Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 52(6); 2018 > Article
-
Letter to the Editor
Alveolar Squamous Cell Metaplasia: Preneoplastic Lesion? -
Adriana Handra-Luca,1,2

-
Journal of Pathology and Translational Medicine 2018;52(6):355-356.
DOI: https://doi.org/10.4132/jptm.2018.09.07
Published online: October 1, 2018
1Service d’Anatomie Pathologique, APHP GHU Avicenne, Bobigny, France
2Universite Paris Nord Sorbonne Cite, Bobigny, France
- Corresponding Author Adriana Handra-Luca, MD, PhD Service d’Anatomie Pathologique, APHP GHU Avicenne, Universite Paris Nord Sorbonne Cite, 125 rue Stalingrad, 93009 Bobigny, France Tel: +33-148955555 (deck 52047), Fax: +33-14895555602/5480 E-mail: 'adriana.handra-luca@aphp.fr', 'adriana.handra-luca@hotmail.com'
• Received: August 27, 2018 • Accepted: September 7, 2018
© 2018 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 4,021 Views
- 108 Download
-
Conflicts of Interest
No potential conflict of interest relevant to this article was reported.
Notes
Acknowledgments
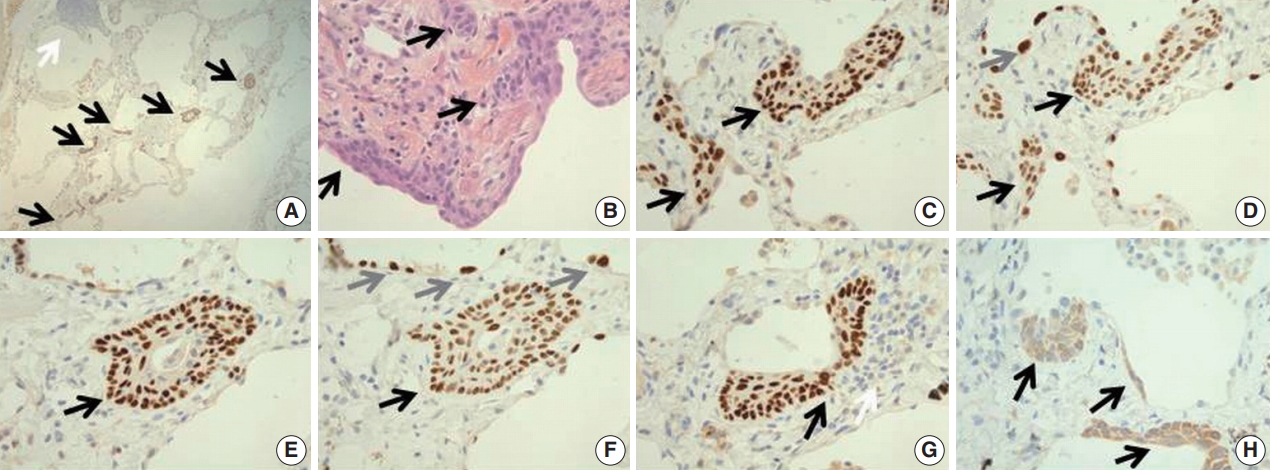
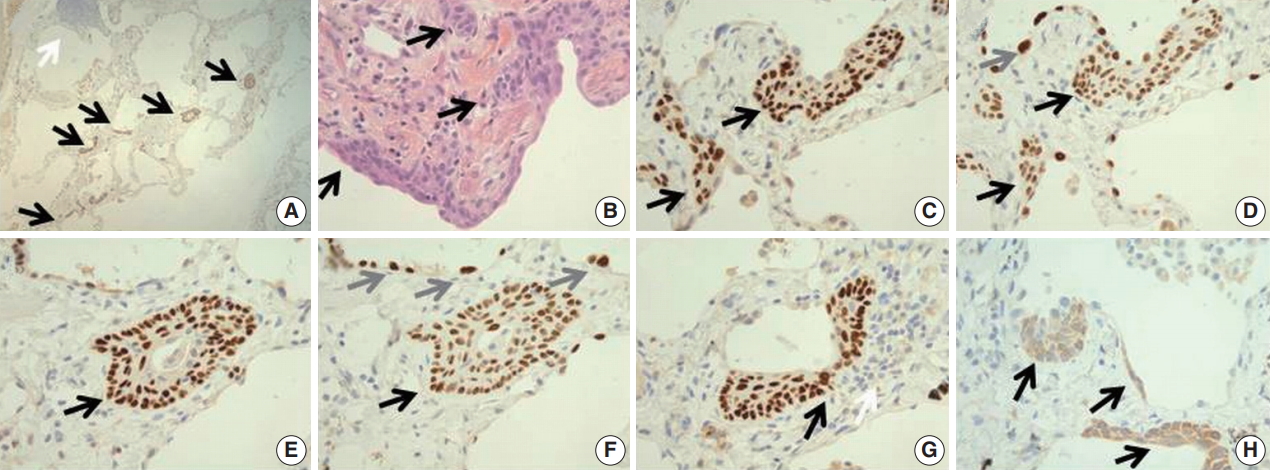
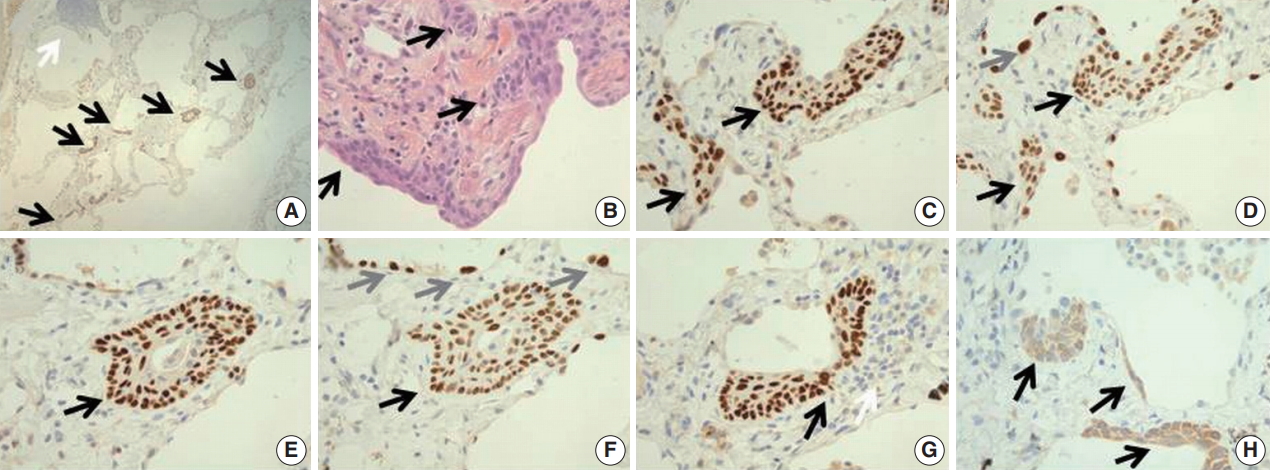
Fig. 1.(A) The lung parenchyma shows a zone of multiple (approximatively 10) p63-positive squamous cell metaplasia (SCM) foci (black arrows for SCM foci, white arrow for lymphocytic focus). (B) On the hematoxylin and eosin stained slide, the lesions consist in a multilayered epithelium composed of basal cuboidal cells, suprabasal cells and superficial spindle-appearing cells (black arrows). (C) The basal and suprabasal cells are immunoreactive for p63 while superficial cells are negative (black arrows for p63+ cells). (D) Thyroid transcription factor 1 is expressed by the cells throughout the entire thickness of the lesion, in both p63+ and p63– cells (black arrows for SCM foci, gray arrow for atypical pneumocyte nuclei). (E, F) A cystic cellular bud (reminiscent of thyroid solid cell nests) is detected in an alveolar septum (black arrows for the SCM bud, gray arrows for binucleated pneumocytes). (G) One of the SCM foci develop at close contact to the lymphocytic infiltrate (p63 immunohistochemistry, black arrow for the SCM focus, white arrow for the lymphcytic infiltrate). To note would be the presence of a binucleation with immunoreactivity to p63 in the SCM focus. (H) Cytokeratin 5/6 is expressed in spindle-appearing cells lining the alveoli and in the SCM foci (black arrows for cytokeratin 5/6+ cells).
- 1. Song DH, Choi IH, Ha SY, et al. Usual interstitial pneumonia with lung cancer: clinicopathological analysis of 43 cases. Korean J Pathol 2014; 48: 10–6. ArticlePubMedPMC
- 2. Meyer EC, Liebow AA. Relationship of interstitial pneumonia honeycombing and atypical epithelial proliferation to cancer of the lung. Cancer 1965; 18: 322–51. ArticlePubMed
- 3. Rosai J. Rosai and Ackerman’s surgical pathology. 10th ed. Philadelphia: Elsevier Mosby, 2011.
- 4. Chilosi M, Poletti V, Murer B, et al. Abnormal re-epithelialization and lung remodeling in idiopathic pulmonary fibrosis: the role of deltaN-p63. Lab Invest 2002; 82: 1335–45. ArticlePubMed
- 5. Zuo W, Zhang T, Wu DZ, et al. p63(+)Krt5(+) distal airway stem cells are essential for lung regeneration. Nature 2015; 517: 616–20. ArticlePubMedPDF
- 6. Kato E, Takayanagi N, Takaku Y, et al. Incidence and predictive factors of lung cancer in patients with idiopathic pulmonary fibrosis. ERJ Open Res 2018; 4: 00111–2016. Article
- 7. Krimsky W, Muganlinskaya N, Sarkar S, et al. The changing anatomic position of squamous cell carcinoma of the lung: a new conundrum. J Community Hosp Intern Med Perspect 2016; 6: 33299.ArticlePubMed
References
Figure & Data
References
Citations
Citations to this article as recorded by 

 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure

 E-submission
E-submission