Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(2); 2012 > Article
-
Case Report
Liquid-Based Cytology of Villoglandular Adenocarcinoma of the Cervix: A Report of 3 Cases - Younghwa Choi, Haeryoung Kim, Haiyoung Choi, Daehyun Hwang, Gheeyoung Choe, Jin-Haeng Chung, So Yeon Park, Hye Seung Lee, Jin Ho Paik, Hyo Jin Park
-
Korean Journal of Pathology 2012;46(2):215-220.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.2.215
Published online: April 25, 2012
Department of Pathology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- Corresponding Author: Haeryoung Kim, M.D. Department of Pathology, Seoul National University Bundang Hospital, 82 Gumi-ro 173 beon-gil, Bundang-gu, Seongnam 463-707, Korea. Tel: +82-31-787-7715, Fax: +82-31-787-4012, medannabel@gmail.com
• Received: January 25, 2012 • Accepted: March 6, 2012
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Villoglandular adenocarcinoma (VGA) is a rare subtype of cervical adenocarcinoma with a more favorable prognosis compared to conventional adenocarcinomas. Although the tumors are usually recognized on colposcopic examination due to the mainly exophytic growth pattern, they may be underdiagnosed as benign lesions by cytology because of their minimal cytologic atypia. We report the liquid-based cytology (LBC) findings of three histologically confirmed VGAs which we have recently identified. They were characterized by hypercellular smears on low-power examination with smooth-bordered three-dimensional papillary fragments. The nuclei were relatively uniform with irregular nuclear membranes. Nucleoli were small but distinct and macronucleoli were also seen. The abnormal architectural patterns such as papillary structures and nuclear overlapping and nuclear hyperchromasia are important clues to the diagnosis of VGA. In addition, nuclear membrane irregularity and prominent nucleoli can be recognized on LBC specimens, further facilitating its diagnosis.
- Case 1
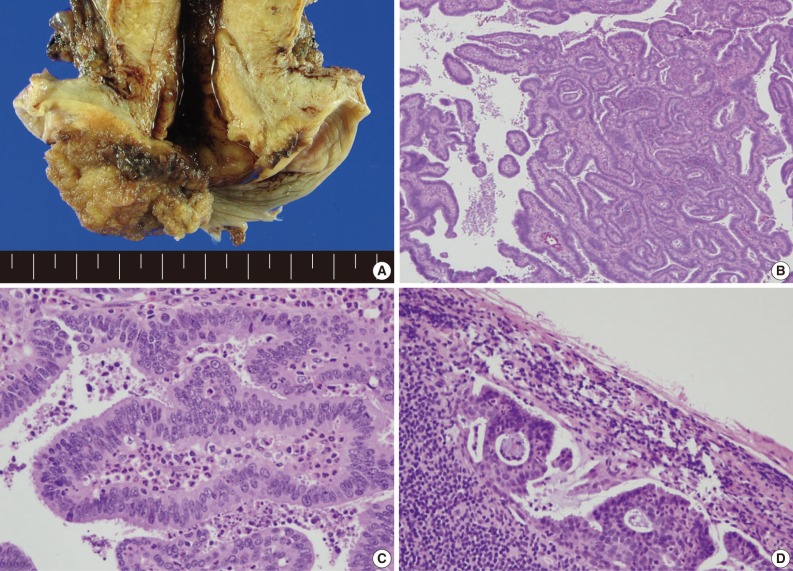
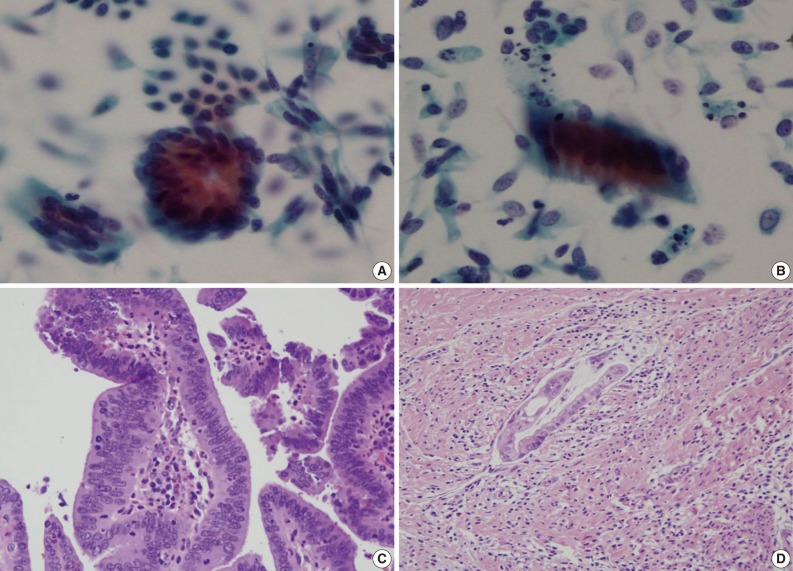
- A 39-year-old woman visited the outpatient clinic with a chief complaint of vaginal bleeding. Colposcopic examination revealed a friable-looking 5×5 cm-sized solid mass in the posterior lip of the uterine cervix which bled easily. A cervicovaginal cytology and a punch biopsy of the lesion was taken. The SurePath™ preparation yielded a hypercellular sample, composed of isolated or tightly cohesive multilayered clusters of neoplastic endocervical cells in a clean background. A few papillary frond-like structures with smooth contours were seen at low power magnification (Fig. 1A). Nuclear overlapping was also seen. The individual cells showed high nuclear: cytoplasmic ratios, and the nuclei were round to oval with some nuclear membrane irregularity. The nuclei were hyperchromatic with evenly distributed granular chromatin, and nucleoli were distinct. Mitoses and apoptotic debris were occasionally observed (Fig. 1B-E). Based on these cytologic findings, the diagnosis of endocervical-type adenocarcinoma was made. The cervical punch biopsy specimen revealed papillary structures with central fibrovascular cores. The papillae were lined by pseudostratified tall columnar non-mucinous epithelium and the degree of nuclear atypia was mild to moderate. Abundant neutrophils and lymphoplasmacytes infiltrated the fibrovascular cores. The patient later underwent a radical hysterectomy with bilateral salpingo-oophorectomy and a bulky exophytic friable papillary mass measuring 5×3×1.5 cm was seen (Fig. 2A-C). The mass was confined to the uterine cervix; however, one pelvic lymph node harbored a metastatic carcinoma (Fig. 2D). The patient received 2 cycles of adjuvant cisplatin treatment and radiotherapy, and is currently healthy at 7 months postoperatively without evidence of disease recurrence.
- Case 2
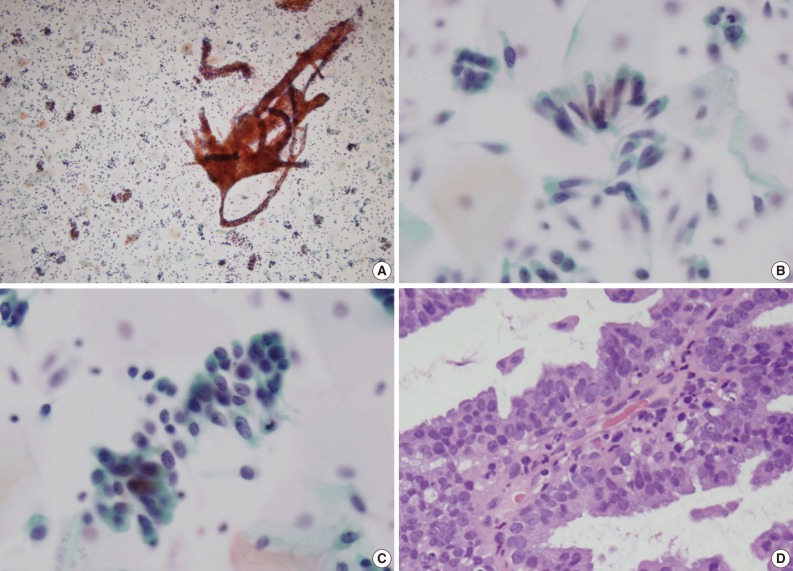
- A 55-year-old woman was referred from a local clinic for further evaluation of a cervical mass. The cervicovaginal smear taken at the local clinic was said to be diagnosed as "reactive cellular changes associated with inflammation." Colposcopic examination demonstrated an exophytic mass-like lesion of 2 cm in maximum dimension which was friable to touch. The SurePath™ preparation revealed numerous crowded sheets of columnar cells and papillary structures in an inflammatory background. Nuclear overlapping was seen in the cellular sheets (Fig. 3A, B). Many individually scattered columnar cells were also seen. The nuclei were uniform, small, elongated and nucleoli were small but visible. The chromatin was moderately granular and evenly distributed. Mitotic figures were occasionally seen. A diagnosis of adenocarcinoma was rendered on the basis of these cytologic findings. A punch biopsy, taken at the same time as the cytology, demonstrated features of VGA characterized by branching or finger-like papillary structures with fibrovascular cores containing an inflammatory infiltrate (Fig. 3C). The papillae were lined by tall, uniform, pseudostratified columnar epithelial cells. The nuclei were uniform and oval to elongated with mild to moderate nuclear atypia. A radical hysterectomy with bilateral salpingo-oophorectomy was performed and the tumor was consistent with a VGA of the cervix measuring 2×1×0.8 cm without evidence of extracervical extension or nodal metastasis. However, endolymphatic tumor emboli were occasionally observed in the invasive fronts of the tumor (Fig. 3D). There was no evidence of other coexistent lesions such as adenocarcinoma in situ or cervical intraepithelial neoplasia. An ancillary genotyping test for human papillomavirus (HPV; GG HPV genotyping chip, Goodgene, Seoul, Korea) revealed the presence of HPV infection, type undetermined. The patient received radiation therapy and showed no evidence of disease recurrence on her latest clinic visit at 13 months postoperatively.
- Case 3
- A 48-year-old woman visited the health promotion center for a comprehensive medical testing. The SurePath™ showed isolated or small sheets of columnar cells with slightly increased nuclear : cytoplasmic ratio in an inflammatory background. The nuclei were small, round to oval shaped and hyperchromatic. A diagnosis of "reactive cellular changes" was initially given; however, a punch biopsy taken simultaneously revealed a VGA, and on retrospective review of the LBC slide, atypical cytoarchitectural features such as papillary clusters (Fig. 4A), nuclear palisading (Fig. 4B) and nuclear overlapping were seen, and some clusters contained atypical cells with nuclear membrane irregularity and prominent nucleoli. Moreover, some atypical cells demonstrated macronucleoli (Fig. 4C). The biopsy specimen revealed an exuberant papillary proliferation of columnar epithelial cells with central fibrovascular cores (Fig. 4D). Intracytoplasmic mucin was found in a majority of the tumor cells. The individual cells showed mild to moderate nuclear pleomorphism and occasional mitotic figures. The fibrovascular cores were heavily infiltrated by neutrophils. The patient subsequently underwent a radical hysterectomy at an outside hospital, which revealed a VGA confined to the uterine cervix. She visited the clinic recently for a routine check-up and is free of disease recurrence at 23 months postoperatively.
CASE REPORTS
- VGA is a rare subtype of cervical adenocarcinoma first described by Young and Scully,2 which has been reported to have a more favorable prognosis compared to conventional adenocarcinomas.1 It is characterized by numerous papillary villous structures which are lined by epithelial cells with only mild cytologic atypia. The epithelial cells may be mucinous or non-mucinous, and the central fibrovascular cores of the papillae usually have variable number of inflammatory cells. Associations between VGA and HPV and oral contraceptives have been reported.3,5,7,13,14
- The diagnosis of VGA has been demonstrated to be rather challenging on cytology as the cytologic features may be deceptively bland-looking, resulting in its misdiagnosis as reactive glandular cells. Indeed, the initial cytologic impression in one of our three cases was a reactive lesion and the neoplastic cell clusters could have been overlooked if it had not been for the simultaneous punch biopsy specimen that harbored a VGA. There are only a few reports to date describing the cytologic features of VGA; most reports are descriptions of conventional smears,8-11 and one other recent case report has described the ThinPrep LBC findings of an "endocervical adenocarcinoma with villoglandular features."12 We report for the first time the SurePath™ LBC findings of VGA.
- The cytologic features of our three cases were in many aspects compatible with the features previously described for conventional smears.8-11 In detail, the specimens were highly cellular in all three cases, and they all showed three-dimensional papillary structures with smooth contours. On higher magnification, nuclear crowding and overlapping could be seen and the individual tumor cells demonstrated increased nuclear: cytoplasmic ratios and nuclear hyperchromasia. Scattered mitotic figures were seen. On the other hand, while the previously reported VGAs were not generally associated with isolated single cells, all three cases in our series demonstrated this feature. In addition, the nuclei were oval or elongated but also somewhat irregular in shape and nucleoli were prominent, with some cells even demonstrating macronucleoli, in contrast to the previously reported VGAs where the nuclei were small, uniform and round to oval and nucleoli were indistinct or absent. There was also no evidence of a tumor diasthesis - the backgrounds of our three cases were rather clean except for scattered inflammatory cells. The latter differences may be attributed to the morphologic changes inherent to LBC preparations, such as the reduced background material and the fragmentation of cell clusters. However, as the nuclear details are better preserved on LBC specimens compared to conventional smears, important nuclear changes including nuclear membrane irregularities and prominent nucleoli can be appreciated better, facilitating the diagnosis of this well-differentiated type of adenocarcinoma by cytology. Prominent nucleoli and thick nuclear membranes have also been described by Wagner et al.12 in their LBC (ThinPrep)-based case report.
- It is also noteworthy that two patients in this series had risk factors for a poorer prognosis: one had lymph node metastasis, and the other case was associated with endolymphatic tumor emboli at the invasive front of the tumor. Although VGA has been associated with infrequent lymphovascular invasion and an excellent prognosis, with most case reports having demonstrated no evidence of recurrence after long-term follow-up,2,5 a few have reported more advanced disease in occasional instances.6,14 Kaku et al.6 emphasized that prior to making a decision to treat VGAs with a conservative approach, it is necessary to search for histologic signs of poor prognosis such as lymphovascular invasion.
- The differential diagnoses of VGA encompass reactive endocervical cells, tubal metaplasia, adenocarcinoma in situ, squamous dysplasia involving the endocervical glands, and other types of cervical adenocarcinomas, such as serous papillary carcinomas.8-12 Although the lack of obvious cytologic atypia may lead to the underdiagnosis of VGA, the presence of architectural abnormalities such as papillary fragments and nuclear crowding and overlapping are helpful clues to suspect the possibility of this tumor, and the presence of nuclear membrane irregularities and prominent nucleoli on LBC preparations also suggest the possibility of adenocarcinoma. Tubal metaplasia is characterized by clusters of oval nuclei, finely granular chromatin, inconspicuous nucleoli and cilia. The cytologic features of endocervical adenocarcinoma and adenocarcinoma in situ may be similar to VGA, especially in LBC specimens where the nuclear features appear more pronounced; however, the typical features of peripheral nuclear palisading (feathering) in endocervical adenocarcinomas has been observed infrequently in VGAs, while VGAs demonstrate smooth-bordered three-dimensional papillary structures which are not frequently seen in the former lesions. Serous adenocarcinomas are usually characterized by overt cytologic atypia which is easily recognizable in both conventional smears and in LBC specimens. Squamous intraepithelial lesions involving the endocervical glands may also be considered in the differential diagnosis; however, these lesions demonstrate hyperchromatic nuclei, high nuclear: cytoplasmic ratios, small or inconspicuous nucleoli and cellular clusters show a loss of polarity. In addition, scattered atypical squamous cells are usually recognizable in the background.
- In conclusion, VGA is a rare well-differentiated form of cervical adenocarcinoma that may be diagnosed at an advanced stage despite its grossly recognizable exophytic growth pattern and should not be missed on cytologic examination. In the absence of clinical information, the abnormal architectural patterns such as three-dimensional papillary structures, nuclear overlapping and nuclear hyperchromasia are important clues to suspect the possibility of a VGA. In addition, in contrast to conventional smears in which the tumor cells may be deceptively bland-looking, LBC preparations of VGA show better preserved nuclear details such as prominent nucleoli and irregular nuclear membranes which should facilitate its diagnosis.
DISCUSSION
- 1. Heatley MK. Villoglandular adenocarcinoma of the uterine cervix: a systematic review of the literature. Histopathology 2007; 51: 268-269. ArticlePubMed
- 2. Young RH, Scully RE. Villoglandular papillary adenocarcinoma of the uterine cervix: a clinicopathologic analysis of 13 cases. Cancer 1989; 63: 1773-1779. ArticlePubMed
- 3. González-Bosquet E, Suñol M, Morante D, Gomez Latre M, Callejo J, Lailla JM. Villoglandular papillary adenocarcinoma of the uterine cervix: a case report and literature review. Eur J Gynaecol Oncol 2009; 30: 211-213. PubMed
- 4. Hopson L, Jones MA, Boyce CR, Tarraza HM Jr. Papillary villoglandular carcinoma of the cervix. Gynecol Oncol 1990; 39: 221-224. ArticlePubMed
- 5. Jones MW, Silverberg SG, Kurman RJ. Well-differentiated villoglandular adenocarcinoma of the uterine cervix: a clinicopathological study of 24 cases. Int J Gynecol Pathol 1993; 12: 1-7. PubMed
- 6. Kaku T, Kamura T, Shigematsu T, et al. Adenocarcinoma of the uterine cervix with predominantly villogladular papillary growth pattern. Gynecol Oncol 1997; 64: 147-152. ArticlePubMed
- 7. Stanley-Christian H, Heim BK, Hines JF, Hall KL, Willett GD, Barnes WA. Villoglandular adenocarcinoma of the cervix: a report of three cases and review of the literature. Gynecol Oncol 1997; 66: 327-330. ArticlePubMed
- 8. Ballo MS, Silverberg SG, Sidawy MK. Cytologic features of well-differentiated villoglandular adenocarcinoma of the cervix. Acta Cytol 1996; 40: 536-540. ArticlePubMed
- 9. Chang WC, Matisic JP, Zhou C, Thomson T, Clement PB, Hayes MM. Cytologic features of villoglandular adenocarcinoma of the uterine cervix: comparison with typical endocervical adenocarcinoma with a villoglandular component and papillary serous carcinoma. Cancer 1999; 87: 5-11. ArticlePubMed
- 10. Khunamornpong S, Siriaunkgul S, Suprasert P. Well-differentiated villoglandular adenocarcinoma of the uterine cervix: cytomorphologic observation of five cases. Diagn Cytopathol 2002; 26: 10-14. ArticlePubMed
- 11. Novotny DB, Ferlisi P. Villoglandular adenocarcinoma of the cervix: cytologic presentation. Diagn Cytopathol 1997; 17: 383-387. ArticlePubMed
- 12. Wagner DG, Weisensel J, Mentrikoski MJ, Leo SD, Bonfiglio TA, Hoda RS. ThinPrep Pap test of endocervical adenocarcinoma with lymph node metastasis: report of a case in a 17-year-old woman. Diagn Cytopathol 2010; 38: 633-638. ArticlePubMed
- 13. Giordano G, D'Adda T, Gnetti L, Merisio C, Gabrielli M, Melpignano M. Villoglandular adenocarcinoma of the cervix: two new cases with morphological and molecular study. Int J Gynecol Pathol 2007; 26: 199-204. PubMed
- 14. Yamazawa K, Matsui H, Seki K, et al. Human papillomavirus-positive well-differentiated villoglandular adenocarcinoma of the uterine cervix: a case report and review of the literature. Gynecol Oncol 2000; 77: 473-477. ArticlePubMed
REFERENCES
Fig. 1Liquid-based cytology features of case 1. (A) Low-power magnification demonstrates a three-dimensional papillary tissue fragment (right) and smaller cellular clusters with individually scattered tumor cells in the background (Papanicolaou stain). (B, C) The edge of the papillary frond is relatively smooth and the fibrovascular core is infiltrated by neutrophils. Nuclear overlapping is seen within the cellular clusters. (D, E) The nuclei are round to oval and show distinct nucleoli and some clumped chromatin. Frequent apoptotic bodies are also seen.
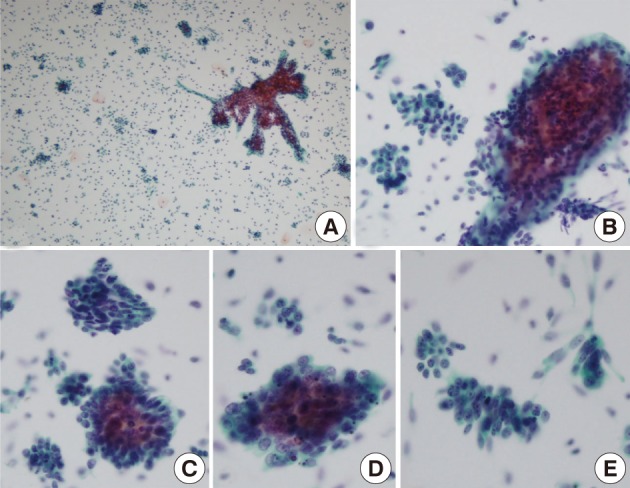
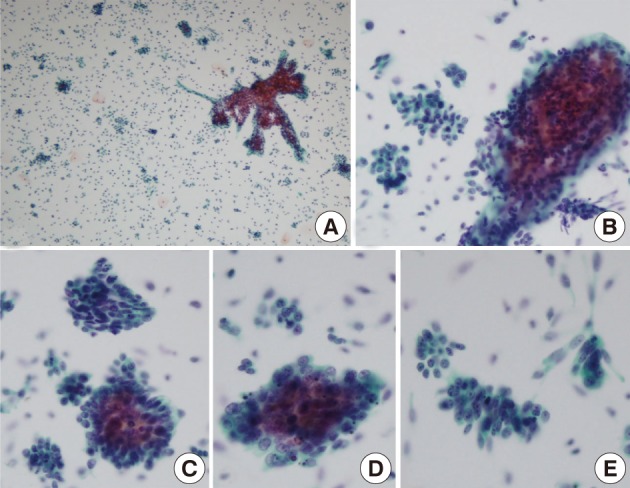
Fig. 2Case 1. (A) Gross examination of the hysterectomy specimen reveals an exophytic papillary cervical mass, measuring 5 cm in maximal dimension. (B) The entire tumor consists of villous projections, lined by tall columnar non-mucinous cells with mild nuclear atypia. (C) A moderate neutrophilic infiltrate is seen within the central cores. (D) Lymph node metastasis is seen in a pelvic lymph node.
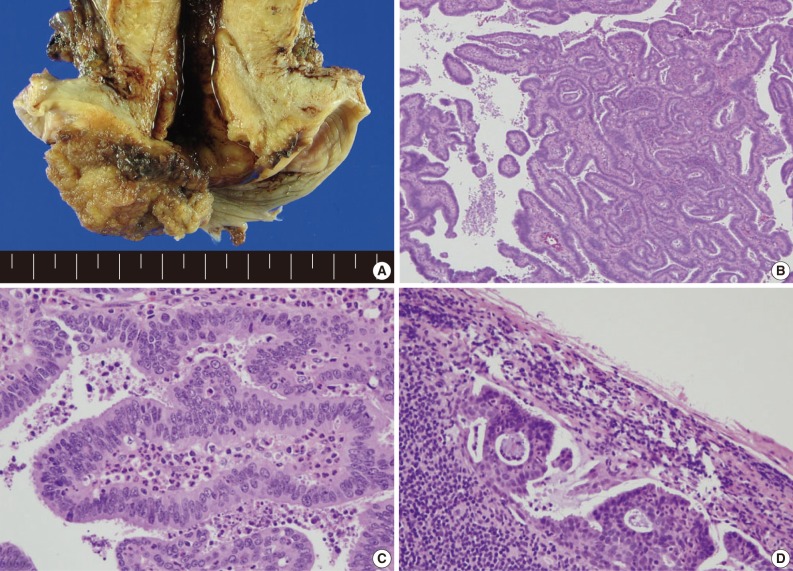
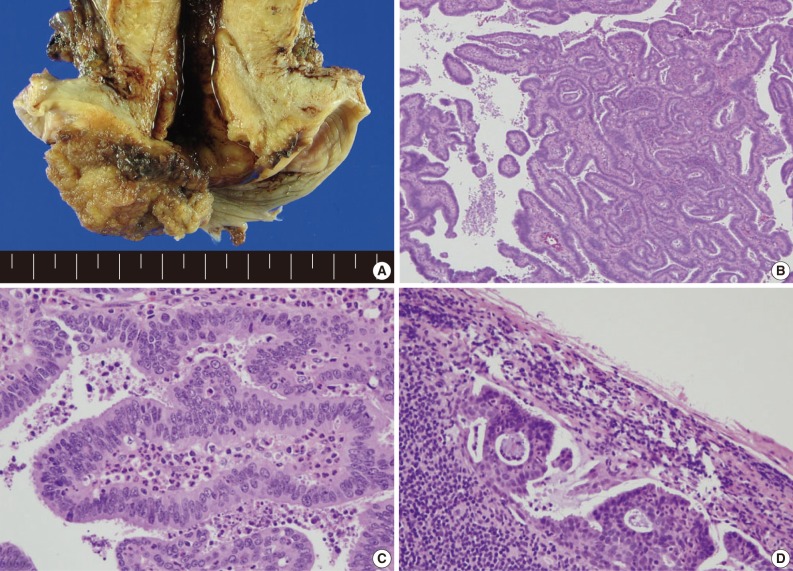
Fig. 3Case 2. (A, B) Liquid-based cytology of case 2 demonstrates tumor cells arranged in rosette-like structures (A) and cellular strips (B). The cellular clusters and strip have a smooth cytoplasmic border. Individually scattered atypical glandular cells are seen demonstrating elongated, hyperchromatic nuclei and irregular nuclear membranes (A, B, Papanicolaou stain). (C) Histologic examination of the hysterectomy specimen demonstrates the long villous fronds lined by mildly atypical columnar cells. (D) Lymphovascular space invasion is evident in the deeper invasive portion of the tumor.
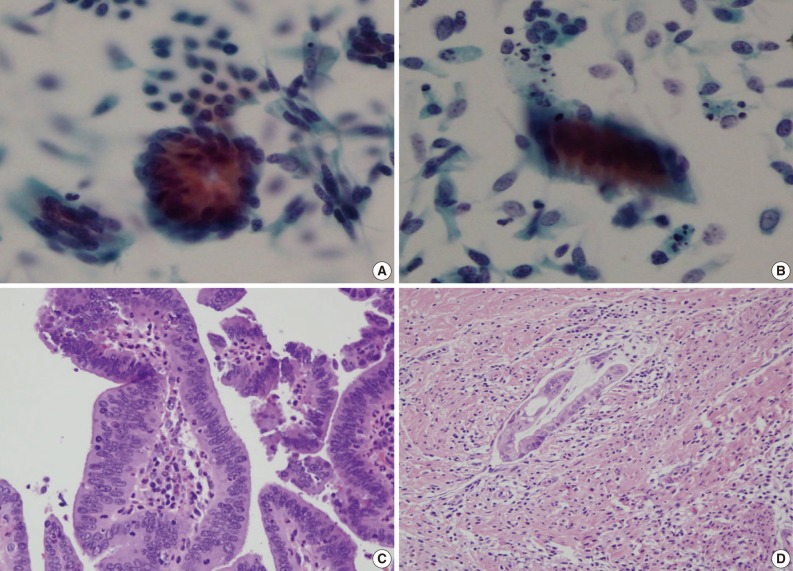
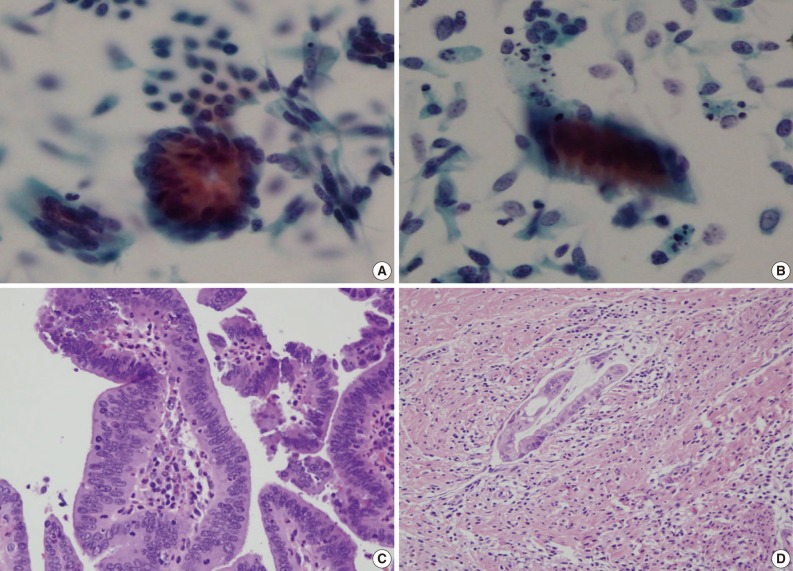
Fig. 4Case 3. (A) The liquid-based cytology preparation demonstrates three-dimensional papillary structures with long fronds. Smaller cellular clusters and individually scattered tumor cells are seen in the background (Papanicolaou stain). (B, C) On higher power magnification, the tumor cells are arranged in loose strips and clusters with some nuclear palisading. The nuclei are oval to elongated, and somewhat irregular in shape. Prominent nucleoli are seen in (C). (D) Case 3 is characterized by papillary structures lined by mucin-containing columnar cells.
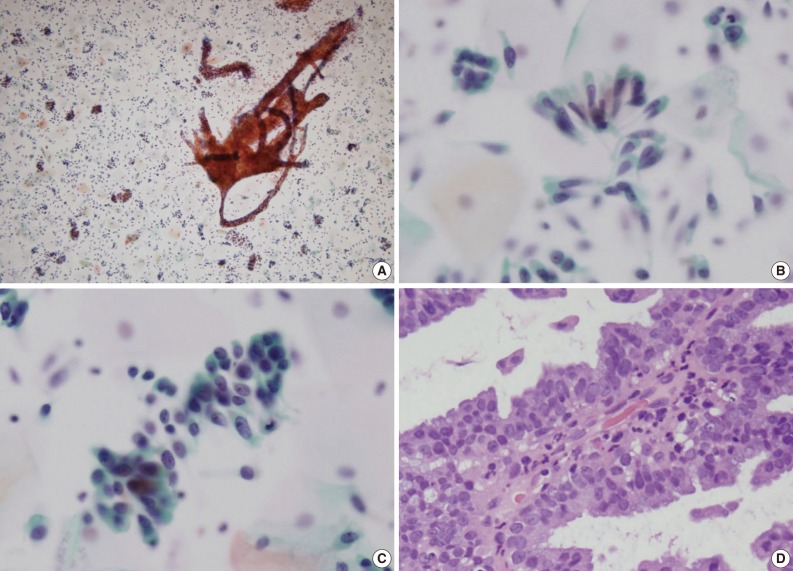
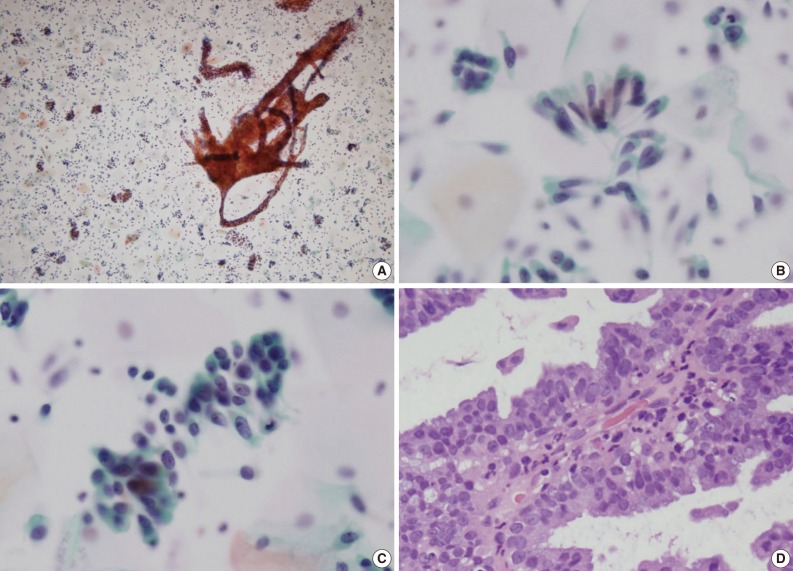
Figure & Data
References
Citations
Citations to this article as recorded by 

- Villoglandular Carcinoma of the Uterine Cervix: Clinic‐Cytopathological‐Histological Features of a Rare Case With Brief Review of the Literature
Neelam Sood, Ruchika Gupta, Sanjay Gupta
Cytopathology.2025; 36(6): 596. CrossRef - Villoglandular adenocarcinoma of the uterine cervix: a systematic review and meta-analysis
Anna K. Dietl, Matthias W. Beckmann, Konrad Aumann
Archives of Gynecology and Obstetrics.2021; 304(2): 317. CrossRef - Les lésions glandulaires du col utérin : cas no 4
Catherine Genestie, Chiraz Hadj Kacem, Pierre Duvillard
Annales de Pathologie.2016; 36(3): 192. CrossRef
Liquid-Based Cytology of Villoglandular Adenocarcinoma of the Cervix: A Report of 3 Cases

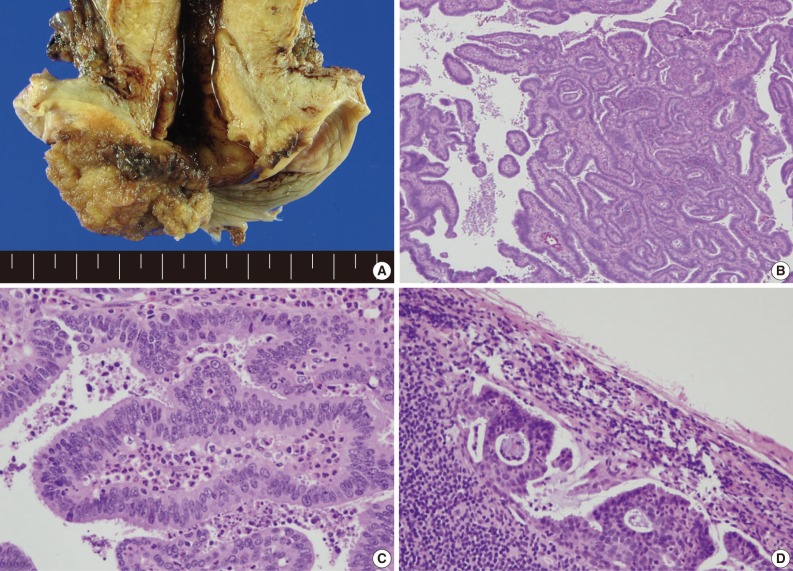
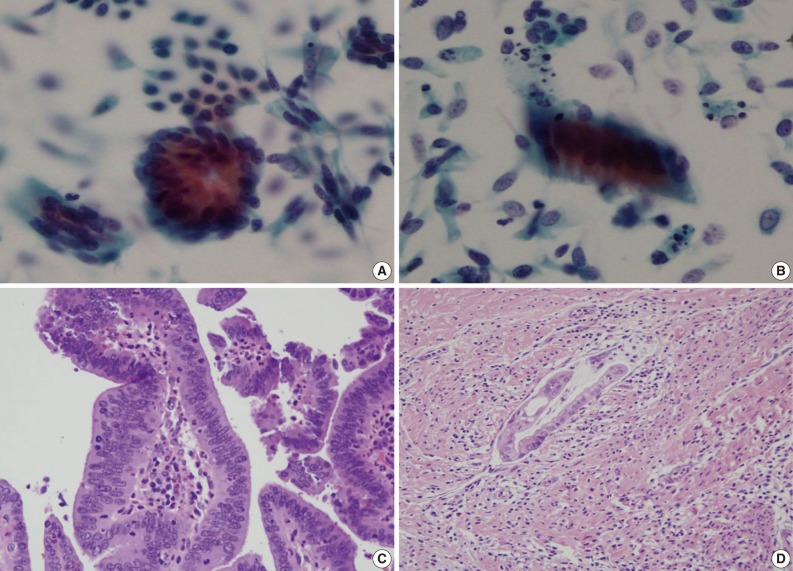
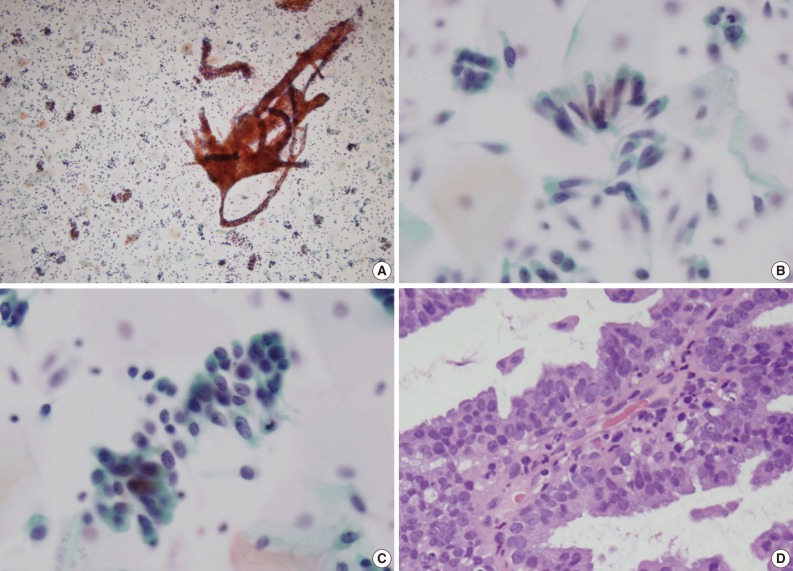
Fig. 1 Liquid-based cytology features of case 1. (A) Low-power magnification demonstrates a three-dimensional papillary tissue fragment (right) and smaller cellular clusters with individually scattered tumor cells in the background (Papanicolaou stain). (B, C) The edge of the papillary frond is relatively smooth and the fibrovascular core is infiltrated by neutrophils. Nuclear overlapping is seen within the cellular clusters. (D, E) The nuclei are round to oval and show distinct nucleoli and some clumped chromatin. Frequent apoptotic bodies are also seen.
Fig. 2 Case 1. (A) Gross examination of the hysterectomy specimen reveals an exophytic papillary cervical mass, measuring 5 cm in maximal dimension. (B) The entire tumor consists of villous projections, lined by tall columnar non-mucinous cells with mild nuclear atypia. (C) A moderate neutrophilic infiltrate is seen within the central cores. (D) Lymph node metastasis is seen in a pelvic lymph node.
Fig. 3 Case 2. (A, B) Liquid-based cytology of case 2 demonstrates tumor cells arranged in rosette-like structures (A) and cellular strips (B). The cellular clusters and strip have a smooth cytoplasmic border. Individually scattered atypical glandular cells are seen demonstrating elongated, hyperchromatic nuclei and irregular nuclear membranes (A, B, Papanicolaou stain). (C) Histologic examination of the hysterectomy specimen demonstrates the long villous fronds lined by mildly atypical columnar cells. (D) Lymphovascular space invasion is evident in the deeper invasive portion of the tumor.
Fig. 4 Case 3. (A) The liquid-based cytology preparation demonstrates three-dimensional papillary structures with long fronds. Smaller cellular clusters and individually scattered tumor cells are seen in the background (Papanicolaou stain). (B, C) On higher power magnification, the tumor cells are arranged in loose strips and clusters with some nuclear palisading. The nuclei are oval to elongated, and somewhat irregular in shape. Prominent nucleoli are seen in (C). (D) Case 3 is characterized by papillary structures lined by mucin-containing columnar cells.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Liquid-Based Cytology of Villoglandular Adenocarcinoma of the Cervix: A Report of 3 Cases

 E-submission
E-submission
 PubReader
PubReader Cite this Article
Cite this Article