Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 57(2); 2023 > Article
-
Case Study
Solitary Peutz-Jeghers type harmartomatous polyp in duodenum with gastric foveolar epithelium: a case report -
Eugene Choi1
 , Junghwan Lee2
, Junghwan Lee2 , Youngsoo Park1
, Youngsoo Park1
-
Journal of Pathology and Translational Medicine 2023;57(2):128-131.
DOI: https://doi.org/10.4132/jptm.2022.11.07
Published online: January 10, 2023
1Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
2Department of Gastroenterology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- Corresponding Author: Youngsoo Park, MD, Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, 88 Olympic-ro 43-gil, Songpa-gu, Seoul 05505, Korea, Tel: +82-2-3010-5608, Fax: +82-2-3010-4560, E-mail: youngspark@amc.seoul.kr
© 2023 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Peutz-Jeghers type hamartomatous polyp is known to be associated with Peutz-Jeghers syndrome, which shows characteristic multiple hamartomatous polyp involvement in the gastrointestinal tract, combined with mucocutaneous symptom, familial history of Peutz-Jeghers syndrome or STK11/LTB1 mutation. However, some cases showing histologic appearance of the polyps discovered in Peutz-Jeghers syndrome while lacking other diagnostic criteria of the syndrome have been reported, and these are called solitary Peutz-Jeghers type polyps. Herein, we report a case of solitary Peutz-Jeghers type polyp covered with heterotopic epithelium. The patient was 47-year-old female without any mucocutaneous symptoms nor familial history of Peutz-Jeghers syndrome. Microscopic examination revealed Peutz-Jeghers type hamartomatous polyp in duodenum covered with gastric type foveolar epithelium. Considering the definition of hamartomatous polyp, which is, the abnormal overgrowth of the indigenous epithelial component, the histological feature of current case is noteworthy in a point that it shows proliferation of heterotopic component, rather than the indigenous component.
- A 47-year-old woman visited outpatient clinic for incidentally discovered duodenal polyp during regular medical check-up. She did not experience any associated symptoms. She had a history of invasive ductal carcinoma of both breasts in her early to mid-30s and been treated for papillary thyroid carcinoma in her late 30s.
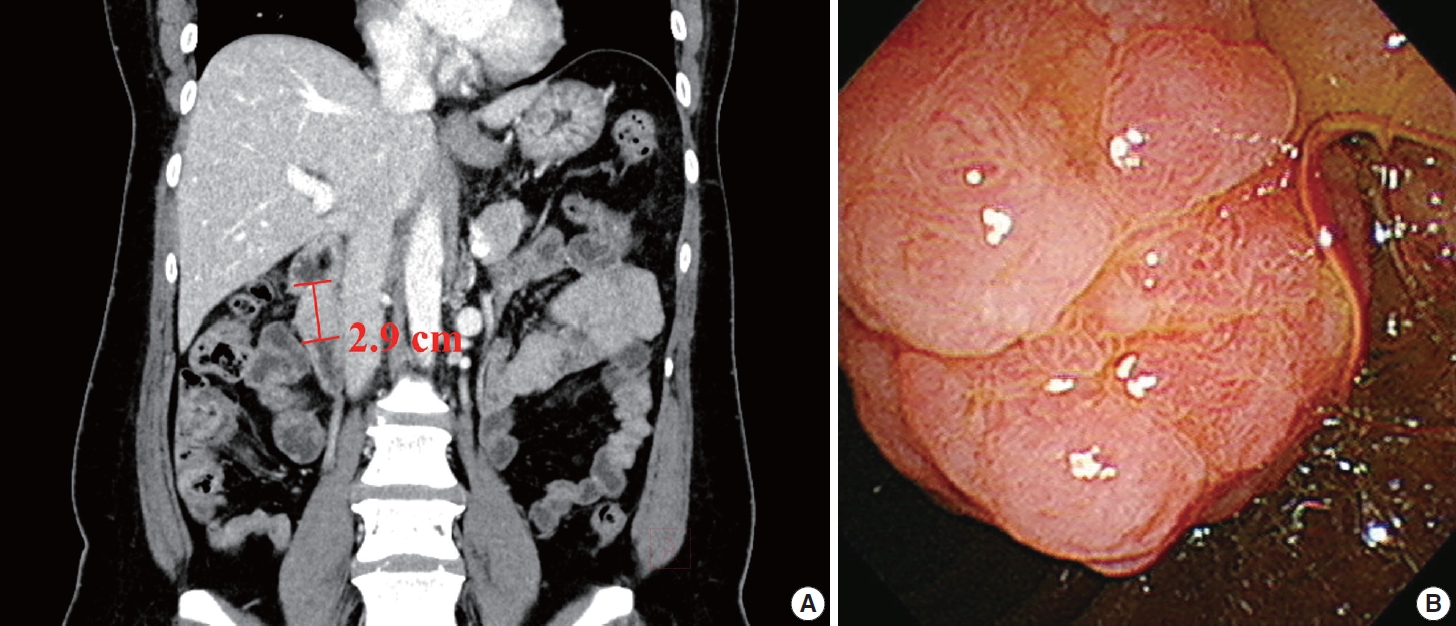
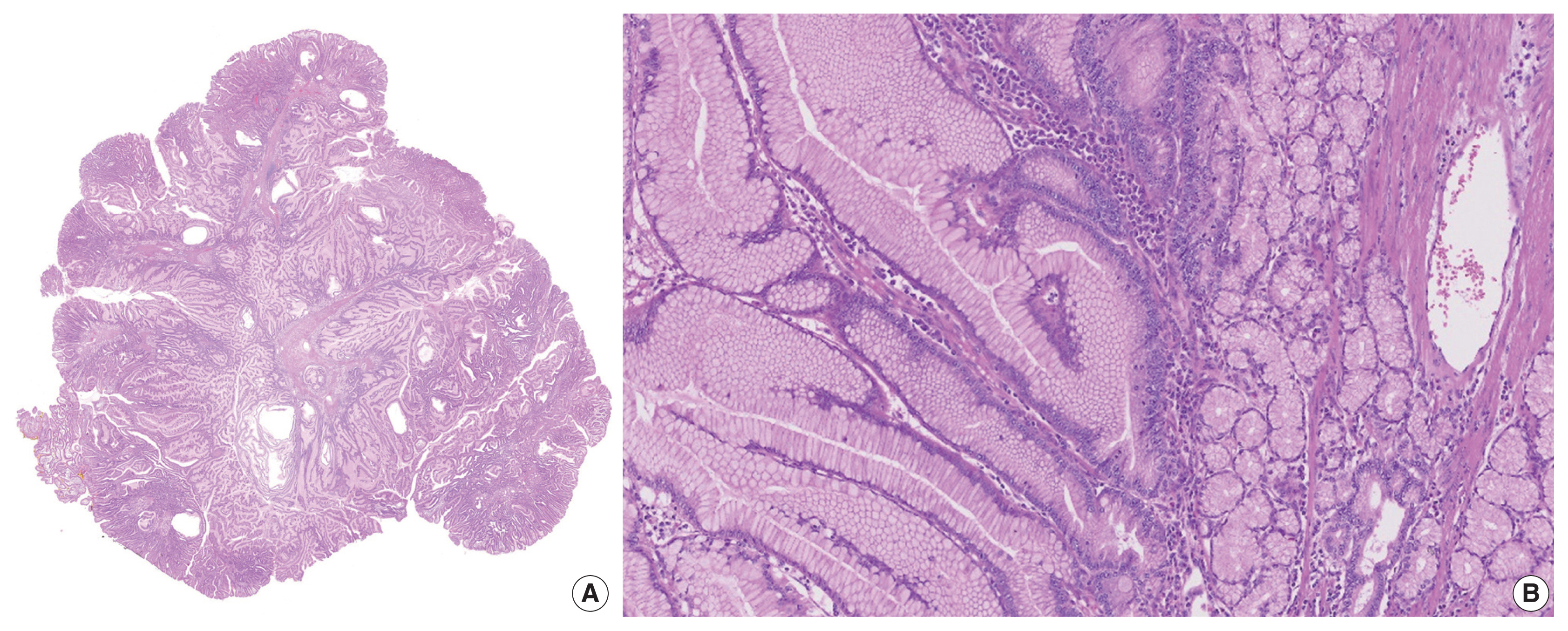
- On initial esophagogastroduodenoscopy, a pedunculated polyp occupying half of the luminal space was found in the 2nd portion of duodenum. Histological examination of a biopsy specimen mainly showed hyperplastic gastric foveolar epithelium. Following computed tomography scan revealed a 2.9-cm-sized polypoid lesion in duodenum without any evidence of metastasis (Fig. 1A). The polyp was entirely resected by endoscopic submucosal dissection (Fig. 1B). The patient was discharged without any post-procedural complications.
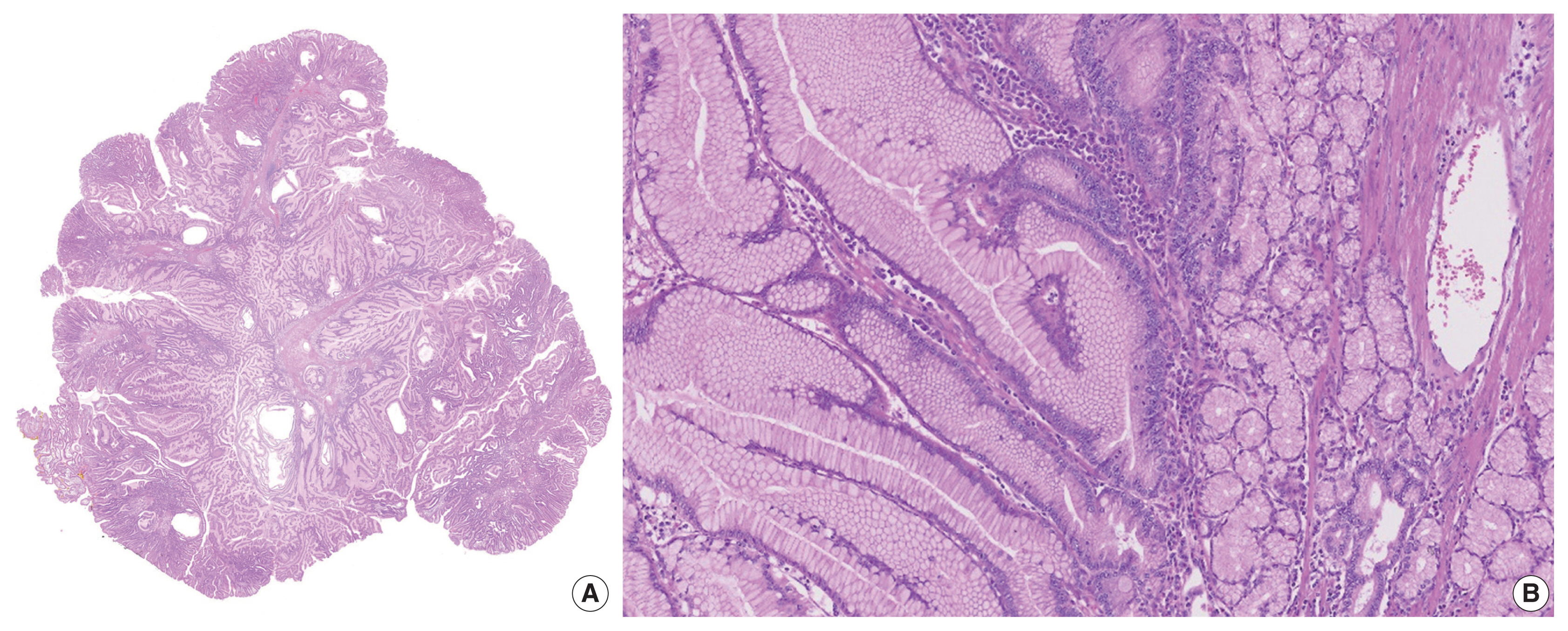
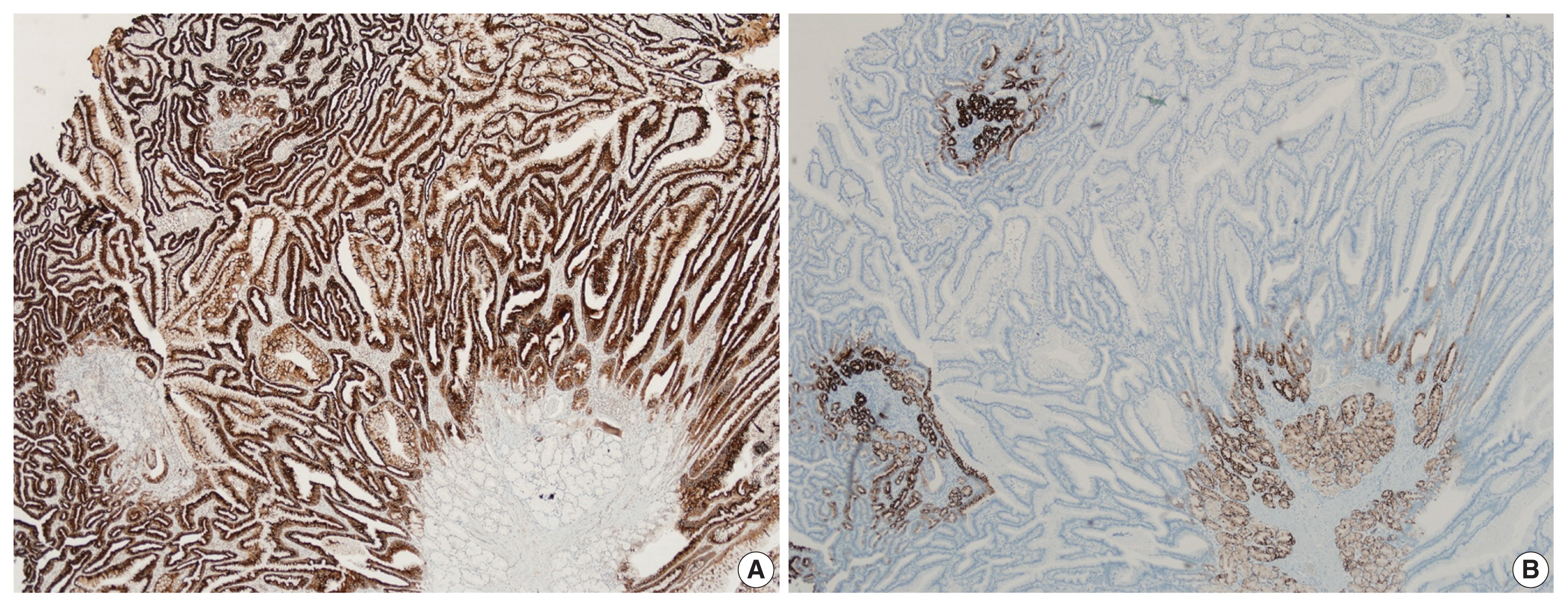
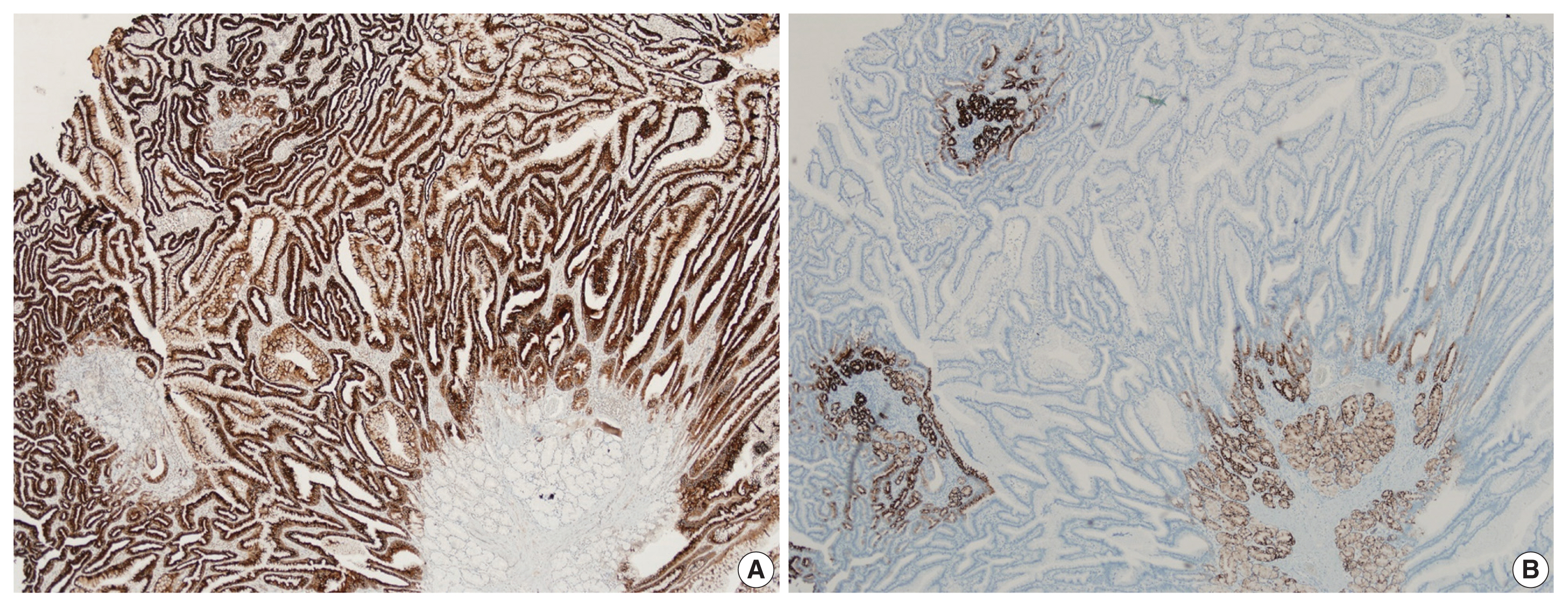
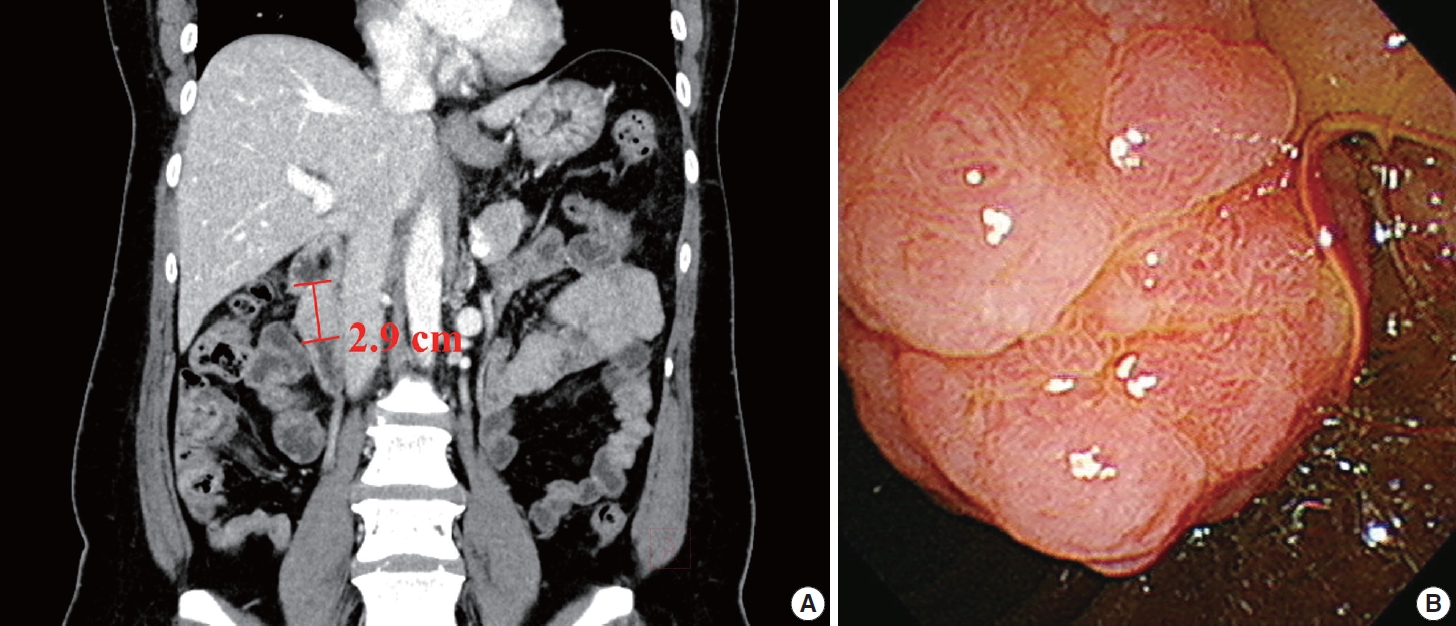
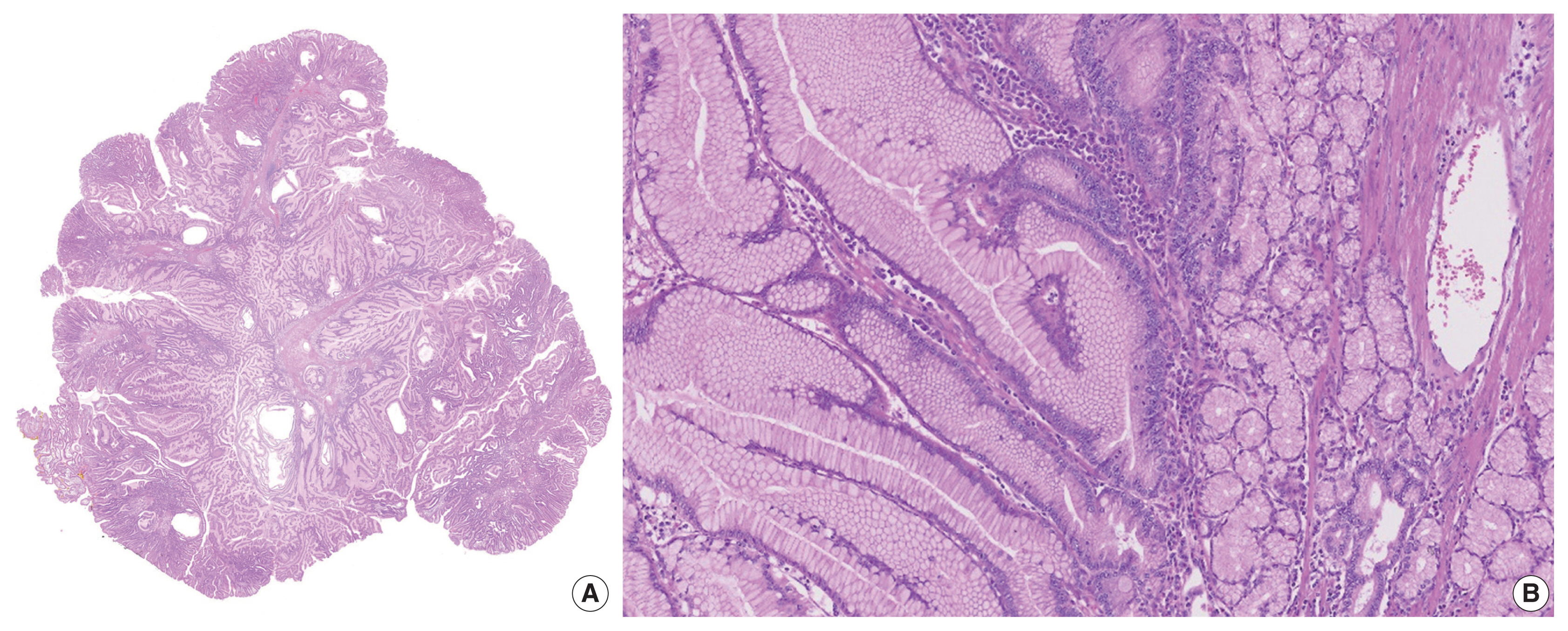
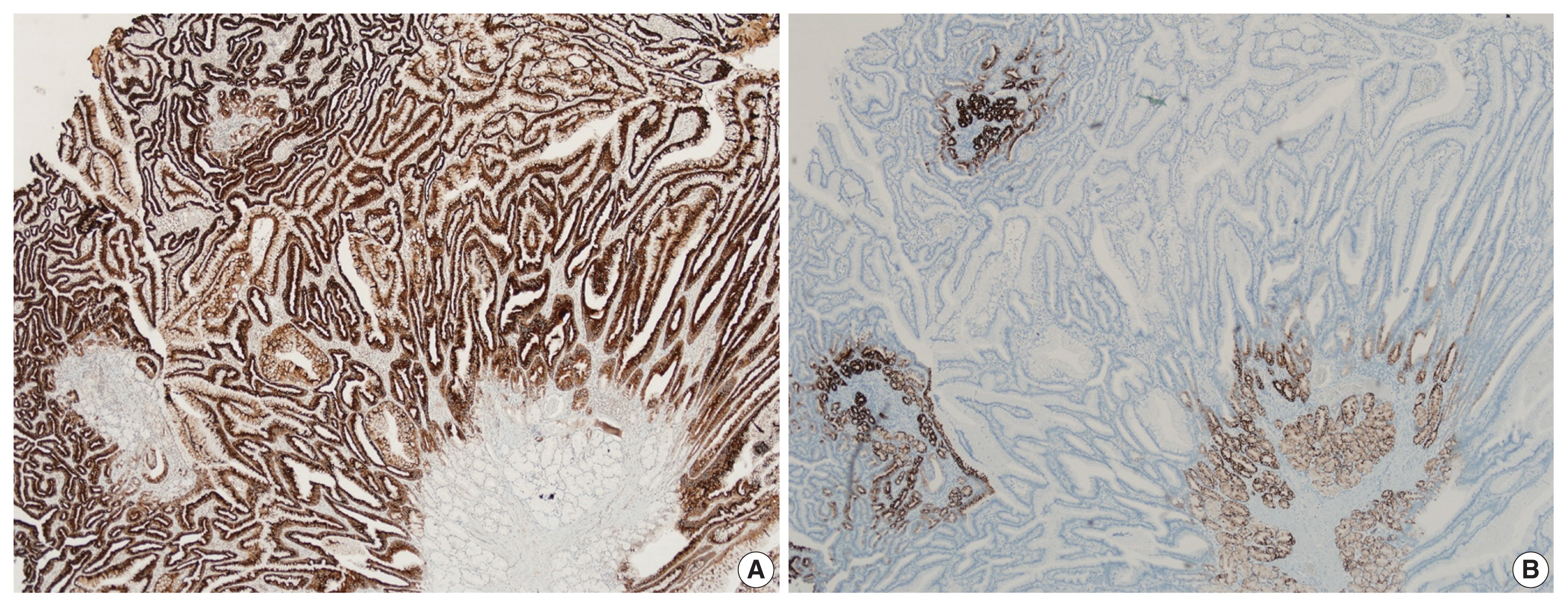
- Histological examination of the resected polyp showed disorganized overgrowth of epithelial cells supported by thick, branching bundles of smooth muscles. The epithelium mainly consisted of foveolar type cells lying over mucinous glands resembling pyloric glands without dysplastic change (Fig. 2A, B). A small amount of surrounding duodenal tissue was identified at the margin of the specimen and it showed focal foveolar type epithelium among normal duodenal villous structures, suggestive of gastric metaplasia. Immunohistochemical staining for MUC5AC and MUC6 confirmed the covering hyperplastic epithelium to be gastric foveolar type with pyloric glands underneath (Fig. 3A, B).
- Follow-up endoscopy after 6 months from the procedure revealed no additional polyps. In an in-depth interview afterwards, the patient insisted she had never been diagnosed with hamartomatous polyp before and denied of any familial history nor any mucocutaneous symptoms. Genetic assessment for STK11/LTB1 mutation was not done. According to these findings, the polyp was finally diagnosed as solitary Peutz-Jeghers type polyp with gastric foveolar epithelium.
CASE REPORT
- Hamartomatous polyp is characterized by the arborization of smooth muscle bundle up to lamina propria with near-normal overlying epithelium. The surface epithelium of hamartomatous polyp is known to be identical with those of adjacent normal mucosa. Multiple hamartomatous polyps are frequently associated with various genetic syndromes, such as juvenile polyposis syndrome, Peutz-Jeghers syndrome and Cowden syndrome [1].
- Of note, multiple GI tract polyps, mucocutaneous symptoms, STK11/LTB1 mutation and familial history of Peutz-Jeghers syndrome are characteristic of Peutz-Jeghers syndrome. As this syndrome represents an increased risk of developing cancers, patient with solitary Peutz-Jeghers type hamartomatous polyp must be meticulously examined to exclude a possibility of syndromic involvement. If the polyp is proved to have no association with Peutz-Jeghers syndrome, it is defined as solitary Peutz-Jeghers type hamartomatous polyp. Although the histological aspect of solitary Peutz-Jeghers type hamartomatous polyp is indistinguishable from the polyps of Peutz-Jeghers syndrome, this solitary polyp seems to be of separated entity, as it does not show STK11/LTB1 mutation characteristic of the syndrome. Furthermore, the frequently involved site is quite different. The polyp of the syndrome mostly occurs in small intestine, whereas the solitary counterpart develops mostly in sigmoid colon, followed by duodenum, rectum, jejunum, and stomach, according to the previously published literatures [2,3].
- Solitary Peutz-Jeghers type hamartomatous polyp itself can provoke GI bleeding and intussusception, which may manifest as acute GI symptoms in some patients [4–6]. Some cases represented with dysplasia and even carcinogenesis [7,8]. Thus, complete resection of the polyp by either endoscopic or surgical procedure should be considered.
- In our case, the patient was asymptomatic, and the polyp was found during routine health check-up. The resected polyp showed hamartomatous proliferation of gastric foveolar epithelium over pyloric gland-like structures in the duodenum. Whether this aspect is related to prior gastric metaplasia or abnormal differentiation of endoderm is unclear at this moment. To date, a case of pyloric metaplasia involving multiple hamartomatous jejunal polyps in a patient with Peutz-Jeghers syndrome and a case of solitary Peutz-Jeghers type polyp with gastric antral and fundic gland mucosa have been reported [6,9]. Considering the definition of hamartomatous polyp, which is, the abnormal overgrowth of the indigenous epithelial component, the histological feature of current case is noteworthy in a point that it shows proliferation of heterotopic component, rather than the indigenous component.
DISCUSSION
Ethics Statement
Formal written informed consent was not required with a waiver by the appropriate IRB (Asan Medical Center IRB No. 2022-1339).
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Code Availability
Not applicable.
Author Contributions
Conceptualization: YP. Data curation: JL. Formal analysis: EC. Investigation: EC. Supervision: YP. Writing—original draft: EC. Writing—review & editing: YP, EC. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
No funding to declare.
- 1. Brosens LA, Jansen M. Peutz-Jeghers syndrome. WHO Classification of Tumours Editorial Board. Digestive system tumours. WHO classification of tumours. 5th ed. Lyon: International Agency for Research on Cancer, 2019; 545-6.
- 2. Sone Y, Nakano S, Takeda I, Kumada T, Kiriyama S, Hisanaga Y. Solitary hamartomatous polyp of Peutz-Jeghers type in the jejunum resected endoscopically. Gastrointest Endosc 2000; 51: 620-2. ArticlePubMed
- 3. Endo K, Kawamura K, Murakami K, et al. A case of jejunal solitary Peutz-Jeghers polyp with intussusception identified by double-balloon enteroscopy. Clin J Gastroenterol 2020; 13: 1129-35. ArticlePubMedPDF
- 4. Oncel M, Remzi FH, Church JM, Goldblum JR, Zutshi M, Fazio VW. Course and follow-up of solitary Peutz-Jeghers polyps: a case series. Int J Colorectal Dis 2003; 18: 33-5. ArticlePubMedPDF
- 5. Itaba S, Namoto M, Somada S, et al. Two cases of solitary Peutz-Jeghers-type hamartoma of the duodenum. Endoscopy 2006; 38(Suppl 2):E32-3. ArticlePubMed
- 6. Liu BL, Zhou H, Risech M, Ky A, Houldsworth J, Ward SC. Solitary Peutz-Jeghers type polyp of jejunum with gastric fundic and antral gland lining mucosa: a case report and review of literature. Int J Surg Pathol 2022; 30: 539-42. ArticlePubMedPDF
- 7. Ichiyoshi Y, Yao T, Nagasaki S, Sugimachi K. Solitary Peutz-Jeghers type polyp of the duodenum containing a focus of adenocarcinoma. Ital J Gastroenterol 1996; 28: 95-7. PubMed
- 8. Suzuki S, Hirasaki S, Ikeda F, Yumoto E, Yamane H, Matsubara M. Three cases of solitary Peutz-Jeghers-type hamartomatous polyp in the duodenum. World J Gastroenterol 2008; 14: 944-7. ArticlePubMedPMC
- 9. Kato N, Sugawara M, Maeda K, Hosoya N, Motoyama T. Pyloric gland metaplasia/differentiation in multiple organ systems in a patient with Peutz-Jegher’s syndrome. Pathol Int 2011; 61: 369-72. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- A Solitary Peutz-Jeghers Hamartomatous Polyp in the Gastric Body: A Case Report
Noelia Madera, Noemí Acevedo, Carmen González-Peralta, Rafael Castro, Vismelis Mezquita-Luna
Cureus.2024;[Epub] CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure

 E-submission
E-submission