Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(4); 2014 > Article
-
Brief Case Report
Undifferentiated Embryonal Sarcoma in Adult Liver - Won Ju Hong, Yu Na Kang, Koo Jeong Kang1
-
Korean Journal of Pathology 2014;48(4):311-314.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.4.311
Published online: August 26, 2014
Department of Pathology, Keimyung University School of Medicine, Daegu, Korea.
1Department of Surgery, Keimyung University School of Medicine, Daegu, Korea.
- Corresponding Author: Yu Na Kang, M.D. Department of Pathology, Keimyung University School of Medicine, 1095 Dalgubeol-daero, Dalseo-gu, Daegu 704-701, Korea. Tel: +82-53-580-3814, Fax: +82-53-580-3823, yunakang@dsmc.or.kr
• Received: August 23, 2013 • Revised: September 23, 2013 • Accepted: September 25, 2013
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
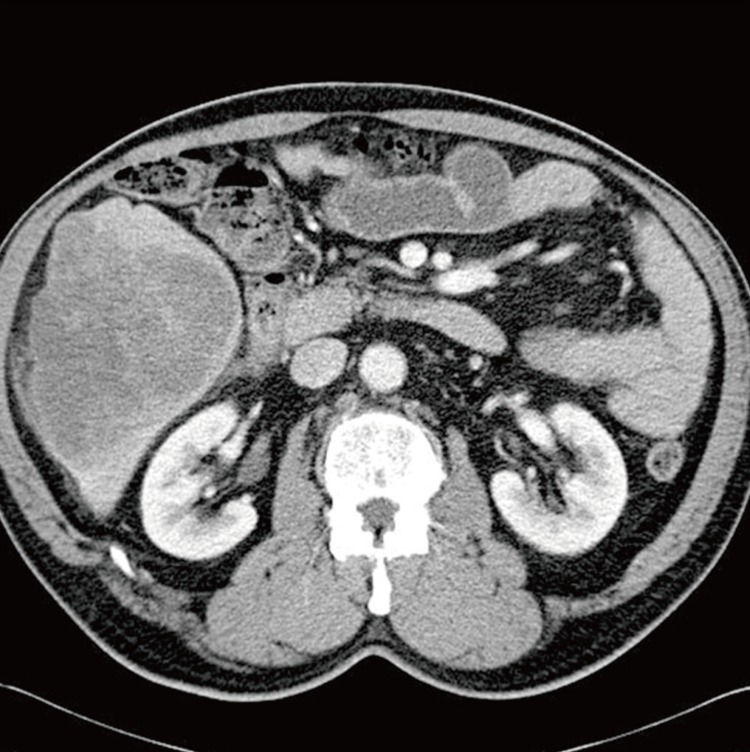
- A 67-year-old man was admitted to our hospital with abdominal pain of 10-day duration. Two days before admission, he experienced abrupt onset of an intermittent sharp pain in the right upper quadrant. His past medical history included underlying hypertension and diabetes mellitus, for which he had been taking medication for 10 years. He had no specific family history. A physical examination on admission demonstrated temperature of 36.4℃, heart rate of 84 beats/minutes, respiratory rate 16/minutes, and blood pressure 130/80 mm Hg. His abdomen was soft and flat, and he had tenderness in the right upper quadrant. Abnormal findings such as jaundice or spider naevi were not present. A chest radiograph showed no pulmonary abnormality. Routine laboratory findings included the following: total bilirubin 1.0 mg/dL (normal range [NR], 0.2 to 1.2 mg/dL), conjugated bilirubin 0.3 mg/dL (NR, 0.0 to 0.4 mg/dL), alkaline phosphatase 121 U/L (NR, 40 to 122 U/L), γ-glutamyl transferase 99 U/L (NR, 11 to 50 U/L), alanine-aminotransferase 32 U/L (NR, 5 to 44 U/L), aspartate-aminotransferase 46 U/L (NR, 13 to 36 U/L), carcinoembryonic antigen 1.64 ng/mL (NR, <5 ng/mL), cancer antigen 19-9 20.51 U/mL (NR, <39 U/mL), and alpha-fetoprotein (AFP) 9.7 ng/mL (NR, <9.6 ng/mL). Anti-hepatitis B surface, anti-hepatitis B core, and anti-hepatitis C virus antibodies, as well as hepatitis B antigen, were not detected. A dynamic computed tomography study found a 13-cm-sized hypoattenuating mass with lobulated contour in the right hepatic lobe, in segments 5 and 6 (Fig. 1). Under the diagnosis of mass-forming intrahepatic cholangiocarcinoma, the patient underwent a segmentectomy (segments 5 and 6), along with cholecystectomy and resection of the omentum.
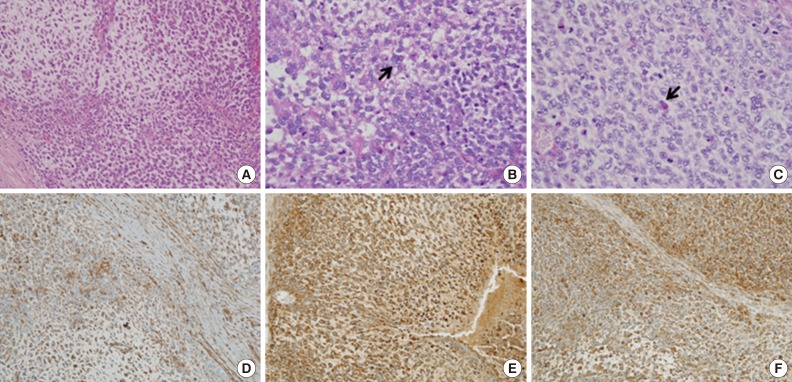
- Grossly, a large mass in segments 5 and 6 of the right hepatic lobe was detected, measuring 14.5×11.2×9.0 cm. The cut section showed a large, variegated, solid, and firm mass with a grey-to-yellow surface. The mass, though mostly solid, also comprised a dark hemorrhagic and necrotic area and a gelatinous cystic area (Fig. 2). Microscopically, the mass contained compactly- or loosely-arranged tumor cells with 20% tumor necrosis, and was surrounded by an abundant myxoid matrix or fibrous stroma. Histologic findings revealed sheets of undifferentiated oval, spindle-shaped, or stellate tumor cells (Fig. 3A). Irregular, hyperchromatic nuclei with numerous abnormal mitoses (>50/10 high power fields) and highly irregular multinucleated giant cells were observed. Multiple intracytoplasmic or extracellular eosinophilic globules were expressed with periodic acid-Schiff (PAS) and diastase-resistant PAS staining (D-PAS) (Fig. 3B, C). Tumor cells had invaded into liver parenchyma, and several entrapped bile ducts were seen in the tumor mass periphery. Cytoplasm from the tumor cells showed diffusely positive expression of vimentin, alpha 1-antichymotrypsin and alpha 1-antitrypsin (Fig. 3D-F). CD68 and smooth muscle actin were positive only focally. Hepatocyte, AFP, cytokeratin (CK) 7, CK19, CD117, CD99, human melanoma black-45 (HMB-45), leukocyte common antigen (LCA), epithelial membrane antigen (EMA), myoglobin, and S-100 were all negative. The Ki-67 proliferation index was 10%. On the basis of these findings, a diagnosis of UES was made.
- One month after the operation, the patient developed a recurrent mass on segments 6 and 7 on the remnant right hepatic lobe. The mass continued to grow, so MAID (mesna, doxorubicin, ifosfamide, and dacarbazine) chemotherapy was started. During the fifth cycle of chemotherapy, the patient developed neutropenic fever and died of sepsis, eight months after his initial diagnosis and operation.
CASE REPORT
- Before it was first named by Stocker and Ishak in 1978,1 UES of the liver was previously called mesenchymal sarcoma, fibromyxosarcoma, embryonal sarcoma, and malignant mesenchymoma. Although common in children between 6 and 10 years old, UES is very rare in adults over 60-years-old; for adults aged >60 years, only 14 UES cases have been reported in the world until now.3,4,5,6,7 UES was known to have no gender predominance in children, but there was female predominance (62.5%) in UES patients over the age of 30 worldwide.9 Clinical diagnosis of UES is difficult as there is no specific clinical feature. Patients complain of nonspecific symptoms such as abdominal pain, weight loss, nausea, vomiting, fatigue, or jaundice.
- UES usually appears as a large, well-circumscribed solitary mass showing variable areas of necrosis, cystic degeneration, and hemorrhage. It ranges in size from 10 to 30 cm. In this case, the UES tumor contained atypical spindle or satellite cells with some giant cells set in compactly- or loosely-arranged myxoid or fibrous stroma. Some cells had nuclear pleomorphism with irregular and hyperchromatic features and numerous abnormal mitoses. Multiple intracytoplasmic or extracellular, eosinophilic, PAS and D-PAS stained, globules were characteristic. With immunohistochemistry, a diagnosis of UES could be made more easily, although immunohistological markers may not be specific. The cytoplasm of the patient's tumor cells diffusely stained positive for vimentin, alpha 1-antichymotrypsin, and alpha 1-antitrypsin, but was negative for hepatocyte marker, AFP, CK, CD117, CD99, HMB-45, LCA, EMA, myoglobin, and S-100. Ultrastructurally, his hepatic UES demonstrated dilated rough endoplasmic reticulum and electron-dense lysosomal precipitates, which correlated with the eosinophilic hyaline bodies seen microscopically. These morphological and ultrastructural findings are the same in pediatric and adult UES, suggesting that UES tumor cells are composed of fibroblastic, fibrohistioblastic, and undifferentiated cells. Other differential lineages have not been identified. UES, unlike hepatocellular carcinoma, is not associated with viral hepatitis, liver cirrhosis, alteration of hepatic function, or elevation of AFP, but the exact pathogenesis of this malignancy is not known.
- In the differential diagnosis for UES, the following factors are considered: malignant fibrous histiocytoma, metastatic gastrointestinal stromal tumour, carcinosarcoma, hepatocellular carcinoma, cholangiocarcinoma (sarcomatoid differentiated), leiomyosarcoma, liposarcoma, hepatobiliary rhabdomyosarcoma (RMS), hepatoblastoma, and mesenchymal hamartoma of the liver (MHL). Both RMS and MHL arise in children and may involve myxoid mesenchymal tissue, however, MHL typically includes small bile ducts and intervening vascular channels, as well as loose mesenchymal structure. In addition, RMS can be differentiated from UES through positive immunohistochemical staining for desmin, myogenin, and myoD.
- UES of the liver has been considered an aggressive type of tumor with an unfavorable prognosis. It is well known to commonly recur even after complete resection, and the majority of patients die within two years of the initial surgery. Radical resection of the tumor is recommended for the best treatment. In addition, recent studies have shown that adjuvant chemotherapy and/or radiotherapy in addition to surgery may be helpful for improving survival.10 For unresectable tumors, systemic chemotherapy and local radiotherapy can be done. The role of neo-adjuvant treatment also is being evaluated for tumors diagnosed preoperatively. Effective chemotherapy regimens include some combination of vincristine, doxorubicin or actinomycin D, cyclophosphamide or ifosfamide, and cisplatin.11 The best choice of treatment for UES of the liver is considered to be surgical resection and chemotherapy. However, the most optimal therapy is still to be proved.
- Since UES of the liver is a very rare entity in adults and can seem similar to mass-forming intrahepatic cholangiocarcinoma, it is important to diagnose UES in a timely and accurate fashion-regardless of tissue quantity-in order to begin effective treatment as soon as possible.
DISCUSSION
- 1. Stocker JT, Ishak KG. Undifferentiated (embryonal) sarcoma of the liver: report of 31 cases. Cancer 1978; 42: 336-348. ArticlePubMed
- 2. Jiménez Fuertes M, López Andújar R, de Juan Burgueño M, et al. Hepatic undifferentiated (embryonal) sarcoma in an adult: a case report and literature review. Gastroenterol Hepatol 2008; 31: 12-17. PubMed
- 3. Lightfoot N, Nikfarjam M. Embryonal sarcoma of the liver in an adult patient. Case Rep Surg 2012; 2012: 382723.ArticlePubMedPMCPDF
- 4. Tucker SM, Cooper K, Brownschidle S, Wilcox R. Embryonal (undifferentiated) sarcoma of the liver with peripheral angiosarcoma differentiation arising in a mesenchymal hamartoma in an adult patient. Int J Surg Pathol 2012; 20: 297-300. ArticlePubMedPDF
- 5. Kim KT, Han SY, Park EH, et al. A case of the treatment in an adult with hepatic undifferentiated (embryonal) sarcoma. Korean J Hepatol 2007; 13: 96-102. PubMed
- 6. Lee JA, Kim TW, Min JH, et al. A case of undifferentiated (embryonal) liver sarcoma mimicking klatskin tumor in an adult. Korean J Gastroenterol 2010; 55: 144-148. ArticlePubMed
- 7. Kim KH, Lee SJ, Lee G, et al. Undifferentiated sarcoma of the liver in adult: a case report and review of the literature. Korean J Hepatol 1998; 4: 283-289.
- 8. Chu YC, Moon YH, Kim IS. Undifferentiated sarcoma of the liver in an adult: a case report. Korean J Pathol 1987; 21: 34-39.
- 9. Li XW, Gong SJ, Song WH, et al. Undifferentiated liver embryonal sarcoma in adults: a report of four cases and literature review. World J Gastroenterol 2010; 16: 4725-4732. ArticlePubMedPMC
- 10. Lenze F, Birkfellner T, Lenz P, et al. Undifferentiated embryonal sarcoma of the liver in adults. Cancer 2008; 112: 2274-2282. ArticlePubMed
REFERENCES
Fig. 1A dynamic computed tomography study shows a 13-cm-sized hypoattenuating mass with lobulated contour in the right hepatic lobe, in segments 5 and 6.
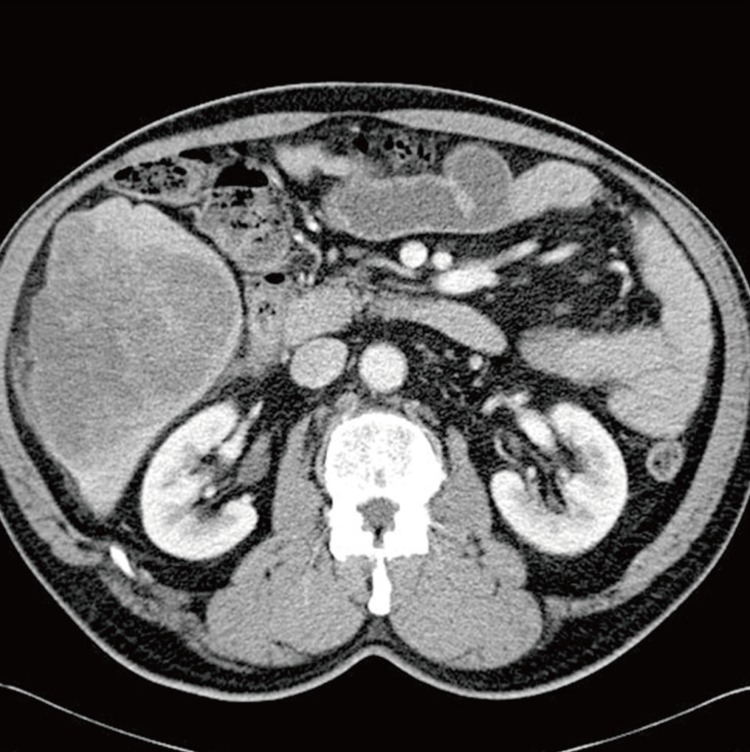
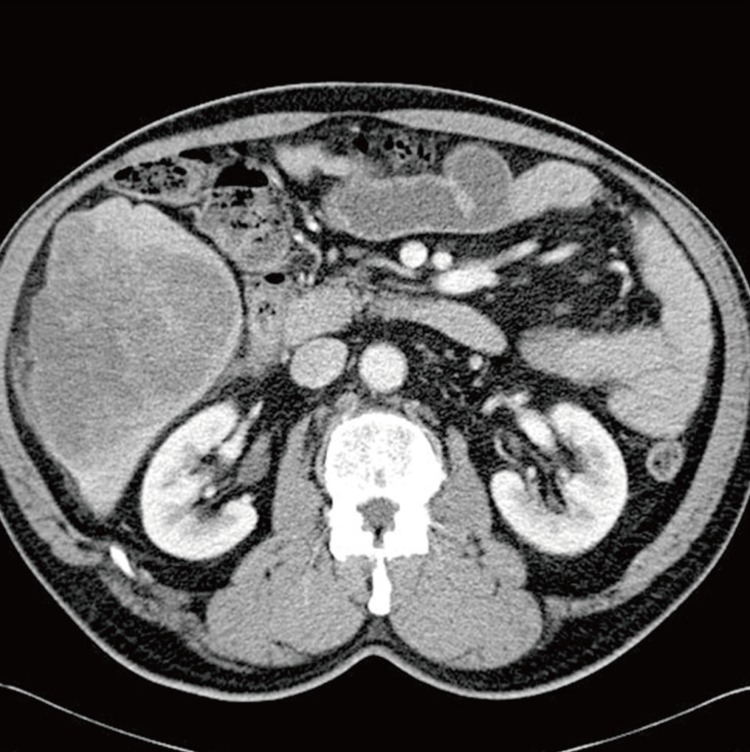
Fig. 2The cut section shows a large variegated solid and firm mass, composed of a grey-to-yellow solid area and a dark red hemorrhagic area.


Fig. 3Microscopic studies of the liver mass show sheets of undifferentiated oval, spindle-shaped, or stellate tumor cells in myxoid or fibrous stroma (A). Intracytoplasmic eosinophilic globules (arrows) are seen in periodic acid-Schiff (PAS, B) and diastase-resistant PAS (C). The cytoplasms of tumor cells are diffusely stained by vimentin (D), alpha 1-antitrypsin (E), and alpha 1-antichymotrypsin (F).
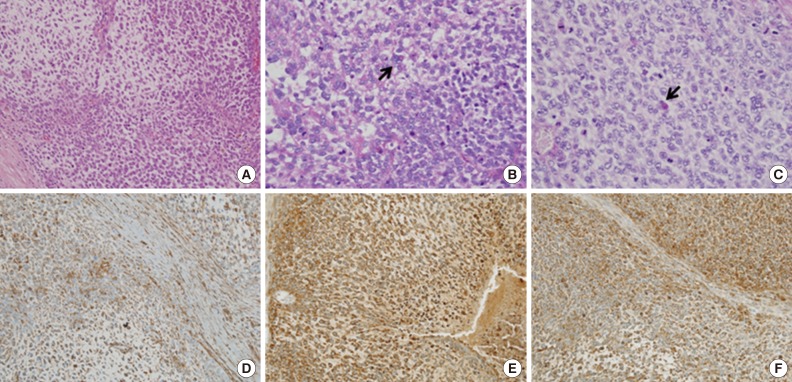
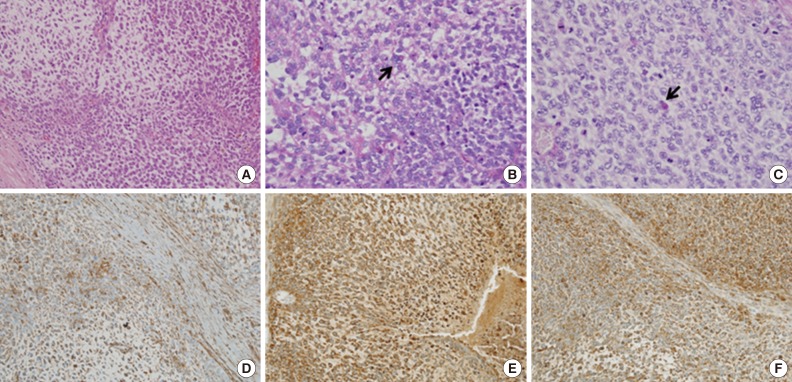
Figure & Data
References
Citations
Citations to this article as recorded by 

- Case Report: Diagnosis and treatment of an undifferentiated embryonal sarcoma of the liver
Xiaojiao Qiu, Lexing Zhang, Fan Sun
Frontiers in Surgery.2025;[Epub] CrossRef - A rare case of undifferentiated embryonal sarcoma of the liver in an adolescent
Nguyen Van Thi, Nguyen Thi Hao, Do Dang Khanh, Do Xuan Duoc, Ngo Le Lam, Nguyen Thuy Linh, Vu Le Minh, Ta Hong Nhung
Sonography.2024; 11(4): 411. CrossRef - Histologically Unclassifiable Hepatic Sarcoma: A Case Report
Daisuke Komatsu, Akira Shimizu, Koji Kubota, Tsuyoshi Notake, Kentaro Umemura, Takamune Goto, Atsushi Kamachi, Hidenori Tomida, Shiori Yamazaki, Hisashi Tamada, Yuji Soejima
The Japanese Journal of Gastroenterological Surgery.2023; 56(6): 315. CrossRef - Undifferentiated embryonal sarcoma of the liver treated with associating liver partition and portal vein ligation for staged hepatectomy in a young adult: A case report
Dmitri Schepelew, Tim Reese, Katja Horling, Christian Frenzel, Karl J. Oldhafer
International Journal of Surgery Case Reports.2020; 66: 221. CrossRef - Hanging Undifferentiated Embryonal Sarcoma of the Liver in Adult: an Unusual Presentation of an Aggressive Tumor
Narendra Pandit, Kunal Bikram Deo, Lokesh Shekher Jaiswal, Anju Pradhan, Shailesh Adhikary
Journal of Gastrointestinal Cancer.2019; 50(3): 689. CrossRef - Unexpected Liver Embryonal Sarcoma in the Adult: Diagnosis and Treatment
Maurizio Pinamonti, Federico Vittone, Francesco Ghiglione, Andrea Borasi, Stefano Silvestri, Sergio Coverlizza
Case Reports in Surgery.2018; 2018: 1. CrossRef - Undifferentiated embryonal sarcoma of the liver in adult patient: A report of two cases
Germán Esteban Sánchez-Morales, Uriel Emilio Clemente-Gutiérrez, Francisco Emmanuel Alvarez-Bautista, Oscar Santes-Jasso, Paulina Carpinteyro-Espin, Miguel Angel Mercado
Annals of Hepato-Biliary-Pancreatic Surgery.2018; 22(3): 269. CrossRef - Undifferentiated Sarcoma of the Liver in an Adult Showing Early Recurrence after Hepatectomy and Rapid Growth Leading to Death
Akira Yasuda, Keisuke Nonoyama, Shunsuke Hayakawa, Kaori Watanabe, Shiro Fujihata, Minoru Yamamoto, Hidehiko Kitagami, Yasunobu Shimizu, Tetsushi Hayakawa, Moritsugu Tanaka
The Japanese Journal of Gastroenterological Surger.2016; 49(5): 409. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
Undifferentiated Embryonal Sarcoma in Adult Liver
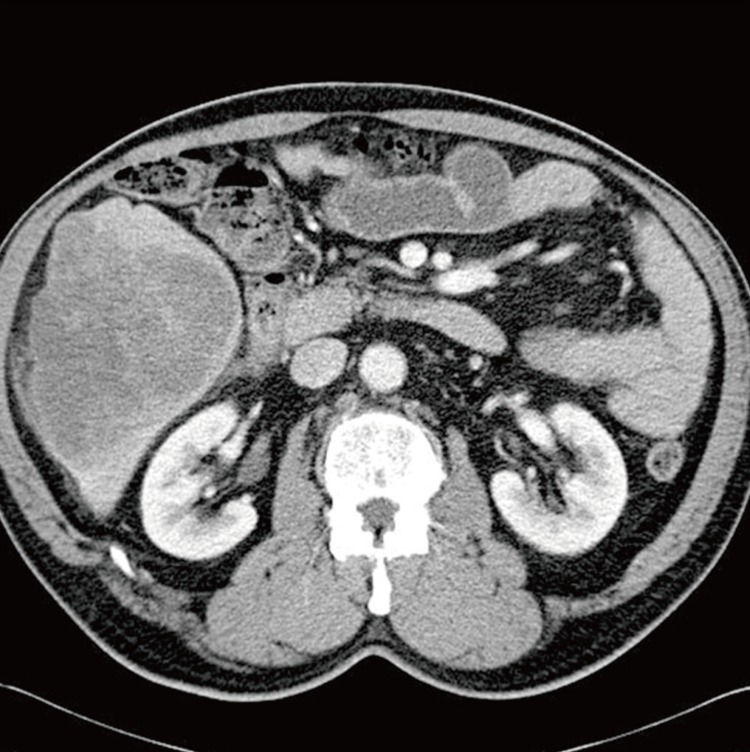

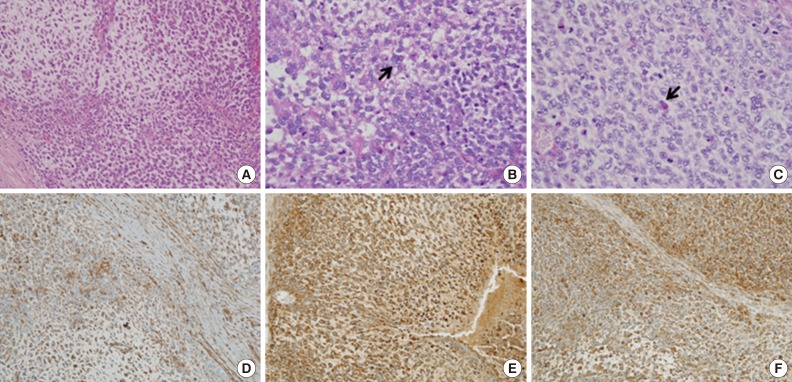
Fig. 1 A dynamic computed tomography study shows a 13-cm-sized hypoattenuating mass with lobulated contour in the right hepatic lobe, in segments 5 and 6.
Fig. 2 The cut section shows a large variegated solid and firm mass, composed of a grey-to-yellow solid area and a dark red hemorrhagic area.
Fig. 3 Microscopic studies of the liver mass show sheets of undifferentiated oval, spindle-shaped, or stellate tumor cells in myxoid or fibrous stroma (A). Intracytoplasmic eosinophilic globules (arrows) are seen in periodic acid-Schiff (PAS, B) and diastase-resistant PAS (C). The cytoplasms of tumor cells are diffusely stained by vimentin (D), alpha 1-antitrypsin (E), and alpha 1-antichymotrypsin (F).
Fig. 1
Fig. 2
Fig. 3
Undifferentiated Embryonal Sarcoma in Adult Liver

 E-submission
E-submission