a recently recognized right breast mass. She had a positive family history of breast cancer and a 30-year history of regular smoking. The patient had a firm, ill-defined, 2-cm mass in the upper inner quadrant of her right breast on physical examination. A trucut biopsy was taken from the breast mass and a diagnosis of infiltrating lobular carcinoma (ILC) was rendered.
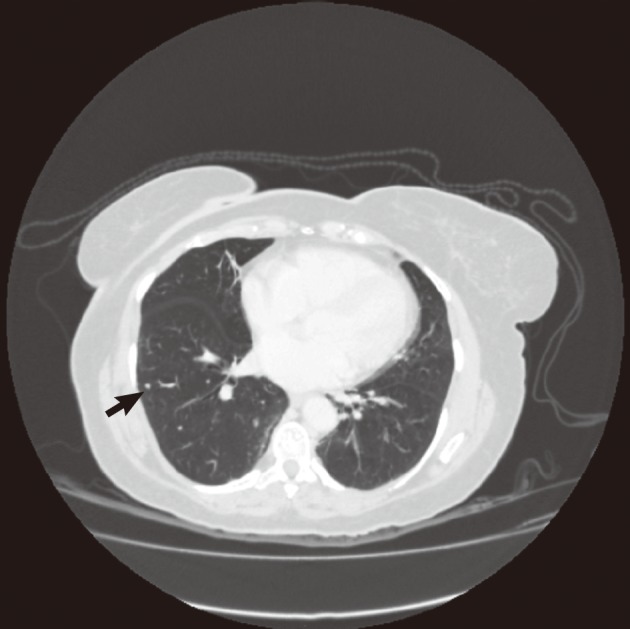
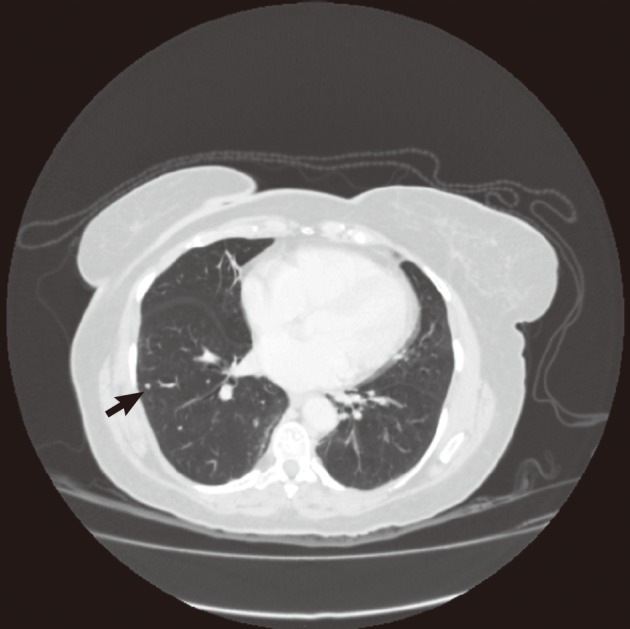
- As part of the staging work-up, the patient underwent a thin-section computed tomography (CT) scan of the chest, abdomen, and pelvis. The chest-CT images showed two small ground-glass opacities; one in the middle lobe and the other in the lower lobe of the right lung (Fig. 1). The radiological findings were nonspecific; thus, metastasis from a primary breast malignancy was suspected, and she was referred to our institution for further investigation. The patient underwent a coil-localization excision of both right lung nodules under general anesthesia.
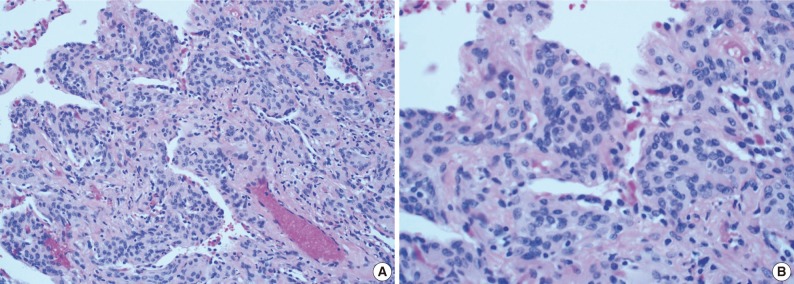
- Two lung wedge biopsies were obtained. Minute nodules (the largest measuring 0.4 cm) comprising nests of cells in a "zellballen"-like arrangement were seen microscopically in both specimens. The nests were either centered around small veins or located within the pulmonary interstitium. These nests consisted of oval to epithelioid cells with a pale eosinophilic cytoplasm and indistinct cellular borders (Fig. 2A). Nuclei were round to oval, uniform, and centrally located. The nuclei showed a fine granular chromatin pattern, occasional nuclear pseudoinclusions and inconspicuous nucleoli (Fig. 2B). No mitotic figures were present.
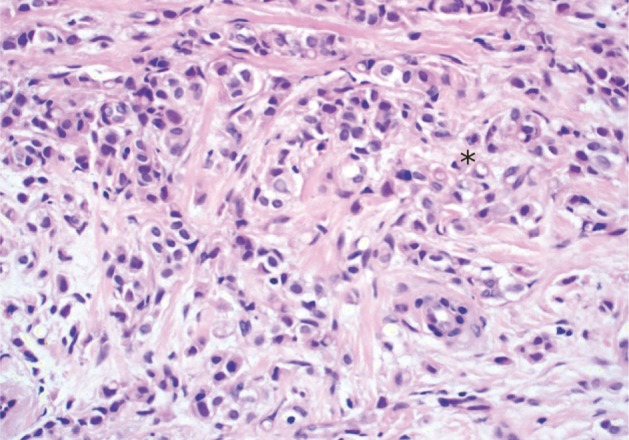
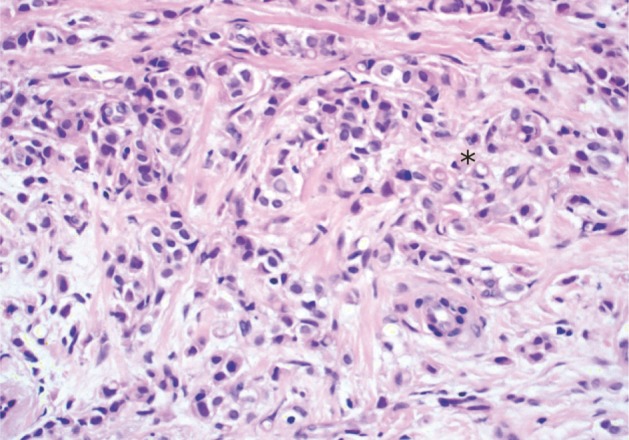
- The outside slides of the breast trucut biopsy were reviewed. These sections showed linear arrangements and individual scattered cells invading the breast stroma and the peripheral adipose tissue. The cells were round to polyhedral with hyperchromatic pleomorphic nuclei. The nuclei frequently acquired an eccentric position caused by intracytoplasmic mucin droplets (Fig. 3).
- Compared with the sections from the lung wedge biopsies, the histological features were distinctly different with prominent discohesiveness of the carcinoma cells, whereas the cells of the lung lesions attempted to form whorls with finely dispersed nuclear chromatin and no intracytoplasmic mucin deposition.
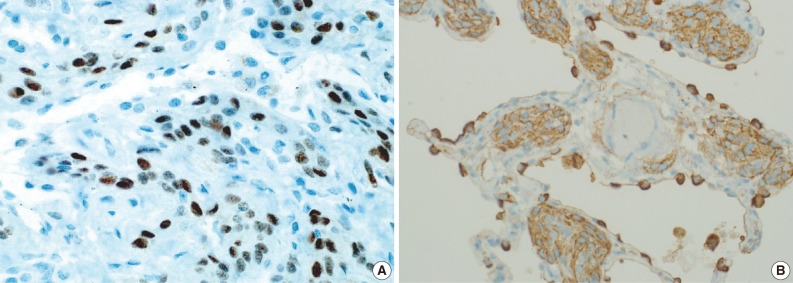
- In addition to hematoxylin and eosin slides, sections were cut and prepared for immunohistochemical analysis using Benchmark, Ventana (Tucson, AZ, USA). The nesting cells showed strong cytoplasmic positivity to vimentin (ready to use, mouse monoclonal, Novocastra, Newcastle, UK), strong membranous positivity to E-cadherin (1:25, mouse monoclonal, Novocastra), moderate membranous positivity to epithelial membrane antigen (EMA; ready to use, mouse monoclonal, Novocastra) (Fig. 4A) and moderate to strong nuclear positivity to progesterone receptor (PR; ready to use, mouse monoclonal, Novocastra) in approximately 80% of the cells (Fig. 4B). The cells were negative for neuroendocrine, vascular, melanocytic, and other epithelial markers. They were also negative for estrogen receptor, human epidermal growth factor receptor 2, and GCDFP15. The diagnosis of MPMNs was established, and no evidence of metastatic carcinoma was observed in either specimen.
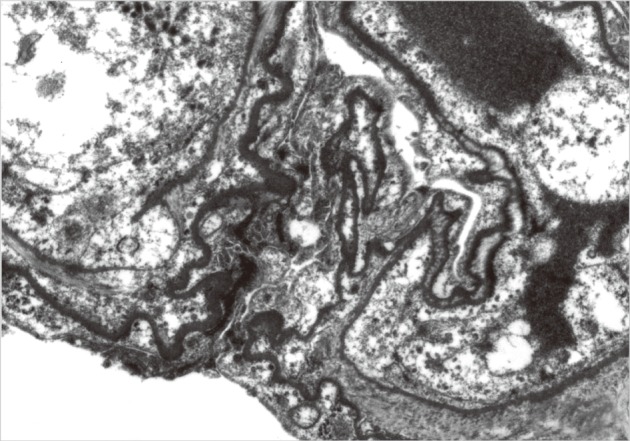
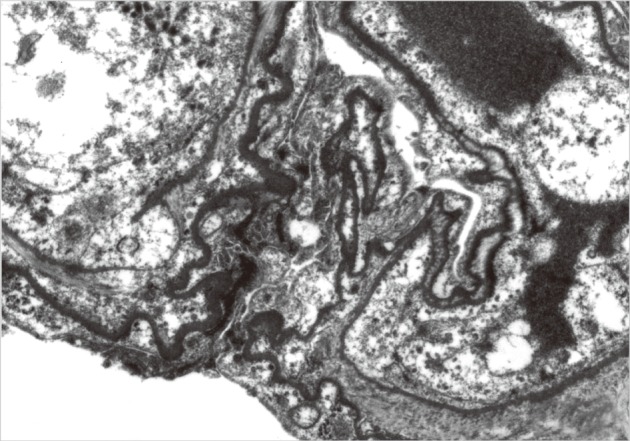
- Tissue from the paraffin-embedded blocks was retrieved and reprocessed for electron microscopy. Ultrastructural features included interdigitating cellular junctions, desmosomes and scattered intracytoplasmic filaments (Fig. 5).
- The thoracoscopy procedure was complicated by a small pneumothorax, which was managed by inserting a right chest tube for 3 days. The patient was discharged on the day 4 post-operatively to be followed up at the oncology clinic of the referring hospital.
CASE REPORT
- In 1960, Korn et al.1 described minute, occasionally multiple tumors composed of nests of epithelioid cells related to anastomosing pulmonary venules. In view of the architectural pattern of the nests, the cytological similarity to carotid body tumors, and the relationship to vessels, these lesions were classified as "pulmonary chemodectomas."1 Subsequently, they were found to lack the immunohistochemical and ultrastructural features of neuroendocrine cells and they rather resembled meningothelial cells. Accordingly, the term "pulmonary chemodectomas" was changed to "minute meningothelial-like nodules," which was proposed by Gaffey et al.2 in 1988.
- MPMNs are often identified as incidental findings in histopathological lung sections or in high-resolution CT scans conducted for unrelated causes. They appear as small persistent attenuated ground-glass opacities radiologically.3 Such findings are nonspecific and raise the probability of metastatic deposits particularly in patients with previously diagnosed primary tumors.4 To our knowledge, our case is the first in the English literature to describe the simultaneous occurrence of MPMNs in a patient with a primary breast lobular carcinoma masquerading as metastatic nodules.
- The microscopic features of our case were compatible with the classic description of MPMNs. They comprised small nests of cells arranged in a "zellballen" pattern around venules within the lung interstitium, although Mukhopadhyay et al.5 showed that half of their studied cases lacked this relationship to venules or other small blood vessels. The cells were epithelioid with pale eosinohpilic cytoplasm. Nuclei were oval with finely granulated chromatin and small or absent nucleoli. The ultrastructural composition (complex interdigitating cell processes connected by desmosomes, occasional cytoplasmic filaments, and the absence of dense-core neurosecretory granules) and the immunohistochemical profile (immunoreactivity to vimentin, EMA, and PR) were consistent with previous findings. Notably, the PR nuclear positivity emphasized the resemblance of MPMNs to arachnoid cells and a role for sex-steroid hormones in their development and growth.6
- MPMNs are most frequent in the sixth decade and reveal a female predominance.1-4,6-12 These lesions are absent in fetuses, infants, and children, indicating that they do not represent congenital rests.5 Patients are usually asymptomatic, as MPMNs run a benign course of which surgical excision is curative. Niho et al.10 analyzed the clonality of 11 MPMNs in two female patients based on an X chromosome-linked polymorphic marker and reported that these lesions were nonclonal cell aggregations. Although the histogenesis of MPMNs is still uncertain, the results of this genetic analysis suggest a reactive rather than a neoplastic origin.10
- The rate of detecting MPMNs varies depending on the source of the lung tissue examined. Detection ranges from 0.07% to 4.9% in autopsy specimens,1,2,7,11 in comparison to 7% to 13.8% in surgically resected specimens.9,10
- MPMNs have been associated with a variety of conditions. The strongest association has been in patients with pulmonary thromboembolism and respiratory bronchiolitis-associated interstitial lung disease/desquamative interstitial pneumonia.7,11 Additionally, associations with atypical adenomatous hyperplasia and congestive heart failure have been suggested.1,7,9 Several studies have shown an association with neoplasia, particularly pulmonary adenocarcinoma, with MPMNs occurring in up to 10% of patients.8-10 The association of MPMNs with breast carcinoma has never been described in the English literature. Invasive lobular carcinoma represents up to 14% of all invasive breast cancers13 and is the second most common type of breast cancer (4.9%) in Saudi women according to the National Cancer Registry Report, 2004.14 The ILC classification includes: the classic, solid, alveolar, apocrine/histiocytoid, pleomorphic and tubulolobular variants.15 Cells of all subtypes are characteristically discohesive and show variable degrees of nuclear pleomorphism and atypia,15 in contrast to the cells of MPMNs. Furthermore, the histogenesis, immunohistochemical, and molecular make up of both lesions are on opposite ends of the spectrum.
- Maintaining a high level of suspicion for this rare entity is important, particularly in association with other neoplasms. In our case, if the lung nodules were deemed metastatic deposits without pathological correlation, the patient would have been upstaged to T4 and treatment options would have been delayed or denied.
- The differential diagnosis of MPMNs includes metastatic carcinoma, pulmonary carcinoid tumors (or pulmonary tumorlets for lesions <5 mm), paraganglioma, pulmonary meningioma and rarely metastasis of a primary intracranial malignant meningioma. Although cells of MPMNs and pulmonary meningiomas are similar, primary lung meningiomas are clonal neoplastic lesions, which usually present as lung masses rather than minute nodules. Spinelli et al.12 suggested that MPMNs may be the precursor lesions of primary pulmonary meningiomas. However, the exact relationship between these entities is unknown. In addition to the microscopic morphology, immunohistochemical stains and a correlation with the clinical and the radiological findings are needed to establish a correct diagnosis.
- In conclusion, we have reported the first case describing MPMNs in the English literature, which were detected incidentally on a thin-section CT, in a patient with invasive lobular carcinoma of the breast. MPMNs should be suspected in lesions with a ground-glass appearance on CT scans. Pathological correlation is essential to stage the disease properly and provide the patients with the optimal treatment options, particularly for patients with known malignancies.
DISCUSSION
- 1. Korn D, Bensch K, Liebow AA, Castleman B. Multiple minute pulmonary tumors resembling chemodectomas. Am J Pathol 1960; 37: 641-672. PubMedPMC
- 2. Gaffey MJ, Mills SE, Askin FB. Minute pulmonary meningothelial-like nodules: a clinicopathologic study of so-called minute pulmonary chemodectoma. Am J Surg Pathol 1988; 12: 167-175. PubMed
- 3. Sellami D, Gotway MB, Hanks DK, Webb WR. Minute pulmonary meningothelial-like nodules: thin-section CT appearance. J Comput Assist Tomogr 2001; 25: 311-313. ArticlePubMed
- 4. Kuroki M, Nakata H, Masuda T, et al. Minute pulmonary meningothelial-like nodules: high-resolution computed tomography and pathologic correlations. J Thorac Imaging 2002; 17: 227-229. ArticlePubMed
- 5. Mukhopadhyay S, El-Zammar OA, Katzenstein AL. Pulmonary meningothelial-like nodules: new insights into a common but poorly understood entity. Am J Surg Pathol 2009; 33: 487-495. PubMed
- 6. Pelosi G, Maffini F, Decarli N, Viale G. Progesterone receptor immunoreactivity in minute meningothelioid nodules of the lung. Virchows Arch 2002; 440: 543-546. ArticlePubMedPDF
- 7. Churg AM, Warnock ML. So-called "minute pulmonary chemodectoma": a tumor not related to paragangliomas. Cancer 1976; 37: 1759-1769. ArticlePubMed
- 8. Kraushaar G, Ajlan AM, English JC, Müller NL. Minute pulmonary meningothelial-like nodules: a case of incidentally detected diffuse cystic micronodules on thin-section computed tomography. J Comput Assist Tomogr 2010; 34: 780-782. PubMed
- 9. Mizutani E, Tsuta K, Maeshima AM, Asamura H, Matsuno Y. Minute pulmonary meningothelial-like nodules: clinicopathologic analysis of 121 patients. Hum Pathol 2009; 40: 678-682. ArticlePubMed
- 10. Niho S, Yokose T, Nishiwaki Y, Mukai K. Immunohistochemical and clonal analysis of minute pulmonary meningothelial-like nodules. Hum Pathol 1999; 30: 425-429. ArticlePubMed
- 11. Spain DM. Intrapulmonary chemodectomas in subjects with organizing pulmonary thromboemboli. Am Rev Respir Dis 1967; 96: 1158-1164. PubMed
- 12. Spinelli M, Claren R, Colombi R, Sironi M. Primary pulmonary meningioma may arise from meningothelial-like nodules. Adv Clin Path 2000; 4: 35-39. PubMed
- 13. Singletary SE, Patel-Parekh L, Bland KI. Treatment trends in early-stage invasive lobular carcinoma: a report from the National Cancer Data Base. Ann Surg 2005; 242: 281-289. PubMedPMC
- 14. Cancer Incidence REPORT, 2004 [Internet]. Saudi Cancer Registry, Ministry of Health. 2008; cited 2011 May 17. Riyadh: Saudi Cancer Registry, Ministry of Health, Available from: http://bportal.kfshrc.edu.sa/wps/wcm/connect/40dcba804a8d741fb731f7e404c39865/SCR2004W.pdf?MOD=AJPERES&CACHEID=40dcba804a8d741fb731f7e404c39865.
- 15. Hanby AM, Hughes TA. In situ and invasive lobular neoplasia of the breast. Histopathology 2008; 52: 58-66. ArticlePubMed
REFERENCES
Fig. 2(A, B) Photomicrographs showing interstitial infiltration of the lung by polyhedral cells with oval nuclei and finely dispersed chromatin.
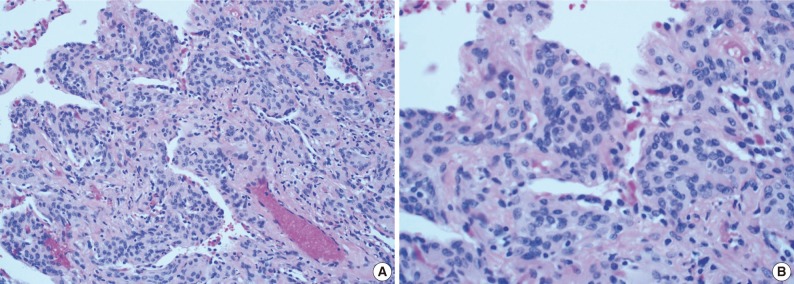
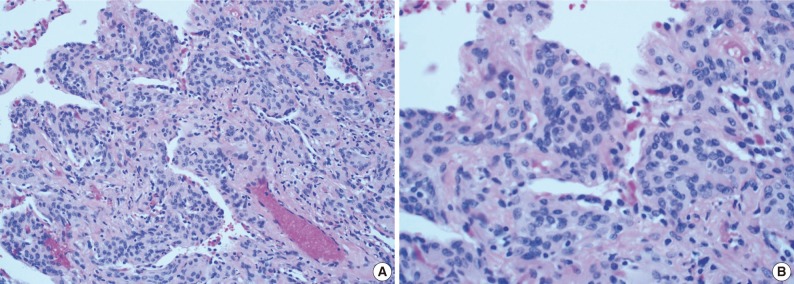
Fig. 4(A) Progesterone receptor (PR) immunohistochemical stain showing nuclear positivity in the minute lung nodules (PR; mouse monoclonal, Novocastra). (B) Epithelial membrane antigen (EMA) immunohistochemical stain showing membranous reactivity in the minute lung nodules (EMA; mouse monoclonal, Novocastra).
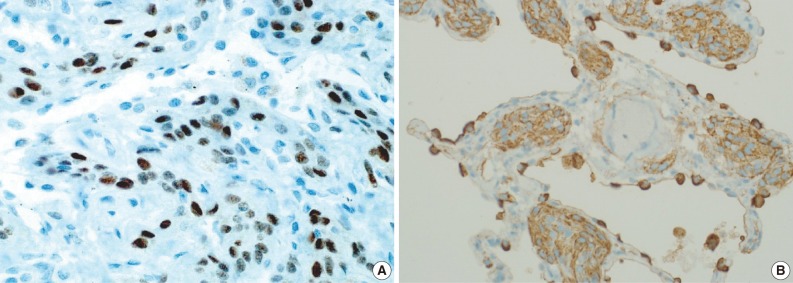
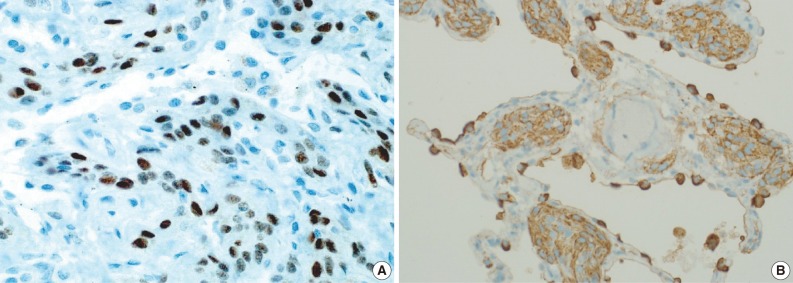
Figure & Data
References
Citations
Citations to this article as recorded by 

- Diffuse pulmonary meningotheliomatosis with pan-TRK expression by immunohistochemistry: a novel finding and potential pitfall
Cansu Karakas, Michael A. Nead, Moises J. Velez
Diagnostic Pathology.2023;[Epub] CrossRef - Diffuse Pulmonary Meningotheliomatosis: Clinic-Pathologic Entity or Indolent Metastasis from Meningioma (or Both)?
Laura Melocchi, Giulio Rossi, Mirca Valli, Maria Cecilia Mengoli, Michele Mondoni, Luigi Lazzari-Agli, Giacomo Santandrea, Fabio Davoli, Chiara Baldovini, Alberto Cavazza, Thomas V. Colby
Diagnostics.2023; 13(4): 802. CrossRef - Pathological diagnosis and immunohistochemical analysis of minute pulmonary meningothelial-like nodules: A case report
Xin Ruan, Liu-Sheng Wu, Zheng-Yang Fan, Qi Liu, Jun Yan, Xiao-Qiang Li
World Journal of Clinical Cases.2023; 11(33): 8022. CrossRef - Benign disease prone to be misdiagnosed as malignant pulmonary nodules: Minute meningothelioid nodules
Xiao‐Xiao Peng, Li‐Xu Yan, Chao Liu, Si‐Yun Wang, Wen‐Feng Li, Xing Gao, Xue‐Wu Wei, Qing Zhou
Thoracic Cancer.2019; 10(5): 1182. CrossRef - Atypical finding of meningothelial-like inclusions in cervical lymph nodes
Rebecca Donkin, Andrew Dettrick, Penelope Wyche, Sarah Grigg
Pathology.2018; 50(7): 785. CrossRef - Minute Pulmonary Meningothelial-Like Nodules Simulating Hematogenous Lung Metastasis: A Case Report
Sang Kook Lee, Gi Jeong Kim, Young Jae Kim, Ah Young Leem, Eu Dong Hwang, Se Kyu Kim, Joon Chang, Young Ae Kang, Song Yee Kim
Tuberculosis and Respiratory Diseases.2013; 75(2): 67. CrossRef - Diffuse Pulmonary Meningotheliomatosis Diagnosed by Transbronchial Lung Biopsy
Roberto Bernabeu Mora, Juan Miguel Sánchez Nieto, Chunshao Hu, Eduardo Alcaraz Mateos, Alberto Giménez Bascuñana, Manuel Rodríguez Rodríguez
Respiration.2013; 86(2): 145. CrossRef
Mimicry of Minute Pulmonary Meningothelial-like Nodules to Metastatic Deposits in a Patient with Infiltrating Lobular Carcinoma: A Case Report and Review of the Literature
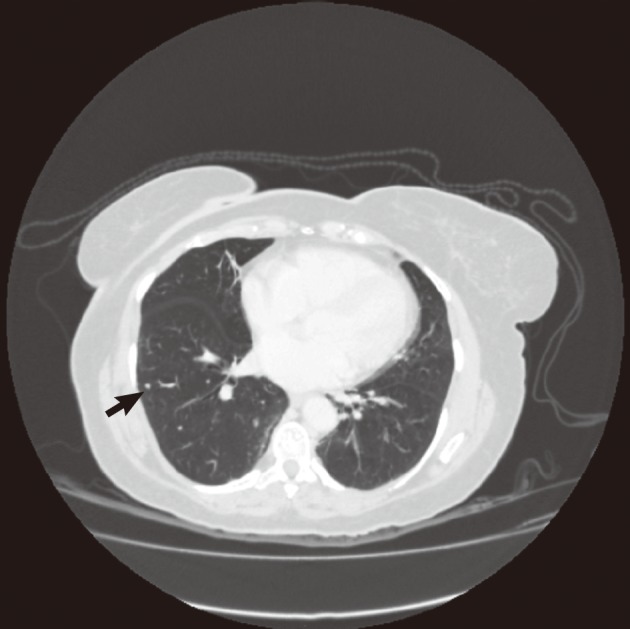
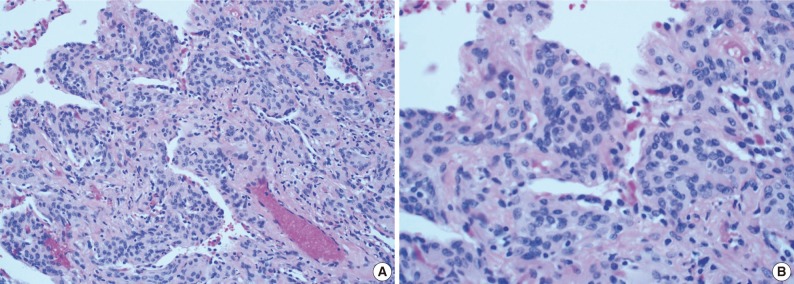
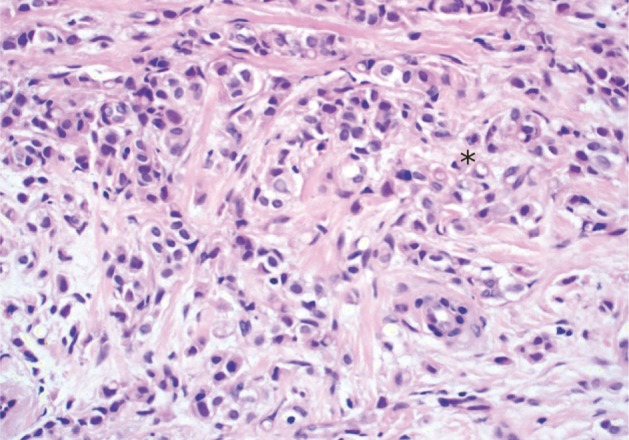
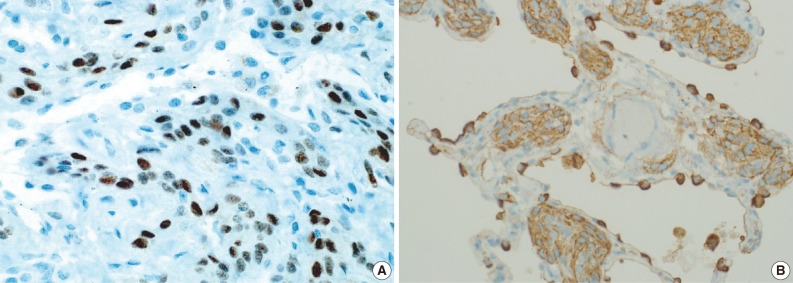
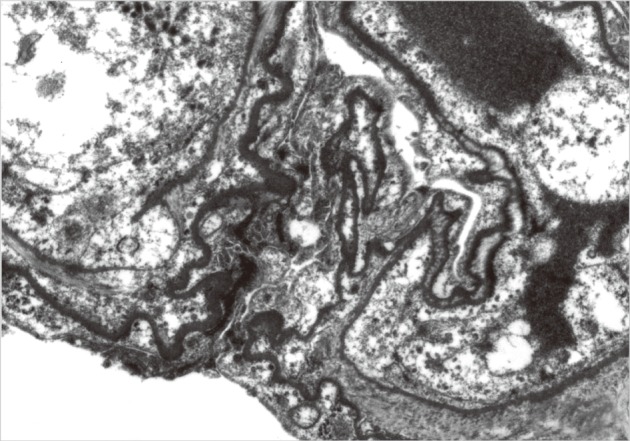
Fig. 1 Computed tomography image showing a small nodule in the right lung (arrow).
Fig. 2 (A, B) Photomicrographs showing interstitial infiltration of the lung by polyhedral cells with oval nuclei and finely dispersed chromatin.
Fig. 3 Infiltrating lobular carcinoma of the breast with focal signet-ring appearance (asterisk).
Fig. 4 (A) Progesterone receptor (PR) immunohistochemical stain showing nuclear positivity in the minute lung nodules (PR; mouse monoclonal, Novocastra). (B) Epithelial membrane antigen (EMA) immunohistochemical stain showing membranous reactivity in the minute lung nodules (EMA; mouse monoclonal, Novocastra).
Fig. 5 Electron photomicrograph showing interdigitating cells and desmosomes (×2,500).
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Mimicry of Minute Pulmonary Meningothelial-like Nodules to Metastatic Deposits in a Patient with Infiltrating Lobular Carcinoma: A Case Report and Review of the Literature

 E-submission
E-submission
 PubReader
PubReader Cite this Article
Cite this Article