Search
- Page Path
- HOME > Search
Original Articles
- Evaluation of human papillomavirus (HPV) prediction using the International Endocervical Adenocarcinoma Criteria and Classification system, compared to p16 immunohistochemistry and HPV RNA in-situ hybridization
- Hezhen Ren, Jennifer Pors, Christine Chow, Monica Ta, Simona Stolnicu, Robert Soslow, David Huntsman, Lynn Hoang
- J Pathol Transl Med. 2020;54(6):480-488. Published online August 31, 2020
- DOI: https://doi.org/10.4132/jptm.2020.07.18
- 8,532 View
- 175 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The International Endocervical Adenocarcinoma Criteria and Classification (IECC) separated endocervical adenocarcinomas into human papillomavirus (HPV) associated (HPVA) and non–HPV-associated (NHPVA) categories by morphology alone. Our primary objective was to assess the accuracy of HPV prediction by the IECC system compared to p16 immunohistochemistry and HPV RNA in-situ hybridization (RISH). Our secondary goal was to directly compare p16 and HPV RISH concordance.
Methods
Cases were classified by IECC and stained for p16 and HPV RISH on tissue microarray, with discordant p16/HPV RISH cases re-stained on whole tissue sections. Remaining discordant cases (p16/HPV, IECC/p16, IECC/HPV discordances) were re-reviewed by the original pathologists (n = 3) and external expert pathologists (n = 2) blinded to the p16 and HPV RISH results. Final IECC diagnosis was assigned upon independent agreement between all reviewers.
Results
One hundred and eleven endocervical adenocarcinomas were classified originally into 94 HPVA and 17 NHPVA cases. p16 and HPV RISH was concordant in 108/111 cases (97%) independent of the IECC. HPV RISH and p16 was concordant with IECC in 103/111 (93%) and 106/111 (95%), respectively. After expert review, concordance improved to 107/111 (96%) for HPV RISH. After review of the eight discordant cases, one remained as HPVA, four were reclassified to NHPVA from HPVA, two were unclassifiable, and one possibly represented a mixed usual and gastric-type adenocarcinoma.
Conclusions
p16 and HPV RISH have excellent concordance in endocervical adenocarcinomas, and IECC can predict HPV status in most cases. Focal apical mitoses and apoptotic debris on original review led to the misclassification of several NHPVA as HPVA. -
Citations
Citations to this article as recorded by- EdgeNeXt-SEDP for cervical adenocarcinoma HPV-associated and non-HPV-associated diagnosis and decision support
Qi Chen, Hao Wang, Hao Zhang, Zhenkun Zhu, Xi Wei
Life Sciences.2025; 380: 123931. CrossRef - Cytology and histology of endocervical glandular lesions: a review with emphasis on recent developments
Natalie Banet, Karen L. Talia
Pathology.2025; 57(7): 817. CrossRef - Role of human papillomavirus status in the classification, diagnosis, and prognosis of malignant cervical epithelial tumors and precursor lesions
Simona Stolnicu
Die Pathologie.2025;[Epub] CrossRef - Joint detection of multiple HPV-testing technologies and evaluation of clinicopathological characteristics discriminate between HPV-independent and low-copy HPV-associated cervical squamous cell carcinoma (CSCC) -an analysis of 3869 cases
Linghui Lu, Tianqi Liu, Shunni Wang, Jing Li, Feiran Zhang, Yan Ning, Yiqin Wang
Gynecologic Oncology.2023; 170: 59. CrossRef - Incidence and Clinicopathologic Characteristics of Human Papillomavirus–independent Invasive Squamous Cell Carcinomas of the Cervix
Simona Stolnicu, Douglas Allison, Aaron M. Praiss, Basile Tessier-Cloutier, Amir Momeni Boroujeni, Jessica Flynn, Alexia Iasonos, Rene Serrette, Lien Hoang, Andrei Patrichi, Cristina Terinte, Anna Pesci, Claudia Mateoiu, Ricardo R. Lastra, Takako Kiyokawa
American Journal of Surgical Pathology.2023; 47(12): 1376. CrossRef - Testing Algorithms for the Diagnosis of Malignant Glandular Tumors of the Uterine Cervix Histotyped per the International Endocervical Adenocarcinoma Criteria and Classification (IECC) System
Máire A. Duggan, Qiuli Duan, Ruth M. Pfeiffer, Mary Anne Brett, Sandra Lee, Mustapha Abubakar, Martin Köbel, Monica Rodriguez, Aylin Sar
Applied Immunohistochemistry & Molecular Morphology.2022; 30(2): 91. CrossRef - Local and Metastatic Relapses in a Young Woman with Papillary Squamous Cell Carcinoma of the Uterine Cervix
Ha Young Woo, Hyun-Soo Kim
Diagnostics.2022; 12(3): 599. CrossRef - Clinical correlation of lymphovascular invasion and Silva pattern of invasion in early-stage endocervical adenocarcinoma: proposed binary Silva classification system
Simona Stolnicu, Lien Hoang, Noorah Almadani, Louise De Brot, Glauco Baiocchi, Graziele Bovolim, Maria Jose Brito, Georgia Karpathiou, Antonio Ieni, Esther Guerra, Takako Kiyokawa, Pavel Dundr, Carlos Parra-Herran, Sofia Lérias, Ana Felix, Andres Roma, An
Pathology.2022; 54(5): 548. CrossRef - Reproducibility of Morphologic Parameters of the International Endocervical Adenocarcinoma Criteria and Classification System and Correlation With Clinicopathologic Parameters: A Multi-Institutional Study
Pinar Bulutay, Nihan Haberal, Özlem Özen, Özlem Erdem, Emine H. Zeren, İbrahim Kulac, Çagatay Taskiran, Dogan Vatansever, Ali Ayhan, Nilgün Kapucuoğlu
International Journal of Gynecological Pathology.2022; 41(5): 447. CrossRef - HPV-Negative Cervical Cancer: A Narrative Review
Francesca Arezzo, Gennaro Cormio, Vera Loizzi, Gerardo Cazzato, Viviana Cataldo, Claudio Lombardi, Giuseppe Ingravallo, Leonardo Resta, Ettore Cicinelli
Diagnostics.2021; 11(6): 952. CrossRef - International Endocervical Adenocarcinoma Criteria and Classification (IECC): An Independent Cohort With Clinical and Molecular Findings
Hezhen Ren, Noorah Almadani, Jennifer Pors, Samuel Leung, Julie Ho, Christine Chow, Monica Ta, Kay J. Park, Simona Stolnicu, Robert Soslow, David Huntsman, Blake C. Gilks, Lynn Hoang
International Journal of Gynecological Pathology.2021; 40(6): 533. CrossRef
- EdgeNeXt-SEDP for cervical adenocarcinoma HPV-associated and non-HPV-associated diagnosis and decision support
- Expressions of MIB-1, p53 and CEA in Endocervical Glandular Lesions.
- Mi Jin Kim, Young Gi Lee, Dong Sug Kim
- Korean J Pathol. 2001;35(1):41-47.
- 2,101 View
- 64 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
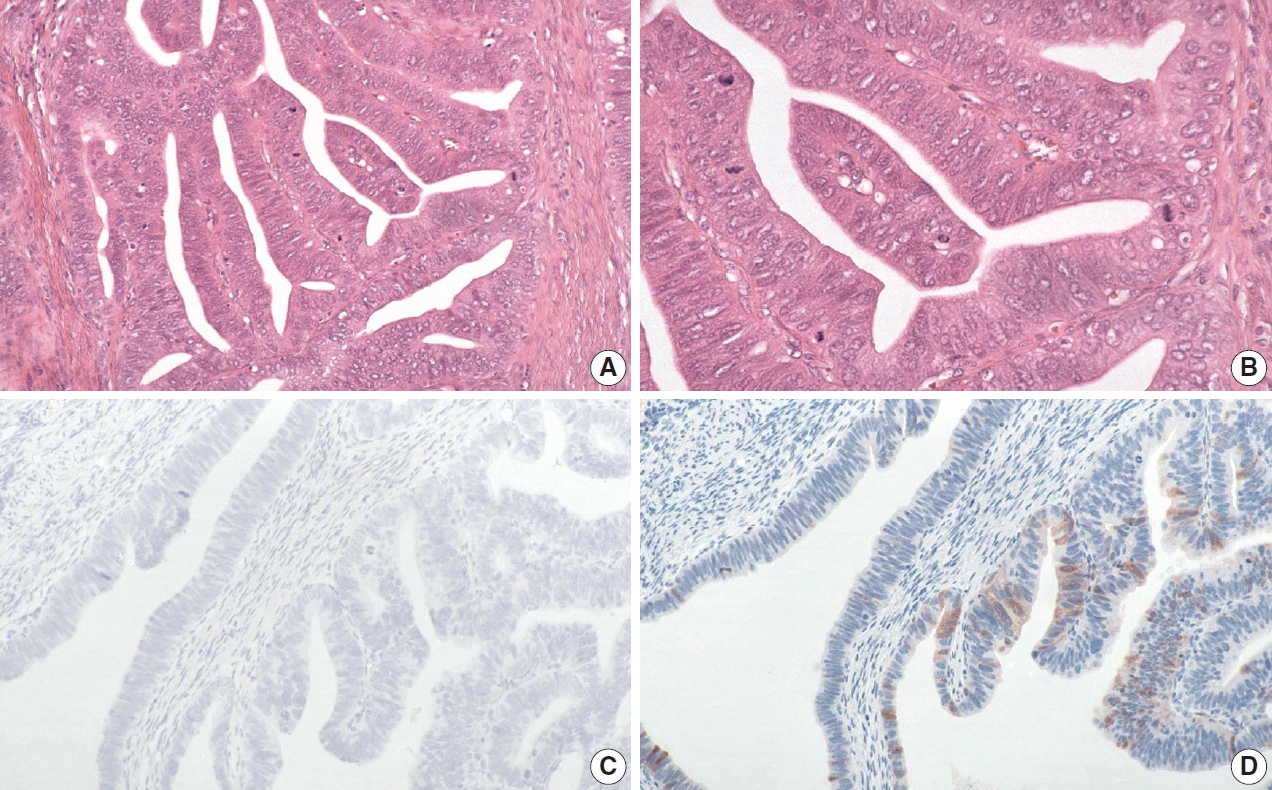
Endocervical glandular lesions include glandular atypia (GA), endocervical glandular dysplasia (EGD), adenocarcinoma in situ (AIS), and invasive adenocarcinoma (IA). The diagnosis of malignant glandular lesions is occasionally difficult to distinguish from benign mimickers, and the morphologic features of EGD remain unsettled.
METHODS
Immunohistochemical stains for MIB-1, p53 and CEA were performed on 81 cases of paraffin-embedded endocervical glandular lesions including 22 IA, 15 AIS, 15 EGD, 13 GA, 8 microglandular hyperplasia (MGH) and 8 tubal metaplasia (TM).
RESULTS
The MIB-1 labelling index of IA was 59.68%, 69.53% for AIS, 26.60% for EGD, 16.03% for benign. p53 overexpression was noted in 4 (18%) cases of IA, 3 (20%) of AIS, but none of EGD and benign lesions. It was Interesting to note that one case of MGH showed p53 staining in low intensity. Diffuse strong cytoplasmic CEA positivity was present in all of IA and AIS, whereas seven (47%) of 15 EGD and 12 (41%) of 29 benign lesions showed focal cytoplasmic CEA positivity. There were significant differences in MIB-1 and CEA immunostainings among the adenocarcinoma, EGD, and benign glandular lesions. Adenocarcinoma was closely related to p53 overexpression, although occurring in a low percentage of the cases.
CONCLUSION
MIB-1 immunostaining can be useful in differentiating among endocervical adenocarcinoma, endocervical glandular dysplasia and benign glandular lesions. p53 overexpression might be helpful in the diagnosis of adenocarcinoma.

 E-submission
E-submission

 First
First Prev
Prev



