Search
- Page Path
- HOME > Search
Original Articles
- Prevalence of HER2-ultralow breast cancer in South Korea: a multicenter study by reassessment of HER2-zero cases
- Min Chong Kim, Eun Yoon Cho, Hee Jin Lee, Ji Shin Lee, Jee Yeon Kim, Wan Seop Kim, Chungyeul Kim, Sun-Young Jun, Hye Jeong Choi, So Mang Lee, Ahrong Kim, Ji-Young Kim, Jeong Yun Shim, Gyungyub Gong, Young Kyung Bae
- Received September 17, 2025 Accepted October 21, 2025 Published online February 23, 2026
- DOI: https://doi.org/10.4132/jptm.2025.10.22 [Epub ahead of print]
- 42 View
- 2 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
This study aimed to determine the prevalence of human epidermal growth factor receptor 2 (HER2)–ultralow breast cancer among cases initially classified as HER2 immunohistochemistry (IHC) 0 and assess interobserver variability in interpreting low-level HER2 expression. Methods: In this multicenter retrospective study, all invasive breast cancer cases diagnosed between January and December 2022 across 10 Korean institutions were retrieved. Institutional pathologists reexamined HER2 IHC slides originally reported as IHC 0 according to the 2018 American Society of Clinical Oncology/College of American Pathologists guidelines and reclassified them as HER2-null (0), HER2-ultralow (0+), or HER2-low (1+). Slides from 10% of HER2-null and HER2-ultralow cases were digitized for central review and independently assessed by two pathologists, with discrepancies resolved by consensus. Results: Among 8,026 cases, 2,836 cases (35.5%) were initially reported as IHC 0. Upon re-review, 1,673 (59.0%), 1,139 (40.2%), and 24 (0.8%) cases were reclassified as HER2-null, HER2-ultralow, and HER2-low, respectively. The prevalence of HER2-ultralow breast cancer varied considerably across institutions (23.7%–78.1%). Central review of 268 digitized cases showed concordance in 193 cases (72.0%). Among the 75 discordant cases, 54 tumors (72.0%) were upgraded from HER2-null to HER2-ultralow, and 18 (24.0%) tumors were upgraded from HER2-ultralow to HER2-low. Furthermore, two tumors (2.7%) were downgraded from HER2-ultralow to HER2-null. Conclusions: Approximately 40% of cases initially categorized as IHC 0 were reclassified as HER2-ultralow. The substantial inter-institutional variability observed in interpreting low-level HER2 expression highlights the need for standardized training and quality assurance to ensure accurate identification of patients eligible for HER2-targeted antibody–drug conjugates.
- A multicenter study of interobserver variability in pathologic diagnosis of papillary breast lesions on core needle biopsy with WHO classification
- Hye Ju Kang, Sun Young Kwon, Ahrong Kim, Woo Gyeong Kim, Eun Kyung Kim, Ae Ree Kim, Chungyeul Kim, Soo Kee Min, So Young Park, Sun Hee Sung, Hye Kyoung Yoon, Ahwon Lee, Ji Shin Lee, Hyang Im Lee, Ho Chang Lee, Sung Chul Lim, Sun Young Jun, Min Jung Jung, Chang Won Jung, Soo Youn Cho, Eun Yoon Cho, Hye Jeong Choi, So Yeon Park, Jee Yeon Kim, In Ae Park, Youngmee Kwon
- J Pathol Transl Med. 2021;55(6):380-387. Published online October 6, 2021
- DOI: https://doi.org/10.4132/jptm.2021.07.29
- 7,395 View
- 226 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
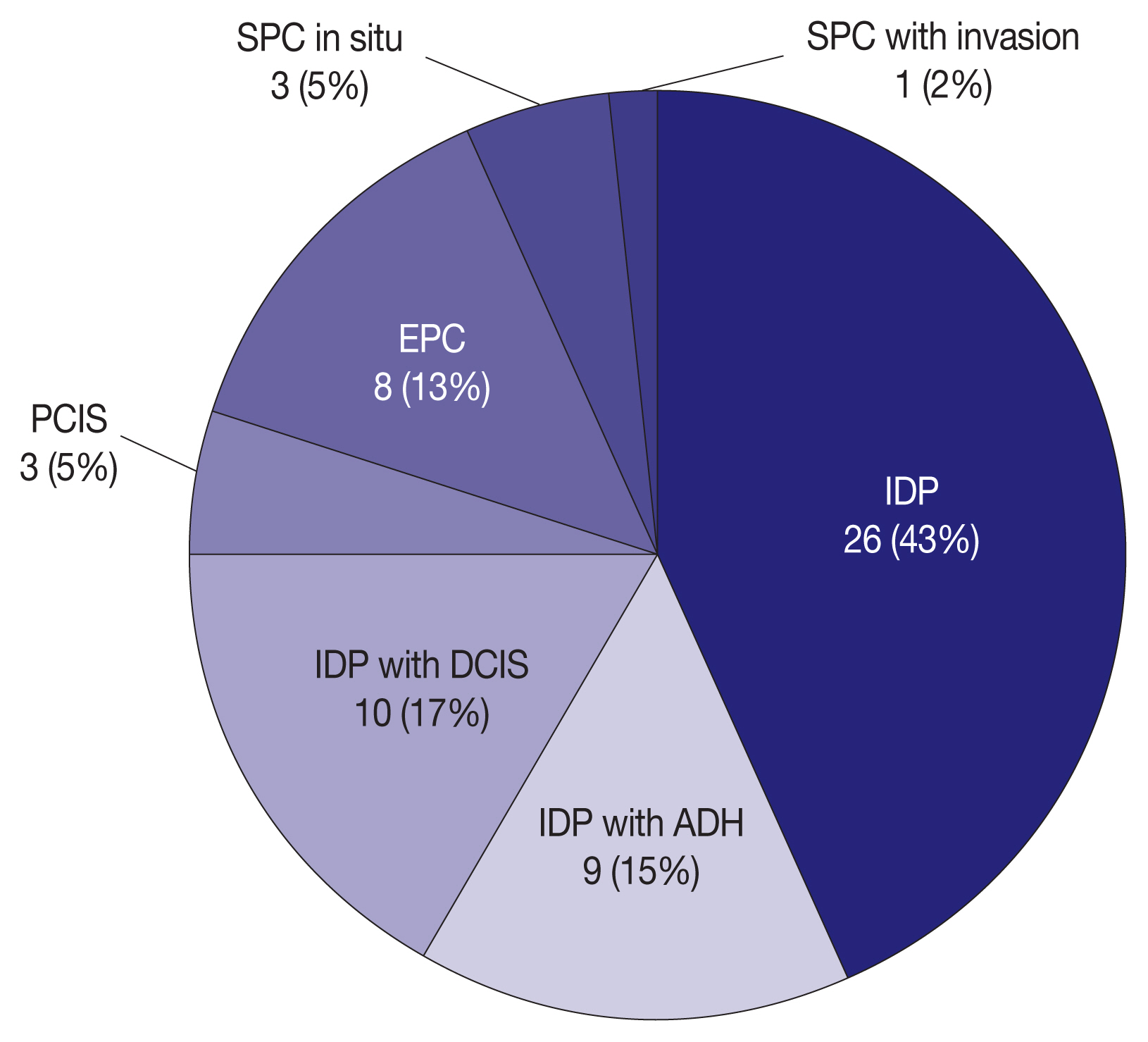
Papillary breast lesions (PBLs) comprise diverse entities from benign and atypical lesions to malignant tumors. Although PBLs are characterized by a papillary growth pattern, it is challenging to achieve high diagnostic accuracy and reproducibility. Thus, we investigated the diagnostic reproducibility of PBLs in core needle biopsy (CNB) specimens with World Health Organization (WHO) classification.
Methods
Diagnostic reproducibility was assessed using interobserver variability (kappa value, κ) and agreement rate in the pathologic diagnosis of 60 PBL cases on CNB among 20 breast pathologists affiliated with 20 medical institutions in Korea. This analysis was performed using hematoxylin and eosin (H&E) staining and immunohistochemical (IHC) staining for cytokeratin 5 (CK5) and p63. The pathologic diagnosis of PBLs was based on WHO classification, which was used to establish simple classifications (4-tier, 3-tier, and 2-tier).
Results
On WHO classification, H&E staining exhibited ‘fair agreement’ (κ = 0.21) with a 47.0% agreement rate. Simple classifications presented improvement in interobserver variability and agreement rate. IHC staining increased the kappa value and agreement rate in all the classifications. Despite IHC staining, the encapsulated/solid papillary carcinoma (EPC/SPC) subgroup (κ = 0.16) exhibited lower agreement compared to the non-EPC/SPC subgroup (κ = 0.35) with WHO classification, which was similar to the results of any other classification systems.
Conclusions
Although the use of IHC staining for CK5 and p63 increased the diagnostic agreement of PBLs in CNB specimens, WHO classification exhibited a higher discordance rate compared to any other classifications. Therefore, this result warrants further intensive consensus studies to improve the diagnostic reproducibility of PBLs with WHO classification. -
Citations
Citations to this article as recorded by- Beyond the benign: A rare case report of myxoid pleomorphic liposarcoma
Arslan Ahmad, Muhammad Ammar, Muhammad Hasnain Saleem Choudary, Muhammad Nouman Sadiq, Rana Uzair Ahmad, Nouman Aziz
Radiology Case Reports.2025; 20(5): 2500. CrossRef - Invasive papillary carcinoma of the breast
Shijing Wang, Qingfu Zhang, Xiaoyun Mao
Frontiers in Oncology.2024;[Epub] CrossRef - Recommendations for Performance Evaluation of Machine Learning in Pathology: A Concept Paper From the College of American Pathologists
Matthew G. Hanna, Niels H. Olson, Mark Zarella, Rajesh C. Dash, Markus D. Herrmann, Larissa V. Furtado, Michelle N. Stram, Patricia M. Raciti, Lewis Hassell, Alex Mays, Liron Pantanowitz, Joseph S. Sirintrapun, Savitri Krishnamurthy, Anil Parwani, Giovann
Archives of Pathology & Laboratory Medicine.2024; 148(10): e335. CrossRef - Encapsulated papillary carcinoma of the breast: A single institution experience
Liang Xu, Qixin Mao, Qiuming Liu, Yufeng Gao, Lihua Luo, Chungen Guo, Wei Qu, Ningning Yan, Yali Cao
Oncology Letters.2023;[Epub] CrossRef - High-risk and selected benign breast lesions diagnosed on core needle biopsy: Evidence for and against immediate surgical excision
Aparna Harbhajanka, Hannah L. Gilmore, Benjamin C. Calhoun
Modern Pathology.2022; 35(11): 1500. CrossRef
- Beyond the benign: A rare case report of myxoid pleomorphic liposarcoma
Case Study
- Primary hepatic extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue
- Soyeon Choi, Ji Hye Kim, Kyungbin Kim, Misung Kim, Hye Jeong Choi, Young Min Kim, Jae Hee Suh, Min Jung Seo, Hee Jeong Cha
- J Pathol Transl Med. 2020;54(4):340-345. Published online April 15, 2020
- DOI: https://doi.org/10.4132/jptm.2020.03.18
- 8,033 View
- 135 Download
- 14 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
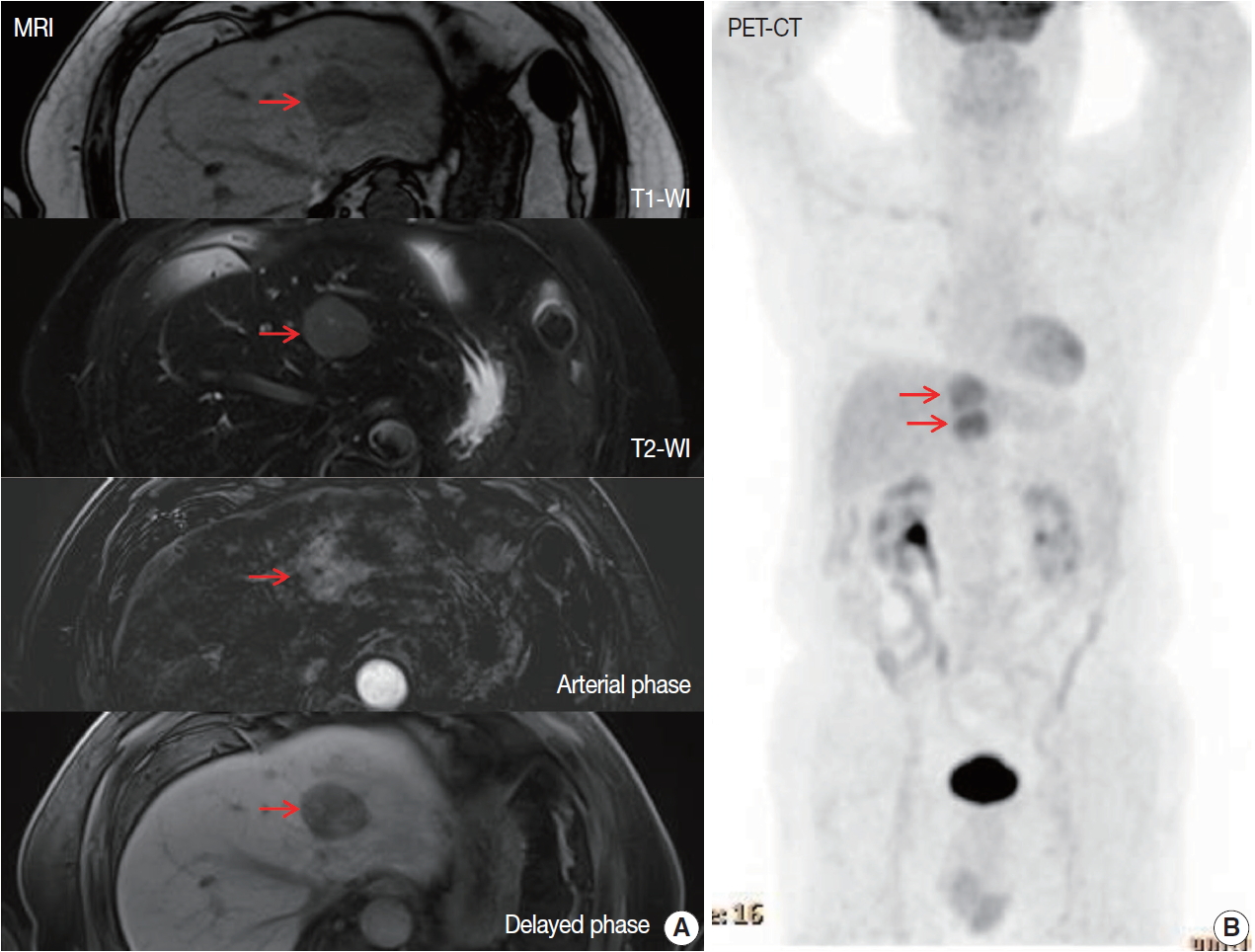
PDF - Extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma), is one of the specific type of low-grade B-cell lymphoma not infrequently found worldwide. It typically involves mucosal sites such as stomach and conjunctiva; however, primary hepatic MALT lymphoma has been extremely rarely reported. We describe a case of hepatic MALT lymphoma in a 70-year-old male patient who underwent left hepatectomy due to the incidentally detected liver masses at a medical checkup. The resected specimen revealed multinodular masses consisting of small-to-intermediate-sized lymphoid cells with serpentine pattern and focal lymphoepithelial lesions. The tumor cells were diffusely positive for CD20 and Bcl-2 but negative for CD3, CD10, CD5, CD23, CD43, and cyclinD1. The Ki-67 labeling index was 10% and immunoglobulin heavy chain gene rearrangement study confirmed monoclonal proliferation. In this paper, we discuss several unique clinicopathologic characteristics which will be helpful to the differential diagnosis of hepatic MALT lymphoma.
-
Citations
Citations to this article as recorded by- Oral administration of Limosilactobacillus reuteri VHProbi® M07 alleviates ovalbumin-induced allergic asthma in mice
Guoqing Meng, Hongchang Cui, Congrui Feng, Chaoqun Guo, Lei Song, Zhi Duan, Misbahuddin Rafeeq
PLOS ONE.2025; 20(1): e0317587. CrossRef - Response‑adapted involved site radiation therapy for hepatic marginal zone B‑cell lymphoma: A case report
Shin-Ting Chen, Yu-Guang Chen, Wen-Yen Huang, Cheng-Hsiang Lo
Oncology Letters.2025;[Epub] CrossRef - Management approaches for primary hepatic lymphoma: 10 year institutional experience with comprehensive literature review
Jennifer Ma, Remy Daou, Josiane Bou Eid, Beatrice Fregonese, Joe El-Khoury, N. Ari Wijetunga, Brandon S. Imber, Joachim Yahalom, Carla Hajj
Frontiers in Oncology.2025;[Epub] CrossRef - Primary Hepatic Mucosa-Associated B-Cell Lymphoma in a Patient with Primary Sclerosing Cholangitis—A Case Ultimately Requiring Liver Transplantation
Jerica Novak, Mihajlo Đokić, Miha Petrič, Diana Vozlič, Milanka Živanović, Branislava Ranković, Blaž Trotovšek
Diagnostics.2025; 15(16): 2082. CrossRef - Primary Hepatic Mucosa-Associated Lymphoid Tissue Lymphoma: A Case Report and Literature Review
Sook Hyun Shin, Jeong-Ju Yoo, Sang Gyune Kim, Young Seok Kim, Susie Chin
Clinical Ultrasound.2025; 10(2): 119. CrossRef - Primary hepatic mucosa-associated lymphoid tissue lymphoma: a case report and literature review
Tao He, Jieyu Zou
Frontiers in Oncology.2024;[Epub] CrossRef - “Speckled Enhancement” on Gd-EOB-DTPA Enhanced MR Imaging of Primary Hepatic Mucosa-associated Lymphoid Tissue Lymphoma
Ryota Hyodo, Yasuo Takehara, Ayumi Nishida, Masaya Matsushima, Shinji Naganawa
Magnetic Resonance in Medical Sciences.2023; 22(3): 273. CrossRef - Primary hepatic extranodal marginal zone B-cell mucosa-associated lymphoid tissue lymphoma treated by laparoscopic partial hepatectomy: a case report
Keisuke Okura, Satoru Seo, Hironori Shimizu, Hiroto Nishino, Tomoaki Yoh, Ken Fukumitsu, Takamichi Ishii, Koichiro Hata, Hironori Haga, Etsuro Hatano
Surgical Case Reports.2023;[Epub] CrossRef - Incidental Findings in Pediatric Patients: How to Manage Liver Incidentaloma in Pediatric Patients
Andrius Cekuolis, Dagmar Schreiber-Dietrich, Rasa Augustinienė, Heike Taut, Judy Squires, Edda L. Chaves, Yi Dong, Christoph F. Dietrich
Cancers.2023; 15(8): 2360. CrossRef - Primary hepatic mucosa‐associated lymphoid tissue lymphoma: Case report and literature review
Wing Yu Lau, Kit‐Man Ho, Fiona Ka‐Man Chan, Shi Lam, Kai‐Chi Cheng
Surgical Practice.2022; 26(1): 56. CrossRef - 18F-FDG Versus 68Ga-FAPI PET/CT in Visualizing Primary Hepatic Extranodal Marginal Zone Lymphoma of Mucosa-Associated Lymphoid Tissue
Yizhen Pang, Long Zhao, Qihang Shang, Tinghua Meng, Haojun Chen
Clinical Nuclear Medicine.2022; 47(4): 375. CrossRef - Primary hepatopancreatobiliary lymphoma: Pathogenesis, diagnosis, and management
Qianwen Wang, Kangze Wu, Xuzhao Zhang, Yang Liu, Zhouyi Sun, Shumei Wei, Bo Zhang
Frontiers in Oncology.2022;[Epub] CrossRef - Positive effect of Bifidobacterium animalis subsp. lactis VHProbi YB11 in improving gastrointestinal movement of mice having constipation
Hongchang Cui, Qian Wang, Congrui Feng, Chaoqun Guo, Jingyan Zhang, Xinping Bu, Zhi Duan
Frontiers in Microbiology.2022;[Epub] CrossRef - A case of primary hepatic extranodal marginal zone B-cell mucosa-associated lymphoid tissue (MALT) lymphoma treated by radiofrequency ablation (RFA), and a literature review
Zhe Xu, Chong Pang, Jidong Sui, Zhenming Gao
Journal of International Medical Research.2021;[Epub] CrossRef
- Oral administration of Limosilactobacillus reuteri VHProbi® M07 alleviates ovalbumin-induced allergic asthma in mice
Original Article
- Programmed death-ligand 1 expression and its correlation with clinicopathological parameters in gallbladder cancer
- Ji Hye Kim, Kyungbin Kim, Misung Kim, Young Min Kim, Jae Hee Suh, Hee Jeong Cha, Hye Jeong Choi
- J Pathol Transl Med. 2020;54(2):154-164. Published online February 10, 2020
- DOI: https://doi.org/10.4132/jptm.2019.11.13
- 9,836 View
- 172 Download
- 16 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
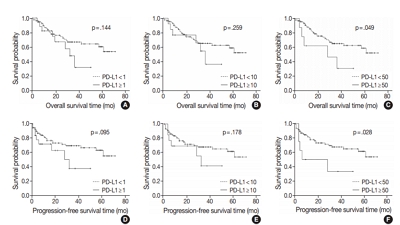
Immunomodulatory therapies targeting the interaction between programmed cell death protein 1 and programmed death-ligand 1 (PD-L1) have become increasingly important in anticancer treatment. Previous research on the subject of this immune response has established an association with tumor aggressiveness and a poor prognosis in certain cancers. Currently, scant information is available on the relationship between PD-L1 expression and gallbladder cancer (GBC).
Methods
We investigated the expression of PD-L1 in 101 primary GBC cases to determine the potential association with prognostic impact. PD-L1 expression was immunohistochemically assessed using a single PD-L1 antibody (clone SP263). Correlations with clinicopathological parameters, overall survival (OS), or progression- free survival (PFS) were analyzed.
Results
PD-L1 expression in tumor cells at cutoff levels of 1%, 10%, and 50% was present in 18.8%, 13.8%, and 7.9% of cases. Our study showed that positive PD-L1 expression at any cutoff was significantly correlated with poorly differentiated histologic grade and the presence of lymphovascular invasion (p < .05). PD-L1 expression at cutoff levels of 10% and 50% was significantly positive in patients with perineural invasion, higher T categories, and higher pathologic stages (p < .05). Additionally, there was a significant association noted between PD-L1 expression at a cutoff level of 50% and worse OS or PFS (p = .049 for OS, p = .028 for PFS). Other poor prognostic factors included histologic grade, T category, N category, pathologic stage, lymphovascular invasion, perineural invasion, growth pattern, and margin of resection (p < .05).
Conclusions
The expression of PD-L1 in GBC varies according to cutoff level but is valuably associated with poor prognostic parameters and survival. Our study indicates that the overexpression of PD-L1 in GBC had a negative prognostic impact. -
Citations
Citations to this article as recorded by- PD-L1 Expression in Biliary Tract Cancer: Comparison Across Antibody Clones and Role as a Predictor of Response to Chemoimmunotherapy: A Meta-Analysis
Juan J. Juarez-Vignon Whaley, Soravis Osataphan, Ben Ponvilawan, Nipith Charoenngam, Mary Linton Peters
JCO Precision Oncology.2025;[Epub] CrossRef - An MRI-based model for preoperative prediction of tertiary lymphoid structures in patients with gallbladder cancer
Ying Xu, Zhuo Li, Weihua Zhi, Yi Yang, Jingzhong Ouyang, Yanzhao Zhou, Zeliang Ma, Sicong Wang, Lizhi Xie, Jianming Ying, Jinxue Zhou, Xinming Zhao, Feng Ye
Insights into Imaging.2025;[Epub] CrossRef - Lacking Immunotherapy Biomarkers for Biliary Tract Cancer: A Comprehensive Systematic Literature Review and Meta-Analysis
Giorgio Frega, Fernando P. Cossio, Jesus M. Banales, Vincenzo Cardinale, Rocio I. R. Macias, Chiara Braconi, Angela Lamarca
Cells.2023; 12(16): 2098. CrossRef - Gallbladder carcinomas: review and updates on morphology, immunohistochemistry, and staging
Whayoung Lee, Vishal S. Chandan
Human Pathology.2023; 132: 149. CrossRef - Prognostic Relevance of PDL1 and CA19-9 Expression in Gallbladder Cancer vs. Inflammatory Lesions
Neetu Rawal, Supriya Awasthi, Nihar Ranjan Dash, Sunil Kumar, Prasenjit Das, Amar Ranjan, Anita Chopra, Maroof Ahmad Khan, Sundeep Saluja, Showket Hussain, Pranay Tanwar
Current Oncology.2023; 30(2): 1571. CrossRef - Identification of genes associated with gall bladder cell carcinogenesis: Implications in targeted therapy of gall bladder cancer
Ishita Ghosh, Ruma Dey Ghosh, Soma Mukhopadhyay
World Journal of Gastrointestinal Oncology.2023; 15(12): 2053. CrossRef - CD73 and PD-L1 as Potential Therapeutic Targets in Gallbladder Cancer
Lu Cao, Kim R. Bridle, Ritu Shrestha, Prashanth Prithviraj, Darrell H. G. Crawford, Aparna Jayachandran
International Journal of Molecular Sciences.2022; 23(3): 1565. CrossRef - Evolving Role of Immunotherapy in Advanced Biliary Tract Cancers
Sandra Kang, Bassel F. El-Rayes, Mehmet Akce
Cancers.2022; 14(7): 1748. CrossRef - Novel immune scoring dynamic nomograms based on B7-H3, B7-H4, and HHLA2: Potential prediction in survival and immunotherapeutic efficacy for gallbladder cancer
Chao Lv, Shukun Han, Baokang Wu, Zhiyun Liang, Yang Li, Yizhou Zhang, Qi Lang, Chongli Zhong, Lei Fu, Yang Yu, Feng Xu, Yu Tian
Frontiers in Immunology.2022;[Epub] CrossRef - PD-1 inhibitors plus nab-paclitaxel-containing chemotherapy for advanced gallbladder cancer in a second-line setting: A retrospective analysis of a case series
Sirui Tan, Jing Yu, Qiyue Huang, Nan Zhou, Hongfeng Gou
Frontiers in Oncology.2022;[Epub] CrossRef - Expression of HER2 and Mismatch Repair Proteins in Surgically Resected Gallbladder Adenocarcinoma
You-Na Sung, Sung Joo Kim, Sun-Young Jun, Changhoon Yoo, Kyu-Pyo Kim, Jae Hoon Lee, Dae Wook Hwang, Shin Hwang, Sang Soo Lee, Seung-Mo Hong
Frontiers in Oncology.2021;[Epub] CrossRef - Programmed Death Ligand-1 (PD-L1) Is an Independent Negative Prognosticator in Western-World Gallbladder Cancer
Thomas Albrecht, Fritz Brinkmann, Michael Albrecht, Anke S. Lonsdorf, Arianeb Mehrabi, Katrin Hoffmann, Yakup Kulu, Alphonse Charbel, Monika N. Vogel, Christian Rupp, Bruno Köhler, Christoph Springfeld, Peter Schirmacher, Stephanie Roessler, Benjamin Goep
Cancers.2021; 13(7): 1682. CrossRef - Immune Microenvironment in Gallbladder Adenocarcinomas
Pallavi A. Patil, Kara Lombardo, Weibiao Cao
Applied Immunohistochemistry & Molecular Morphology.2021; 29(8): 557. CrossRef - Molecular Targets and Emerging Therapies for Advanced Gallbladder Cancer
Matteo Canale, Manlio Monti, Ilario Giovanni Rapposelli, Paola Ulivi, Francesco Giulio Sullo, Giulia Bartolini, Elisa Tiberi, Giovanni Luca Frassineti
Cancers.2021; 13(22): 5671. CrossRef - Overview of current targeted therapy in gallbladder cancer
Xiaoling Song, Yunping Hu, Yongsheng Li, Rong Shao, Fatao Liu, Yingbin Liu
Signal Transduction and Targeted Therapy.2020;[Epub] CrossRef
- PD-L1 Expression in Biliary Tract Cancer: Comparison Across Antibody Clones and Role as a Predictor of Response to Chemoimmunotherapy: A Meta-Analysis
Letter to the Editor
- Perineural Involvement in Benign Mixed Tumor
- Se Jin Jung, Jong Cheol Lee, Hye Jeong Choi, Hee Jeong Cha, Young Min Kim, Young Wha Koh, Jae Hee Suh
- Korean J Pathol. 2013;47(5):403-404. Published online October 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.5.403
- 7,296 View
- 55 Download
- 3 Crossref
-
 PDF
PDF -
Citations
Citations to this article as recorded by- Sclerosing Odontogenic Carcinoma: A Review of a Challenging Entity in Malignant Odontogenic Classification With a Focus on Perineural Invasion and Cellular Proliferation
Merva Soluk‐Tekkesin, Keith David Hunter, Ronell Bologna‐Molina, Kelly Magliocca, Liam Robinson, Akinyele Olumuyiwa Adisa, Jiang Li, Elizabeth Ann Bilodeau, Haizal Mohd Hussaini, Madhu Shrestha, Ricardo Santiago Gomez, Willie van Heerden, Wanninayake Mudi
Journal of Oral Pathology & Medicine.2026;[Epub] CrossRef - Benign Pleomorphic Adenoma in the Facial Nerve
Gemma E. Hogg, Richard A. Steven, Patrick M. Spielmann
Ear, Nose & Throat Journal.2020; 99(6): 361. CrossRef - Benign pleomorphic adenoma of minor salivary gland showing perineural invasion: a rare entity
Rahul Jayaram, Dipen Patel, Vijay Santhanam
British Journal of Oral and Maxillofacial Surgery.2015; 53(1): 81. CrossRef
- Sclerosing Odontogenic Carcinoma: A Review of a Challenging Entity in Malignant Odontogenic Classification With a Focus on Perineural Invasion and Cellular Proliferation
Case Reports
- Acute Appendicitis Associated with Aspergillosis in a Leukemia Patient: A Case Report.
- Bong Hee Park, Jae Hee Suh, Hye Jeong Choi, Hee Jeong Cha, Chang Woo Nam, Young Min Kim
- Korean J Pathol. 2010;44(3):330-332.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.3.330
- 4,279 View
- 34 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - Herein we describe a rare case of acute appendicitis associated with localized aspergillosis in an 8-year-old boy with acute lymphoblastic leukemia. During chemotherapy, the patient complained of mild abdominal pain in the peri-umbilical area and displayed an increased C-reactive protein level. Abdominal ultrasonography disclosed appendicitis and consequently an appendectomy was done. Histologically, acute appendicitis and Aspergillus hyphae were identified in the lumen and necrotic mucosa. However, there was no evidence of systemic aspergillosis. While aspergillosis is a common fungal infection in immunocompromised patients treated with chemotherapy, acute appendicitis associated with localized aspergillosis without systemic infection is a very rare occurrence.
-
Citations
Citations to this article as recorded by- A scoping review on acute gastrointestinal surgical complications in immunocompromised pediatric patients
Tarek Bou Dargham, Mohamad Bahij Moumneh, Christine Atallah, Ahmad Zaghal
Annals of Pediatric Surgery.2022;[Epub] CrossRef - Acute isolated Aspergillus appendicitis in pediatric leukemia
Yutaro Yada, Yuhki Koga, Hiroaki Ono, Yoshitomo Motomura, Genshiro Esumi, Kenichi Kohashi, Yasunori Muraosa, Katsuhiko Kamei, Toshiharu Matsuura, Yoshinao Oda, Shouichi Ohga
Journal of Infection and Chemotherapy.2020; 26(11): 1229. CrossRef - Isolated Acute Appendicitis Caused by Aspergillu s in a Patient Who Underwent Lung Transplantation: A Case Report
H.S. Kim, H.J. Yeo, D.H. Shin, W.H. Cho, D. Kim
Transplantation Proceedings.2018; 50(4): 1199. CrossRef - Fungal Appendicitis in Immunocompromised Children. Indications and Contraindications for Laparoscopic Appendectomy: A Report on 2 Successful Cases
Veronica Carlini, Valeria Calcaterra, Nunzia Decembrino, Laura Rubert, Noemi Pasqua, Mattia Novario, Marco Lucioni, Marco Brunero, Gloria Pelizzo
Journal of Pediatric Hematology/Oncology.2016; 38(7): 581. CrossRef - Characteristic clinical features ofAspergillusappendicitis: Case report and literature review
Mihajlo Gjeorgjievski
World Journal of Gastroenterology.2015; 21(44): 12713. CrossRef
- A scoping review on acute gastrointestinal surgical complications in immunocompromised pediatric patients
- Intraductal Papillary Mucinous Tumor Simultaneously Involving the Liver and Pancreas: A Case Report.
- Bong Hee Park, Jae Hee Suh, Hee Jeong Cha, Young Min Kim, Hye Jeong Choi
- Korean J Pathol. 2010;44(1):83-86.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.1.83
- 4,248 View
- 31 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - We describe here a 67-year-old man who was diagnosed with a rare case of intraductal papillary mucinous tumors that occurred simultaneously in the liver and pancreas. Abdominal computed tomography showed a tubular and cystic dilatation of the pancreatic duct in the pancreas tail, which suggested an intraductal papillary mucinous tumor (IPMT), and multiple intrahepatic duct stones. The patient underwent a distal pancreatectomy with splenectomy and a lateral segmentectomy of the liver. Microscopic examination showed an intraductal papillary mucinous neoplasms of borderline malignancy in the pancreas and a non-invasive intraductal papillary mucinous tumor with moderate dysplasia of the bile duct. Although several cases of intraductal papillary mucinous neoplasm of the liver (IPNL) without any pancreatic association have been described, the simultaneous presentation of both IPMT of the pancreas and IPNL is very rare. The patient has been doing well for 10 months postoperatively.
-
Citations
Citations to this article as recorded by- Surgical resection for simultaneous intraductal papillary mucinous neoplasm of the bile duct and pancreatic duct: A case report
Xiao-Rui Huang, Deng-Sheng Zhu, Ya-Hong Yu
World Journal of Gastrointestinal Surgery.2025;[Epub] CrossRef - Reoperation for heterochronic intraductal papillary mucinous neoplasm of the pancreas after bile duct neoplasm resection: A case report
Gang Xiao, Tao Xia, Yi-Ping Mou, Yu-Cheng Zhou
World Journal of Gastrointestinal Surgery.2023; 15(7): 1542. CrossRef - Intraductal papillary neoplasm of the bile duct: The new frontier of biliary pathology
Federico Mocchegiani, Paolo Vincenzi, Grazia Conte, Daniele Nicolini, Roberta Rossi, Andrea Benedetti Cacciaguerra, Marco Vivarelli
World Journal of Gastroenterology.2023; 29(38): 5361. CrossRef - Multicentric recurrence of intraductal papillary neoplasm of bile duct after spontaneous detachment of primary tumor: A case report
Hiroki Fukuya, Akifumi Kuwano, Shigehiro Nagasawa, Yusuke Morita, Kosuke Tanaka, Masayoshi Yada, Akihide Masumoto, Kenta Motomura
World Journal of Clinical Cases.2022; 10(3): 1000. CrossRef - Co-occurrence of IPMN and malignant IPNB complicated by a pancreatobiliary fistula: A case report and review of the literature
Xu Ren, Chun-Lan Zhu, Xu-Fu Qin, Hong Jiang, Tian Xia, Yong-Ping Qu
World Journal of Clinical Cases.2019; 7(1): 102. CrossRef - Synchronous pancreatic adenocarcinoma and intrahepatic cholangiocarcinoma arising in the context of intraductal papillary neoplasms
Anmol Bansal, Swan N. Thung, Hongfa Zhu, Myron Schwartz, Sara Lewis
Clinical Imaging.2016; 40(5): 897. CrossRef
- Surgical resection for simultaneous intraductal papillary mucinous neoplasm of the bile duct and pancreatic duct: A case report
- Fine Needle Aspiration Cytology of Langerhans Cell Histiocytosis of Mandible: A Case Report.
- Sang Ryung Lee, Jae Hee Suh, Hee Jung Cha, Young Min Kim, Hye Jeong Choi
- Korean J Pathol. 2010;44(1):106-109.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.1.106
- 4,260 View
- 24 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - We present a case of mandibular involvement with Langerhans cell histiocytosis (LCH), diagnosed by ultrasound-guided aspiration and subsequently confirmed by incisional biopsy and immunohistochemistry in an eight-year-old boy. The cytologic findings included the presence of characteristic Langerhans cells of both mononucleate and multinucleate form. Diagnostic confirmation was obtained by immunopositivity for S-100 protein and CD1a of Langerhans histiocytes on paraffin-embedded sections obtained during incisional biopsy of the right mandibular area. By reporting a case of childhood LCH, we correlate the cytologic findings with histologic features and discuss the role of aspiration cytologic diagnosis in such a rare and cytomorphologically characteristic case.
-
Citations
Citations to this article as recorded by- Bronchial Washing Cytology of Pulmonary Langerhans Cell Histiocytosis: A Case Report
Taeyeong Kim, Hyeong Ju Kwon, Minseob Eom, Sang Wook Kim, Min Hi Sin, Soon-Hee Jung
Journal of Pathology and Translational Medicine.2017; 51(4): 444. CrossRef
- Bronchial Washing Cytology of Pulmonary Langerhans Cell Histiocytosis: A Case Report
- Nasal Chondromesenchymal Hamartoma: A Case Report.
- Jun Kang, Young Ok Hong, Geung Hwan Ahn, Young Min Kim, Hee Jeong Cha, Hye Jeong Choi
- Korean J Pathol. 2007;41(4):258-262.
- 2,267 View
- 28 Download
-
 Abstract
Abstract
 PDF
PDF - We report a case of nasal chondromesenchymal hamartoma. A 14-year-old boy presented with a 5 cm sized mass in the left maxillary sinus, facial swelling and a loose tooth. A subtotal left maxillectomy with a bone graft was performed. The excised mass was composed of partly encapsulated, solid and cystic fragments of soft tissues. The mass contained chondroid and myxoid areas consisting of mesenchymal tissues including hyaline cartilage, osteoid and spindle cells in various proportions. The hyaline cartilage component was the most prominent. The spindle cell component had a fibrous matrix with variable myxoid or sclerotic changes. Thick hyalinized eosinophilic osteoid-like trabeculae were focally present. Immunohistochemically, all the mesenchymal cells tested positive for vimentin. The chondrocytes tested positive for the S-100 protein, and the spindle cell component showed focal immunoreactivity for smooth muscle actin and desmin. However, the cells were negative to pan-cytokeratin and p63.
- Cellular Angiofibroma of the Vulva: A Report of Three Cases.
- Hye Jeong Choi, Sung Nam Kim, Kyu Rae Kim
- Korean J Pathol. 2001;35(3):259-262.
- 2,132 View
- 28 Download
-
 Abstract
Abstract
 PDF
PDF - Cellular angiofibroma is a recently described, distinctive soft tissue tumor of the vulvovaginal region which is characterized by small, well-circumscribed tumors with fibroblastic differentiation. We report three cases of cellular angiofibroma of the vulva in middle-aged women. All three patients presented with painless swelling in the labium majora. The age of the three patients ranged from 43 to 56 years old (mean: 48 years old) and the size of the tumor ranged from 2 to 5 cm. The microscopic appearance was characterized by a cellular, well-circumscribed mass composed of uniform, bland, spindle stromal cells, numerous thick-walled, hyalinized vessels, and a scarce component of mature adipocytes. Immunohistochemical stains of the tumor cells show positivity for vimentin but negativity for smooth muscle actin, S-100 protein, desmin, factor VIII-related antigen and epithelial membrane antigen. The tumor should be differentiated from aggressive angiomyxoma and angiomyofibroblastoma because of its different clinicopathologic features, cells of origin and immunohistochemical findings.
- Superficial Endometriosis of the Uterine Cervix as a Source of Atypical Glandular Cells of Undetermined Significance in the Cervicovaginal Smear: A Report of Two Cases.
- Hye Jeong Choi, Seung Koo Lee, Kyu Rae Kim
- Korean J Pathol. 2001;35(3):263-266.
- 2,809 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Superficial endometriosis of the uterine cervix refers to a lesion in which endometrial stroma and/or gland is located immediately subjacent to the surface epithelium. The cells on the cervicovaginal smear shed from the lesion can be a significant source of atypical glandular cells of undetermined significance (AGUS), or can be easily mistaken for glandular dysplasia or adenocarcinoma in situ. Not infrequently it occurs at the conization site for cervical neoplasia. We describe the cytologic and histologic features of 2 cases of superficial endometriosis of the uterine cervix, which were discovered during an evaluation for AGUS detected on the cervicovaginal smears, with an emphasis on the utility of trichrome and reticulin staining for the diagnosis of superficial endometriosis. The cervicovaginal smears show sheets and clusters of glandular cells having mild to moderately pleomorphic oval nuclei with inconspicuous nucleoli and indistinct cytoplasmic border. Single cells or tumor diathesis were not present. Diagnostic histologic findings were the absence of thick or abundant collagen bundles, the encasement of individual stromal cells by a fine reticulin network and thick reticulin fibers around the spiral arterioles within the endometriotic foci. Therefore, superficial endometriosis should be considered as a potential source of AGUS, especially during follow-up after conization for cervical intraepithelial neoplasia.
- Intraosseous Lipoma A report of four cases.
- Hye Jeong Choi, Mi Jin Gu, Joon Hyuk Choi, Duk Seop Shin, Kil Ho Cho
- Korean J Pathol. 1999;33(6):467-470.
- 2,185 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - Intraosseous lipoma is a very rare primary tumor of the bone. We report four cases of intraosseous lipoma. The patient ranged in age from 34 to 59-year-old (median age: 35 year-old). There were three men and one woman. All of four cases presented with pain. The involved bones were calcaneus in two cases, tibia in one case and ilium in one case, respectively. In all cases plain x-ray film revealed well-defined lytic lesion. Their size ranged 2 to 4.5 cm (mean size: 3.5 cm). Histologic examination showed mature adipose tissue. Three cases showed secondary changes such as atrophic bone, fat necrosis, fibrosis, dystrophic calcification, and reactive ischemic bone formation. The clinicopathologic and roentgenographic correlation are necessary in establishing correct diagnosis of this tumor.
- Combined Mucinous Tumor and Carcinoid of Appendix Associated with Mucinous Tumor of Ovary and Pseudomyxoma Peritonei: A case report .
- Hye Jeong Choi, Mi Jin Kim
- Korean J Pathol. 1999;33(11):1094-1096.
- 2,227 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - We report a case of mucinous cystadenoma of uncertain malignant potential and carcinoid of appendix associated with bilateral mucinous cystadenoma of ovary and pseudomyxoma peritonei. The patient was a 46-year-old female. She suffered from dyspnea and lower abdominal palpable masses for several months. Ultrasonogram showed multilocular huge ovarian cysts. Appendectomy, transabdominal hysterectomy, bilateral salphingo-oophorectomy and biopsy of omentum were performed. The bilateral ovaries measured 16 11 cm and 7X5 cm in size, respectively. The both ovaries showed multilocular cysts filled with thick mucus material. The ovarian cysts were covered by a single layer of columnar epithelium with focal proliferation. Mucus materials dissected through the ovarian stroma (pseudomyxoma ovarii). The tip of appendix was dilated and covered by mucus material. The cut surface showed a cyst and a yellowish solid mass proximal to the cyst. Microscopically, the appendiceal cyst was lined by stratified columnar epithelium with moderate cytologic atypia. Mucus material dissected through the wall. In the proximal portion of the appendix, a classic carcinoid with focal tubular form was present in submucosa and muscle layer. The omentum was covered by thick mucus material. Microscopically, the omentum showed mucinous epithelium and mucus material (pseudomyxoma peritonei).
Review
- Differential Diagnosis of Fine Needle Aspiration Cytology of Benign Lymphadenopathy.
- Eun Mee Han, Dong Eun Song, Dae Un Eom, Hye Jeong Choi, Hee Jeong Cha, Jooryung Huh
- J Pathol Transl Med. 2006;17(2):99-107.
- 2,769 View
- 36 Download
-
 Abstract
Abstract
 PDF
PDF - In the investigation of superficial lymphadenopathy of unknown cause, fine needle aspiration (FNA) cytology plays an invaluable role. It enables the differentiation of benign lymphadenopathy from lymphoid and non-lymphoid malignancies, obviating the need for open biopsy, and allowing the triage of patients. Cytopathologists should be familiar with the typical FNA patterns of benign lymphadenopathy, and recognize and differentiate among categories. In a minority of cases of benign lymphadenopathy, FNA can render a specific diagnosis. Benign lymphadenopathies are generally categorized into reactive lymphoid hyperplasia (RLH), inflammatory or infectious processes, and benign lymphoproliferative disorders. RLH characteristically presents with a heterogeneous and polymorphous smear composed of normal cellular constituents of lymph nodes, in contrast with the homogeneous or monomorphic smear of most lymphomas. The caveat is that various malignant disorders may also present with polymorphous populations. It is also important to recognize thatbenign lymphoid smears may sometimes contain atypical cells that raise the suspicion of malignancy. Clinical information should always be the integral part of the diagnostic criteria in FNA of lymphadenopathy. If there is any doubt about the benign nature of the smear, it is prudent to suggest biopsy and ancillary studies.
Case Report
- Metastatic Melanoma Mimicking a Papillary Carcinoma of the Thyroid in Fine Needle Aspiration Cytology: A Case Report.
- Young Ok Hong, Jae Hee Suh, Hee Jeong Cha, Hye Jeong Choi, Young Min Kim
- J Pathol Transl Med. 2007;18(2):161-164.
- 2,598 View
- 44 Download
-
 Abstract
Abstract
 PDF
PDF - Metastasis to the thyroid gland is very rare in clinical practice. We recently encountered a 65-year-old woman who presented with a large thyroid nodule that mimicked the cytologic features of a papillary thyroid carcinoma on fine needle aspiration biopsy (FNAB). Although initially diagnosed as a papillary thyroid carcinoma, a thorough clinical work-up revealed multiple lesions in the bones, liver, and nasal cavity, which were confirmed as metastases of a malignant melanoma. Despite a thorough physical examination, however, the primary skin lesion could not be identified. Although FNAB shows a high degree of accuracy in diagnosing primary thyroid tumors, it is less accurate in diagnosing metastases to the thyroid gland. A thorough clinical history with appropriate immunohistochemical staining assays is necessary for the accurate diagnosis of metastatic malignant melanoma.
Original Article
- Expression of c-erbB-2 and Cyclooxygenase-2 in Pancreatic Ductal Adenocarcinoma.
- Hye Jeong Choi, Hong Jin Kim, Sung Soo Yun, Joon Hyuck Choi
- Korean J Pathol. 2007;41(3):171-175.
- 2,263 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Background
: Carcinoma of the pancreas is a fatal malignant disease with limited therapeutic options. Cyclooxygenase-2 (COX-2) and c-erbB-2 are known to be involved in the carcinogenesis, differentiation and invasiveness of various neoplasms. We studied the immunohistochemical expressions of c-erbB-2 and COX-2 and the correlation between these expressions and the clinicopathologic parameters and the relation between the expressions.
Methods
: Immunohistochemical staining for c-erbB-2 and COX-2 were performed on the paraffin embedded sections of 36 cases of surgically resected ductal adenocarcinoma of the pancreas and 10 cases of non-neoplastic pancreas tissue.
Results
: The non-neoplastic control group showed a c-erbB-2 expression in the acini (8/10) and ducts (2/10), and a COX-2 expression in the acini (6/10) and ducts (3/10). The overexpression of c-erbB-2 was observed in 58% (21/36) of the carcinoma specimens. No significant correlation was found between c-erbB-2 and age, gender, tumor size, gross type, histologic grade, vascular invasion, perineural invasion, lymph node metastasis, and the TNM stage. The overexpression of COX-2 was observed in 41.7% (15/36) of the carcinoma specimens. The COX-2 expression was significantly high in the lymph node metastasis group (p<0.05), but it was not correlated with the other clinicopathologic parameters. Also there was no significant correlation between the c-erbB-2 and COX-2 expressions.
Conclusions
: In pancreatic ductal adenocarcinomas, c-erbB-2 and COX-2 were frequently overexpressed, and COX-2 overexpression was correlated with lymph node metastasis.

 E-submission
E-submission

 First
First Prev
Prev



