Intravascular Papillary Endothelial Hyperplasia of the Chest Wall Misdiagnosed as a Malignancy on Fine Needle Aspiration
Article information
Intravascular papillary endothelial hyperplasia (IPEH) is an exuberant proliferation of endothelial cells that may occur within the lumen of a pre-existing vessel or vascular malformation.1 Although IPEH is regarded as a non-neoplastic reactive process, misdiagnoses as a malignancy have been reported, particularly based on fine needle aspiration (FNA) findings.2-4 We report a case of IPEH on the chest wall that was initially misdiagnosed as an adenocarcinoma on FNA.
CASE REPORT
A 75-year-old male underwent a subtotal gastrectomy at 62 years of age. He was diagnosed as a well-differentiated adenocarcinoma confined to the gastric mucosa. He remained in good health until 3 years ago, at which time he noticed a 2 cm asymptomatic mass on the chest wall. The mass was situated 10 cm apart from the previous surgical scar. One week before hospital admission, he experienced pain at the site of the mass and was referred for further evaluation.
The clinical condition of the patient was good. Physical examination revealed a firm, smooth, round mass on the anterior chest wall. The size of the mass had not changed since initial presentation. The mass was initially presumed to be a lipoma or epidermal inclusion cyst on physical palpation. However FNA was necessary to rule out a metastatic adenocarcinoma originating from the stomach.
The FNA cytology showed low cellular smears containing a few cohesive sheets of polygonal pleomorphic cells with vesicular chromatin, prominent nucleoli, abundant dense cytoplasm, and cytoplasmic vacuoles. Scattered individual polygonal cells were also present in a hemorrhagic background (Fig. 1). Some fibrins were intermingled, and some of the cells showed long cytoplasmic processes suggestive of spindling. Pleomorphic polygonal cells were arranged in alveolar or glandular patterns that were suspected to be metastatic adenocarcinoma.
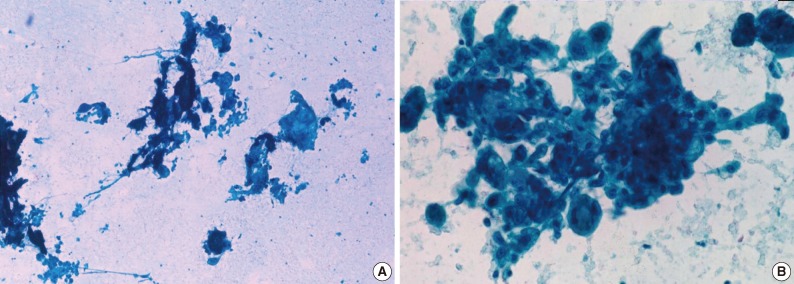
(A) Fine needle aspiration shows several cohesive sheets with a papillary configuration and fibrin materials in a hemorrhagic background. (B) The sheets are composed of pleomorphic polygonal cells with abundant cytoplasm and cytoplasmic vacuole (A, B, Papanicolaou stain).
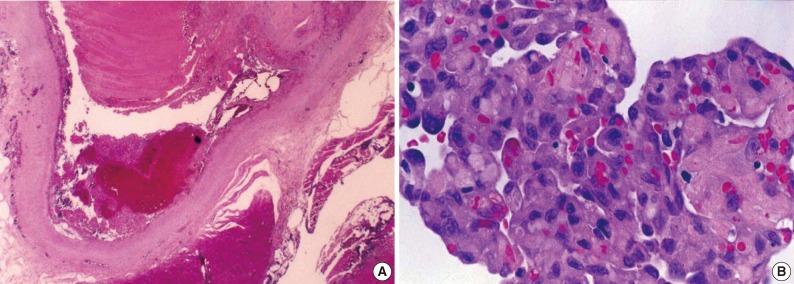
The pathologic findings of the excised mass showed a well-demarcated vascular lesion within the skeletal muscle associated with a hematoma. There was an anastomosing papillary core lined by plump endothelial cells. The papillae contained fibrin-like materials and the endothelial cells were pleomorphic with vesicular nuclei and prominent nucleoli (Fig. 2). Mitotic figures were not observed. The overall cellular features were similar to those observed in the aspirate smears. The cells showed diffuse strong cytoplasmic immunoreactivity for CD34 and factor VIII-related antigen, and were negative for cytokeratin, confirming the diagnosis of intravascular papillary endothelial hyperplasia.
DISCUSSION
IPEH may be confused with a malignancy based on FNA, particularly when the lesion occurs in uncommon anatomic locations. IPEH is an unusual form of organizing thrombus and frequently occurs within the vessels of the head, neck, and fingers, while it is rarely occurs on the chest wall.1,5 IPEH is characterized by endothelial cell proliferation and fibrous capsulation. And it has been regarded as a reactive process rather than a true neoplasm. Although trauma is believed to be a factor in the development of IPEH, a history of trauma was elicited in only 4% of 314 cases in the literature.6 A history of trauma to the chest wall was not given by the patient in our case.
For this case, the initial diagnosis was drawn from the cytologic features suggesting an adenocarcinoma, such as pleomorphic large polygonal cell sheets, prominent nucleoli, abundant cytoplasm containing cytoplasmic vacuoles, and a history of subtotal gastrectomy due to gastric cancer. However, the cytologic diagnosis was falsely positive compared to the histologic diagnosis. On reviewing the cytologic slides of this case, there was lack of other features to support the diagnosis of adenocarcinoma, including absence of tumor necrosis, lack of coarse chromatin with nuclear hyperchromatism, no mitotic figures, and low nuclear: cytoplasm ratio. Although endothelial cells in IPEH resemble neoplastic epithelial cells, careful attention to fibrin materials, vasoformative structures, and hemorrhagic background could be helpful in diagnosing a vascular lesion on FNA.7,8 Furthermore, the tumor size did not change from the initial presentation 3 years prior, and the patient was otherwise doing well.
The cytologic features of IPEH in the published literature show diverse morphologies, leading to frequent diagnostic error.1-3,9,10 IPEH has been misdiagnosed as malignant vascular tumor, embryonal carcinoma, squamous cell carcinoma, adenoid cystic carcinoma, and giant cell tumor. Handa et al.10 suggested two types of cell populations that can assist in cytologic diagnosis of IPEH: spindle cells and round cells. The spindle cells in IPEH are scattered or tagged onto a capillary network and have fine granular chromatin, prominent nucleoli, and wispy cytoplasm. The round cells in IPEH are present around hyaline cores and have hyperchromatic nuclei and scant cytoplasm. Immunocytochemical stains for Factor VIII and CD31 can also added to the cytologic diagnosis of vascular lesion.
In conclusion, the cytologic features of IPEH are not specific, which often result in diagnostic challenges. However, it is important to suspect a vascular lesion when atypical cells are found in a hemorrhagic background. Furthermore, combination of cytologic features with immunocytochemistry will aid in a correct diagnosis of IPEH.
Notes
No potential conflict of interest relevant to this article was reported.