Search
- Page Path
- HOME > Search
Correspondence
- Erratum: Breast fine-needle aspiration cytology in the era of core-needle biopsy: what is its role?
- Ahrong Kim, Hyun Jung Lee, Jee Yeon Kim
- J Pathol Transl Med. 2025;59(2):147-147. Published online March 14, 2025
- DOI: https://doi.org/10.4132/jptm.2024.11.01.r
- Corrects: J Pathol Transl Med 2025;59(1):26
- 1,550 View
- 53 Download
Review
- Breast fine-needle aspiration cytology in the era of core-needle biopsy: what is its role?
- Ahrong Kim, Hyun Jung Lee, Jee Yeon Kim
- J Pathol Transl Med. 2025;59(1):26-38. Published online January 15, 2025
- DOI: https://doi.org/10.4132/jptm.2024.11.01
- Correction in: J Pathol Transl Med 2025;59(2):147
- 12,221 View
- 428 Download
- 3 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
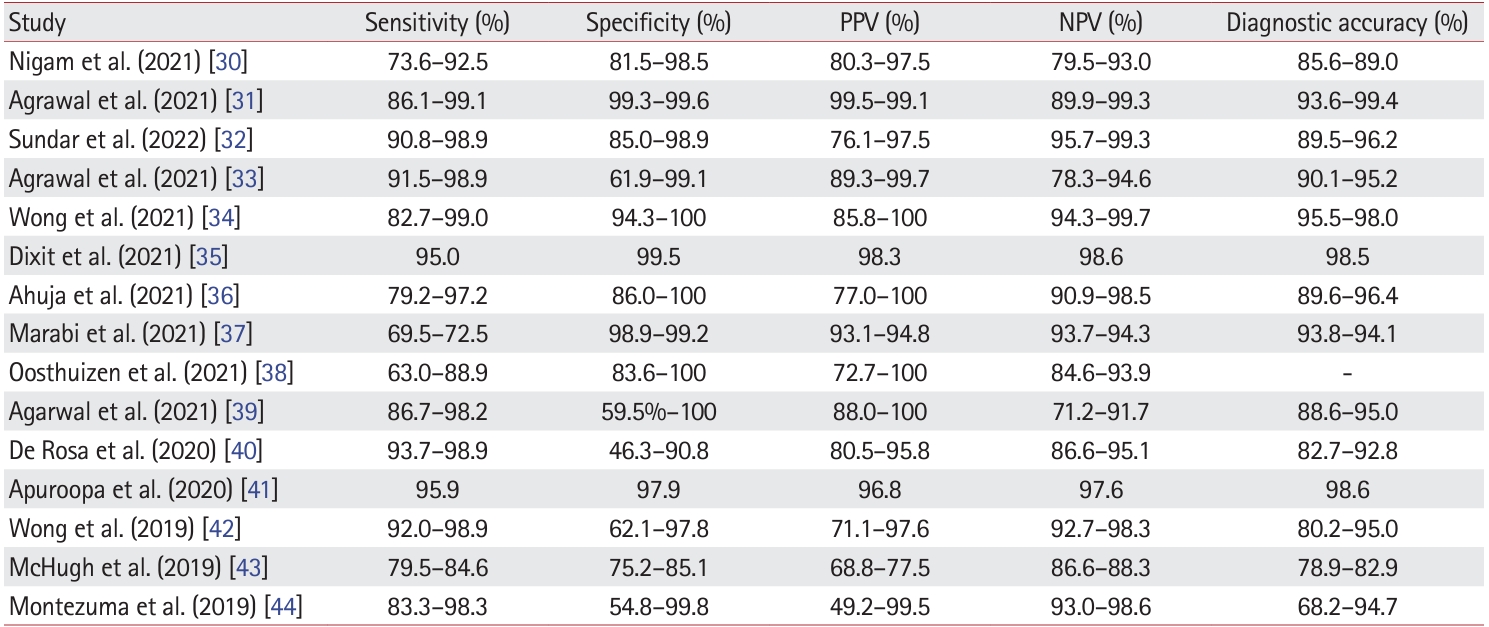
PDF - Fine-needle aspiration cytology (FNAC) has long been recognized as a minimally invasive, cost-effective, and reliable diagnostic tool for breast lesions. However, with the advent of core-needle biopsy (CNB), the role of FNAC has diminished in some clinical settings. This review aims to re-evaluate the diagnostic value of FNAC in the current era, focusing on its complementary use alongside CNB, the adoption of new approaches such as the International Academy of Cytology Yokohama System, and the implementation of rapid on-site evaluation to reduce inadequate sample rates. Advances in liquid-based cytology, receptor expression testing, molecular diagnostics, and artificial intelligence are discussed, highlighting their potential to enhance the diagnostic accuracy of FNAC. Despite challenges, FNAC remains a valuable diagnostic method, particularly in low-resource settings and specific clinical scenarios, and its role continues to evolve with technology.
-
Citations
Citations to this article as recorded by- Bulk-lysis protocols as a sensitive method for investigation of circulating CK19 cells in the peripheral blood of patients with breast cancer by flow cytometry
Daniella Serafin Couto Vieira, Laura Otto Walter, Maria Eduarda Cunha da Silva, Lisandra de Oliveira Silva, Heloísa Zorzi Costa, Chandra Chiappin Cardoso, Fernando Carlos de Lander Schmitt, Maria Cláudia Santos-Silva
Analytical Methods.2025; 17(23): 4771. CrossRef
- Bulk-lysis protocols as a sensitive method for investigation of circulating CK19 cells in the peripheral blood of patients with breast cancer by flow cytometry
Original Article
- Comparison of tissue-based and plasma-based testing for EGFR mutation in non–small cell lung cancer patients
- Yoon Kyung Kang, Dong Hoon Shin, Joon Young Park, Chung Su Hwang, Hyun Jung Lee, Jung Hee Lee, Jee Yeon Kim, JooYoung Na
- J Pathol Transl Med. 2025;59(1):60-67. Published online January 15, 2025
- DOI: https://doi.org/10.4132/jptm.2024.10.01
- 4,716 View
- 198 Download
-
 Abstract
Abstract
 PDF
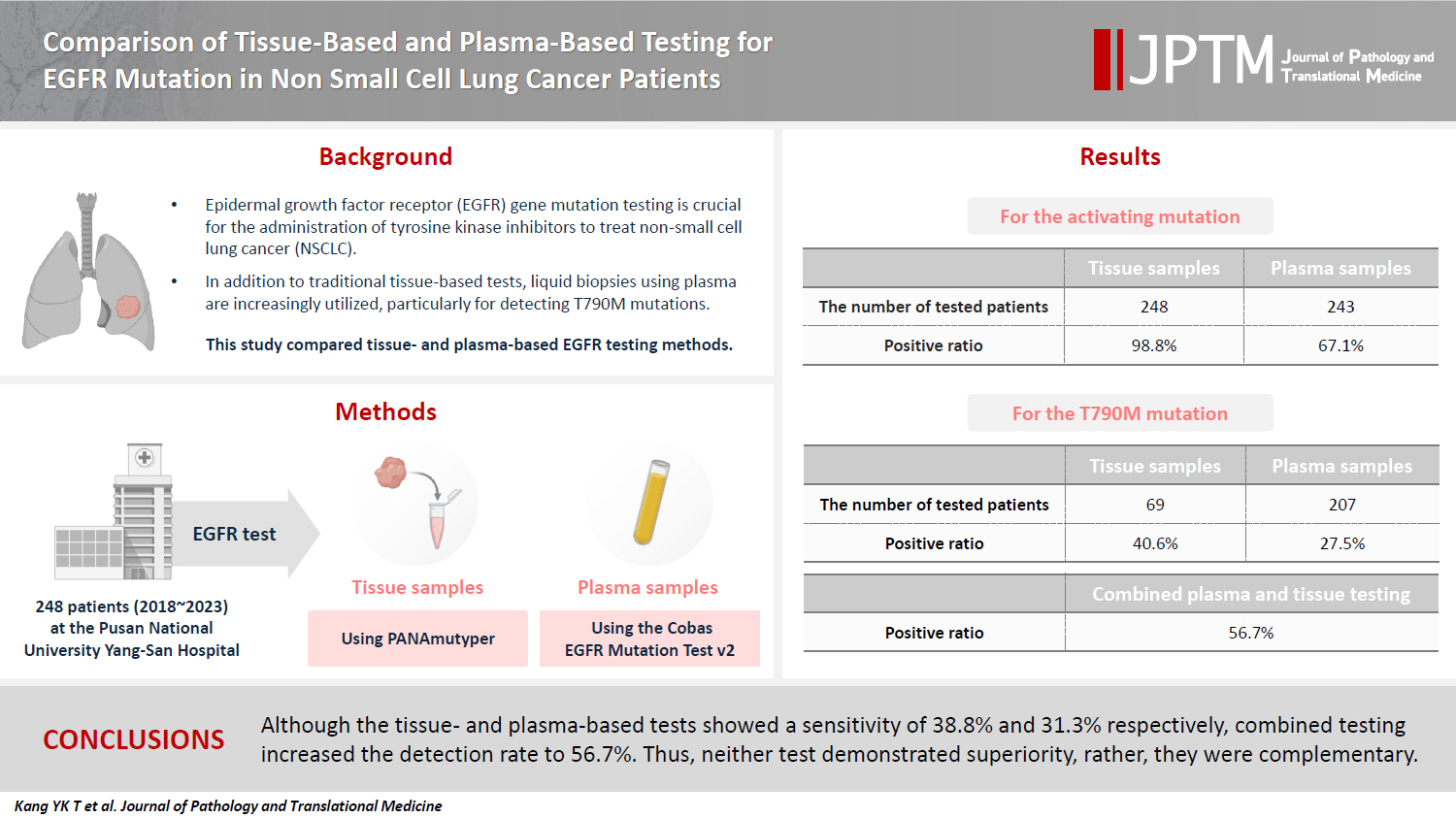
PDF - Background
Epidermal growth factor receptor (EGFR) gene mutation testing is crucial for the administration of tyrosine kinase inhibitors to treat non–small cell lung cancer. In addition to traditional tissue-based tests, liquid biopsies using plasma are increasingly utilized, particularly for detecting T790M mutations. This study compared tissue- and plasma-based EGFR testing methods.
Methods
A total of 248 patients were tested for EGFR mutations using tissue and plasma samples from 2018 to 2023 at Pusan National University Yangsan Hospital. Tissue tests were performed using PANAmutyper, and plasma tests were performed using the Cobas EGFR Mutation Test v2.
Results
All 248 patients underwent tissue-based EGFR testing, and 245 (98.8%) showed positive results. Of the 408 plasma tests, 237 (58.1%) were positive. For the T790M mutation, tissue biopsies were performed 87 times in 69 patients, and 30 positive cases (38.6%) were detected. Plasma testing for the T790M mutation was conducted 333 times in 207 patients, yielding 62 positive results (18.6%). Of these, 57 (27.5%) were confirmed to have the mutation via plasma testing. Combined tissue and plasma tests for the T790M mutation were positive in nine patients (13.4%), while 17 (25.4%) were positive in tissue only and 12 (17.9%) in plasma only. This mutation was not detected in 28 patients (43.3%).
Conclusions
Although the tissue- and plasma-based tests showed a sensitivity of 37.3% and 32.8%, respectively, combined testing increased the detection rate to 56.7%. Thus, neither test demonstrated superiority, rather, they were complementary.
Case Study
- Primary testicular carcinoid tumor with marked lymphovascular invasion
- Hyun Jung Lee, Joon Young Park, So Young Kim, Chung Su Hwang, Jung Hee Lee, Dong Hoon Shin, Jee Yeon Kim
- J Pathol Transl Med. 2021;55(6):410-414. Published online October 20, 2021
- DOI: https://doi.org/10.4132/jptm.2021.09.11
- 4,943 View
- 121 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
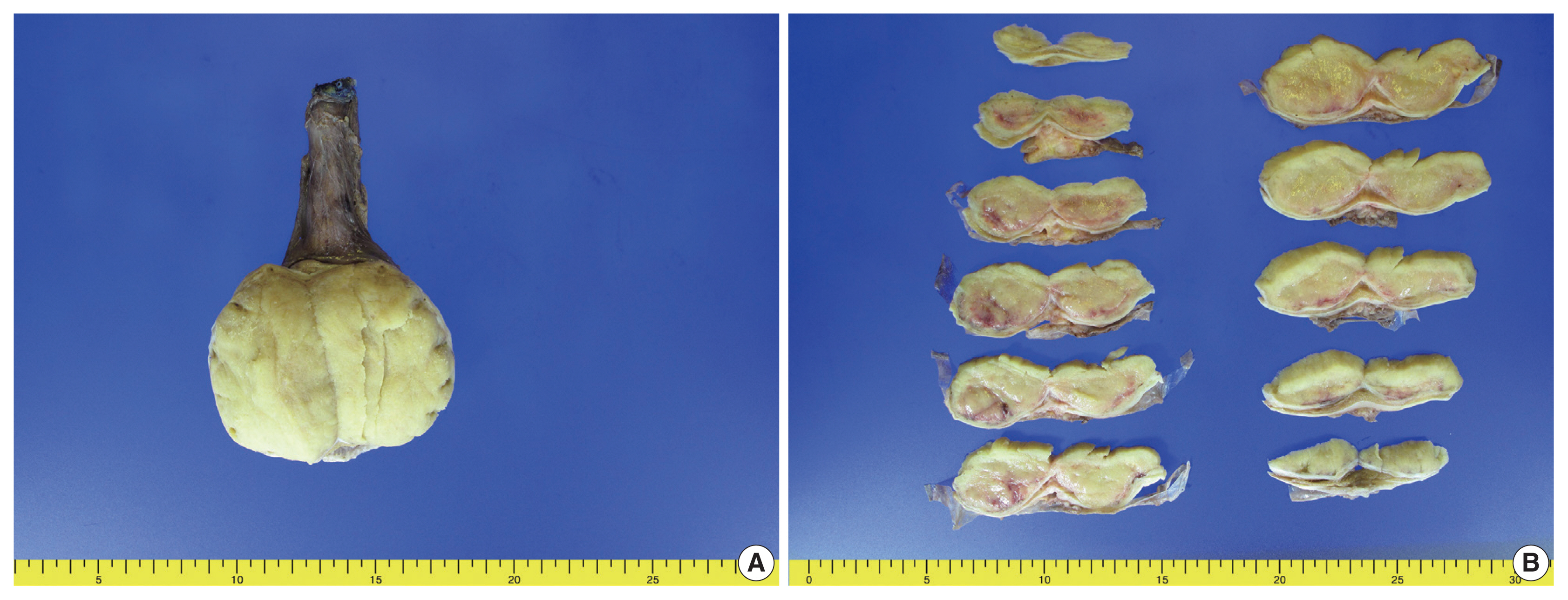
PDF - Testicular carcinoid tumors are very rare, accounting for less than 1% of all testicular tumors. We report a rare case of a testicular carcinoid tumor with extensive lymphatic invasion. A 42-year-old man presented with a painless, enlarged right testicular mass. There was no history of injury or discomfort in this region. Right radical orchiectomy was performed, which showed a well-defined, non-encapsulated solid white mass with calcification (7.0 × 4.5 × 3.5 cm) and absence of cystic components. Microscopic examination using hematoxylin and eosin staining of the tumor sections identified organoid, trabecular, and solid patterns with rosette formation. Extensive multifocal lymphatic invasion was observed. Immunohistochemistry was positive for synaptophysin, chromogranin, and CD56. Testicular carcinoid tumors usually show good prognoses; however, there was extensive lymphovascular invasion in this case. Thus, in the case of unusual presentation of the disease, close follow-up is necessary.
-
Citations
Citations to this article as recorded by- Testicular Primary Well-Differentiated Neuroendocrine Tumor: Clinicopathologic, Immunohistochemical, and Molecular Characterization of Two Patients
Liwei Jia, Bo Zhang, Daniel Shen, Prasad R. Koduru
International Journal of Surgical Pathology.2024; 32(8): 1574. CrossRef
- Testicular Primary Well-Differentiated Neuroendocrine Tumor: Clinicopathologic, Immunohistochemical, and Molecular Characterization of Two Patients
Case Reports
- Lymphocytic Phlebitis of the Stomach: A Case Report with Literature Review.
- Meeran Kim, Hyun Jung Lee, Min Kyung Yeo, Young Suk Lee, Hee Seok Moon, Sang Il Lee, June Sik Cho, Kyu Sang Song
- Korean J Pathol. 2011;45(6):654-658.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.6.654
- 3,891 View
- 23 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Lymphocytic phlebitis of gastrointestinal (GI) tract is a rare diseaes. Approximately 50 cases of lymphocytic phlebitis of the GI tract have been reported. Most of these involved the colon or small intestine and presented as acute abdomen. We report the second case of lymphocytic phlebitis of the stomach. A 73-year-old female complaining of dizziness had endoscopic and computed tomography findings strongly suggested gastric cancer, while gastric biopsy was negative for carcinoma. The partial gastrectomy specimen showed lymphocytic phlebitis involving veins in the submucosa, muscularis propria, and serosa while the adjacent arteries were spared. The veins were mainly surrounded by lymphocytes. When a patient has a lesion in the GI tract that is suggesting cancer without biopsies revealing any carcinoma, the pathologist should recommend a deeper biopsy for a proper examination of the submucosa.
-
Citations
Citations to this article as recorded by- A case report of gastric lymphocytic phlebitis, a rare mimic for malignancy
Daniel L. Chan, Praveen Ravindran, Dorothy Chua, Jason D. Smith, King S. Wong, Michael A. Ghusn
International Journal of Surgery Case Reports.2017; 41: 269. CrossRef
- A case report of gastric lymphocytic phlebitis, a rare mimic for malignancy
- Sclerosing Angiomatoid Nodular Transformation (SANT) in Spleen: A Case Report.
- Hyun Jung Lee, Song Yi Choi, Song Mei Huang, Ji Young Sul, Jin Man Kim
- Korean J Pathol. 2011;45(1):111-114.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.1.111
- 5,206 View
- 56 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Sclerosing angiomatoid nodular transformation (SANT) of spleen is a rare inflammatory tumor-like vascular lesion composed of angiomatoid nodules in a fibrosclerotic background. We report herein on a case of SANT in the spleen with its pathologic features, and review the related literature. A 50-year-old woman presented with mild left upper quadrant discomfort and tenderness and she showed a 6 cm-sized solitary splenic mass on computed tomography. She underwent laparoscopic splenectomy. Grossly, the spleen showed a well circumscribed round-shaped solid mass with multinodular hemorrhagic surfaces. Microscopically, the mass consisted of multiple angiomatoid nodules surrounded by collagen bundles with fibroblasts and a lymphoplasma cell infiltration. Immunohistochemically, the cells of the angiomatoid nodules were positive for CD31, CD30, CD34, alpha-smooth muscle actin, and VWF-VIII, but they were negative for CD8, anaplastic lymphoma kinase protein, and D2-40. The patient has been under close follow-up without recurrence.
-
Citations
Citations to this article as recorded by- Sclerosing angiomatoid nodular transformation of the spleen presenting rapid growth after adrenalectomy: Report of a case
Yasuo Nagai, Daisuke Satoh, Hiroyoshi Matsukawa, Shigehiro Shiozaki
International Journal of Surgery Case Reports.2017; 30: 108. CrossRef - A Case of Sclerosing Angiomatoid Nodular Transformation of the Spleen: Spoke Wheel Pattern on Computed Tomography
Joo Han Park, Sun Hyuk Hwang, Ki Chan Kim, Si Yeon Kim, Ga Won Song, Jae Ho Han, Joon Seong Park
Korean Journal of Medicine.2014; 86(3): 357. CrossRef - Differentiation of an Unclear Splenic Lesion in a Patient With Cholangiocarcinoma
Constantin Lapa, Ulrich Steger, Christian O. Ritter, Vanessa Wild, Ken Herrmann
Clinical Nuclear Medicine.2014; 39(5): 470. CrossRef - Sclerosing Angiomatoid Nodular Transformation of the Spleen: CT and MRI Features With Pathologic Correlation
Rachel B. Lewis, Grant E. Lattin, Meenakshi Nandedkar, Nadine S. Aguilera
American Journal of Roentgenology.2013; 200(4): W353. CrossRef
- Sclerosing angiomatoid nodular transformation of the spleen presenting rapid growth after adrenalectomy: Report of a case

 E-submission
E-submission

 First
First Prev
Prev



