Actinomycotic Brain Abscess Developed 10 Years after Head Trauma
Article information
Actinomyces species are members of the endogenous flora of mucous membranes, and are frequently cultured from the gastrointestinal tract, bronchi, and female genital tract. Infections due to Actinomyces are usually associated with the breakdown of normal physical barriers, such as disruption of mucosal membranes in the mouth and gastrointestinal tract. The major sites of actinomycoses are cervicofacial, abdominopelvic, and thoracic sites, where it usually presents with the development of an abscess, a draining sinus tract, fistulae, and tissue fibrosis.1 Less common sites of actinomycotic infection include the central nervous system (CNS) and musculoskeletal soft tissue. In Korea, only two cases of CNS actinomycoses have been reported.2,3 Herein, we report a rare case of CNS actinomycosis that caused a cerebral abscess.
CASE REPORT
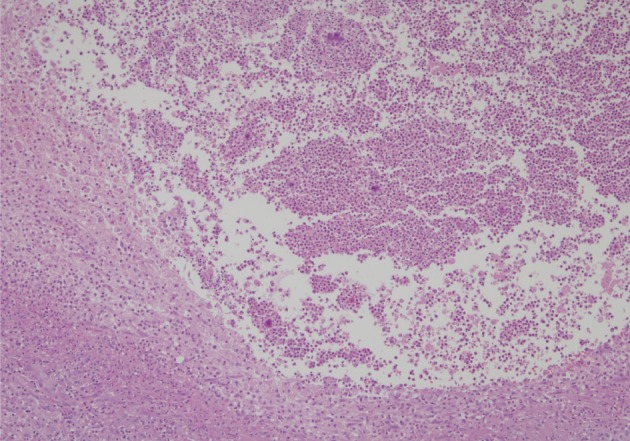
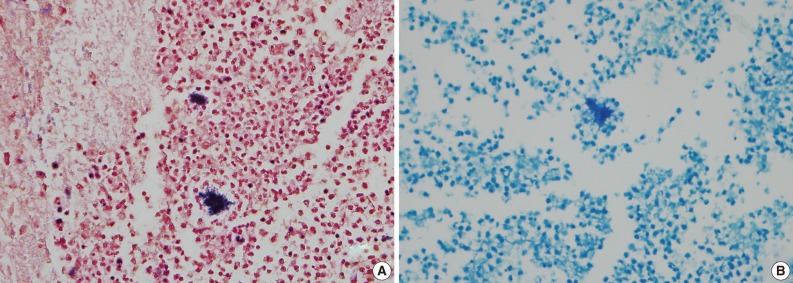
A healthy 45-year-old man presented with 3 days of left-sided weakness, left-sided facial palsy, and dysarthria. His medical history was remarkable for a laceration head injury 10 years prior. He received a surgical suture and was admitted to the intensive care unit because mild intracranial hemorrhage was identified. He recovered with conservative management and the injury did not leave any neurologic sequelae. The patient and his family denied having any history of heavy alcohol consumption, dental carries, cancer, diabetes mellitus, or surgery on orofacial, thoracic, or abdominal areas. Physical examination revealed that the patient was drowsy but well oriented and afebrile. Laboratory examinations showed a white blood cell count of 9,900/mm3 with a differential count of 68% segmented cells and 23% lymphocytes. The erythrocyte sedimentation rate was 18 mm/hr and the C-reactive protein was 0.3 mg/dL. The initial non-enhanced brain computed tomography demonstrated a 3.5×2.5 cm irregular mass in the right frontal lobe with severe perilesional edema. Brain magnetic resonance imaging showed that the lesion was hypointense on a T1-weighted image and hyperintense on a T2-weighted image, with thick and irregular ring-like enhancement. A diffusion weighted image demonstrated high signal intensity, reflecting restricted diffusion (Fig. 1). For a definite diagnosis and treatment, the patient underwent open surgery and the mass was excised along with surrounding brain parenchyma. Grossly, the specimen included an abscess cavity containing yellowish green pus, surrounded by a thick fibrous capsule. Histological examination showed multiple filamentous organisms appearing as radiating rosettes in the central areas of the abscess (Fig. 2). These structures stained positively with periodic acid-Schiff, Grocott's methenamine silver, Gram stain, and negative with acid-fast stain (Fig. 3). These findings were consistent with the sulfur granules of actinomycoses.4 After the operation, the patient recovered consciousness and 4 weeks of intravenous ampicillin therapy was started (12 g/day). Streptococcus viridans was isolated from the infected brain during antibiotic treatment. However, Actinomyces species were not isolated, despite prolonged culture. The patient was discharged with a good outcome after 4 weeks and continued with 4 months of oral administration of ampicillin.
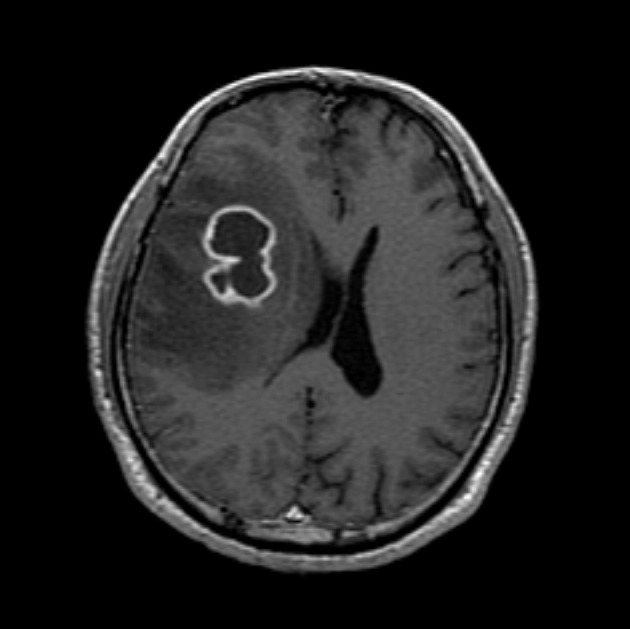
Magnetic resonance imaging of the brain. Gadolinium-enhanced T1-weighted images show a ring-like enhancing lesion in the right frontal lobe.
DISCUSSION
In 1937, Frideman and Levy conducted a review of CNS actinomycoses by collecting 108 cases reported in the literature.5 However, as nocardiosis has been a recognized medical condition, many cases in Frideman and Levy's report5 were later considered to be nocardioses. Bolton and Ashenhurst6 described 17 cases of CNS actinomycoses. In addition, Smego7 performed a comprehensive analysis by collecting 70 cases of newly reported CNS actinomycoses and describing its main features. CNS actinomycoses have been reported to account for 1-15% of actinomycotic infections. A cerebral abscess is the most common presentation and typically appears as a single or multiple lesions involving the frontal or temporal lobe. In addition, CNS actinomycoses can present subdurally or epidurally. Common clinical manifestations are focal neurologic signs, headache, seizure, and diplopia. High fever and intracranial hypertension are not typical. The mean duration of symptoms prior to diagnosis is >2 months, which is longer than most causes of pyogeneic CNS infections. Most CNS actinomycoses are monomicrobial, although multiple organisms may be seen, which include Aggregatibacter, Capnocytophaga, Fusobacterium, Haemophilus, Staphylococcus, and Streptococcus species.6,7 These pathogens are believed to facilitate actinomycotic infection by inhibiting host defenses and establishing a microaerophilic environment.8
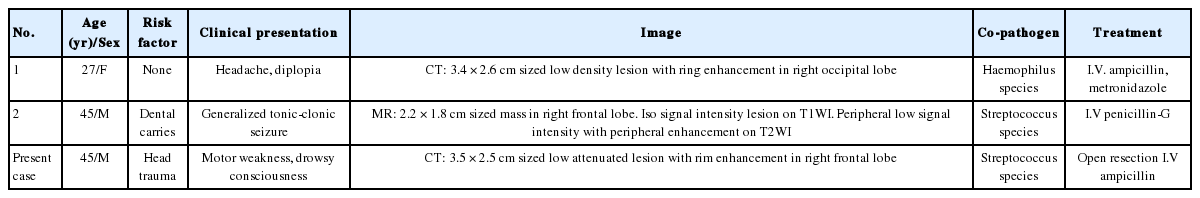
Table 1 summarizes the features of CNS actinomycoses in Korea. Among them, one was found to be a cerebral abscess in a patient with 2 weeks of headache and diplopia, and another in a patient with a recent seizure episode. In these cases, Haemophilus and Streptococcus species were found coinfecting the patient.2,3 The clinical features of CNS actinomycoses in Korea, including the presenting case, seem to be typical.
Predisposing conditions for CNS actinomycoses include dental infections, manipulations, oromaxillofacial trauma, gastrointestinal surgery, and the use of an intrauterine device. Less commonly, CNS actinomycoses develop in immunocompromised patients who have diabetes mellitus, neoplasm, or heavy alcohol consumption. These conditions are frequently associated with impairment of local defense barriers. Endogenous infection occurs when organisms enter into damaged tissue. CNS infection can result by direct extension or hematogenous spread from a primary focus. Although primary CNS actinomycoses have been suggested, it is more widely accepted that such cases should be classified as isolated CNS actinomycoses from an unknown primary focus.1,7 In this presenting case, the patient did not have any predisposing factors except for a history of a surgical procedure for a laceration head injury ten years earlier. CNS actinomycoses have been previously reported developing 8, 10, and 22 years after a surgical procedure for a penetrating head injury.4,8 The precise primary sites of infection in these cases are not well defined, however, past head trauma or surgical procedures might contribute to the development of CNS actinomycoses. Makhija et al.9 reported acute exacerbation of actinomycoses in a patient who had a windshield forehead injury. At the time of trauma, the lesion remained painless with only mild swelling, but the lesion increased and became tender with additional trauma after 16 years. It was speculated that actinomycotic implantation might have occurred at the time of initial trauma and the organism was in a chronic and slowly progressive phase, and later transformed from dormancy to produce acute actinomycoses after physical stimulation.9 This theory may be a possible explanation for the development of actinomycotic cerebral abscess an extended period of time after head injury.
A definite diagnosis of actinomycoses is established by isolation of an actinomyces species in cultures. However, the cultures are negative in up to 70% of cases. Detection of sulfur granules on histological examination is a pathognomic clue to diagnosis. Sulfur granules are clusters of organisms that appear as round or oval basophilic masses with eosinophilic projections on hematoxylin and eosin staining.10 The differential diagnosis should include nocardiosis, which also can form sulfur granules and cause similar clinical syndromes involving the lungs, bones, joints, soft tissue, and the CNS. It is critical to distinguish between these two types of organisms because they respond differently to antibiotics. Microbiologically, Nocardia species are Gram-positive, acid-fast organisms with aerobic requirements, whereas Actinomycetes are Gram-positive, non-acid-fast organisms with anaerobic or microaerophilic requirements.1 Diagnosis of the presenting case was made by the detection of Gram-positive and acid-fast negative sulfur granules.
In conclusion, we report a cerebral actinomycotic abscess in a patient presenting with motor weakness, which developed 10 years after laceration head trauma. Although CNS actinomycoses are rare, they should be considered causes of cerebral abscess if the patient has the associated risk factors.
Notes
No potential conflict of interest relevant to this article was reported.