Benign Triton Tumor: A Rare Entity in Head and Neck Region
Article information
Abstract
Benign triton tumors (BTT) are very rare lesions composed of mature skeletal muscle and neural tissue. We report a case of a 14-year-old boy who presented with asymptomatic swelling of the chin over an 18-month duration which increased gradually to involve the left side of the lower lip. Clinically, a diagnosis of neurofibroma was made. Excisional biopsy confirmed the diagnosis of a BTT. Having an affinity for large nerve trunks like the brachial and sciatic, these tumors rarely occur in the head and neck region. When they do, they may involve the large central cranial nerve trunk and present as intracranial masses or involve the smaller peripheral nerve twigs and present as asymptomatic skin nodules, of which only four cases involving peripheral nerves are reported in the English literature. Here, we report the fifth documented case of a BTT involving the mental branch of the trigeminal nerve. A brief review of the literature is also provided.
Benign triton tumors (BTTs) are rare tumors composed of mature neural and skeletal muscle tissue.1 Regarded as neuromuscular hamartomas or choristomas, the most common site of predilection includes the large peripheral nerve trunks like the brachial and sciatic.2,3 Very rarely, these tumors have been reported to occur in the head and neck region, arising either in the large central cranial nerves or the smaller peripheral nerve twigs. An extensive review of the literature revealed only four cases of BTT involving peripheral nerves of the head and neck.2-5 We also report an additional case of BTT of the head and neck region involving the mental branch of the trigeminal nerve.
CASE REPORT
A 14-year-old boy presented with asymptomatic swelling of the chin that had been occurring over 18 months. The lesion gradually increased to involve the left side of the lower lip. There was no history of similar lesions elsewhere in the patient or his family members. There was no history of pain, alteration in speech or difficulty in speaking.
On examination, there was a skin colored, non-tender, firm and irregular swelling over the left mentolabial groove extending onto the lower lip (Fig. 1). There was bulging of the left part of the lower lip with distortion of the lip architecture even on occlusion of the lips. The mass produced an irregular, smooth protrusion on the mucosal surface of the lower lip without any discoloration. There was no local depigmentation or hypertrichosis. There was no evidence of freckles or café au lait macules and no bruit over the lesion. Clinically a diagnosis of neurofibroma was made and excisional biopsy under local anesthesia and aseptic conditions was performed. The specimen was sent for histopathological examination.
Gross observation showed that the tumor consisted of a skin covered nodule measuring 1×0.5×0.5 cm. The cut surface was solid grey white. Histopathology sections showed an unremarkable superficial skin and a sub-epithelial tumor. The tumor was ill defined and consisted of fascicles of mature nerve tissue arranged in a multinodular pattern separated by fibrocollagenous septa. The cells were seen surrounding the pilosebaceous unit. The nerve fascicles showed an intricate admixture, with mature striated skeletal muscle bundles of varying sizes ranging from 15 to 20 µm with some being up to 50 µm (Figs. 2, 3). Few muscle fibers were seen to be contained within the perineural sheath (Fig. 3B). Areas of myxoid change were noted as were many capillary sized blood vessels. Mild chronic inflammation was seen. A histopathology diagnosis of BTT involving the mental branch of the trigeminal nerve was made. There was no evidence of any neurologic dysfunction 8 months after the surgery.
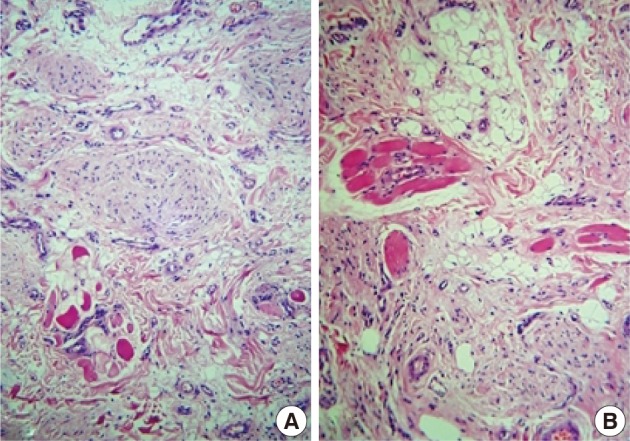
Microphotograph showing neural tissue arranged in nodular aggregates admixed with mature skeletal muscle fibers (A). Mature neural tissue in sheets along with skeletal muscle fibers (B).
DISCUSSION
A wide variety of benign soft tissue tumors occur in the head and neck region. These include tumors arising from adipocytes, fibrohistiocytes, as well as vascular and neural tissue. The latter include neurofibroma, schwannoma, neuromas and other uncommon tumors like meningioma, granular cell tumor, ganglioneuroma, and very rarely, neuromuscular hamartoma or triton tumors.1,6
Triton tumors are neoplasms composed of neural and skeletal muscle cells of which fewer than 20 cases have been reported in the English language literature.4 The name triton has been derived from the amphibian triton salamander, in which the normal nerve was believed to induce regeneration of skeleton muscle.7 Tumors included under these categories are BTT, neurofibroma with rhabdomyomatous differentiation, medulloblastoma with rhabdomyosarcoma elements, rhabdomyosarcoma with ganglion cells (ectomesenchymoma) and malignant peripheral nerve sheath tumor with rhabdomyosarcoma, the latter being the most commonly recognized entity.1
BTTs commonly occur in infants and children, though it has been rarely reported in adults.2,8 The most common sites of predilection are the large peripheral nerves, especially the brachial and sciatic nerves.1 Very rarely have these cases been reported in the head and neck region.2-5 BTTs of the head and neck fall into two categories. First, are the aggressive central types involving large cranial nerve trunks (V, VII, and XII) with occasional aggressive behavior. These cases usually affect infants and children. The other variant is the nonaggressive peripheral type which presents as asymptomatic slow growing skin nodules and is known to occur in adults.5 In the peripheral category, only four cases have been reported including two cases occurring in the tongue, both affecting adults.2,5 Two other cases were in a 3-month-old infant in the submandibular skin and a 17-year-old female in the left chin.3,4 All four of these cases in the peripheral category were cured by simple surgical excision except in one case report by Demir et al.,4 which had a local recurrence. Our case belongs to the peripheral type, involving the mental nerve, which is the terminal branch of the inferior alveolar branch of the trigeminal nerve.
Though the histogenesis of these unusual tumors has initiated much discussion, the exact mechanism is not known. Some authors believe that the cell lines are derived from primitive neural crest cells, while others consider it to represent a muscle spindle. Recently, Daley et al.5 put forth an alternative theory that an epigenetic or sporadic alteration of the motor end-plate leads to reactive proliferation of neural and skeletal muscle tissue in an organoid pattern.1
Clinically, patients are usually asymptomatic, except for the presence of a palpable mass, which may be solitary or multinodular. However, depending on the site of involvement, pain, neurologic dysfunction in the form of muscle weakness, parasthesia and headache including oculomotor ophthalmoplegic migraine, has been reported.6,8,9 Computed tomography scans provide a good guide to suggest the diagnosis and serve to define the entire scope of the lesion, especially in the central type of tumors.6
Due to the rarity of these lesions, clinical diagnosis is difficult and histopathology is required. Histopathologically these tumors are multinodular, subdivided by collagenous connective tissue into smaller nodules and fascicles. The fascicles are comprised of mature striated muscle fibers intimately associated with nerve fibers and enclosed within the same perimysial-like fibrous sheath. Sometimes the fibrous tissue predominates, rendering the diagnosis difficult.7
Treatment involves excision which is usually more aggressive in cases of the central type and conservative for the peripheral tumors. Even incomplete resection was found to ameliorate symptoms. Post-resection nerve palsies are always a risk, and hence, nerve sparing is advocated.1,5,7,10 Though prognosis is excellent, recurrence has been reported rarely, which mandates follow-up.4
An important generalization to bear in mind is that, though rare, BTTs should be considered in the differential diagnosis of head and neck tumors. Since treatment of some of these tumors results in residual nerve dysfunction on attempted surgical resection, while others spontaneously regress, recognition of this entity is important for planning appropriate treatment.
Notes
No potential conflict of interest relevant to this article was reported.

