Search
- Page Path
- HOME > Search
Original Article
- TRPS1 expression in non-melanocytic cutaneous neoplasms: an immunohistochemical analysis of 200 cases
- Yi A. Liu, Phyu P. Aung, Yunyi Wang, Jing Ning, Priyadharsini Nagarajan, Jonathan L. Curry, Carlos A. Torres-Cabala, Doina Ivan, Victor G. Prieto, Qingqing Ding, Woo Cheal Cho
- J Pathol Transl Med. 2024;58(2):72-80. Published online February 26, 2024
- DOI: https://doi.org/10.4132/jptm.2024.01.23
- 6,969 View
- 389 Download
- 13 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
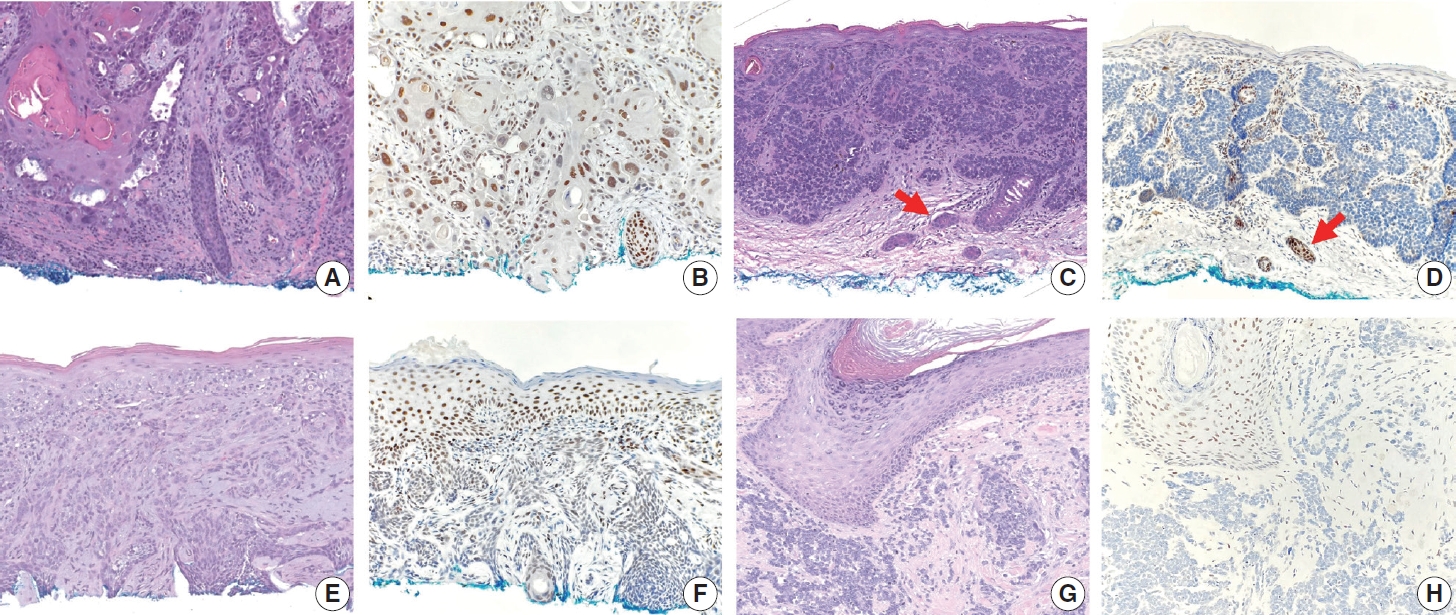
Although trichorhinophalangeal syndrome type 1 (TRPS1) was initially thought to be highly sensitive and specific for carcinomas and mesenchymal tumors of mammary origin, more recent data suggest its expression is not limited to breast neoplasms but also can be seen in other cutaneous neoplasms, such as extramammary Paget disease and squamous cell carcinoma (SCC) in situ.
Methods
Two-hundred cases of non-melanocytic cutaneous neoplasm, including basal cell carcinomas (BCCs) (n = 41), SCCs (n = 35), Merkel cell carcinomas (MCCs) (n = 25), and adnexal neoplasms (n = 99), were tested for TRPS1 expression using a monoclonal anti- TRPS1 rabbit anti-human antibody.
Results
TRPS1 expression was present in almost all cases of SCC (94%), with a median H-score of 200, while it was either absent or only focally present in most BCCs (90%), with a median H-score of 5. The difference between BCCs and SCCs in H-score was significant (p < .001). All MCCs (100%) lacked TRPS1 expression. TRPS1 expression was frequently seen in most adnexal neoplasms, benign and malignant, in variable intensity and proportion but was consistently absent in apocrine carcinomas. All endocrine mucin-producing sweat gland carcinomas (EMPSGCs) (100%, 6/6) showed diffuse and strong TRPS1 immunoreactivity, with a median H-score of 300, which was significantly different (p < .001) than that of BCCs.
Conclusions
Our study shows that TRPS1 may be an effective discriminatory marker for BCCs and SCCs. It also has a role in distinguishing BCCs from EMPSGCs. -
Citations
Citations to this article as recorded by- Metastatic Vulvar Paget's Disease Presenting in a Supraclavicular Lymph Node: A Diagnostic Challenge on Fine Needle Aspiration Cytology
Thiri Htoo Aung, Neha Seth, Anam Khan, Kasturi Das
Diagnostic Cytopathology.2026;[Epub] CrossRef - Trichorhinophalangeal syndrome type 1 (TRPS1) in breast pathology: diagnostic utility and pitfalls
Atif Ali Hashmi, Edi Brogi, Hannah Y. Wen
Diagnostic Pathology.2025;[Epub] CrossRef - Refining NTRK Fusion Detection in Papillary Thyroid Carcinoma Through Pan-TRK Immunohistochemistry and Histopathologic Features
Hyun Lee, Sue Youn Kim, Ji Min Park, Seung-Hyun Jung, Ozgur Mete, Chan Kwon Jung
Endocrine Pathology.2025;[Epub] CrossRef - Endocrine mucin-producing sweat gland carcinoma: Case report and literature review
Nan Guo, Zhenlin Fan, Yitong Chen, Qian Li, Limin Guo
European Journal of Ophthalmology.2025;[Epub] CrossRef - Updates on utility of immunohistochemistry in diagnosis of metastatic breast cancer
Hongxia Sun, Aysegul A. Sahin, Qingqing Ding
Human Pathology.2025; 162: 105821. CrossRef - Primary Cutaneous NUT Adnexal Carcinoma With BRD4::NUTM1 Fusion: A 19-Year Follow-Up
Elsayed Ibrahim, Richard K. Yang, Maria A. Gubbiotti, Victor G. Prieto, Woo Cheal Cho
The American Journal of Dermatopathology.2025; 47(9): 731. CrossRef - Primary mucinous carcinoma of the skin with co-expression of TRPS1 and GATA3: a case report
Liling Song, Ning Zhu, Lei Jiang, Dong Gao, Guohua Yu
Frontiers in Oncology.2025;[Epub] CrossRef - Diagnostic Algorithm for Secondary Extramammary Paget Disease from Institutional Cases and Literature Review
Salin Kiratikanon, Ayaka Fukui, Masahiro Hirata, Jakob M. T. Moran, Masakazu Fujimoto, Mai P. Hoang
Cancers.2025; 17(24): 4014. CrossRef - TRPS1 Expression Is Frequently Seen in a Subset of Cutaneous Mesenchymal Neoplasms and Tumors of Uncertain Differentiation: A Potential Diagnostic Pitfall
Moon Joo Kim, Yi A. Liu, Yunyi Wang, Jing Ning, Woo Cheal Cho
Dermatopathology.2024; 11(3): 200. CrossRef - TRPS1 expression in MPNST is correlated with PRC2 inactivation and loss of H3K27me3
Rossana Lazcano, Davis R. Ingram, Gauri Panse, Alexander J. Lazar, Wei-Lien Wang, Jeffrey M. Cloutier
Human Pathology.2024; 151: 105632. CrossRef - Syringocystadenoma Papilliferum-Like Features in Poroma: An Unusual Morphologic Pattern of Poroma or True Synchronous Occurrence of 2 Distinct Neoplasms?
Mouaz Alsawas, Fiorinda F. Muhaj, Phyu P. Aung, Priyadharsini Nagarajan, Woo Cheal Cho
The American Journal of Dermatopathology.2024; 46(12): 871. CrossRef - A Comprehensive Review of TRPS1 as a Diagnostic Immunohistochemical Marker for Primary Breast Carcinoma: Latest Insights and Diagnostic Pitfalls
Antonia-Carmen Georgescu, Tiberiu-Augustin Georgescu, Simona-Alina Duca-Barbu, Lucian Gheorghe Pop, Daniela Oana Toader, Nicolae Suciu, Dragos Cretoiu
Cancers.2024; 16(21): 3568. CrossRef - Expression of TRPS1 in Metastatic Tumors of the Skin: An Immunohistochemical Study of 72 Cases
Kassiani Boulogeorgou, Christos Topalidis, Triantafyllia Koletsa, Georgia Karayannopoulou, Jean Kanitakis
Dermatopathology.2024; 11(4): 293. CrossRef
- Metastatic Vulvar Paget's Disease Presenting in a Supraclavicular Lymph Node: A Diagnostic Challenge on Fine Needle Aspiration Cytology
Case Reports
- A Case of Endocrine Mucin-Producing Sweat Gland Carcinoma Co-existing with Mucinous Carcinoma: A Case Report.
- Sunhee Chang, Sang Hwa Shim, Mee Joo, Hanseong Kim, Yong Kyu Kim
- Korean J Pathol. 2010;44(1):97-100.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.1.97
- 5,514 View
- 51 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF - An endocrine mucin-producing sweat gland carcinoma (EMPSGC) is a rare skin tumor that most commonly occurs on the eyelids of elderly women. This tumor is morphologically analogous to endocrine ductal carcinoma in situ and solid papillary carcinoma of the breast. We describe one case of a 51-year-old male with an EMPSGC co-existing with mucinous carcinoma of the eyelid. The tumor was composed of dilated ducts with a smooth border and was partially filled with a papillary proliferation. Tumor cells were uniform, small-to-medium in size, and oval-to-polygonal with light eosinophilic cytoplasm. Nuclei were bland with diffusely stippled chromatin and inconspicuous nucleoli. Tumor cells expressed chromogranin, synaptophysin, estrogen and progesterone receptors, cytokeratin 7, and epithelial membrane antigen.
-
Citations
Citations to this article as recorded by- A Case of Endocrine Mucin-Producing Sweat Gland Carcinoma of the Eyelid
Ji Eon Kang, Sung Eun Kim, Suk-Woo Yang
Journal of the Korean Ophthalmological Society.2023; 64(2): 149. CrossRef - Endocrine mucin-producing sweat gland carcinoma: a systematic review and meta-analysis
Michael H. Froehlich, Keith R. Conti, Ivy I. Norris, Jordan J. Allensworth, Nicole A. Ufkes, Shaun A. Nguyen, Evelyn T. Bruner, Joel Cook, Terry A. Day
Journal of Dermatological Treatment.2022; 33(4): 2182. CrossRef - Next-generation sequencing analysis suggests varied multistep mutational pathogenesis for endocrine mucin-producing sweat gland carcinoma with comments on INSM1 and MUC2 suggesting a conjunctival origin
Joseph G. Mathew, Anita S. Bowman, Jad Saab, Klaus J. Busam, Kishwer Nehal, Melissa Pulitzer
Journal of the American Academy of Dermatology.2022; 86(5): 1072. CrossRef - Endocrine mucin‐producing sweat gland carcinoma and associated primary cutaneous mucinous carcinoma: Review of the literature
Rebecca Tian Mei Au, Manish M. Bundele
Journal of Cutaneous Pathology.2021; 48(9): 1156. CrossRef - An Update on Endocrine Mucin-producing Sweat Gland Carcinoma
Meghana Agni, Meisha L. Raven, Randy C. Bowen, Nora V. Laver, Patricia Chevez-Barrios, Tatyana Milman, Charles G. Eberhart, Steven Couch, Daniel D. Bennett, Daniel M. Albert, R. Nick Hogan, Paul O. Phelps, Hillary Stiefel, Norberto Mancera, Martin Hyrcza,
American Journal of Surgical Pathology.2020; 44(8): 1005. CrossRef - A Case of Endocrine Mucin-Producing Sweat Gland Carcinoma: Is it Still an Under-Recognized Entity?
Khaled A. Murshed, Mohamed Ben-Gashir
Case Reports in Dermatology.2020; 12(3): 255. CrossRef - Endocrine Mucin-Producing Sweat Gland Carcinoma, a Histological Challenge
Mary Anne Brett, Samih Salama, Gabriella Gohla, Salem Alowami
Case Reports in Pathology.2017; 2017: 1. CrossRef - Endocrine mucin‐producing sweat gland carcinoma occurring on extra‐facial site: a case report
Jia‐Huei Tsai, Tzu‐Lin Hsiao, Yi‐Ying Chen, Cheng‐Hsiang Hsiao, Jau‐Yu Liau
Journal of Cutaneous Pathology.2014; 41(6): 544. CrossRef - Endocrine Mucin-Producing Sweat Gland Carcinoma
Catharine A. Dhaliwal, Antonia Torgersen, Jonathan J. Ross, James W. Ironside, Asok Biswas
The American Journal of Dermatopathology.2013; 35(1): 117. CrossRef
- A Case of Endocrine Mucin-Producing Sweat Gland Carcinoma of the Eyelid
- Adenoid Cystic Carcinoma of Skin: A case report.
- Eun Duk Chang, Young Hee Jee, Sun Moo Kim
- Korean J Pathol. 1989;23(3):378-381.
- 2,038 View
- 11 Download
-
 Abstract
Abstract
- A primary skin adenoid cystic carcinoma first described by Boggio in 1975, is one of the rarest type of eccrine sweat gland carcinoma. Histologically, a tumor with typical morphologic features closely resembles adenoid cystic carcinoma was found in other tissues but in the skin must be distinguished from aggressive basal cell carcinoma. The natural history of this tumor is not yet fully determined but suggests a long indolent and progressive course. We report a case of a 77-year-old male with a small skin nodule in the abdomen.
- Eccrine Poroma: A report of five cases.
- Young Shin Kim, Seok Jin Kang, Byoung Kee Kim, Sun Moo Kim
- Korean J Pathol. 1991;25(4):357-362.
- 2,296 View
- 52 Download
-
 Abstract
Abstract
 PDF
PDF - The eccrine poroma was described first by Pinkus et al. in 1956 as a subgroup of benign solid hidradenoma with the histologic structure resembling acrosyringium. The histologic appearance of eccrine poroma greatly resembles that of seborrheic keratosis and basal cell carcinoma. But the clinical lesion is fairly unique and the tumor is most commonly found almost exclusively on the foot, in the skin of the plantar surface. During the past four years, the authors experienced five cases of eccrine poroma which were diagnosed by histopathological examination of the tumor mass. All the cases occurred in the sole and lateral sides of the foot as well. Clinical and pathological features were reviewed and a brief review of the literatures was done.

 E-submission
E-submission

 First
First Prev
Prev



