Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(4); 2014 > Article
-
Brief Case Report
Heterotopic Pancreas in Omphalomesenteric Duct Remnant Results in Persistent Umbilical Discharge - Eunhyang Park, Hyojin Kim, Kyu Whan Jung1, Jin-Haeng Chung
-
Korean Journal of Pathology 2014;48(4):323-326.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.4.323
Published online: August 26, 2014
Department of Pathology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
1Department of Pediatric Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
- Corresponding Author: Jin-Haeng Chung, M.D. Department of Pathology, Seoul National University Bundang Hospital, 82 Gumi-ro 173beon-gil, Bundang-gu, Seongnam 463-707, Korea. Tel: +82-31-787-7713, Fax: +82-31-787-4012, 'chungjh@snu.ac.kr'
• Received: July 2, 2013 • Revised: September 3, 2013 • Accepted: September 10, 2013
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
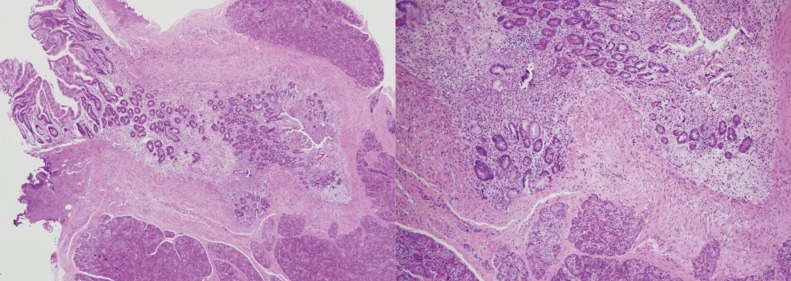
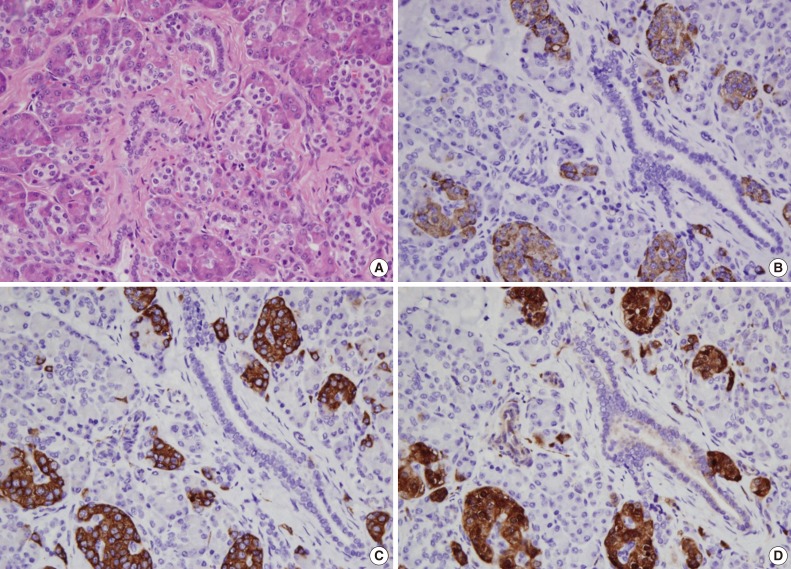
- A 3-month-old female infant presented with persistent umbilical discharge since birth. The infant was born through normal vaginal delivery following an uneventful gestational period and had no congenital anomalies. She had been gaining weight well and had no family history of genitourinary or gastrointestinal problems. Ultrasonography of the abdomen revealed an iso-echoic tract posterior to the umbilicus, and the diagnosis of urachal remnant was suspected. On physical examination, small droplets of clear fluid constantly discharged from a normal-looking umbilicus. Laboratory examination results were within normal limits. Under general anesthesia, an incision was made below umbilicus. Surgical exploration showed a fibrous sinus posterior to the umbilicus which was attached to the inner aspect of the umbilicus and the outer wall of the ileum by a fibrous band. Fibrous tissue was excised close to both ends, and the rest was ligated by suture tie. The excised specimen was a 7×6×5-mm-sized whitish fibrous tissue. Histologically, the excised specimen included pancreatic tissue with some small intestinal mucosa and fibrous extracellular components (Fig. 1). Both exocrine and endocrine pancreatic tissues were observed, including acini, ducts, and islets of Langerhans. Acini were separated into lobules by connective tissue. Intercalated ducts were lined by simple low cuboidal epithelium (Fig. 2). The patient was discharged without any postoperative complications and is currently alive without any sequelae.
CASE REPORT
- The omphalomesenteric duct is a long narrow tube that connects the yolk sac to the midgut lumen of the developing fetus. It normally regresses during the 5th to 9th weeks of fetal development, but a part or all of it may persist postnatally and result in various abnormalities including a Meckel's diverticulum, an umbilical fistula, an omphalomesenteric duct cyst, an umbilical sinus, or an umbilical polyp. Meckel's diverticulum often contains heterotopic gastric or pancreatic mucosa which can result in some clinical manifestations such as massive rectal bleeding. However, heterotopic tissue in other types of remnant omphalomesenteric duct which present on the umbilicus has been rarely reported. To our knowledge, there have been 13 cases of heterotopic pancreatic tissue in the umbilicus (Table 1).1,2,3,4
- Various explanations have been offered for heterotopic pancreas in the umbilicus, but there is no universally accepted theory about the cause of this aberrant tissue.5 The three influential pathogeneses include misplacement theory,6 in which embryonic tissue is located in an inappropriate place and develops into mature pancreatic tissue; metaplasia theory,7 stating that endodermal tissues migrate to the submucosa during embryogenesis and transform into pancreatic tissue; and the totipotent cell theory,8,9 in which totipotent endodermal cells lining the gut or omphalomesenteric duct differentiate into pancreatic tissue. The misplacement theory proposes that, during rotation of the foregut, several elements of the primitive pancreas become separated and eventually form mature pancreatic tissue along the length of the gastrointestinal tract. In this theory, the heterotopic rests are prone to drop off from the dorsal primordium and develop in the distal part of the stomach and proximal part of the duodenum, the most common sites of heterotopic pancreas. While it cannot explain other rarely discovered locations of heterotopic pancreas such as Meckel's diverticulum, ampulla of Vater, gallbladder, umbilicus, fallopian tube, and mediastinum, the totipotent cell theory is quite reliable for heterotopic pancreas in omphalomesenteric duct remnant because the cells lining the omphalomesenteric duct are known to pluripotent and can express either gastric, pancreatic, hepatic, or other terminal endoderm-derived phenotypes. While normal tissue is under the restriction to differentiate into certain cell types, tissue in this case seems to escape the normal restriction to maintain its pluripotent ability.
- Because preoperative diagnosis is still a challenge, primary treatment for umbilical discharge is silver nitrate application. However, if symptoms are persistent despite this intervention, other differential diagnoses like patent urachus and omphalomesenteric duct remnant should be considered for early and relevant management. If heterotopic tissue is present, as in the presented case, severe local excoriation can occur and may lead to severe complications when not treated appropriately. Limited local excision has been shown to be a safe and adequate procedure to address this affliction. Awareness of this finding in biopsy can aid with appropriate treatment decisions for the patient.
DISCUSSION
- 1. Harris LE, Wenzl JE. Heterotopic pancreatic tissue and intestinal mucosa in the umbilical cord. Report of a case. N Engl J Med 1963; 268: 721–722. PMID: 13952938. ArticlePubMed
- 2. Avolio L, Cerritello A, Verga L. Heterotopic pancreatic tissue at umbilicus. Eur J Pediatr Surg 1998; 8: 373–375. PMID: 9926310. ArticlePubMed
- 3. Lee WT, Tseng HI, Lin JY, Tsai KB, Lu CC. Ectopic pancreatic tissue presenting as an umbilcal mass in a newborn: a case report. Kaohsiung J Med Sci 2005; 21: 84–87. PMID: 15825694. ArticlePubMed
- 4. Sharma S, Maheshwari U, Bansal N. Ectopic pancreatic, gastric, and small intestine tissue in an umbilical polyp, causing persistent umbilical discharge in a 2 year old child: a rare case report. J Evol Med Dent Sci 2013; 2: 447–451. Article
- 5. Armstrong CP, King PM, Dixon JM, Macleod IB. The clinical significance of heterotopic pancreas in the gastrointestinal tract. Br J Surg 1981; 68: 384–387. PMID: 7237066. ArticlePubMed
- 6. Chandan VS, Wang W. Pancreatic heterotopia in the gastric antrum. Arch Pathol Lab Med 2004; 128: 111–112. PMID: 14692822. ArticlePubMedPDF
- 7. Gupta MK, Karlitz JJ, Raines DL, Florman SS, Lopez FA. Clinical case of the month. Heterotopic pancreas. J La State Med Soc 2010; 162: 310–313. PMID: 21294486. PubMed
- 8. Baysoy G, Balamtekin N, Uslu N, Karavelioğlu A, Talim B, Ozen H. Double heterotopic pancreas and Meckel's diverticulum in a child: do they have a common origin? Turk J Pediatr 2010; 52: 336–338. PMID: 20718198. PubMed
- 9. Bossard P, Zaret KS. Repressive and restrictive mesodermal interactions with gut endoderm: possible relation to Meckel's diverticulum. Development 2000; 127: 4915–4923. PMID: 11044405. ArticlePubMedPDF
References
Fig. 1Pancreatic tissue (upper and lower) with some small intestinal mucosa (middle) and fibrous extracellular components.
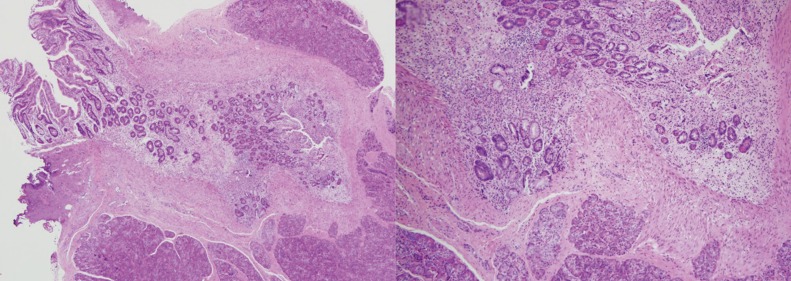
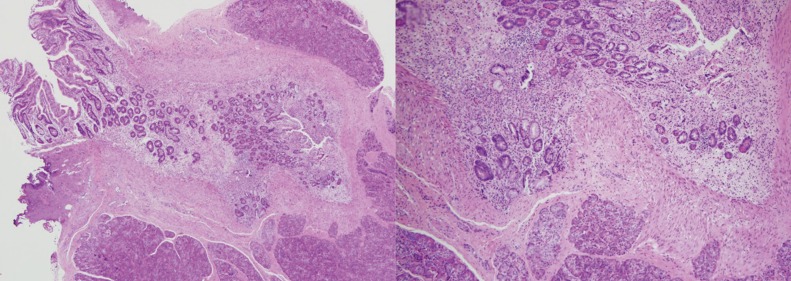
Fig. 2Acini are separated into lobules by connective tissue, and intercalated ducts are lined with simple low cuboidal epithelium. Pancreatic tissue including acini, ducts, and islets of Langerhans (A). Expression of chromogranin (B), synaptophysin (C), and neuron-specific enolase (D) in islets of Langerhans.
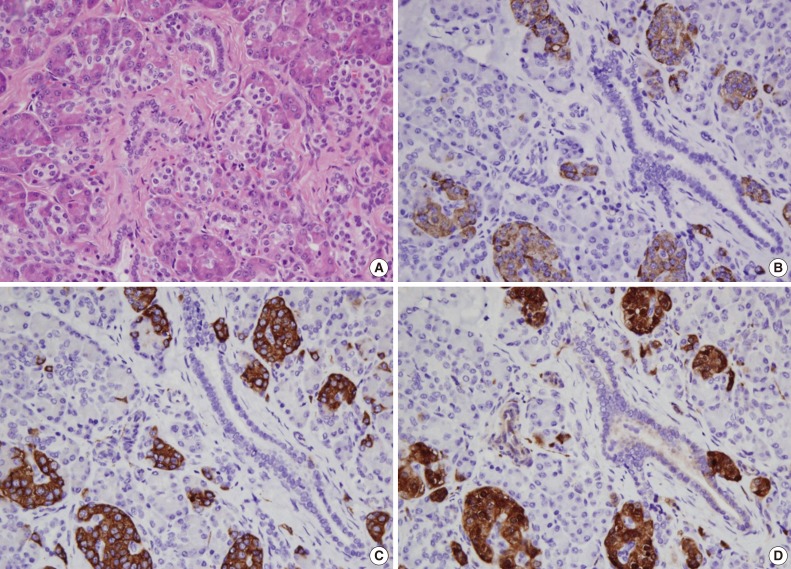
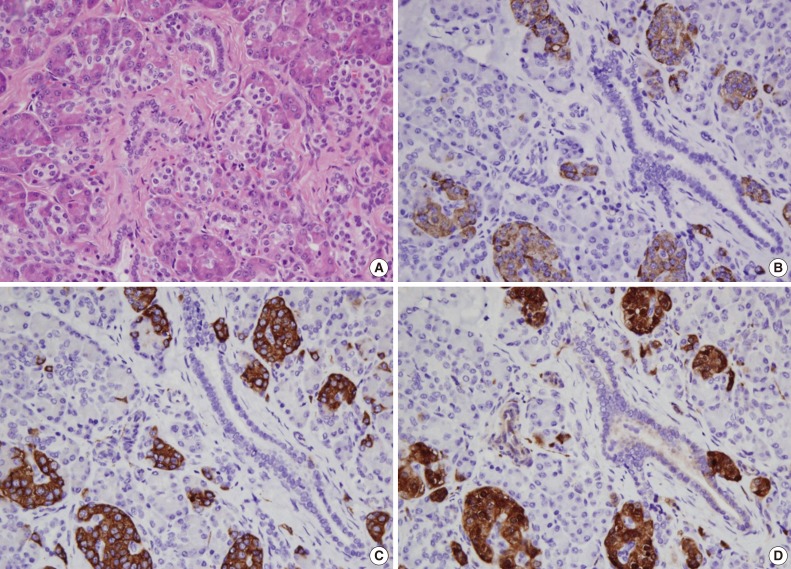
Table 1.Cases of heterotopic pancreatic tissue at the umbilicus reported in the English literature
| No. | Age/Sex | Mass | Discharge | Size | Site | Reference |
|---|---|---|---|---|---|---|
| 1 | 12 yr/F | N/A | N/A | N/A | Umbilical subcutaneous tissue | Wright (1900), cited by Harris and Wenzl [1] |
| 2 | 22 yr/M | – | + | N/A | Umbilical cyst | Trimingham (1943), cited by Harris and Wenzl [1] |
| 3 | 6 mo/M | – | N/A | 3-mm nodule | Umbilical nodule | Steck and Helwig (1964), cited by Avolio et al. [2] |
| 4 | 13 mo/M | + | + | 12 × 9 × 5 mm | Umbilical mass | Caberwal et al. (1977), cited by Avolio et al. [2] |
| 5 | 60 yr/M | + | – | N/A | Umbilical polyp | Kondoh et al. (1994), cited by Avolio et al. [2] |
| 6 | 8 mo/M | +/– | + | N/A | Umbilical mass | Avolio et al. [2] (1998) |
| 7 | 15 mo/M | – | + | N/A | Umbilical mass | Avolio et al. [2] (1998) |
| 8 | 6 mo/M | – | + | N/A | Urachus | Perez-Martinez et al. (1999), cited by Lee et al. [3] |
| 9 | 3 mo/M | – | + | 1-cm cyst | Umbilical cyst | Tan et al. (2000), cited by Lee et al. [3] |
| 10 | 7 wk/M | – | + | N/A | Umbilical cyst | Tan et al. (2000), cited by Lee et al. [3] |
| 11 | 8 days/M | + | + | 26 × 20 × 7 mm | Umbilical mass | Lee et al. [3] (2005), |
| 12 | 18 mo/M | + | + | N/A | Umbilical mass | Silva et al. (2010), cited by Sharma et al. [4] |
| 13 | 2 yr/M | + | + | 12 × 12 × 10 cm | Umbilical mass | Sharma et al. (2013), cited by Sharma et al. [4] |
| 14 | 3 mo/F | – | + | 7 × 6 × 5 mm | Umbilical cyst | Present case |
Figure & Data
References
Citations
Citations to this article as recorded by 

- Heterotopic Pancreas Mimicking Metastases From Renal Carcinoma
Deepanksha Datta, Rajesh Kumar, Peeyush Varshney, Sudeep Khera, Tanisha Gupta
Clinical Nuclear Medicine.2023; 48(2): e74. CrossRef - Amylase Levels Are Useful for Diagnosing Omphalomesenteric Cysts: A Case Report
Hiroko Yoshizawa, Keita Terui, Mitsuyuki Nakata, Tetsuya Mitsunaga, Shugo Komatsu, Takeshi Saito, Tomoro Hishiki
Pediatric Reports.2022; 14(1): 127. CrossRef - Persistent umbilical polyp in a 5-year-old boy – A rare case report with literature review
Asitava Deb Roy, Ritu Roy, Shilpa
IP Archives of Cytology and Histopathology Research.2022; 7(2): 126. CrossRef - Ectopic pancreas
Fang-Chin Hsu, Hai-Ning Hsu, Yi-Jen Peng, Kuo-Feng Hsu
Formosan Journal of Surgery.2021; 54(6): 244. CrossRef - Heterotopic Pancreas Located at the Gastroesophageal Junction in a Hiatal Hernia: A Case Report
Joshua K Jenkins, Forest Smith, Stephen Mularz, Shweta Chaudhary
Cureus.2021;[Epub] CrossRef - Loss of GATA4 causes ectopic pancreas in the stomach
Elisa Rodríguez‐Seguel, Laura Villamayor, Noelia Arroyo, Mónica P De Andrés, Francisco X Real, Franz Martín, David A Cano, Anabel Rojas
The Journal of Pathology.2020; 250(4): 362. CrossRef - Bleeding Umbilical Papule: Answer
Cuong V. Nguyen, Patrick J. McMahon, Ata S. Moshiri, Tricia R. Bhatti, Adam I. Rubin
The American Journal of Dermatopathology.2020; 42(3): 224. CrossRef - Atypical presentations of ectopic pancreatic tissue
P.S. Sulser, S. Azarhoush, D.C. Aronson, S.J. Tharakan, N. Zweifel, U. Moehrlen
Journal of Pediatric Surgery Case Reports.2020; 58: 101450. CrossRef - Intramural ectopic pancreatic tissue of the stomach: A case report of an uncommon origin of a non-cancerous gastric tumour
Enrica Chiriatti, Paulina Kuczma, Domenico Galasso, E. Koliakos, Edgardo Pezzetta, Olivier Martinet
International Journal of Surgery Case Reports.2020; 73: 48. CrossRef - Surgical abdominal exploration in children with umbilical ectopic gastrointestinal tissue
Yi-Li Hou, Jao-Yu Lin
Journal of Pediatric Surgery Case Reports.2019; 49: 101281. CrossRef - Rare case of ectopic pancreas presenting with persistent umbilical discharge
Kazuhiko Nakame, Roko Hamada, Masaya Suzuhigashi, Atsushi Nanashima, Satoshi Ieiri
Pediatrics International.2018; 60(9): 891. CrossRef - Heterotopic Pancreas: Histopathologic Features, Imaging Findings, and Complications
Maryam Rezvani, Christine Menias, Kumaresan Sandrasegaran, Jeffrey D. Olpin, Khaled M. Elsayes, Akram M. Shaaban
RadioGraphics.2017; 37(2): 484. CrossRef - Heterotopic pancreas in the omphalomesenteric duct remnant in a 9-month-old girl: a case report and literature review
Zitong Zhao, Chiang Khi Sim, Sangeeta Mantoo
Diagnostic Pathology.2017;[Epub] CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure

 E-submission
E-submission