Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 58(1); 2024 > Article
-
Letter To The Editor
Comment on “A stepwise approach to fine needle aspiration cytology of lymph nodes” -
Elisabetta Maffei
 , Valeria Ciliberti
, Valeria Ciliberti , Pio Zeppa
, Pio Zeppa , Alessandro Caputo,
, Alessandro Caputo,
-
Journal of Pathology and Translational Medicine 2024;58(1):40-42.
DOI: https://doi.org/10.4132/jptm.2023.11.05
Published online: January 10, 2024
Department of Pathology, University Hospital of Salerno, Salerno, Italy
- Corresponding Author: Alessandro Caputo, MD Department of Pathology, University Hospital of Salerno, 84131 Salerno, Italy Tel: +39-089672840, Fax: +39-089672841, E-mail: alcap94@gmail.com
© 2024 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Dear Editor,
- We read with great interest the article “A stepwise approach to fine needle aspiration cytology of lymph nodes” by Chong et al. [1], recently published in J Pathol Transl Med. The Authors proposed a morphological stepwise algorithm, separate but complementary to the Sydney system, for the cytological diagnosis of lymphadenopathies [2]. In the proposed algorithm the basic diagnostic criteria are structured in a stepwise approach for cytological diagnosis of adenopathy. Regarding the diagnostic classification the Authors basically agree with the Sydney system [2] but they state that “…the epithelial or lymphomatous nature of the lesion is not clearly separated into different categories and is not emphasized due to the ambiguity of the lymph node features on FNAC. In other words, even though a diagnosis was made on a certain case using the Sydney system, it is still unclear whether the case is lymphoid or metastatic.” We disagree with this observation because when a case is atypical, suspicious, or malignant, the Sydney System strongly encourages to report the nature (lymphoid/metastatic) of the nosologic entity. This is also in keeping with clinical practice, since no hematocytopathologist would ever omit such information from a report. Even in cases in which the cytomorphology is insufficient to distinguish between a lymphoid or metastatic malignancy, a comment will be added to state this.
- One additional important point is that the stepwise system proposed by the authors is purely morphological and does not consider ancillary techniques. While the two-level structure of the Sydney System was intentionally conceived to be applicable even in settings where ancillary testing is unavailable, it is important to note that cytopathologists should strive to perform ancillary techniques whenever possible, for three reasons. First, it helps limit atypical and suspicious cases and categorize them in a definite category instead (benign or malignant) [3]. Second, it helps to further subclassify the nosological process responsible for the lymphadenopathy (e.g., “malignant, lymphoma” can become “malignant, follicular B-cell lymphoma” after flow cytometry; “malignant, metastasis” can become “malignant, breast cancer metastasis” after immunocytochemistry; and “benign, granulomatous” can become “benign, tuberculous lymphadenopathy” after polymerase chain reaction). Third, in some cases a fully actionable diagnosis, including prognostic and predictive biomarkers, can be performed on lymph node fine needle aspiration cytology (LN-FNAC). For example, after harvesting non– small-cell lung cancer material from a nodal metastasis, it is possible to employ cytologic material to guide targeted therapy [4].
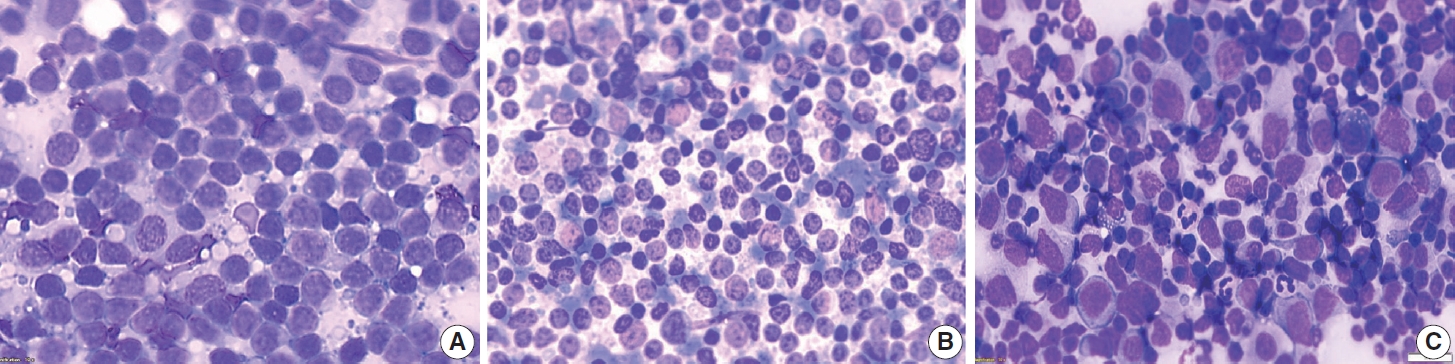
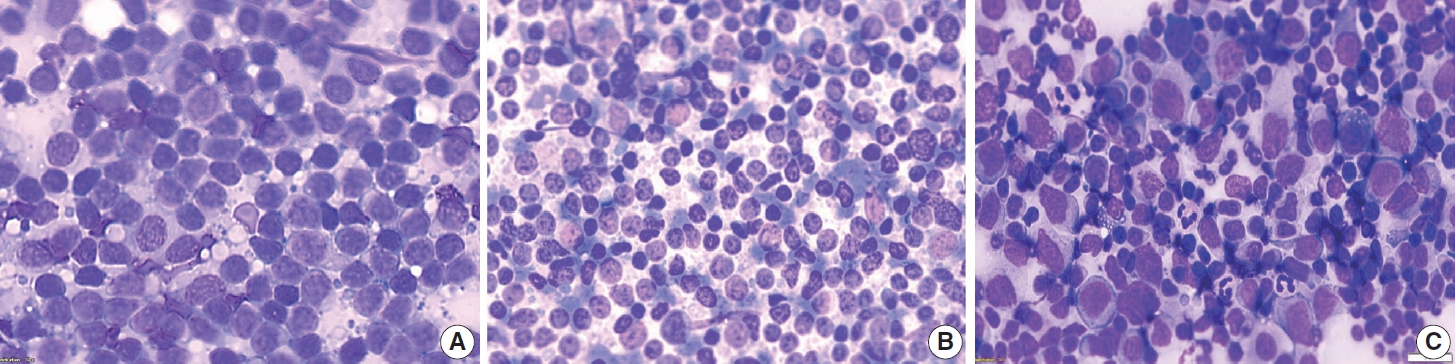
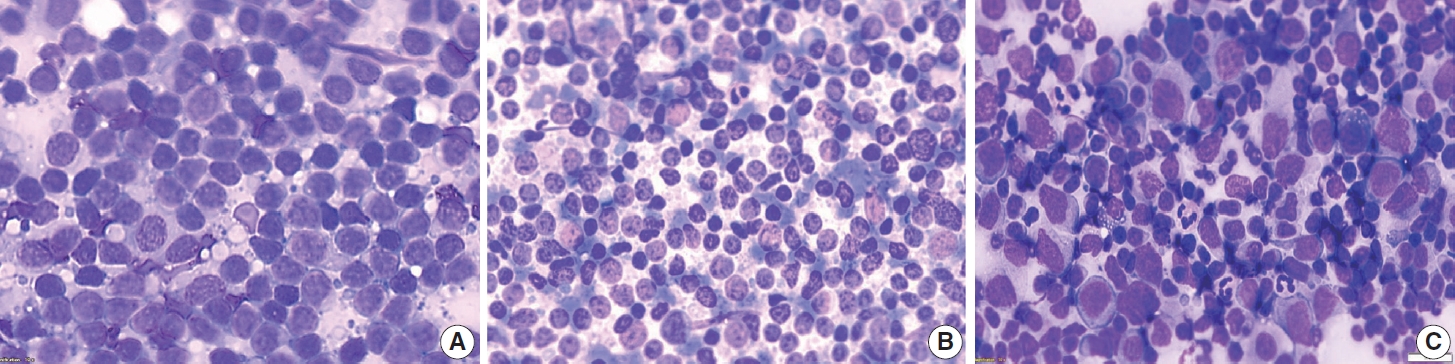
- In fact, the relatively high risk of malignancy (ROM) registered for the category atypical (atypical, undermined significance– atypical lymphoid uncertain significance, AUS-ALUS) by Gupta et al. [5] was the highest among similar series which applied the Sydney System to LN-FNAC [3], mainly because no ancillary techniques were utilized. This high ROM was foreseen by the authors of the Sydney System because some differential diagnoses, such as that between florid reactive hyperplasia and follicular lymphoma or other low-grade non-Hodgkin lymphoma, can be difficult or almost impossible using only cytomorphological criteria (Fig. 1). This differential diagnosis by FNAC, other than in lymphadenopathies, is crucial in extranodal lymphoproliferative processes in which diagnostic excision or invasive biopsies might be useless or even harmful [6,7]. Focusing on the proposed algorithm, we do not believe that only cytomorphological criteria will reduce the incidence of this diagnostic category and its ROM. On the other hand, ancillary techniques (flow cytometry, immunohistochemistry or molecular testing) combined with clinical data and cytological features, can discriminate these entities in many cases. For this reason, the Sydney System [2] strongly suggests the application of ancillary techniques in these cases because cytological criteria alone cannot discriminate between entities included with similar cytological patterns. Moreover, repetition of LN-FNAC in AUS-ALUS cases, after six-eight weeks may show dramatically changed cytological features in case of reactive hyperplasia. The authors [1] also state that “the L3 category, which includes AUS and ALUS, is a good example. It is often quite challenging to discriminate a certain lesion as lymphoid or epithelial in origin” and that the Sydney System includes “cases in which the FNAC features favor certain diseases, the cases should be described specifically as “AUS, favor poorly differentiated carcinoma,” This sentence is not reported in the Sydney system text in which suspicious lymphoma and metastases are included in the category suspicious, which has a higher ROM and different clinical implications than the atypical category. Regarding some specific entities (progressive transformation of germinal centers, Kikuchi-Fujimoto disease, Rosai-Dorfman disease, or others) there is relatively little FNAC experience on their cytological features and few case reports or small series are available in the literature to foresee their diagnostic category (AUS-ALUS or suspicious) and corresponding ROM. We are aware that the ROM of diagnostic categories largely depends on technical issues, different clinical contexts, local epidemiology, and on the reproducibility of diagnostic criteria. For this purpose, a recent experience on LN-FNAC digital slides has been performed producing quite encouraging results [8]. In conclusion we think that the algorithm proposed by Chong et al. [1] matches with the Sydney system which will be reproduced in five diagnostic categories and two diagnostic levels also by the near to be published WHO Reporting System for Lymph Node, Spleen, and Thymus Cytopathology.
Ethics Statement
Not applicable.
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Code Availability
Not applicable.
Author contributions
Conceptualization: PZ, AC. Supervision: PZ, AC. Visualization: VC, EM. Writing—original draft: EM, PZ. Writing—review & editing: EM, VC, PZ, AC. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
No funding to declare.
- 1. Chong Y, Park G, Cha HJ, et al. A stepwise approach to fine needle aspiration cytology of lymph nodes. J Pathol Transl Med 2023; 57: 196-207. ArticlePubMedPMCPDF
- 2. Al-Abbadi MA, Barroca H, Bode-Lesniewska B, et al. A proposal for the performance, classification, and reporting of lymph node fine-needle aspiration cytopathology: the Sydney system. Acta Cytol 2020; 64: 306-22. ArticlePubMedPDF
- 3. Caputo A, Ciliberti V, D’Antonio A, et al. Real-world experience with the Sydney System on 1458 cases of lymph node fine needle aspiration cytology. Cytopathology 2022; 33: 166-75. ArticlePubMedPDF
- 4. D’Ardia A, Caputo A, Fumo R, et al. Advanced non-small cell lung cancer: rapid evaluation of EGFR status on fine-needle cytology samples using Idylla. Pathol Res Pract 2021; 224: 153547.ArticlePubMed
- 5. Gupta P, Gupta N, Kumar P, et al. Assessment of risk of malignancy by application of the proposed Sydney system for classification and reporting lymph node cytopathology. Cancer Cytopathol 2021; 129: 701-18. ArticlePubMedPDF
- 6. Caleo A, Vigliar E, Vitale M, et al. Cytological diagnosis of thyroid nodules in Hashimoto thyroiditis in elderly patients. BMC Surg 2013; 13 Suppl 2: S41.ArticlePubMedPDF
- 7. Vigliar E, Cozzolino I, Fernandez LV, et al. Fine-needle cytology and flow cytometry assessment of reactive and lymphoproliferative processes of the breast. Acta Cytol 2012; 56: 130-8. ArticlePubMedPDF
- 8. Caputo A, Fraggetta F, Cretella P, et al. Digital Examination of LYmph node CYtopathology Using the Sydney system (DELYCYUS): an international, multi-institutional study. Cancer Cytopathol 2023; 131: 679-92. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Response to comment on “A stepwise approach to fine needle aspiration cytology of lymph nodes”
Yosep Chong, Gyeongsin Park, Hee Jeong Cha, Hyun-Jung Kim, Chang Suk Kang, Jamshid Abdul-Ghafar, Seung-Sook Lee
Journal of Pathology and Translational Medicine.2024; 58(1): 43. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure

 E-submission
E-submission