Clinically undetected plasmacytoid urothelial carcinoma of the urinary bladder with non-mass-forming metastases in multiple organs: an autopsy case
Article information
Abstract
This case report outlines a clinically undetected urinary bladder plasmacytoid urothelial carcinoma (PUC) with multiple metastases detected at autopsy. An 89-year-old man presented with edema in the lower limbs. Pleural fluid cytology revealed discohesive carcinomatous cells, although imaging studies failed to identify the primary site of tumor. The patient died of respiratory failure. Autopsy disclosed a prostate tumor and diffusely thickened urinary bladder and rectum without distinct tumorous lesions. Histologically, the tumor consisted of acinar-type prostate adenocarcinoma with no signs of metastasis. Additionally, small, plasmacytoid tumor cells were observed in the urinary bladder/rectum as isolated or small clustering fashions. These metastasized to the lungs, intestine, generalized lymph nodes in a non-mass-forming manner. Combined with immunohistochemical studies, these tumor cells were diagnosed PUC derived from the urinary bladder. Both clinicians and pathologists should recognize PUC as an aggressive histological variant, which can represent a rapid systemic progression without mass-forming lesions.
Plasmacytoid urothelial carcinoma (PUC) was first reported in 1991 as a rare histologic variant of urothelial carcinoma (UC) characterized by isolated tumor cells that morphologically resemble plasma cells with eccentric nuclei and eosinophilic cytoplasm [1–3]. In addition to its high risk of peritoneal spread, positive margins at cystectomy, and tumor recurrence, PUC has been recognized as an independent prognostic factor for poor prognosis in patients with urinary bladder carcinoma [4]. PUC may pose a significant diagnostic problem, particularly when it occurs in its exclusively pure or predominant pattern in a limited biopsy, cytology, or transurethral resection specimen. Moreover, reflecting an infiltration pattern arranged as diffuse, thick sheets, cords, or nests of small discohesive tumor cells without forming a focal mass [5], it is challenging to detect PUC via imaging procedures [6,7]. Initial manifestations of PUC may include distant metastasis or peritoneal dissemination [8]. Thus, a generalized histological analysis is required to precisely assess the spreading/metastasis of the tumor. However, there are only a limited number of autopsy case reports on PUC [7–10]. Herein, we describe a case of urinary bladder PUC that was initially recognized as a “carcinoma of unknown origin” through pleural fluid cytology, but an autopsy revealed extensive locoregional spreading and distant metastasis of the tumor.
CASE REPORT
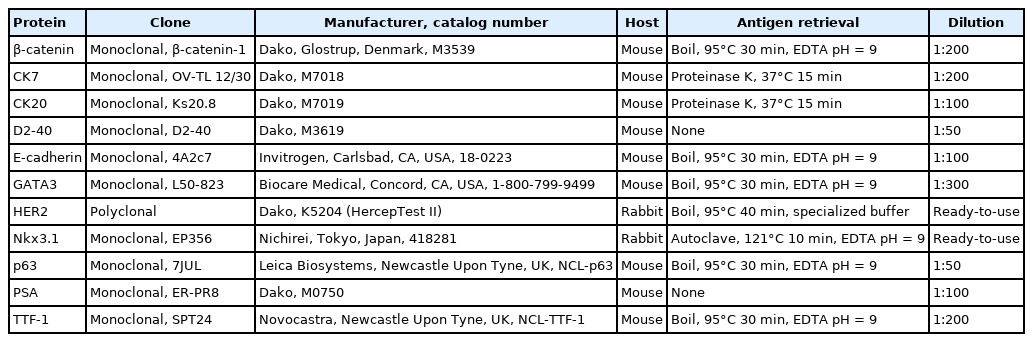
An 89-year-old Japanese man was admitted to our hospital with severely edematous lower limbs. The patient was diagnosed with prostate cancer at the age of 80 and received hormone therapy for 8 years. Because of atypical urothelial cells in urine smear cytology, he underwent transurethral resection of bladder tumor (TURBT) 1 year and 4 months before admission, that revealed UC in situ with a stromal microinvasion (Fig. 1A). A follow-up abdominal computed tomography (CT) scan taken 3 months before admission showed thickening of the rectal wall; however, no significant deformation was found in the urinary bladder. At the time of admission, a high level of carbohydrate antigen 19-9 (2,771 U/mL; normal, < 37 U/mL) was detected in serum, whereas levels of carcinoembryonic antigen and prostate-specific antigen (PSA) were normal.
Premortem microscopic findings. (A) Transurethral resection specimen showing urothelial carcinoma in situ with a stromal microinvasion. (B) Discohesive carcinomatous cells with signet-ring or plasmacytoid features in the cell block from pleural fluid was noted. Gross examination at autopsy. (C) Anterior view of the gross description of the pelvic organs. (D) A prostate tumor protruding into the urethra is detected (arrowheads). Around this tumor, the rectal wall and posterior wall of the urinary bladder are diffusely thickened.
Following admission, bilateral pleural effusion progressed, and pleural fluid smear/cell block cytology revealed discohesive carcinomatous cells (Fig. 1B) that were immunoreactive for cytokeratin (CK) 7 and CK20 and negative for PSA and thyroid transcription factor-1. Various organs, including the stomach, bile duct, pancreas, and urinary tract, were speculated to be the origin of tumor. However, fluorodeoxyglucose positron emission tomography/CT scan taken 20 days after admission failed to detect any primary lesions (i.e., carcinoma of unknown origin). The patient’s respiratory function gradually deteriorated because of aspiration pneumonia. The patient was treated with only palliative therapy and died 27 days after admission. An autopsy was performed on the same day (postmortem, 7 hours).
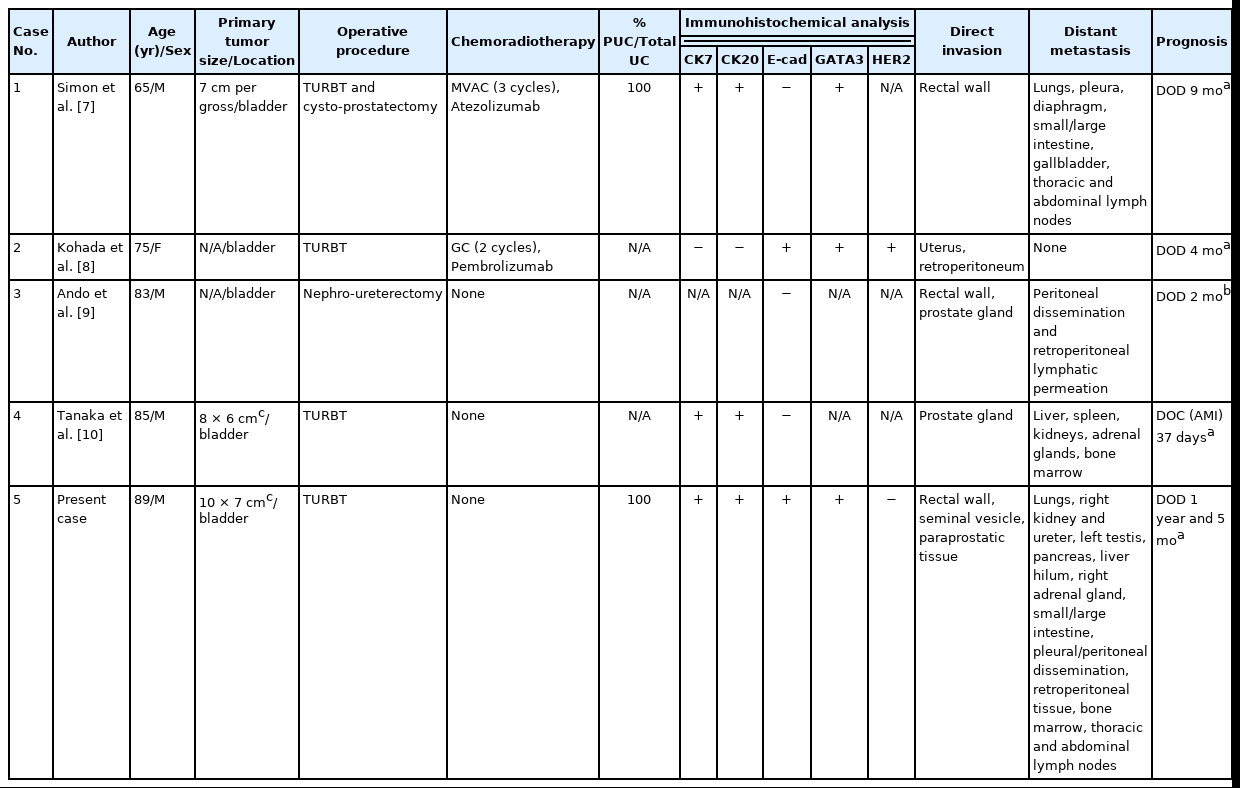
Grossly, a prostate tumor measuring 3.5 cm in the largest diameter, protruding into the urethra, was detected. Around this tumor, the rectal wall and posterior wall of the urinary bladder were diffusely thickened, but no other mass-forming lesions were observed in the whole body examined (Fig. 1C, D). Histologically, the prostate tumor showed fused-gland features of acinar-type adenocarcinoma, Gleason Grade Group 4, extending to the rectal wall and urethra. Examination of the thickened urinary bladder wall revealed diffuse infiltration of discohesive, plasmacytoid tumor cells in a single file pattern and small nests in the edematous lamina propria (Fig. 2A), muscularis propria (Fig. 2B), and perivesical adipose tissue. The individual tumor cells displayed oval-to-round eccentrically located nuclei and abundant densely eosinophilic and occasionally vacuolated/signet-ring-cell-like cytoplasm (Fig. 2C). The tumor was exposed to the serosal surface of the urinary bladder and massively extended into the thickened rectal wall, seminal vesicles, and periprostatic tissue, surrounding the prostate cancer (Fig. 2D). Autopsy failed to detect any colorectal intramucosal lesions of the tumor.
Microscopic findings. (A, B) The thickened lesion in the urinary bladder wall, showing diffuse infiltration of discohesive, plasmacytoid tumor cells in a single file pattern and small nests in the edematous lamina propria (A) and muscularis propria (B). (C) The plasmacytoid tumor cells consisted of oval-to-round, eccentrically located nuclei and abundant densely eosinophilic and occasionally vacuolated/signet-ring-cell like cytoplasm. (D) Massive tumor extension into the thickened rectal wall, seminal vesicles, and periprostatic tissue (arrows) close to the prostate cancer (arrowheads) is observed. (E, F) Diffuse positive immunoreactivity for GATA binding protein 3 (E) and negative immunoreactivity for NK3 homeobox1 (F) in the plasmacytoid tumor cells (arrows, both E and F), and vice versa, in the prostate cancer cells (arrowheads, both E and F) is observed.
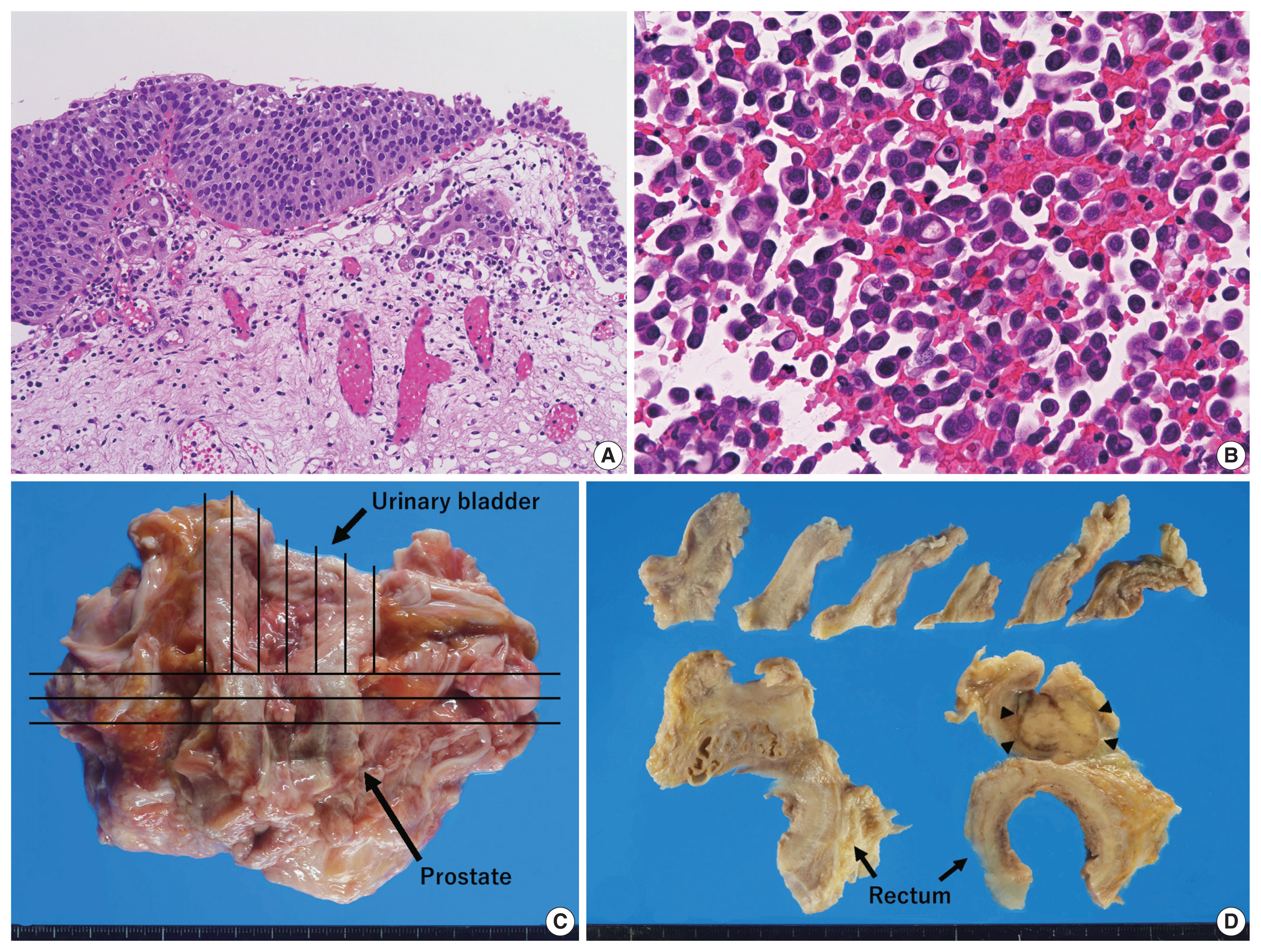
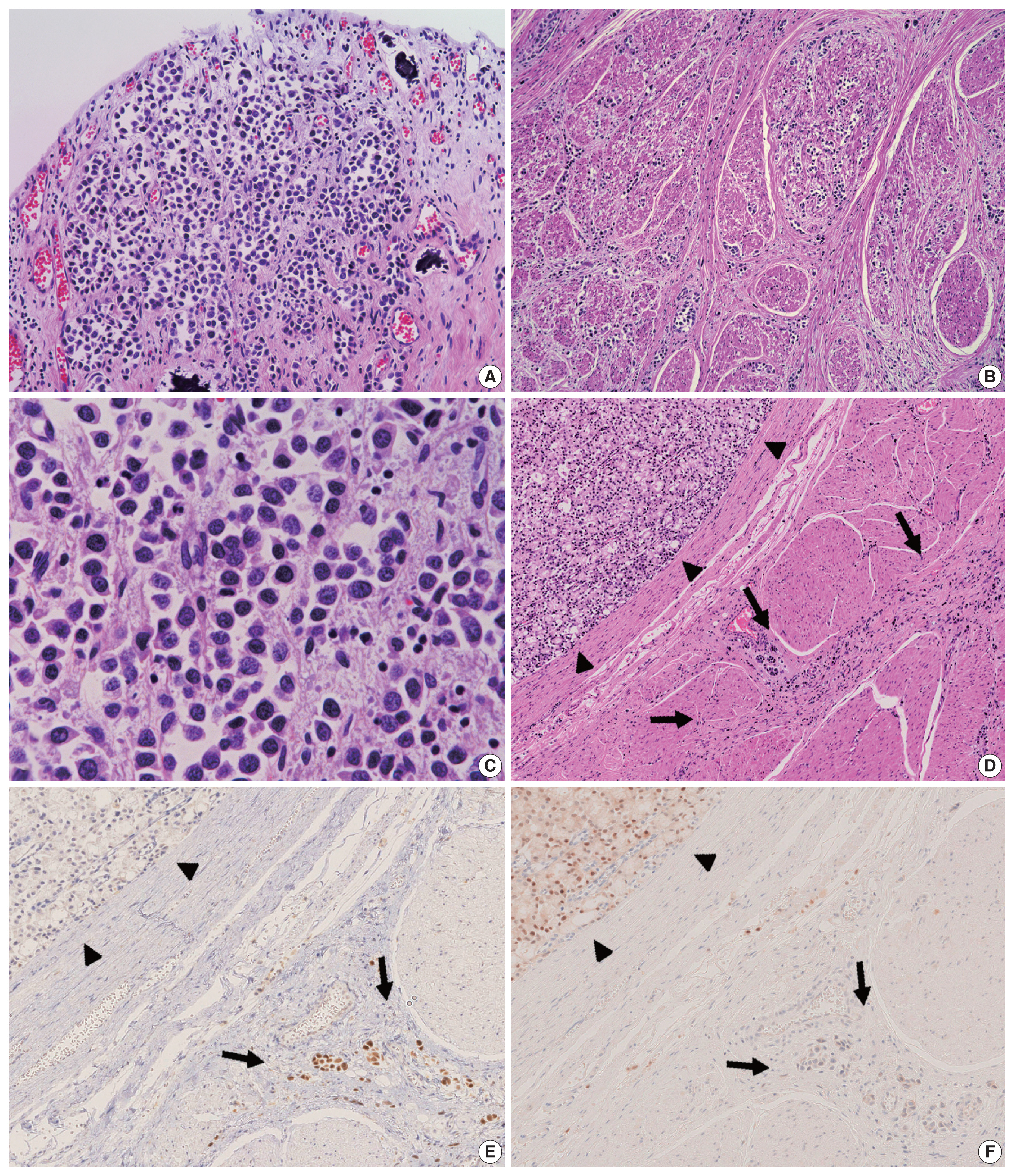
Characteristics of primary antibodies used in immunohistochemical analysis are summarized in Table 1. Immunohistochemically, the plasmacytoid tumor cells were diffusely positive for CK7, CK20, p63, and GATA binding protein 3 (GATA3) and negative for NK3 homeobox 1 (Nkx3.1), while the opposite was observed in the prostate cancer cells (i.e., Nkx3.1+ and CK7/CK20/p63/GATA3−) (Fig. 2E, F). The plasmacytoid tumor cells were also negative for CDX2 and nuclear β-catenin. Immunoreactivity for E-cadherin was retained in the plasmacytoid tumor cells, and that for human epidermal growth factor receptor 2 (HER2) had a score of 2+ (Fig. 3A). PathVysion HER2 DNA probe kit (HER2 SpectrumOrange/CEP17 SpectrumGreen DNA probes, Abbott Molecular, Downers Grove, IL, USA) was used for fluorescence in situ hybridization analysis, as described previously [11]. Hybridization was performed between the denatured probes and denatured DNA on tissue sections at 37°C for 14–18 hours. The sections were counterstained with 4,6-diamidino-2-phenylindone. The number of fluorescence signals from both centromeric region of chromosome 17 (CEP17) and HER2 probes in the 40 interphase tumor cell nuclei was counted. The HER2/CEP17 ratio and mean HER2 signal were less than 2.0 and 4.0, respectively (Fig. 3B). PUC in the present case showed no HER2 amplification. Based on these findings, the urinary bladder tumor was diagnosed as PUC that histologically involved an area measuring 10 × 7 cm.
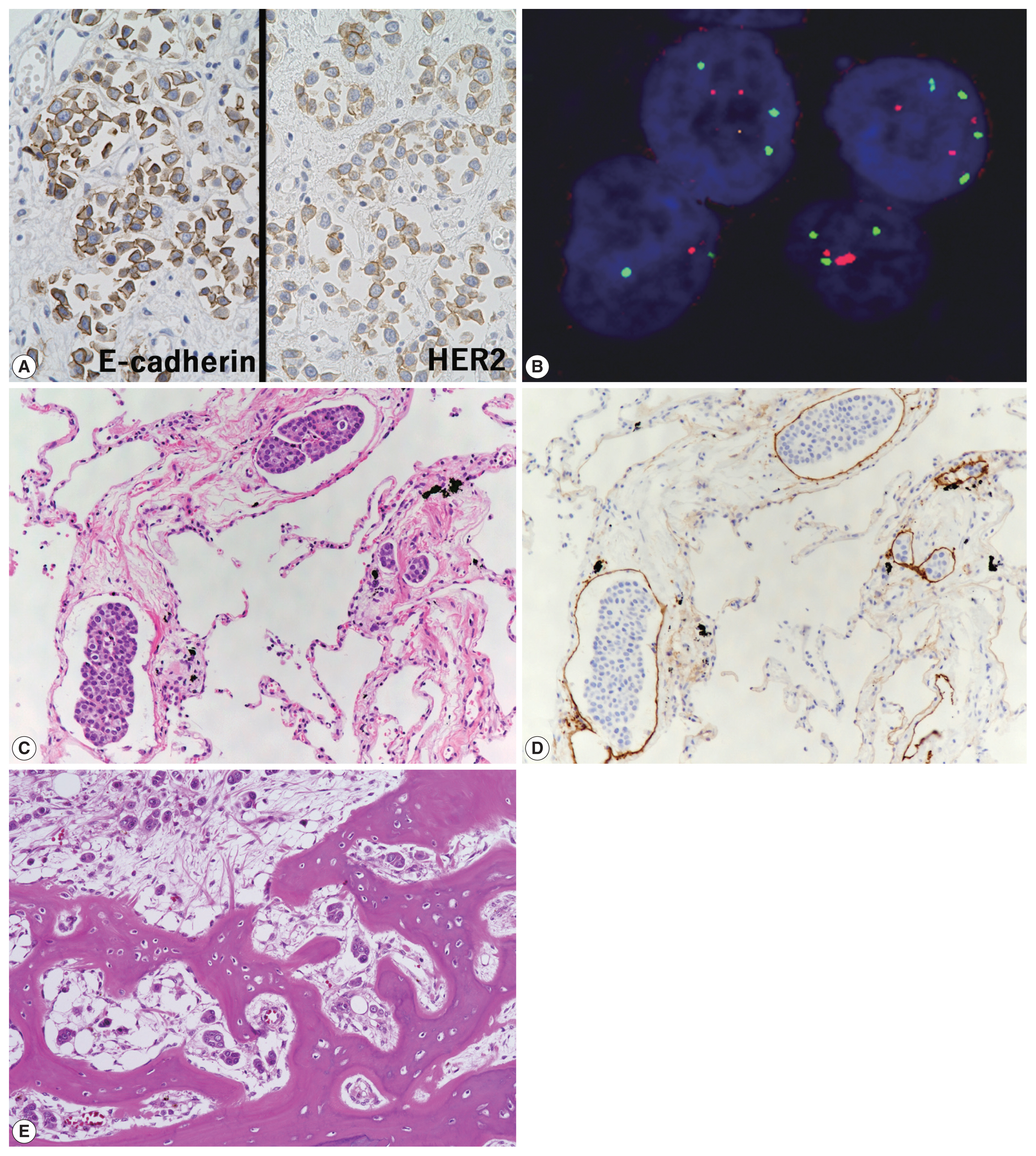
(A) Retained immunoreactivity for E-cadherin and moderate-intensity immunoreactivity for human epidermal growth factor receptor 2 (HER2) were noted in cancer cells. (B) Fluorescence in situ hybridization for the copy number of HER2 gene showing no HER2 amplification in cancer cells. DAPI-counterstained interphase nuclei are observed; the red and green signals indicate the HER2 and CEP17 signals, respectively. (C) Metastatic small clusters or isolated cancer cells in the lungs. (D) Immunostaining for D2-40 highlighting lymphatic invasion of cancer cells. (E) Metastatic cancer cells in the sacral bone marrow.
Non-mass-forming multiple metastases of PUC were found in the lungs (bilateral), jejunum, sigmoid colon, sacrum, and generalized lymph nodes and in peritoneal and pleural disseminations, with or without lymphatic invasion (Fig. 3C–E). No features of conventional UC were found in the primary and metastatic sites. Autopsy failed to detect distant metastases of the prostate cancer.
DISCUSSION
Emerging evidence demonstrates that PUC is associated with adverse clinicopathological features, advanced stage at cystectomy, and poor prognosis [3,12–16]. In a recent meta-analysis of eight case series, PUC of the bladder showed a higher frequency of pathological stage ≥ T3, increased risk of perivesical/ureteral margin positivity, and lymph node metastasis, and elevated overall mortality rate compared to conventional UC [4]. While early tumor detection and accurate evaluation of tumor spreading are important for proper clinical management of PUC [3], its unique non-mass-forming progression makes it difficult to diagnose. Some reports indicate that PUCs tend to invade along the perirectal/perivesical fascial plane [12,15,16], which is usually challenging to detect using conventional CT/magnetic resonance imaging [6]. In the present case, autopsy showed an extensive local spreading to the perivesical fascial plane and generalized metastases of the tumor; however, it could not be detected via clinical imaging. PUC of the bladder is a rare disease; most histological data in previous case series were only from TURBT or cystectomy specimens. We suggest that the lack of data regarding precise histological evaluation of such generalized disease (i.e., autopsy study) is one of the major factors that makes clinical/imaging analysis of PUC difficult.
Only four other autopsy cases of PUC have been reported to date [7–10]. The clinicopathological features of these cases (cases 1–4) and the present case (case 5) are summarized in Table 2. In all five cases, the primary tumor location was the bladder, and four patients were men. The percentage of PUC in the total UC area was described in only one case (case 1); the tumor was a pure type PUC, similar to that in the present case. Immunohistochemically, three of four cases (75%) were positive for CK7 and CK20, three of three cases (100%) were positive for GATA3, and loss of E-cadherin staining was detected in three of five cases (60%). In cases 1, 2, and 4, PUC was diagnosed using TURBT specimens. In the present case, TURBT revealed only a minor amount of stromal invasion of cancer cells. However, no obvious detrusor muscle was detected in the whole specimen, indicating a high risk of residual tumor. In this context, if re-TURBT had been performed, the PUC invading the muscle layer might have been disclosed. All cases showed direct invasion of tumor to adjacent organs, and cases 1 and 3 showed progression along the perirectal fascial plane, similar to that seen in the present case. In all cases except case 2, multiple distant metastases were found in the intra-abdominal organs (cases 1, 3–5), thoracic cavity (cases 1 and 5), and bone (cases 4 and 5). PUC was the main cause of death in all cases except for case 4 (myocardial infarction), and all five patients died within 2 years from the initial diagnosis of the tumor.
In the present case, although plasmacytoid carcinomatous cells were detected during pleural fluid cytology, we could not consider those in relation to the conventional UC in the previous TURBT specimens. PUC is often observed at advanced stages with metastasis [6], and its differential diagnosis includes a wide variety of diseases such as signet-ring cell adenocarcinoma (especially colorectal origin due to the perirectal spreading pattern of PUC), carcinoma with rhabdoid features, lymphoma/myeloma, and melanoma [13]. The first case of PUC was also identified in a bone metastatic lesion and was reported to mimic a myeloma [1]. In such situations, the possibility of PUC should be recognized initially, and effective immunohistochemical analysis should be performed. GATA3 is the most sensitive marker for tumors derived from urinary epithelium, and CDX2/β-catenin might be useful to distinguish PUC from colorectal signet-ring adenocarcinoma [17]; hence, these markers should have been included in our immunohistochemical panel for pleural fluid cytology examination for diagnosing the present case. Although loss of E-cadherin expression is observed in 70%–80% of cases and is thought to be one of the diagnostic hallmarks of PUC [18], its frequency was found to be 57% in another case series [17]. Retention of cytoplasmic expression of E-cadherin is not sufficient to rule out PUCs.
Although there was moderate immunoreactivity for HER2, no gene amplification was detected in the tumor cells in the present case. A recent molecular study of 1005 UC cases revealed that HER2 gene amplification was found in approximately 10% of the cases, and concluded that anti-HER2 antibody is expected to be applied to the novel standard treatment of UC [19]. Interestingly, HER2 amplification is one of the features characterizing “luminal unstable” type in the recent consensus molecular classification, which is enriched in plasmacytoid histology of the bladder UC [20]. Further investigations directed towards HER2 status and the effectiveness of HER2-targeted therapy for this aggressive variant of UC are required.
In summary, we described a case of clinically undetected PUC that was initially identified as a “cancer of unknown primary” through pleural fluid cytology but autopsy revealed broad local spreading and multiple organ metastasis. This rare form of UC should be considered in the differential diagnosis of aggressive occult tumors. Data accumulation and analysis of additional autopsy case reports are essential to clarify the peculiar non-mass-forming spread of PUC, which can help in its early detection.
Acknowledgments
We thank Mr. Susumu Tominaga and Ms. Chinami Onuma (National Defense Medical College) for their excellent technical assistance.
Notes
Ethics Statement
This single case report in exempted submission to Institutional Review Board and subsequent informed consent by the National Defense Medical College, Tokorozawa, Japan (Registration number, 4007; decision date, August 8, 2021).
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Author Contributions
Conceptualization: YA, KM. Data curation: YA, KM. Formal analysis: KM. Investigation: YA, KM, SY. Methodology: KM. Resources: SM. Supervision: MS, KI, SM. Visualization: KM. Writing—original draft: YA, KM. Writing—review & editing: SY, MS, KI, SM. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
No funding to declare.