Solitary fibrous tumor: an updated review
Article information
Abstract
Solitary fibrous tumor (SFT) is a fibroblastic neoplasm characterized by a branching, thin-walled dilated staghorn-shaped (hemangiopericytoma-like) vasculature and a NAB2::STAT6 gene fusion. SFTs can occur in almost any anatomical location, including superficial and deep soft tissues, visceral organs, and bone. They most commonly occur in extrapleural locations, equally affect both sexes, and are typically present in adults. Although metastasis is rare, SFTs frequently show local recurrence. The diagnosis of SFTs is difficult because of their broad histological and morphological overlap with other neoplasms. An accurate diagnosis is important for guiding disease management and prognosis. Despite advances in molecular diagnostics and therapeutic strategies, the biological complexity and unpredictable clinical behavior of SFTs present significant challenges. This review provides an updated overview of SFT, with a focus on its molecular genetics, histopathological features, and diagnostic considerations.
INTRODUCTION
Solitary fibrous tumor (SFT) is a rare fibroblastic neoplasm defined by a distinctive network of thin-walled, branching staghorn-shaped (hemangiopericytoma-like) vessels [1]. It may occur in almost any anatomical location, such as superficial and deep soft tissue, visceral organs, and bone, although it most often arises in extrapleural sites. SFT affects both sexes equally and is typically diagnosed in adults.
Many tumors previously classified as hemangiopericytomas are now recognized as SFTs and reflect fibroblastic rather than true pericytic differentiation [2]. Histologically, SFTs exhibit a wide morphological spectrum, usually consisting of spindle to ovoid cells arranged haphazardly within a collagen-rich stroma and associated with prominent staghorn-shaped vasculature [3]. However, its biological behavior is often unpredictable and cannot be reliably inferred from morphology alone [4].
Recent advances in molecular pathology, particularly the discovery of the NAB2::STAT6 gene fusion and its downstream effects, have provided considerable insight into the biology, classification, and potential therapeutic targets of SFT [5-7]. Nonetheless, diagnosis remains difficult because of marked histological heterogeneity and overlap with other spindle cell neoplasms.
Most SFTs pursue an indolent course; however, a clinically important subset shows aggressive behavior, including local recurrence or distant metastasis. Therefore, accurate pathological classification, integrated with molecular findings, is essential for guiding management and prognostication.
In this review, the clinicopathological and molecular features of SFT are summarized, including the histological subtypes, diagnostic approaches, and key differential diagnoses.
HISTORICAL ASPECTS
The term hemangiopericytoma was first introduced in the 1940s by Stout and Murray [8] and Stout [9,10] to describe tumors thought to originate from pericytes, which are specialized contractile cells surrounding capillaries and venules; however, their original definition lacked specificity and encompassed a heterogeneous group of neoplasms, including entities now classified as myofibromas. In 1976, Enzinger and Smith [11] refined the concept, characterizing these tumors by their undifferentiated small round-to-spindle cells and the presence of prominent, branching staghorn-shaped vessels. Despite this refinement, its classification remains problematic because of inconsistent ultrastructural evidence of pericytic differentiation [12-15], infrequent actin expression [16-19], and poor diagnostic reproducibility [20], which has resulted in a gradual decline in the use of the term.
The entity known as SFT subsequently emerged. First described by Klemperer and Rabin [21] as a pleural-based lesion designated “fibrous mesothelioma” or “benign fibrous tumor of the pleura,” it was more clearly defined by England in 1989 [22], who proposed the term “localized fibrous tumor of the pleura.” By the late 1980s and early 1990s, histologically indistinguishable tumors were increasingly recognized at extrapleural sites, which supported the concept of a broader, site-independent lesion.
Extrapleural tumors with a hemangiopericytoma-like morphology frequently express CD34, similar to SFTs, which suggests a shared lineage. This was confirmed by the discovery of the recurrent NAB2::STAT6 gene fusion and its corresponding nuclear signal transducer and activator of transcription 6 (STAT6) expression in SFTs and tumors, which were previously diagnosed as hemangiopericytomas, regardless of anatomical site [23-26].
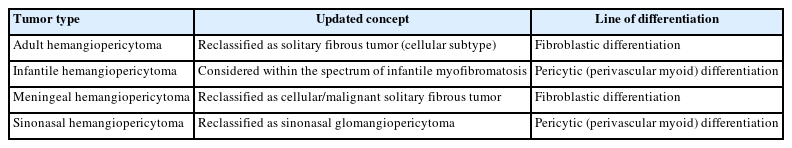
Based on this evidence, the 2002 WHO classification of tumors of soft tissue and bone (3rd edition) [27] revised the definition of hemangiopericytoma. It was recognized that most remaining cases closely resemble the cell variant of SFT morphologically and clinically. In 2013, the 4th edition of the WHO classification [28] eliminated the term hemangiopericytoma, reclassifying nearly all such tumors under the unified diagnosis of SFT. Table 1 lists the conceptual changes in hemangiopericytoma classification.
EPIDEMIOLOGY
SFTs affect both sexes equally and predominantly occur in adults, with a peak incidence between 40 and 70 years of age [29-31]. Although SFTs may arise anywhere in the body, extrapleural locations are more common. Approximately 30%–40% occur in the extremities, 30%–40% in the deep soft tissues of the abdomen, pelvis, or retroperitoneum, 10%–15% in the head and neck, and 10%–15% in the trunk [30,32].
In the gastrointestinal system, SFTs typically develop in adults aged 20–70 years, but are rare in children and adolescents. The liver, pancreas, mesentery, or serosal surfaces of the gastrointestinal tract are considered common sites. A slight male predominance was reported in the lipomatous (fat-forming) subtype [33-35]. In the female genital tract, SFTs primarily affect women aged 22–75 years, with a peak incidence during the fifth decade. Common sites include the vulva, vagina, and cervix [36].
In the thorax, SFTs primarily occur from the visceral pleura and typically present in the sixth decade. They may also arise in the lung or pericardium, whereas mediastinal involvement is rare. No sex predilection is evident [22,37]. In the central nervous system (CNS), SFTs are extremely rare and account for less than 1% of all CNS tumors. They often present in middle-aged to older adults. Most are dural-based and are often located in the supratentorial region, with occasional cases reported in the skull base, spinal cord, or pineal region [38-40].
In the urinary and male genital tracts, SFTs generally occur in adults between 20 and 70 years of age, with no clear sex predilection. Reported locations include the kidney, bladder, prostate, seminal vesicles, and penis [41,42]. In the endocrine system, SFTs most commonly involve the thyroid gland or pituitary fossa, whereas other endocrine organs are rare. These tumors typically occur between ages of 50 and 60, with no sex predilection [43,44].
In the head and neck, a marked male predominance is observed in the larynx (male-to-female ratio ~6:1), whereas tumors arising in the orbit, nasal cavity, or paranasal sinuses occur across a broad age range in both sexes [45,46]. Orbital SFTs are most common in individuals in their mid-40s and are rare in children. These tumors may occur in the intraconal and extraconal compartments, with occasional involvement of the lacrimal gland, conjunctiva, or eyelid [47-49].
CLINICAL FEATURES
The clinical presentation of SFTs varies by anatomical site, but they most commonly manifest as a slow-growing, painless mass. Abdominopelvic SFTs may cause symptoms, such as abdominal distention, constipation, urinary retention, or early satiety [50,51], whereas head and neck lesions result in nasal obstruction, hoarseness, or epistaxis [52,53]. Orbital SFTs typically present with periorbital fullness, proptosis, globe displacement, and diplopia, whereas deeper lesions may compromise the optic nerve [47,49,54].
Thoracic SFTs are often asymptomatic and incidentally detected; however, larger tumors can result in cough, dyspnea, or chest pain [55]. CNS SFTs generally present with mass effect symptoms or increased intracranial pressure [56]. In the digestive, urinary, and endocrine systems, tumors are usually painless but may produce compressive symptoms depending on their size and anatomical relationships [41,43,57].
A subset of large or aggressive SFTs secretes insulin-like growth factor 2 (IGF2), which results in paraneoplastic hypoglycemia (Doege-Potter syndrome) and, rarely, acromegaloid features [58,59].
RADIOLOGICAL FEATURES
Upon imaging, SFTs typically show nonspecific radiographic features [60,61], whereas computed tomography (CT) usually yields a well-defined, occasionally lobulated, isodense mass relative to the skeletal muscle (Fig. 1). They exhibit heterogeneous contrast enhancement because of their rich vascularity [62,63]. Magnetic resonance imaging (MRI) typically shows intermediate T1 signal intensity and variable T2 signals, which correspond to fibrous (low T2) and cellular or myxoid (high T2) components [63-65]. Larger or more aggressive tumors may display heterogeneity because of fibrosis, necrosis, hemorrhage, or cystic changes [63].

Radiological findings of solitary fibrous tumor. Axial contrast-enhanced abdominal computed tomography demonstrates a large central abdominal mass. Prominent feeding vessels (arrow) are visible along the anterior aspect of the lesion.
In the thorax, SFTs are usually present as sharply marginated, pleural-based masses without chest wall invasion. Malignant lesions may exhibit increased fluorodeoxyglucose uptake on positron emission tomography; however, overlap with benign tumors may occur [66,67]. In the CNS, SFTs often mimic meningiomas on imaging. The lesions exhibit isointensity on T1-weighted MRI, variable T2 signals, and peripheral dural enhancement (dural tail); however, no specific CT or MRI features reliably distinguish them from other dural-based tumors [68,69].
In the head and neck region, SFTs typically appear as well-circumscribed, contrast-enhanced masses by CT and MRI [70,71]. In the orbit, MRI typically exhibits iso-intense signals on T1-weighted images, whereas CT demonstrates contrast enhancement and is valuable for assessing bone involvement [47,72].
MOLECULAR CHARACTERISTICS
Most SFTs harbor a recurrent paracentric inversion on chromosome 12q13. This inversion results in the fusion of the NAB2 and STAT6 genes [26,73,74]. This fusion replaces the C-terminal repression domain of NAB2 with the transcriptional activation domain of STAT6, thereby converting NAB2 from a transcriptional repressor into a constitutive activator of EGR1. Consequently, EGR1 drives the expression of downstream targets, such as IGF2 and FGFR1, as well as other genes that promote growth and survival [73].
Multiple NAB2::STAT6 gene fusion variants have been discovered, with the length of the retained STAT6 portion correlating with tumor morphology and clinical behavior. For example, fusions involving NAB2 exon 4 and STAT6 exon 2 or 3 are associated with a reduced cellular and more indolent course. In contrast, fusions involving NAB2 exons 6–7 and STAT6 exons 16–17 more commonly occur in cellular or clinically aggressive variants [75,76].
No distinct molecular features have been identified that can reliably distinguish benign from malignant SFTs; however, other genetic alterations linked to high-grade transformation or aggressive behavior have been identified, including TERT promoter mutations [55,77], TP53 mutations, and p16 overexpression [78-81]. Moreover, IGF2, a key mediator of Doege-Potter syndrome in SFTs, is a target gene of EGR1 and may be dysregulated by the NAB2::STAT6 fusion, which may account for the relatively high frequency of this paraneoplastic syndrome [26].
The NAB2::STAT6 gene fusion is definitively diagnostic; however, its detection by molecular methods is challenging because of the close proximity of the genes on chromosome 12q and the heterogeneity of the fusion breakpoints. Thus, STAT6 immunohistochemistry demonstrating strong, diffuse nuclear staining, serves as a sensitive and specific surrogate marker for all fusion variants and is widely used in routine diagnostic practice [23,25,82].
HISTOPATHOLOGICAL FEATURES
Macroscopic features
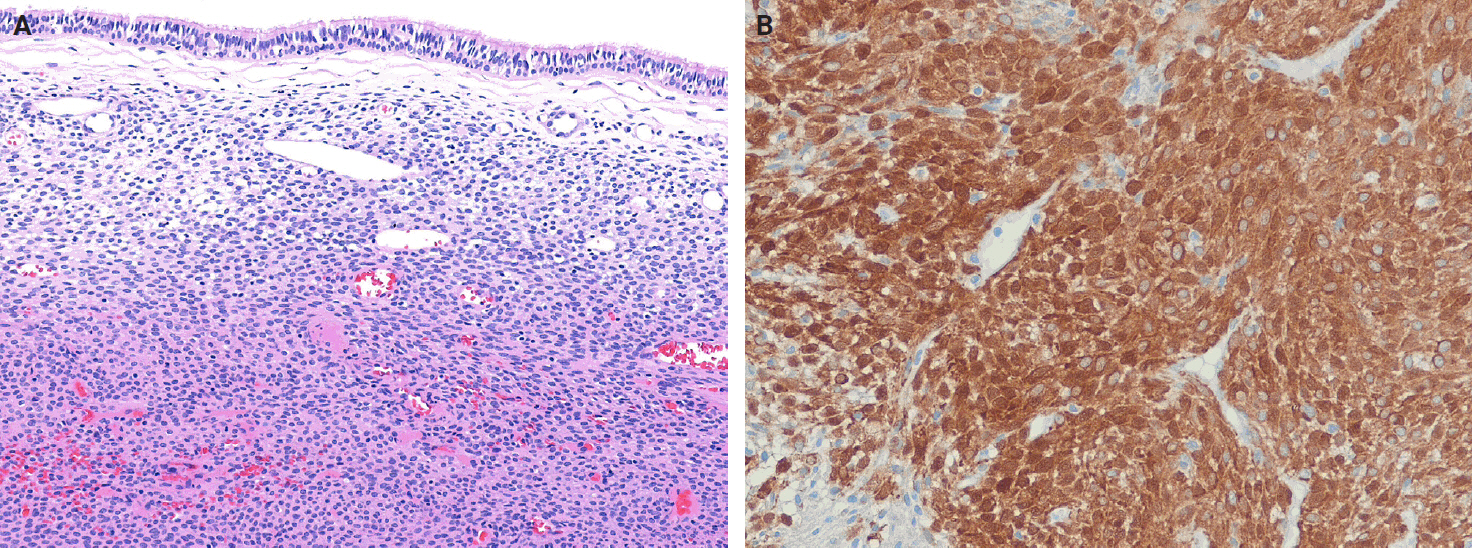
SFTs are usually well-circumscribed, solid masses ranging in size from 1 cm to greater than 25 cm, with most measuring between 5−10 cm in diameter [83,84]. The cut surface varies from firm and white in more fibrous tumors to tan and fleshy in highly cellular lesions (Fig. 2). Hemorrhage, calcification, or necrosis may occur, particularly in the larger tumors [85-88]. Benign SFTs are typically well-circumscribed, but unencapsulated, whereas malignant tumors often exhibit infiltrative borders and areas of necrosis [89].
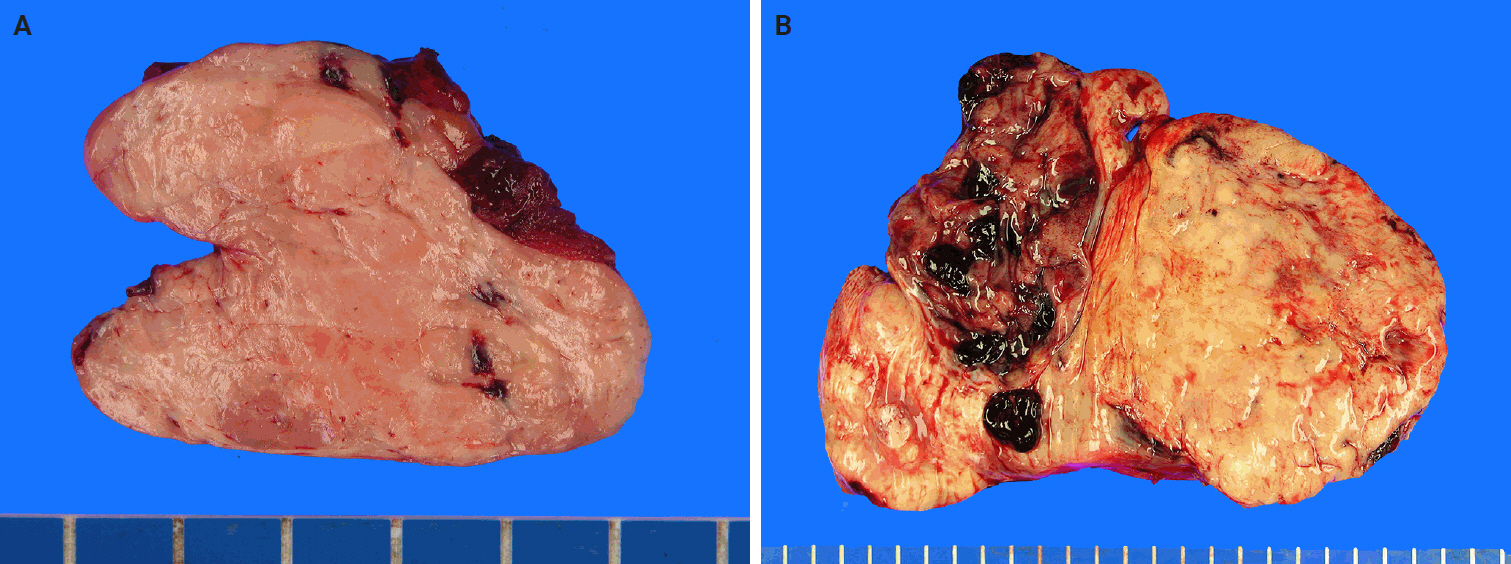
Macroscopic findings of solitary fibrous tumor. (A) The cut surface of the tumor is well-circumscribed, with a pinkish-gray, fleshy, and solid appearance. (B) The tumor is multilobulated, with yellow-tan to gray coloration and prominent areas of hemorrhage.
Tumors arising from serosal surfaces often exhibit an exophytic appearance, whereas those within body cavities may be present as polypoid, stalk-attached fibrous masses [3]. Pleural SFTs are often large (>10 cm) and pedunculated, with a pedicle containing prominent feeder vessels. Some cases lack direct pleural attachment and can appear enclosed within the lung parenchyma [37].
In the CNS, SFTs are usually dural-based, well-circumscribed, firm, white to reddish-brown masses; however, they may occasionally exhibit infiltrative growth or lack dural attachment [90-92]. In the head and neck region, tumor size varies by anatomical site, including approximately 2.5 cm in the larynx, 4 cm in the salivary glands, and 5 cm in the sinonasal tract [46,52,53,89].
Histopathology
Histologically, classic SFTs display the so-called patternless pattern, characterized by alternating hypocellular and hypercellular areas, with tumor cells frequently interposed between collagen bundles (Fig. 3A). The tumor cells are ovoid to spindle-shaped, with vesicular nuclei, pale eosinophilic cytoplasm, and indistinct cell borders, and are embedded in a variably collagenous stroma (Fig. 3B). A characteristic feature is the presence of thin-walled, branching, staghorn-shaped vessels (Fig. 3C). Perivascular hyalinization may also be observed (Fig. 3D). The degree of cellularity varies considerably, ranging from sparsely scattered individual cells or linear clusters to highly cellular areas, even within the same tumor. The tumor cells are haphazardly arranged within the stroma, often in a storiform configuration or as randomly oriented fascicles. Mitoses are typically infrequent, and significant nuclear pleomorphism or necrosis is absent in conventional cases. Additional histological features may include multinucleated giant cells, myxoid or cystic changes, and hemorrhage (Fig. 3E). Rarely, the foci of epithelioid or rhabdoid tumor cells may also be present (Fig. 3F).
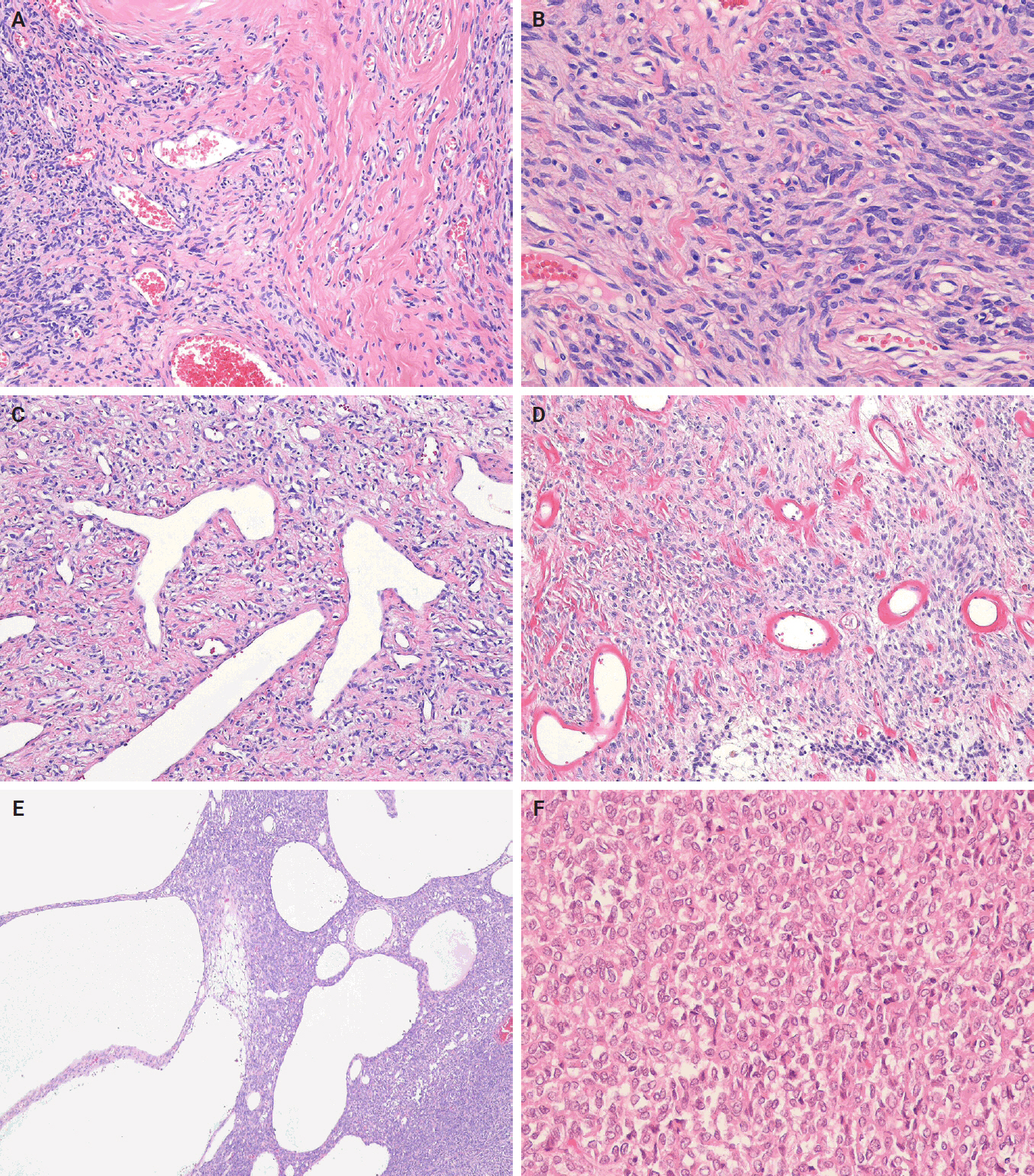
Histological findings of classic solitary fibrous tumor. (A) The tumor shows variation in cellularity, with prominent stromal collagen deposition in the hypocellular regions. (B) The tumor cells are relatively uniform and spindle-shaped, with vesicular nuclei and scant pale eosinophilic cytoplasm, arranged in a patternless architecture. (C) Branching, staghorn-shaped vessels are present. (D) Perivascular hyalinization is present. (E) Cystic changes are present. (F) Epithelioid tumor cells are observed.
Subtypes of solitary fibrous tumor
SFT subtypes share clinical, histological, and immunohistochemical characteristics that support their close relationship.
Cellular solitary fibrous tumor
Cellular SFT is characterized by densely packed tumor cells with indistinct cytoplasmic borders and prominent thin‑walled, branching staghorn-shaped vessels, with little or no intervening stroma. This subtype corresponds to the originally described hemangiopericytoma. The tumor cells are typically monotonous, showing loss of spindled morphology and transition to a more ovoid or rounded shape (Fig. 4A). Hemorrhage is common in cellular SFT, whereas necrosis may also be present.
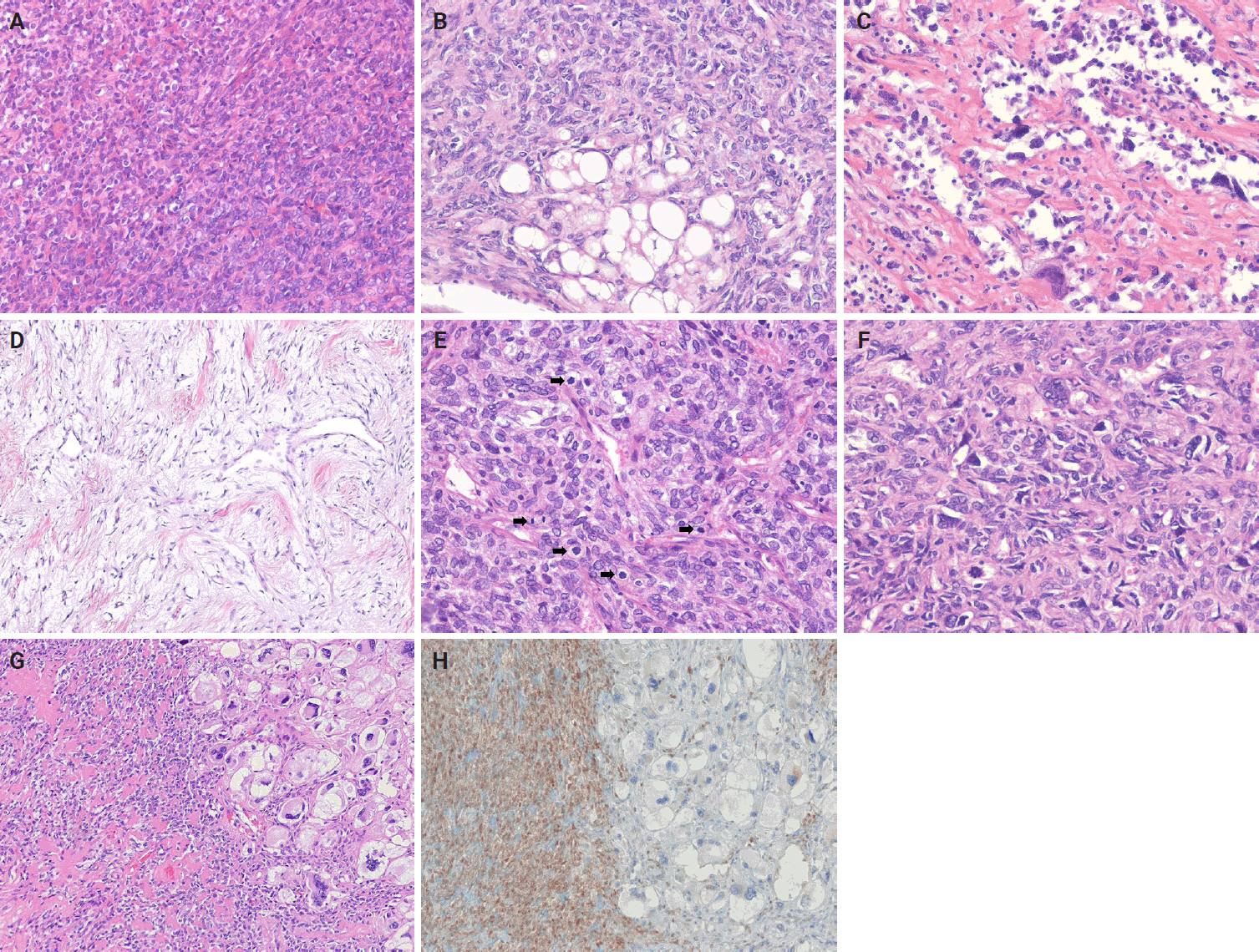
Histological findings of solitary fibrous tumor subtypes. (A) Cellular subtypes. The tumor shows predominantly increased cellularity, and the tumor cells exhibit a more ovoid or rounded cytomorphology. (B) Lipomatous (fat-forming) subtypes. The tumor shows areas of mature adipose tissue. (C) Giant cell-rich subtypes. There are abundant multinucleated tumor giant cells, which frequently line pseudovascular spaces. (D) Myxoid subtype. The tumor shows prominent myxoid stroma with hypocellularity. Dilated, thin-walled vessels are present. (E) Malignant subtype (high-risk solitary fibrous tumor). Mitotic figures (arrows) are frequently observed. (F) Malignant subtype (high-risk solitary fibrous tumor). The tumor cells exhibit marked nuclear pleomorphism and cytological atypia. (G) Dedifferentiated subtype. The tumor shows an abrupt transition from solitary fibrous tumor (left) to high-grade dedifferentiated area (right). (H) Dedifferentiated subtype. Classic solitary fibrous tumor shows strong, diffuse nuclear expression of STAT6, whereas the dedifferentiated area demonstrates loss of STAT6 expression.
Lipomatous (fat-forming) solitary fibrous tumor
Lipomatous (fat-forming) SFT is a rare histological subtype characterized by mature adipose tissue forming an integral component of the tumor. Histologically, it displays the typical features of SFT mixed with a variable amount of mature fat (Fig. 4B) [35,93-95]. An immature lipoblastic component may also be present. Although the majority of lipomatous SFTs are benign, cases with malignant histological features have also been reported [96].
Giant cell-rich solitary fibrous tumor
Giant cell-rich SFT (formerly known as giant cell angiofibroma) is a rare SFT subtype that retains the typical morphological features of conventional SFT, but contains a mixed population of multinucleated giant cells scattered within the stroma and lining pseudovascular spaces [97,98]. The tumor is composed of bland, round-to-spindle cells and multinucleated giant cells (Fig. 4C). It exhibits alternating hypocellular/sclerotic and hypercellular areas, often associated with staghorn-shaped vasculature.
Myxoid solitary fibrous tumor
Focal myxoid change is a common finding in SFTs and may result from an increase in mucin production by neoplastic cells within the connective tissue. Myxoid SFT is a rare SFT subtype characterized by diffuse and prominent myxoid changes involving most of the tumor and exhibit a hypocellular, bland histological appearance (Fig. 4D) [99].
Malignant solitary fibrous tumor
Malignant SFT is defined by one or more adverse histological features, including hypercellularity, increased mitotic activity (>4 mitoses per 10 high-power fields [HPFs]), cytological atypia, tumor necrosis, and/or infiltrative margins (Fig. 4E, F) [84,100,101]. Of these, a high mitotic count is considered the most reliable predictor of aggressive behavior and poor clinical outcome [30,102]. In accordance with the College of American Pathologists (CAP) and WHO guidelines, it is currently recommended that mitotic activity be reported as the number of mitoses per mm². With older models of microscopes, 10 HPFs are equivalent to 1 mm². With a modern microscope featuring a 0.5 mm field diameter, 5 HPFs correspond to an area of approximately 1 mm². Risk-stratification models, such as that of Demicco et al. [103], integrate clinical and pathological parameters to improve prognostic accuracy.
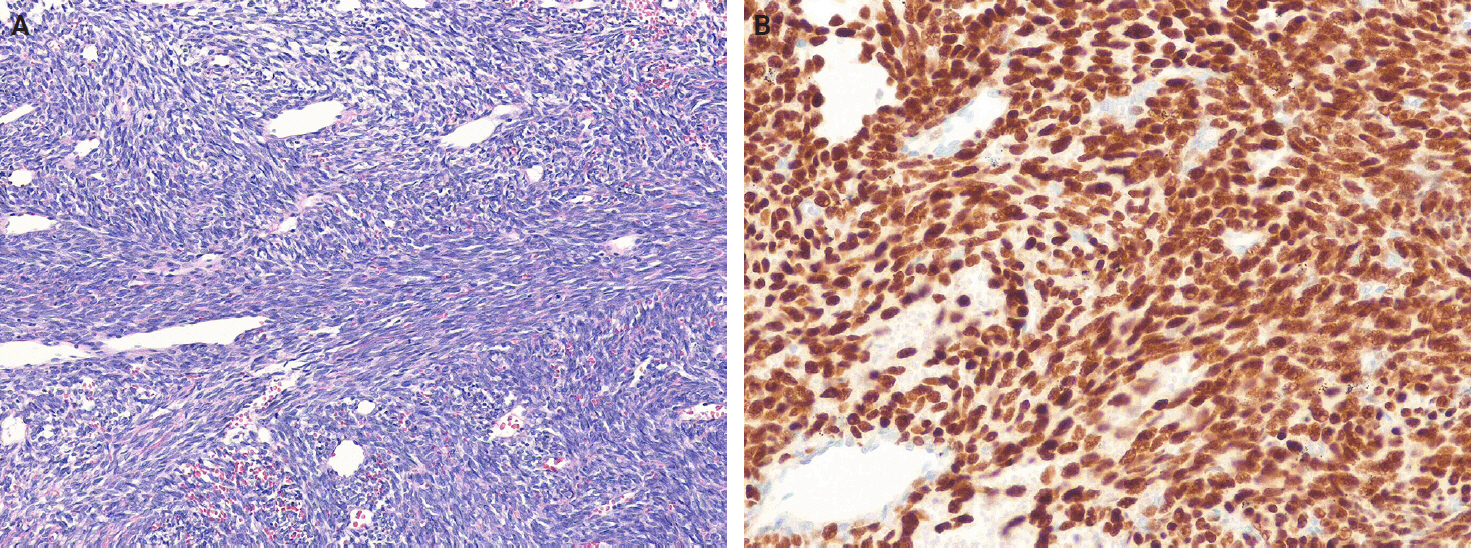
Dedifferentiated solitary fibrous tumor
Dedifferentiated SFT accounts for less than 1% of all cases and is characterized by an abrupt transition from conventional SFT morphology to high-grade spindle or pleomorphic sarcoma features (Fig. 4G, H) [104-112]. It may occur in various anatomical sites, including the meninges and orbit. Heterologous elements, such as rhabdomyosarcoma or osteosarcoma, have also been described. Dedifferentiated SFT has a high risk of recurrence and metastasis and portends a poor prognosis.
IMMUNOHISTOCHEMICAL FEATURES
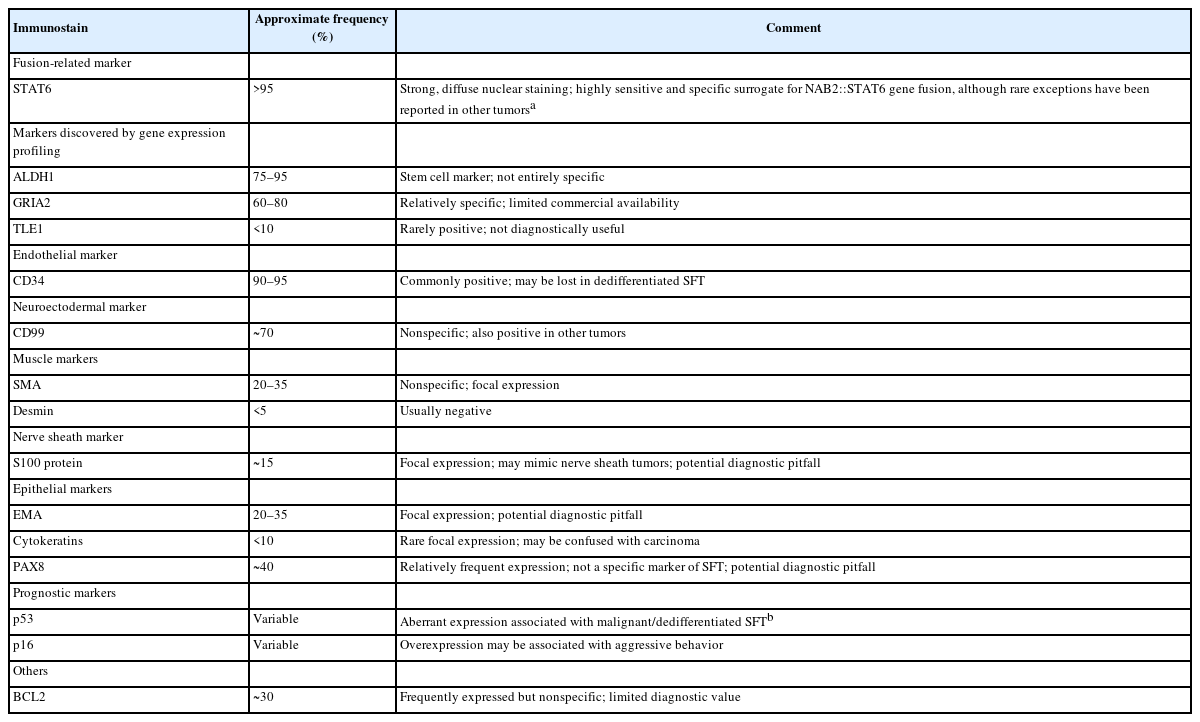
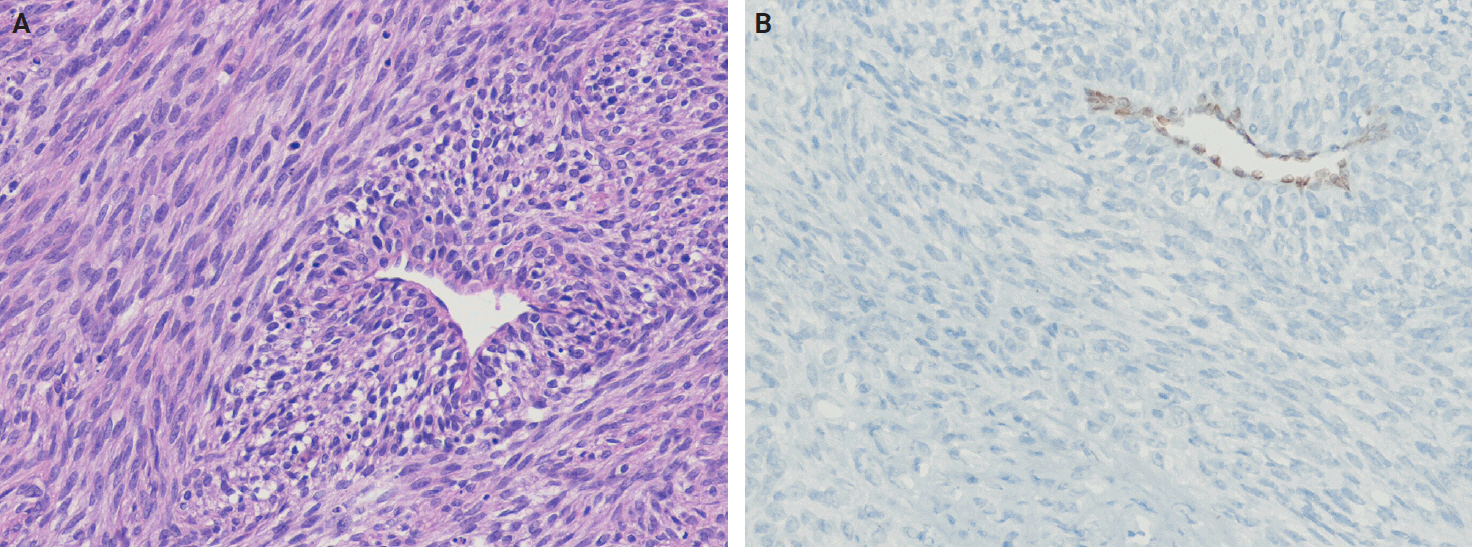
Immunohistochemical studies have shown that SFTs typically exhibit strong, diffuse nuclear expression of STAT6 and CD34 (Fig. 5) [23,25,73,84,113]. The nuclear localization of STAT6 reflects the presence of the NAB2::STAT6 fusion and serves as a sensitive and specific diagnostic marker that distinguishes SFT from histological mimics [114-117]. However, STAT6 expression has also been reported in dedifferentiated liposarcoma (DDLPS) [118] and GLI1-altered soft tissue tumor [119]. CD34 is expressed in approximately 81%–95% of cases, particularly in low-grade tumors; however, its expression may be decreased or lost in high-grade or dedifferentiated SFTs [120-123]. Similarly, loss of STAT6 expression has been observed in dedifferentiated or embolized tumors [121].
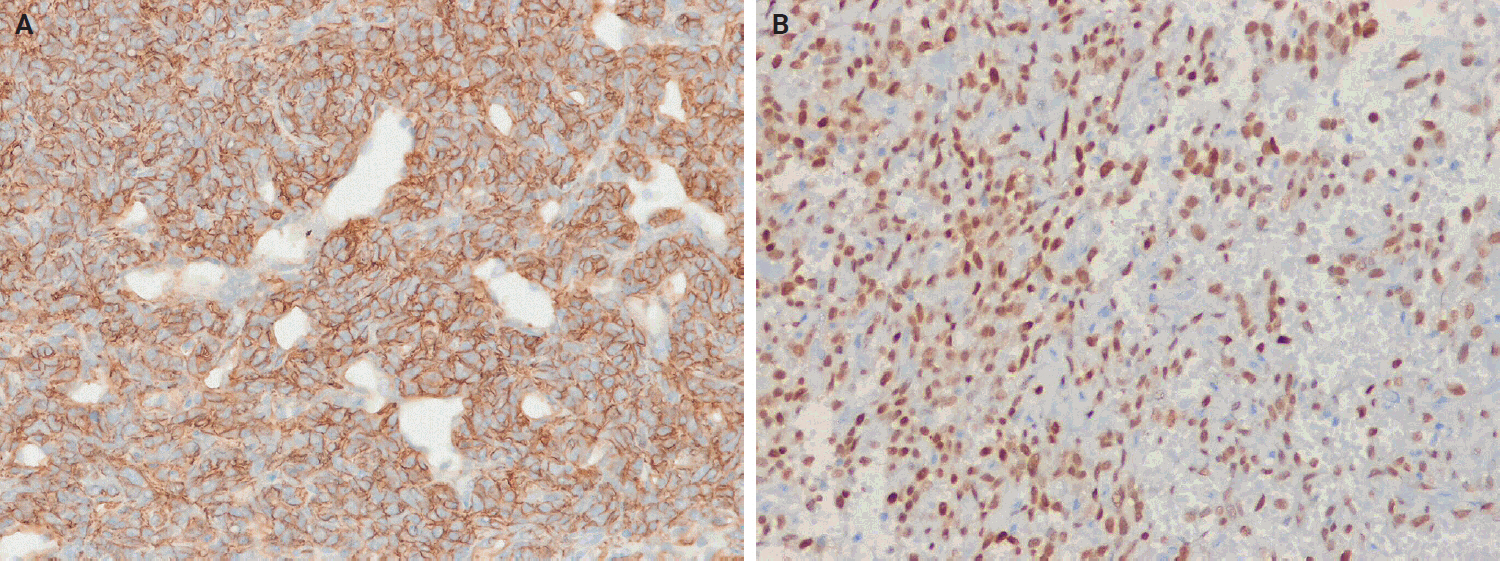
Immunohistochemical findings of solitary fibrous tumor. (A) The tumor cells demonstrate strong, diffuse cytoplasmic and membranous expression of CD34. (B) The tumor cells show strong, diffuse nuclear expression of STAT6.
Gene expression profiling identified other markers that can distinguish SFTs from their histological mimics. Among these, glutamate ionotropic receptor AMPA type subunit 2 (GRIA2) shows 80%–93% sensitivity for SFT [124]. Cytoplasmic aldehyde dehydrogenase 1 (ALDH1) demonstrates 84% sensitivity and 99% specificity in differentiating SFT from meningioma and synovial sarcoma (SS) [125]. Subsequent studies indicate that ALDH1 sensitivity ranges from 76% to 97% and GRIA2 sensitivity ranges from 64% to 84%, with GRIA2 exhibiting lower specificity compared with ALDH1 and STAT6 [111,112,126].
Other immunohistochemical markers, such as BCL2 and CD99, are frequently positive. Epithelial membrane antigen (EMA) and smooth muscle actin (SMA) show variable expression, whereas desmin, S100 protein, SOX10, actins, cytokeratins, and the progesterone receptor are typically negative or only focally expressed [83,127,128]. Transducin-like enhancer of split 1 (TLE1) may show weak positivity [129]. Occasional PAX8 expression has also been reported, which may cause diagnostic confusion with renal cell carcinoma [130]. Table 2 summarizes the immunohistochemistry profiles for SFT.
DIAGNOSTIC APPROACH
A systematic and integrated approach is required to accurately diagnose SFTs. The process begins with a thorough histopathological evaluation of hematoxylin and eosin sections, particularly at low magnification, to assess tumor borders, cellular uniformity, and overall architecture. Key histological features include bland spindle cell morphology, patternless or short fascicular architecture, and stromal characteristics, such as hyalinization, myxoid change, and the distinctive staghorn-shaped vascular pattern. Recognizing these features is critical for distinguishing SFTs from other spindle cell neoplasms with overlapping morphologies.
The clinical context, including patient age, tumor location, and symptomatology, together with radiological findings, provides valuable complementary information. For example, a well-circumscribed, hypervascular mass on imaging in a middle-aged or older adult supports the presumptive diagnosis of SFT. These clinical-radiological correlations are particularly helpful when histological findings are equivocal.
Immunohistochemistry plays an essential role in the diagnostic algorithm and has largely replaced electron microscopy due to its accessibility and diagnostic utility. It is necessary not only for establishing the line of differentiation but also for identifying molecular surrogates of specific genetic alterations. For SFTs, strong, diffuse nuclear STAT6 expression, which serves as a surrogate marker for the NAB2::STAT6 gene fusion, together with CD34 positivity, constitutes a highly sensitive and specific marker combination. These two markers are routinely used and are generally sufficient to confirm an SFT diagnosis in most cases. However, they are not entirely specific, as focal STAT6 expression may also occur in other mesenchymal tumors, creating potential diagnostic pitfalls. Moreover, additional diagnostic confusion may arise, particularly in tumors occurring in visceral organs, such as the lung, salivary gland, or prostate [32,131]. For example, entrapment of normal glandular epithelium should not be misinterpreted as a biphasic neoplasm, such as phyllodes tumor, pleomorphic adenoma, or sarcomatoid carcinoma (Fig. 6). If STAT6 is negative, second-line antibodies, such as GRIA2 and ALDH1, may be used.
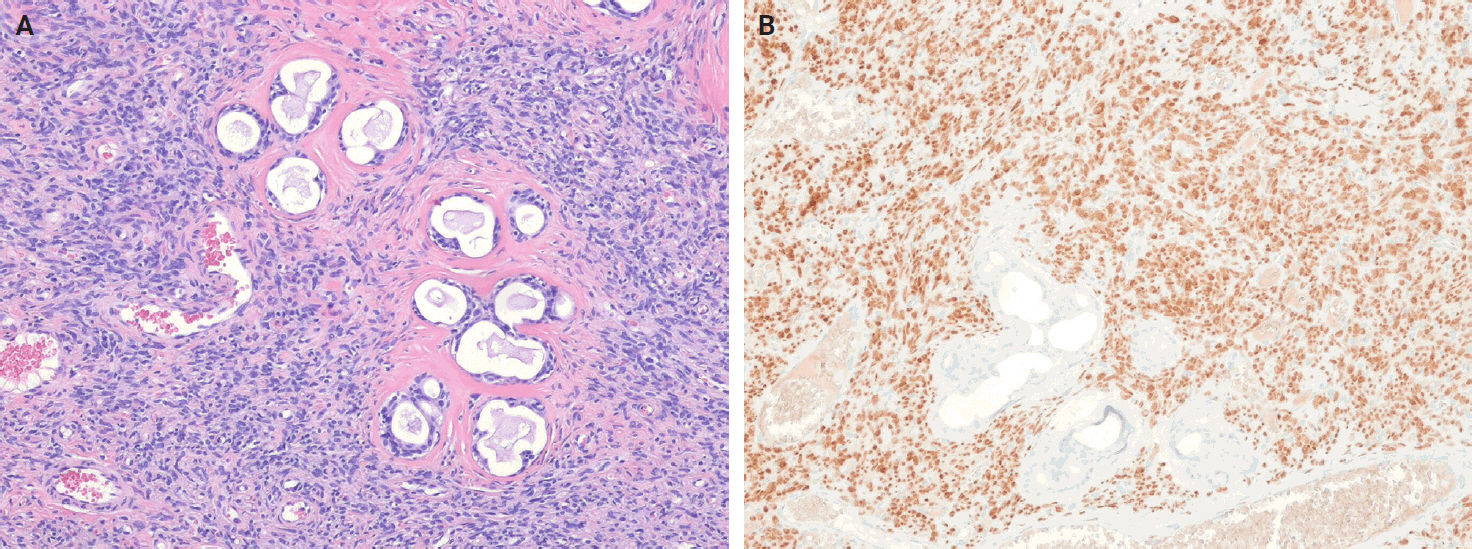
Solitary fibrous tumor of the oral cavity. (A) Entrapped benign glandular inclusions are present within the tumor, mimicking pleomorphic adenoma. (B) The spindled tumor cells show strong, diffuse nuclear STAT6 expression, supporting the diagnosis of solitary fibrous tumor.
For diagnostically challenging or histologically atypical cases, fluorescence in situ hybridization (FISH) or next-generation sequencing may provide additional diagnostic clarity. These approaches are also helpful for detecting fusion genes or mutations associated with dedifferentiation. They have been incorporated into routine diagnostic workflows to enhance diagnostic precision and enable prognostic stratification, particularly in high-grade or dedifferentiated subtypes. In summary, a comprehensive diagnostic approach that integrates morphologic, immunophenotypic, clinical, and molecular data is essential for achieving diagnostic accuracy, refining risk stratification, and guiding appropriate patient management.
HISTOLOGICAL DIFFERENTIAL DIAGNOSIS
The histological differential diagnosis of SFT depends on the location and morphology of the tumor; however, it may be substantially improved by immunohistochemical detection of nuclear STAT6 expression. Accurate diagnosis requires a combination of clinical context, anatomic site, histopathological features, and a focused immunohistochemical panel.
Spindle cell lipoma
Spindle cell lipoma (SCL) is a benign adipocytic tumor consisting of variable amounts of mature adipocytes, bland spindle cells, and ropy collagen [132]. It occurs most commonly in men aged 45–60 years and typically arises in the subcutaneous tissue of the posterior neck, back, and shoulders. SCL is histologically characterized by bland spindle cells arranged in small, aligned clusters within a myxoid matrix, accompanied by mature adipose tissue and ropy collagen. The spindle cells are typically CD34-positive [133,134] and show loss of nuclear RB1 protein expression [135]. SFTs with hyalinized stroma and admixed adipose tissue may resemble SCL; however, SCLs rarely exhibit a staghorn-shaped vasculature and lack nuclear STAT6 expression.
Nodular fasciitis
Nodular fasciitis (NF) is a benign, self-limited fibroblastic/myofibroblastic neoplasm that frequently exhibits a recurrent USP6 rearrangement [136]. It is usually found in the subcutaneous tissue of the extremities and is typically <3 cm in size. NF is relatively common and can present at any age, although it most frequently occurs in young adults. Histologically, NF consists of plump, uniform fibroblasts and myofibroblasts arranged in a tissue culture-like pattern, within a variably myxoid stroma that often contains microcystic changes and extravasated erythrocytes. The tumor cells are positive for SMA and muscle-specific actin (MSA), with occasional desmin expression, but consistently negative for STAT6. The identification of a USP6 rearrangement can assist in diagnostically challenging cases [137-139].
Desmoid fibromatosis
Desmoid fibromatosis (DFM) is a locally aggressive, non-metastasizing myofibroblastic neoplasm that is characterized by infiltrative growth and a high propensity for local recurrence [140]. It frequently arises in the extremities, abdominal cavity, retroperitoneum, abdominal wall, and chest wall, and predominantly affects young female adults, with a median age of 37–39 years. DFM is driven by somatic CTNNB1 mutations or inactivating germline APC mutations [141-144]. Histologically, it consists of uniform fibroblastic cells arranged in long, sweeping fascicles with collagen deposition. Small-caliber vessels with perivascular edema are also present. Immunohistochemically, DFM is positive for SMA and MSA, and nuclear β-catenin expression is observed in most cases. STAT6 negativity helps distinguish DFM from SFT.
Cellular angiofibroma
Cellular angiofibroma (CAF) is a benign, cellular, and richly vascular fibroblastic neoplasm that typically arises in the vulvar or inguinoscrotal region [145]. It affects both sexes with a similar frequency, with peak incidence in women during the fifth decade and in men during the seventh decade. Loss of 13q14, including RB1, is a characteristic genetic alterations in CAFs [146,147]. Histologically, it consists of bland spindle cells arranged in short fascicles among delicate collagen fibers, accompanied by numerous small- to medium-sized thick-walled vessels, and may contain intermixed adipose tissue. Immunohistochemically, CD34 is expressed in 30%–60% of cases, whereas SMA and desmin are variably expressed in a minority of cases [145,148]. Loss of nuclear RB1 expression is frequently observed. CAF can mimic SFT morphologically; however, the vessels are generally smaller, more hyalinized, and fibrotic. STAT6 expression is consistently negative.
Angiofibroma of soft tissue
Angiofibroma of soft tissue (AFST) is a benign fibroblastic neoplasm characterized by a prominent, arborizing network of numerous branching, thin-walled blood vessels [149]. It primarily affects middle-aged adults, with a peak incidence in the sixth decade of life [150-152]. AFSTs typically arise in the extremities, particularly the legs. A recurrent t(5;8)(p15;q13) translocation, resulting in an AHRR::NCOA2 gene fusion, occurs in approximately 60%–80% of cases [151-153]. Histologically, AFST is composed of bland, uniform short spindle cells embedded in a variable myxoid or collagenous stroma with innumerable small, thin-walled, branching blood vessels (Fig. 7). Immunohistochemically, the tumor cells variably express EMA and CD34, whereas desmin positivity may be observed in scattered dendritic cells [150,152]. AFST often exhibits morphologic overlap with SFT; however, STAT6 expression is consistently absent.
Dermatofibrosarcoma protuberans
Dermatofibrosarcoma protuberans (DFSP) is a superficial, locally aggressive fibroblastic neoplasm. It is characterized by a storiform arrangement of uniform spindle cells and is typically associated with a COL1A1::PDGFB or related gene [154]. DFSP usually occurs on the trunk and proximal extremities, followed by the head and neck region. It predominantly affects young to middle-aged adults with a slight male predominance. Histologically, DFSP shows diffusely infiltrative growth into surrounding tissues, often producing a characteristic honeycomb pattern within the subcutaneous fat. Immunohistochemically, the tumor cells are diffusely positive for CD34 and negative for STAT6. In contrast, SFTs are usually well-circumscribed and show nuclear STAT6 expression, which serves as a distinguishing feature.
Deep fibrous histiocytoma
Deep fibrous histiocytoma (DFH) is a benign morphological variant of fibrous histiocytoma that arises entirely within the subcutaneous or deep soft tissue [155]. It occurs over a wide age range (6–84 years old, with a median age of 37 years) with a slight male predominance. The extremities are the most commonly affected sites, followed by the head and neck region. Approximately 10% of cases occur in visceral soft tissues, such as the retroperitoneum, mediastinum, and pelvis [156]. Rearrangements of either PRKCB or PRKCD have been identified [157,158]. Histologically, DFH is a well‑circumscribed lesion that exhibits monomorphic spindle‑shaped or histiocytoid cells arranged in a mixed fascicular and storiform pattern, which is often accompanied by prominent branching vessels. Approximately 40% of DFHs express CD34 [156]. These cases may be challenging to distinguish from SFTs; however, they are characteristically negative for STAT6.
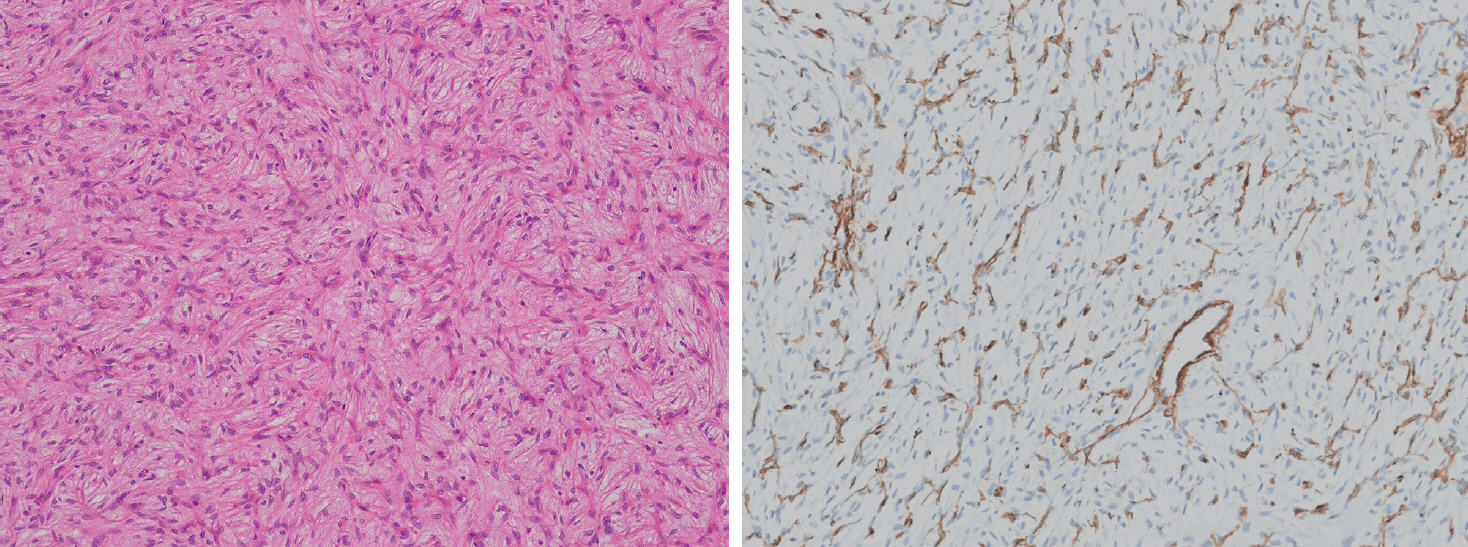
Myopericytoma
Myopericytoma is a distinctive perivascular myoid neoplasm that forms part of a morphological spectrum with myofibroma [159]. It occurs at any age but is most commonly observed in adults. It usually involves the distal extremities, followed by the proximal extremities, neck, trunk, and oral cavity. Mutations in the PDGFRB gene may underlie a shared pathogenesis among myopericytoma, myopericytomatosis, and myofibroma [160,161]. In addition, cellular or atypical myofibromas are associated with SRF::RELA gene fusions [162]. Histologically, myopericytoma consists of bland, myoid-appearing spindled cells arranged in a concentric perivascular pattern around numerous small vessels (Fig. 8A). Immunohistochemically, myopericytomas express SMA and caldesmon, with focal positivity for desmin and/or CD34 (Fig. 8B). In contrast, SFTs do not show concentric perivascular architecture but instead demonstrate diffuse CD34 and STAT6 positivity.
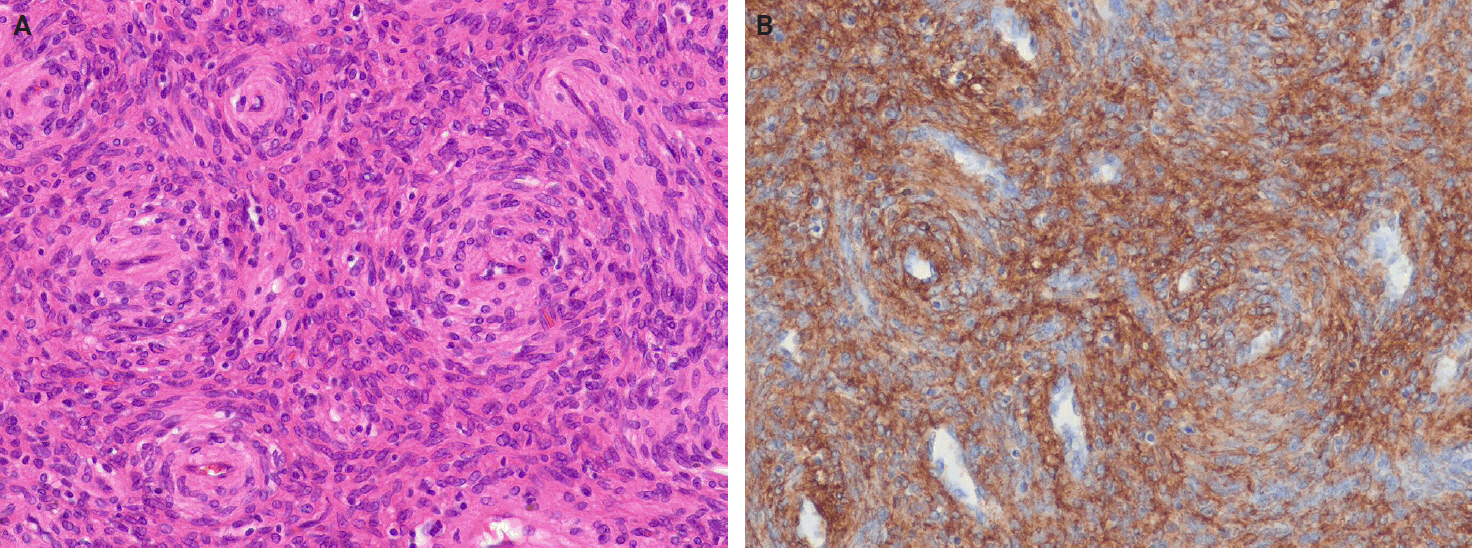
Sinonasal glomangiopericytoma
Sinonasal glomangiopericytoma is a distinctive soft tissue tumor of the sinonasal tract characterized by perivascular myoid differentiation [163]. It occurs at any age, but most commonly presents in the sixth or seventh decade of life, with a slight female predilection. Unilateral involvement of the nasal cavity, particularly the turbinates and septum, is typical, whereas bilateral disease is rare and occurs in fewer than 5% of cases. Molecular alterations include recurrent missense mutations in exon 3 of CTNNB1. Histologically, the tumor appears as an ovoid to spindled syncytium of myoid-type cells within a richly vascularized stroma (Fig. 9A). Perivascular hyalinization with extravasated erythrocytes, mast cells, and eosinophils is commonly observed. The tumor cells exhibit strong SMA and nuclear β-catenin expression, with variable CD34 positivity (Fig. 9B) [164,165]. In contrast, SFTs are positive for CD34 and STAT6, but negative for SMA.
Dedifferentiated liposarcoma
DDLPS arises through progression from an atypical lipomatous tumor (ALT) or well-differentiated liposarcoma (WDLPS) into a non-lipogenic sarcoma of variable histologic grade [166]. It most frequently occurs in the retroperitoneum, followed by the spermatic cord and, more rarely, the mediastinum, head and neck, and trunk. DDLPS predominantly affects middle-aged adults, with a peak incidence in the fourth to fifth decade of life, and show no significant sex predilection. Approximately 90% of cases develop de novo, whereas about 10% arise from recurrent ALT/WDLPS [167]. DDLPS shares molecular features with ALT/WDLPS, as both harbor amplification of MDM2 (mouse double minute 2 homolog) and CDK4 (cyclin-dependent kinase 4) on chromosome 12q14-q15 [168,169]. Histologically, DDLPS shows an abrupt or gradual transition from a WDLPS to a spindle cell or pleomorphic non-lipogenic tumor (rarely lipogenic), which may be low or high grade. Immunohistochemically, nuclear positivity for MDM2 and CDK4 is observed in most cases. Lipomatous SFTs may be mistaken for WDLPS or DDLPS because of their fat-containing appearance, particularly in limited biopsy samples or imaging studies. Rarely, DDLPS may display an SFT‑like morphology and even show STAT6 positivity [118], whereas SFTs are typically negative for MDM2 and CDK4. Myxoid SFT may resemble myxoid liposarcoma; however, DDIT3 FISH is negative, and STAT6 expression is diffusely positive in SFTs.
Gastrointestinal stromal tumor
Gastrointestinal stromal tumors (GISTs) are mesenchymal neoplasms with variable biological behavior and are characterized by differentiation toward the interstitial cells of Cajal [170]. GISTs can occur at any site within the gastrointestinal tract, whereas extragastrointestinal GISTs most commonly develop in the mesentery, omentum, and retroperitoneum. Sporadic GISTs occur at any age, but most cases appear in the sixth decade of life (median age, 60 to 65 years), with a slight male predominance [171]. Most GISTs have activating mutations in KIT or PDGFRA. Histologically, GISTs display a broad morphological spectrum and typically consist of relatively monomorphic spindle cells, epithelioid cells, or a mixture of both. Immunohistochemically, GISTs positively express CD34, CD117 (KIT), and DOG1. They may closely resemble SFTs, but can be distinguished by their positive CD117 (KIT) and DOG1 expression, and negative STAT6 expression.
Malignant peripheral nerve sheath tumor
Malignant peripheral nerve sheath tumor (MPNST) is a malignant spindle cell neoplasm with Schwannian differentiation [172]. It most commonly arises in older adults during the seventh decade of life, although it can occur across a wide age range [173]. Approximately 50% of cases occur in association with neurofibromatosis type 1 (NF1), 10% are associated with prior radiation exposure, and the remainder are sporadic [174]. MPNST most frequently involves the trunk and extremities, followed by the head and neck region. At the molecular level, MPNSTs exhibit complex structural and numerical chromosomal abnormalities, and biallelic inactivation of the NF1 gene is commonly observed in MPNST [175,176]. Histologically, conventional MPNST displays fascicular growth of relatively uniform spindle cells, alternating hypercellular and hypocellular areas, perivascular accentuation, and geographical necrosis (Fig. 10A). The tumor cells show focal positivity for S100 protein and SOX10 expression, along with loss of H3K27me3 expression (Fig. 10B) [177]. MPNST may resemble cellular SFT; however, it is usually negative for CD34 and STAT6, while showing focal expression of S100 protein and SOX10.
Synovial sarcoma
SS is a monomorphic spindle cell sarcoma with variable epithelial differentiation. It is defined by SS18::SSX1, SS18::SSX2, or SS18::SSX4 gene fusions [178]. Approximately 70% of the cases occur in the deep soft tissue of the extremities, often near joints, with 15% in the trunk and 7% in the head and neck. SS can occur at any age, with no sex predilection, although half of the patients are adolescents or young adults [179]. Histologically, SS may be classified into three subtypes: monophasic (dense fascicles of monomorphic spindle cells with staghorn-shaped vasculature), biphasic (containing epithelial and spindle components), and poorly differentiated (high cellularity, nuclear atypia, and brisk mitotic activity) (Fig. 11A) [180]. TLE1 shows nuclear positivity in up to 95% of cases, with patchy to focal cytokeratin and EMA staining. SS18::SSX fusion–specific and SSX-specific C-terminal antibodies have recently been developed that yield strong, diffuse nuclear staining with >95% sensitivity and specificity (Fig. 11B) [181]. Cellular SFT can mimic SS; however, SSs are typically negative for CD34 and STAT6.
Phosphaturic mesenchymal tumor
Phosphaturic mesenchymal tumors (PMTs) are morphologically distinct neoplasms that cause tumor-induced osteomalacia, most often through overproduction of fibroblast growth factor 23 (FGF23) [182]. PMTs may arise in almost any soft tissue or bone, but are uncommon in the retroperitoneum, viscera, and mediastinum. They frequently affect middle‑aged adults with no sex predilection, although they can also develop in pediatric and elderly patients. Approximately half of all PMTs harbor FN1::FGFR1 fusions and, rarely, FN1::FGF1 fusions [183,184]. Histologically, PMT consists of bland spindle-shaped cells with characteristic grungy calcification and a prominent capillary network, with occasional staghorn-shaped vessels. PMT exhibits variable ERG, SATB2, and CD56 expression. FGF23 expression has been reported in some cases, but currently available antibodies lack specificity, which limits their diagnostic utility [185,186]. PMTs may mimic SFTs; however, SFTs lack the grungy calcified matrix typical of PMTs and usually show CD34 and STAT6 positivity.
Mesenchymal chondrosarcoma
Mesenchymal chondrosarcoma (MCS) is a high‑grade malignant tumor with a distinct biphasic pattern. It consists of primitive undifferentiated mesenchymal cells and well‑differentiated hyaline cartilage [187]. MCS most commonly arises in the second or third decade of life, with a median age of approximately 30 years and a slight male predominance. MCS exhibits a broad anatomical distribution, involving bone, soft tissue, and intracranial locations. Approximately 40% of cases occur in somatic soft tissues, and the meninges are a common extra-skeletal site [188]. At a molecular level, MCS harbors a specific and recurrent HEY1::NCOA2 fusion, which has been identified in nearly all cases [189]. Histologically, MCS exhibits undifferentiated tumor cells, cartilage islands, and a staghorn-shaped vascular pattern. The undifferentiated tumor cells often express CD99, SOX9, and NKX2.2 [190], and may occasionally show aberrant expression of desmin, myogenin, and MYOD1. Because the cartilage foci may be scant or absent in limited biopsies, MCS may be mistaken for malignant SFT; however, SFTs are distinguished by nuclear STAT6 positivity, which is absent in MCSs.
Table 3 provides an overview of the differential diagnosis of SFTs, summarizing the clinical, histological, immunohistochemical, and molecular features of morphologically similar entities.
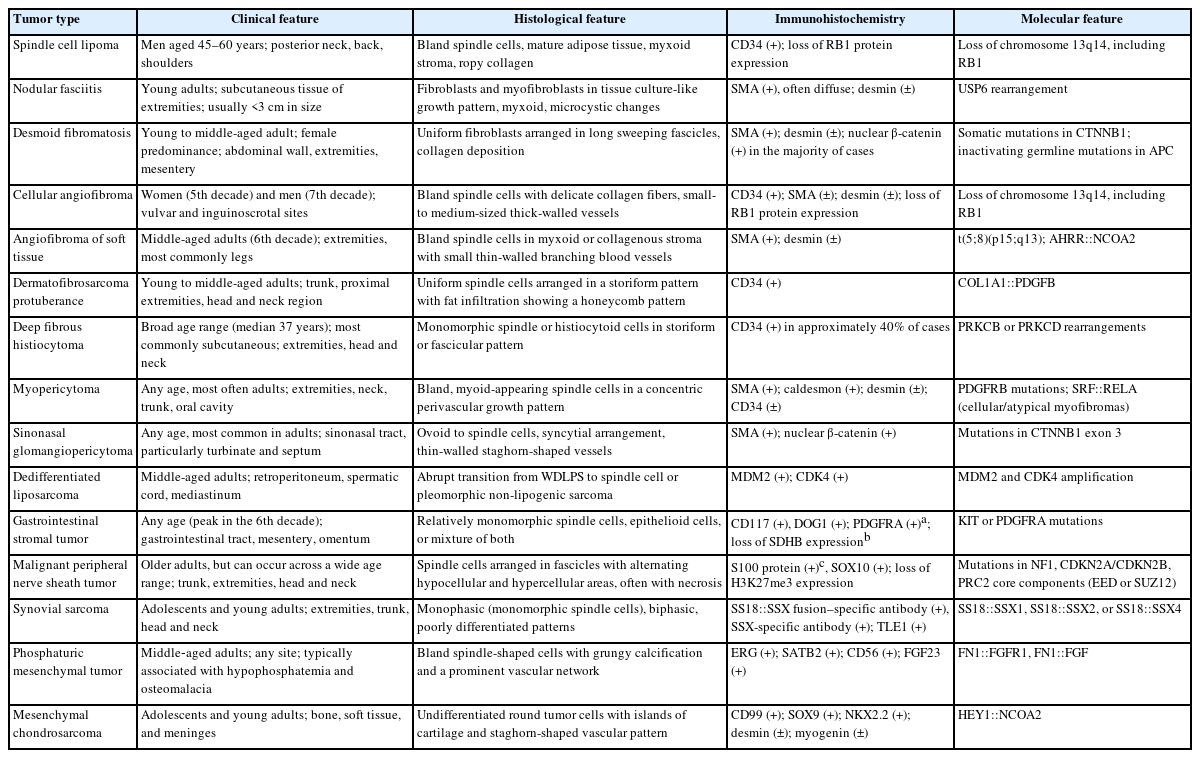
Differential diagnosis of solitary fibrous tumor by clinical, histological, immunohistochemical, and molecular features
Fig. 12 shows diagnostic algorithm and differential diagnosis of SFT.
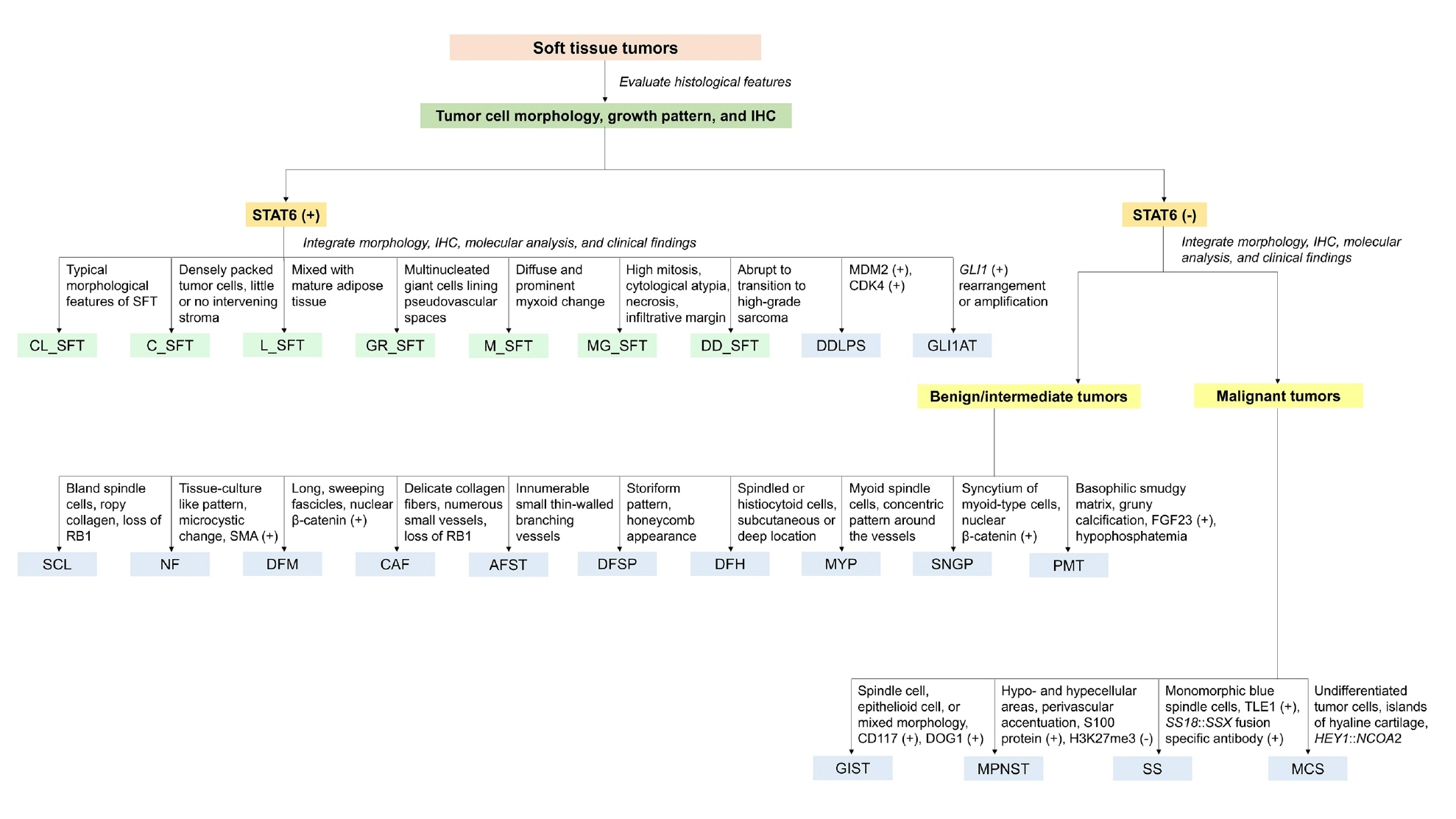
Diagnostic algorithm and differential diagnosis of solitary fibrous tumor (SFT). This flowchart illustrates a systematic approach to diagnosing soft tissue tumors with spindle cell morphology, emphasizing the importance of histological assessment, immunohistochemistry (IHC), and molecular analysis. The algorithm distinguishes between STAT6-positive tumors, encompassing the SFT subtypes and mimickers, and STAT6-negative tumors. STAT6, signal transducer and activator of transcription 6; CL_SFT, classic SFT; C_SFT, cellular SFT; L_SFT, lipomatous SFT; GR_SFT, giant cell-rich SFT; M_SFT, myxoid SFT; MG_SFT, malignant SFT; DD_SFT, dedifferentiated SFT; DDLPS, dedifferentiated liposarcoma; GLI1AT, GLI1-altered soft tissue tumor; SCL, spindle cell lipoma; NF, nodular fasciitis; SMA, smooth muscle actin; DFM, desmoid fibromatosis; CAF, cellular angiofibroma; AFST, angiofibroma of soft tissue; DFSP, dermatofibrosarcoma protuberans; DFH, deep fibrous histiocytoma; MYP, myopericytoma; SNGP, sinonasal glomangiopericytoma; FGF23, fibroblast growth factor 23; PMT, phosphaturic mesenchymal tumor; DOG1, discovered on GIST-1; GIST, gastrointestinal stromal tumor; H3K27me3, histone H3 lysine 27 trimethylation; MPNST, malignant peripheral nerve sheath tumor; TLE1, transducin-like enhancer of split 1; SS, synovial sarcoma; MCS, mesenchymal chondrosarcoma.
PROGNOSIS
SFTs exhibit a broad spectrum of clinical behavior, with local or distant recurrence occurring in 10%–30% of cases and, occasionally, >15 years after treatment [30,31,101,191]. To improve prognosis, multivariate risk models have been developed and validated across various anatomical sites. The most commonly used model includes mitotic count, tumor size (≥5 cm), and patient age (≥55 years), with some modifications that also include necrosis as a fourth parameter [31,103,192]. Table 4 presents three-variable and modified four-variable risk models for predicting metastatic risk in SFTs [31,103]. These models are superior to the traditional benign versus malignant classification and may be applied to thoracic, extra-thoracic, and gynecologic SFTs.
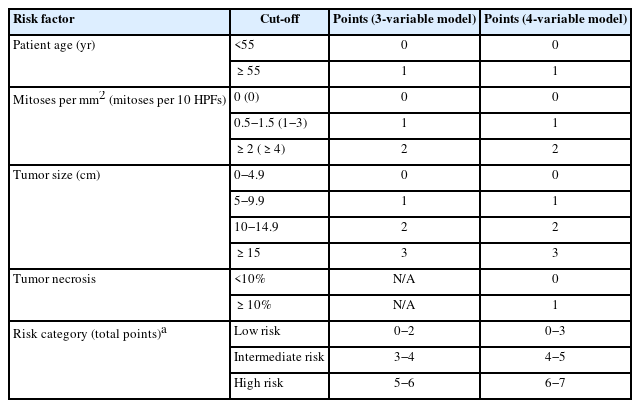
Three-variable and four-variable risk models for predicting metastatic risk in solitary fibrous tumors
At the molecular level, TERT promoter mutations and TP53 loss are more frequently observed in high-grade or dedifferentiated tumors [77,193]. Positive p53 expression and elevated Ki-67 index (>5%) are associated with poorer prognosis in some studies [54].
In the CNS, SFTs exhibit higher rates of long-term recurrence and metastasis, even in WHO grade 1 cases. Mitotic activity and necrosis, rather than tumor size or patient age, are the strongest predictors of progression. A three-tiered histologic grading scheme was recommended for CNS SFTs [39,76]. In the head and neck region, most SFTs behave indolently, with recurrence rates <10%; however, ocular adnexal SFTs exhibit a higher local recurrence rate (~25%) with a low metastatic potential (~2%) [46,194]. Positive surgical margins and dedifferentiation are independent risk factors of relapse. If metastasis occurs, it most often involves the lungs, bones, and liver [55].
TREATMENT
The management of SFT should be done in specialized sarcoma centers with a multidisciplinary team experienced in this rare entity [7]. Treatment response is generally assessed using Response Evaluation Criteria in Solid Tumors (RECIST); however, because of the hypervascular nature of SFT, some studies also use the Choi criteria, which is defined as a ≥10% decrease in tumor size or a >15% decrease in tumor density [195-197].
Localized lesions
Complete en bloc surgical resection with negative margins (R0) is the gold standard for treatment. The 10-year overall survival rate following R0 resection ranges from 54% to 89% [198-200]. If margins are positive (R1/R2), re‑resection should be considered where feasible. Adjuvant radiotherapy (RT) can achieve >80% 5-year local control for high-risk or margin-positive cases, although no survival benefit has been demonstrated [68,201-204]. Preoperative RT may be considered in selected cases to increase resectability; however, there is no proven role for neoadjuvant or adjuvant chemotherapy [205-207]. SFTs generally do not respond well to conventional sarcoma regimens. Thus, systemic therapy should be reserved for clinical trials or in very high‑risk situations.
Advanced or metastatic lesions
Isolated, resectable metastases (e.g., lung) can be treated with surgery or ablative methods. RT is an option for local control in selected cases. Conventional chemotherapy demonstrates low overall response rates (0%–20%) [208,209]. Anthracycline-based regimens are used as first-line therapy. Ifosfamide, dacarbazine, or trabectedin may be administered in later lines [210-212]. Median progression‑free survival is generally limited to 4–5 months. Because SFTs are highly vascular, antiangiogenic therapy has shown promising results. Pazopanib, sunitinib, sorafenib, and temozolomide plus bevacizumab have achieved partial responses and significant disease control [213-218]. In prospective trials, pazopanib produced partial responses in >50% of patients by Choi criteria, supporting its role as a potential first-line therapy for advanced SFT. IGF-1 is frequently overexpressed in SFTs. Figitumumab, an anti–IGF-1 receptor monoclonal antibody, has shown efficacy in some advanced cases [218,219]. Data on immunotherapy are limited, although anecdotal durable responses have been reported with programmed death-1 inhibitors (e.g., pembrolizumab) [220,221]. Ongoing studies are evaluating combinatorial approaches with immune checkpoint inhibitors and antiangiogenic agents.
FUTURE PERSPECTIVES
The current understanding of SFTs is primarily based on retrospective case series and preclinical studies, which limits the generalizability and robustness of existing diagnostic and therapeutic strategies [222]. Consequently, substantial gaps remain in the areas of tumor biology, prognostication, and optimal treatment pathways.
A critical area of investigation is the prognostic relevance of the specific NAB2::STAT6 gene fusion variants. Although the NAB2::STAT6 fusion is a molecular hallmark of SFTs, its transcript variants and their effects on tumor behavior, metastatic potential, and treatment response remain unclear. Prospective studies integrating molecular and clinicopathological data are essential for developing reliable, fusion-based risk stratification models.
The development of advanced molecular platforms, such as NGS, offers the ability not only to detect NAB2::STAT6 gene fusions but also to identify additional genetic alterations with prognostic or therapeutic significance. In addition, ongoing research into the immunologic profile of SFTs warrants further study of immune checkpoint inhibitors and other immunotherapeutic strategies.
Ultimately, progress in SFT management will depend on coordinated efforts to refine molecular classification, improve diagnostic accuracy, and develop targeted therapies tailored to individual patient risk profiles.
Recent advances in artificial intelligence and digital pathology suggest new opportunities for prognostic assessment in SFTs. By enabling quantitative and reproducible evaluation of histomorphological features, AI-based image analysis may complement existing clinicopathological models. Although data are still limited, future integration of these technologies could enhance risk stratification and individualized patient management.
CONCLUSION
SFT is a rare fibroblastic neoplasm that poses significant diagnostic and therapeutic challenges. Its broad histological spectrum and frequent morphological overlap with other soft tissue tumors make accurate diagnosis difficult, often requiring an integrated approach that combines immunohistochemistry and molecular testing. A comprehensive understanding of SFT, including its histological variants, molecular subtypes, and variable clinical behavior, is essential for optimizing surgical management, identifying patients requiring systemic therapy, and establishing effective long-term surveillance protocols. As the molecular mechanisms underlying SFT are further elucidated, it will be critical to incorporate these advances into clinical practice to enhance diagnostic precision, refine risk stratification, and enable the development of personalized treatment strategies.
Notes
Ethics Statement
Not applicable.
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Code Availability
Not applicable.
Conflicts of Interest
J.H.C., a contributing editor of the Journal of Pathology and Translational Medicine, was not involved in the editorial evaluation or decision to publish this article.
Funding Statement
No funding to declare.