Multicystic Biliary Hamartoma of the Liver
Article information
Abstract
Multicystic biliary hamartoma (MCBH) is a very rare hamartomatous cystic nodule of the liver, which has recently been described as a new entity of a hepatic nodular lesion. We report a unique case of MCBH with a review of the literatures. A hepatic multicystic mass of segment 3 was detected in a 52-year-old male by abdominal computed tomography, and resection of this lesion was performed. Macroscopic examination revealed a 2.7×2.0 cm nodular mass with a multicystic honeycomb cut surface. Histologically, this lesion consisted of multiple dilated cystic ducts lined by biliary type epithelial cells, periductal glands and connective tissue, which included small amounts of hepatic parenchyma and blood vessels. Recognition of this unusual lesion is essential to avoid confusion with other cystic tumors of the liver, and to learn more about its natural history and response to treatment.
Diagnosis of small cystic lesions of the liver has become more frequent during the past several decades due to technological progress and increased use of various imaging modalities. Recently, a hitherto undescribed hamartomatous cystic lesion was termed a multicystic biliary hamartoma (MCBH).1 Clinically and radiologically, MCBH can be difficult to distinguish from other cystic lesions of the liver, including malignant cystic tumors. Presently, we described a case of MCBH and included a review of the literature. To our knowledge, only eight cases have been reported in the English literature, and this is the first reported case in Korea.1-4
CASE REPORT
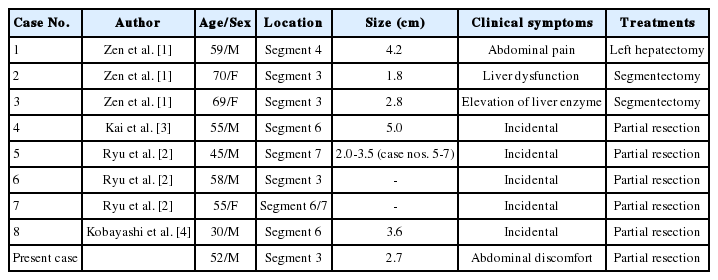
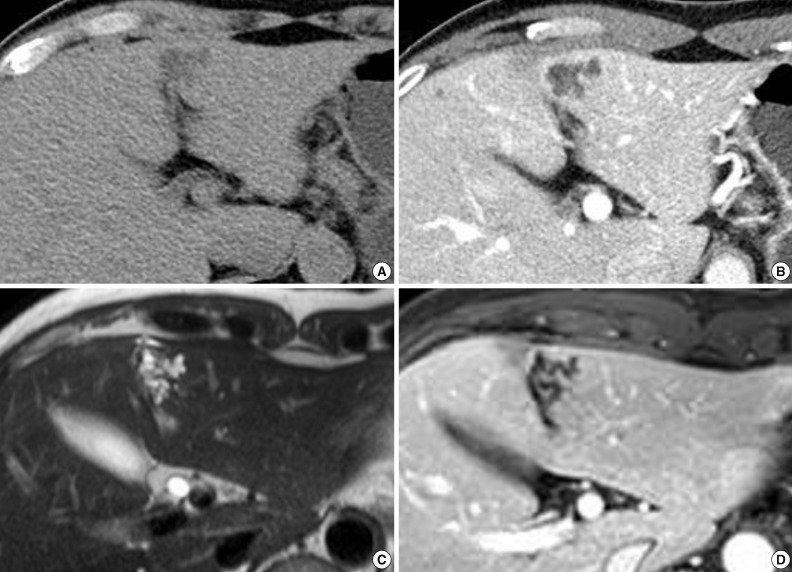
A 52-year-old male patient was referred to our hospital on February 12, 2012 with a complaint of abdominal discomfort. The physical examination of the patient was unremarkable. The serum levels for alanine aminotransferase (21 IU/L; normal range, 5 to 35 IU/L) and aspartate aminotransferase (23 IU/L; normal range, 12 to 33 IU/L) were normal. Tumor markers (alpha-fetoprotein, carcinoembryonic antigen, and carbohydrate antigen 19-9) were within normal limits. Serological tests for hepatitis B and hepatitis C were negative. All other parameters were normal. An abdominal computed tomography (CT) scan demonstrated an irregularly-shaped low-density lesion measuring 2.7 cm in diameter in segment 3 of the left lobe just beneath the hepatic capsule (Fig. 1A). This lesion was slightly enhanced after contrast medium injection and revealed a multicystic appearance in the portal phase (Fig. 1B). Abdominal magnetic resonance imaging (MRI) more clearly depicted the multicystic nodule in segment 3 of the liver. On T2-weighted MRI, conglomerated multiple cystic nodules with a high signal intensity were seen (Fig. 1C). Thin septae and the wall of the lesion were enhanced on contrast-enhanced, T1-weighted MRI (Fig. 1D). Surgical exploration revealed a 2.7×2.0 cm, relatively well-demarcated nodular mass. The cut surface had a multicystic honeycomb appearance that was composed of a number of cystically dilated ductal structures embedded in the fibrous tissue (Fig. 2A). Histologically, this lesion consisted of dilated cystic ducts, periductal glands and connective tissue, which included small amounts of hepatic parenchyma and blood vessels. Bile materials were observed in some of the cystic ducts (Fig. 2B, C). The ducts were lined by a monolayer of low columnar or cuboidal epithelial cells (Fig. 2D). There was no ovarian-like stroma. No mitotic figures were observed in the epithelial cells, and there was no evidence of pleomorphism or nuclear atypia suggesting malignant tumor. Immunohistochemical stainings for mucin core protein (Muc) 1, Muc2, Muc5Ac, Muc6, and biliary type keratin (K) 7 and, K19 were performed. Similar to previous findings,1,3 the duct-lining epithelial cells were diffusely positive for K7, K19 and showed focal Muc1 expression, whereas they were negative for Muc2, Muc5Ac, and Muc6 (Fig. 2D). On the basis of these histologic and immunohistochemical findings, a final diagnosis of MCBH was made.
Images of the hepatic lesion. (A) Precontrast computed tomography (CT) reveals an irregularly-shaped low-density lesion in segment 3 of the liver. (B) Portal phase CT demonstrats a multicystic lesion with thin enhancing septae. (C) T2-weighted turbo spin echo magnetic resonance imaging (MRI) (TR/TE; 911.8/80.0) shows a honeycomb-like lesion with a bright high signal intensity. (D) Contrast-enhanced T1-weighted MRI (TR/TE; 3.1/1.5) demonstrates thin enhancing septae without any enhancing solid portions.
Pathologic findings of the present case. (A) The cut surface of the cystic mass reveals a multicystic honeycomb appearance composed of many small cystic ductal structures. (B) Microscopically, this cystic nodule contains cystic ducts, periductal glands, and connective tissue. (C) Hepatic parenchyma is observed in the fibrous connective tissue between the cystic ducts. (D) These ducts are lined by a monolayer of cuboidal epithelial cells. Positive keratin 19 immunohistochemical staining of the lining epithelial cells and periductal glands (inset) are also noted.
DISCUSSION
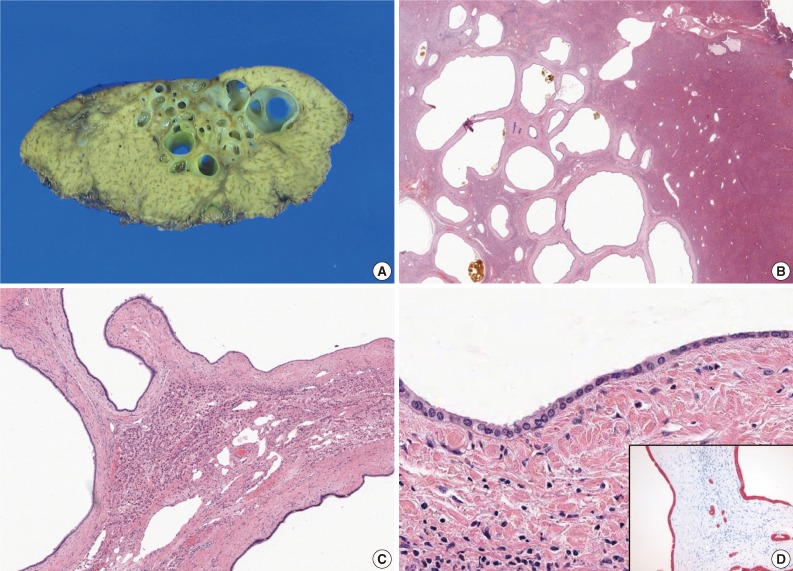
MCBH is a rare cystic disease of the liver.1 Since the first description of MCBH in 2006, there have only been a eight published cases worldwide.1-4 These publications are shown in Table 1. The reported mean age at the presentation of the disease was 55±12 years (n=9), with a range from 30-70 years. The disease is twice more common in males than in females, with a male-to-female ratio of 6:3. The majority of patients are asymptomatic, and the cyst is found incidentally and most commonly in segment 3 in the left lobe and in segment 6 in the right lobe just beneath the hepatic capsule. The average size of the six lesions for which data are available was 3.35±1.15 cm (n=6) in the greatest dimension (range, 1.8 to 5 cm). The exact size was not reported in three patients. The pathogenesis of MCBH is not clear. Zen et al.1 proposed that MCBHs might be related to developmental abnormalities of the biliary tract or embryonic foregut.
On ultrasonography, the most consistent findings in MCBHs are a conglomerate of hypoechoic irregular masses with hyperechoic cystic walls.2 CT usually displays these lesions at as low density with enhancing septae, as in our case. On MRI, MCBHs are hypointense on T1-weighted imaging. T2-weighted imaging reveals a multicystic, honeycomb-like lesion with bright, high signal intensity. Although most MCBHs have some typical imaging features, radiology alone is non-diagnostic. The radiologic features of biliary mucinous cystic neoplasm, echinococcosis, and hepatic lymphangioma resemble those of MCBH.2
The key histological features of MCBH include the following: location around the hepatic capsule close to the fissure of the falciform ligament; protrusion from the liver; composition of ductal structures, periductal glands, and fibrous connective tissue; presence of bile-like materials in the ducts; and positivity for biliary type keratins on the cyst lining-epithelium.1 All these features, except for liver protrusion, were observed in the present case; five of the eight previously reported MCBHs also did not protrude from the liver.1-4 Previous reports additionally showed that MCBH occurs not only on the liver's surface but also in the intrahepatic portion.3 Therefore, we ultimately diagnosed this lesion as MCBH. Histologically, the differential diagnoses of MCBH included ciliated hepatic foregut cyst (CHFC), Caroli's disease, mucinous cystic neoplasm, and von Meyenburg's complex (biliary microhamartoma). The histological features of CHFC are the presence of a four-layered cyst wall, which consists of a mostly inner lining of pseudostratified ciliated columnar epithelium followed by a layer of loose subepithelial connective tissue, a smooth muscle layer and an outer layer of dense fibrous tissue.5 No characteristic pathological features of CHFC, such as ciliated cells and a smooth muscle layer were observed in the present case. Caroli's disease is characterized by segmental or multiple dilatations of the intrahepatic ducts. Ductal structures in Caroli's disease are cystically dilated preexisting bile ducts, whereas ducts in MCBH derive from hamartomaous or abnormal ducts.6 Moreover, Caroli's disease is often accompanied by congenital hepatic fibrosis. Mucinous cystic neoplasm should always be included in the differential diagnosis, because mucinous cystic neoplasm is a true neoplasm with the potential for progression to biliary cystadenocarcinoma. The presence of ovarian-like stroma in addition to mucinous lining epithelium in the wall of the cyst defines the mucinous cystic neoplasm.7 We excluded mucinous cystic neoplasm because there was no ovarian-like stroma or mucinous cells, which are necessary for the diagnosis of mucinous cystic neoplasm. Biliary microhamartomas appear as a focal disorderly collection of bile ducts and ductules surrounded by abundant fibrous stoma. They are usually multiple and located adjacent to a portal region.8 Contrary to the relatively larger size of MCBH (1.8-5.0 cm),1-4 biliary microhamartomas usually range from 2 to 5 mm in diameter.8
The clinical course of MCBH is benign.1-4 After three months of follow-up, the patient is in good health without any evidence of recurrence. Because only a small number of cases have been documented in the literature, it is essential to be able to recognize MCBH to learn more about its natural history and response to treatment.
Acknowledgments
This work was supported by the National Research Foundation of Korea Grant funded by the Korean Government (No. 2012-0009320).
Notes
No potential conflict of interest relevant to this article was reported.