Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 59(6); 2025 > Article
-
Original Article
Diagnostic value of cytology in detecting human papillomavirus–independent cervical malignancies: a nation-wide study in Korea -
Hye-Ra Jung1
 , Junyoung Shin2
, Junyoung Shin2 , Chong Woo Yoo2
, Chong Woo Yoo2 , Eun Na Kim3
, Eun Na Kim3 , Cheol Lee3
, Cheol Lee3 , Kyeongmin Kim4
, Kyeongmin Kim4 , Ho-chang Lee5
, Ho-chang Lee5 , Yonghee Lee6, Ji Hye Kim7
, Yonghee Lee6, Ji Hye Kim7 , Soo Jin Jung8
, Soo Jin Jung8 , Yumin Chung9
, Yumin Chung9 , Joo Yeon Kim10
, Joo Yeon Kim10 , Hye Eun Park11
, Hye Eun Park11 , Tae Hoen Kim12
, Tae Hoen Kim12 , Wonae Lee13
, Wonae Lee13 , Min-Sun Cho14
, Min-Sun Cho14 , Ran Hong15
, Ran Hong15 , Yoon Jung Choi16
, Yoon Jung Choi16 , Younghee Choi17
, Younghee Choi17 , Young Sub Lee18
, Young Sub Lee18 , Sang-Ryung Lee19
, Sang-Ryung Lee19 , Myunghee Kang20
, Myunghee Kang20 , Young Jin Seo21
, Young Jin Seo21 , Seung-Sook Lee22
, Seung-Sook Lee22 , Yoon-Jung Hwang23
, Yoon-Jung Hwang23 , Hyun-Jung Kim24
, Hyun-Jung Kim24
-
Journal of Pathology and Translational Medicine 2025;59(6):444-452.
DOI: https://doi.org/10.4132/jptm.2025.10.21
Published online: November 11, 2025
1Department of Pathology, Keimyung University School of Medicine, Daegu, Korea
2Department of Pathology, National Cancer Center, Goyang, Korea
3Department of Pathology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
4Department of Pathology, Soonchunhyang University Seoul Hospital, Seoul, Korea
5Department of Pathology, Chungbuk University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea
6Department of Pathology, Ajou University School of Medicine, Suwon, Korea
7Department of Pathology, Ulsan University, Ulsan, Korea
8Department of Pathology, Inje University Busan Paik Hospital, Busan, Korea
9Department of Pathology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
10Department of Pathology, Inje University Haeundae Paik Hospital, Busan, Korea
11Department of Pathology, Seoul Metropolitan Government Boramae Hospital, Seoul National University, Seoul, Korea
12Department of Pathology, Bundang Medical Center, CHA University, Seongnam, Korea
13Department of Pathology, Dankook University Hospital, Cheonan, Korea
14Department of Pathology, Ewha Women’s University College of Medicine, Seoul, Korea
15Department of Pathology, Chosun University Hospital, Gwangju, Korea
16Department of Pathology, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
17Department of Pathology, Hallym University Dongtan Sacred Heart Hospital, Hwaseong, Korea
18Department of Pathology, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
19Department of Pathology, CHA Gangnam Medical Center, CHA University, Seoul, Korea
20Department of Pathology, Gachon University Gil Medical Center, Incheon, Korea
21Department of Pathology, National Forensic Service Daegu Institute, Daegu, Korea
22Department of Pathology, Korea Cancer Center Hospital, Seoul, Korea
23Department of Pathology, Seoul National University Bundang Hospital, Seongnam, Korea
24Department of Pathology, Inje University Sanggye Paik Hospital, Seoul, Korea
- Corresponding Author Hyun-Jung Kim, MD, Department of Pathology, Inje University Sanggye Paik Hospital, 1342 Dongil-ro, Nowon-gu, Seoul 01757, Korea Tel: +82-2-950-1261 Fax: +82-2-951-6964 E-mail: hjkim@paik.ac.kr
© The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,882 Views
- 104 Download
Abstract
-
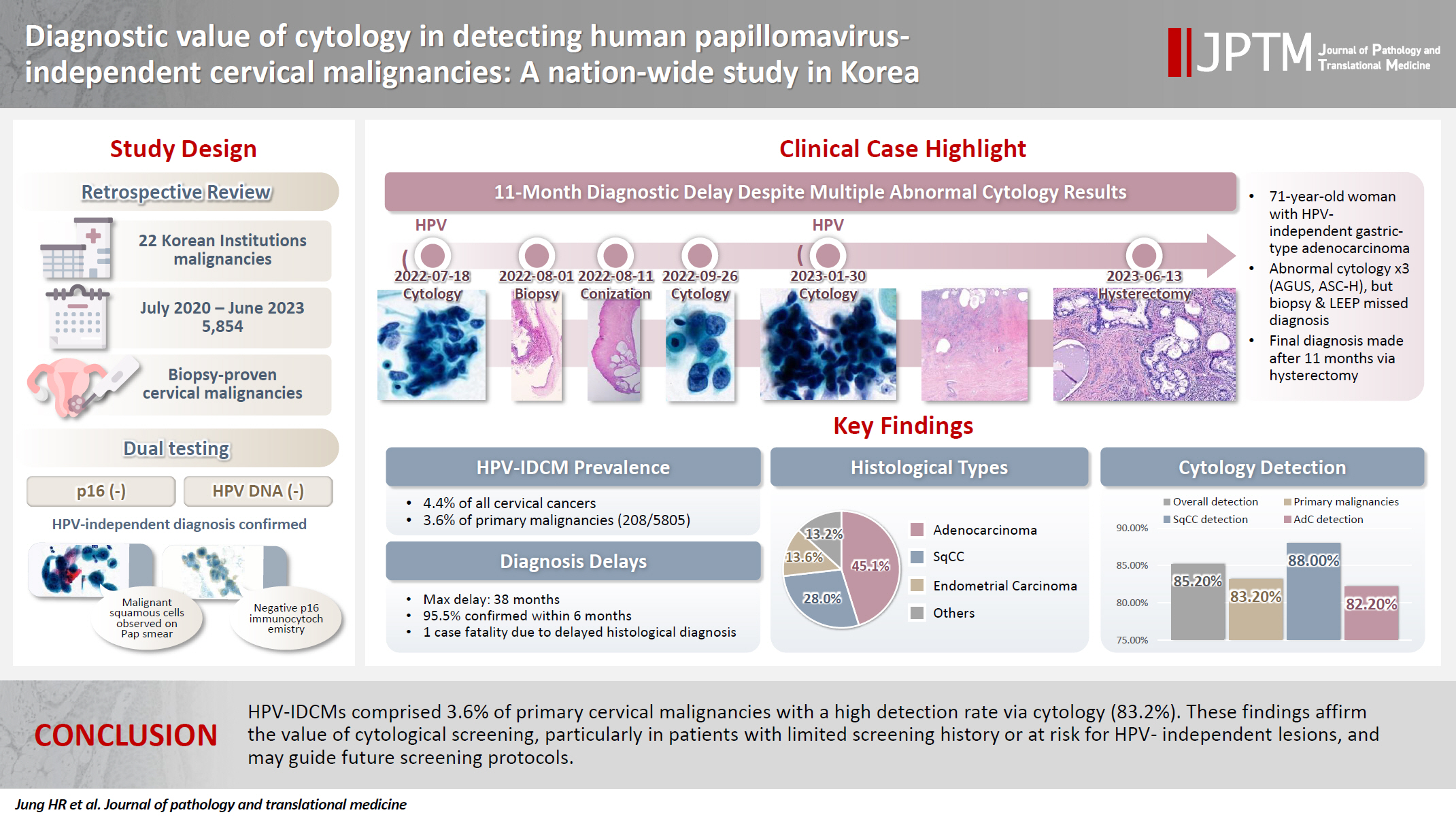
Background
- Human papillomavirus (HPV) independent cervical malignancies (HPV-IDCMs) have recently been classified by the World Health Organization (WHO) 5th edition. These malignancies have historically received limited attention due to their rarity and the potential for evasion of HPV-based screening.
-
Methods
- We retrospectively reviewed 5,854 biopsy-confirmed cervical malignancies from 22 institutions over 3 years (July 2020–June 2023). Histologic classification followed the WHO guidelines. HPV independence was confirmed by dual negativity for p16 and HPV; discordant cases (p16-positive/HPV-negative) underwent additional HPV testing using paraffin-embedded tissue. Cytological results were matched sequentially to histological confirmation.
-
Results
- The prevalence of HPV-IDCM was 4.4% (257/5,854) overall and was 3.6% (208/5,805 cases) among primary cervical malignancy. Patient age of HPV-IDCM was 29 to 89 years (median, 57.79). Its histologic subtypes included primary adenocarcinoma (n = 116), endometrial adenocarcinoma (n = 35), squamous cell carcinoma (n = 72), metastatic carcinoma (n = 14), carcinoma, not otherwise specified (n = 10), neuroendocrine carcinoma (n = 3), and others (n = 7). Among 155 cytology-histological matched cases, the overall and primary Pap test detection rates were 85.2% (132/155) and 83.2% (104/125), respectively. The interval between cytology and histologic confirmation extended up to 38 months.
-
Conclusions
- HPV-IDCMs comprised 3.6% of primary cervical malignancies with a high detection rate via cytology (83.2%). These findings affirm the value of cytological screening, particularly in patients with limited screening history or at risk for HPV-independent lesions, and may guide future screening protocols.
- The Papanicolaou (Pap) test has markedly contributed to the global reduction in the incidence and mortality rates of cervical cancer. In the United States, the number of new cervical cancer cases per 100,000 individuals declined from 14.81 in 1975 to 6.67 in 2018 [1-3]. In South Korea, the incidence rate decreased from 9.2 to 6.2 per 100,000, and the mortality rate fell from 3.4 to 2.5 per 100,000 population between 2001 and 2022 [4].
- With increasing recognition of the role of persistent high-risk human papillomavirus (HPV) infection in cervical carcinogenesis, HPV testing has become a primary screening modality in many Western countries [5-7]. In 2014, the US Food and Drug Administration (FDA) approved the cobas HPV test (Roche Diagnostics, Basel, Switzerland) as a stand-alone screening method for women aged 25 and older [8-10].
- This shift has been accelerated by the widespread adoption of HPV vaccination. The efficacy of the HPV vaccines in preventing high-grade cervical lesions has been well established. A nationwide Swedish study (2006–2017) reported incidence rates of 0.51, 0.37, and 0.1 per 100,000 for unvaccinated individuals, those vaccinated between 17-30, and those vaccinated before age 17, respectively [11]. Since 2012, the Korean national immunization program has included HPV vaccination for girls under 13 years of age [12].
- The 5th edition of the World Health Organization (WHO) classification of Female Genital Tumors formally recognizes HPV-independent cervical malignancies (HPV-IDCMs) and their precursor lesions in both squamous and glandular categories [13]. The 5 recognized glandular subtypes include gastric, clear cell, mesonephric, endometrioid, and not otherwise specified (NOS). According to the WHO classification, HPV-independent tumors account for approximately 5%–7% of squamous cell carcinomas (SqCCs) and up to 20% of adenocarcinomas. Emerging HPV-independent neoplasms include intraepithelial neoplasia, SqCC, and precursor lesions associated with uterine prolapse and lichen planus (LP) [14-17].
- In Japan, the overall prevalence of gynecologic tumors has changed, with rising rates of endometrial and ovarian carcinomas and declining cervical carcinoma rates [18]. Similarly, Taiwan has reported a proportional increase in adenocarcinomas relative to SqCC [19]. In Korea, the most recent data (2024) show a histological distribution of 60.9% SqCC and 23.1% adenocarcinoma [20].
- The primary aim of this study was to assess the prevalence rate of HPV-IDCM and to evaluate the diagnostic utility of the Pap test during this period of dynamic screening practices and histologic trends.
INTRODUCTION
- Data collection
- A nationwide study of biopsy–proven cervical malignancies was conducted at 22 institutions across South Korea over 3 years (July 2020 to June 2023). All contributors were actively practicing gynecologic cytopathologists. A total of 5,854 cases were collected along with clinical data including patient age, specimen type, and survival status. Histological subtypes were classified according to the WHO classification of female genital tumors, 5th edition. HPV independence was determined by negativity for both p16INK4a (CDKNA2A) immunohistochemistry and HPV testing. For p16-positive and HPV-negative cases, additional HPV real-time PCR testing (Allplex HPV Detection, Seegene, Seoul, Korea) was performed using paraffin blocks (silica-membrane technology (QIAamp), Qiagen, Hilden, Germany). Highly sensitive molecular techniques for detecting HPV DNA or mRNA were not available for this study.
- Cytological-histological correlation
- Cytological findings were reviewed sequentially, based on temporal relationship to the histological confirmation. Among multiple cytology reports, the report most relevant to the histologic outcome was selected. Cytological diagnoses were classified according to the Bethesda System, 3rd edition. Detection rates included diagnoses of atypical squamous cells, undetermined significance (ASC-US), and atypical glandular cells, undetermined significance (AG-US) or higher.
- Interval to final diagnosis
- The interval between a significant cytological diagnosis and the initial histological diagnosis was assessed. Cases with an interval longer than 6 months were classified as delayed diagnoses.
MATERIALS AND METHODS
- Sample characteristics
- Overall, HPV-IDCM account for 4.4% (257/5,854) of all cases and 3.6% (208/5,805) of primary cervical malignancies (Fig. 1). Patient age of HPV-IDCM ranged from 29 to 89 years, with a median of 57.79 years. Of the 257 cases, the most common specimen type was punch biopsy (n = 158), followed by hysterectomy (n = 74), loop electrosurgical excision procedure conization (n = 18), and other excisions (n = 7). Among the 167 patients with available follow-up data, 137 were alive, 23 had died (due to disease or other causes), and seven were lost to follow-up (Table 1).
- Histologic types of HPV-IDCM
- Histologic subtypes were as follows; primary adenocarcinoma (n = 116), which comprised gastric (n = 41), NOS (n = 37), clear cell (n = 17), mesonephric (n = 7), adenocarcinoma in situ (AIS) (n = 14); endometrial adenocarcinoma (n = 35); SqCC (n = 72); metastatic carcinoma (n = 14); carcinoma, NOS (n = 10); neuroendocrine carcinoma (n = 3); and other histological malignancies (n = 7) (Table 2).
- Cyto-pathologic correlation
- Among 155 cytology-histological matched cases, the overall/primary Pap test detection rate were 85.2% (132/155) and 83.2% (104/125) (Table 3). A case of 86-year-old women was cytologically evident SqCC. However, two times of real-time HPV-PCR test failed to demonstrate the HPV dependency. The subsequent biopsy showed invasive squamous carcinoma (Fig. 2). Despite the fact that no HPV relationship has been supported, the cytological abnormality has been detected in 29 out of 33 SqCCs (88%). In adenocarcinoma group, the cytological detection rate was 82.2% (65/79 cases).
- Interval of final histological diagnosis
- Of the matched cases, 148 (95.5%) received histological confirmation within 6 months, while seven cases experienced diagnostic delays from 7 to 38 months (Table 4). In our cohort, one patient with gastric-type adenocarcinoma had three abnormal cytology reports (AG-US, favor neoplastic and 2 times of ASC-H [atypical squamous cells, cannot exclude high-grade intraepithelial lesion]) and two negative HPV tests before a definitive diagnosis was made via hysterectomy 11 months later. (Fig. 3)
RESULTS
- In recent years, global cervical cancer screening has increasingly shifted toward primary HPV testing [1-3]. In 2014, the US FDA approved the cobas HPV test (Roche Diagnostics) for stand-alone cervical cancer screening in women aged ≥25 years [8-10].
- Despite this, a 2017 survey by the College of American Pathologists reported that nearly 60% of responding laboratories did not offer stand-alone primary HPV testing, concerns about the efficacy of cytology co-testing strategies [19,21,22].
- Our study aimed to assess the role of cytology in detecting HPV-independent precursors and malignancies. Recent literature highlights the presence of HPV-negative SqCC and precursor lesions. These cases showed frequent p16 negativity, nuclear p53 overexpression, and diverse genetic alterations (including PIK3CA, STK11, TP53, SMARCB2, and GNAS) along with the consistent presence of the Q472H germline polymorphism in the KDR gene and chromosome 3q gain [14]. HPV-negative precursors showed TP53-mutated differentiated cervical intraepithelial neoplasia and p53 wild-type verruciform intraepithelial neoplasia based on next-generation sequencing data [15].
- LP-associated HPV–independent SqCC of the vulva and vagina has also been reported [16], accounting for approximately 70% of vulvar SqCCs. The largest study to date has reported 38 cases of LP-associated SqCC and vulvar intraepithelial neoplasia.
- Additionally, a recent study described HPV-independent/p53-abnormal keratinizing SqCC associated with uterine prolapse. Cytological features of SqCC include prominent keratinizing, clear glycogen-rich cytoplasm, and some intracytoplasmic mucin [17].
- According to the WHO, HPV-independent invasive cervical SqCC accounts for approximately 5%–7% of all cases [11]. At least 90.9% of HPV-negative lesions were flagged by abnormal cytology [23]. Although large-scale cohort studies are lacking, HPV-negative squamous lesions appear prone to delayed histologic confirmation, particularly in case with indeterminate abnormal cytological findings (ASC-US, ASC-H, low-grade squamous intraepithelial lesion). In our series, one patient with high-grade intraepithelial lesion cytology experienced a 23-month delay before histologic diagnosis and subsequently died from disease, underscoring the importance of timely cytological evaluation.
- HPV-independent adenocarcinomas represent a minority of endocervical adenocarcinomas. According to the WHO 5th edition, HPV-independent adenocarcinoma of the uterine cervix include AIS, gastric type, clear cell type, mesonephric type, and NOS [11]. In our primary cohort, gastric-type adenocarcinoma was the most common subtype (41/116 cases). These tumors were associated with aggressive behavior including destructive invasion, extrauterine spread, and advanced-stage diagnosis [24,25].
- Cytologically, gastric-type adenocarcinomas may appear morphologically subtle, mimicking benign cervical glands with a low nuclear to cytoplasmic ratio [26]. Gastric-type adenocarcinoma accounts for nearly 20% of all cervical adenocarcinomas in Japan. A low detection rate was observed via cytology due to the high location of lesion in endocervical canal and bland morphology [27].
- Endometrial carcinomas comprise the majority of HPV-negative lesions in our matched cohort. Karaaslan et al. [23] reported that 78.8% of HPV-negative cervical malignancies were endometrial in origin. In our cohort, 22 of 23 endometrial carcinomas were detected cytologically, although the precise diagnostic role of cytology remains unclear due to high stage/grade and concurrent endometrial sampling.
- Seven cases in our study experienced histologic diagnostic delays exceeding 6 months, including two cases each of gastric-type adenocarcinomas, squamous (or in situ) carcinomas, and endometrial or serous carcinoma, as well as 1 adenocarcinoma, NOS. This study is limited for a statistically significant difference between HPV dependent vs. independent tumor groups for a diagnostic delay due to no control data.
- HPV-negative lesions represent a blind spot in primary HPV-based screening systems, because these cases may escape detection. The impact of high-risk–HPV DNA–based screening on HPV-independent malignancies remains questionable [28]. Missed cases were overlooked due to their small subset. In our cohort, 3.6% of primary cervical cancers were HPV negative proportion that may increase with the rising incidence of adenocarcinoma and the impact of HPV vaccination. In Japan, HPV-negative CIN2+ or adenocarcinoma has not been considered a major barrier to the implementation of HPV-based screening; however, a new nationwide management algorithm has recently been proposed [29].
- This study has a limitation that HPV-IDCM cannot exclude an undetectable subtype, which are not included in HPV genotypes as well as no supportive RNA works. The incidence of HPV typing-negative cervical cancer has been reported as 5%–30% with different HPV detection methods [30]. The cytology-histologic matching case are too small volume for an overall detection rate. The clinical outcome was also limited for evidence of poorer outcomes than HPV-dependent group due to no control group.
- In summary, HPV-IDCM accounted for 3.6% of primary cervical malignancies, with a cytology (Pap test) detection rate of 83.2%. These findings underscore the ongoing importance of cytological evaluation, particularly in patients with limited screening history or at risk for HPV independent lesions. This evidence may contribute to future refinements in cervical cancer screening strategies.
DISCUSSION
Ethics Statement
All procedures performed in the current study were approved by the institutional review boards (IRB) of all participating institutions following the Declaration of Helsinki and its later amendments. Waiver of the informed consent can only be granted by the appropriate IRB. Formal written informed consent was not required with a waiver by the appropriate IRB or national research ethics committee. The approvals were granted by the following ethics committees: Sanggye Paik Hospital (IRB approval number: SGPAIK2024-04-011; date: April 30, 2024), Soonchunhyang University Seoul Hospital (IRB approval number: 2024-04-012-002), Chungbuk National University (IRB approval number: 2024-05-003), Busan Paik Hospital (BPIRB approval number: 2024-04-030), Kangbuk Samsung Hospital (IRB approval number: KBSMC 2024-05-028-001), Chosun University Hospital (IRB approval number: CHOSUN2024-04-012), Eunpyeong St Mary’s Hospital (IRB approval number: PC24RIDI0058), and Seoul National University Bundang Hospital (IRB approval number: B-2505-973-103).
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Author Contributions
Conceptualization: HJK. Data curation: HJK. Formal analysis: HJK, HRJ, JYK, HEP, YJS, SSL. Investigation: HJK, HRJ, JYK, HEP, YJS, SSL. Funding acquisition: HJK, HRJ, JYK, HEP, YJS, SSL. Methodology: HRJ, JS, CWY, ENK, CL, KK, HL, YL, JK, SJJ, JYK, HEP, THK, WL, MSC, RH, YJC, YSL, YC, SRL, MK, YJS, YJH, HJK. Project administration: HJK, HRJ, JYK, HEP, YJS, SSL. Supervision: YJC, SSL. Validation: HJK, HRJ, JYK, HEP, YJS, SSL. Writing—original draft: HJK. Writing—review & editing: HJK, YJC, SSL. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
This research was supported in part by The Korean Society for Cytopathology (Grant No. 23-01), Republic of Korea.
Acknowledgments
The authors gratefully acknowledge the cooperation and scholarly discussions provided by members of the Korean Society of Cytopathologists during the course of this study.


NIL, negative for intraepithelial lesion or malignancy; ASC-US, atypical squamous cells of undetermined significance; ASC-H, atypical squamous cells cannot excluded HSIL; LSIL, low-grade squamous intraepithelial lesion; HSIL, high-grade intraepithelial lesion; SqCC, squamous cell carcinoma; AG-US, atypical glandular cells of undetermined significance; AGUS-N, atypical glandular cells of undetermined significance, favor neoplastic; AIS, adenocarcinoma in situ; AdC, adenocarcinoma; Others, Other malignant neoplasms; NOS, not otherwise specified; Ca, NOS, carcinoma, not otherwise specified; SCC/NE, small cell (neuroendocrine) carcinoma; EmC, endometrial carcinoma; Mets, metastatic malignancy.
HPV, human papillomavirus; FU, follow-up; AdC, adenocarcinoma; AG-US, atypical glandular cells of undetermined significance; CIS, carcinoma in situ; LSIL, low-grade squamous intraepithelial lesion; HPVIPT, human papillomavirus independent; SqCC, squamous cell carcinoma; NIL, negative for intraepithelial lesion or malignancy; HSIL, high-grade intraepithelial lesion; DOD, patient died as a result of the malignancy.
- 1. Yang DX, Soulos PR, Davis B, Gross CP, Yu JB. Impact of widespread cervical cancer screening: number of cancers prevented and changes in race-specific incidence. Am J Clin Oncol 2018; 41: 289-94. ArticlePubMedPMC
- 2. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2021; 71: 209-49. ArticlePubMedPDF
- 3. National Cancer Institute. Surveillance, Epidemiology, and End Results Program. Cancer stat facts: cervical cancer [Internet]. Bethesda: National Cancer Institute, 2025 [cited 2022 Aug 21]. Available from: http://www.seer.cancer.gov/statfacts/html/cervix.html.
- 4. Current status of cancer incidence and mortality [Internet]. Daejeon: Ministry of Data, 2025 [cited 2022 Aug 21]. Available from: https://www.index.go.kr/unity/potal/main/EachDtlPageDetail.do?idx_cd=2770.
- 5. Moscicki AB, Schiffman M, Burchell A, et al. Updating the natural history of human papillomavirus and anogenital cancers. Vaccine 2012; 30 Suppl 5: F24-33. ArticlePubMedPMC
- 6. Saslow D, Solomon D, Lawson HW, et al. American Cancer Society, American Society for Colposcopy and Cervical Pathology, and American Society for Clinical Pathology screening guidelines for the prevention and early detection of cervical cancer. J Low Genit Tract Dis 2012; 16: 175-204. ArticlePubMedPMC
- 7. Perkins RB, Guido RS, Castle PE, et al. Erratum: 2019 ASCCP risk-based management consensus guidelines for abnormal cervical cancer screening tests and cancer precursors. J Low Genit Tract Dis 2021; 25: 330-1. ArticlePubMed
- 8. Wright TC Jr, Massad LS, Dunton CJ, et al. 2006 Consensus guidelines for the management of women with abnormal cervical screening tests. J Low Genit Tract Dis 2007; 11: 201-22. ArticlePubMed
- 9. Nayar R, Goulart RA, Tiscornia-Wasserman PG, Davey DD. Primary human papillomavirus screening for cervical cancer in the United States-US Food and Drug Administration approval, clinical trials, and where we are today. Cancer Cytopathol 2014; 122: 720-9. ArticlePubMed
- 10. Huh WK, Ault KA, Chelmow D, et al. Use of primary high-risk human papillomavirus testing for cervical cancer screening: interim clinical guidance. Gynecol Oncol 2015; 136: 178-82. ArticlePubMed
- 11. Lei J, Ploner A, Elfstrom KM, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med 2020; 383: 1340-8. ArticlePubMed
- 12. Min KJ, Kwon SH, Kim S, et al. Preventive vaccination against cervical cancer: Korean Society of Gynecologic Oncology Guideline. J Gynecol Oncol 2016; 27: e30.ArticlePubMedPMCPDF
- 13. WHO Classification of Tumours Editorial Board. WHO classification of tumours: female genital tumours. 5th ed. Lyon: International Agency for Research on Cancer, 2020.
- 14. Regauer S, Reich O. The histologic and molecular spectrum of highly differentiated HPV-independent cervical intraepithelial neoplasia. Am J Surg Pathol 2023; 47: 942-9. ArticlePubMed
- 15. Regauer S, Reich O, Kashofer K. HPV-negative squamous cell carcinomas of the cervix with special focus on intraepithelial precursor lesions. Am J Surg Pathol 2022; 46: 147-58. ArticlePubMed
- 16. Day T, Otton G, Jaaback K, Weigner J, Scurry J. Is vulvovaginal lichen planus associated with squamous cell carcinoma? J Low Genit Tract Dis 2018; 22: 159-65. ArticlePubMedPMC
- 17. Horn LC, Brambs CE, Aktas B, et al. Human papilloma virus-independent/p53 abnormal keratinizing squamous cell carcinoma of the uterine cervix associated with uterine prolapse. Int J Gynecol Pathol 2025; 44: 2-14. ArticlePubMed
- 18. Yamagami W, Nagase S, Takahashi F, et al. Clinical statistics of gynecologic cancers in Japan. J Gynecol Oncol 2017; 28: e32.ArticlePubMedPMCPDF
- 19. Chiang YC, Chen YY, Hsieh SF, et al. Screening frequency and histologic type influence the efficacy of cervical cancer screening: a nationwide cohort study. Taiwan J Obstet Gynecol 2017; 56: 442-8. ArticlePubMed
- 20. Ministry of Health and Welfare, National Cancer Registration and Analysis Division. National Cancer Registration Statistics (for the Year 2022) [Internet]. Seoul: Ministry of Health and Welfare, National Cancer Registration and Analysis Division, 2024 [cited 2025 Nov 4]. Available from: https://cancer.go.kr/lay1/S1T639C640/contents.do.
- 21. Davey DD, Souers RJ, Goodrich K, Mody DR, Tabbara SO, Booth CN. Bethesda 2014 Implementation and human papillomavirus primary screening: practices of laboratories participating in the College of American Pathologists PAP Education Program. Arch Pathol Lab Med 2019; 143: 1196-202. ArticlePubMedPDF
- 22. Kaufman HW, Alagia DP, Chen Z, Onisko A, Austin RM. Contributions of liquid-based (Papanicolaou) cytology and human papillomavirus testing in cotesting for detection of cervical cancer and precancer in the United States. Am J Clin Pathol 2020; 154: 510-6. ArticlePubMedPMCPDF
- 23. Karaaslan S, Dilcher TL, Abdelsayed M, Goyal A. Significant outcomes associated with high-risk human papillomavirus negative Papanicolaou tests. J Am Soc Cytopathol 2023; 12: 189-96. ArticlePubMed
- 24. Mikami Y. Gastric-type mucinous carcinoma of the cervix and its precursors: historical overview. Histopathology 2020; 76: 102-11. ArticlePubMedPDF
- 25. Schwock J, Starova B, Khan ZF, et al. Cytomorphologic features of gastric-type endocervical adenocarcinoma in liquid-based preparations. Acta Cytol 2021; 65: 56-66. ArticlePubMedPMCPDF
- 26. Yeo MK, Bae GE, Kim DH, Seong IO, Suh KS. Cytopathologic features of human papillomavirus-independent, gastric-type endocervical adenocarcinoma. J Pathol Transl Med 2022; 56: 260-9. ArticlePubMedPMCPDF
- 27. Nishio H, Matsuda R, Iwata T, Yamagami W. Gastric-type adenocarcinoma of the uterine cervix: clinical features and future directions. Jpn J Clin Oncol 2024; 54: 516-20. ArticlePubMedPMCPDF
- 28. Vassilakos P, Tran PL, Sahli R, Low N, Petignat P. HPV-negative CIN3 and cervical cancer in Switzerland: any evidence of impact on screening policies? Swiss Med Wkly 2017; 147: w14559.ArticlePubMedPDF
- 29. Hideshima M, Hashiguchi M, Honda A, et al. Are HPV-negative lesions concerned for the introduction of primary HPV testing for cervical cancer screening in Japan? J Obstet Gynaecol Res 2023; 49: 2860-7. ArticlePubMed
- 30. Xu Y, Sun Y, Chang H, et al. The expression of HPV E6/E7 mRNA in situ hybridization in HPV typing-negative cervical cancer. Int J Gynecol Pathol 2023; 42: 11-20. ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure



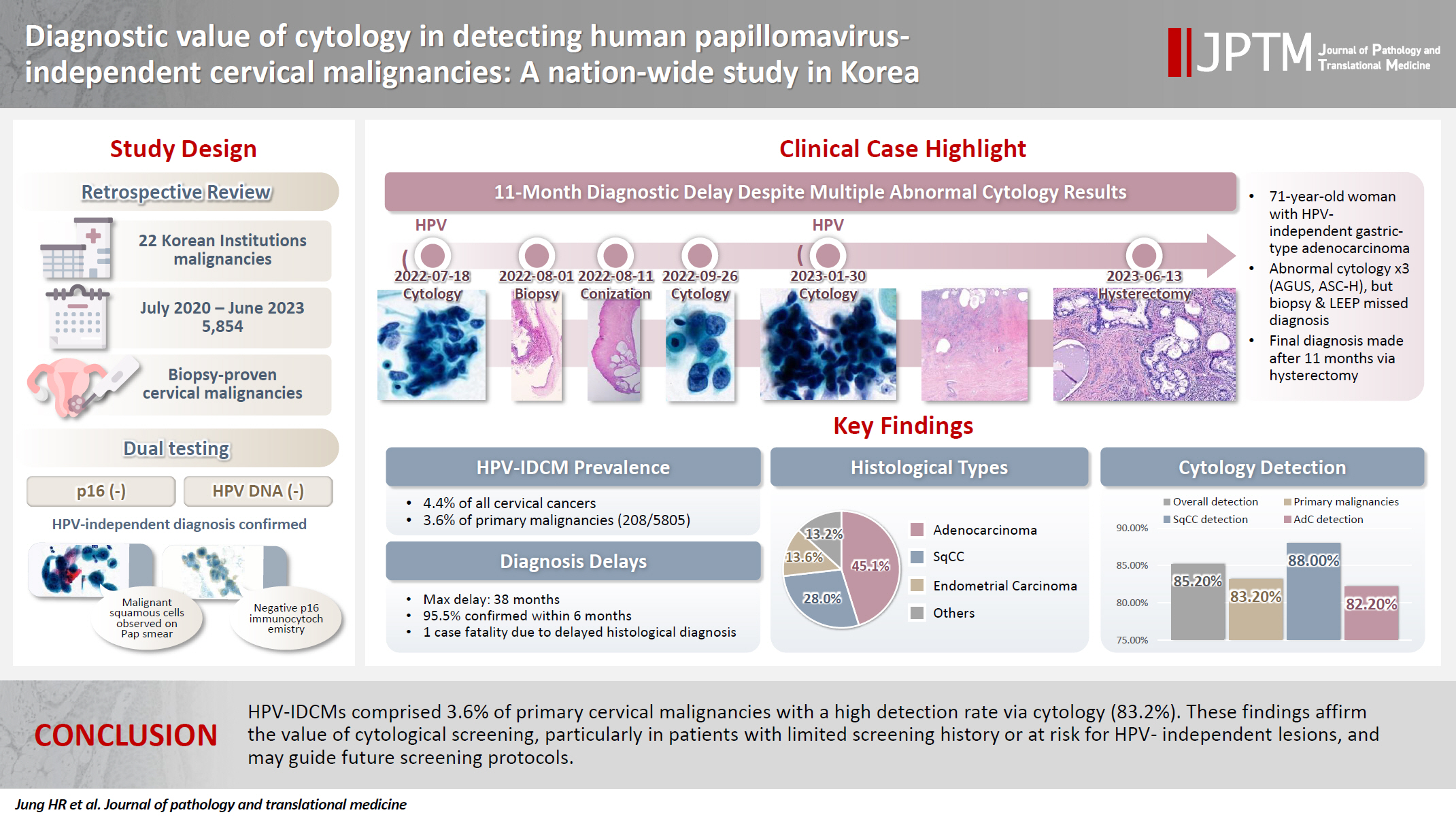
Fig. 1.
Fig. 2.
Fig. 3.
Graphical abstract
| Value | |
|---|---|
| Age (yr), median (range) | 57.79 (29–89) |
| Type of specimen (n = 257) | |
| Punch biopsy | 158 |
| Excisional biopsy | 7 |
| LEEP conization | 18 |
| Hysterectomy | 74 |
| Clinical follow-up (n = 167) | |
| Alive | 137 |
| Died of disease or other causes | 23 |
| Lost to follow-up | 7 |
| No. | |
|---|---|
| Primary | 208 |
| Squamous cell carcinoma | 72 |
| Adenocarcinoma | 116 |
| Gastric type | 41 |
| NOS | 37 |
| Clear cell | 17 |
| Mesonephric | 7 |
| Adenocarcinoma in situ | 14 |
| Neuroendocrine carcinoma | 3 |
| Carcinoma, NOS | 10 |
| Others | 7 |
| Secondary | 49 |
| Endometrial carcinoma | 35 |
| Metastatic carcinoma | 14 |
| NIL | ASC-US | ASC-H | LSIL | HSIL | SqCC | AG-US | AGUS-N | AIS | AdC | Others | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Primary (n = 125) | 21 | 14 | 7 | 7 | 14 | 4 | 17 | 7 | 4 | 23 | 7 |
| SqCC (n = 33) | 4 | 6 | 3 | 7 | 9 | 2 | 0 | 0 | 0 | 0 | 2 |
| AdC (n = 79) | |||||||||||
| NOS (n = 31) | 6 | 5 | 2 | 0 | 1 | 1 | 6 | 1 | 3 | 5 | 1 |
| Gastric (n = 26) | 4 | 1 | 0 | 0 | 1 | 0 | 6 | 4 | 0 | 10 | 0 |
| AIS (n = 10) | 2 | 0 | 1 | 0 | 1 | 1 | 1 | 2 | 0 | 2 | 0 |
| Clear (n = 9) | 1 | 0 | 0 | 0 | 0 | 0 | 3 | 0 | 1 | 4 | 0 |
| Meso (n = 3) | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 |
| Ca, NOS (n = 7) | 1 | 2 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 1 | 1 |
| SCC/NE (n = 1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 |
| Others (n = 5) | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 2 |
| EmC (n = 23) | 1 | 0 | 1 | 1 | 2 | 1 | 7 | 1 | 4 | 5 | 0 |
| Mets (n = 7) | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 2 |
| Interval (mo) | Histological diagnosis | Cytological diagnosis | Age (yr) | FU (mo) | Outcome |
|---|---|---|---|---|---|
| 8 | Endometrial AdC | AG-US | 66 | 2 | Lost |
| 9 | Squamous CIS | LSIL | 63 | 2 | Survived |
| 11 | AdC-HPVIPT, gastric type | AG-US | 71 | 2 | Lost |
| 11 | Invasive AdC | SqCC | 77 | 35 | Survived |
| 18 | AdC-HPVIPT, gastric type | NIL | 43 | 11 | Survived |
| 23 | SqCC | HSIL | 79 | 7 | DOD |
| 38 | Serous carcinoma | AdC | 66 | 17 | Survived |
HPV, human papillomavirus; LEEP, loop electrosurgical excision procedure.
HPV, human papillomavirus; NOS, not otherwise specified.
NIL, negative for intraepithelial lesion or malignancy; ASC-US, atypical squamous cells of undetermined significance; ASC-H, atypical squamous cells cannot excluded HSIL; LSIL, low-grade squamous intraepithelial lesion; HSIL, high-grade intraepithelial lesion; SqCC, squamous cell carcinoma; AG-US, atypical glandular cells of undetermined significance; AGUS-N, atypical glandular cells of undetermined significance, favor neoplastic; AIS, adenocarcinoma in situ; AdC, adenocarcinoma; Others, Other malignant neoplasms; NOS, not otherwise specified; Ca, NOS, carcinoma, not otherwise specified; SCC/NE, small cell (neuroendocrine) carcinoma; EmC, endometrial carcinoma; Mets, metastatic malignancy.
HPV, human papillomavirus; FU, follow-up; AdC, adenocarcinoma; AG-US, atypical glandular cells of undetermined significance; CIS, carcinoma in situ; LSIL, low-grade squamous intraepithelial lesion; HPVIPT, human papillomavirus independent; SqCC, squamous cell carcinoma; NIL, negative for intraepithelial lesion or malignancy; HSIL, high-grade intraepithelial lesion; DOD, patient died as a result of the malignancy.

 E-submission
E-submission