Search
- Page Path
- HOME > Search
Original Articles
- Primary squamous cell carcinoma of the salivary gland: immunohistochemical analysis and comparison with metastatic squamous cell carcinoma
- Uiree Jo, Joon Seon Song, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim, Kyung-Ja Cho
- J Pathol Transl Med. 2020;54(6):489-496. Published online August 31, 2020
- DOI: https://doi.org/10.4132/jptm.2020.07.19
- 10,128 View
- 206 Download
- 18 Web of Science
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
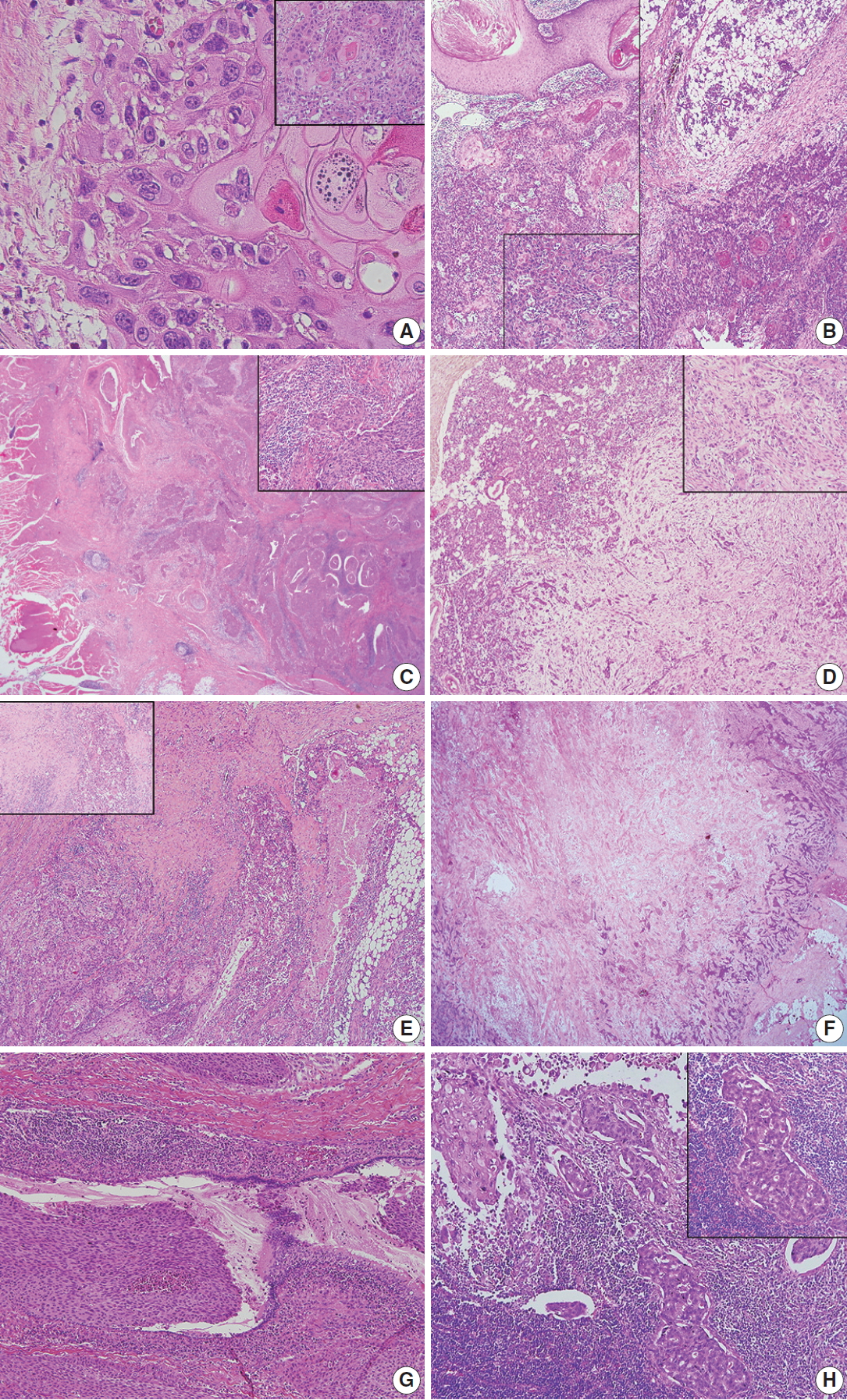
Primary squamous cell carcinoma (SCC) of the salivary gland is a rare disease, and distinguishing primary SCC from metastatic SCC is difficult. This study investigated the histological and immunohistochemical differences between primary and metastatic salivary gland SCC to improve the accuracy of diagnosis and to explore the pathogenesis of this disease.
Methods
Data of 16 patients who underwent surgery for SCC of salivary glands between 2000 and 2018 at Asan Medical Center were retrieved. Eight patients had a history of SCC at other sites, and eight patients had only salivary gland SCC. Immunostaining for p16, p53, androgen receptor (AR), gross cystic disease fluid protein 15 (GCDFP-15), and c-erbB2, as well as mucicarmine staining, were compared between the two groups.
Results
Most tumors were located in the center of the salivary glands with extraparenchymal extension. The histology of primary SCC of the salivary gland was consistent with moderately differentiated SCC with extensive desmoplastic reaction and peritumoral inflammation. Involvement of the salivary gland ducts and transition into the ductal epithelium were observed in two cases. Metastatic SCC resembled the primary tumor histologically and was associated with central necrosis. Both groups exhibited negative mucin staining. Two, one, and one primary SCC case exhibited AR, GCDFP-15, and c-erbB2 positivity, respectively.
Conclusions
A subset of primary SCCs originated in salivary ducts or was related to salivary duct carcinoma. Distinguishing primary from metastatic SCC of the salivary gland is difficult using histologic features and immunoprofiles. A comprehensive review of the medical history is essential. -
Citations
Citations to this article as recorded by- Clinical diagnosis, treatment, and survival analysis of 61 cases of salivary duct carcinoma: a retrospective study
Shubin Dong, Mengru Li, Zhiwei Zhang, Bowei Feng, Wei Ding, Jiang Chang, Feng Liu
PeerJ.2025; 13: e19626. CrossRef - Characterization of undifferentiated carcinoma of the salivary gland: clinicopathological and immunohistochemical analyses in comparison with lymphoepithelial carcinoma
Sangjoon Choi, Gyuheon Choi, Hee Jin Lee, Joon Seon Song, Yoon Se Lee, Seung-Ho Choi, Kyung-Ja Cho
Journal of Pathology and Translational Medicine.2025; 59(6): 361. CrossRef - Primary salivary gland squamous cell carcinoma with sialolithiasis in the submandibular gland: A case report and literature review
Sawako Ono, Katsutoshi Hirose, Yuji Hirata, Marie Yamada, Satoko Nakamura, Hidetaka Yamamoto
Journal of Oral and Maxillofacial Surgery, Medicine, and Pathology.2024; 36(5): 768. CrossRef - A case of primary squamous cell carcinoma of the parotid gland and review of the literature
Jingli Zhao, Xinrong Nan, Chuhuan Zhou, Nan Jiang, Liangliang Tian
Journal of Case Reports and Images in Oncology.2024; 10(1): 7. CrossRef - Metastatic cutaneous squamous cell carcinoma accounts for nearly all squamous cell carcinomas of the parotid gland
Patrick J. Bradley, Göran Stenman, Lester D. R. Thompson, Alena Skálová, Roderick H. W. Simpson, Pieter J. Slootweg, Alessandro Franchi, Nina Zidar, Alfons Nadal, Henrik Hellquist, Michelle D. Williams, Ilmo Leivo, Abbas Agaimy, Alfio Ferlito
Virchows Archiv.2024; 485(1): 3. CrossRef - Common skin cancers and their association with other non-cutaneous primary malignancies: a review of the literature
Lindsay Holic
Medical Oncology.2024;[Epub] CrossRef - Salivary duct carcinoma with squamous differentiation: histomorphological and immunophenotypical analysis of six cases
Melad N Dababneh, Christopher C Griffith, Kelly R Magliocca, Ivan J Stojanov
Histopathology.2024; 85(4): 590. CrossRef - Comprehensive Next Generation Sequencing Reveals that Purported Primary Squamous Cell Carcinomas of the Parotid Gland are Genetically Heterogeneous
Justin A. Bishop, Masato Nakaguro, Ilan Weinreb, Doreen Palsgrove, Lisa M. Rooper, Travis W. Vandergriff, Brian Carlile, Jeffrey A. Sorelle, Jeffrey Gagan, Toshitaka Nagao
Head and Neck Pathology.2024;[Epub] CrossRef - Salivary gland fine needle aspiration: a focus on diagnostic challenges and tips for achieving an accurate diagnosis
Carla Saoud, Hansen Lam, Sandra I. Sanchez, Zahra Maleki
Diagnostic Histopathology.2023; 29(8): 357. CrossRef - Salivary gland pathologies: evolution in classification and association with unique genetic alterations
Michał Żurek, Łukasz Fus, Kazimierz Niemczyk, Anna Rzepakowska
European Archives of Oto-Rhino-Laryngology.2023; 280(11): 4739. CrossRef - A retrospective study of nonneoplastic and neoplastic disorders of the salivary glands
Sorin Vamesu, Oana Andreea Ursica, Ana Maria Gurita, Raluca Ioana Voda, Mariana Deacu, Mariana Aschie, Madalina Bosoteanu, Georgeta Camelia Cozaru, Anca Florentina Mitroi, Cristian Ionut Orasanu
Medicine.2023; 102(42): e35751. CrossRef - Pembrolizumab as a first line therapy in a patient with extensive mucoepidermoid salivary gland carcinoma. A complete clinical, radiological and pathological response. A very specific case
Raed Farhat, Noam Asna, Yaniv Avraham, Ashraf Khater, Majd Asakla, Alaa Safia, Sergio Szvalb, Nidal Elkhatib, Shlomo Merchavy
Discover Oncology.2022;[Epub] CrossRef - Morphologic CT and MRI features of primary parotid squamous cell carcinoma and its predictive factors for differential diagnosis with mucoepidermoid carcinoma
Xiaohua Ban, Huijun Hu, Yue Li, Lingjie Yang, Yu Wang, Rong Zhang, Chuanmiao Xie, Cuiping Zhou, Xiaohui Duan
Insights into Imaging.2022;[Epub] CrossRef - A Rare Case of Primary Squamous Cell Carcinoma of the Submandibular Salivary Gland: Brief Overview of Diagnostic Ambiguity and Treatment Challenges
Pawan Hingnikar, Anendd Jadhav, Nitin D Bhola
Cureus.2022;[Epub] CrossRef - Necrotizing Sialometaplasia of the Hard Palate: Diagnosis and
Treatment
Sangeun Lee, Yun Sung Lim, Kyuho Lee, Bo Hae Kim
Journal of Clinical Otolaryngology Head and Neck Surgery.2022; 33(4): 236. CrossRef - Parotid Salivary Duct Carcinoma With a Prominent Squamous Component: Immunohistochemical Profile, Diagnostic Pitfalls, and Therapeutic Implications
Naomi Hardy, Joshua Thompson, Ranee Mehra, Cinthia B. Drachenberg, Kyle Hatten, John C. Papadimitriou
International Journal of Surgical Pathology.2021; 29(7): 726. CrossRef - Intrasalivary Thymic Carcinoma: A Case Report and Literature Review
Michał Kunc, Alexandra Kamieniecki, Grzegorz Walczak, Tomasz Nowicki, Bartosz Wasąg, Bogusław Mikaszewski, Dominik Stodulski, Wojciech Biernat
Head and Neck Pathology.2021; 16(3): 857. CrossRef - Cancer Stem Cell Markers in Squamous Cell Carcinomas of the Salivary Glands
Mattis Bertlich, Julia Kitz, Marie Kruizenga, Jennifer Lee Spiegel, Martin Canis, Friedrich Ihler, Frank Haubner, Bernhard G. Weiss, Mark Jakob
Oncology.2021; 99(6): 402. CrossRef
- Clinical diagnosis, treatment, and survival analysis of 61 cases of salivary duct carcinoma: a retrospective study
- Analysis of PAX8 immunohistochemistry in lung cancers: a meta-analysis
- Jae Han Jeong, Nae Yu Kim, Jung-Soo Pyo
- J Pathol Transl Med. 2020;54(4):300-309. Published online July 10, 2020
- DOI: https://doi.org/10.4132/jptm.2020.06.08
- 9,322 View
- 153 Download
- 11 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
In this meta-analysis, we aimed to evaluate the PAX8 immunohistochemical expressions in primary lung cancers and metastatic cancers to the lung.
Methods
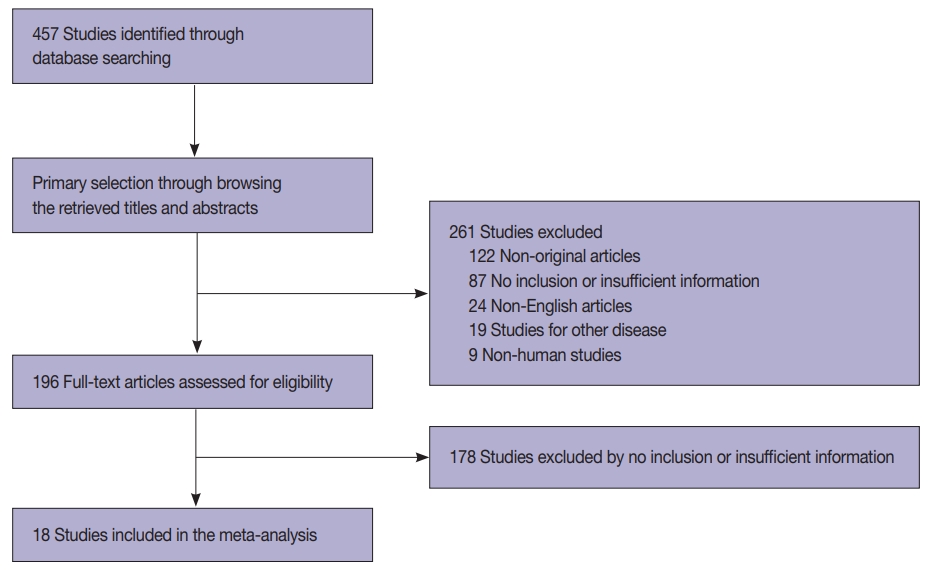
We identified and reviewed relevant articles from the PubMed databases. Ultimately, 18 articles were included in this meta-analysis. PAX8 expression rates were analyzed and compared between primary and metastatic lung cancers.
Results
The PAX8 expression rate in primary lung cancers was 0.042 (95% confidence interval [CI], 0.025 to 0.071). PAX8 expression rates of small cell (0.129; 95% CI, 0.022 to 0.496) and non-small cell carcinomas of the lung (0.037; 95% CI, 0.022 to 0.061) were significantly different (p=.049 in a meta-regression test). However, the PAX8 expression rates of adenocarcinoma (0.013; 95% CI, 0.006 to 0.031) and squamous cell carcinoma (0.040; 95% CI, 0.016 to 0.097) were not significantly different. PAX8 expression rates of metastatic carcinomas to the lung varied, ranging from 1.8% to 94.9%. Metastatic carcinomas from the lung to other organs had a PAX8 expression rate of 6.3%. The PAX8 expression rates of metastatic carcinomas from the female genital organs, kidneys, and thyroid gland to the lung were higher than those of other metastatic carcinomas.
Conclusions
Primary lung cancers had a low PAX8 expression rate regardless of tumor subtype. However, the PAX8 expression rates of metastatic carcinomas from the female genital organs, kidneys, and thyroid were significantly higher than those of primary lung cancers. -
Citations
Citations to this article as recorded by- Clinical significance of lncRNA PAX8-AS1 and miR-96-5p in non-small cell lung cancer
Qiaoling Ying, Hui Xu, Xiaojiao Wu, Hang Fang, Jingjing Shi, Hangcheng Pan
Journal of Cardiothoracic Surgery.2025;[Epub] CrossRef - Lung Metastatic Recurrence as Carcinosarcoma from Ovarian Mesonephric-Like Adenocarcinoma: A Case Report
Kaito Nakama, Masayuki Ota, Takanori Aihara, Satoko Kageyama, Jun-ichiro Ikeda
International Journal of Surgical Pathology.2025;[Epub] CrossRef - The TTF-1 and Napsin A Trap: Metastatic Endometrial Carcinoma Masquerading as Lung Primary
Carmen Alfonso-Rosa, Jesús Machuca-Aguado, Ana María Montaña-Ramírez, Francisco Javier Rubio-Garrido
International Journal of Surgical Pathology.2025;[Epub] CrossRef - Prognostic value of PAX8 in small cell lung cancer
Fengyun Tao, Hangyan Zhu, Jiayun Xu, Yanan Guo, Xin Wang, Lei Shao, Deng Pan, Guosheng Li, Rong Fang
Heliyon.2024; 10(7): e28251. CrossRef - Cystic primary squamous cell carcinoma of the thyroid
Sakurako Harada‐Kagitani, Yusuke Kouchi, Yoshiki Shinomiya, Takuto Hiramoto, Tomoyuki Arai, Toyoyuki Hanazawa, Kiyotaka Onodera, Kaito Nakama, Takanori Aihara, Masayuki Ota, Jun‐Ichiro Ikeda, Takashi Kishimoto
Pathology International.2024; 74(5): 292. CrossRef - The combination of p16 and Rb expression pattern is helpful to predict high-risk HPV infection and the primary site in lymph node metastases of squamous cell carcinoma
Ryosuke Kuga, Hidetaka Yamamoto, Fumiya Narutomi, Misa Suzuki, Rina Jiromaru, Takahiro Hongo, Kazuhisa Hachisuga, Nobuko Yasutake, Kiyoko Kato, Takashi Nakagawa, Yoshinao Oda
Pathology - Research and Practice.2024; 263: 155642. CrossRef - Mesonephric adenocarcinoma of the uterine cervix with a prominent spindle cell component
Yingying Fan, Ying He, Liang Sun, Tianmin Liu, Yangmei Shen
Oncology Letters.2024;[Epub] CrossRef - Immunocytochemistry of effusions: Processing and commonly used immunomarkers
Vinod B. Shidham, Beata Janikowski
Cytojournal.2022; 19: 6. CrossRef - Significance analysis of PAX8 expression in endometrial carcinoma
Shan Hu, Hua Gan, Fengmei Yang
Medicine.2022; 101(42): e31159. CrossRef
- Clinical significance of lncRNA PAX8-AS1 and miR-96-5p in non-small cell lung cancer
- Prognostic Role of Metastatic Lymph Node Ratio in Papillary Thyroid Carcinoma
- Jung-Soo Pyo, Jin Hee Sohn, Kyungseek Chang
- J Pathol Transl Med. 2018;52(5):331-338. Published online August 30, 2018
- DOI: https://doi.org/10.4132/jptm.2018.08.07
- 9,192 View
- 131 Download
- 16 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The aim of this study is to elucidate the clinicopathological significances, including the prognostic role, of metastatic lymph node ratio (mLNR) and tumor deposit diameter in papillary thyroid carcinoma (PTC) through a retrospective review and meta-analysis.
Methods
We categorized the cases into high (≥ 0.44) and low mLNR (< 0.44) and investigated the correlations with clinicopathological parameters in 64 PTCs with neck level VI lymph node (LN) metastasis. In addition, meta-analysis of seven eligible studies was used to investigate the correlation between mLNR and survival.
Results
Among 64 PTCs with neck level VI LN metastasis, high mLNR was found in 34 PTCs (53.1%). High mLNR was significantly correlated with macrometastasis (tumor deposit diameter ≥ 0.2 cm), extracapsular spread, and number of metastatic LNs. Based on linear regression test, mLNR was significantly increased by the largest LN size but not the largest metastatic LN (mLN) size. High mLNR was not correlated with nuclear factor κB or cyclin D1 immunohistochemical expression, Ki-67 labeling index, or other pathological parameters of primary tumor. Based on meta-analysis, high mLNR significantly correlated with worse disease-free survival at the 5-year and 10-year follow-up (hazard ratio [HR], 4.866; 95% confidence interval [CI], 3.527 to 6.714 and HR, 5.769; 95% CI, 2.951 to 11.275, respectively).
Conclusions
Our data showed that high mLNR significantly correlated with worse survival, macrometastasis, and extracapsular spread of mLNs. Further cumulative studies for more detailed criteria of mLNR are needed before application in daily practice. -
Citations
Citations to this article as recorded by- The application of a clinical-multimodal ultrasound radiomics model for predicting cervical lymph node metastasis of thyroid papillary carcinoma
Chang Liu, Shangjie Yang, Tian Xue, Qian Zhang, Yanjing Zhang, Yufang Zhao, Guolin Yin, Xiaohui Yan, Ping Liang, Liping Liu
Frontiers in Oncology.2025;[Epub] CrossRef - The Predictive Value of a Nomogram Based on Ultrasound Radiomics, Clinical Factors, and Enhanced Ultrasound Features for Central Lymph Node Metastasis in Papillary Thyroid Microcarcinoma
Lei Gao, Xiuli Wen, Guanghui Yue, Hui Wang, Ziqing Lu, Beibei Wu, Zhihong Liu, Yuming Wu, Dongmei Lin, Shijian Yi, Wei Jiang, Yi Hao
Ultrasonic Imaging.2025; 47(2): 93. CrossRef - Lymph Node Metastasis Ratio: Prognostic Significance in Papillary Thyroid Cancer
Ana Rita Ferreira, Diogo Ramalho, Daniela Martins, Andreia Amado, Susana Graça, Carlos Soares, Bela Pereira, Maria João Oliveira, Manuel Oliveira, Antónia Póvoa
Indian Journal of Surgery.2025; 87(6): 1047. CrossRef - CD105 (Endoglin) Expression as a Prognostic Marker in Aggressive Papillary Thyroid Carcinoma
İlker Çordan, Tuğba Günler
Clinical Endocrinology.2025; 103(4): 596. CrossRef - Application and subgroup analysis of competing risks model based on different lymph node staging systems in differentiated thyroid cancer
Zhe Xu Cao, Jiang Sheng Huang, Ming Ming Wang
Updates in Surgery.2024; 76(5): 1927. CrossRef - Цитологічне прогнозування агресії раку щитоподібної залози як новий перспективний напрямок у клінічній тиреоїдології
H.V. Zelinska
Endokrynologia.2024; 29(4): 363. CrossRef - Thyroglobulin expression, Ki-67 index, and lymph node ratio in the prognostic assessment of papillary thyroid cancer
Helene Lindfors, Marie Karlsen, Ellinor Karlton, Jan Zedenius, Catharina Larsson, Catharina Ihre Lundgren, C. Christofer Juhlin, Ivan Shabo
Scientific Reports.2023;[Epub] CrossRef - Incidental Node Metastasis as an Independent Factor of Worse Disease-Free Survival in Patients with Papillary Thyroid Carcinoma
Renan Aguera Pinheiro, Ana Kober Leite, Beatriz Godoi Cavalheiro, Evandro Sobroza de Mello, Luiz Paulo Kowalski, Leandro Luongo Matos
Cancers.2023; 15(3): 943. CrossRef - A High-Quality Nomogram for Predicting Lung Metastasis in Newly Diagnosed Stage IV Thyroid Cancer: A Population-Based Study
WenYi Wang, JiaJing Liu, XiaoFan Xu, LiQun Huo, XuLin Wang, Jun Gu
Technology in Cancer Research & Treatment.2023;[Epub] CrossRef - Lymph Node Ratio Predicts Recurrence in Patients with Papillary Thyroid Carcinoma with Low Lymph Node Yield
Il Ku Kang, Joonseon Park, Ja Seong Bae, Jeong Soo Kim, Kwangsoon Kim
Cancers.2023; 15(11): 2947. CrossRef - Superiority of metastatic lymph node ratio over number of node metastases and TNM/AJCC N classification in predicting cancer‐specific survival in medullary thyroid cancer
Andreas Machens, Kerstin Lorenz, Frank Weber, Henning Dralle
Head & Neck.2022; 44(12): 2717. CrossRef - Value of Combining Clinical Factors, Conventional Ultrasound, and Contrast-Enhanced Ultrasound Features in Preoperative Prediction of Central Lymph Node Metastases of Different Sized Papillary Thyroid Carcinomas
Yanfang Wang, Fang Nie, Guojuan Wang, Ting Liu, Tiantian Dong, Yamin Sun
Cancer Management and Research.2021; Volume 13: 3403. CrossRef - Atypical Histiocytoid Cells and Multinucleated Giant Cells in Fine-Needle Aspiration Cytology of the Thyroid Predict Lymph Node Metastasis of Papillary Thyroid Carcinoma
Ji Eun Choi, Ja Seong Bae, Dong-Jun Lim, So Lyung Jung, Chan Kwon Jung
Cancers.2019; 11(6): 816. CrossRef - Patients Aged ≥55 Years With Stage T1-2N1M1 Differentiated Thyroid Cancer Should Be Downstaged in the Eighth Edition AJCC/TNM Cancer Staging System
Zeming Liu, Sichao Chen, Yihui Huang, Di Hu, Min Wang, Wei Wei, Chao Zhang, Wen Zeng, Liang Guo
Frontiers in Oncology.2019;[Epub] CrossRef - Prognostic Implication of Metastatic Lymph Node Ratio in Colorectal Cancers: Comparison Depending on Tumor Location
Jung-Soo Pyo, Young-Min Shin, Dong-Wook Kang
Journal of Clinical Medicine.2019; 8(11): 1812. CrossRef
- The application of a clinical-multimodal ultrasound radiomics model for predicting cervical lymph node metastasis of thyroid papillary carcinoma
Brief Case Reports
- Periductal Stromal Tumor of Breast: A Case Report and A Review of Literature
- Salma L. Abbasi, Kate McNamara, Mohammed S. Absar, Alison Darlington, Francene Clucas, Sami Titi
- Korean J Pathol. 2014;48(6):442-444. Published online December 31, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.6.442
- 13,335 View
- 89 Download
- 5 Crossref
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Genetic profiling of mammary periductal stromal tumors with histologic correlation highlights high-grade and low-grade groups and similarities to phyllodes tumors
Gregor Krings, Gregory R. Bean, Elizabeth M. Hosfield, J.J. Rowe, Joseph Geradts, Yunn-Yi Chen
Modern Pathology.2026; : 100961. CrossRef - Survey of recurrent diagnostic challenges in breast phyllodes tumours
Benjamin Yongcheng Tan, Stephen B Fox, Sunil R Lakhani, Puay Hoon Tan
Histopathology.2023; 82(1): 95. CrossRef - Management of a periductal stromal tumor in a young woman: Our breast unit experience
Irene Valente, Adela Ristani, Cristina Mancini, Eugenia Martella, Leonardo Quartieri, Cecilia D'Aloia
The Breast Journal.2020; 26(7): 1375. CrossRef - A Diagnostic Approach to Fibroepithelial Breast Lesions
Benjamin Yongcheng Tan, Puay Hoon Tan
Surgical Pathology Clinics.2018; 11(1): 17. CrossRef - A case of local recurrence of periductal stromal sarcoma of the breast
Kana TERAMOTO, Yasuro DOI, Kayo YAMAMOTO, Kaname MATSUKAWA, Hisaka IWAIHARA, Rumi MOTOSHIMA, Noboru TAKATA, Ichiro YOSHINAKA, Kazunori HARADA
Choonpa Igaku.2018; 45(1): 61. CrossRef
- Genetic profiling of mammary periductal stromal tumors with histologic correlation highlights high-grade and low-grade groups and similarities to phyllodes tumors
- Digital Papillary Carcinoma
- Sharon Lim, Inju Cho, Mi Ja Lee
- Korean J Pathol. 2014;48(6):438-441. Published online December 31, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.6.438
- 10,182 View
- 50 Download
- 5 Crossref
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Digital Papillary Adenocarcinoma: Uncommon Malignancy of Sweat Glands - Two Rare Cases
Neeti Goyal, Pawan Dhaman, Jasvinder Kaur Bhatia, Pragya Sharma, Prabha Shankar Mishra, Vikram Singh, Anvesh Rathore
Journal of Marine Medical Society.2025; 27(1): 103. CrossRef - Digital papillary adenocarcinoma: A case report of a rare malignant tumour with recommendations on management and follow-up
Varanindu Mudduwa, Mohammad Goodarzi, Richard Chalmers, Haitham Khashaba
International Journal of Surgery Case Reports.2025; 127: 110922. CrossRef - Digital Papillary Carcinoma: A Literature Review of Epidemiology, Management Strategies, and Patient Outcomes
William Liu, Rahul Nanda, David Zloty
Dermatologic Surgery.2025;[Epub] CrossRef - Digital papillary adenocarcinoma: A case report
Betty A. Kasimo, Vivian Akello, James J. Yahaya
Clinical Case Reports.2021;[Epub] CrossRef - A rare case of a digital papillary carcinoma of the hand with secondary conservative management
Rabeet Khan, Renu Irri, Effie Katsarma
Journal of Surgical Case Reports.2020;[Epub] CrossRef
- Digital Papillary Adenocarcinoma: Uncommon Malignancy of Sweat Glands - Two Rare Cases
Review
- The Cytopathology of Body Cavity Fluid.
- Eun Kyung Hong
- J Pathol Transl Med. 2008;19(2):72-85.
- DOI: https://doi.org/10.3338/kjc.2008.19.2.72
- 3,391 View
- 30 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Cytologic examination of the body cavity fluid is very important because the specimens represent a significant percentage of nongynecologic samples and this cytologic examination may be the first, best or only chance for making the diagnosis of an underlying malignancy. The purposes of body cavity fluid examination are to correctly identify cancer cells and if possible, to identify the tumor types and primary sites when presented with unknown primary tumor sites. The most important basic differential diagnosis is that of benign and reactive disease vs malignant disease. Reactive mesothelial cells are a consistent population in body cavity fluid, and these are the most versatile cells in the body. Due to the specific environment of the body cavity, the exfoliated reactive mesothelial cells may show significant morphologic overlap with the morphology of cancer cells. With a focus on the differential points between reactive mesothelial cells and metastatic adenocarcinoma cells, the practical diagnostic approaches, the diagnostic clues and the pitfalls to achieve a correct diagnosis are presented in this review.
-
Citations
Citations to this article as recorded by- A cytological observation of the fluid in the primo-nodes and vessels on the surfaces of mammalian internal organs
Baeckkyoung Sung, Min Su Kim, Byung-Cheon Lee, Seong-Hun Ahn, Sung-Yeoun Hwang, Kwang-Sup Soh
Biologia.2010; 65(5): 914. CrossRef
- A cytological observation of the fluid in the primo-nodes and vessels on the surfaces of mammalian internal organs
Original Article
- The p53 Mutation and DNA Ploidy in Human Metastatic Breast Cancer.
- Seong Jin Cho, Ae Ree Kim, Nam Hee Won
- Korean J Pathol. 1997;31(2):135-144.
- 2,043 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - The p53 gene, one of the tumor suppressor genes, is believed to play an important role through mutation and overexpression in the progression of various human malignant tumors. To compare the p53 mutation status between the primary and metastatic lesions of breast cancers and to investigate the mutational pattern of p53, immunohistochemistry (IHC) and polymerase chain reaction and single strand conformational polymorphism (PCR-SSCP) were performed in 25 cases of breast cancers with paraffin embedded tissue. Mutant protein products or point mutation were detected through IHC or PCR-SSCP method. And flow cytometrical (FCM) analysis were performed in the same paraffin blocks to correlate the DNA ploidy and p53 mutation. The following results are summarized. 1. The detection of the p53 gene mutation and overexpression of the p53 protein were measured in 40% and 48%, respectively, in 25 primary tumors, either or both methods was detected in 64%. 2. A concordance rate of the p53 protein expression between the primary and metastatic lesions of 25 breast cancers was 100%, but the concordance rate of the p53 gene mutation was 72%. 3. The correlation between the p53 mutation and the DNA aneuploidy was not statistically significant (p=0.38) 4. A p53 mutation by IHC or PCR-SSCP was more frequently detected in grade III breast cancers than in grade I or II. 5. Among 5 to 9 exons of the p53 gene, exon 7 was the most frequent mutation spot in this study. 6. Additional mutation of the p53 gene was developed in the three metastatic lesions. With the above results it is suggested that the p53 protein overexpression by immunohistochemistry is not correlated with the p53 mutation by PCR-SSCP. The p53 mutation pattern between the primary and metastatic lesions are not idenitical and an additional point mutation can occur in the metastatic lesion. The DNA aneuploidy is more frequently detected in the cases with the p53 protein overexpression than in the p53 protein negative, but it is not statistically significant.
Case Report
- Metastatic Adenoid Cystic Carcinoma of the Lung Diagnosed by Fine Needle Aspiration Biopsy.
- So Yeon Park, Kwang Gil Lee
- J Pathol Transl Med. 1990;1(2):175-178.
- 2,448 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - A case of metastatic adenoid cystic carcinoma of the lung, originated from the trachea, was diagnosed by fine needle aspiration. Although the cytologic features of adenoid cystic carcinoma have been well described, it is easy to confuse adenoid cystic carcinoma with more common primary small cell neoplasms of the lung, i.e., small cell carcinoma, well differentiated adenocarcinoma, and carcinoid tumor of the lung. The features distinguishing adenoid cystic carcinoma from these neoplasms include 1) tight, globular, honeycomb pattern of cells, 2) acellular basement membrane material in the lumen, and 3) cells lacking true nuclear molding and having bland chromatin pattern. The morphologic feature of metastatic adenoid cystic carcinoma in this case was so distinctive as to permit a definite diagnosis by aspiration cytology.
Original Articles
- Cytologic Diagnosis of Metastatic Hepatocellular Carcinoma by Aspiration Cytology of Sacrum.
- Jungweon Shim, Illhyang Ko
- J Pathol Transl Med. 1990;1(2):179-184.
- 2,160 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Bone metastasis of hepatocellular carcinoma appears to be peculiar when clinical manifestation of liver disease is not apparent, and initial diagnosis of metastatic hepatocellular carcinoma by fine needle aspiration cytology is rarely obtained. We experienced a case of 45-year-old man with metastatic hepatocellular carcinoma in the sacrum, which was diagnosed by fine needle aspiration cytology. The intrahepatic mass, measuring 1.2 cm in diameter and kept unchanged in size for two years, was never proved to be hepatocellular carcinoma histopathologically. The aspirated neoplastic cells were mostly in sheets, showing abundant acidophilic cytoplasm and large, round. centrally located nuclei with single, prominent acidophilic mucleoti. In the cell block section, diagnosis of metastatic well-differentiated hepatocellular carcinoma was made without difficulty, and definite trabecular fashion with sinusoidal endothelial cell lining was found.
- Immunohistochemical Study on the Ha-ras p21 Expression in the Gastric Carcinoma.
- Kwang Min Lee, Joo Yong Yoo
- Korean J Pathol. 1990;24(1):1-9.
- 1,961 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - We have investigated an immunohistochemical expression of the Human-Ha-ras oncogene product p21 in tumor cells of the primary mass and metastatic lymph nodes with different histological features of gastric cancer by using avidinbiotin complex immunoperoxidase method in formalin-fixed tissue sections from 73 cases of primary tumor mass and 23 cases of metastatic lymph node. Histologic type of the gastric cancer was classification. The results obtained were as follows: 1) Expression of Ha-ras p21 was consistantly increased in the well differentiated tubular adenocarcinoma as compared with poorly differentiated tubular adenocarcinoma (p<0.01), and was substantially decreased in mucinous carcinoma and signet ring cell carcinoma. 2) Signet ring cell carcinoma showed that positive immunoperoxidase reaction for Ha-ras p21 exhibited in the majority of immature signet ring cell with scant cytoplasm rather than in the mature signet ring cells which have abundant cytoplasm filled with mucin. This findings indicate that mucin production from the tumor cell was not correlated with activation of ras gene in the tumor tissue of gastric carcinoma. 3) In general Ha-ras p21 expression was enhanced in the metastatic tumor cells of the regional lymph node compared with primary tumor, especially it was consistantly increase in the well differentiated tubular adenocarcinoma.
Case Report
- Fine Needle Aspiration Cytology of Metastatic Adenocarcinoma of Thyroid Gland from the Colon: Report of A case.
- Sook Kim, So Young Jin, Dong Wha Lee
- J Pathol Transl Med. 1994;5(1):41-45.
- 2,008 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Most common metastatic tumors of the thyroid gland are squamous cell carcinoma of head and neck region, adenocarcinoma of breast and lung, malignant melanoma, and renal cell carcinoma of kidney in order of frequency. Metastasis from gastrointestinal tract to the thyroid gland rarely occurs. We experienced a case of fine needle aspiraton cytology of metastatic adenocarcinoma of both thyroid glands from the colon. Cytologic smears showed picket-fence like arrangement of nuclei of carcinoma cells and syncytial type of tissue fragments with acinar pattern on necrotic or mucoid background.
Original Articles
- Sinusoidal Involvement of Malinant Lymphoma in Lymph Nodes Simulating Metastatic Carcinoma.
- Young Seak Kim, Mi Kyung Shin, In Sun Kim
- Korean J Pathol. 1991;25(1):45-49.
- 2,245 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - We present a case of this distinctive variety of malignant lymphoma, which was diagnosed in the axillary lymph nodes of a 66-year-old woman. The patient was admitted to the GS department due to palpable mass on the right axillary area for two months. A 2 x 1 cm sized mass was also palpated on the cervical area. The laboratory and radiologic findings were unremarkable. Axillary dissection was done under the impression of metastatic carcinoma from breast. Received lymph nodes were multiple and variable in size, ranging from 0.5 cm to 5.0 cm in diameter. Histologically, the lymph nodes were partly effaced and involved by nodular and diffuse infiltrations of large lymphoid cells in the subcapsular and medullary sinuses. In diffuse areas, typical starry-sky pattern was seen. Immunohistochemically, the tumor cells were negative for broad-spectrum keratin, but positive for leukocyte antigen, ML, and B cell markers, L26, and 4KB5. T cell marker. UCHL1 was negative. On staining with histiocytic marker, Mac387 antibody, the tingible-body macrophages were only positive. Interstitial plasma cells and some of the tumor cells were positive for lambda light chain. Electron microscopic study, which was done on paraffin embedded tissue showed lymphoid-type of nuclei without cellular junction suggestive for carcinoma.
- Expression Patterns of Tumor Related Proteins for Differential Diagnoses of Intrahepatic Adenocarcinomas.
- Ghil Suk Yoon, Mi Sung Kim, Young Hwa Li, Ji Hyun Uhm, Sun Ju Kim, Tae Sook Kim, In Su Suh, Han Ik Bae
- Korean J Pathol. 2005;39(4):229-235.
- 2,027 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Background
: Differential diagnoses of intrahepatic adenocarcinomas (IHAC) play an important role in the detecting primary sites and the determining type of treatment and overall prognosis of the patient. However, histopathologic findings alone have limitations of differential diagnoses of IHAC. Methods : To clarify which tumor related proteins (TRP) are useful for differential diagnoses of IHAC, TRP expression were investigated immunohistochemically, using MUC5AC, MUC2, mAb 91.9H, MUC1, and pS2, and by high iron diamine (HID) staining in 61 clinically confirmed IHACs. Results : MUC5AC (9/18, p<0.05) and MUC1 (17/18, p>0.05) displayed the most frequent expression in cholangiocarcinomas, and MUC2 (11/18, p<0.05), mAb 91.9H (16/18, p<0.05), and HID (16/18, p<0.05) in colorectal adenocarcinomas. pS2 (3/11, p>0.05) was expressed more often in pancreatic adenocarcinomas than other IHAC, while MUC2 and 91.9H were not expressed at all in pancreatic adenocarcinomas. The positivity of several TRP did not correlate with tumor differentiation. Conclusions : MUC5AC, MUC2, mAb 91.9H, and HID may be useful in differentiating cholangiocarcinomas from colorectal adenocarcinomas.
- Cytopathology of Metastatic Mucoepidermoid Carcioma of the Lung.
- Weon Seo Park, Eui Keun Ham
- J Pathol Transl Med. 1994;5(2):180-183.
- 1,753 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - A case of metastatic mucoepidermoid carcinoma of the lung, originating from the hard palate, was diagnosed by sputum and bronchial washing cytology. Although the cytologic features of mucoepidermoid carcinoma have been well described, it is easy to confuse mucoepidermoid carcinoma with the more common primary adenocarcinoma or squamous cell carcinoma of the lung. The features distinguishing mucoepidermoid carcinoma from other primary neoplasms includ 1) mucus-secreting cells individually and in clusters admixed with other cell components, 2) epidermoid cells identified by the presence of abundant spread-out cytoplasm and an oval dark nucleus and 3) intermediate cells resembiling normal ductal epithelial cells with moderate-toscanty cytoplasm, a central, round vesicular nucleus and a prominent nucleolus, The morphologic features of metastatic mucoepidermoid carcinoma in the case were similar to those of primary sallvary mucoepidermoid carcinoma.
- Metastatic Carcinoma in Lymph Nodes of Neck: Analysis of 221 Cases Diagnosed by Fine Needle Aspiration Cytology.
- Duck Hwan Kim, Youn Ju Kim, Seung Eun Yang, Sung Suk Paeng, Hee Jin Chang, Jin Hee Sohn, Jung Il Suh
- J Pathol Transl Med. 1995;6(1):41-47.
- 2,228 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - Two hundreds and twenty one consecutive patients with enlarged lymph nodes of neck areas were diagnosed as metastatic carcinoma by fine needle aspiration. The metastatic carcinomas were most frequent in the supraclavicular lymph nodes(p<0.05). As a primary site, lung, stomach, upper respiratory tract and breast were common sites in descending order of frequency. In overall cytologic types, squamous cell carcinoma was the most common in males(43%) while adenocarcinoma was the most common in females(72%) (p<0.05). While carcinomas of the esophagogastro -intestinal tract showed a tendency to metastasis to the left supraclavicular lymph nodes, the metastatic carcinomas of lung and breast usually metastasized to the same side primary cancers with predilection for the supraclavicular lymph nodes. The submandibular lymph nodes were frequently involved by the carcinoma of upper and lower respiratory tract, in which squamous cell carcinoma is the most prevalent cytologic type. diagnosis by fine needle aspiration cytology is the first step in the workup of patients with nodal enlargement suspicious for malignancy, particularly in metastatic carcinoma.
Case Report
- Metastatic Adenocarcinoma of Colon in Meningioma: A case report.
- Yung Suk Lee, Hyun I Cho, Jong Sang Choi, In Sun Kim
- Korean J Pathol. 1994;28(2):173-178.
- 2,308 View
- 30 Download
-
 Abstract
Abstract
 PDF
PDF - Cases of metastases from extracranial tumor to intracranial tumor are very rare. The world wide review of the literatures until 1992 revealed 44 cases of primary intracranial tumors containing metastatic tumors which are unrelated extracranial primary malignant tumors; the intracranial recipient tumor is a meningioma in 35 cases among them. Carcinomas of the lung and the breast are the most common extracranial donor tumors. Metastases from colon cancer to meningioma are extremely rare. A 74 year-old-female presented with headache for 2 weeks. CT revealed a round mass with high signal intensity, measuring 4 cm in diameter, which is located in the left parietal lobe. The patient had colon cancer 2 years ago and lymphoma I year ago. On operation, the tumor is relatively well delineated and attached to the meninx. Microscopically, the tumor is composed of fascicles of long slender, fibroblast-like spindle cells with indistinct cytoplasmic border, variable amount of collagen deposit and many psammoma bodies. A few scattered glands are present in periphery of the meningioma. The tumor glands are composed of columnar cells with basally located hyperchromatic nuclei and similiar to the glands of the adenocarcinoma of the colon.
Original Articles
- Cytologic Analysis of Metastatic Malignant Tumor in Pleural and Ascitic Fluid.
- Mee Joo, Hye Je Cho
- J Pathol Transl Med. 1995;6(2):125-132.
- 3,224 View
- 85 Download
-
 Abstract
Abstract
 PDF
PDF - Cytodiagnosis of pleural and ascitic fluid is a commonly performed laboratory examination. Especially, positivity for malignant cells in effusion cytology is very effective and also presents the first sign of malignancy in unknown primary site of the tumor. We examined each 34 cases of pleural and ascitic fluid cytologic specimen diagnosed as metastatic tumor, which was selected among 964 pleural fluid cytology cases and 662 ascitic fluid cytology cases from September 1989 to June 1995. Among the ascitic fluid cytology specimens examined, 34 specimens were positive in 29 patients. The most common primary neoplasms were carcinomas of ovary (32%), stomach (32%), colon (6%), breast (3%), pancreas (3%), and lung (3%) and lymphoreticular neoplasms (3%). The metastatic tumor was predominantly adenocarcinoma type in both pleural (82%) and ascitic (91%) fluid. The study of metastatic adenocarcinoma in effusion from lung, ovary, and stomach was undertaken to find distinctive features for the identification of the primary site. The smears of metastatic pulmonary adenocarcinoma had a tendency to show high grade pleomorphism and many large tight cell clusters, whereas that of the ovarian adenocarcinoma showed low grade pleomorphism with abundant intracytoplasmic vacuoles in relatively clear background. That of the stomach revealed the intermediate features.
- Cytologic Features of Metastatic Melanoma.
- Jae Hee Suh, Joo Ryung Huh, Gyung Yub Gong
- J Pathol Transl Med. 1996;7(2):185-191.
- 3,837 View
- 155 Download
-
 Abstract
Abstract
 PDF
PDF - Metastatic melanoma is often difficult to diagnose morphologically. However, the prognostic and therapeutic decision in cases of metastatic melanoma depends upon the morphologic documentation of the metastatic disease, which may rapidly and accurately be done by cytologic methods such as aspiration cytology of clinically suspicious lesion. Cytological features of 12 metastatic melanoma are described. Evaluation for melanin pigment, background composition, cytoplasmic vacuoles, intranuclear inclusions, bi or multinucleated cells, eccentric nuclei, nucleoli, and degree of cellular cohesion were made. the presence of melanin pigment, prominent nucleoli, intranuclear cytoplasmic inclusions, lack of cell cohesion, and eccentric nuclei are the important and useful cytologic features in the diagnosis of metastatic melanoma. Bior multinucleated cells, cytoplasmic vacuoles, and bloody background are also frequently found in smears from metastatic melanoma.
- Analysis of Fine Needle Aspiration Cytology and Ultrasonography of Metastatic Tumors to the Thyroid.
- Eun Yoon Cho, Young Lyun Oh
- J Pathol Transl Med. 2007;18(2):133-142.
- 1,980 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - Cytologic diagnosis of the metastatic tumors to the thyroid is important in the management of the patients. There have been rare reports analyzing fine-needle aspiration (FNA) cytology of metastatic tumors to the thyroid. This study examines comprehensive cytologic findings of metastatic tumors to the thyroid with radiologic findings. The FNA cytology slides obtained from 12 cases with metastatic tumors of the thyroid; lung cancer (n=5), tongue and tonsil cancer (n=3), esophageal cancer (n=2), and breast cancer (n=2) were reviewed. Radiological study showed single mass with heterogeneous texture or multiple masses without calcification. Metastatic tumor was easily considered in a differential diagnosis of FNA cytology because they had peculiar cytological features which were not seen in primary thyroid tumor. The smear background varied from predominantly necrotic, bloody, and inflammatory to colloid. The aspirates exhibited a mixture of benign follicular cells and malignant cells in 6 cases. The characteristic cytoplasmic features of the tumor cells, such as keratin, mucin and melanin, were found in 9 cases. Although some cases mimic primary thyroid neoplasm, a careful examination of the cytological characteristics may help cytopathologists to recognize a metastatic tumor in the thyroid by FNA, and may help the clinicians to establish a proper treatment plan.
Case Report
- Metastatic Gestational Trophoblastic Disease in the Lung Occuring with Hydatidiform-mole in Tubal Pregnancy: A case report.
- Hee Jeong Ahn, Kyu Rae Kim, Chang Jo Chung
- Korean J Pathol. 1996;30(9):851-853.
- 2,373 View
- 32 Download
-
 Abstract
Abstract
 PDF
PDF - Gestational trophoblastic disease associated with the tubal pregnancy is uncommon, and the incidence has been described as 1/5000 tubal pregnancy. We have experienced a case of metastatic gestational trophoblastic disease(GTD) in the lung occuring with complete hydatidiform mole arising in tubal pregnancy. The patient was a 39-year-old, G4P2A2L2 woman with amenorrhea for 5 weeks. Ectopic pregnancy in the right fallopian tube was suspected on transvaginal ultrasonogram. A right adnexectomy was performed. The fallopian tube was markedly dilated and ruptured. The right ovary and a round hematoma had adhered to the external surface of the fallopian tube. On gross examination, no molar tissue was identified. On microscopic examination, the lumen of the dilated fallopian tube was filled with blood clots admixed with several chorionic villi showing hydropic swelling and marked proliferation of atypical trophoblasts. Proliferating syncytio-and cytotrophoblasts invaded the wall of the blood vessels of the fallopian tube and sheets of trophoblasts and some villi were identified in the lumen of blood vessels. Multiple pulmonary nodules thought to be metastatic nodules were identified in the chest X-ray and serum beta-HCG had increased 2 weeks later. This case indicates that a careful pathological examination in the ectopic pregnancy is mandatory, because tubal GTD is not clinically distinguishable from ordinary tubal pregnancy.
Original Articles
- Hepatic Fascioliasis Mimicking Metastatic Tumor.
- Jong Yup Bae, Chan Il Park
- Korean J Pathol. 1996;30(10):928-932.
- 1,818 View
- 15 Download
-
 Abstract
Abstract
 PDF
PDF - A case of hepatic fascioliasis misdiagnosed as metastatic carcinoma was reported. The patient was a 22-year-old woman who had had rectal adenocarcinoma (Duke stage C2), and had been treated by Mile'operation 8 months ago. A computed tomogram(CT) demonstrated multiple low density nodules in the liver suggesting a metastatic tumor. A partial liver lobectomy was performed. The resected liver showed multiple necrotic nodules, which appeared to be abscesses containing eggs of the Fasciola species. Parasitic infection should be considered as one of the possible etiologies of hepatic nodules which mimic metastatic carcinoma either clinically or radiologically.
- Immunohistochemical Expression of p53, E-cadherin, and nm23 Proteins in Metastatic Carcinoma of Neck Lymph Node and Corresponding Primary Carcinoma.
- Jong Kook Kim, O Jun Kwon, Byung Heon Kim
- Korean J Pathol. 2000;34(9):615-624.
- 1,883 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - This study was carried out to evaluate the immunohistochemical expressions of p53, E-cadherin, and nm23 proteins in 114 cases of metastatic carcinoma of the neck lymph node (MTLNCA) and corresponding primary carcinoma (PRCA). The positive expressions of p53, E-cadherin, and nm23 proteins were 62.3%, 58.8% and 64.0%, respectively in PRCA, and 40.4%, 38.6%, and 43.9%, respectively in MTLNCA with significant down-regulation from PRCA to MTLNCA (p<0.05). The down-regulation was correlated with female gender, moderate and poor differentiation, and adenocarcinoma in p53 protein, female gender, respiratory and gastrointestinal carcinoma in E-cadherin protein, and female gender, respiratory carcinoma, moderate differentiation, and squamous cell carcinoma in nm23 protein (p<0.05). There was no significant relationship among expressions of p53, E-cadherin, and nm23 proteins (p<0.05). In conclusion, these results suggest that the expressions of p53, E-cadherin, and nm23 proteins seem to be down-regulated from PRCA to MTLNCA and this down-regulation may play a role in invasion and metastasis.
- Fine Needle Aspiration Cytologic Findings of Metastatic Sex Cord Tumor with Annular Tubules to the Neck.
- So Yeong Oh, Myoung Jae Kang, Myoung Ja Chung, Woo Sung Moon, Dong Geun Lee
- J Pathol Transl Med. 1997;8(2):185-189.
- 1,782 View
- 13 Download
-
 Abstract
Abstract
 PDF
PDF - A sex cord tumor with annnular tubules is a relatively rare ovarian neoplasm. The cytologic findings from a fine needle aspiration biopsy of neck metastasis of a sex cord tumor with annnular tubules are described. The origin of the neck metastasis was the right ovary, and the tumor was diagnosed six years ago. The cytologic findings were characterized by tumor cells arranged in solid or follicular patterns. The tumor cells formed rosette-like or complex tubular structures with central rounded or coalesced hyaline materials. It was difficult to distinguish this tumor cytologically from granulosa cell tumor, thyroid follicular neoplasm, Sertoli-Leydig cell tumor, and Brenner tumor, but complex tubular structures were helpful in discriminating between these tumors.
- Cytologic Analysis of Malignant Tumor Cells in Cerebrospinal Fluid.
- Jae Hee Suh, Gyungyub Gong, Shin Kwang Khang, On Ja Kim
- J Pathol Transl Med. 1998;9(1):21-28.
- 2,901 View
- 59 Download
-
 Abstract
Abstract
 PDF
PDF - Cytologic evaluation of cerebrospinal fluid(CSF) is an effective tool in diagnosing many disorders involving the central nervous system(CNS). CSF examination has been found to be of particular value in the diagnosis of metastatic carcinoma, lymphomatous or leukemic involvement of CNS and certain primary CNS tumors. As a survey of metastatic tumors to CSF and an evaluation of the preparation techniques increasing cellular yield in our laboratory, 713 CSF specimens examined between July 1995 and April 1997(1 year 10 months), were reviewed. There were 75 positive and 5 suspicious cases, the latter have had no evidence of tumors clinically. Primary tumors of 75 positive cases were classified as follows; 4(5.3%) as primary brain tumors, 40(53.3%) as secondary carcinomas, 13(17.3%) as leukemias, and 18 (24.0%) as lymphomas. The most common primary site of metastatic carcinomas was the lung in 17 cases(42.5%) followed by the stomach in 13(32.5%), breast in 8 (20.0%), and unknown primary in 2(5.0%). Four primary brain tumors were 3 cerebellar medulloblastomas and a supratentorial primitive neuroectodermal tumor (PNET). All 40 metastatic carcinomas were adenocarcinoma presented as single cells or cell clusters. Although signet ring cells were frequent in the cases of gastric primary cancers, no significant cytologic differences according to the primary site were observed. The cytologic features of leukemia and lymphoma were characterized by hypercellular smears presenting as individual atypical cells with increased N/C ratio, presence of nucleoli, and nuclear protrusions. In medulloblastomas and PNET, the principal cytologic findings were small undifferentiated cells arranged singly or in loose clusters with occasional rosettoid features. This study suggests that the CSF cytology is useful in the diagnosis of malignancy, especially metastatic extracranial tumors and the diagnostic accuracy can be improved by increasing cellular yield using cytocentrifuge.
Case Report
- Fine Needle Aspiration Cytology of Metastatic Melanoma in the Breast: A Case Report.
- Young Lyun Oh, Young Hyeh Ko
- J Pathol Transl Med. 1998;9(1):111-116.
- 2,213 View
- 30 Download
-
 Abstract
Abstract
 PDF
PDF - Although the characteristic cytologic features of melanoma have been well described, the diagnosis of metastatic melanoma by fine needle aspiration cytology (FNAC) may be difficult in the case of amelanotic melanoma and in the absence of awareness of clinical history. Furthermore, when the breast is the site of initial presentation, it could simulate a primary breast carcinoma leading to misdiagnosis. The recognition of metastatic malignant melanoma in FNAC material is essential to avoid an unnecessary mastectomy and to ensure appropriate chemotherapy. We experienced a case of metastatic melanoma of breast which presented as solitary breast mass in a 56-year-old woman. She had a history of surgical excision of right foot for melanoma one year ago. The cytologic smears were composed of noncohesive epithelioid cells with round or eccentric nuclei, bi-or multi-nucleation, prominent nucleoli, fine chromatin, and intranuclear inclusions. The cytoplasm of tumor cells had scanty melanin pigment but were diffusely positive for S-100 protein.
Original Article
- Expression of Cytokeratins 7 and 20 in Cholangiocarcinoma and Metastatic Colonic Adenocarcinoma of the Liver.
- Cheol Keun Park, Mi Kyung Kim
- Korean J Pathol. 1999;33(1):42-47.
- 3,034 View
- 34 Download
-
 Abstract
Abstract
 PDF
PDF - The distinction between cholangiocarcinoma (CC) and metastatic colonic adenocarcinoma of the liver (MCA) is often difficult, particularly in needle biopsy and fine-needle aspiration specimens, if histologic features alone are used. To examine the differences in the expressions of the cytokeratin (CK) 7 and 20 in the CCs and MCAs, we performed immunohistochemical studies on surgically resected 19 CCs and 23 MCAs. We used monoclonal antibodies against CK 7 and CK 20, and applied microwave antigen retrieval technique on formalin-fixed, paraffin-embedded tissue. We interpreted diffuse cytoplasmic reactivity found in > or =5% of tumor cells as positive. CCs showed CK 7+/CK 20- immunophenotype in 63%, CK 7+/CK 20+ in 32%, CK 7-/CK 20+ in 5%, and CK 7-/CK 20- in 0%. MCAs exhibited CK 7-/CK 20+ immunophenotype in 87%, CK 7+/CK 20+ in 9%, CK 7-/CK 20- in 4%, and CK 7+/CK 20- in 0%. CK 20-reactive cells in CCs were frequently columnar in shape (p<0.05). In conclusion, the CK 7/CK 20 immunophenotype was useful in the differentiation of CCs from MCAs: the CK 7+/CK 20- immunophenotype strongly suggested CCs, whereas the CK 7-/CK 20+ immunophenotype strongly suggested MCAs.

 E-submission
E-submission

 First
First Prev
Prev



