A Rare Case of Pulmonary Papillary Adenoma in Old Aged Woman: A Brief Case Report
Article information
Pulmonary papillary adenoma may be an unusual neoplasm of the lung. Since 1980 when Spencer et al.1 first described two cases of papillary adenoma of the lung, 23 cases have been reported worldwide including one case in Korea.2-4 Its rarity and shared histologic features of both benign and malignant tumors demand special attention for diagnosis, especially on the intraoperative consultation.2
Herein, we report a case of papillary adenoma of the lung that histologically mimicked a carcinoid tumor and review the histologic findings with differential diagnoses.
CASE REPORT
A 68-year-old female, who was undergoing preoperative evaluation for known rectal cancer, received percutaneous needle biopsy for a pulmonary nodule (Fig. 1A) and endobronchial sono-guided biopsy for enlarged mediastinal lymph nodes, which showed no evidence of metastasis. However, the core of the pulmonary nodule was composed of bland papillae-like structures lined with a single layer of uniform cuboidal cells, suspicious for carcinoid or low-grade epithelial neoplasm. On consideration of double primary pulmonary neoplasm, she received combined laparoscopic low anterior resection of the rectum and wedge resection of the left lobe of the lung.
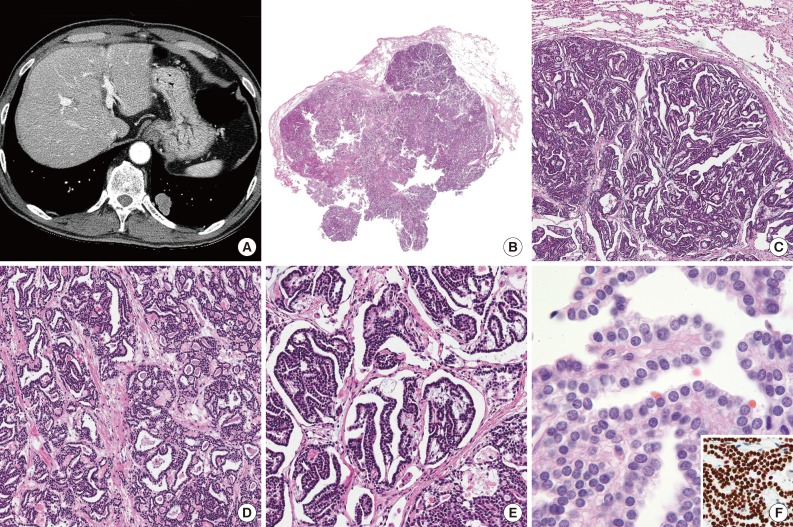
(A) Computed tomography of chest discloses a 25-mm-sized nodule in the left lower lobe, suggesting pulmonary metastasis from rectal cancer. (B) The mass is peripherally originated and well circumscribed. (C) The tumor shows a dominant papillary area and a focal microcystic area. (D) The microcystic area contains colloid- or amyloid-like eosinophilic material. (E) The papillae contain prominent or delicate fibrovascular cores and are lined with monotonous cuboidal cells. (F) Tumor cells contain ovoid, relatively uniform and centrally located nuclei showing a finely granular chromatin pattern with inconspicuous nucleoli. Positive nuclear staining for thyroid transcription factor-1 is noted (inset).
The resected specimen of lung contained a 2.5×1.5-cm-sized, peripherally located mass with a granular cut surface. At low power view, it is well demarcated without necrosis or hemorrhage (Fig. 1B). Microscopically, it showed dominant papillary architecture and focal microcystic area (Fig. 1C, D). The papillae contained prominent or delicate fibrovascular cores and were lined by monotonous cuboidal cells (Fig. 1E). The epithelial cells had moderate or small amount of cytoplasm and round, centrally located nuclei with inconspicuous nucleoli, and no nuclear atypia or mitosis was found (Fig. 1F). The chromatin was relatively uniformly distributed and finely granular, suspicious for neuroendocrine tumor. The microcystic area were lined with same epithelial cells and filled with amorphous eosinophilic material, similar to colloid or amyloid.
For the differential diagnoses with papillary adenoma of lung, metastatic follicular or medullary carcinoma of thyroid gland and less likely metastatic adenocarcinoma of rectum, immunohistochemical staining was performed. The tumor cells showed negativity for chromogranin (1:400, DAK-A3, Dako, Glostrup, Denmark), thyroglobulin (1:500, DAK-Tg6, Dako), calcitonin (1:4,000, Dako) and CDX-2 (1:50, AMT28, Novocastra, Newcastle upon Tyne, UK) and positivity for thyroid transcription factor-1 (1:100, 8G7G3/1, Dako) (Fig. 1F, inset). The eosinophilic material was negative by Congo-red stain and polarizing microscopy.
The patient was confirmed to have primary papillary adenoma of the lung and adenocarcinoma of the rectum (pT3N0Mx), and was discharged without any complications.
DISCUSSION
Papillary adenoma is a rare pulmonary neoplasm for which 23 cases (range of age, 7 to 66 years in English literature) have been reported to date. We add a case of papillary adenoma that occurred in a 68-year-old woman.
Although the present case seemed to be microscopically simple and uneventful, the rarity of the tumor and its uncommon finding at intraoperative consultation made it possible to be mistaken as malignancy, as we suggested primary or metastatic adenocarcinoma on frozen section due to solid area with mild atypia. Nakano et al.2 reviewed previously reported 16 cases and their one case of pulmonary papillary adenoma, which four cases of them had description of intraoperative consultation by the frozen section or imprint cytology. Only one case was diagnosed as papillary adenoma on frozen section, while the possibilities of malignancy were not excluded in other three cases. They also concluded that one of the diagnostic clues might be the macroscopic findings, in which the fresh tumor mass had a granular cut surface that became gradually obscure in shape and leaked out from the stump during manipulation of the frozen section.
The nuclear feature and monotonous appearance were sufficient to suggest carcinoid tumor as the first impression, after which repeated chromogranin stains for the biopsied and operated specimens were performed. Although carcinoid tumor also can show a papillary or follicular growth pattern, most of them grow in an organoid nesting or trabecular arrangement, and single-layered tumor cells regardless of growth pattern may be unusual in carcinoid tumor. On the review of cytological features of previously reported cases, two cases reported by Hegg et al.5 were described similar to present case, but no immunohistochemical study was performed. Although two cases reported by Dessy et al.6 included with chromogranin A and synaptophysin analysis and revealed negative results, those histologic findings were very different from our case, having no impression of carcinoid tumor. One case that was suspected to papillary adenoma with carcinoid-like feature was reported by Yamamoto et al.,7 in which peripherally-located papillary adenoma were histologically very similar to our case and showed negativity for chromogranin staining.
Metastatic thyroid cancer was also considered due to papillary or cyst-like structures lined by monotonous cuboidal cells resembling those of thyroid follicles and colloid-like material. However, the nuclear features are different from those of papillary thyroid carcinoma, and the results of immunohistochemical and Congo-red staining can exclude the possibilities of metastatic follicular or medullary carcinoma.
We previously experienced cases of fetal adenocarcinoma of the lung that showed irregularly-shaped tubules, papillary structure and a minute rosette-like growth pattern. However, they also showed pseudostratified lining epithelium, unlike the uniform single-layered epithelium of the present case.
Of benign pulmonary neoplasm, alveolar adenoma should be included in the differential diagnosis due to shared histologic findings with papillary adenoma. Alveolar adenoma can show a papillary structure, but it mainly consists of variable-sized cysts filled with proteinaceous material, variably thickened septa and a centrally located large cyst. Even though this case showed multiple small cysts, the predominant papillary structure and lack of spindle and inflammatory cells suggest papillary adenoma rather than alveolar adenoma.4 The peripheral type of glandular papilloma also can be considered due to papillary fronds, but its epithelial lining consists of a stratified columnar or cuboidal epithelium and mucous cells with varying proportion.8 This is distinct from our case that consisted of overall uniform cuboidal cells having centrally located bland nuclei.
Papillary adenoma of the lung is not often encountered, considering only one case report of pulmonary papillary adenoma in Korea.3 However, if we encounter such a case, it will be a difficult situation that asks pathologists many considerations, especially when the tumor shares carcinoid-like features or complicated clinical situation. Herein, we report a case of papillary adenoma of the lung, mimicking carcinoid tumor and neoplasm of thyroid gland.
Notes
No potential conflict of interest relevant to this article was reported.