Search
- Page Path
- HOME > Search
Review
- Cervical intraepithelial neoplasia and cervical cytology in pregnancy
- Ji-Young Kim, Jeong Yun Shim
- J Pathol Transl Med. 2024;58(6):283-290. Published online November 7, 2024
- DOI: https://doi.org/10.4132/jptm.2024.10.17
- 10,578 View
- 445 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
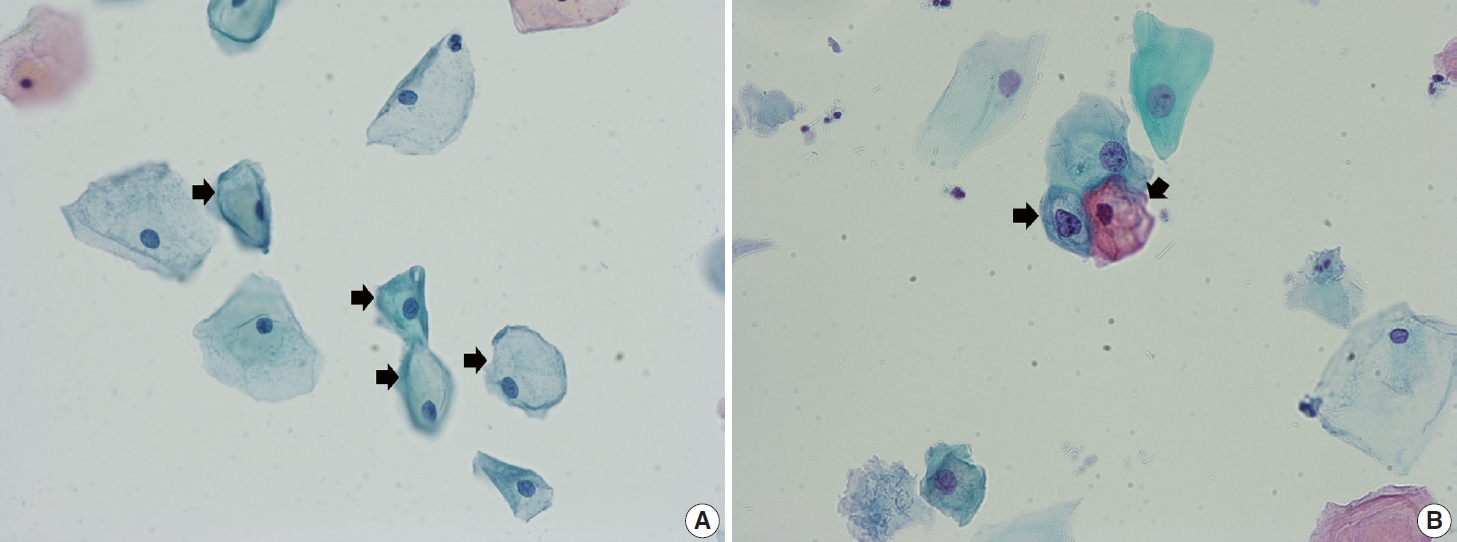
PDF - Cervical cancer screening during pregnancy presents unique challenges for cytologic interpretation. This review focuses on pregnancy-associated cytomorphological changes and their impact on diagnosis of cervical intraepithelial neoplasia (CIN) and cervical cancer. Pregnancy-induced alterations include navicular cells, hyperplastic endocervical cells, immature metaplastic cells, and occasional decidual cells or trophoblasts. These changes can mimic abnormalities such as koilocytosis, adenocarcinoma in situ, and high-grade squamous intraepithelial lesions, potentially leading to misdiagnosis. Careful attention to nuclear features and awareness of pregnancy-related changes are crucial for correct interpretation. The natural history of CIN during pregnancy shows higher regression rates, particularly for CIN 2, with minimal risk of progression. Management of abnormal cytology follows modified risk-based guidelines to avoid invasive procedures, with treatment typically deferred until postpartum. The findings reported in this review emphasize the importance of considering pregnancy status in cytological interpretation, highlight potential problems, and provide guidance on differentiating benign pregnancy-related changes from true abnormalities. Understanding these nuances is essential for accurate diagnosis and proper management of cervical abnormalities in pregnant women.
-
Citations
Citations to this article as recorded by- The significance of biological samples from pregnant women in cervical intraepithelial neoplasia
Xue Mi, Maharjan Rashmi, Zangyu Pan, Di Wu, Jinwei Miao
Frontiers in Medicine.2025;[Epub] CrossRef - Oncologic and pregnancy outcomes of cervical high-grade intraepithelial lesions and delivery mode
Olga P. Matylevich, Ilya A. Tarasau, Sviatlana Y. Shelkovich, Aliaksandr F. Martsinkevich
Academia Oncology.2025;[Epub] CrossRef
- The significance of biological samples from pregnant women in cervical intraepithelial neoplasia
Original Articles
- Idiopathic Duct Centric Pancreatitis in Korea: A Clinicopathological Study of 14 Cases.
- Hyo Jeong Kang, Tae Jun Song, Eunsil Yu, Jihun Kim
- Korean J Pathol. 2011;45(5):491-497.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.5.491
- 4,209 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Idiopathic duct centric pancreatitis (IDCP) is a subtype of autoimmune pancreatitis (AIP) that is histologically characterized by granulocytic epithelial lesion and scarce IgG4-positive cells. This subtype of AIP has not been documented in Asian countries.
METHODS
We reviewed 38 histologically confirmed AIP cases and classified them into lymphoplasmacytic sclerosing pancreatitis (LPSP) and IDCP. Then, clinicopathological characteristics were compared between LPSP and IDCP.
RESULTS
Fourteen cases (36.8%) were IDCP. IDCP affected younger patients more than LPSP. IDCP was associated with ulcerative colitis in 35.7% of cases, whereas LPSP was associated with IgG4-related sclerosing diseases such as cholangitis, retroperitoneal fibrosis or sialadenitis in 41.7% of cases. IDCP was microscopically characterized by neutrophilic ductoacinitis with occasional granulocytic epithelial lesions, whereas LPSP was characterized by storiform inflammatory cell-rich fibrosis and obliterative phlebitis. IgG4-positive cells were not detected in any IDCP case but more than 20 IgG4-positive cells per high-power-field were invariably detected in LPSP cases. All patients with IDCP responded dramatically to steroids without recurrence, whereas 33.3% of patients with LPSP developed recurrences.
CONCLUSIONS
IDCP is clinicopathologically distinct from LPSP and can be diagnosed when neutrophilic ductoacinitis or granulocytic epithelial lesions are observed in a pancreatic biopsy under the appropriate clinical setting.
- Qualification of Atypical Squamous Cells of Undetermined Significance - "ASCUS, R/O HSIL": Cytologic Features and Histologic Correlation.
- Hye Sun Kim, Bock Man Kim, Yee Jung Kim, Hy Sook Kim
- J Pathol Transl Med. 2002;13(1):14-20.
- 2,631 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - Cytologic and histopathologic features and human papillomavirus (HPV) DNA detection associated with 101 cervicovaginal smears which are classified as 'atypical squamous cells of undetermined significance, rule out high grade squamous intraepithelial lesion(ASCUS, R/O HSIL)' were reviewed and compared to 89 smears of 'ASCUS, not otherwise specified(NOS)' . Cytologic fieatures of ASCUS, R/O HSIL included atypical single small cells(36.6%), hyperchromatic tissue fragments(35.6%), atypical metaplastic cells(18.8%), endometrial cell-like clusters(5.9%), and atypical parakeratotic cells(3.0%). A final diagnosis of HSIL on biopsy was assigned to 47(54.0%) of 87 women with ASCUS, R/O HSIL and to 13(14.6%) of 89 women with ASCUS, NOS ( p=0.000). There was no difference in HPV DNA detection rate between ASCUS, R/O HSIL and ASCUS, NOS smears. These data suggest that subclassification of ASCUS is helpful to manage patients because ASCUS, R/O HSIL is more often associated with an underlying HSIL on biopsy. Therefore, women with ASCUS, rule out HSIL should be actively managed with colposcopic examination.
- Cytologic Features of Papillary Immature Metaplasia of Uterine Cervix.
- Hye Sun Kim, Mee Im Seon, Yee Jung Kim, Hy Sook Kim
- J Pathol Transl Med. 2002;13(1):21-27.
- 3,291 View
- 61 Download
-
 Abstract
Abstract
 PDF
PDF - Papillary immature metaplasia (PIM) of the uterine cervix (immature condyloma) is a subset of low grade squamous intraepithelial lesion (LSIL) which is frequently associated with human papilloma virus (HPV) types 6 and 11. The histologic features of PIM include filiform papillae lined by evenly spaced immature metaplastic-type cells with frequent nucleoli, mild anisokaryosis, and a low mitotic index. To characterize the cytologic changes associated with PIM, we analyzed 14 cases of PIM from our file. We reviewed biopsy slides and the cervicovaginal smears taken proximate to the time of biopsy. Histologically, nine cases had either flat condyloma (7 cases) or high grade squamous intraepithelial lesion (HSIL) (2 cases). Cytologic changes included cells in various stages of maturation with karyomegaly (14 cases), cells with irregularities in the nuclear membrane (13 cases), intermediate cells with karyomegaly(13 cases), cells with binucleation (13 cases), and aborted koilocytes (11 cases). Cervicovaginal smears from all cases were interpreted as atypical squamous cells of undetermined significance (ASCUS), NOS or ASCUS, rule out squamous intraepithelial lesion (SIL) or LSIL in two cases with flat condyloma or HSIL in a case with severe dysplasia. PIM is a distinct histologic entity that can present with a spectrum of cytologic findings, but cytologic findings may resemble variable reactive conditions and immature HSIL. Therefore, it is difficult to diagnose PIM by cytology alone. However, the meticulous efforts for making the cytologic diagnoses which can induce active management of patients are recommended because PIM is a variant of LSIL and frequently has a flat condyloma or HSIL.
- Correlation Of Human Papillomavirus Infection and Postmenopausal Squamous Atypia in Cervical Cytology.
- Yi Kyeong Chun, In Gul Moon, Sung Ran Hong, Hye Sun Kim, Jong Sun Choi, Ji Young Park, Jong Sook Park, Tae Jin Kim, Hy Sook Kim
- J Pathol Transl Med. 2004;15(2):81-85.
- 2,290 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - Postmenopausal squamous atypia (PSA) is a phenomenon characterized by cellular alterations mimicking condyloma in the uterine cervix of postmenopausal women. It is not associated with human papillomavirus (HPV) infection. The aim of this study is to correlate findings with HPV infection and the cytohistologic findings of PSA. Eighty-three smears from postmenopausal women, initially interpreted as ASCUS and low-grade squamous intraepithelial lesions(LSIL), were reviewed according to the criteria of PSA. Fifty-eight cases were subsequently reclassified as PSA. Forty cases categorized as PSA were available for HPV-DNA detection by a nested polymerase chain reaction. Eight of these 40 cases(20%) showed biopsy-proven LSIL lesions. The HPV-DNA was detected in 42.5%(17/40), compared to 25%(5/20) of control cases. The HPV-DNA detection rate of biopsy-proven LSIL was 62.5%(5/8). It has been concluded that cytologic differential diagnosis of PSA from LSIL is difficult due to because of poor histologic and viral correlation.
- A Study of beta 2-Microglobulin Expression in Uterine Cervical Epithelial Lesion.
- Na Hye Myong, Eui Keun Ham
- Korean J Pathol. 1991;25(5):436-445.
- 2,385 View
- 10 Download
-
 Abstract
Abstract
- Beta-2-microglubulin(beta 2m), the invariable light chain of the histocompatibility antigen is present on the surfaces of most human nucleated cells. It has proved to be reduced or disappeared on the cell surfaces of variable skin cancers. Patterns of beta 2m stainability in normal uterus and of the loss in several cervical epithelial lesions were examined by immunohistochemical staining using rat monoclonal and rabbit polyclonal anti-beta 2m, repectively on fresh tissues of 13 cases and formalin-fixed paraffin-embedded tissues of 23 cases. To know patterns of loss of beta 2m stainability and measure its extent and degree, only fixed tissues were examined. Fresh uterine tissue showed beta 2m stainability present on the cell membranes of squamous epithelium, endocervical gland, and capillary endothelium. Of these, squamous epithelium of uterine cervix revealed most characteristic lace-like staining along the cell outlines. Paraffin-embedded 23 cases were classified as group I (6 normal conrol and metaplasia), II (5 mild and moderate dysplasia), III (6 severe dysplasia and carcinome in situ), and IV ( 6 microinvasive and invasive squamous cell carcinoma). Group 2-4 showed reduced beta 2m stainability when compared to group 1 that exhibited the similar stainability as fresh normal cervical epithelium. The reduction or less proved to be statistically significant(p-value<0.001) in group 3 and 4 except for group 2. In spite of being invasive cases, a few disclosed beta 2m positive cells mainly in well-differentiated areas. In sum, ABC immunohistochemical staining of beta 2m showed the tendency tend to decrease or disappear in uterine cervical epithelial lesions with premalignant or malignant change and rather to appear in some well-differentiated areas of malignant lesions.

 E-submission
E-submission

 First
First Prev
Prev



