Primary Extraskeletal Mesenchymal Chondrosarcoma of the Anterior Mediastinum
Article information
Primary extraskeletal mesenchymal chondrosarcoma (EMC) of the mediastinum is an extremely rare disease. To date, only seven cases have been reported in the literature 1-4 since it was first reported by Chetty in 1990.1 We experienced a case of primary mediastinal EMC presenting as an anterior mediastinal mass, a previously unreported site. Here, we describe the characteristic features of the lesion with a review of the literature to emphasize that EMC should be considered in the differential diagnosis of mediastinal tumors.
CASE REPORT
A 21-year-old woman visited an outside hospital with the chief complaint of intermittent chest discomfort and respiratory difficulty for 2 months. In the medical history, the patient had taken medication for schizophrenia for several years. On the chest computed tomography (CT) scan, the patient had a 13-cm heterogeneous enhancing mass with multifocal calcification in the anterior mediastinum that invaded the pericardium and was associated with massive left pleural effusion. The mass encased the aortic arch and branch along with the left and main pulmonary arteries, but did not appear to be originating from the osteocartilaginous structures of the thoracic region (Fig. 1A). The patient then underwent a CT-guided needle biopsy, for which a diagnosis of solitary fibrous tumor was suggested on a biopsy. Then, the patient was referred to the Dong-A University Medical Center to confirm the diagnosis and undergo further treatment. Although the tumor could not be resected completely due to the extensive invasion into the main vessels, a surgical excision of the mass along with wedge resection of the left upper lung and partial resection of the pericardium was performed. The tumor at the time of surgery was found to invade the pericardium and to be tightly adhered to the left upper lung. However, it could be easily separated from the adjacent ribs. The resected tumor, measuring 13×7.5 cm, was solid, lobulated, and partially covered by a thin fibrous capsule. On the cut section, the tumor was tan white, and soft to fish-flesh, while the lobulated cut surface exhibited focal areas of irregularly sized glistening cartilage and coarse calcification (Fig. 1B). Microscopically, the lesion was composed of a highly cellular proliferation of undifferentiated round, oval, or spindle-shaped cells with an abrupt transition with small islands of well-differentiated hyaline cartilage, frequently associated with central calcification and ossification (Fig. 2A). In some areas, the undifferentiated cells were separated by branching, sinusoidal vascular channels imparting the lesion with a hemangiopericytoma-like pattern (Fig. 2B). Immunohistochemically, the cartilaginous portion of the tumor showed S100 protein positivity, but the undifferentiated cells showed negative immunoreactivity for the S100 protein (Fig. 2C). Undifferentiated cells showed strong membranous immunoreactivity for CD99, whereas only isolated cells in the cartilaginous portion stained for CD99 (Fig. 2D). The tumor cells exhibited negative immunoreactivities for cytokeratin and CD34. The patient made an uneventful postoperative recovery and was discharged on postoperative day 5 with advice to undergo chemotherapy and local radiotherapy. However, the patient refused any further treatment. The patient is still alive with a residual tumor at the time of writing this report (8 months postoperatively).
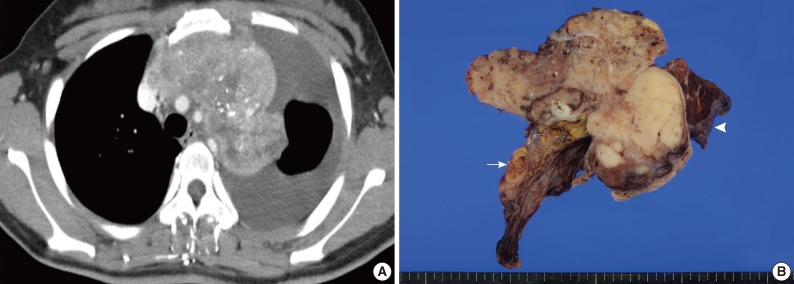
Radiologic and gross findings. (A) The chest computed tomography shows a huge, heterogeneous enhancing mass with multifocal calcifications in the anterior mediastinum, which invades the pericardium and is associated with massive left pleural effusion. (B) The resected tumor, measuring 13×7.5 cm, is tan white, soft to fish-flesh, and lobulated, showing focal areas of cartilage and calcification on the cut surface. The tumor invades the attached pericardium (arrow), but the wedge resected lung exhibits no tumor invasion (arrowhead).
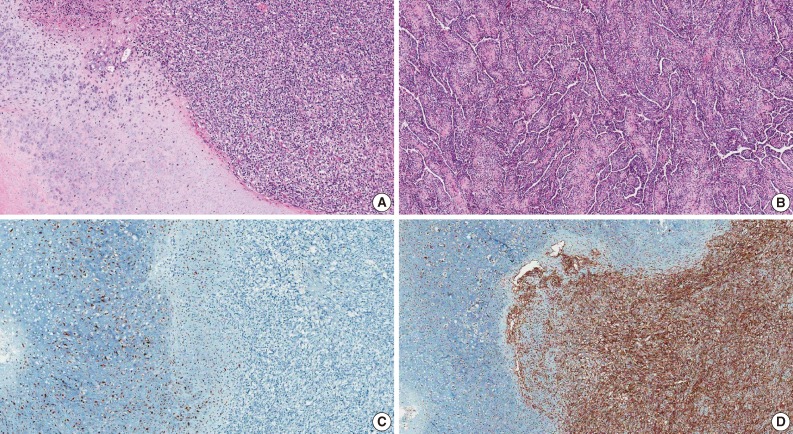
Microscopic and immunohistochemical findings. (A) The tumor is composed of a highly cellular proliferation of undifferentiated round, oval, or spindle-shaped cells with an abrupt transition with small islands of well-differentiated hyaline cartilage. (B) In some areas, the undifferentiated cells are separated by branching, sinusoidal vascular channels imparting the lesion with a hemangiopericytoma-like pattern. (C) The cartilaginous portion of the tumor shows positive immunoreactivity for the S100 protein, but the undifferentiated cells show a negative immunoreactivity for the S100 protein. (D) The undifferentiated cells exhibit strong membranous immunoreactivity for CD99, whereas only the isolated cells in the cartilaginous portion of the tumor stain for CD99.
DISCUSSION
To date, a total of 11 cases of primary chondrosarcoma of the mediastinum have been reported in the literature. However, 10 cases were found in PubMed and KoreaMed searches of English- and Korean-language articles.1-5 Among the 10 cases, seven cases have presented as EMC and the remaining two had the conventional type with one having the myxoid type. The clinicopathologic features of the seven patients with EMC reported in the literature are summarized in Table 1. The patient in our case report presented with the largest tumor mass (13 cm). Of note, all the tumors except our case have been reported to involve the posterior mediastinum. To our knowledge, this is the first case report of EMC involving the anterior mediastinum.

Primary mediastinal extraskeletal mesenchymal chondrosarcomas: literature summary of the clinicopathologic features
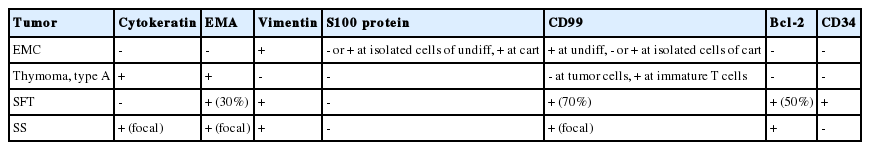
Due to an exceedingly rare incidence of EMC presented as mediastinal tumors, the diagnosis of this tumor may be difficult with small biopsy or needle biopsy specimens that demonstrate only one of the two tissue elements. In particular, tumors having a hemangiopericytoma-like pattern without the cartilaginous elements may be mistaken for other tumors having a hemangiopericytoma-like pattern occurring in the anterior mediastinum, such as type A thymoma, solitary fibrous tumor, and synovial sarcoma, as a solitary fibrous tumor was suggested for the diagnosis of this case upon biopsy from an outside hospital. Immunohistochemistry may play an important role in the differential diagnosis of these tumors (Table 2). Although the preoperative diagnosis of EMC is difficult and the incidence is exceedingly rare, it has to be distinguished for the differential diagnosis among the list of anterior mediastinal tumors.
Notes
No potential conflict of interest relevant to this article was reported.