Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(2); 2012 > Article
-
Case Report
Parathyromatosis: Critical Diagnosis Regarding Surgery and Pathologic Evaluation - Ayşegül Aksoy-Altinboga, Ayşegül Akder Sari, Türkan Rezanko, Mehmet Haciyanli1, Aylin Orgen Calli
-
Korean Journal of Pathology 2012;46(2):197-200.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.2.197
Published online: April 25, 2012
Department of Pathology, Izmir Atatürk Training and Research Hospital, Yesilyurt, Izmir, Turkey.
1Department of General Surgery, Izmir Atatürk Training and Research Hospital, Yesilyurt, Izmir, Turkey.
- Corresponding Author: Ayşegül Aksoy-Altınboga, M.D. Department of Pathology, Izmir Ataturk Training and Research Hospital, Yesilyurt, Izmir 35360, Turkey. Tel: +90-506-4028068, Fax: +90-532-2431530, 'aysegulaksoy@hotmail.com'
• Received: December 23, 2010 • Revised: March 15, 2011 • Accepted: April 18, 2011
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Parathyromatosis, in which several nodules of hyperfunctioning parathyroid tissue form in the neck and mediastinum, is a rare cause of recurrent hyperparathyroidism. However, there are some theories regarding the origin of parathyromatosis, and seeding after rupture of the parathyroid gland capsule during surgical removal of a parathyroid lesions is the most regarded one. Herein, we report a 41-year-old man who presented with multiple parathyroid nodules in and around the left thyroid lobe 5 years after parathyroid surgery for secondary hyperparathyroidism that was finally diagnosed as parathyromatosis. We discuss the differential diagnosis of parathyromatosis from other parathyroid tumors, particularly from parathyroid carcinoma, which is important in the management of a suspected lesion.
- A 41-year-old man with chronic renal failure and secondary hyperparathyroidism, with a serum calcium level of 11 mg/dL and a parathyroid hormone (PTH) level of 1,520 pg/dL, underwent a two-gland total parathyroidectomy. A histopathological examination of the superior and inferior left parathyroid glands revealed hyperplastic nodular parathyroid tissue. After the first operation, his serum calcium and PTH levels decreased to 7.3 mg/dL and 211 pg/mL, respectively. Hyperparathyroidism (PTH, 1,814 pg/mL) and hypercalcemia (calcium, 10.7 to 11.1 mg/dL) recurred 5 years later, and multiple parathyroid nodules were detected on neck ultrasound imaging (USG), which were 8-20 mm in diameter in and around the left thyroid lobe. No pathological lymph node was detected on neck USG.
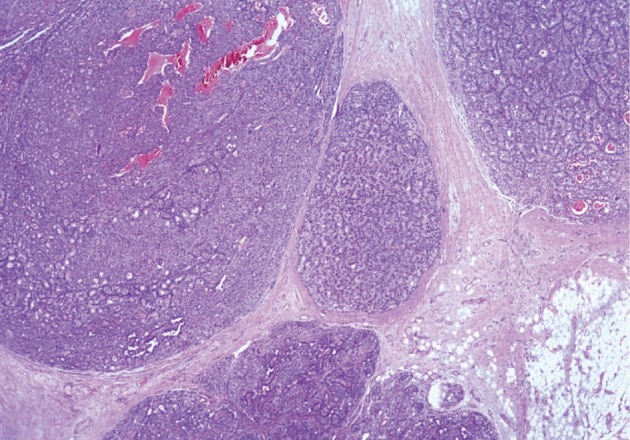
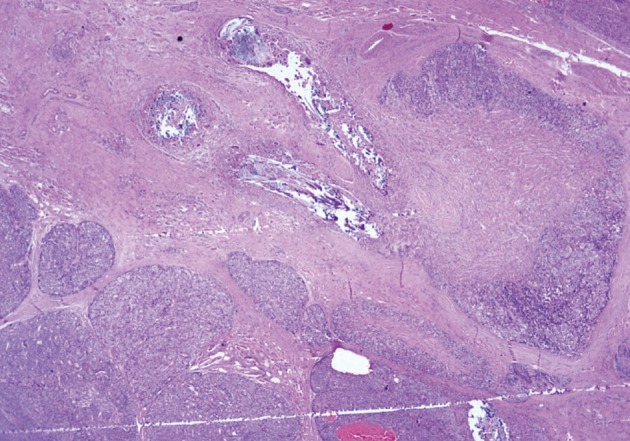
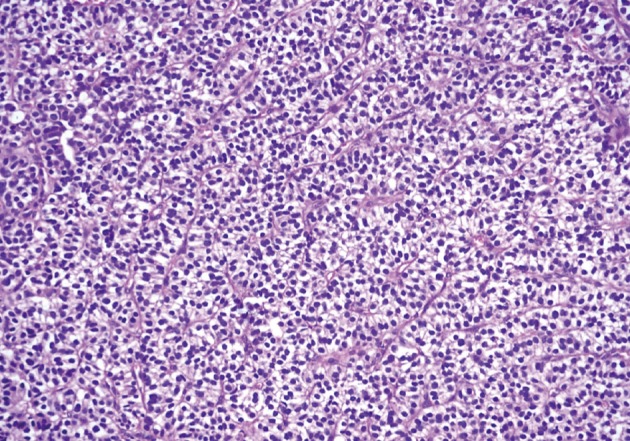
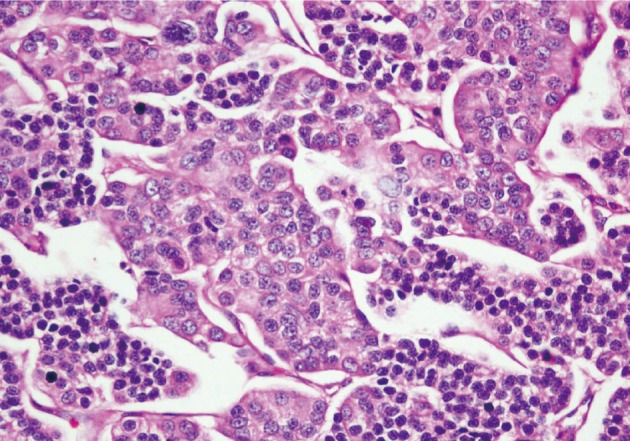
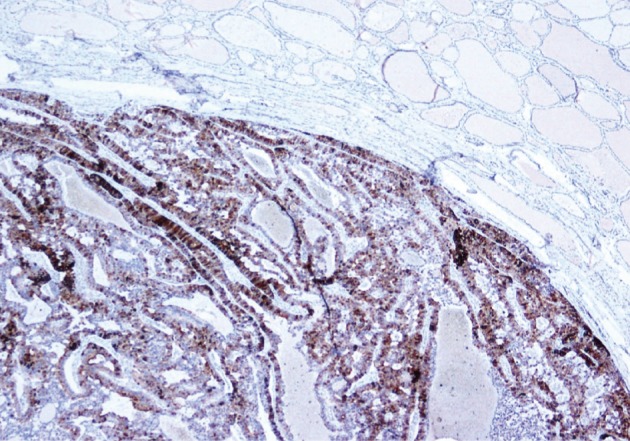
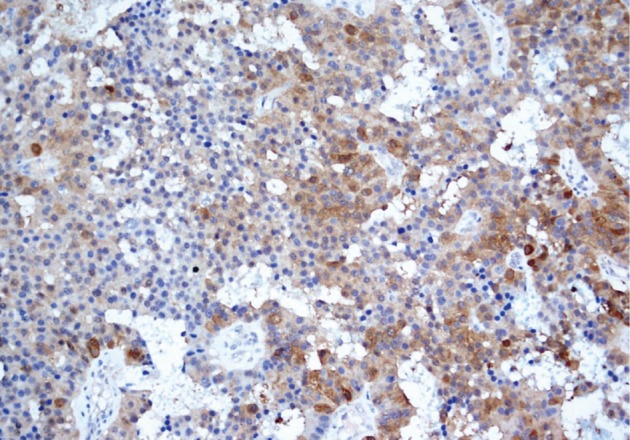
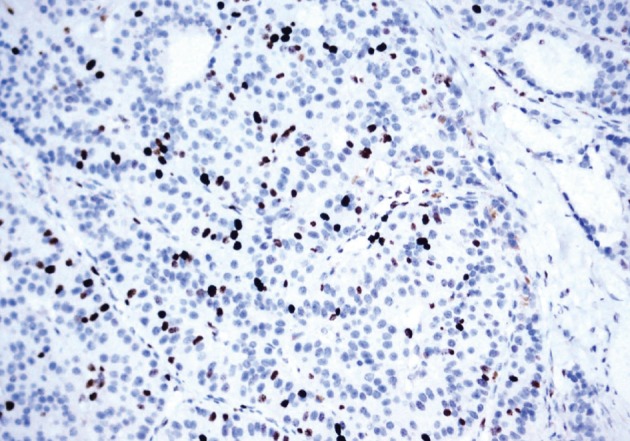
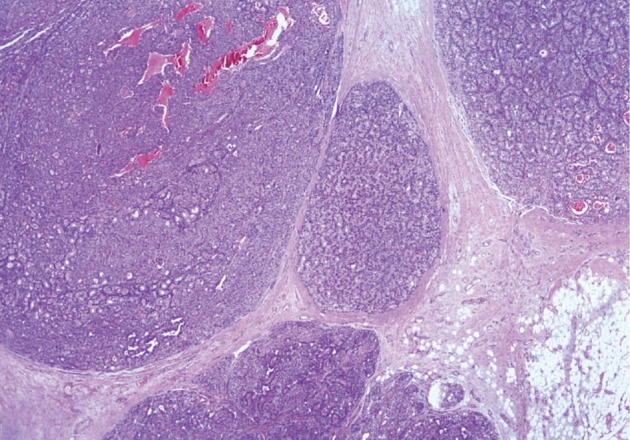
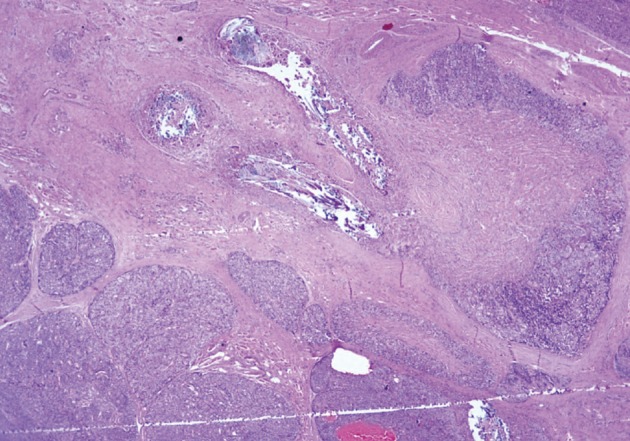
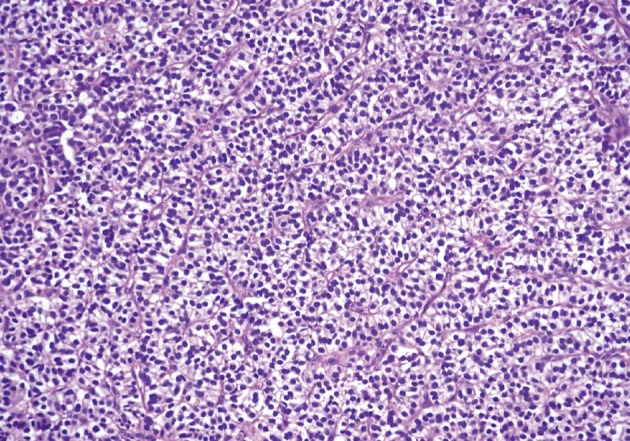
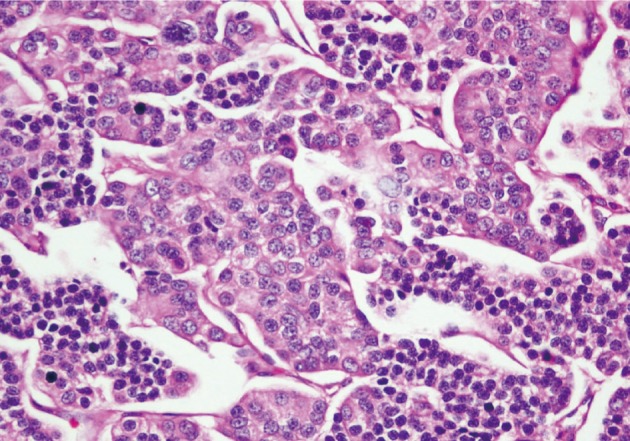
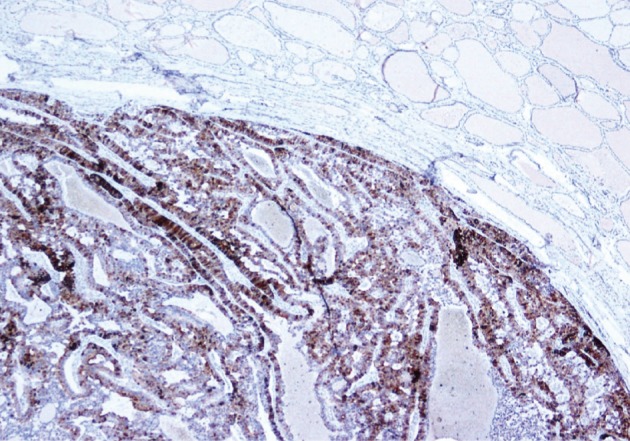
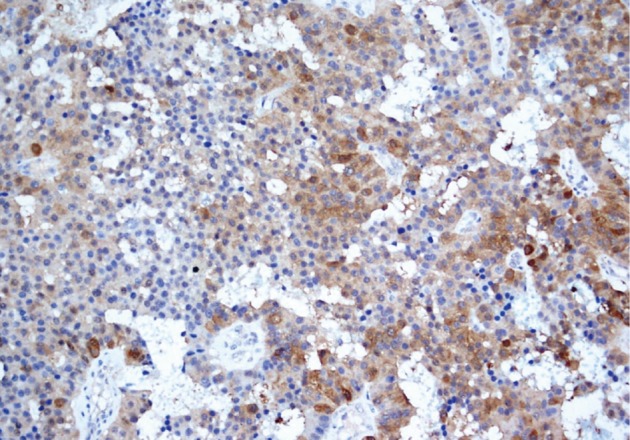
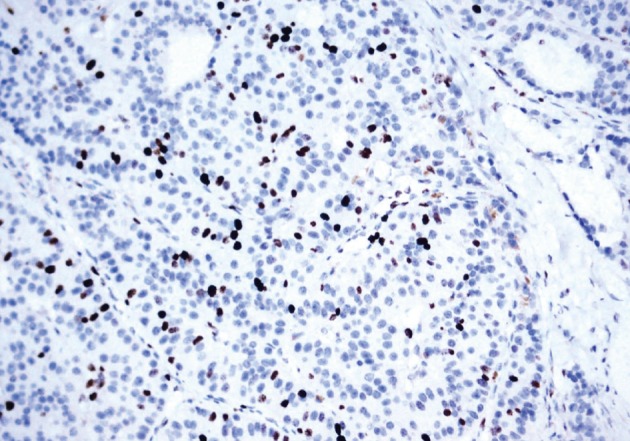
- He underwent surgery again, and the left thyroid lobe with surrounding masses was resected en bloc. The resected tissue showed nodules of varying sizes with smooth edges in the periphery of the left thyroid gland and in the skeletal muscle extending into the thyroid gland. Histopathologically, there were nodular parathyroid tissues of varying cellularity and configurations (Fig. 1). The nodules were round with smooth noninfiltrative borders. In one field, suture material was evident between the nodules, which was surrounded by multinucleated giant cells and indicating the previous operation (Fig. 2). Most of the nodules were composed of uniform cells with clear to amphophilic cytoplasm and small dark nuclei, resembling chief cells (Fig. 3). Nuclear enlargement and a prominent nucleolus were detected in only a few cells of some nodules (Fig. 4). The mitotic rate was 1-2 in 50 high power fields (HPF) but was as high as 7 in 50 HPF in a limited number of fields. Atypical mitoses were not present. No desmoplastic or inflammatory response in or around the nodules was observed, and no vascular invasion was detected. PTH showed a diffuse immunohistochemical staining pattern (Fig. 5) whereas galectin-3 showed focal positivity (Fig. 6) in the parathyroid nodules. The Ki-67 proliferation index was low at 1-2% in most of the fields but was as high as 10% in some fields (Fig. 7).
- His postoperative serum PTH level decreased to 11.5 pg/mL, and his serum calcium level ranged from 6-9.4 mg/dL at different times. The patient was free of recurrence and metastatic disease at the 12 months follow-up.
CASE REPORT
- Parathyromatosis may arise primarily or more commonly secondarily in patients who have had prior neck surgery for secondary hyperparathyroidism.4 Two theories have been suggested for the development of parathyromatosis. The first speculates that parathyromatosis is the result of improper handling of the glands during surgical extirpation, whereas the second defines it as parathyroid gland left behind during ontogenesis that developed under physiological pressure into hyperfunctioning nests of tissue.2 Additionally some authors have proposed a third theory that regards parathyromatosis as a low grade parathyroid malignancy.3 However this theory has not been accepted by further study.
- Parathyroid carcinoma is the main entity to be excluded clinicoradiologically and histopathologically in the differential diagnosis of parathyromatosis. Parathyroid carcinoma is most often associated with primary hyperparathyroidism. Patients with parathyroid carcinoma usually have more profound hypercalcemia and metastases.1 Fernandez-Ranvier et al.1 found that calcium levels were significantly higher (≥14 mg/dL) in patients with parathyroid carcinomas than those in patients with parathyromatosis.
- A differential diagnosis between parathyroid carcinoma and parathyromatosis can be challenging intraoperatively. Parathyroid carcinomas usually present as solitary tumors, whereas parathyromatosis present as small and numerous nodules. In contrast, parathyromatosis is often surrounded by adherent fibrous tissue due to prior surgery, which gives the impression of a parathyroid carcinoma. Intraoperative findings can be challenging for the surgeon who tries to distinguish parathyromatosis from parathyroid carcinoma. Some authors recommend treating all such patients as if their lesions are cancerous, because occult tumors can be present in both conditions.1,5
- Histopathological criteria to diagnose parathyroid carcinoma should include a trabecular growth pattern, thick fibrous trabecula, mitotic figures (>1/10 HPF), capsular invasion, vascular invasion, and lymph node metastases or distant metastasis.1 In contrast to adenomas and primary parathyroid carcinomas, the real capsule is absent in the nests of the parathyroid tissue in patients with parathyromatosis. In the present case, although high mitotic rate focal areas (7/50 HPF), a trabecular growth pattern, and nuclear pleomorphism were present, these did not provide a definitive diagnosis of parathyroid carcinoma alone. Furthermore, all of these features that support the diagnosis of parathyroid carcinoma were also described in patients with parathyromatosis by Fernandez-Ranvier et al.1 Additionally, vascular invasion, lymph node metastases, or distant metastasis, which are the reliable criteria for malignancy of endocrine neoplasms, were not present in our case.
- Some immunohistochemical studies have been conducted to distinguish parathyroid carcinoma from benign masses. Loss of parafibromin expression, Rb expression, and galectin-3 overexpression distinguish parathyroid carcinoma from other parathyroid tumors.6 As in other studies that documented galectin-3 expression in some parathyroid adenomas and hyperplastic parathyroid glands,6-8 galectin-3 overexpression occurred in our case. However, this finding alone does not permit a malignant diagnosis.
- In conclusion, parathyromatosis must be considered in the differential diagnosis of a parathyroid tumor during clinical, radiological, and pathological evaluations. It is critical for the differential diagnosis to evaluate a tumor for any features that support a parathyroid carcinoma (infiltrative borders, lymphovascular invasion, and solitary nodules) or for the presence of metastatic disease. Patient history should also be reviewed for a previous parathyroid surgery.
DISCUSSION
- 1. Fernandez-Ranvier GG, Khanafshar E, Jensen K, et al. Parathyroid carcinoma, atypical parathyroid adenoma, or parathyromatosis? Cancer 2007; 110: 255–264. PMID: 17559137. ArticlePubMed
- 2. Matsuoka S, Tominaga Y, Sato T, et al. Recurrent renal hyperparathyroidism caused by parathyromatosis. World J Surg 2007; 31: 299–305. PMID: 17219279. ArticlePubMed
- 3. Barnes BA, Cope O. Carcinoma of the parathyroid glands: report of 10 cases with endocrine function. JAMA 1961; 178: 556–559. PMID: 13865086. ArticlePubMed
- 4. Baloch ZW, Fraker D, LiVolsi VA. Parathyromatosis as cause of recurrent secondary hyperparathyroidism: a cytologic diagnosis. Diagn Cytopathol 2001; 25: 403–405. PMID: 11747238. ArticlePubMed
- 5. Sokol MS, Kavolius J, Schaaf M, D'Avis J. Recurrent hyperparathyroidism from benign neoplastic seeding: a review with recommendations for management. Surgery 1993; 113: 456–461. PMID: 8456402. PubMed
- 6. Fernandez-Ranvier GG, Khanafshar E, Tacha D, et al. Defining a molecular phenotype for benign and malignant parathyroid tumors. Cancer 2009; 115: 334–344. PMID: 19107770. ArticlePubMed
- 7. Bergero N, De Pompa R, Sacerdote C, et al. Galectin-3 expression in parathyroid carcinoma: immunohistochemical study of 26 cases. Hum Pathol 2005; 36: 908–914. PMID: 16112008. ArticlePubMed
- 8. Saggiorato E, Bergero N, Volante M, et al. Galectin-3 and Ki-67 expression in multiglandular parathyroid lesions. Am J Clin Pathol 2006; 126: 59–66. PMID: 16753595. ArticlePubMed
References
Figure & Data
References
Citations
Citations to this article as recorded by 

- Intractable Parathyromatosis despite extensive surgical interventions: A case report with literature review
Shada Khaled Bashantoof, Mansoor Abdulmajeed Alramadhan, Modhi Hamad Alawadh, Nada Abdulaziz Bin Samaih, Rania Abdullah Alshammari, Abdulsalam Aodah
International Journal of Surgery Case Reports.2024; 114: 109172. CrossRef - Late recurrence of a single gland primary hyperparathyroidism—Atypical parathyroid adenoma or misdiagnosed parathyroid carcinoma
Jessica Kotliarevskaia, Udo Siebolts, Henning Dralle, Frank Schuppert
Clinical Case Reports.2024;[Epub] CrossRef - Retrosternal parathyromatosis in a patient with prior total parathyroidectomy
Tariq Saleh, Marwan Alaswad, Abdullah Otry, Waleed Saleh
Journal of Surgical Case Reports.2023;[Epub] CrossRef - Histological alterations following fine‐needle aspiration for parathyroid adenoma: Incidence and diagnostic problems
Mitsuyoshi Hirokawa, Ayana Suzuki, Miyoko Higuchi, Toshitetsu Hayashi, Seiji Kuma, Akihiro Miya, Akira Miyauchi
Pathology International.2021; 71(6): 400. CrossRef - Parathyromatosis as a cause of recurrence primary hyperparathyroidism: A case report
Elena A. Ilyicheva, Gleb A. Bersenev
International Journal of Surgery Case Reports.2021; 80: 105689. CrossRef - Seguridad y rendimiento diagnóstico de la medición de PTH en el lavado del aspirado de lesiones sospechosas de adenomas de paratiroides
Florentino Carral, Ana Isabel Jiménez, Mariana Tomé, Javier Alvarez, Ana Díez, Concepción García, Vicente Vega, Carmen Ayala
Endocrinología, Diabetes y Nutrición.2021; 68(7): 481. CrossRef - Safety and diagnostic performance of parathyroid hormone assay in fine-needle aspirate in suspicious parathyroid adenomas
Florentino Carral, Ana Isabel Jiménez, Mariana Tomé, Javier Alvarez, Ana Díez, Concepción García, Vicente Vega, Carmen Ayala
Endocrinología, Diabetes y Nutrición (English ed.).2021; 68(7): 481. CrossRef - Persistent secondary hyperparathyroidism caused by parathyromatosis and supernumerary parathyroid glands in a patient on haemodialysis
Jun Yang, Jun Zhang, Ning-hu Liu, Hao Liu, Meng-jie Dong
BMC Nephrology.2020;[Epub] CrossRef - Parathyromatosis: A Rare Case of Recurrent Hyperparathyroidism Localized by Four-Dimensional Computed Tomography
Abraham E. Wei, Matthew R. Garrett, Ankur Gupta
AACE Clinical Case Reports.2019; 5(6): e384. CrossRef - Parathyromatosis: a very rare cause of recurrent primary hyperparathyroidism – case report and review of the literature
M Haciyanli, S Karaisli, S Gucek Haciyanli, A Atasever, D Arikan Etit, EO Gur, T Acar
The Annals of The Royal College of Surgeons of England.2019; 101(8): e178. CrossRef - Parathyromatose : une cause rare d’hyperparathyroïdie récidivante
I. Achour, S. Charfi, M.A. Chaabouni, A. Chakroun, F. Guermazi, B. Hammami, A. Ghorbel
La Revue de Médecine Interne.2017; 38(1): 61. CrossRef - Recurrent primary hyperparathyroidism due to Type 1 parathyromatosis
Monica Jain, David L. Krasne, Frederick R. Singer, Armando E. Giuliano
Endocrine.2017; 55(2): 643. CrossRef

 E-submission
E-submission
 PubReader
PubReader Cite this Article
Cite this Article