Search
- Page Path
- HOME > Search
Original Articles
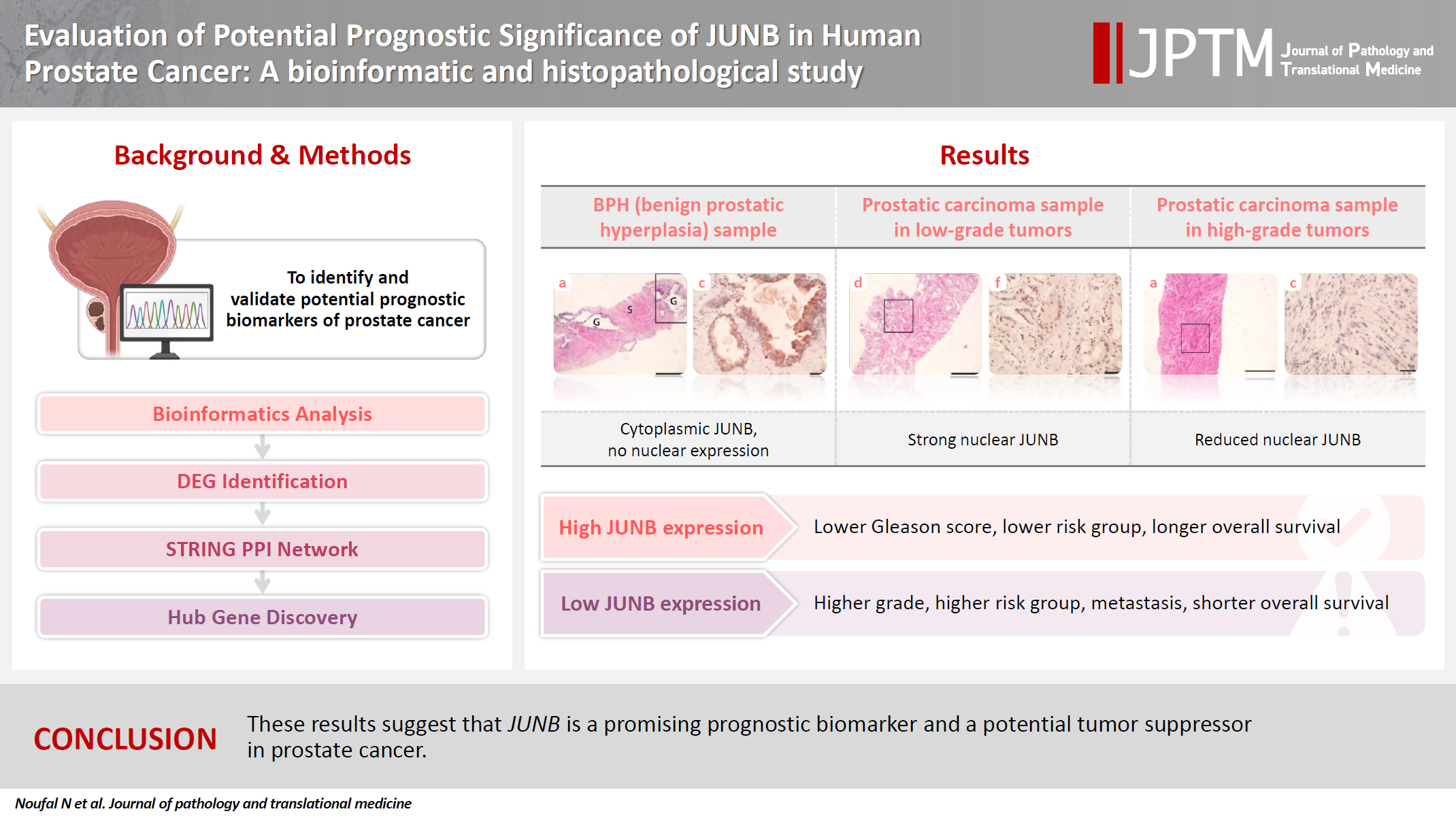
- Evaluation of potential prognostic significance of JUNB in human prostate cancer: a bioinformatic and histopathological study
- Noha R. Noufal, Einas M. Yousef, Mohamed Taha
- J Pathol Transl Med. 2025;59(5):291-305. Published online September 8, 2025
- DOI: https://doi.org/10.4132/jptm.2025.06.06
- 1,422 View
- 114 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Prostate cancer is one of the most common malignancies in males worldwide. Serum prostate-specific antigen is a frequently employed biomarker in the diagnosis and risk stratification of prostate cancer; however, it is known for its low predictive accuracy for disease progression. New prognostic biomarkers are needed to distinguish aggressive prostate cancer from low-risk disease. This study aimed to identify and validate potential prognostic biomarkers of prostate cancer. Methods: Two prostate cancer datasets from the Gene Expression Omnibus were analyzed to identify differentially expressed genes between benign prostatic hyperplasia (BPH) and prostatic carcinoma. Immunohistochemistry was used to evaluate the JUNB proto-oncogene, a subunit of the AP-1 transcription factor (JUNB), in 70 prostate cancer patients and 10 BPH samples. Results: Our findings showed that JUNB was significantly enriched in prostate cancer-related pathways and biological processes. JUNB expression was considerably higher in prostatic adenocarcinoma patients than in BPH patients. Regarding JUNB expression in prostate cancer cases, lower levels of JUNB expression were associated with higher grades of prostatic adenocarcinoma. Lower JUNB expression was associated with a higher risk of prostatic adenocarcinoma progression and shorter overall survival. Conclusions: These results suggest that JUNB is a promising prognostic biomarker and a potential tumor suppressor in prostate cancer.
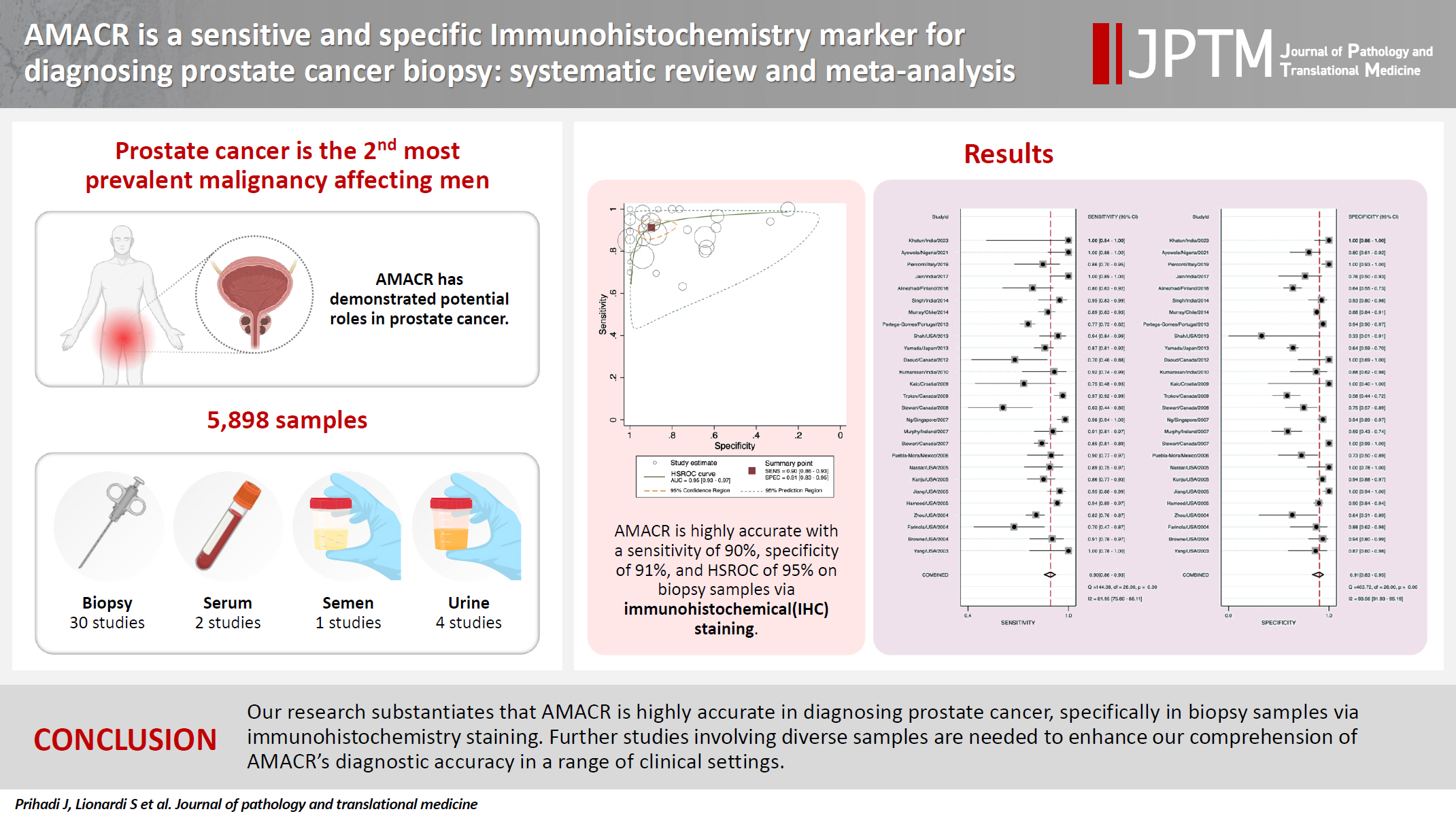
- AMACR is a highly sensitive and specific immunohistochemical marker for diagnosing prostate cancer on biopsy: a systematic review and meta-analysis
- Johannes Cansius Prihadi, Stevan Kristian Lionardi, Nicolas Daniel Widjanarko, Steven Alvianto, Fransiskus Xaverius Rinaldi, Archie Fontana Iskandar
- J Pathol Transl Med. 2025;59(4):235-248. Published online July 3, 2025
- DOI: https://doi.org/10.4132/jptm.2025.04.16
- 6,262 View
- 206 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Alpha-methylacyl-CoA racemase (AMACR) is the preferred biomarker for distinguishing malignant from benign glands in prostate biopsies, showing high sensitivity and specificity for prostate cancer. A meta-analysis of immunohistochemistry (IHC) for AMACR is essential to further assess its diagnostic accuracy across diverse sample sources. Methods: A systematic search of databases including MEDLINE, ScienceDirect, ProQuest, Google Scholar, and the Cochrane Library was performed, focusing on studies of AMACR to diagnose prostate cancer, particularly in biopsy samples analyzed through IHC over the last 20 years. Quality of studies was assessed using the Quality Assessment of Diagnostic Accuracy Studies 2 tool, followed by a meta-analysis of regions and subgroups to calculate summary estimates of diagnostic test accuracy. Results: In the final analysis, 37 studies, with a pooled size of 5,898 samples, were included from the examination of 94 full-text papers. Among them, 27 studies with similar sample sources and testing methodologies underwent meta-analysis, yielding a combined sensitivity estimate of 0.90 (95% confidence interval [CI], 0.86 to 0.93) and specificity of 0.91 (95% CI, 0.83 to 0.95), both with significant heterogeneity (p < .01). The region beneath the hierarchical summary receiver operating characteristic curve was 0.95 (95% CI, 0.93 to 0.97), positive likelihood ratio was 9.6 (95% CI, 5.3 to 17.4), negative likelihood ratio was 0.11 (95% CI, 0.08 to 0.15), and diagnostic odds ratio was 88 (95% CI, 42 to 181). Conclusions: Our meta-analysis findings substantiate AMACR as a highly accurate tool for diagnosing prostate cancer, specifically in biopsy samples, via immunohistochemical staining. Further studies involving diverse samples are needed to enhance our understanding of the AMACR diagnostic accuracy in a range of clinical settings. -
Citations
Citations to this article as recorded by- Pathogenesis-Guided Biomarker Assessment: A Shift in Prostate Cancer Diagnostics
Jessica M. Logan, Victoria Malone, John J. O’Leary, Doug A. Brooks
International Journal of Molecular Sciences.2025; 26(24): 11786. CrossRef
- Pathogenesis-Guided Biomarker Assessment: A Shift in Prostate Cancer Diagnostics
Case Study
- Malignant Pleural Effusion from Metastatic Prostate Cancer: A Case Report with Unusual Cytologic Findings
- Jinyoung Jeon, Tae-Jung Kim, Hong Sik Park, Kyo-Young Lee
- J Pathol Transl Med. 2018;52(4):257-261. Published online June 7, 2018
- DOI: https://doi.org/10.4132/jptm.2018.05.08
- 11,318 View
- 132 Download
- 3 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - We present a case of 55-year-old man who complained of dyspnea and sputum for a month. He was an ex-smoker with a history of prostate cancer and pulmonary tuberculosis. Chest radiographs revealed bilateral pleural effusions of a small to moderate amount. Pigtail catheters were inserted for drainage. The pleural fluid consisted of large clusters and tightly cohesive groups of malignant cells, which however could not be ascribed to prostate cancer with certainty. We performed immunocytochemical panel studies to determine the origin of cancer metastasis. The immunostaining results were positive for prostate-specific antigen, alpha-methylacyl-coenzyme A racemase, and Nkx 3.1, consistent with prostate cancer. Pleural effusion associated with prostate cancer is rare. To our knowledge, this is the first case report in Korea to describe cytologic features of malignant pleural effusion associated with prostate cancer.
-
Citations
Citations to this article as recorded by- Pleural Metastasis as an Initial Presentation of Prostate Cancer: Case Report and Literature Review
Katarzyna Skrobisz, Kevin Miszewski, Laura Miszewska, Michał Bieńkowski, Marcin Matuszewski, Michał Studniarek
Diagnostics.2025; 15(6): 666. CrossRef - EBUS-TBNA pleural biopsy reveals prostate cancer metastasis: A rare case report and review of the literature
Fotios Sampsonas, Dimitrios Komninos, Vasilina Sotiropoulou, Matthaios Katsaras, Dimitra Gkanetsou, Ourania Papaioannou, Panagiota Tsiri, Vasiliki Tzelepi, Argyrios Tzouvelekis
Pneumon.2024; 37(2): 1. CrossRef - Cytopathological Features of Extensive Bilateral Pleural Effusions in Metastatic Prostate Cancer: Report of a Rare Case
Hehua Huang, Caroline Yap
Cureus.2024;[Epub] CrossRef - Bilateral pleural effusion: etiology, diagnostics
N. A. Stogova
PULMONOLOGIYA.2022; 32(6): 885. CrossRef - Rare Metastatic Prostate Cancer Mimicking Lymphoma with Malignant Pleural Effusion
Tung Liu, En Meng, Yu-Chun Lin, Tai-Kuang Chao, Yi-Ming Chang
Journal of Medical Sciences.2021; 42(1): 46. CrossRef
- Pleural Metastasis as an Initial Presentation of Prostate Cancer: Case Report and Literature Review
Original Articles
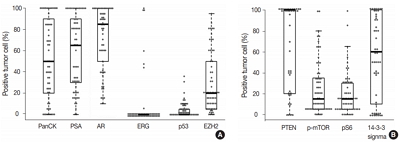
- Diverse Immunoprofile of Ductal Adenocarcinoma of the Prostate with an Emphasis on the Prognostic Factors
- Se Un Jeong, Anuja Kashikar Kekatpure, Ja-Min Park, Minkyu Han, Hee Sang Hwang, Hui Jeong Jeong, Heounjeong Go, Yong Mee Cho
- J Pathol Transl Med. 2017;51(5):471-481. Published online August 9, 2017
- DOI: https://doi.org/10.4132/jptm.2017.06.02
- 10,718 View
- 208 Download
- 14 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Ductal adenocarcinoma (DAC) of the prostate is an uncommon histologic subtype whose prognostic factors and immunoprofile have not been fully defined. Methods: To define its prognostic factors and immunoprofile, the clinicopathological features, including biochemical recurrence (BCR), of 61 cases of DAC were analyzed. Immunohistochemistry was performed on tissue microarray constructs to assess the expression of prostate cancer-related and mammalian target of rapamycin (mTOR) signaling-related proteins. Results: During the median follow-up period of 19.3 months, BCR occurred in 26 cases (42.6%). DAC demonstrated a wide expression range of prostate cancer-related proteins, including nine cases (14.8%) that were totally negative for pan-cytokeratin (PanCK) immunostaining. The mTOR signaling-related proteins also showed diverse expression. On univariate analysis, BCR was associated with high preoperative serum levels of prostate-specific antigen (PSA), large tumor volume, predominant ductal component, high Gleason score (GS), comedo-necrosis, high tumor stage (pT), lymphovascular invasion, and positive surgical margin. High expressions of phospho-mTOR (p-mTOR) as well as low expressions of PSA, phospho-S6 ribosomal protein (pS6) and PanCK were associated with BCR. On multivariable analysis, GS, pT, and immunohistochemical expressions of PanCK and p-mTOR remained independent prognostic factors for BCR. Conclusions: These results suggest GS, pT, and immunohistochemical expressions of PanCK and p-mTOR as independent prognostic factors for BCR in DAC. Since DAC showed diverse expression of prostate cancer–related proteins, this should be recognized in interpreting the immunoprofile of DAC. The diverse expression of mTOR-related proteins implicates their potential utility as predictive markers for mTOR targeted therapy. -
Citations
Citations to this article as recorded by- Intermediate risk prostate tumors contain lethal subtypes
William L. Harryman, James P. Hinton, Rafael Sainz, Jaime M. C. Gard, John M. Ryniawec, Gregory C. Rogers, Noel A. Warfel, Beatrice S. Knudsen, Raymond B. Nagle, Juan J. Chipollini, Benjamin R. Lee, Belinda L. Sun, Anne E. Cress
Frontiers in Urology.2025;[Epub] CrossRef - High GLUT1 membrane expression and low PSMA membrane expression in Ductal Adenocarcinoma and Intraductal Carcinoma of the prostate
Xingming Wang, Li Zhou, Lin Qi, Ye Zhang, Hongling Yin, Yu Gan, Xiaomei Gao, Yi Cai
Prostate Cancer and Prostatic Diseases.2024; 27(4): 720. CrossRef - Association of Lymphovascular Invasion with Biochemical Recurrence and Adverse Pathological Characteristics of Prostate Cancer: A Systematic Review and Meta-analysis
Jakub Karwacki, Marcel Stodolak, Andrzej Dłubak, Łukasz Nowak, Adam Gurwin, Kamil Kowalczyk, Paweł Kiełb, Nazar Holdun, Wojciech Szlasa, Wojciech Krajewski, Agnieszka Hałoń, Anna Karwacka, Tomasz Szydełko, Bartosz Małkiewicz
European Urology Open Science.2024; 69: 112. CrossRef - Impact of Epithelial Histological Types, Subtypes, and Growth Patterns on Oncological Outcomes for Patients with Nonmetastatic Prostate Cancer Treated with Curative Intent: A Systematic Review
Giancarlo Marra, Geert J.L.H. van Leenders, Fabio Zattoni, Claudia Kesch, Pawel Rajwa, Philip Cornford, Theodorus van der Kwast, Roderick C.N. van den Bergh, Erik Briers, Thomas Van den Broeck, Gert De Meerleer, Maria De Santis, Daniel Eberli, Andrea Faro
European Urology.2023; 84(1): 65. CrossRef - Impact of comedonecrosis on prostate cancer outcome: a systematic review
Kaveri T S Aiyer, Lisa J Kroon, Geert J L H van Leenders
Histopathology.2023; 83(3): 339. CrossRef - Survival after radical prostatectomy vs. radiation therapy in ductal carcinoma of the prostate
Francesco Chierigo, Marco Borghesi, Christoph Würnschimmel, Rocco Simone Flammia, Benedikt Horlemann, Gabriele Sorce, Benedikt Höh, Zhe Tian, Fred Saad, Markus Graefen, Michele Gallucci, Alberto Briganti, Francesco Montorsi, Felix K. H. Chun, Shahrokh F.
International Urology and Nephrology.2022; 54(1): 89. CrossRef - Defining Diagnostic Criteria for Prostatic Ductal Adenocarcinoma at Multiparametric MRI
Weranja K. B. Ranasinghe, Patricia Troncoso, Devaki Shilpa Surasi, Juan José Ibarra Rovira, Priya Bhosale, Janio Szklaruk, Andrea Kokorovic, Xuemei Wang, Mohamed Elsheshtawi, Miao Zhang, Ana Aparicio, Brian F. Chapin, Tharakeswara K. Bathala
Radiology.2022; 303(1): 110. CrossRef - Oncological outcomes of patients with ductal adenocarcinoma of the prostate receiving radical prostatectomy or radiotherapy
Mengzhu Liu, Kun Jin, Shi Qiu, Pengyong Xu, Mingming Zhang, Wufeng Cai, Xiaonan Zheng, Lu Yang, Qiang Wei
Asian Journal of Urology.2021; 8(2): 227. CrossRef - Ductal Prostate Cancers Demonstrate Poor Outcomes with Conventional Therapies
Weranja Ranasinghe, Daniel D. Shapiro, Hyunsoo Hwang, Xuemei Wang, Chad A. Reichard, Mohamed Elsheshtawi, Mary F. Achim, Tharakeswara Bathala, Chad Tang, Ana Aparicio, Shi-Ming Tu, Nora Navone, Timothy C. Thompson, Louis Pisters, Patricia Troncoso, John W
European Urology.2021; 79(2): 298. CrossRef - Optimizing the diagnosis and management of ductal prostate cancer
Weranja Ranasinghe, Daniel D. Shapiro, Miao Zhang, Tharakeswara Bathala, Nora Navone, Timothy C. Thompson, Bradley Broom, Ana Aparicio, Shi-Ming Tu, Chad Tang, John W. Davis, Louis Pisters, Brian F. Chapin
Nature Reviews Urology.2021; 18(6): 337. CrossRef - A first case of ductal adenocarcinoma of the prostate having characteristics of neuroendocrine phenotype with PTEN, RB1 and TP53 alterations
Hiroaki Kobayashi, Takeo Kosaka, Kohei Nakamura, Kazunori Shojo, Hiroshi Hongo, Shuji Mikami, Hiroshi Nishihara, Mototsugu Oya
BMC Medical Genomics.2021;[Epub] CrossRef - Knowing what’s growing: Why ductal and intraductal prostate cancer matter
Mitchell G. Lawrence, Laura H. Porter, David Clouston, Declan G. Murphy, Mark Frydenberg, Renea A. Taylor, Gail P. Risbridger
Science Translational Medicine.2020;[Epub] CrossRef - Integrative Genomic Analysis of Coincident Cancer Foci Implicates CTNNB1 and PTEN Alterations in Ductal Prostate Cancer
Marc Gillard, Justin Lack, Andrea Pontier, Divya Gandla, David Hatcher, Adam G. Sowalsky, Jose Rodriguez-Nieves, Donald Vander Griend, Gladell Paner, David VanderWeele
European Urology Focus.2019; 5(3): 433. CrossRef - Genomic Characterization of Prostatic Ductal Adenocarcinoma Identifies a High Prevalence of DNA Repair Gene Mutations
Michael T. Schweizer, Emmanuel S. Antonarakis, Tarek A. Bismar, Liana B. Guedes, Heather H. Cheng, Maria S. Tretiakova, Funda Vakar-Lopez, Nola Klemfuss, Eric Q. Konnick, Elahe A. Mostaghel, Andrew C. Hsieh, Peter S. Nelson, Evan Y. Yu, R. Bruce Montgomer
JCO Precision Oncology.2019; (3): 1. CrossRef
- Intermediate risk prostate tumors contain lethal subtypes
- Cytologic Features of Prostatic Adenocarcinoma in Urine: Comparison with Urothelial Carcinoma.
- Lucia Kim, Joo Young Song, Suk Jin Choi, In Suh Park, Jee Young Han, Joon Mee Kim, Young Chae Chu
- Korean J Pathol. 2011;45(1):79-86.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.1.79
- 4,725 View
- 74 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Prostate adenocarcinoma (PACa) cells are rarely identified in urine cytology specimens and might be easily overlooked or misdiagnosed as urothelial neoplasm when clinically unsuspected.
METHODS
We reviewed 19 urine cytology specimens obtained from 13 patients with PACa and evaluated the characteristic features discriminating PACa from urothelial carcinoma (UCa). For comparison, 27 cases of high-grade UCa (HGUCa) and 10 cases of urothelial carcinoma in situ (UCis) were also evaluated.
RESULTS
The urine cytologic evaluation of PACa revealed clustered cells forming 3-dimensional syncytial fragments with occasional microacinar grouping in a clean background. Most tumor cells were small and uniform with a high nuclear-to-cytoplasmic ratio and indistinct cell borders. The nuclei were round-to-oval and the cytoplasm was scanty and thin. One or more centrally-located prominent nucleoli were characteristically noted in one half of the cases. The nucleoli had a well-defined, large, round and eosinophilic appearance. In four high-grade cases, large tumor cells were encountered and had relatively monotonous cells with smooth-outlined cell clusters, well-defined and thin cytoplasm, and round nuclei with characteristic prominent nucleoli.
CONCLUSIONS
Combining the information of prostate cancer and the recognition of cytomorphologic features of PACa will help differentiate PACa from HGUCa and UCis. -
Citations
Citations to this article as recorded by- Cas no 8. Infiltration de la paroi vésicale par un adénocarcinome prostatique
Monique Courtade-Saïdi
Annales de Pathologie.2025; 45(2): 147. CrossRef - Bladder Washing Cytology in the Detection of High-Grade Prostatic Adenocarcinoma: A Case Report
Gabriel Pastrana, Camille L Santiago Negron, Suheidy Cardona, Juan C Santa Rosario, María D Rivera Rolón
Cureus.2025;[Epub] CrossRef - The diagnostic challenge of suspicious or positive malignant urine cytology findings when cystoscopy findings are normal: an outpatient blue-light flexible cystoscopy may solve the problem
Marie Andersson, Marthe Berger, Karsten Zieger, Per-Uno Malmström, Mats Bläckberg
Scandinavian Journal of Urology.2021; 55(4): 263. CrossRef - Sensitive Time-Gated Immunoluminescence Detection of Prostate Cancer Cells Using a TEGylated Europium Ligand
Nima Sayyadi, Irene Justiniano, Russell E. Connally, Run Zhang, Bingyang Shi, Liisa Kautto, Arun V. Everest-Dass, Jingli Yuan, Bradley J. Walsh, Dayong Jin, Robert D. Willows, James A. Piper, Nicolle H. Packer
Analytical Chemistry.2016; 88(19): 9564. CrossRef
- Cas no 8. Infiltration de la paroi vésicale par un adénocarcinome prostatique
- p16INK4a, PTEN, E-cadherin, Bcl-2 and Ki-67 Expression in Prostate Cancer: Its Relationship with the Metastatic Potential and Known Prognostic Factors.
- Seok Ju Park, Woo Jung Sung, Mi Jin Kim
- Korean J Pathol. 2010;44(6):597-604.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.6.597
- 4,555 View
- 33 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
At present, adequate prognostic markers for prostate cancer progression are still lacking, in spite of intensive investigation. Accordingly, our study examined the relationship between expression of candidate biomarkers and metastasis in prostate cancer patients. Correlation of molecular markers with prostate-specific antigen (PSA) level, Gleason sum score and tumor stage were also evaluated.
METHODS
A total of 105 prostate tumor specimens and specimens from 19 cases of nodular hyperplasia were obtained through Yeungnam University Hospital from 2007 to 2008. Immunohistochemical analyses for p16INK4a, phosphatase and tensin homolog (PTEN), E-cadherin, Ki-67 and Bcl-2 were performed.
RESULTS
Overexpression of Bcl-2 was significantly related to bone (p = 0.006) and nodal metastases (p = 0.017). Other biomarkers were not related to metastatic potential. There were statistically significant relationships between increased PSA level and loss of expression of PTEN (p = 0.019) and E-cadherin (p = 0.001). High Ki-67 index was significantly correlated with nodal metastasis (p = 0.029) as well as with loss of p16INK4a expression (p = 0.002) and high Gleason score (p = 0.011).
CONCLUSIONS
High Gleason score, Bcl-2 overexpression and increased Ki-67 labeling have significant predictive value in assessing the potential for prostate cancer metastasis. In addition, a high Ki-67 index is related to high Gleason score and loss of p16INK4a expression. -
Citations
Citations to this article as recorded by- Over-expression of β-catenin is associated with high grade of prostatic cancer in Libyan patients
W. Said, F. Emaetig, K. El Gehani, T. Eldarat, A. Buhmeida, N. Enattah, A. Elzagheid, O. Al-Fituri
African Journal of Urology.2017; 23(2): 133. CrossRef - Bcl2 en cáncer avanzado de próstata y asociación con resistencia a la castración
R.F. Velázquez-Macías, F.E. De La Torre-Rendón, G. Ramos-Rodríguez, C.A. Calzada-Mendoza, R.M. Coral-Vázquez
Revista Mexicana de Urología.2016; 76(5): 288. CrossRef - Hedgehog signaling protein expression and its association with prognostic parameters in prostate cancer: A retrospective study from the view point of new 2010 anatomic stage/prognostic groups
Tae‐Jung Kim, Ji Youl Lee, Tae‐Kon Hwang, Chang Suk Kang, Yeong‐Jin Choi
Journal of Surgical Oncology.2011; 104(5): 472. CrossRef
- Over-expression of β-catenin is associated with high grade of prostatic cancer in Libyan patients
- Pathological Analysis of 1,000 Cases of Transrectal Ultrasoundguided Systematic Prostate Biopsy: Establishment of New Sample Processing Method and Diagnostic Utility of Immunohistochemistry.
- Chang Lim Hyun, Hee Eun Lee, Haeryung Kim, Hye Seung Lee, So Yeon Park, Jin Haeng Chung, Gheeyoung Choe
- Korean J Pathol. 2006;40(6):406-419.
- 2,283 View
- 37 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
We developed a new processing method for extended prostate needle biopsy, and evaluated diagnostic utility of routine immunohistochemistry in 1,000 consecutive unselected cases of transrectal ultrasound-guided systematic prostate biopsy.
METHODS
Four to five biopsy cores were embedded in one paraffin block. All the biopsy cores were immunohistochemically stained with basal cell markers.
RESULTS
The new sample processing method was technically perfect for making a diagnosis from extended prostate needle biopsy. Among 1,000 cases, there were 323 cases (32.3%) of adenocarcinoma, 5 cases of other malignant tumors, 9 cases of high-grade prostatic intraepithelial neoplasia without a carcinoma, and only 8 cases of atypical small acinar proliferation. Among the 323 cases of adenocarcinoma, there were 38 cases (11.8%) of microcarcinomas <0.1 cm and 101 cases (31.3%) of small adenocarcinomas <0.3 cm in length. In the needle biopsy specimens, 59 cases (18.3%) were classified as clinically insignificant carcinomas. Among them, 37 cases underwent radical prostatectomy, which turned out to be clinically significant carcinomas in 24 cases (64.9%).
CONCLUSIONS
Routinely performed immunohistochemistry combined with the new sample processing method is very effective for detecting microscopic carcinoma foci as well as differentiating carcinoma from benign conditions mimicking cancer.

 E-submission
E-submission

 First
First Prev
Prev



