Esophageal Squamous Cell Carcinoma In Situ Overlying Leiomyoma Mimicking Invasive Cancer: A Brief Case Report
Article information
Leiomyoma is the most common benign submucosal mesenchymal tumor of the esophagus, and squamous cell carcinoma is most common epithelial tumor of the esophagus. However, esophageal squamous cell carcinoma overlying leiomyoma has rarely been reported. Herein, we report a case of esophageal squamous cell carcinoma in situ overlying leiomyoma. In addition, we reviewed other reported cases of esophageal squamous cell carcinoma overlying leiomyoma.
CASE REPORT
An asymptomatic 53-year-old man underwent esophagogastroduodenoscopy as a health checkup. Esophagogastroduodenoscopy revealed an elevated mass, 1.8 cm in diameter, with irregular central small erosion in the upper thoracic esophagus. The lesion was clearly identified as a non-staining area by Lugol's iodine solution (Fig. 1A). By the endoscopic biopsy, the lesion was diagnosed as squamous cell carcinoma in situ with the additional comment of not being able to encounter definite invasion due to the shallowness of the biopsy. The patient underwent subtotal esophagectomy, and a 1.8×1.6-cm-sized, elevated, nodular lesion was identified (Fig. 1B) with a well demarcated, white, solid cut surface (Fig. 1C). The scanning view of the lesion showed a well demarcated submucosal mass with an overlying abnormal epithelial lesion (Fig. 1D). Microscopically, the lesion was a submucosal spindle cell tumor with overlying squamous cell carcinoma in situ (Fig. 2A). Immunohistochemically, the squamous cell carcinoma in situ was strongly positive for p53 (Fig. 2B). The submucosal tumor showed low cellularity, and was composed of interlacing bundles of bland spindle cells without mitosis (Fig. 2C). Immunohistochemical staining showed that the tumor was strongly positive for alpha-smooth muscle actin (Fig. 2D), but negative for CD34, CD117, and S100 (data not shown). Collectively, the lesion was diagnosed as a leiomyoma with overlying squamous cell carcinoma in situ. The patient showed no evidence of recurrence for four years.
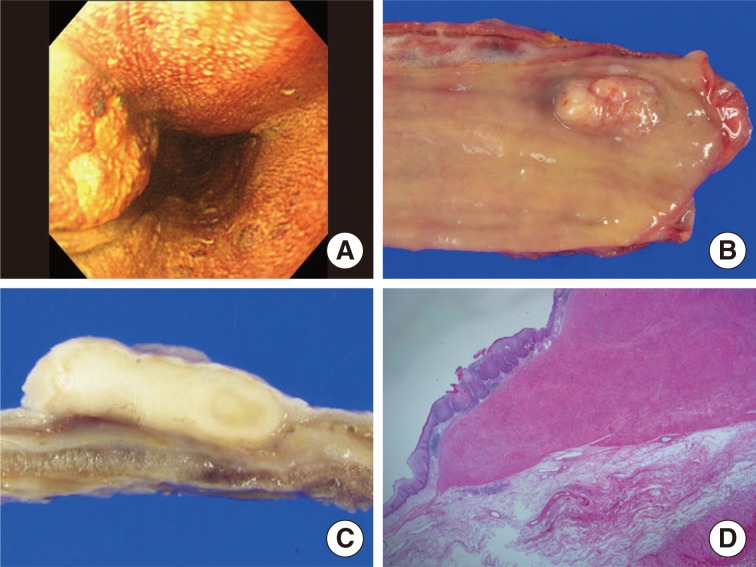
(A) Endoscopic examination reveals an esophageal tumor in the proximal third of the esophagus, clearly identified as a nonstaining area by Lugol's iodine solution. The esophagectomy specimen shows an elevated lesion with central ulcer (B) and the cut surface shows a well demarcated, white, solid mass (C). (D) The scanning view shows a well demarcated submucosal mass with an overlying abnormal epithelial lesion.
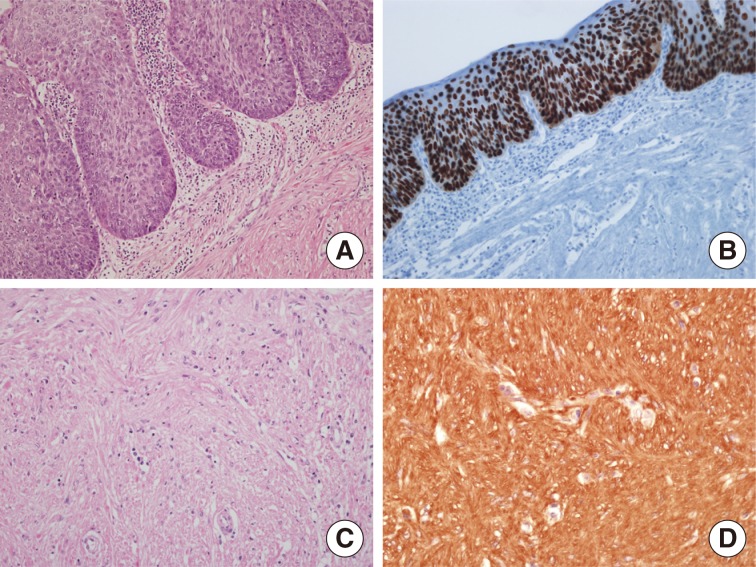
(A) Microscopic findings show squamous cell carcinoma in situ overlying submucosal leiomyoma. (B) The squamous cell carcinoma in situ component shows strong p53 immunopositivity. The submucosal spindle tumor is composed of interlacing bundles of bland spindle cells (C) and is immunoreactive for actin (D).
DISCUSSION
Squamous cell carcinomas and leiomyomas are common epithelial and mesenchymal tumors of the esophagus, respectively. But the coexistence of these two diseases is rare. Regarding their coexistence, however, squamous cell carcinoma and submucosal leiomyoma have been reported as either the overlying type or the separated type.1 Cases with squamous cell carcinoma overlying leiomyoma are extremely rare, and there have only been 15 cases reported, to our knowledge.1,2,3,4,5 All fifteen cases were male. Eight cases underwent esophagectomy, six cases underwent endoscopic mucosal resection and one case underwent blunt excision. Most cases of squamous cell carcinoma overlying leiomyoma were superficial; 12 cases (80%) were confined to within either the intraepithelium or mucosal layer and three cases (20%) showed invasion into muscular layer. Some authors have suggested that the pathogenesis of squamous cell carcinoma overlying leiomyoma probably involves constant chronic stimulation of the esophageal mucosa leading to carcinoma development, because of the intraluminal protrusion of leiomyoma.4 The other theory is that the underlying leiomyoma prevents the dissemination and widespread invasion of the squamous cell carcinoma.5 In the present case, although the biopsy revealed squamous cell carcinoma in situ, the possibility of invasive cancer could not be ruled out due to the irregular erosion in the center of mass. The clinicians could have approached this case with mucosectomy if they were aware of the coexistence of squamous cell carcinoma and leiomyoma using endoscopic ultrasonography (EUS),3 or with more accurate pathologic information regarding the invasion or presence of the submucosal tumor by deep biopsy. In summary, the condition of carcinoma coexisting with underlying leiomyoma is rare and difficult for both pathologists and clinicians to diagnose. To avoid overestimating the extent of tumor invasion and the resultant aggressive radical surgery in such a case, deep biopsy and EUS are recommended.
Notes
No potential conflict of interest relevant to this article was reported.