Pulmonary Calciphylaxis Associated with Acute Respiratory and Renal Failure Due to Cryptogenic Hypercalcemia: An Autopsy Case Report
Article information
Abstract
Metastatic calcification is rare; it is found during autopsy in patients who underwent hemodialysis. Diffuse calcium precipitation of small and medium-sized cutaneous vessels, known as calciphylaxis, can result in progressive tissue necrosis secondary to vascular calcification. This condition most commonly involves the skin; however, a rare occurrence of visceral calciphylaxis has been reported. Here we report on an autopsy case. Despite a thorough evaluation, and even performing an autopsy, the underlying cause of acute-onset hypercalcemia, resulting in the production of pulmonary calciphylaxis and metastatic renal calcification associated with acute respiratory and renal failure, could not be determined. Metastatic calcification often lacks specific symptoms, and the degree of calcification is a marker of the severity and chronicity of the disease. This unusual autopsy case emphasizes the importance of rapidly progressing visceral calciphylaxis, as well as its early detection.
Calciphylaxis, also called uremic calcific arteriolopathy, is a rare life-threatening entity of progressive cutaneous necrosis secondary to calcification of small and medium-sized blood vessels, which shows rapid development.1,2 Calciphylaxis has been regarded as a systemic disease involving mainly the skin, subcutaneous fat, or muscle; however, a rare occurrence of calciphylaxis of other organs has been reported.3
Here, we report on a rare autopsy case involving a massive visceral and cutaneous calciphylaxis due to cryptogenic hypercalcemia, along with a discussion of the undetermined pathogenesis of the calciphylaxis.
CASE REPORT
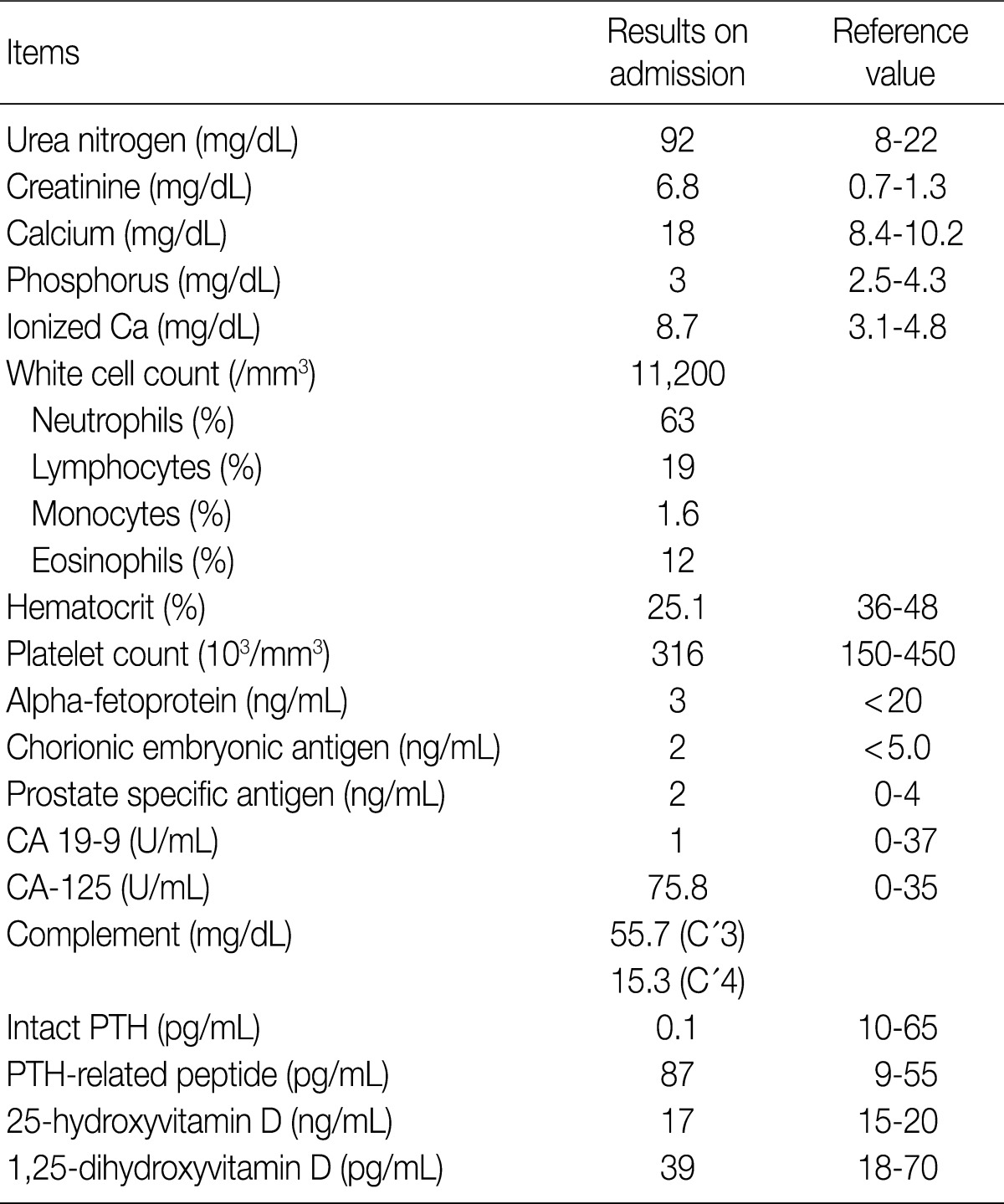
A 40-year-old male patient was transferred to our hospital due to acute renal failure and hypercalcemia. Except for the eight weeks prior to admission, the patient had a history of good health. First, mild fever and generalized myalgia developed, and he was then admitted to a local general hospital with a drowsy mentality approximately two weeks later. With the impression of acute respiratory distress syndrome, support from a mechanical ventilator was administered immediately. The blood chemistry showed increased levels of urea nitrogen, creatinine, calcium, and ionized calcium in the serum. Increased levels of carbohydrate antigen 125 (CA-125) and parathyroid hormone (PTH)-related peptide were also observed. Other laboratory findings are shown in Table 1. Emergent hemodialysis was performed and pamidronate was administered for treatment of the hypercalcemia. Physical examination showed multiple scattered, violaceous, ulcerative, cutaneous lesions on both limbs, and no palpable lymph nodes were observed. High resolution chest computed tomography indicated diffuse ground-glass attenuation and calcified consolidation in both lungs, with diffuse thickening of bronchovascular bundles and pleural effusion. Computed tomography of the abdomen, brain, and spinal cord showed no evidence of tumors. Results of a bone marrow study showed normocellular marrow with trilineage hematopoiesis. Growth of a methicillin-resistant Staphylococcus aureus was observed on the sputum culture. Despite treatment with hydration, intravenous administration of furosemide and salcatonin, the serum calcium level showed a progressive increase, up to 17.4 mg/dL, and the patient went into cardiac arrest on the 40th hospital day. Cardiopulmonary resuscitation failed. A limited autopsy, except on the brain and spinal cord, was performed.
Pathologic findings
On opening of the thorax, a bilateral brownish pleural effusion of 300 mL was observed, and clear effusion of 100 mL was present in the pericardial sac. The thyroid gland and all of the four parathyroid glands were found to be normal and not enlarged. Enlarged mediastinal lymph nodes and periaortic lymph nodes were observed, with conglomeration up to 10 mm. The cut surfaces of the bilateral lungs were found to be heavy, firm, and brittle (Fig. 1A). On opening of the peritoneal cavity, accumulated brownish ascites was observed. The mesenteric vessels were firm, and luminal calcification was observed on the cut surface. Coarse, thin bone marrow was taken from the iliac wing. The cut surface of the bilateral kidneys was brittle and showed no demonstrable hemorrhage or necrosis. Careful examination of the pelvic and abdominal cavity, including the gastrointestinal tract, found no gross abnormalities.
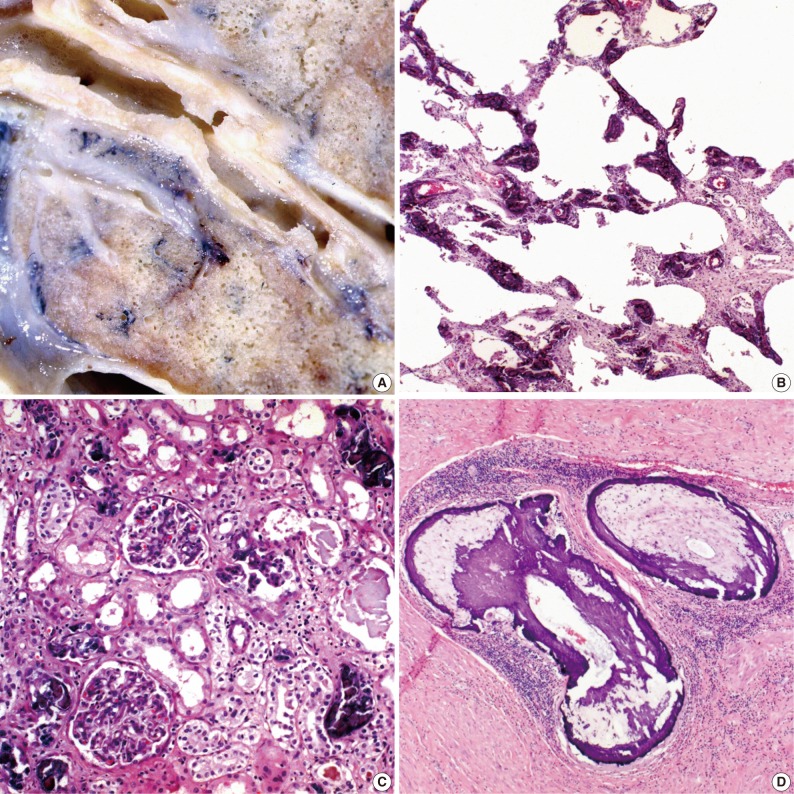
(A) Gross photography of a dissected right lung shows a firm, brittle, gray-tan, chalky appearance. (B) The lung shows marked fibrous thickening of the alveolar wall and calcium deposition. (C) The kidney shows diffuse calcific deposits in the glomeruli and interstitial spaces. (D) The epidermis and dermis are totally necrotic due to occlusion of the thrombotic small cutaneous vessels by calcification.
Histologically, near complete destruction of the pulmonary architecture caused by calcium deposits (Fig. 1B), which were stained using a von-Kossa stain, was observed. Calcification was observed in the alveolar septa, bronchus, bronchioles, and blood vessels. Diffuse calcific deposits, mainly in the glomeruli and interstitial spaces, were observed in the parenchyma of the kidney (Fig. 1C). The skin necropsied from the violaceous extremity was characterized by total epidermal necrosis and calcification (calciphylaxis) was observed in small and medium-sized cutaneous vessels in the deep dermis and subcutaneous tissue (Fig. 1D). The enlarged lymph nodes showed angiomatous changes, presumably caused by congestion and impaired local circulation due to vascular calcification, rather than direct calcium deposits.
DISCUSSION
Calciphylaxis is characterized by diffuse precipitation of tissue calcium, and is a rare fatal entity of calcific vasculopathy associated with tissue necrosis.1 Its description was first reported in skin, and the calciphylaxis of other organs has rarely been reported.3 Unlike metastatic calcification, calciphylaxis is accompanied by damage to ischemic and necrotic tissue.4,5 Metastatic calcification and calciphylaxis are metabolic disorders,3 for which the precise pathogenesis has not yet been determined. Multifactorial causes have been suggested: persistent or transient hyperphosphatemia, vitamin D intoxication, hypercalcemia, steroid therapy in renal transplant recipients, and deficiencies or functional abnormalities of proteins C and S, warfarin therapy, or secondary hyperparathyroidism.6-8 Hypoparathyroidism as well as hyperparathyroidism are rare causes of metastatic calcification.9 Other theories involving proinflammatory cytokines, including interleukin-6 and tumor necrosis factor α, which may cause calciphylaxis through induction of endothelial damage by vascular calcification, have been suggested. Low levels of osteoprotegerin, a calcification inhibitor acting as a compensatory protector for vascular calcification, may be another possible cause.10 PTH-related peptide that shares structural and functional homology with native PTH can cause indirect stimulation of osteoclastic bone resorption and restriction of renal calcium excretion.11 Occurrence of calciphylaxis and metastatic calcification has been reported in cases involving both benign and malignant causes.3,12,13 Malignant causes include metastatic breast cancer, pulmonary metastases of osteogenic sarcoma, or malignant melanoma. The patient described in the present case showed slight elevation of PTH-related peptide along with CA-125, and subsequently hidden malignancy was suspected. An autopsy was performed, but failed to find any tumorous lesions. Specificity of CA-125 was low, and its increase has been observed in various neoplastic and non-neoplastic conditions: ovarian malignancies, acute leukemia with extramedullary localization, non-Hodgkin's lymphoma, melanomas, breast, lung, or gastrointestinal carcinomas, abdominal surgery, bacterial peritonitis, pelvic inflammatory disease, or tuberculosis.14 Unlike CA-125, serum PTH-related peptide is regarded as a useful indicator of tumor-related hypercalcemia and bone metastasis of solid tumor and hematologic malignancies.15 However, production of PTH-related peptide has also been reported in nonneoplastic tissues and several endocrine glands, including non-tumorous thyroid follicular epithelium, colloid nodules, non-tumorous testicular Leydig cells, normal ovarian granulosa-theca cells, placental trophoblast, deciduas, and normal adrenal cortex.16 As observed in our case, elevated CA-125 and PTH-related peptide might be a compensatory physiologic response to pleural effusion and hypoparathyroidism.
Occurrence of pulmonary calciphylaxis is rare, whereas occurrence of pulmonary metastatic calcification is more common. Several cases of pulmonary calciphylaxis have been reported.2,3,8,12,13,17,18 Most of the reported cases have been associated with long-term dialysis therapy; however, pulmonary calciphylaxis observed in the present case occurred under cryptogenic hypercalcemia immediately after the first hemodialysis treatment. Not all cases of pulmonary calciphylaxis are associated with calciphylaxis of the skin or other organs. Even in cases involving successful treatment of hypercalcemia, diagnosis of pulmonary calciphylaxis is not made until death due to supervention of acute respiratory failure. Causative factors for most of the reported cases remain complex and unknown; therefore, treatment is challenging and is based on symptoms. However, treatment should be aimed at stopping progression of calcific vasculopathy in order to restore tissue perfusion and oxygenation. Recent therapy has been developed for modulation of local production of PTH-related peptide levels and may prevent fatal pulmonary calciphylaxis.18,19
The present case was unique in that development of calciphylaxis involving the skin and visceral organs occurred immediately after the first hemodialysis treatment under the condition of acute renal failure and cryptogenic hypercalcemia. This autopsy case emphasizes the importance of visceral calciphylaxis and its early identification.
Notes
No potential conflict of interest relevant to this article was reported.