Spectrum of thyroiditis types: clinical, cytomorphological, and radiological findings
Article information
Abstract
Background
Thyroiditis encompasses a range of inflammatory conditions affecting the thyroid gland. Lymphocytic thyroiditis (LT) is a common form of thyroiditis, with acute suppuration of the thyroid, while tuberculous thyroiditis is relatively rare. Fine-needle aspiration cytology (FNAC) remains a safe and cost-effective tool for diagnosing thyroid-related diseases, especially when paired with ultrasound (US) and clinical examination.
Methods
This is a cross-sectional study including 21 cases. The cases were reported as thyroiditis on US and FNAC, and the findings were correlated with patient clinical history, symptoms during presentation, and serological profiles.
Results
The cases of thyroiditis encompassed the more common forms, LT and subacute granulomatous thyroiditis (SAT), as well as relatively rare forms like tuberculous thyroiditis and thyroid abscess. Cases of follicular neoplasms (FN) arising in the context of LT also are included in this study. The case of tuberculous thyroiditis presented as a bulky thyroid gland that appeared heterogeneous on US with extensive necrosis on FNAC. The cases of thyroid abscess and SAT presented with painful neck swellings, with granulomas in the latter cases. US features of LT showed an array of appearances ranging from pseudonodular to an atrophic thyroid gland. All cases of FN showed a lymphocytic background.
Conclusions
Thyroiditis is a commonly encountered condition that needs to be sub-categorized accurately into acute, subacute, and chronic types for appropriate clinical management, as they can sometimes show overlapping features. Though rare, acute suppurative and tuberculous thyroiditis are often encountered and warrant immediate care and treatment.
INTRODUCTION
Thyroid fine-needle aspiration cytology (FNAC) remains an easy, safe, and cost-effective diagnostic tool for thyroid-related lesions with a high sensitivity and positive predictive value. It has led to a reduction in the number of surgeries for benign conditions and a subsequent increase in resection of malignancies [1]. Ultrasound (US) of the thyroid gland, compared to other radiological modalities, is more useful and effective in detecting thyroid pathologies [2].
Thyroiditis is most commonly caused by autoimmune conditions, which include lymphocytic thyroiditis (LT), Graves’ disease, postpartum thyroiditis, and painless sporadic thyroiditis [3]. LT is more common in women, causing painless enlargement of the thyroid gland, with most of the patients presenting in a euthyroid state. However, in some patients, hypothyroidism is observed with an initial transient phase of hyperthyroidism. It is associated with elevated levels of serum antithyroid antibodies, which include anti-thyroglobulin, anti–thyroid peroxidase (TPO), and anti–thyroid-stimulating hormone (TSH) receptor antibodies (Fig. 1) [4]. The ultrasonographic features can vary from a diffusely enlarged thyroid gland to an atrophic gland in chronic stages. Presence of multiple ill-defined hypoechoic nodules with surrounding echogenic areas of thyroid parenchyma, giving it a pseudonodular appearance, is also common [5].

Etio-pathogenesis of thyroiditis highlighting the clinical and cytomorphological features of acute suppurative thyroiditis, subacute granulomatous thyroiditis, and lymphocytic thyroiditis.
Subacute granulomatous thyroiditis (SAT), also known as de Quervain's thyroiditis, is an inflammatory condition of the thyroid that is often self-limiting in nature. It usually occurs a few weeks following viral infections such as coxsackie, echovirus, mumps, measles, and hepatitis B and C [6,7]. Newer studies have also shown the association of SAT with coronavirus disease 2019 infection [8]. Patients usually present with a painful thyroid swelling, low-grade fever, and fatigue (Fig. 1), and US shows heterogeneously hypoechoic areas in the affected thyroid regions [9]. Most of the lesions subside within a few weeks to months following only anti-inflammatory treatment [10,11]. The presence of both epithelioid cell granulomas with admixed neutrophils and lymphocytes is a characteristic finding differentiating the condition from acute suppurative thyroiditis (AST) and LT [12].
Being an encapsulated and highly vascular organ with extensive lymphatic drainage, the thyroid gland is seldom associated with acute suppuration. When present, it is most commonly associated with bacterial infection by gram-positive bacteria like streptococcus or staphylococcus spreading through a hematogenous route [13]. It is commonly seen in malnourished individuals and immune-compromised conditions and sometimes is associated with history of trauma (Fig. 1). Clinically these patients present with painful neck swelling, fever, dysphagia, odynophagia, and raised levels of C-reactive protein [14]. On US, acute suppurative lesions are known to show hypoechoic lesions with destruction of the lobe and extension beyond the affected thyroid lobe [15].
Tuberculosis (TB) of the thyroid gland is an extremely rare condition with only a few cases reported in the literature. It is observed that tissues like thyroid, heart, pancreas, and striated muscle are much less susceptible to TB infection [16]. The low incidence of tuberculous thyroiditis can be explained by various mechanisms, including the bactericidal properties of colloids, high iodine content, and the high vascularity of the organ [17]. The spread of the Mycobacterium into the thyroid can occur by the hematogenous, lymphatic, or direct route. The clinical presentation can vary from mild to severe presenting with abscess or thyroiditis [16].
MATERIALS AND METHODS
This cross-sectional study presents 21 cases of patients diagnosed with different types of thyroiditis. The cases were evaluated based on clinical history, US imaging, and FNAC findings (Table 1) and included one case (n = 1) of tuberculous thyroiditis, two cases (n = 2) of AST/thyroid abscess, three cases (n = 3) of SAT, 10 cases (n = 10) of LT, and five cases (n = 5) of follicular neoplasm (FN) in the context of LT.
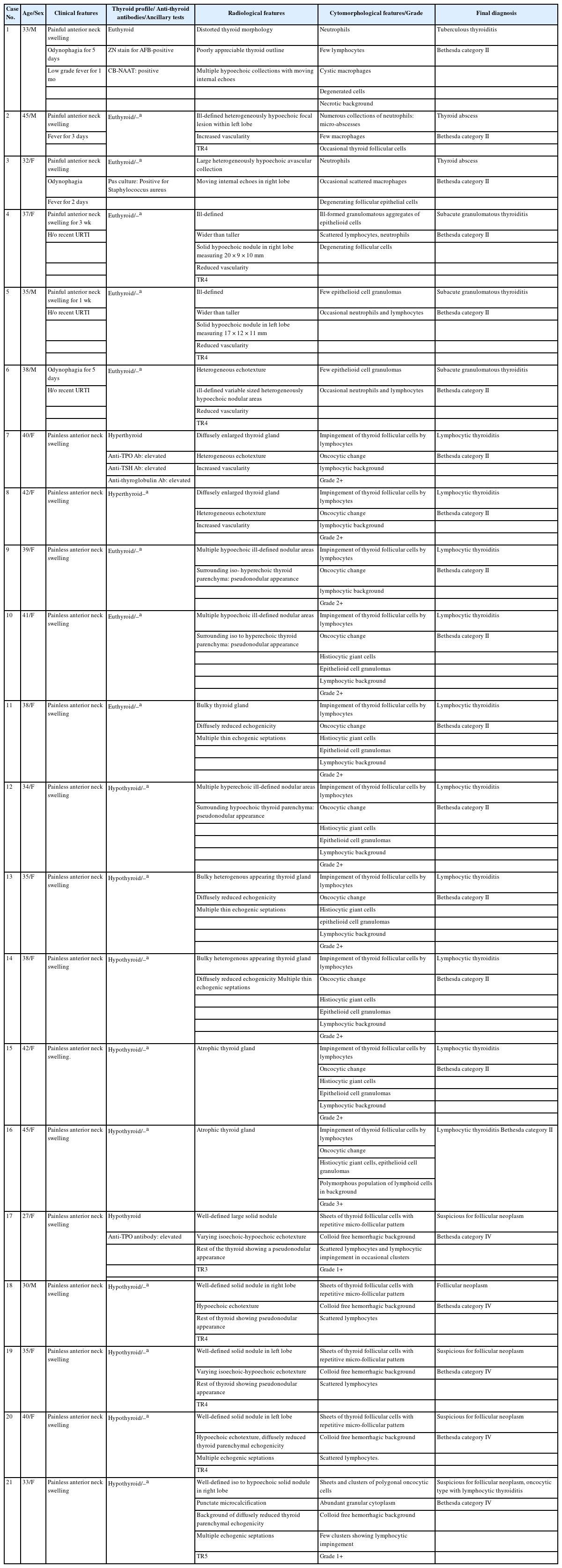
Epidemiological details and clinical, radiological, and cytomorphological features of 21 cases diagnosed as thyroiditis
Each patient's clinical symptoms were documented, US findings were recorded, and US-guided FNAC was performed to analyze cytomorphological features. Patient laboratory investigations pertaining to their thyroid function tests and serological testing of antithyroid antibodies were also recorded and interpreted with their clinical, radiological, and cytomorphological findings. US was performed using a high-frequency linear transducer with a 2–14 MHz frequency operated by a trained radiologist. The cytological smears prepared following fine-needle aspiration (FNA) were stained with Giemsa, Papanicolaou stain, and special stains wherever needed. The slides were examined by a trained pathologist, the findings were recorded, and the diagnosis was further classified using the Bethesda system for reporting thyroid cytopathology. The cases of LT were further graded into 0, 1+, 2+, or 3+ according to the Bhatia et al. [18] grading system for cytology. Grade 1+ showed few lymphoid cells infiltrating the follicles. Grade 2+ showed moderate lymphocytic infiltration or mild lymphocytic infiltration with oncocytic cell change/giant cells/anisonucleosis. Grade 3+ showed florid lymphocytic inflammation with a germinal center and very few follicular cells remaining. The clinicians were immediately informed of the cases of tuberculous thyroiditis and AST/thyroid abscess owing to the emergent nature of these cases. Histopathological findings could be obtained in all five of the cases of follicular neoplasms following subtotal thyroidectomy.
RESULTS
A total of 21 cases were included in the study, with ages ranging from 28 to 45 years. The cases included one case of tuberculous thyroiditis (n = 1), two of thyroid abscess (n = 2), three cases of SAT (n = 3), 10 cases of LT (n = 10) and five cases of FN in the context of LT (n = 5).
Tuberculous thyroiditis
A 33-year-old male presented with chief complaints of a painful anterior neck swelling with odynophagia for the previous five days and low-grade fever for the previous month with no other complaints. On examination, the swelling was tender and moved with deglutition. No cervical or axillary lymph nodes were palpable. Neck US revealed a bulky, heterogeneous-appearing thyroid gland with multiple ill-defined hypoechoic areas involving both lobes of the thyroid and the isthmus. It also showed diffusely increased vascularity in the entire thyroid parenchyma, suggestive of acute inflammation of the thyroid gland. No significant cervical lymphadenopathy was noted. The patient was advised to undergo FNAC, and the treating surgeon was informed; however, the patient subsequently was lost to follow up. The patient revisited two months later for a review scan. Clinically, the swelling had increased in size with severe pain, redness, and tenderness. This time, the US showed a distorted thyroid morphology with poorly appreciable thyroid outline. Multiple hypoechoic collections were noted within the thyroid with moving internal echoes. Extra-thyroidal extension was also noted. The visualized thyroid parenchyma showed increased vascularity (Fig. 2A). An US-guided FNA from one of the collections in the isthmus yielded 1.5 mL of whitish-caseous material (Fig. 2B), and smears prepared from it revealed neutrophils with few lymphocytes, cystic macrophages and degenerated cells, against a dirty necrotic background suggestive of necrotizing thyroiditis (Fig. 2D). No giant cells or epithelioid cell granulomas were noted. Ziehl-Neelson (ZN) staining for acid fast bacilli (AFB; 20% H2SO4) was performed on the smear owing to the necrotic background, which showed positive Mycobacterium tubercular bacilli (Fig. 2C). No thyroid follicular cells were noted. The diagnosis was tuberculous thyroiditis, Bethesda category II. The remaining aspirate was also sent for cartridge-based nucleic acid amplification testing (CB-NAAT), and the result was positive. However, the patient’s chest X-ray was normal, and abdominal US showed no free fluid and no lymphadenopathy or bowel wall thickening, indicating no pulmonary or abdominal tuberculous infection. The patient responded well to anti-tubercular therapy (ATT), and a repeat follow-up US scan revealed atrophic, heterogeneous-appearing thyroid morphology with resolution of the inflammation.

Tuberculous thyroiditis. (A) Ultrasonography showing multiple hypoechoic collections with moving internal echoes and distorted thyroid morphology. (B) A total of 1.5 mL of caseous material aspirated from the thyroid lesion. (C) Ziehl-Neelson stain showing two red-stained acid fast bacilli. (D) Giemsa-stained smear revealing occasional neutrophils and degenerated cells against a necrotic background.
Thyroid abscess/AST
A 45-year-old male presented with a painful tender anterior neck swelling that moved with deglutition, with high-grade fever for the preceding three days. US findings revealed an ill-defined heterogeneously hypoechoic focal lesion within the left lobe of the thyroid, with increased vascularity. Extrathyroidal extension was noted. Aspiration of the lesion under US guidance yielded blood-mixed aspirate. The smears prepared revealed occasional thyroid follicular cells with numerous collections of neutrophils forming micro-abscesses along with few histiocytes, supporting the diagnosis of AST/thyroid abscess, Bethesda category II. No pus culture could be performed due to the scant nature of the aspirate. However, the patient responded well to broad spectrum intravenous antibiotics, signifying a possible bacterial etiology. Similarly, the second case was a 32-year-old pregnant female in her 3rd trimester who reported a history of root canal treatment three months prior and no other relevant past medical history. She presented with painful anterior neck swelling, odynophagia, and fever for the preceding two days. US showed a large, heterogeneously hypoechoic avascular collection with moving internal echoes in the right lobe of the thyroid (Fig. 3A). FNA yielded frank pus, and cytology revealed numerous neutrophils with occasional scattered histiocytes and degenerating follicular epithelial cells (Fig. 3B). Subsequent pus culture was positive for Staphylococcus aureus. Due to the risk of fatality associated with these cases, the surgeon was informed of the diagnosis to confer immediate treatment to the patient.
Subacute granulomatous thyroiditis
A 37-year-old female presented with pain and swelling in the anterior neck for the previous three weeks. She also relayed a history of severe upper respiratory tract infection (URTI) one and a half months earlier. US revealed a normal-sized thyroid with an ill-defined, wider-than-tall solid hypoechoic nodule in the right lobe of the thyroid measuring 20 × 9 × 10 mm and showing reduced vascularity (Fig. 4A). A few benign colloid nodules were also noted in bilateral lobes of the thyroid. An US-guided FNAC of the lesion yielded scant blood-mixed aspirate revealing a paucicellular smear with occasional ill-formed granulomatous aggregates of epithelioid cells (Fig. 4C). Also seen was a collection of neutrophils with scattered lymphocytes and degenerating follicular cells (Fig. 4D). No lymphocytic impingement of thyroid follicular cells was seen. Based on the clinical, radiological, and cytological findings, the possibility of SAT, Bethesda category II was suggested. The second case was a 35-year-old male who also presented with painful anterior neck swelling following an episode of URTI. US revealed an ill-defined wider-than-tall solid hypoechoic nodule in the left lobe of the thyroid measuring 17 × 12 × 11 mm with reduced vascularity. The third case was a 38-year-old male who had developed odynophagia five days prior. On US, the thyroid gland showed heterogeneous echotexture with ill-defined, variably sized heterogeneously hypoechoic nodular areas with reduced vascularity (Fig. 4B). US-guided FNAC showed similar findings to the previous case, showing focal aggregates of epithelioid cells with scattered neutrophils and lymphocytes.

Subacute granulomatous thyroiditis. (A) Ultrasonography (US) showing an ill-defined, wider-than-tall solid hypoechoic nodule in the right lobe of the thyroid. (B) Giemsa-stained smear revealing ill-formed clusters of epithelioid cells with scattered lymphocytes. (C) US showing heterogeneous echotexture of the thyroid gland with ill-defined variably sized heterogeneously hypoechoic nodular areas. (D) Giemsa-stained smear revealing areas of collection of neutrophils with admixed lymphocytes.
Lymphocytic thyroiditis
All the cases (n = 10) of LT presented with clinical features of a painless thyroid swelling, and five cases (n = 5) had elevated levels of TSH, with low T3 and T4 serum thyroid hormones. Two (n = 2) of the patients presented with symptoms of hyperthyroidism, which can be seen sometimes during the initial phases of the disease, and the rest of the cases (n = 3) were euthyroid. One (n = 1) of the hyperthyroid cases subsequently underwent testing for anti-thyroid antibodies and was found to have elevated levels of anti-thyroglobulin, anti-TPO, and anti-TSH receptor antibodies. In the remaining nine cases (n = 9), serological antibody testing was advised, but the patients were lost to follow-up. US features of the two cases (n = 2) who presented with symptoms of hyperthyroidism showed a diffusely enlarged thyroid gland with a heterogeneous echotexture and increased vascularity (Fig. 5A). Two of the euthyroid cases (n = 2) showed multiple hypoechoic ill-defined nodular areas varying from 1–6 mm in size on US with surrounding iso to hyperechoic thyroid parenchyma giving a pseudonodular appearance (Fig. 5B). One (n = 1) of the euthyroid cases showed a bulky thyroid gland with diffusely reduced echogenicity and multiple thin echogenic septations. The US finding of one (n = 1) of the hypothyroid cases showed multiple hyperechoic ill-defined nodular areas varying from 1–7 mm with surrounding hypoechoic thyroid parenchyma also giving a pseudonodular appearance. Two (n = 2) of the hypothyroid cases revealed a bulky heterogenous appearing thyroid gland with diffusely reduced echogenicity and multiple thin echogenic septations. The remaining two (n = 2) of the hypothyroid cases revealed atrophic thyroid gland (Fig. 5C).

Lymphocytic thyroiditis. (A) Ultrasonography (US) showing a diffusely enlarged thyroid gland with a heterogeneous echotexture. (B) US showing multiple hypoechoic ill-defined nodular areas with surrounding iso-hyperechoic thyroid parenchyma giving a pseudonodular appearance. (C) US showing an atrophic thyroid gland. (D) Giemsa-stained smear showing sheets of follicular epithelial with impinging lymphocytes (grade 2+) and a lymphocytic background. (E) Giemsa-stained smear showing a histiocytic giant cell. (F) Giemsa-stained smear sheets of follicular epithelia with impinging lymphocytes and oncocytic cell change against a polymorphous maturing population of lymphocytes (grade 3+). (G) Giemsa-stained smear showing a well-formed epithelioid cell granuloma.
The cytomorphological findings in all 10 cases revealed benign cohesive sheets of thyroid follicular cells showing impingement by variable numbers of lymphocytes with numerous lymphoid cells in the background. Oncocytic changes were noted in all cases (n = 10) (Fig. 5D). Histiocytic giant cells and well-formed epithelioid cell granulomas were seen in seven (n = 7) of the 10 cases, in all the hypothyroid cases (n = 5) and two of the euthyroid cases (n = 2) (Fig. 5E, G). The degree of lymphocytic infiltration was graded from 0 to 3+ according to the Bhatia et al. grading system on cytology. Nine of the cases (n = 9) were graded as 2+, and only one case (n = 1) was graded as grade 3+, which showed a florid population of reactive polymorphous lymphoid cells in the background (Fig. 5F). The grade 3+ morphology was noted in the hypothyroid case with atrophic thyroid gland.
Follicular neoplasm in LT
Five (n = 5) of the cases presented with clinical features of painless thyroid swelling. One (n = 1) of the cases was known LT with elevated anti-TPO antibodies. All cases (n = 5) were hypothyroid. US in four of the cases (n = 4) showed a well-defined, wider-than-tall iso- to hypoechoic solid nodule, with the rest of the thyroid showing either a pseudonodular appearance (Fig. 6B) or diffusely reduced thyroid parenchymal echogenicity with multiple echogenic septations suggestive of chronic thyroiditis. The fifth case showed a well-defined iso- to hypoechoic solid nodule in the right lobe with punctate microcalcification against a background of diffusely reduced thyroid parenchymal echogenicity with multiple echogenic septations (Fig. 6A). US-guided FNAC of the first four cases (n = 4) revealed moderate to highly cellular smears showing thyroid follicular cells arranged in sheets and in repetitive micro-follicular patterns against a hemorrhagic background with scant or no colloids (Fig. 6D) and scattered lymphocytes, and one of the cases (n = 1) with elevated anti-TPO levels also showed grade 1+ lymphocytic impingement in a few sheets of follicular cells. The cases were diagnosed as follicular neoplasm/ suspicious for follicular neoplasm; Bethesda category IV and histopathological correlation was advised, which showed follicular adenomas in all cases. The last case (n = 1) showed high cellularity with sheets and clusters of thyroid follicular cells, with most of the cells revealing oncocytic changes (Fig. 6C) against a hemorrhagic background with scant colloid, few scattered lymphocytes, and occasional follicular clusters showing lymphocytic impingement (grade 1+). The case was diagnosed as follicular neoplasm, oncocytic type, Bethesda category IV, and was diagnosed as oncocytic adenoma on histopathology.

Follicular neoplasm in the context of lymphocytic thyroiditis. (A) Ultrasonography (US) showing a well-defined iso to hypoechoic solid nodule in the right lobe with punctate microcalcifications against a background of diffusely reduced thyroid parenchymal echogenicity with multiple echogenic septations. (B) Giemsa-stained smear revealing sheets and a repetitive micro-follicular pattern of thyroid cells against a hemorrhagic background. (C) US showing a well-defined hypoechoic solid nodule with surrounding thyroid parenchyma showing a pseudonodular appearance. (D) Giemsa-stained smear showing sheets of thyroid follicular cells with oncocytic change.
DISCUSSION
The age distribution varied between 27-45 years. A notable finding was the female predominance in LT (10/10 cases) and in FN arising in the context of LT (4/5 cases). SAT is more commonly described in females than in males; however, two of the three of our cases (2/3) were males. The one case (1/1) of tuberculous thyroiditis and one case (1/2) of thyroid abscess were also males.
All the cases of AST/thyroid abscess and SAT presented with painful thyroid swellings as expected, while all the LT cases and cases of follicular neoplasm in the context of LT had painless thyroid enlargements. All the cases diagnosed with SAT reported a recent history of severe URTI, which correlates with the etio-pathogenesis of the disease. Both cases of AST/thyroid abscess were previously healthy individuals and reported no history of immunocompromise, human immunodeficiency virus, or trauma. However, one of the cases was a pregnant female with recent past history of root canal treatment. The development of acute suppuration could be attributable to hypertrophy and hyperplasia of the thyroid gland owing to increased levels of circulating human chorionic gonadotropin that tend to cross bind to TSH receptors [19]. The literature regarding association of both pregnancy and root canal treatment with acute suppuration of thyroid gland is, however, scant. On subsequent follow-up, the case with tuberculous thyroiditis also tested positive for CB-NAAT and responded well to ATT. The tuberculous infection was likely confined to the thyroid gland, as the chest X-ray and abdominal US showed normal findings with no cervical or axillary lymphadenopathy. This was a rare occurrence. The initial US also showed no extra-thyroidal extension, ruling out the possibility of secondary involvement of thyroid from any adjacent cervical lymph node. On subsequent US, the case of tuberculous thyroiditis showed complete effacement and distortion of the thyroid parenchyma with internal echoes; similar findings were described by Baidya et al. [20], in which they described multiple variably sized cysts in both lobes of the thyroid [20]. Tuberculous thyroiditis is rare, with scant treatment in the literature [16]. The cases of thyroid abscess showed moving internal echoes in one case and ill-defined heterogeneously hypoechoic focal lesion with extrathyroidal extension in the other. SAT on US showed ill-defined hypoechoic wider-than-tall focal nodules with normal-sized gland in two of the cases and minimally enlarged, heterogeneous-appearing thyroid gland with multiple ill-defined hypoechoic nodules in the third case. All cases showed reduced vascularity on color Doppler in the affected areas of the gland, but with absent hypervascularity in the surrounding normal thyroid parenchyma, as described in the literature in cases of SAT. This allows differentiation from AST, which shows increased vascularity in the surrounding thyroid parenchyma [21-23]. Ill-defined hypoechoic lesions can sometimes be confused with malignant lesions, and FNAC is often advised in these cases [22]. The cases of LT showed a spectrum of US findings varying from a pseudonodular appearance, diffuse thyroid enlargement with reduced echogenicity, to an atrophic thyroid gland. In the literature, LT has also been variably described and broadly classified into nodular and diffuse forms. The diffuse forms initially can show a nodular appearance and can eventually progress to complete atrophy of the gland [23].
The cytology in AST/thyroid abscess cases typically revealed numerous neutrophils with few histiocytes, indicative of abscess formation. The case of tuberculous thyroiditis on FNA yielded caseous aspirate revealing a necrotic background with scattered neutrophils and occasional AFB on ZN staining using 20% H2SO4. Normally, tuberculous infection presents as giant cells and epithelioid cell granulomas, but the presence of extensive necrosis could possibly be due to long-standing and untreated illness [24]. SAT cases showed neutrophils, occasional epithelioid cell granulomas, and lymphocytes with a paucity of thyroid follicular cells and a recent history of URTI. The presence of neutrophils and neutrophilic micro-abscesses were noted in both acute and subacute cases and need to be differentiated as both can present with painful thyroid swellings. AST will show a predominance of neutrophils, with degenerating cellular debris in the absence of lymphocytes, epithelioid cell granulomas, and giant cells [12]. In addition to varying degrees of lymphocytic impingement, histiocytic giant cells and epithelioid cell granulomas were observed in a majority of the cases (7/10) of LT, whereas SAT cases showed both neutrophils and epithelioid cell granulomas with a paucity of thyroid follicular cells. Colloid was scant in all cases. Most of the cases (n = 9) of LT showed grade 2+ impingement of lymphocytes, except for one case that showed grade 3+ impingement against a reactive polymorphous population of lymphoid cells. All the cases of FN with LT showed a lymphocytic colloid-free hemorrhagic background, and grade 1+ impingement by lymphocytes was seen in two of the cases. The majority of the cases showed sheets of repetitive micro-follicles as described in the literature, with one of the cases showing a predominant oncocytic morphology. The literature describes the association of LT with thyroid lymphomas and papillary carcinoma thyroid; however, there are limited data regarding its association with FN.
In conclusion, thyroiditis is commonly encountered by clinicians, pathologists, and radiologists. Evaluation of the symptoms with the US findings and FNAC can greatly help in the diagnosis and decrease mortality rates, especially in cases with AST. SAT can present with a characteristic history of previous viral infection, painful thyroid swelling, and the presence of both neutrophils and granulomas on FNAC. LT is one of the most common types of thyroiditis, frequently associated with granulomas and epithelioid giant cells, predominantly seen in females. AST/thyroid abscess and tuberculous thyroiditis are rare entities in clinical practice. This study aims to assess the clinical, cytomorphological, and radiological findings of common and uncommon forms of thyroiditis; however, the study is limited by the small number of cases included. A larger sample size is planned for future work.
Notes
Ethics Statement
All procedures performed in the current study were approved by the IRB and/or national research ethics committee (EC-2024-1145 and 7 July 2024) in accordance with the 1964 Helsinki Declaration and its later amendments. Informed consent was obtained from all individual participants included in the study.
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Code Availability
Not applicable.
Author Contributions
Conceptualization: AN. Data curation: AN, IK. Formal analysis: AN, IK. Investigation: AN, IK. Methodology: AN, IK. Supervision: AN, IK. Validation: AN, IK. Visualization: AN, IK. Writing—original draft: AN, IK. Writing—review & editing: AN, IK. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
No funding to declare.


